Abstract
H5N1 influenza viruses are capable of causing severe disease and death in humans, and represent a potential pandemic subtype should they acquire a transmissible phenotype. Due to the expanding host and geographic range of this virus subtype, there is an urgent need to better understand the contribution of both virus and host responses following H5N1 virus infection to prevent and control human disease. The use of mammalian models, notably the mouse and ferret, has enabled the detailed study of both complex virus–host interactions as well as the contribution of individual viral proteins and point mutations which influence virulence. In this review, we describe the behavior of H5N1 viruses which exhibit high and low virulence in numerous mammalian species, and highlight the contribution of inoculation route to virus pathogenicity. The involvement of host responses as studied in both inbred and outbred mammalian models is discussed. The roles of individual viral gene products and molecular determinants which modulate the severity of H5N1 disease in vivo are presented. This research contributes not only to our understanding of influenza virus pathogenesis, but also identifies novel preventative and therapeutic targets to mitigate the disease burden caused by avian influenza viruses.
Keywords: Influenza, H5N1, Pathogenesis, Mice, Mammalian, Ferret, Avian influenza
1. Introduction
Avian influenza viruses represent a persistent threat to public health. Wild aquatic birds, the reservoir for all influenza A viruses, harbor numerous virus subtypes to which humans have little to no preexisting immunity. Among these, H5, H7, and H9 avian influenza viruses have been found to circulate in domestic poultry, causing human disease and further increasing the risk of human exposure to these subtypes (Abdel-Ghafar et al., 2008; Belser et al., 2009a; Peiris et al., 1999). As previous pandemic viruses have derived from avian host origins, understanding the pathogenicity of avian influenza viruses in mammalian species is critical to predict the pandemic potential of these viruses (Garten et al., 2009). Should an avian virus to which humans lack neutralizing antibody acquire the ability to cause illness in humans and possess the capacity for sustained human-to-human transmission, a pandemic could result.
Since 2003, there have been over 600 documented cases of human infection with H5N1 viruses, with most cases among young, previously healthy individuals (WHO, 2013). Severe cases have been distinguished by high viral load and intense inflammatory responses, progressing to severe pneumonia, acute respiratory distress syndrome and death; the fatality rate is approximately 60% (Abdel-Ghafar et al., 2008; de Jong et al., 2006; WHO, 2013). While the majority of documented cases of H5N1 infection represent severe illnesses, milder cases have also been reported; based on limited seroepidemiologic studies, additional undocumented mild or asymptomatic cases have likely occurred (Abdel-Ghafar et al., 2008). Most cases of H5N1 human infection have occurred following exposure to H5N1 virus-infected poultry, however selected reports of familial clusters suggest a host genetic component in susceptibility (Kandun et al., 2006; Olsen et al., 2005). Collectively, these epidemiologic studies support the existence of H5N1 viruses of varying virulence in humans, with an additional role for host factors in the resulting course of illness. There is an urgent need to study the contribution of both virus and host responses following H5N1 virus infection to improve our ability to both prevent and control human disease.
Mammalian models have become invaluable for the study of H5N1 virus pathogenicity. The intravenous pathogenicity index (IVPI), which classifies avian influenza viruses as high or low pathogenicity in 6-week-old chickens, does not reflect the pathogenesis of these viruses in mammals (WHO, 2002). Clinical and epidemiological data collected from human cases does not provide a biological or molecular basis of virus pathogenicity in humans. Furthermore, only the use of well-characterized laboratory models can provide the ability to study the contribution of individual viral genes and/or point mutations as well as complex virus–host interactions. While the mouse and ferret represent the mammalian models most typically used for the study of H5N1 virus pathogenesis, and whose use has enabled much of our understanding of viral pathogenesis discussed in this review, they are among several species which support influenza virus replication and are employed in the laboratory. As will be described below, each model possesses its own set of advantages and limitations, which include distribution patterns of cellular receptors, presentation of clinical signs and symptoms during acute infection, cost and size considerations, a well-characterized genome, and availability of species-specific reagents. The use of these models has provided a greater understanding of the pathogenicity of avian influenza viruses in mammals as well as the molecular determinants which confer a high virulence phenotype, information which is vitally needed in public health response to H5N1 virus infection in humans.
2. H5N1 viral pathogenesis in mice
2.1. Viral pathogenesis following intranasal inoculation
Despite several limitations, mice have traditionally been the most common mammalian model used for the study of influenza virus pathogenesis due to their small size, low cost, easy husbandry and well-characterized genetics. While avian influenza viruses typically replicate efficiently in mouse lungs without prior adaptation, the relative paucity of α(2-6)-linked sialic acids (SA) in murine respiratory tissues limits the ability to study many human influenza viruses which possess this receptor binding preference (Ibricevic et al., 2006; van Riel et al., 2006). Furthermore, H5N1 virus attachment in the mouse is most abundant in tracheal cells, becoming progressively weaker toward the alveoli, opposite to the pattern of virus attachment with this virus subtype in humans (van Riel et al., 2007). Unlike humans, mice do not run fevers or develop easy-to-measure respiratory clinical signs following influenza virus infection. However, mice display numerous physical signs of illness (including weight loss, ruffled fur, and lethargy) that can be used as measurable outcomes and markers of virulence depending on the strain used to infect. Furthermore, the temporal association between virus replication and symptom onset, lung pathology, and induction of innate immune responses in the mouse lead this model to be frequently used for studies of influenza virus pathogenesis (Conn et al., 1995; Hennet et al., 1992).
Like most avian influenza viruses, H5N1 subtype viruses are highly infectious in mice and typically replicate to high titer in murine lungs following intranasal (i.n.) inoculation (Gao et al., 1999; Gubareva et al., 1998; Lu et al., 1999; Maines et al., 2005). Depending on the strain, H5N1 viruses generally fall into either a high or low pathogenicity phenotype in this species (Gao et al., 1999; Katz et al., 2000; Maines et al., 2005). While maintaining a high degree of infectivity, viruses of low virulence cause mild to modest weight loss (generally <15% of pre-inoculation body weight), are typically restricted to replication in respiratory tract tissues, and usually clear by days 7–9 post-inoculation (p.i.) (Maines et al., 2005). In contrast, infection with highly virulent viruses leads to pronounced morbidity, systemic spread of virus, cytokine dys-regulation, severe tissue pathology, and death (Maines et al., 2005). Infectious virus is frequently detected in the brains of mice infected with highly virulent H5N1 viruses, with elevated levels of numerous proinflammatory cytokines and chemokines also induced in this tissue (Park et al., 2002; Tanaka et al., 2003; Tumpey et al., 2000). However, select H5N1 viruses can cause lethality in mice in the absence of extrapulmonary virus detection (Tumpey et al., 2002).
Numerous parameters contribute to the virulence of H5N1 viruses in the mouse model. H5N1 viral load in the lungs of mice has been associated with disease severity (Boon et al., 2011; Hatta et al., 2010). Highly virulent viruses induce greater levels of apoptosis in the lung and spleen following infection and cause a significant reduction in the number of circulating lymphocytes in peripheral blood (Maines et al., 2005; Tumpey et al., 2000). Lymphocyte destruction and diminished expression of chemotactic factors can lead to reduced migration of immune cells to infected lung tissue, prolonging the viral infection and contributing to virus-induced pathology (Katz et al., 2000; Tumpey et al., 2000). Furthermore, exacerbated proinflammatory cytokine responses are frequently detected during severe H5N1 virus infection in mice, contributing to tissue pathology and fatal outcomes (Maines et al., 2008; Szretter et al., 2007). There is considerable variation among inbred mouse strains to H5N1 virus susceptibility and disease severity, indicating that host genetic components additionally contribute to H5N1 pathogenesis in mammals, as will be discussed in more detail in subsequent sections (Boon et al., 2011).
2.2. Viral pathogenesis following alternate inoculation routes
While intranasal administration of a liquid inoculum is the traditional method for assessment of influenza virus pathogenicity in mammalian species, it does not encapsulate all potential routes of exposure which can result in human disease (Fig. 1). Use of the mouse model to evaluate alternate inoculation routes capable of causing a productive infection has allowed for a greater understanding of the capacity of H5N1 viruses to cause disease and death. Notably, conjunctivitis and other ocular complications following influenza virus infection in humans are most frequently associated with the H7 subtype, but have been documented rarely during H5N1 virus infection (Belser et al., 2009a). Furthermore, the presence of SA on the corneal surface and linkage of ocular and respiratory tract tissues by the nasolacrimal ducts identifies the ocular system as both a potential site of replication as well as a route of entry to establish a respiratory infection (Kumlin et al., 2008). Although H5N1 viruses do not demonstrate a particular tropism for this tissue, ocular inoculation (with or without prior corneal scarification) of mice with H5N1 viruses resulted in a systemic infection, with infectious virus recovered from the lungs, brain, and eye of mice p.i. (Belser et al., 2009b; Sun et al., 2009). Selected H5N1 viruses were capable of mounting a lethal infection by this route, albeit with a 2–3 delay in mortality compared with i.n. inoculation (Belser et al., 2009b).
Fig. 1.
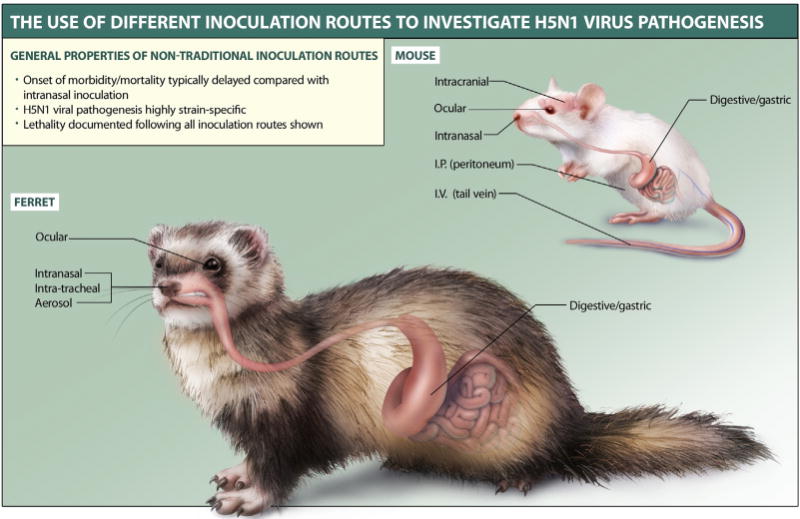
The use of different inoculation routes to investigate H5N1 virus pathogenesis. H5N1 viruses are capable of causing systemic and lethal disease following multiple inoculation routes in mammalian models. Mouse studies represented in this illustration: Belser et al. (2009b), Bright et al. (2003), Lipatov et al. (2009), Lu et al. (1999) and Sun et al. (2009). Ferret studies represented in this illustration: Belser et al. (2012), Bodewes et al. (2011), Gustin et al. (2011a), Lednicky et al. (2010), Lipatov et al. (2009), Maines et al. (2005) and Shinya et al. (2011b).
The detection of H5N1 virus in raw meat from land-based poultry has raised concerns regarding the ability of this virus subtype to cause disease following digestive exposure (Swayne, 2006; Tumpey et al., 2002). H5N1 subtype viruses shown to cause severe disease and death following i.n. inoculation in mice exhibited a range of pathogenicies following intragastric (i.g.) inoculation in this species (Lipatov et al., 2009). Select H5N1 viruses were capable of systemic spread and lethality, with infectious virus detected in the lungs, brain, and intestine following i.g. challenge. While the transmission of avian influenza viruses to humans via the consumption of contaminated poultry products is considered unlikely, evaluation of this inoculation route nonetheless provides a greater understanding of this property, especially given the detection of H5N1 viruses in poultry and egg products (Chmielewski and Swayne, 2011).
The mouse has been further employed to evaluate the ability of H5N1 viruses to cause disease following direct introduction in discrete organ systems. Systemic spread of virus was detected following intraperitoneal (i.p.) challenge with H5N1 virus, although infectious virus in the brain was not detected (Sun et al., 2009). Intravenous (i.v.) inoculation with H5N1 viruses resulted in a systemic and fatal infection of mice (Bright et al., 2003). H5N1 viruses also caused fatal infections in the mouse following intracranial (i.c.) inoculation, with detection of systemic spread of virus beyond the inoculated tissue with some strains (Bright et al., 2003). Collectively, these studies demonstrate that H5N1 viruses are capable of causing severe disease and death following numerous routes of entry to the experimental host.
3. H5N1 viral pathogenesis in ferrets
3.1. H5N1 viruses of low virulence
The high susceptibility of ferrets (Mustela putorius furo) to influenza virus infection was identified shortly after first isolation of the virus (Shope, 1934). The ferret has proved to be an attractive mammalian model for the study of influenza virus pathogenesis as, unlike mice, this species emulates numerous clinical features associated with human disease, including sneezing, fever, and nasal discharge (Belser et al., 2011b). Furthermore, similarities between ferret and human lung physiology allow for a greater extrapolation of experimental results to humans. Like humans, ferrets possess a predominance of α(2-6)-linked SA on upper airway epithelia, and avian and human influenza virus subtypes exhibit comparable patterns of virus attachment to respiratory tract tissues of both species (Maher and DeStefano, 2004; van Riel et al., 2006, 2007). As a result, ferrets support the efficient replication of human and avian influenza viruses following intranasal inoculation without prior adaptation.
Generally, ferret infection with human influenza viruses and low pathogenic avian influenza (LPAI) viruses of the H6, H7, and H9 subtypes presents as a mild, transient illness (Fig. 2) (Belser et al., 2007; Gillim-Ross et al., 2008; Smith and Sweet, 1988; Wan et al., 2008; Zitzow et al., 2002). Despite their classification as highly pathogenic avian influenza (HPAI) viruses, it is not atypical for H5N1 viruses to exhibit a similarly mild infection following i.n. inoculation in ferrets. Ferret infection with H5N1 viruses of low virulence is typically characterized by fever, mild to modest weight loss (<15% of pre-inoculation body weight), relatively mild lethargy and minimal clinical signs (Govorkova et al., 2005; Imai et al., 2010; Lu et al., 2003; Maines et al., 2005; Yen et al., 2007b). Lymphopenia in peripheral blood is transient, and neurological complications and death are rare (Maines et al., 2005). Ferrets return to pre-inoculation body weight and activity levels by 14 days p.i.
Fig. 2.
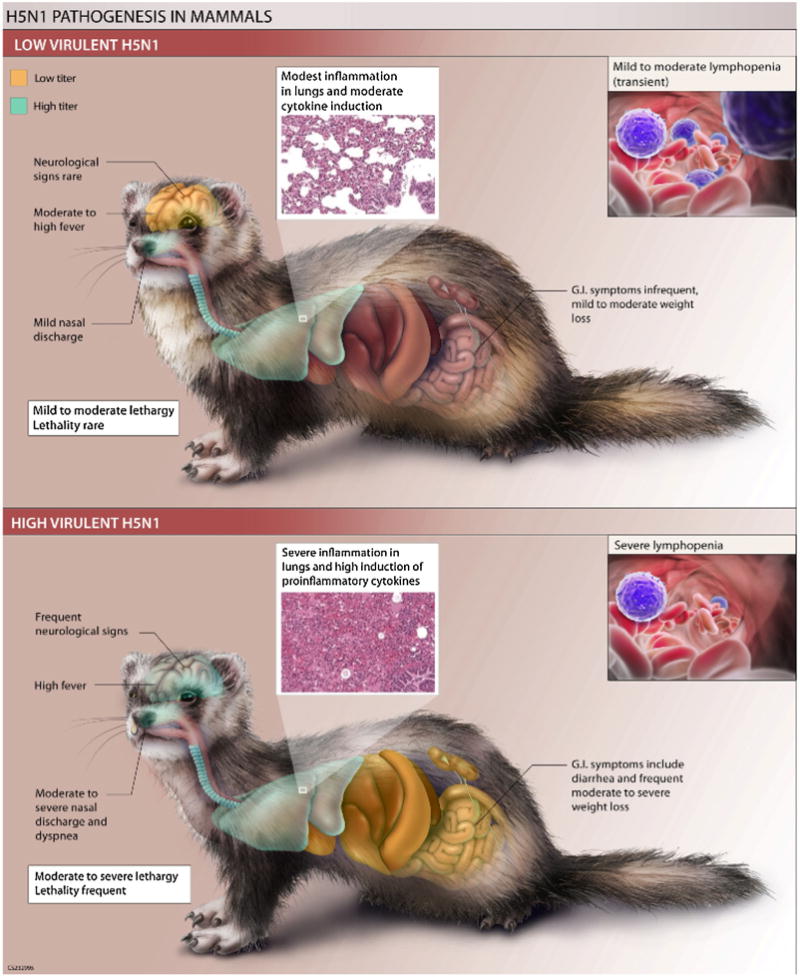
H5N1 pathogenesis in mammals. Virus and host features associated with H5N1 viruses which exhibit low or high virulence in the ferret model. Inset of lung histopathology is from Maines et al. (2005). Low titer generally represents ≤103 EID50/g or ml, high titer generally represents ≥105 EID50/g or ml (Maines et al., 2005).
H5N1 viruses which exhibit low virulence in the ferret model replicate to moderate titer (peak mean titers generally ~105 EID50/ml) in the nasal cavities of ferrets through day 5 p.i. but typically clear infection at/around day 7 p.i., similar to human influenza viruses in this model (Maines et al., 2005). However, unlike H1N1 and H3N2 subtype viruses, H5N1 viruses of low virulence in the ferret model are capable of efficient replication throughout the respiratory tract, with infectious virus frequently detected in the trachea and lungs of ferrets by day 3 p.i. (Maines et al., 2005). Despite the presence of viral antigen in the lung, macroscopic pulmonary discoloration in these ferrets is mild, with only localized inflammation present during acute infection. With the exception of virus detected in the olfactory bulb of the brain following i.n. inoculation with both avian and human influenza viruses (likely due to the proximity of high titers of infectious virus in the nasal turbinates), H5N1 viruses of low virulence in ferrets generally do not spread to extra-pulmonary tissues (Govorkova et al., 2005; Maines et al., 2005; Zitzow et al., 2002). Inflammation in the brain is not typically associated with infection with these viruses, and viral antigen is not consistently detected in this tissue (Maines et al., 2005).
3.2. Highly virulent H5N1 viruses
While not universal among all viruses in this subtype, HPAI H5N1 viruses have the capacity to cause severe and fatal disease in ferrets (Fig. 2). This severe disease is typically characterized by the presence of numerous clinical features, including fever, nasal discharge, lethargy, anorexia, diarrhea, and dyspnea, with pronounced weight loss (>15% of preinfection body weight) (Govorkova et al., 2005; Maines et al., 2005; Zitzow et al., 2002). Inoculation with highly virulent H5N1 viruses in the ferret often leads to a fatal infection; depending on the isolate, ferrets die during the acute phase of infection (typically days 5–7 p.i.) in the absence of neurological dysfunction, or develop neurological symptoms (typically days 7–13 p.i.) necessitating euthanasia (Maines et al., 2005). It should be noted that due to strain-specific differences and the outbred nature of ferrets, not all highly virulent H5N1 viruses which cause severe disease in ferrets result in 100% lethality of inoculated animals (Gustin et al., 2011b; Imai et al., 2010; Maines et al., 2005; Song et al., 2009).
Laboratory abnormalities in hematologic and serum chemistry parameters frequently observed in severe human cases of H5N1 virus infection are also detected in the ferret model (Abdel-Ghafar et al., 2008; Belser et al., 2011a; Yuen et al., 1998; Zitzow et al., 2002). Infection with highly virulent H5N1 viruses in ferrets can cause pronounced lymphocyte depletion in peripheral blood (as high as >75% reduction of lymphocytes compared with preinfection levels), in addition to leukopenia and thrombocytopenia (Belser et al., 2011a; Maines et al., 2005). Severe H5N1 disease in ferrets has further been shown to result in alterations to numerous blood chemistry parameters, indicative of multi-organ dysfunction (Belser et al., 2011a). Among these are atypical levels of alanine aminotransferase, amylase, and albumin, all of which have been reported among severe cases of H5N1 infection in humans (Kandun et al., 2006; Oner et al., 2006).
H5N1 viruses associated with severe disease in ferrets replicate to high titer in the nasal cavities of ferrets, with infectious virus persisting in the upper respiratory tract through day 7 p.i. (Maines et al., 2005). Like H5N1 viruses of low virulence in this model, highly virulent H5N1 viruses replicate efficiently throughout the respiratory tract, but are detected at higher titer than less virulent viruses. The pattern of H5N1 virus attachment in ferret respiratory tract tissues closely mirrors that of humans, with greatest attachment in the alveoli and bronchioles (van Riel et al., 2007). However, infection with highly virulent H5N1 viruses results in severe macroscopic pathology and diffuse interstitial inflammation in pulmonary tissues, with more severe lesions present in the alveoli and bronchioles compared with the trachea and bronchi (Maines et al., 2005; van den Brand et al., 2010). Bronchopneumonia and acute bronchiolitis are detected as early as day 1 p.i. in H5N1 virus-infected ferrets (Zitzow et al., 2002). Systemic spread of virus is common, with infectious virus detected in peripheral blood, spleen, liver, and intestine, among other organs (Govorkova et al., 2005; Maines et al., 2005).
Detection of virus in cerebrospinal fluid and development of acute encephalitis in isolated cases of severe H5N1 infection in humans indicates a role for neurologic involvement in H5N1 pathogenesis (Abdel-Ghafar et al., 2008; de Jong et al., 2005). Infectious virus and viral antigen are detected in the olfactory bulb and brain of ferrets infected with highly virulent H5N1 viruses, with neurons representing the major cell type infected in the central nervous system (Maines et al., 2005; Peng et al., 2012; Rowe et al., 2003). Viral load in the ferret brain has been shown to correlate with the severity of meningoencephalitis; high viral titers and inflammatory lesions in the brain can be detected by days 3–4 p.i., with widely distributed lesions present by days 5–6 p.i. (Peng et al., 2012). While the precise route of virus entry to the brain has yet to be elucidated, the olfactory system is a likely source of virus for brain invasion in ferrets infected with highly virulent H5N1 viruses, with entry via cranial nerve pathways or the brain vasculature also possible following disruption of the blood–brain barrier (Peng et al., 2012; Shinya et al., 2011a; Yamada et al., 2012).
3.3. H5N1 viral pathogenesis following alternate inoculation routes
As ferrets share a greater number of clinical signs and symptoms with humans following influenza virus infection compared with mice, use of the ferret model has provided additional insight in elucidating the role of inoculation volume and route on virus pathogenicity. While the studies discussed above represent i.n. inoculation using a liquid virus suspension, modulation of the volume used during i.n. inoculation of ferrets can result in divergent disease profiles (Fig. 1). Compared with the 1 ml volume of inoculum which is frequently used during i.n. inoculation, a reduction in volume to 500 l or even 100 l can limit the respiratory tract tissues exposed to virus during the initial inoculation (Belser et al., 2012; Bodewes et al., 2011). These studies demonstrate that the appropriate choice of inoculation method can greatly influence the resulting disease in ferrets.
While i.n. inoculation using a liquid virus suspension is the standard method for virus inoculation in ferrets, it does not accurately model the inhalation of small (<5 m) particles suspended in the air which represents a more natural route of virus transmission between humans. Furthermore, standard i.n. inoculation may result in the animal swallowing a portion of the inoculum, diverting the inoculum away from the respiratory tract. Recent advances in the generation and characterization of aerosolized virus particles in the laboratory have allowed for the establishment of aerosol methods of inoculation in the ferret to more closely model natural influenza virus infections in this model (Gustin et al., 2011a). Inoculation of ferrets by inhalation of aerosolized H5N1 virus resulted in a lethal infection, with systemic spread of virus detected p.i. (Gustin et al., 2011a; Lednicky et al., 2010). However, aerosol inoculation resulted in more gradual progress of disease compared with i.n. delivery, likely attributable to differences in virus dissemination (Gustin et al., 2011a).
Use of the ferret model has demonstrated the capacity of H5N1 viruses to cause severe disease in the absence of standard i.n./inhalation inoculation. Similar to studies performed in mice, H5N1 viruses are capable of maintaining a lethal phenotype following ocular inoculation in ferrets (Belser et al., 2009b, 2012). While there is a 2–3 day delay in onset of morbidity and mortality following ocular inoculation compared with i.n. administration of virus, comparable viral titers were detected in both respiratory tract and extrapulmonary tissues at time of death. In contrast to the mouse model, i.g. challenge with H5N1 virus in a liquid medium in ferrets did not result in a productive infection, likely due to inactivation of virus in the stomach before reaching the intestines (Lipatov et al., 2009). However, consumption of H5N1 virus-infected chicken tissues by ferrets lead to either mild respiratory disease (likely initiated in pharyngeal tissues in contact with virus-infected meat during consumption) or systemic disease (representing virus spread from the alimentary tract via the intestinal lymphatic system resulting in subsequent systemic circulation), depending on the virus strain used (Lipatov et al., 2009; Shinya et al., 2011b). This work highlights the ability of H5N1 viruses to cause varying disease profiles depending on the site of initial virus infection, and underscores the importance of choosing the appropriate method of inoculation when establishing an experimental design in the laboratory.
4. H5N1 viral pathogenesis in other mammalian models
While the mouse and ferret represent the mammalian models most frequently employed in the laboratory to study H5N1 virus pathogenicity, many other species have also been examined. This work has allowed for a greater understanding of the potential for H5N1 viruses to cause disease in a range of non-human hosts as well as providing for an assessment of the susceptibility of several mammalian species which are routinely handled as domestic animals or which pose a potential occupational hazard for individuals in close contact with these species.
The guinea pig has emerged as an alternate small mammalian model for the study of influenza viruses, notably with regard to the evaluation of virus transmissibility and the contribution of environmental factors on this property (Lowen et al., 2007). However, guinea pigs lack many of the clinical signs of infection seen in humans following influenza virus infection, and H5N1 viruses generally do not maintain a virulent phenotype in this species despite detection of infectious virus throughout the respiratory tract and the detection of bronchointerstitial pneumonia p.i. (Gao et al., 2009; Kwon et al., 2009; Steel et al., 2009a; Van Hoeven et al., 2009). While H5N1 viruses do not transmit efficiently from infected to naïve animals in the ferret model, guinea pigs inoculated with H5N1 viruses were capable of virus transmission when placed in direct contact with naïve animals (Gao et al., 2009; Steel et al., 2009a). Similar to studies in the ferret, i.g. inoculation of guinea pigs with H5N1 virus suspended in a liquid inoculum did not result in a productive infection (Kwon et al., 2009; Lipatov et al., 2009).
Non-human primates offer the advantage of a higher order species, but are only infrequently used in studies of H5N1 viral pathogenesis due to practical and ethical constraints. Cynomolgus macaques inoculated with H5N1 virus presented with numerous clinical signs of disease p.i., including coughing, fever, anorexia, and lethargy, leading to severe respiratory illness (Rimmelzwaan et al., 2001). Infectious virus was detected throughout the respiratory tract of these animals, as supported by the observation of severe necrotizing bronchointerstitial pneumonia, but virus was not isolated from the cerebellum or cerebrum in multiple studies (Kuiken et al., 2003; Rimmelzwaan et al., 2001; Ruat et al., 2008). Similar results highlighting the efficient replication of H5N1 virus in the lower respiratory tract in the absence of extrapulmonary virus detection were observed in rhesus macaques (Chen et al., 2009; Fan et al., 2009b). H5N1 virus replication in the upper respiratory tract of non-human primates in the absence of severe disease has also been reported, indicating strain-specific differences in virus pathogenicity in this species; similar to the guinea pig model discussed above, H5N1 viruses are typically nonlethal in non-human primates (Itoh et al., 2008; Van Hoeven et al., 2009). These studies have proven valuable in assessing vaccine efficacy to mitigate viral replication and pulmonary damage following H5N1 viral challenge, but studies of viral pathogenesis remain limited in comparison to more widely available models (Fan et al., 2009b; Itoh et al., 2008; Ruat et al., 2008). However, with high physiologic similarity with humans, the non-human primate model has been utilized for studies of system biology and the evaluation of host responses following H5N1 virus infection and nonlethal viral pneumonia, as will be discussed in the subsequent section (Baskin et al., 2009; Cilloniz et al., 2009; Li et al., 2011b; McDermott et al., 2011; Shinya et al., 2012a; Tolnay et al., 2010).
Companion animals are not frequently used in laboratory settings to study influenza virus pathogenesis, but the potential for infection of dogs and cats with H5N1 virus (most likely following consumption of virus-infected poultry carcasses) and the resulting potential for viral adaptation or subsequent transmission to humans warrants closer study of H5N1 virus infection in these species (Harder and Vahlenkamp, 2010). Despite the emergence of H3N8 canine influenza viruses in 2004, it is generally believed that species barriers restrict the permissiveness of dogs to influenza virus infection (Crawford et al., 2005; Harder and Vahlenkamp, 2010). Following the isolation of an H5N1 virus which caused a fatal infection of a dog in Thailand, this species was more closely examined for the ability to support H5N1 virus infection, with strain-specific results (Songserm et al., 2006). Infectious virus was detected in respiratory samples collected from beagles inoculated with H5N1 virus but animals were generally asymptomatic aside from a transient rise in body temperature in two studies (Giese et al., 2008; Maas et al., 2007). However, severe disease following H5N1 virus inoculation was detected in a separate study, with infected beagles presenting with fever, anorexia, diarrhea; infectious virus was recovered from respiratory tract samples only (Chen et al., 2010b). The detection of infectious virus recovered from both upper and lower respiratory tract samples was in accordance with patterns of virus attachment demonstrating that H5N1 virus binds to α(2-3) linked SA distributed throughout the upper and lower respiratory tract of dogs (Chen et al., 2010b; Maas et al., 2007).
While felids are not generally considered susceptible to influenza virus infection, reports of lethal H5N1 disease in domestic cats, tigers, and leopards have demonstrated the capacity for these species to succumb to HPAI virus infection (Kuiken et al., 2006). Cats inoculated with H5N1 virus by the i.n. or i.g. route presented with clinical signs of illness (including fever, lethargy, and dyspnea) with detection of infectious virus in respiratory and intestinal tissues (Giese et al., 2008; Kuiken et al., 2004; Vahlenkamp et al., 2010). Extapulmonary spread to numerous organ systems, including the brain, has also been reported in this species (Rimmelzwaan et al., 2006). The pattern of H5N1 virus attachment to cells of the lower respiratory tract in cats closely mirrors that observed in humans; in contrast, seasonal influenza viruses did not bind well to respiratory tract tissues in this species (van Riel et al., 2007). These studies collectively demonstrate the extraordinary nature of H5N1 viruses to cause disease by multiple exposure routes in species not generally considered susceptible to influenza virus infection.
Other mammals are infrequently evaluated for their permissiveness to H5N1 virus infection. Golden Syrian hamsters have been used to model seasonal influenza virus infection but have only rarely been used in H5N1 pathogenesis studies, despite the ability of H5N1 viruses to spread systemically in this species following either i.n. or i.g. inoculation (Shinya et al., 2011b). New Zealand White rabbits have been used to evaluate toxicity and protective immune responses to H5N1 influenza vaccination, but are rarely used for pathogenesis studies (Heldens et al., 2010; Zhu et al., 2011). However, rabbits were inoculated i.n. following the isolation of H5N1 virus in wild pikas (a closely related species) in China; infected rabbits shed virus from the upper respiratory tract and presented with fever p.i. but the virus was otherwise not pathogenic in this species (Zhou et al., 2009). To determine the susceptibility of cattle to H5N1 virus infection, calves were inoculated by the i.n. route with H5N1 virus, resulting in asymptomatic virus shedding and seroconversion (Kalthoff et al., 2008). These studies demonstrate the ability to use mammalian models not typically employed for studies of influenza virulence to nonetheless address if viruses that arise from serological or other surveillance activities pose a threat to mammalian health.
5. Contribution of host responses to H5N1 pathogenesis
5.1. Host cytokine responses in inbred mammalian models
The presentation of symptoms associated with the acute respiratory infection caused by influenza virus infection generally correlates with the onset and magnitude of host innate immune responses (Hayden et al., 1998). During uncomplicated influenza virus infection, the production of proinflammatory cytokines and chemokines in respiratory tract tissues, notably the early-phase cytokines such as type 1 interferons (IFN) and tumor necrosis factor (TNF) alpha, recruit numerous cell types to the site of infection, limit virus spread, and contribute to the induction of effective adaptive immune responses (Julkunen et al., 2001). However, during severe H5N1 virus infection in humans, cytokine dysregulation (or “cytokine storm”) leading to elevated levels of serum cytokines and chemokines has been reported in tandem with viremia and extra-pulmonary virus dissemination (de Jong et al., 2006; Peiris et al., 2004). This exacerbated proinflammatory response is believed to contribute to the pathogenesis of H5N1 disease by leading to increased damage to host tissues, acute respiratory distress syndrome, and multiple organ dysfunction (Bhatia and Moochhala, 2004; Peiris et al., 2004; To et al., 2001). The contribution of individual cytokines and chemokines to H5N1 virus pathogenesis has been frequently studied with the use of animal models, including transgenic mice deficient in individual cytokines, ferrets which display numerous clinical signs of illness which correlate with inflammatory cytokine production, and macaques which possess the greatest physiologic similarity to humans.
Numerous cytokines and chemokines are expressed in the lungs of mice following infection with virulent H5N1 viruses, including the acute phase cytokines IL-1, IL-6, and TNF, macrophage inflammatory protein 1 alpha (MIP-1), monocyte chemotactic protein (MCP-1), and others (Szretter et al., 2007; Tumpey et al., 2000). Production of these cytokines elicits a rapid recruitment of macrophages and neutrophils into the lungs, contributing to subsequent acute lung inflammation in H5N1 virus-infected mice (Perrone et al., 2008). Due to overlapping functions, identification of individual roles of these cytokines has been achieved via the use of transgenic mice. Mice deficient in IL-1 receptor (IL-1R), IL-17, or IFNα/β receptor exhibited greater morbidity and mortality following H5N1 virus inoculation compared with wild-type controls, suggesting that these cytokines play a role in effective virus clearance and controlling systemic spread of virus (Szretter et al., 2007, 2009; Wang et al., 2011). Mice lacking TNFα or TNF receptors succumbed to H5N1 virus infection, with only modest reductions in morbidity observed in TNF receptor (TNFR) 1 deficient mice prior to death (Salomon et al., 2007a; Szretter et al., 2007). However, triple mutant mice deficient in three signaling receptors (TNFR1, TNFR2, and IL-1R) exhibited reduced morbidity, mortality, diminished cytokine production in the lungs, and decreased cellular infiltrates in the lungs following H5N1 virus infection compared with wild-type mice (Perrone et al., 2010). Interestingly, mice deficient in IL-6, MIP-1, and CC chemokine ligand 2 (CCL2) showed no distinct phenotype compared with wild-type control mice following H5N1 virus inoculation (Salomon et al., 2007a; Szretter et al., 2007). Collectively, these studies highlight the redundancy of the host innate immune response, but nonetheless identify particular cytokines and pathways which serve critical roles in modulating H5N1 viral pathogenesis in this model.
As excessive cytokine production has been implicated in H5N1 disease pathogenesis, several studies have examined if suppression of cytokines could mitigate disease severity. Treatment of H5N1 virus-inoculated mice with the natural murine glucocorticoid cortiocosterone resulted in modest reductions in morbidity but did not protect mice from death; furthermore, treatment with the glycocorticoid dexamethasone had no beneficial effect (Salomon et al., 2007a; Xu et al., 2009). Mice deficient in NF-κB p50 exhibited reductions in hypercytokinemia following H5N1 infection but exhibited no difference in viral load or mortality compared with wild-type mice, suggesting that inhibition of local cytokine responses in the lung is not sufficient to alleviate H5N1 virus-mediated pathogenesis (Droebner et al., 2008). These studies are in agreement with microarray analyses which postulate that H5N1 viral pathogenesis is mediated primarily at the level of viral replication and not local cytokine responses (Cilloniz et al., 2010). Engagement of the IFN response prior to virus infection has also been purported to represent a viable therapeutic therapy to control influenza virus infection. Pretreatment of murine lung cells in vitro with IFNα/β resulted in a significant reduction in H5N1 viral replication, with comparable reductions in viral load observed in H5N1 virus-infected guinea pigs treated with exogenous IFNα (Szretter et al., 2009; Van Hoeven et al., 2009). Similarly, induction of Th1 responses and IFNγ in mice (either mediated by exposure to a Th1-inducing parasite or chitin microparticles, or via administration of exogenous IFNγ) resulted in decreased mortality following H5N1 virus challenge compared with untreated controls (Ichinohe et al., 2007; O’Brien et al., 2011b). These studies illustrate the important role of exploiting host innate antiviral responses to control influenza virus infection, and support the development of compounds which elicit or enhance this response in humans.
5.2. Host cytokine responses in outbred mammalian models
Outbred mammalian models used in the study of influenza virus pathogenesis, notably the ferret and macaque, provide a greater understanding of the complex responses following H5N1 virus infection and their role during human infection. While a general lack of ferret-specific immunological reagents has limited our ability to use this model to examine induction of innate immune responses following influenza virus infection, analysis of genomic sequences in H5N1 virus-infected ferrets has nonetheless allowed for a greater understanding of host responses as they pertain to influenza virus pathogenicity and transmissibility. These studies have revealed a strong correlation between sites of virus replication and induction of local inflammatory mediators (Maines et al., 2012). Infection of ferrets with HPAI H5N1 viruses, which replicate efficiently in the lower respiratory tract, leads to higher levels of numerous cytokines and chemokines (including TNFα, IL-6, IL-8, IFNα/β, IFNγ, and CXCL9-11) in the lungs compared with ferrets infected with seasonal and 2009 H1N1 viruses (Cameron et al., 2008; Maines et al., 2012). Correspondingly, ferrets infected with transmissible human viruses possessed higher levels of numerous inflammatory mediators in the nasal turbinates compared with H5N1 viruses which do not transmit efficiently in this model (Maines et al., 2012). Treatment of H5N1 virus-infected ferrets with a CXCR3 antagonist (resulting in a blockade of CXCL10 signaling) resulted in reduced morbidity and delayed mortality compared with untreated ferrets, further underscoring the role of host factors in H5N1 viral pathogenesis (Cameron et al., 2008).
Similar to what is observed in humans, infection of macaques with highly virulent influenza viruses can result in aberrant innate immune responses contributing to acute respiratory distress syndrome and death (Kobasa et al., 2007). Macaques infected with HPAI H5N1 viruses exhibit stronger IFN, inflammatory, and innate immune transcriptional induction in lung tissue compared with seasonal virus infection (Baskin et al., 2009). Many genes which were highly induced in this model, including IL-1, IL-6, TNFα, and CXCL10, were similarly induced in ferret lungs following H5N1 virus infection (Cameron et al., 2008). While the majority of studies have examined host responses in respiratory tract tissues, upregulation of select inflammatory markers, notably hypoxia inducible factor-1α (HIF-1α), have been found to serve as indicators of extra-pulmonary tissue reactions during H5N1 virus infection in the macaque model (Tolnay et al., 2010). In addition to location, the timing of induction of genes related to inflammatory responses may contribute to the resulting severity of disease. Viruses which mount a lethal infection in macaques exhibit upregulation of numerous genes as early as 12 h p.i. compared with viruses which cause a non-lethal infection (Cilloniz et al., 2009). However, nonlethal viral pneumonia following H5N1 virus infection in rhesus macaques has been shown to elicit transcriptional changes in the lung as early as 6 h p.i., leading to the upregulation of numerous inflammatory, antiviral, and apoptotic genes in this tissue, mirroring that observed in humans (Shinya et al., 2012a).
5.3. Role of other host factors
Following H5N1 influenza virus infection in mammals, there is a rapid virus-mediated antagonism of host factors to counteract the establishment of a strong antiviral state (Hale et al., 2010). The interferon-induced resistance factor Mx1, known to inhibit primary transcription of the influenza A virus genome, is a key component of the innate immune system in outbred mammalian species but is not intact in standard laboratory mouse strains (Grimm et al., 2007). Many influenza viruses which cause severe disease in standard laboratory Mx1−/− mice, including HPAI H5N1 viruses, do not maintain this high virulence in mice carrying a wild-type Mx1 gene (Mx1+/+) (Salomon et al., 2007b; Tumpey et al., 2007b). Compared with standard laboratory mouse strains, Mx1+/+ mice downregulate the expression of genes associated with hypercytokinemia and hyperchemokinemia, and upregulate genes associated with establishment of an antiviral state (Cilloniz et al., 2012). The identification of Mx1 expression to inhibit viral polymerase activity following infection, resulting in reduced viral replication and spread, identifies a potential mechanism for future antiviral drug development in humans (Grimm et al., 2007; Salomon et al., 2007b). Unlike mice, guinea pigs possess a functional Mx gene, which may contribute to the limited virulence of HPAI H5N1 viruses additionally observed in this model (Van Hoeven et al., 2009).
Numerous other host factors contribute to pathogen recognition and response and, with the use of mammalian models, have been identified to contribute to H5N1 pathogenesis. Activation of Toll-like receptor (TLR) signaling pathways (notably TLR3 and TLR4 via prestimulation of mice with TLR-specific ligands) has been shown to increase protection against HPAI H5N1 virus infection in mice (Shinya et al., 2011c; Wong et al., 2009). More specifically, the use of inactivated H5N1 virus and H5N1 viral infection of primary lung cultures derived from mice deficient in components of TLR4 signaling has identified roles for the TLR4-TRIF pathway in the development of acute lung injury and the stimulation of protective innate immune responses following virus infection (Imai et al., 2008; Shinya et al., 2012b). These studies also identified higher production of reactive oxygen species (ROS) in alveolar macrophages from mice treated with inactivated H5N1 but not H1N1 virus, and enhanced generation of oxidized phospholipids in lungs of mice infected with H5N1 virus, indicating that H5N1 virus infection triggers oxidative stress machinery contributing to severe lung disease (Imai et al., 2008). Elevated levels of autophagosomes are present in the lungs of humans and mice following H5N1 virus infection compared with seasonal viruses, and H5N1 virus infection has been linked to suppression of the mammalian target of rapamycin in mouse cell models, resulting in increased autophagic cell death and acute lung injury following virus infection. These results suggest that autophagy inhibitors may represent potential agents for prophylactic or therapeutic use against this virus (Ma et al., 2011; Sun et al., 2012). It is clear that the identification of signaling pathways whose activation contributes to the establishment of an antiviral state against H5N1 viruses is urgently needed to develop novel methods to prevent and treat disease caused by influenza viruses.
Several studies have demonstrated that the dysregulation of host innate immune responses following H5N1 virus infection in mammals extends to the complement system, a major effector mechanism of antibody dependent and independent immunity which leads to optimal pathogen recognition and elimination (Daha, 2010). Mice deficient in hemolytic complement or complement component C3 exhibited greater mortality following H5N1 virus challenge compared with wild-type mice, demonstrating the need for an intact complement pathway to mount adequate adaptive responses to H5N1 virus infection (Boon et al., 2009; O’Brien et al., 2011a). The dysregulation of complement proteins following H5N1 virus infection has been documented in mice, ferrets, and macaques, identifying important roles for complement in T cell priming and migration to the lung in addition to promoting T cell expansion during influenza virus infection (Baskin et al., 2009; Boon et al., 2009; Cameron et al., 2008; O’Brien et al., 2011a).
Depletion of lymphocytes in H5N1 virus-infected mammals can result in multiple immunologic defects, contributing to greater virus replication and host range in addition to impairing appropriate induction of adaptive responses. As first shown in the mouse model, increased levels of apoptosis in H5N1 virus-infected mice leads to the depletion of lymphocytes in peripheral blood and tissues (Tumpey et al., 2000). Thymic involution and depletion of CD4–CD8 double-positive thymocytes are also detected in mice infected with virulent H5N1 viruses (Szretter et al., 2007; Tumpey et al., 2000). This loss of innate immune cells, notably macrophages and dendritic cells, in addition to the T cell depletion observed following H5N1 virus infection in mice, can result in an inability to mount adaptive immune responses, negatively affecting host outcome (Perrone et al., 2008). Studies in outbred mammalian models have supported these findings. H5N1 virus-infected macaques exhibit a dramatic depletion of circulating CD4+ and CD8+ T cells compared to infection with seasonal viruses, likely due to interactions with circulating type I IFNs inducing vascular margination of T lymphocytes or apoptosis (Baskin et al., 2009). Activated dendritic cells in these animals are also depleted due to apoptosis, resulting in a likely disruption of cell-mediated antiviral responses and initiation of adaptive immune responses due to H5N1 virus infection (Baskin et al., 2009). The dysregulation of inflammation and cell death-related pathways observed in these macaques may be attributed in part to virus-induced changes in expression signatures of cellular microRNAs, resulting in the alteration of expression profiles of target genes associated with the inflammatory process (Li et al., 2011b). While it is clear that lymphocyte depletion following H5N1 virus infection can have a negative effect on host outcome, aberrant increases in cell populations can also contribute to viral pathogenesis. H5N1 virus infection has been shown to cause the increased selective accumulation of a particular dendritic cell subset (TNFα/inducible nitric oxide synthase producing dendritic cells, or tipDCs) in the lungs of mice; while ablation of this population did not alter the severe disease seen with this virus subtype, selectively reducing the accumulation of this subset resulted in increased survival (Aldridge et al., 2009). Collectively, these studies underscore the complex relationship between the innate and adaptive immune responses and how perturbation of this balance following H5N1 virus infection can have a detrimental effect on the host.
6. Modulation of H5N1 virus pathogenicity in the laboratory
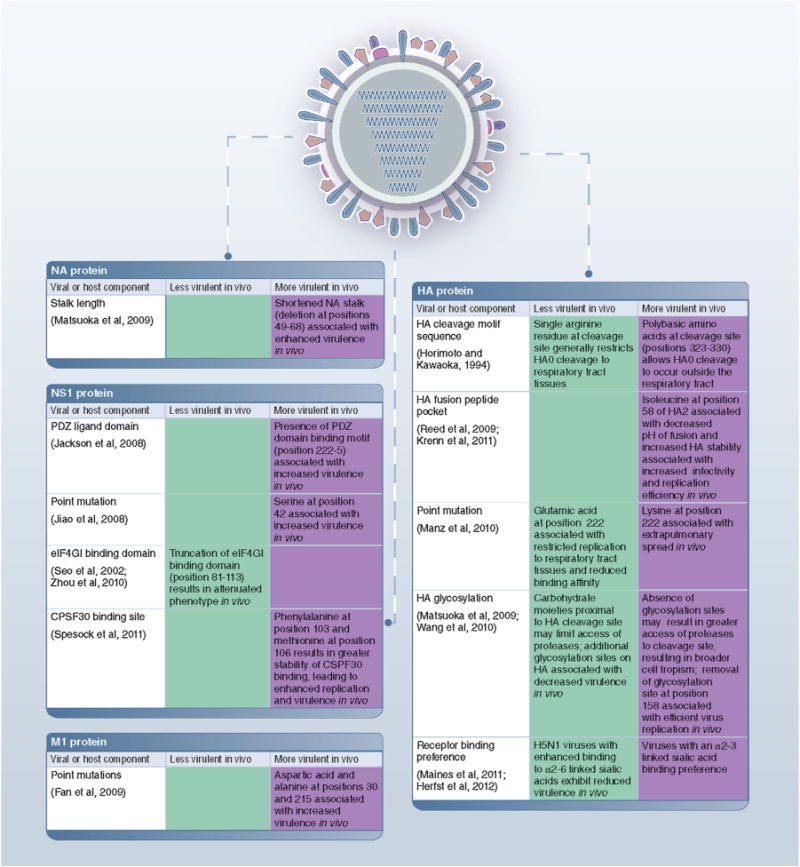
6.1. HA protein
The influenza hemagglutinin (HA) is the major target of host protective antibodies. This protein undergoes continuous genetic and antigenic evolution, resulting in the emergence of several phylogenetically and geographically distinct clades and subclades (Abdel-Ghafar et al., 2008). Despite the important role of the HA in influenza virulence, numerous studies have shown that the surface glycoproteins by themselves are not the sole determinants of virus pathogenicity in mammals (Fig. 3). Reassortant viruses that possess the HA (with or without the neuraminidase (NA)) from a virulent H5N1 virus with all internal genes derived from nonlethal avian or human viruses do not typically exhibit pronounced increases in pathogenicity in mice or ferrets compared with the backbone wild-type strain, though modest strain-specific increases in virulence have been documented (Chen et al., 2007; Imai et al., 2010, 2012; Maines et al., 2006, 2011a; Salomon et al., 2006).
Fig. 3.
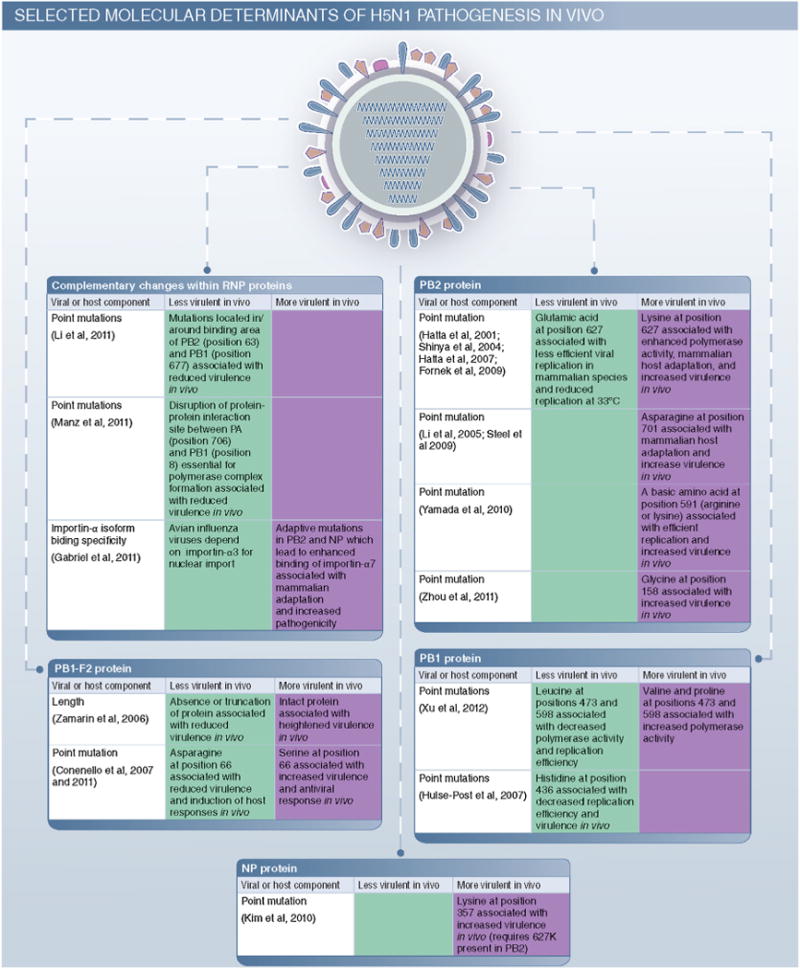
Selected molecular determinants of H5N1 pathogenesis in vivo. Shown are selected viral and host components associated with changes in virulence in mammalian species.
The posttranslational cleavage of HA0 into HA1 and HA2 subunits activates the membrane fusion potential of the HA and as such serves as a necessary step for virus infectivity (Steinhauer, 1999). The majority of avian influenza viruses possess a single arginine residue at the HA cleavage site which is sufficient for cleavage to occur by extracellular trypsin-like proteases that are generally limited to the respiratory tract (Böttcher et al., 2006). In contrast, passage of H5N1 viruses through terrestrial poultry typically results in the acquisition of multiple basic amino acids at the HA cleavage site, which permits HA0 cleavage by ubiquitously expressed intracellular proteases, including furin-like proteases, enabling dissemination of virus beyond respiratory tract tissues (Steinhauer, 1999). A necessary role for a multibasic amino acid cleavage site in H5N1 mammalian virulence has been identified, as removal or replacement of this sequence with that from an avirulent avian strain results in reduced lethality, lower virus titers in respiratory tract tissues, restricted virus spread to extrapulmonary tissues, and weakened induction of host responses in vivo (Hatta et al., 2001; Horimoto and Kawaoka, 1994; Suguitan et al., 2012). However, possession of a multibasic amino acid cleavage site is not sufficient for a virulent phenotype, as not all HPAI H5N1 viruses which contain this feature are lethal in mammals (Maines et al., 2005).
The presence a multibasic amino acid cleavage site is not the only molecular determinant associated with the activation of HA protein leading to membrane fusion. As membrane fusion and conformational changes are pH-dependent, residues in the fusion peptide pocket which regulate the acid stability of the HA protein can play an important role in virus infectivity and replication (Reed et al., 2009). Demonstrating a role for the HA fusion peptide pocket in mammalian virulence of H5N1 viruses, a K58I substitution in the HA2 resulted in a decreased pH of fusion, increased HA stability, and higher virus infectivity in mice (Krenn et al., 2011). Additionally, the passage of avian H5N1 viruses through terrestrial poultry can frequently result in the acquisition of additional glycosylation sites proximal to the HA receptor binding site (Banks and Plowright, 2003). Glycosylation of the H5 HA protein has been shown to restrict the access of proteases to the cleavage site, mask antigenic epitopes, modulate receptor binding preference and restrict virus replication (Deshpande et al., 1987; Wang et al., 2010). In accordance with this, the presence of additional carbohydrate moities on the HA protein, in particular at position 158, has been shown to cause decreased virulence of H5N1 viruses in mice and ferrets compared with wild-type virus (Chen et al., 2007; Matsuoka et al., 2009; Wang et al., 2010).
As discussed previously, the HA mediates binding of influenza viruses to host cell glycoconjugates containing terminal SA residues. H5N1 avian influenza viruses typically exhibit preferential binding to SA linked to galactose by an α(2-3) linkage, whereas human influenza viruses preferentially bind to receptors that possess an α(2-6) linkage, which are more prevalent on human respiratory tract epithelia (Matrosovich et al., 2000; Steinhauer, 1999). It is generally believed that, in order to cause a pandemic, currently circulating H5N1 viruses must acquire a human receptor binding preference to achieve a transmissible phenotype. Mutational studies using the virulent 1918 H1N1 pandemic strain have demonstrated that changing the receptor binding preference of this virus (by introducing the amino acid changes D190E and D225G in the HA) does not abolish the lethal phenotype of this virus in ferrets (Tumpey et al., 2007a). However, as the severity of H5N1 disease is believed to be due in part to virus attachment to α(2-3) linked SA present in high proportions in the human lower respiratory tract, a receptor binding switch of this virus subtype could in turn alter the cellular tropism and virus pathogenicity in mammals. A wild-type H5N1 virus isolated in 2003 which exhibited dual α2-3/α2-6 SA binding did not possess a lethal phenotype in mice or ferrets, but also was found to lack other molecular correlates associated with virulence in these models (Shinya et al., 2005).
The use of reverse genetics has allowed for a greater understanding of the contribution of receptor binding preference as it contributes to virus pathogenicity. H5N1 viruses bearing mutations in the HA which conferred increased binding to α(2-6) linked SA glycans and/or reduced binding to some α(2-3) linked SA generally exhibited comparable to reduced virulence in the ferret model compared with wild-type virus (Chen et al., 2012; Maines et al., 2011b). Furthermore, a genetically modified H5N1 virus capable of transmission by respiratory droplets in the ferret model lacked the high virulent phenotype observed with wild-type virus unless the virus was inoculated intratracheally at a high volume and concentration (Herfst et al., 2012). These studies are in support of additional work which has revealed that alteration of the HA receptor binding pocket is capable of modulating viral pathogenesis. Amino acid position 222 lies within the 220 loop of the receptor binding site of the HA and has been proposed to contribute to viral replication efficiency and organ tropism, as a lysine at this position facilitated extrapulmonary virus spread in mice whereas a glutamic acid at this position limited virus replication and reduced binding affinity to sialic acids (Manz et al., 2010).
6.2. NA protein
An evolutionary balance between the HA and NA surface proteins of influenza viruses plays an important role in virus entry and egress from host cells (Baigent and McCauley, 2001). As a result, mutations within the active sites of either the HA or NA can influence the enzymatic activity of both surface glycoproteins. For example, adaptation of H5N1 viruses to terrestrial poultry results not only in the addition of increased HA glycosylation but also a shortening of the NA stalk. These changes can greatly affect the virulence of H5N1 viruses in mammals, as H5N1 viruses with a truncated NA protein exhibit enhanced virulence in mice compared with viruses with longer NA stalks (Matsuoka et al., 2009). Compatibility between the HA and NA has also been shown to contribute to the high virulence of H5N1 viruses in the ferret model. Substitution of the NA gene of an H5N1 virus of low virulence in the ferret model on the backbone of a highly virulent H5N1 virus was sufficient to reduce peak virus titers, morbidity, and mortality following infection compared with wild-type virus (Maines et al., 2011a). The reciprocal constellation did not result in an increase in virulence, demonstrating the importance of maintaining compatibility between the HA and NA to achieve maximal virulence in mammals. However, substitution of the NA gene of a human H3N2 virus on the backbone of a highly virulent H5N1 virus reduced the lethality or efficient virus replication of the backbone virus in ferrets but not mice, indicating that the ability of NA to functionally support the activity of the H5 HA is both host- and strain-dependent (Chen et al., 2008; Jackson et al., 2009).
Neuraminidase inhibitors (oseltamivir and zanamivir) are a critical class of antiviral drugs for the treatment of both human and avian influenza viruses, but the isolation of oseltamivir-resistant H5N1 viruses from infected patients demonstrates that resistant variants can cause severe disease in humans (Abdel-Ghafar et al., 2008). Viruses which possess H274Y in this protein (conferring a resistant phenotype to this class of drug) are capable of causing severe and fatal disease in both the mouse and ferret models (Govorkova et al., 2010; Yen et al., 2007a). Additional mutations in the NA which confer reduced susceptibility to oseltamivir, notably E119A and N294S, can also result in a lethal infection in these species, with viral titers and inflammation in the lungs matching or exceeding that observed during wild-type virus infection (Ilyushina et al., 2010). However, this effect is strain-specific, as H5N1 viruses bearing H274Y or N294S can also exhibit an attenuated phenotype in mice and ferrets (Govorkova et al., 2010; Kiso et al., 2011). These studies underscore the importance of studying the contribution of these mutations on virus fitness in mammals in addition to highlighting the need for new therapeutic agents against this virus.
6.3. Polymerase complex
The polymerase PB2, PB1, PA, and the nucleocapsid protein (NP) together form the ribonucleoprotein complex (RNP). This complex, which possesses RNA-dependent RNA polymerase activity and contains nuclear localization signals to facilitate transcription of viral RNA (vRNA), has known roles in both virulence and determination of host restriction (Naffakh et al., 2008). Demonstrating a role for the polymerase genes in H5N1 pathogenesis in mammalian models, reassortant viruses bearing polymerase genes from a human H3N2 virus (RNP in ferrets, PB2, PB1, PA in mice) on the backbone of a highly virulent H5N1 virus abolished the high virulence observed with the wild-type H5N1 virus in both species (Chen et al., 2008; Maines et al., 2006). Furthermore, substitution of the PB2, PB1, and PA from an H5N1 virus of low virulence in the ferret model on the backbone of a highly virulent H5N1 virus was sufficient to abolish the high pathogenicity observed with the wild-type strain in both mice and ferrets (Maines et al., 2011a; Salomon et al., 2006). The reciprocal constellation generally restored the high pathogenicity phenotype in both species, with slight strain-specific differences observed in the ferret model. Study of the cooperative nature of genes within the polymerase complex has identified properties which influence the host range and virulence of wild-type H5N1 viruses. Adaptive mutations in the PB2 and NP genes which modulate binding specificity of importin-α, an adaptor protein that mediates nuclear transport, have been associated with avian-mammal adaptation and interspecies transmission of H5N1 viruses (Gabriel et al., 2008, 2011). Due to the importance of optimal polymerase complex activity in viral replication and virulence, identification of mutations in the PA and PB1 genes or PB1 and PB2 genes, which lead to modulations in polymerase assembly, activity, and virulence, have been proposed as a novel mechanism to attenuate H5N1 viruses (Li et al., 2011a; Manz et al., 2011). These studies highlight the importance for compatibility between the viral genes which comprise the RNP.
Critical roles have been identified for each polymerase gene in the virulence of H5N1 viruses in mammals. The use of single gene reassortant viruses has identified that the presence of either the PB1, PB2, or PA gene derived from an H5N1 virus of low virulence on the backbone of a highly virulent H5N1 virus is sufficient to greatly reduce or abolish the virulence of the parental strain in ferrets (Maines et al., 2011a; Salomon et al., 2006). Similar studies which have created single gene reassortant viruses between human H3N2 virus and H5N1 virus polymerase genes in mice have yielded similar results (Chen et al., 2008). Reciprocal studies have found that the addition of either the PB2, PB1, or PA gene derived from a highly virulent H5N1 virus greatly increases the pathogenicity of a virus which is otherwise not highly pathogenic in mice or ferrets (Chen et al., 2008; Maines et al., 2011a). The role of PB1, a protein which initiates transcription and catalyzes nucleotide additions during elongation, has been of particular interest as all three pandemic viruses of the 20th century possessed an avian PB1 gene (Kawaoka et al., 1989; Naffakh et al., 2008; Taubenberger et al., 2005). The substitution of a PB1 gene from a human H3N2 virus on the backbone of a virulent H5N1 virus was sufficient to abrogate the lethal phenotype of the H5N1 virus in ferrets, and did not increase the pathogenicity of H5N1 viruses of reduced virulence in mice (Jackson et al., 2009; Li et al., 2010). Substitution of an avian H5N1 PB1 gene enhanced the polymerase activity of an attenuated human virus in mammalian cells, with a valine at position 473 and a proline at position 598 attributed to conferring this phenotype (Xu et al., 2012). Furthermore, a histidine at position 436 attenuated the lethality of an H5N1 virus in both mice and ferrets (Hulse-Post et al., 2007). Just as balanced enzymatic activity between the influenza virus surface glycoproteins contributes to H5N1 virulence in mammals, optimal compatibility between the proteins which form the RNP is also an important contributor to the overall pathogenesis of avian influenza virus infection.
6.4. PB2 protein
Avian H5N1–human H3N2 influenza virus reassortant studies have identified that the presence of a human PB2 is a major determinant for the pathogenicity of resulting viruses in mice (Li et al., 2010). The principle PB2 molecular determinant associated with the determination of host range and pathogenicity of H5N1 viruses in mammals is the amino acid present at position 627 (Chen et al., 2006; Hatta et al., 2001; Subbarao et al., 1993). Human influenza viruses typically possess a lysine at this position, whereas most avian viruses bear a glutamic acid, though this can vary between H5N1 virus clades (Bogs et al., 2011). With the use of plasmid-based reverse genetics, numerous studies have investigated the role of this amino acid position on H5N1 pathogenesis. A single E627K mutation is sufficient to convert a nonlethal H5N1 virus to a lethal virus in mice, and conversely, the K627E substitution attenuates the highly virulent phenotype of H5N1 viruses in mice and ferrets (Hatta et al., 2001; Shinya et al., 2004). The presence of a lysine at this position confers to H5N1 viruses the ability to replicate with higher efficiency in upper and lower respiratory tract tissues in mice compared with viruses bearing a glutamate at this position (Hatta et al., 2007). This increase in virus replication is correlated with a highly activated inflammatory response in the lungs of mice, characterized by increased apoptosis in the lungs and a decrease in oxygen saturation; T-cell receptor activation is also impaired (Fornek et al., 2009). The E627K substitution also provides the ability for avian influenza viruses to replicate at 33 °C, the temperature of the human respiratory tract (Hatta et al., 2007; Massin et al., 2001). Furthermore, mutations in PB2 and NP genes can influence virus pathogenicity, as a lysine at position 357 of NP contributes to virulence in vivo when the 627 K mutation is present (Gabriel et al., 2011; Kim et al., 2010). Collectively, these studies indicate that infection with an H5N1 virus bearing a lysine at position 627 can contribute to an inability for an infected mammal to contain the virus at the primary site of replication, resulting in systemic spread of virus and ultimately a lethal outcome.
While a lysine at position 627 is frequently associated with a lethal phenotype in mammals, it is not necessary for a virulent phenotype in mammalian hosts (Govorkova et al., 2005; Maines et al., 2005). This is further supported by the absence of a clear correlation between the amino acid present at position 627 and the clinical outcome of H5N1 human infections (de Jong et al., 2006). In the absence of E627K, additional mutations at other sites of PB2 can compensate to maintain a virulent phenotype in mammals (Li et al., 2009). Infection of mice with an H5N1 virus bearing an asparagine at position 701 was associated with systemic spread of virus and enhanced mortality compared with a virus bearing an aspartic acid at this position (Li et al., 2005). An asparagine at position 701 has also been shown to compensate for the lack of a lysine at position 627 with regard to H5N1 virus infectivity and transmissibility in the guinea pig model (Steel et al., 2009a). Additional amino acids in this protein have been associated with modulation of virus pathogenicity, including the substitutions T271A, the presence of which enhanced polymerase activity in mammalian cells, and E158G and 591K, both of which were associated with increased morbidity and mortality of H5 influenza viruses in mice (Bussey et al., 2010; Yamada et al., 2010; Zhou et al., 2011). It is clear from these studies that point mutations in the PB2 protein of H5N1 viruses can drastically influence virus pathogenicity in mammals, warranting their close surveillance to better predict virus pathogenicity in mammalian models.
6.5. PB1-F2 protein
Produced by an alternate reading frame in the PB1 gene, PB1-F2 is a proapoptotic protein which localizes to the inner and outer membrane of host mitochondria and causes the destruction of alveolar macrophages (Chen et al., 2001; Coleman, 2007; Zamarin et al., 2005). While PB1-F2 is present in all influenza virus subtypes, many viruses possess a truncated PB1-F2 sequence which renders the protein nonfunctional, influencing viral pathogenicity in mammalian species (Zell et al., 2007). In support of this, influenza virus PB1-F2 knockout mutants were less virulent in mice and displayed reduced viral polymerase activity compared with viruses bearing a full-length protein (Chen et al., 2010a; Zamarin et al., 2006). The H5N1 PB1-F2 has been shown to contribute to mammalian pathogenesis, as the presence of this protein was associated with a delay in viral clearance in mice following infection, allowing for prolonged viral replication and increased immunopathology in the lungs (Zamarin et al., 2006). PB1-F2 expression has also been associated with susceptibility to secondary bacterial pneumonia following infection with highly pathogenic influenza viruses, although the contribution of this to H5N1 pathogenesis has not been fully evaluated (McAuley et al., 2007).
Beyond the presence of an intact PB1-F2 protein contributing to viral pathogenicity, additional virulence markers have been identified for this protein. H5N1 viruses from the 1997 outbreak bearing a serine at amino acid position 66 exhibited a high pathogenicity phenotype in mice compared with viruses bearing an asparagine at this position (Conenello et al., 2007). Presence of this 66S mutation in the H5N1 PB1-F2 led to delayed activation of IFN-stimulated gene expression, increased cytokine and chemokine levels, and increased infiltration of monocytes and neutrophils in the lungs of mice compared with 66N (Conenello et al., 2011). Furthermore, a N66S substitution in a HPAI H5N1 virus isolated from a fatal case in 2004 was associated with increased neurotropism in Mx+/+ mice compared with infection with wild-type virus (Schmolke et al., 2011). These studies have identified that N66S-induced pathogenesis is due to inhibition of early type I IFN responses at the level of the mitochondrial antiviral signaling protein (MAVS) and not via modulation of adaptive immune responses (Conenello et al., 2011; Varga et al., 2011). The C-terminus of PB1-F2 (which contains a mitochondrial targeting sequence) has also been shown to enhance the inflammatory response leading to heightened immunopathology of H5N1 viruses in mice (McAuley et al., 2010). Collectively, this work has identified this protein as an important yet strain-specific pathogenicity factor of highly pathogenic avian influenza viruses.
6.6. NS1 protein
The NS gene of influenza virus encodes two proteins: NS1, a multi-functional nonstructural RNA-binding protein that functions as an antagonist to block type I IFN-mediated host antiviral responses following infection, and NS2, also known as nuclear export protein (NEP), which is encoded by a spliced mRNA (Garcia-Sastre, 2001). During influenza virus infection, NS1 sequesters double-stranded RNA (dsRNA) generated during virus replication, inhibiting PKR activity to binding to free dsRNA, and preventing transcription of antiviral genes among other functions (Garcia-Sastre, 2001). To demonstrate this, infection of epithelial cells with NS1-deficient viruses resulted in the heightened expression of numerous antiviral response genes, including retinoic acid inducible gene I (RIG-I) and melanoma differentiation-associated gene 5 (MDA5) compared to infection with wild-type viruses (Guo et al., 2007; Opitz et al., 2007). Infection of mammalian models with single-gene reassortant viruses has further identified a contribution of the NS gene to H5N1 virus pathogenicity. Substitution of the NS gene of a HPAI H5N1 virus onto the backbone of a human H1N1 virus or reassortant H3N2 virus resulted in increased viral pathogenicity in mice and a strong modulation of lymphohe-matopoietic and cytokine-mediated antiviral responses following infection, respectively (Hyland et al., 2006; Lipatov et al., 2005). Furthermore, the presence of an NS gene from a human H3N2 virus on the backbone of a highly virulent H5N1 virus resulted in decreased virulence in mice compared with wild-type virus (Chen et al., 2008). However, many of the contributions of NS1 to mammalian virulence appear to be strain-specific, as substitution of the NS gene of an H5N1 virus of low virulence onto the backbone of a highly virulent H5N1 virus resulted in a partially attenuated phenotype in ferrets but not in mice, and substitution of the NS gene of an H5N1 virus of high virulence onto the backbone of an H5N1 virus of low virulence did not increase virus pathogenicity in ferrets (Salomon et al., 2006). Furthermore, substitution of the NS gene of an H5N1 virus of high virulence onto the backbone of an H5N1 virus of low virulence was not sufficient to increase virus pathogenicity in ferrets without the concurrent substitution of a high virulence HA gene (Imai et al., 2010).
Several molecular correlates of virulence have been identified within the NS1 protein of H5N1 subtype viruses. The presence of a glutamic acid at residue 92 of the H5N1 NS1 protein has been associated with increased pathogenicity in pigs and mice, as mice infected with reassortant viruses being E92D at this position exhibit reduced mortality, lower viral titers, and reduced levels of proin-flammatory cytokines and chemokines in lung tissue (Lipatov et al., 2005; Seo et al., 2002). The presence of a serine at position 42 in the NS1 protein has also been associated with increased virulence of an H5N1 virus in mice (Jiao et al., 2008). Furthermore, introduction of two mutations in the cleavage and polyadenylation specificity factor (CPSF30) binding site of the H5N1 NS1, resulting in greater stability of CSPF30 binding in infected cells which leads to inhibition of IFNβ mRNA production, resulted in enhanced replication and virulence compared with wild-type virus in mice (Dankar et al., 2011; Spesock et al., 2011).
Following viral infection, the NS1 eukaryotic translation initiation factor 4GI (eIF4GI) binding domain (position 81–113) is recruited to the 5 untranslated region of viral mRNA, resulting in preferential translation of viral proteins (de la Luna et al., 1995). The presence of a 5aa deletion (residues 80–84) in the NS1 protein among some H5N1 viruses conferred resistance to the antiviral effects of type I IFNs in vitro but infection of mice with a reassortant virus bearing this deletion did not result in an increase in virulence unless the D92E mutation was also present (Li et al., 2004; Lipatov et al., 2005; Long et al., 2008; Seo et al., 2002). However, additional truncation of the eIF4GI binding domain resulted in an attenuated phenotype in mice compared with wild-type H5N1 virus, likely associated with the ability of these mutant viruses to induce IFNβ following infection (Zhou et al., 2010).
Unlike seasonal human viruses, the four C-terminal resides of most H5N1 NS1 proteins bear a type I PDZ domain binding motif which can associate with numerous cellular targets, resulting in a range of activities which include the disruption of cellular tight junctions and modulating apoptosis in infected cells, contributing to the severity of disease (Golebiewski et al., 2011; Jackson et al., 2008). The presence of these avian H5N1 NS1 C-terminal residues was found to enhance the pathogenicity of a mouse-adapted H1N1 virus but not an H5N1 virus, indicating that this motif likely acts in a strain-specific and host-specific manner (Jackson et al., 2008; Soubies et al., 2010; Zielecki et al., 2010). Due to the attenuated phenotype observed in mammalian species following deletion of key regions of the NS1 protein, live attenuated vaccines based on truncations of this protein have been proposed (Steel et al., 2009b).
6.7. M1 protein
The matrix (M) gene codes for two proteins, M1 and M2; M1 has numerous roles in viral assembly due to its association with the RNP, while M2 modulates the pH of intracellular compartments which enable HA-mediated fusion of viral and endosomal membranes during virus entry (Rossman and Lamb, 2011). Studies using mouse-adapted influenza A and B viruses have identified that modifications of the M1 protein, notably in the C-terminal domain, are associated with adaptation and efficient virus replication in this species (Govorkova et al., 2000; McCullers et al., 2005). Demonstrating a role for the matrix gene in H5N1 viral pathogenesis, a reassortant virus bearing a human H3N2 M gene on the backbone of a highly virulent H5N1 virus abolished the high virulence of the parental strain in mice (Chen et al., 2008). Further study identified that, specifically, an aspartic acid at position 30 and alanine at position 215 in the M1 protein were associated with increased virulence of an H5N1 virus in mice (Fan et al., 2009a). As the matrix gene represents a proposed target for vaccine strategies, a greater understanding of the contribution of M1 and M2 to H5N1 pathogenesis is warranted (Steel, 2011; Tompkins et al., 2007).
7. Conclusions
While H5N1 influenza viruses are responsible for a relatively low number of human infections each year, the high case fatality associated with human infection and potential for these viruses to acquire a transmissible phenotype and cause a pandemic renders this virus subtype a formidable public health threat. The expanding host range and geographic spread of this virus subtype further underscores the need to study this virus subtype (Munster and Fouchier, 2009). As discussed in this review, both viral and host factors contribute to the pathogenesis of H5N1 viruses in mammalian species. A greater understanding of the virus–host interactions which confer a highly pathogenic phenotype is essential to best prepare for and respond to future influenza pandemics.
It is important to note that H5N1 viruses are not the only avian virus subtype associated with human infection and death. H7 subtype viruses have caused over 100 confirmed or presumed human infections, with one lethality (Belser et al., 2009a). Similar to H5N1 viruses, HPAI H7 viruses are capable of efficient replication and systemic spread in mice and ferrets (Belser et al., 2007). Furthermore, many of the molecular correlates of virulence identified for H5N1 viruses in mammalian species are also found for HPAI H7N7 viruses (de Wit et al., 2010; Munster et al., 2007). LPAI H9N2 viruses have also caused sporadic human infections, but do not cause severe disease in laboratory mammalian models (Lu et al., 2001; Peiris et al., 1999; Wan et al., 2008). Nevertheless, similar to other HPAI virus subtypes, the contribution of the PB2 gene and position 627 to mammalian virulence is maintained in H9N2 viruses (Li et al., 2012). While not typically associated with human disease, many other virus subtypes can productively infect mammalian species and have the capacity to support a highly pathogenic phenotype (Gillim-Ross et al., 2008; Veits et al., 2012).
Our understanding of the molecular basis of H5N1 virulence has improved dramatically in the past few years. However, the continued evolution of HPAI H5N1 viruses over the past decade has resulted in the emergence of numerous phylogenetic groups (WHO/OIE/FAO, 2012); future study will be needed to determine additional potential genetic changes which contribute to mammalian pathogenesis. The recent discovery of a twelfth influenza virus protein coded by an alternate reading frame of PA, termed PA-X, has been shown to modulate host responses to infection; future work is needed to determine the potential role of this protein in H5N1 viral pathogenesis (Jagger et al., 2012). Continued study of previous pandemic strains may also further our ability to best assess the pandemic potential of H5N1 and other avian influenza viruses.
Acknowledgments
The authors thank Alissa Eckert for graphical assistance. The findings and conclusions in this report are those of the authors and do not necessarily reflect the views of the funding agency.
References
- Abdel-Ghafar AN, Chotpitayasunondh T, Gao Z, Hayden FG, Nguyen DH, de Jong MD, Naghdaliyev A, Peiris JS, Shindo N, Soeroso S, Uyeki TM. Update on avian influenza A (H5N1) virus infection in humans. New England Journal of Medicine. 2008;358(3):261–273. doi: 10.1056/NEJMra0707279. [DOI] [PubMed] [Google Scholar]
- Aldridge JR, Jr, Moseley CE, Boltz DA, Negovetich NJ, Reynolds C, Franks J, Brown SA, Doherty PC, Webster RG, Thomas PG. TNF/iNOS-producing dendritic cells are the necessary evil of lethal influenza virus infection. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(13):5306–5311. doi: 10.1073/pnas.0900655106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baigent SJ, McCauley JW. Glycosylation of haemagglutinin and stalk-length of neuraminidase combine to regulate the growth of avian influenza viruses in tissue culture. Virus Research. 2001;79(1/2):177–185. doi: 10.1016/s0168-1702(01)00272-6. [DOI] [PubMed] [Google Scholar]
- Banks J, Plowright L. Additional glycosylation at the receptor binding site of the hemagglutinin (HA) for H5 and H7 viruses may be an adaptation to poultry hosts, but does it influence pathogenicity? Avian Diseases. 2003;47(3 Suppl):942–950. doi: 10.1637/0005-2086-47.s3.942. [DOI] [PubMed] [Google Scholar]
- Baskin CR, Bielefeldt-Ohmann H, Tumpey TM, Sabourin PJ, Long JP, Garcia-Sastre A, Tolnay AE, Albrecht R, Pyles JA, Olson PH, Aicher LD, Rosenzweig ER, Murali-Krishna K, Clark EA, Kotur MS, Fornek JL, Proll S, Palermo RE, Sabourin CL, Katze MG. Early and sustained innate immune response defines pathology and death in nonhuman primates infected by highly pathogenic influenza virus. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(9):3455–3460. doi: 10.1073/pnas.0813234106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belser JA, Bridges CB, Katz JM, Tumpey TM. Past, present, and possible future human infection with influenza virus A subtype H7. Emerging Infectious Diseases. 2009a;15(6):859–865. doi: 10.3201/eid1506.090072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belser JA, Gustin KM, Maines TR, Blau DM, Zaki SR, Katz JM, Tumpey TM. Pathogenesis and transmission of triple-reassortant swine H1N1 influenza viruses isolated before the 2009 H1N1 pandemic. Journal of Virology. 2011a;85(4):1563–1572. doi: 10.1128/JVI.02231-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belser JA, Gustin KM, Maines TR, Pantin-Jackwood MJ, Katz JM, Tumpey TM. Influenza virus respiratory infection and transmission following ocular inoculation in ferrets. PLoS Pathogens. 2012;8(3):e1002569. doi: 10.1371/journal.ppat.1002569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belser JA, Katz JM, Tumpey TM. The ferret as a model organism to study influenza A virus infection. Disease Models & Mechanisms. 2011b;4(5):575–579. doi: 10.1242/dmm.007823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belser JA, Lu X, Maines TR, Smith C, Li Y, Donis RO, Katz JM, Tumpey TM. Pathogenesis of avian influenza (H7) virus infection in mice and ferrets: enhanced virulence of Eurasian H7N7 viruses isolated from humans. Journal of Virology. 2007;81(20):11139–11147. doi: 10.1128/JVI.01235-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belser JA, Wadford DA, Xu J, Katz JM, Tumpey TM. Ocular infection of mice with influenza A (H7) viruses: a site of primary replication and spread to the respiratory tract. Journal of Virology. 2009b;83(14):7075–7084. doi: 10.1128/JVI.00535-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatia M, Moochhala S. Role of inflammatory mediators in the pathophysiology of acute respiratory distress syndrome. Journal of Pathology. 2004;202(2):145–156. doi: 10.1002/path.1491. [DOI] [PubMed] [Google Scholar]
- Bodewes R, Kreijtz JH, van Amerongen G, Fouchier RA, Osterhaus AD, Rimmelzwaan GF, Kuiken T. Pathogenesis of Influenza A/H5N1 virus infection in ferrets differs between intranasal and intratracheal routes of inoculation. American Journal of Pathology. 2011;179(1):30–36. doi: 10.1016/j.ajpath.2011.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogs J, Kalthoff D, Veits J, Pavlova S, Schwemmle M, Manz B, Mettenleiter TC, Stech J. Reversion of PB2-627E to -627K during replication of an H5N1 Clade 2.2 virus in mammalian hosts depends on the origin of the nucleoprotein. Journal of Virology. 2011;85(20):10691–10698. doi: 10.1128/JVI.00786-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boon AC, deBeauchamp J, Hollmann A, Luke J, Kotb M, Rowe S, Finkelstein D, Neale G, Lu L, Williams RW, Webby RJ. Host genetic variation affects resistance to infection with a highly pathogenic H5N1 influenza A virus in mice. Journal of Virology. 2009;83(20):10417–10426. doi: 10.1128/JVI.00514-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boon AC, Finkelstein D, Zheng M, Liao G, Allard J, Klumpp K, Webster R, Peltz G, Webby RJ. H5N1 influenza virus pathogenesis in genetically diverse mice is mediated at the level of viral load. MBio. 2011;2(5) doi: 10.1128/mBio.00171-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Böttcher E, Matrosovich T, Beyerle M, Klenk HD, Garten W, Matrosovich M. Proteolytic activation of influenza viruses by serine proteases TMPRSS2 and HAT from human airway epithelium. Journal of Virology. 2006;80(19):9896–9898. doi: 10.1128/JVI.01118-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bright RA, Cho DS, Rowe T, Katz JM. Mechanisms of pathogenicity of influenza A (H5N1) viruses in mice. Avian Diseases. 2003;47(3 Suppl):1131–1134. doi: 10.1637/0005-2086-47.s3.1131. [DOI] [PubMed] [Google Scholar]
- Bussey KA, Bousse TL, Desmet EA, Kim B, Takimoto T. PB2 residue 271 plays a key role in enhanced polymerase activity of influenza A viruses in mammalian host cells. Journal of Virology. 2010;84(9):4395–4406. doi: 10.1128/JVI.02642-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron CM, Cameron MJ, Bermejo-Martin JF, Ran L, Xu L, Turner PV, Ran R, Danesh A, Fang Y, Chan PK, Mytle N, Sullivan TJ, Collins TL, Johnson MG, Medina JC, Rowe T, Kelvin DJ. Gene expression analysis of host innate immune responses during Lethal H5N1 infection in ferrets. Journal of Virology. 2008;82(22):11308–11317. doi: 10.1128/JVI.00691-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CJ, Chen GW, Wang CH, Huang CH, Wang YC, Shih SR. Differential localization and function of PB1-F2 derived from different strains of influenza A virus. Journal of Virology. 2010a;84(19):10051–10062. doi: 10.1128/JVI.00592-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen H, Bright RA, Subbarao K, Smith C, Cox NJ, Katz JM, Matsuoka Y. Polygenic virulence factors involved in pathogenesis of 1997 Hong Kong H5N1 influenza viruses in mice. Virus Research. 2007;128(1/2):159–163. doi: 10.1016/j.virusres.2007.04.017. [DOI] [PubMed] [Google Scholar]
- Chen H, Li Y, Li Z, Shi J, Shinya K, Deng G, Qi Q, Tian G, Fan S, Zhao H, Sun Y, Kawaoka Y. Properties and dissemination of H5N1 viruses isolated during an influenza outbreak in migratory waterfowl in western China. Journal of Virology. 2006;80(12):5976–5983. doi: 10.1128/JVI.00110-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LM, Blixt O, Stevens J, Lipatov AS, Davis CT, Collins BE, Cox NJ, Paulson JC, Donis RO. In vitro evolution of H5N1 avian influenza virus toward human-type receptor specificity. Virology. 2012;422(1):105–113. doi: 10.1016/j.virol.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LM, Davis CT, Zhou H, Cox NJ, Donis RO. Genetic compatibility and virulence of reassortants derived from contemporary avian H5N1 and human H3N2 influenza A viruses. PLoS Pathogens. 2008;4(5):e1000072. doi: 10.1371/journal.ppat.1000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W, Calvo PA, Malide D, Gibbs J, Schubert U, Bacik I, Basta S, O’Neill R, Schickli J, Palese P, Henklein P, Bennink JR, Yewdell JW. A novel influenza A virus mitochondrial protein that induces cell death. Nature Medicine. 2001;7(12):1306–1312. doi: 10.1038/nm1201-1306. [DOI] [PubMed] [Google Scholar]
- Chen Y, Deng W, Jia C, Dai X, Zhu H, Kong Q, Huang L, Liu Y, Ma C, Li J, Xiao C, Liu Y, Wei Q, Qin C. Pathological lesions and viral localization of influenza A (H5N1) virus in experimentally infected Chinese rhesus macaques: implications for pathogenesis and viral transmission. Archives of Virology. 2009;154(2):227–233. doi: 10.1007/s00705-008-0277-5. [DOI] [PubMed] [Google Scholar]
- Chen Y, Zhong G, Wang G, Deng G, Li Y, Shi J, Zhang Z, Guan Y, Jiang Y, Bu Z, Kawaoka Y, Chen H. Dogs are highly susceptible to H5N1 avian influenza virus. Virology. 2010b;405(1):15–19. doi: 10.1016/j.virol.2010.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chmielewski R, Swayne DE. Avian influenza: public health and food safety concerns. Annual Review of Food Science Technology. 2011;2:37–57. doi: 10.1146/annurev-food-022510-133710. [DOI] [PubMed] [Google Scholar]
- Cilloniz C, Pantin-Jackwood MJ, Ni C, Carter VS, Korth MJ, Swayne DE, Tumpey TM, Katze MG. Molecular signatures associated with Mx1-mediated resistance to highly pathogenic influenza virus infection: mechanisms of survival. Journal of Virology. 2012;86(5):2437–2446. doi: 10.1128/JVI.06156-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cilloniz C, Pantin-Jackwood MJ, Ni C, Goodman AG, Peng X, Proll SC, Carter VS, Rosenzweig ER, Szretter KJ, Katz JM, Korth MJ, Swayne DE, Tumpey TM, Katze MG. Lethal dissemination of H5N1 influenza virus is associated with dysregulation of inflammation and lipoxin signaling in a mouse model of infection. Journal of Virology. 2010;84(15):7613–7624. doi: 10.1128/JVI.00553-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cilloniz C, Shinya K, Peng X, Korth MJ, Proll SC, Aicher LD, Carter VS, Chang JH, Kobasa D, Feldmann F, Strong JE, Feldmann H, Kawaoka Y, Katze MG. Lethal influenza virus infection in macaques is associated with early dysregulation of inflammatory related genes. PLoS Pathogens. 2009;5(10):e1000604. doi: 10.1371/journal.ppat.1000604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman JR. The PB1-F2 protein of Influenza A virus: increasing pathogenicity by disrupting alveolar macrophages. Virology. 2007;4:9. doi: 10.1186/1743-422X-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conenello GM, Tisoncik JR, Rosenzweig E, Varga ZT, Palese P, Katze MG. A single N66S mutation in the PB1-F2 protein of influenza A virus increases virulence by inhibiting the early interferon response in vivo. Journal of Virology. 2011;85(2):652–662. doi: 10.1128/JVI.01987-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conenello GM, Zamarin D, Perrone LA, Tumpey T, Palese P. A single mutation in the PB1-F2 of H5N1 (HK/97) and 1918 influenza A viruses contributes to increased virulence. PLoS Pathogens. 2007;3(10):1414–1421. doi: 10.1371/journal.ppat.0030141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conn CA, McClellan JL, Maassab HF, Smitka CW, Majde JA, Kluger MJ. Cytokines and the acute phase response to influenza virus in mice. American Journal of Physiology. 1995;268(1 Pt 2):R78–R84. doi: 10.1152/ajpregu.1995.268.1.R78. [DOI] [PubMed] [Google Scholar]
- Crawford PC, Dubovi EJ, Castleman WL, Stephenson I, Gibbs EP, Chen L, Smith C, Hill RC, Ferro P, Pompey J, Bright RA, Medina MJ, Johnson CM, Olsen CW, Cox NJ, Klimov AI, Katz JM, Donis RO. Transmission of equine influenza virus to dogs. Science. 2005;310(5747):482–485. doi: 10.1126/science.1117950. [DOI] [PubMed] [Google Scholar]
- Daha MR. Role of complement in innate immunity and infections. Critical Reviews in Immunology. 2010;30(1):47–52. doi: 10.1615/critrevimmunol.v30.i1.30. [DOI] [PubMed] [Google Scholar]
- Dankar SK, Wang S, Ping J, Forbes NE, Keleta L, Li Y, Brown EG. Influenza A virus NS1 gene mutations F103L and M106I increase replication and virulence. Virology. 2011;8:13. doi: 10.1186/1743-422X-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong MD, Bach VC, Phan TQ, Vo MH, Tran TT, Nguyen BH, Beld M, Le TP, Truong HK, Nguyen VV, Tran TH, Do QH, Farrar J. Fatal avian influenza A (H5N1) in a child presenting with diarrhea followed by coma. New England Journal of Medicine. 2005;352(7):686–691. doi: 10.1056/NEJMoa044307. [DOI] [PubMed] [Google Scholar]
- de Jong MD, Simmons CP, Thanh TT, Hien VM, Smith GJ, Chau TN, Hoang DM, Chau NV, Khanh TH, Dong VC, Qui PT, Cam BV, Ha do Q, Guan Y, Peiris JS, Chinh NT, Hien TT, Farrar J. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nature Medicine. 2006;12(10):1203–1207. doi: 10.1038/nm1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de la Luna S, Fortes P, Beloso A, Ortin J. Influenza virus NS1 protein enhances the rate of translation initiation of viral mRNAs. Journal of Virology. 1995;69(4):2427–2433. doi: 10.1128/jvi.69.4.2427-2433.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit E, Munster VJ, van Riel D, Beyer WE, Rimmelzwaan GF, Kuiken T, Osterhaus AD, Fouchier RA. Molecular determinants of adaptation of highly pathogenic avian influenza H7N7 viruses to efficient replication in the human host. Journal of Virology. 2010;84(3):1597–1606. doi: 10.1128/JVI.01783-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deshpande KL, Fried VA, Ando M, Webster RG. Glycosylation affects cleavage of an H5N2 influenza virus hemagglutinin and regulates virulence. Proceedings of the National Academy of Sciences of the United States of America. 1987;84(1):36–40. doi: 10.1073/pnas.84.1.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Droebner K, Reiling SJ, Planz O. Role of hypercytokinemia in NF-kappaB p50-deficient mice after H5N1 influenza A virus infection. Journal of Virology. 2008;82(22):11461–11466. doi: 10.1128/JVI.01071-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan S, Deng G, Song J, Tian G, Suo Y, Jiang Y, Guan Y, Bu Z, Kawaoka Y, Chen H. Two amino acid residues in the matrix protein M1 contribute to the virulence difference of H5N1 avian influenza viruses in mice. Virology. 2009a;384(1):28–32. doi: 10.1016/j.virol.2008.11.044. [DOI] [PubMed] [Google Scholar]
- Fan S, Gao Y, Shinya K, Li CK, Li Y, Shi J, Jiang Y, Suo Y, Tong T, Zhong G, Song J, Zhang Y, Tian G, Guan Y, Xu XN, Bu Z, Kawaoka Y, Chen H. Immunogenicity and protective efficacy of a live attenuated H5N1 vaccine in nonhuman primates. PLoS Pathogens. 2009b;5(5):e1000409. doi: 10.1371/journal.ppat.1000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fornek JL, Gillim-Ross L, Santos C, Carter V, Ward JM, Cheng LI, Proll S, Katze MG, Subbarao K. A single-amino-acid substitution in a polymerase protein of an H5N1 influenza virus is associated with systemic infection and impaired T-cell activation in mice. Journal of Virology. 2009;83(21):11102–11115. doi: 10.1128/JVI.00994-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabriel G, Herwig A, Klenk HD. Interaction of polymerase subunit PB2 and NP with importin alpha1 is a determinant of host range of influenza A virus. PLoS Pathogens. 2008;4(2):e11. doi: 10.1371/journal.ppat.0040011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabriel G, Klingel K, Otte A, Thiele S, Hudjetz B, Arman-Kalcek G, Sauter M, Shmidt T, Rother F, Baumgarte S, Keiner B, Hartmann E, Bader M, Brownlee GG, Fodor E, Klenk HD. Differential use of importin-alpha isoforms governs cell tropism and host adaptation of influenza virus. Nature Communications. 2011;2:156. doi: 10.1038/ncomms1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao P, Watanabe S, Ito T, Goto H, Wells K, McGregor M, Cooley AJ, Kawaoka Y. Biological heterogeneity, including systemic replication in mice, of H5N1 influenza A virus isolates from humans in Hong Kong. Journal of Virology. 1999;73(4):3184–3189. doi: 10.1128/jvi.73.4.3184-3189.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Y, Zhang Y, Shinya K, Deng G, Jiang Y, Li Z, Guan Y, Tian G, Li Y, Shi J, Liu L, Zeng X, Bu Z, Xia X, Kawaoka Y, Chen H. Identification of amino acids in HA and PB2 critical for the transmission of H5N1 avian influenza viruses in a mammalian host. PLoS Pathogens. 2009;5(12):e1000709. doi: 10.1371/journal.ppat.1000709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Sastre A. Inhibition of interferon-mediated antiviral responses by influenza A viruses and other negative-strand RNA viruses. Virology. 2001;279(2):375–384. doi: 10.1006/viro.2000.0756. [DOI] [PubMed] [Google Scholar]
- Garten RJ, Davis CT, Russell CA, Shu B, Lindstrom S, Balish A, Sessions WM, Xu X, Skepner E, Deyde V, Okomo-Adhiambo M, Gubareva L, Barnes J, Smith CB, Emery SL, Hillman MJ, Rivailler P, Smagala J, de Graaf M, Burke DF, Fouchier RA, Pappas C, Alpuche-Aranda CM, Lopez-Gatell H, Olivera H, Lopez I, Myers CA, Faix D, Blair PJ, Yu C, Keene KM, Dotson PD, Jr, Boxrud D, Sambol AR, Abid SH, St George K, Bannerman T, Moore AL, Stringer DJ, Blevins P, Demmler-Harrison GJ, Ginsberg M, Kriner P, Waterman S, Smole S, Guevara HF, Belongia EA, Clark PA, Beatrice ST, Donis R, Katz J, Finelli L, Bridges CB, Shaw M, Jernigan DB, Uyeki TM, Smith DJ, Klimov AI, Cox NJ. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science. 2009;325(5937):197–201. doi: 10.1126/science.1176225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giese M, Harder TC, Teifke JP, Klopfleisch R, Breithaupt A, Mettenleiter TC, Vahlenkamp TW. Experimental infection and natural contact exposure of dogs with avian influenza virus (H5N1) Emerging Infectious Diseases. 2008;14(2):308–310. doi: 10.3201/eid1402.070864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillim-Ross L, Santos C, Chen Z, Aspelund A, Yang CF, Ye D, Jin H, Kemble G, Subbarao K. Avian influenza h6 viruses productively infect and cause illness in mice and ferrets. Journal of Virology. 2008;82(21):10854–10863. doi: 10.1128/JVI.01206-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golebiewski L, Liu H, Javier RT, Rice AP. The avian influenza virus NS1 ESEV PDZ binding motif associates with Dlg1 and Scribble to disrupt cellular tight junctions. Journal of Virology. 2011;85(20):10639–10648. doi: 10.1128/JVI.05070-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Govorkova EA, Gambaryan AS, Claas EC, Smirnov YA. Amino acid changes in the hemagglutinin and matrix proteins of influenza a (H2) viruses adapted to mice. Acta Virologica. 2000;44(5):241–248. [PubMed] [Google Scholar]
- Govorkova EA, Ilyushina NA, Marathe BM, McClaren JL, Webster RG. Competitive fitness of oseltamivir-sensitive and -resistant highly pathogenic H5N1 influenza viruses in a ferret model. Journal of Virology. 2010;84(16):8042–8050. doi: 10.1128/JVI.00689-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Govorkova EA, Rehg JE, Krauss S, Yen HL, Guan Y, Peiris M, Nguyen TD, Hanh TH, Puthavathana P, Long HT, Buranathai C, Lim W, Webster RG, Hoffmann E. Lethality to ferrets of H5N1 influenza viruses isolated from humans and poultry in 2004. Journal of Virology. 2005;79(4):2191–2198. doi: 10.1128/JVI.79.4.2191-2198.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimm D, Staeheli P, Hufbauer M, Koerner I, Martinez-Sobrido L, Solorzano A, Garcia-Sastre A, Haller O, Kochs G. Replication fitness determines high virulence of influenza A virus in mice carrying functional Mx1 resistance gene. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(16):6806–6811. doi: 10.1073/pnas.0701849104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO/OIE/FAO H5N1 Evolution Working Group. Continued evolution of highly pathogenic avian influenza A (H5N1): updated nomenclature. Influenza and Other Respiratory Viruses. 2012;6(1):1–5. doi: 10.1111/j.1750-2659.2011.00298.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubareva LV, McCullers JA, Bethell RC, Webster RG. Characterization of influenza A/HongKong/156/97 (H5N1) virus in a mouse model and protective effect of zanamivir on H5N1 infection in mice. Journal of Infectious Diseases. 1998;178(6):1592–1596. doi: 10.1086/314515. [DOI] [PubMed] [Google Scholar]
- Guo Z, Chen LM, Zeng H, Gomez JA, Plowden J, Fujita T, Katz JM, Donis RO, Sambhara S. NS1 protein of influenza A virus inhibits the function of intracytoplasmic pathogen sensor, RIG-I. American Journal of Respiratory Cell and Molecular Biology. 2007;36(3):263–269. doi: 10.1165/rcmb.2006-0283RC. [DOI] [PubMed] [Google Scholar]
- Gustin KM, Belser JA, Wadford DA, Pearce MB, Katz JM, Tumpey TM, Maines TR. Influenza virus aerosol exposure and analytical system for ferrets. Proceedings of the National Academy of Sciences of the United States of America. 2011a;108(20):8432–8437. doi: 10.1073/pnas.1100768108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustin KM, Maines TR, Belser JA, van Hoeven N, Lu X, Dong L, Isakova-Sivak I, Chen LM, Voeten JT, Heldens JG, van den Bosch H, Cox NJ, Tumpey TM, Klimov AI, Rudenko L, Donis RO, Katz JM. Comparative immunogenicity and cross-clade protective efficacy of mammalian cell-grown inactivated and live attenuated H5N1 reassortant vaccines in ferrets. Journal of Infectious Diseases. 2011b;204(10):1491–1499. doi: 10.1093/infdis/jir596. [DOI] [PubMed] [Google Scholar]
- Hale BG, Albrecht RA, Garcia-Sastre A. Innate immune evasion strategies of influenza viruses. Future Microbiology. 2010;5(1):23–41. doi: 10.2217/fmb.09.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harder TC, Vahlenkamp TW. Influenza virus infections in dogs and cats. Veterinary Immunology and Immunopathology. 2010;134(1/2):54–60. doi: 10.1016/j.vetimm.2009.10.009. [DOI] [PubMed] [Google Scholar]
- Hatta M, Gao P, Halfmann P, Kawaoka Y. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science. 2001;293(5536):1840–1842. doi: 10.1126/science.1062882. [DOI] [PubMed] [Google Scholar]
- Hatta M, Hatta Y, Kim JH, Watanabe S, Shinya K, Nguyen T, Lien PS, Le QM, Kawaoka Y. Growth of H5N1 influenza A viruses in the upper respiratory tracts of mice. PLoS Pathogens. 2007;3(10):1374–1379. doi: 10.1371/journal.ppat.0030133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatta Y, Hershberger K, Shinya K, Proll SC, Dubielzig RR, Hatta M, Katze MG, Kawaoka Y, Suresh M. Viral replication rate regulates clinical outcome and CD8 T cell responses during highly pathogenic H5N1 influenza virus infection in mice. PLoS Pathogens. 2010;6(10):e1001139. doi: 10.1371/journal.ppat.1001139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden FG, Fritz R, Lobo MC, Alvord W, Strober W, Straus SE. Local and systemic cytokine responses during experimental human influenza A virus infection. Relation to symptom formation and host defense. Journal of Clinical Investigation. 1998;101(3):643–649. doi: 10.1172/JCI1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heldens JG, Glansbeek HL, Hilgers LA, Haenen B, Stittelaar KJ, Osterhaus AD, van den Bosch JF. Feasibility of single-shot H5N1 influenza vaccine in ferrets, macaques and rabbits. Vaccine. 2010;28(51):8125–8131. doi: 10.1016/j.vaccine.2010.09.097. [DOI] [PubMed] [Google Scholar]
- Hennet T, Ziltener HJ, Frei K, Peterhans E. A kinetic study of immune mediators in the lungs of mice infected with influenza A virus. Journal of Immunology. 1992;149(3):932–939. [PubMed] [Google Scholar]
- Herfst S, Schrauwen EJ, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. Airborne transmission of influenza A/H5N1 virus between ferrets. Science. 2012;336(6088):1534–1541. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horimoto T, Kawaoka Y. Reverse genetics provides direct evidence for a correlation of hemagglutinin cleavability and virulence of an avian influenza A virus. Journal of Virology. 1994;68(5):3120–3128. doi: 10.1128/jvi.68.5.3120-3128.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulse-Post DJ, Franks J, Boyd K, Salomon R, Hoffmann E, Yen HL, Webby RJ, Walker D, Nguyen TD, Webster RG. Molecular changes in the polymerase genes (PA and PB1) associated with high pathogenicity of H5N1 influenza virus in mallard ducks. Journal of Virology. 2007;81(16):8515–8524. doi: 10.1128/JVI.00435-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland L, Webby R, Sandbulte MR, Clarke B, Hou S. Influenza virus NS1 protein protects against lymphohematopoietic pathogenesis in an in vivo mouse model. Virology. 2006;349(1):156–163. doi: 10.1016/j.virol.2006.02.012. [DOI] [PubMed] [Google Scholar]
- Ibricevic A, Pekosz A, Walter MJ, Newby C, Battaile JT, Brown EG, Holtz-man MJ, Brody SL. Influenza virus receptor specificity and cell tropism in mouse and human airway epithelial cells. Journal of Virology. 2006;80(15):7469–7480. doi: 10.1128/JVI.02677-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ichinohe T, Nagata N, Strong P, Tamura S, Takahashi H, Ninomiya A, Imai M, Odagiri T, Tashiro M, Sawa H, Chiba J, Kurata T, Sata T, Hasegawa H. Prophylactic effects of chitin microparticles on highly pathogenic H5N1 influenza virus. Journal of Medical Virology. 2007;79(6):811–819. doi: 10.1002/jmv.20837. [DOI] [PubMed] [Google Scholar]
- Ilyushina NA, Seiler JP, Rehg JE, Webster RG, Govorkova EA. Effect of neuraminidase inhibitor-resistant mutations on pathogenicity of clade 2.2 A/Turkey/15/06 (H5N1) influenza virus in ferrets. PLoS Pathogens. 2010;6(5):e1000933. doi: 10.1371/journal.ppat.1000933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai H, Shinya K, Takano R, Kiso M, Muramoto Y, Sakabe S, Murakami S, Ito M, Yamada S, Le MT, Nidom CA, Sakai-Tagawa Y, Takahashi K, Omori Y, Noda T, Shimojima M, Kakugawa S, Goto H, Iwatsuki-Horimoto K, Horimoto T, Kawaoka Y. The HA and NS genes of human H5N1 influenza A virus contribute to high virulence in ferrets. PLoS Pathogens. 2010;6(9):e1001106. doi: 10.1371/journal.ppat.1001106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature. 2012;486(7403):420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai Y, Kuba K, Neely GG, Yaghubian-Malhami R, Perkmann T, van Loo G, Ermolaeva M, Veldhuizen R, Leung YH, Wang H, Liu H, Sun Y, Pasparakis M, Kopf M, Mech C, Bavari S, Peiris JS, Slutsky AS, Akira S, Hultqvist M, Holmdahl R, Nicholls J, Jiang C, Binder CJ, Penninger JM. Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell. 2008;133(2):235–249. doi: 10.1016/j.cell.2008.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itoh Y, Ozaki H, Tsuchiya H, Okamoto K, Torii R, Sakoda Y, Kawaoka Y, Ogasawara K, Kida H. A vaccine prepared from a non-pathogenic H5N1 avian influenza virus strain confers protective immunity against highly pathogenic avian influenza virus infection in cynomolgus macaques. Vaccine. 2008;26(4):562–572. doi: 10.1016/j.vaccine.2007.11.031. [DOI] [PubMed] [Google Scholar]
- Jackson D, Hossain MJ, Hickman D, Perez DR, Lamb RA. A new influenza virus virulence determinant: the NS1 protein four C-terminal residues modulate pathogenicity. Proceedings of the National Academy of Sciences of the United States of America. 2008;105(11):4381–4386. doi: 10.1073/pnas.0800482105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson S, Van Hoeven N, Chen LM, Maines TR, Cox NJ, Katz JM, Donis RO. Reassortment between avian H5N1 and human H3N2 influenza viruses in ferrets: a public health risk assessment. Journal of Virology. 2009;83(16):8131–8140. doi: 10.1128/JVI.00534-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagger BW, Wise HM, Kash JC, Walters KA, Wills NM, Xiao YL, Dunfee RL, Schwartzman LM, Ozinsky A, Bell GL, Dalton RM, Lo A, Efstathiou S, Atkins JF, Firth AE, Taubenberger JK, Digard P. An overlapping protein-coding region in influenza A virus segment 3 modulates the host response. Science. 2012;337(6091):199–204. doi: 10.1126/science.1222213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao P, Tian G, Li Y, Deng G, Jiang Y, Liu C, Liu W, Bu Z, Kawaoka Y, Chen H. A single-amino-acid substitution in the NS1 protein changes the pathogenicity of H5N1 avian influenza viruses in mice. Journal of Virology. 2008;82(3):1146–1154. doi: 10.1128/JVI.01698-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julkunen I, Sareneva T, Pirhonen J, Ronni T, Melen K, Matikainen S. Molecular pathogenesis of influenza A virus infection and virus-induced regulation of cytokine gene expression. Cytokine and Growth Factor Reviews. 2001;12(2/3):171–180. doi: 10.1016/s1359-6101(00)00026-5. [DOI] [PubMed] [Google Scholar]
- Kalthoff D, Hoffmann B, Harder T, Durban M, Beer M. Experimental infection of cattle with highly pathogenic avian influenza virus (H5N1) Emerging Infectious Diseases. 2008;14(7):1132–1134. doi: 10.3201/eid1407.071468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandun IN, Wibisono H, Sedyaningsih ER, Yusharmen Hadisoedarsuno W, Purba W, Santoso H, Septiawati C, Tresnaningsih E, Heriyanto B, Yuwono D, Harun S, Soeroso S, Giriputra S, Blair PJ, Jeremijenko A, Kosasih H, Put-nam SD, Samaan G, Silitonga M, Chan KH, Poon LL, Lim W, Klimov A, Lindstrom S, Guan Y, Donis R, Katz J, Cox N, Peiris M, Uyeki TM. Three Indonesian clusters of H5N1 virus infection in 2005. New England Journal of Medicine. 2006;355(21):2186–2194. doi: 10.1056/NEJMoa060930. [DOI] [PubMed] [Google Scholar]
- Katz JM, Lu X, Frace AM, Morken T, Zaki SR, Tumpey TM. Pathogenesis of and immunity to avian influenza A H5 viruses. Biomedicine and Pharmacotherapy. 2000;54(4):178–187. doi: 10.1016/S0753-3322(00)89024-1. [DOI] [PubMed] [Google Scholar]
- Kawaoka Y, Krauss S, Webster RG. Avian-to-human transmission of the PB1 gene of influenza A viruses in the 1957 and 1968 pandemics. Journal of Virology. 1989;63(11):4603–4608. doi: 10.1128/jvi.63.11.4603-4608.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JH, Hatta M, Watanabe S, Neumann G, Watanabe T, Kawaoka Y. Role of host-specific amino acids in the pathogenicity of avian H5N1 influenza viruses in mice. Journal of General Virology. 2010;91(Pt 5):1284–1289. doi: 10.1099/vir.0.018143-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiso M, Ozawa M, Le MT, Imai H, Takahashi K, Kakugawa S, Noda T, Horimoto T, Kawaoka Y. Effect of an asparagine-to-serine mutation at position 294 in neuraminidase on the pathogenicity of highly pathogenic H5N1 influenza A virus. Journal of Virology. 2011;85(10):4667–4672. doi: 10.1128/JVI.00047-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobasa D, Jones SM, Shinya K, Kash JC, Copps J, Ebihara H, Hatta Y, Kim JH, Halfmann P, Hatta M, Feldmann F, Alimonti JB, Fernando L, Li Y, Katze MG, Feldmann H, Kawaoka Y. Aberrant innate immune response in lethal infection of macaques with the 1918 influenza virus. Nature. 2007;445(7125):319–323. doi: 10.1038/nature05495. [DOI] [PubMed] [Google Scholar]
- Krenn BM, Egorov A, Romanovskaya-Romanko E, Wolschek M, Nakowitsch S, Ruthsatz T, Kiefmann B, Morokutti A, Humer J, Geiler J, Cinatl J, Michaelis M, Wressnigg N, Sturlan S, Ferko B, Batishchev OV, Indenbom AV, Zhu R, Kastner M, Hinterdorfer P, Kiselev O, Muster T, Romanova J. Single HA2 mutation increases the infectivity and immunogenicity of a live attenuated H5N1 intranasal influenza vaccine candidate lacking NS1. PLoS One. 2011;6(4):e18577. doi: 10.1371/journal.pone.0018577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuiken T, Fouchier R, Rimmelzwaan G, Osterhaus A, Roeder P. Feline friend or potential foe? Nature. 2006;440(7085):741–742. doi: 10.1038/440741a. [DOI] [PubMed] [Google Scholar]
- Kuiken T, Rimmelzwaan G, van Riel D, van Amerongen G, Baars M, Fouchier R, Osterhaus A. Avian H5N1 influenza in cats. Science. 2004;306(5694):241. doi: 10.1126/science.1102287. [DOI] [PubMed] [Google Scholar]
- Kuiken T, Rimmelzwaan GF, Van Amerongen G, Osterhaus AD. Pathology of human influenza A (H5N1) virus infection in cynomolgus macaques (Macaca fascicularis) Veterinary Pathology. 2003;40(3):304–310. doi: 10.1354/vp.40-3-304. [DOI] [PubMed] [Google Scholar]
- Kumlin U, Olofsson S, Dimock K, Arnberg N. Sialic acid tissue distribution and influenza virus tropism. Influenza and Other Respiratory Viruses. 2008;2(5):147–154. doi: 10.1111/j.1750-2659.2008.00051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon YK, Lipatov AS, Swayne DE. Bronchointerstitial pneumonia in guinea pigs following inoculation with H5N1 high pathogenicity avian influenza virus. Veterinary Pathology. 2009;46(1):138–141. doi: 10.1354/vp.46-1-138. [DOI] [PubMed] [Google Scholar]
- Lednicky JA, Hamilton SB, Tuttle RS, Sosna WA, Daniels DE, Swayne DE. Ferrets develop fatal influenza after inhaling small particle aerosols of highly pathogenic avian influenza virus A/Vietnam/1203/2004 (H5N1) Virology. 2010;7:231. doi: 10.1186/1743-422X-7-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, Hatta M, Nidom CA, Muramoto Y, Watanabe S, Neumann G, Kawaoka Y. Reassortment between avian H5N1 and human H3N2 influenza viruses creates hybrid viruses with substantial virulence. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(10):4687–4692. doi: 10.1073/pnas.0912807107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J, Ishaq M, Prudence M, Xi X, Hu T, Liu Q, Guo D. Single mutation at the amino acid position 627 of PB2 that leads to increased virulence of an H5N1 avian influenza virus during adaptation in mice can be compensated by multiple mutations at other sites of PB2. Virus Research. 2009;144(1/2):123–129. doi: 10.1016/j.virusres.2009.04.008. [DOI] [PubMed] [Google Scholar]
- Li J, Li Y, Hu Y, Chang G, Sun W, Yang Y, Kang X, Wu X, Zhu Q. PB1-mediated virulence attenuation of H5N1 influenza virus in mice is associated with PB2. Journal of General Virology. 2011a;92(Pt 6):1435–1444. doi: 10.1099/vir.0.030718-0. [DOI] [PubMed] [Google Scholar]
- Li KS, Guan Y, Wang J, Smith GJ, Xu KM, Duan L, Rahardjo AP, Puthavathana P, Buranathai C, Nguyen TD, Estoepangestie AT, Chaisingh A, Auewarakul P, Long HT, Hanh NT, Webby RJ, Poon LL, Chen H, Shortridge KF, Yuen KY, Webster RG, Peiris JS. Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature. 2004;430(6996):209–213. doi: 10.1038/nature02746. [DOI] [PubMed] [Google Scholar]
- Li X, Qi W, He J, Ning Z, Hu Y, Tian J, Jiao P, Xu C, Chen J, Richt J, Ma W, Liao M. Molecular Basis of Efficient Replication and Pathogenicity of H9N2 Avian Influenza Viruses in Mice. PLoS One. 2012;7(6):e40118. doi: 10.1371/journal.pone.0040118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Li J, Belisle S, Baskin CR, Tumpey TM, Katze MG. Differential microRNA expression and virulence of avian, 1918 reassortant, and reconstructed 1918 influenza A viruses. Virology. 2011b;421(2):105–113. doi: 10.1016/j.virol.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z, Chen H, Jiao P, Deng G, Tian G, Li Y, Hoffmann E, Webster RG, Matsuoka Y, Yu K. Molecular basis of replication of duck H5N1 influenza viruses in a mammalian mouse model. Journal of Virology. 2005;79(18):12058–12064. doi: 10.1128/JVI.79.18.12058-12064.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipatov AS, Andreansky S, Webby RJ, Hulse DJ, Rehg JE, Krauss S, Perez DR, Doherty PC, Webster RG, Sangster MY. Pathogenesis of Hong Kong H5N1 influenza virus NS gene reassortants in mice: the role of cytokines and B- and T-cell responses. Journal of General Virology. 2005;86(Pt 4):1121–1130. doi: 10.1099/vir.0.80663-0. [DOI] [PubMed] [Google Scholar]
- Lipatov AS, Kwon YK, Pantin-Jackwood MJ, Swayne DE. Pathogenesis of H5N1 influenza virus infections in mice and ferret models differs according to respiratory tract or digestive system exposure. Journal of Infectious Diseases. 2009;199(5):717–725. doi: 10.1086/596740. [DOI] [PubMed] [Google Scholar]
- Long JX, Peng DX, Liu YL, Wu YT, Liu XF. Virulence of H5N1 avian influenza virus enhanced by a 15-nucleotide deletion in the viral nonstructural gene. Virus Genes. 2008;36(3):471–478. doi: 10.1007/s11262-007-0187-8. [DOI] [PubMed] [Google Scholar]
- Lowen AC, Mubareka S, Steel J, Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathogens. 2007;3(10):1470–1476. doi: 10.1371/journal.ppat.0030151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu X, Cho D, Hall H, Rowe T, Sung H, Kim W, Kang C, Mo I, Cox N, Klimov A, Katz J. Pathogenicity and antigenicity of a new influenza A (H5N1) virus isolated from duck meat. Journal of Medical Virology. 2003;69(4):553–559. doi: 10.1002/jmv.10344. [DOI] [PubMed] [Google Scholar]
- Lu X, Renshaw M, Tumpey TM, Kelly GD, Hu-Primmer J, Katz JM. Immunity to influenza A H9N2 viruses induced by infection and vaccination. Journal of Virology. 2001;75(10):4896–4901. doi: 10.1128/JVI.75.10.4896-4901.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu X, Tumpey TM, Morken T, Zaki SR, Cox NJ, Katz JM. A mouse model for the evaluation of pathogenesis and immunity to influenza A (H5N1) viruses isolated from humans. Journal of Virology. 1999;73(7):5903–5911. doi: 10.1128/jvi.73.7.5903-5911.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J, Sun Q, Mi R, Zhang H. Avian influenza A virus H5N1 causes autophagy-mediated cell death through suppression of mTOR signaling. Journal of Genetics and Genomics. 2011;38(11):533–537. doi: 10.1016/j.jgg.2011.10.002. [DOI] [PubMed] [Google Scholar]
- Maas R, Tacken M, Ruuls L, Koch G, van Rooij E, Stockhofe-Zurwieden N. Avian influenza (H5N1) susceptibility and receptors in dogs. Emerging Infectious Diseases. 2007;13(8):1219–1221. doi: 10.3201/eid1308.070393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher JA, DeStefano J. The ferret: an animal model to study influenza virus. Lab Animal (NY) 2004;33(9):50–53. doi: 10.1038/laban1004-50. [DOI] [PubMed] [Google Scholar]
- Maines TR, Belser JA, Gustin KM, van Hoeven N, Zeng H, Svitek N, von Messling V, Katz JM, Tumpey TM. Local innate immune responses and influenza virus transmission and virulence in ferrets. Journal of Infectious Diseases. 2012;205(3):474–485. doi: 10.1093/infdis/jir768. [DOI] [PubMed] [Google Scholar]
- Maines TR, Chen LM, Belser JA, Van Hoeven N, Smith E, Donis RO, Tumpey TM, Katz JM. Multiple genes contribute to the virulent phenotype observed in ferrets of an H5N1 influenza virus isolated from Thailand in 2004. Virology. 2011a;413(2):226–230. doi: 10.1016/j.virol.2011.02.005. [DOI] [PubMed] [Google Scholar]
- Maines TR, Chen LM, Matsuoka Y, Chen H, Rowe T, Ortin J, Falcon A, Nguyen TH, Mai le Q, Sedyaningsih ER, Harun S, Tumpey TM, Donis RO, Cox NJ, Subbarao K, Katz JM. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(32):12121–12126. doi: 10.1073/pnas.0605134103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maines TR, Chen LM, Van Hoeven N, Tumpey TM, Blixt O, Belser JA, Gustin KM, Pearce MB, Pappas C, Stevens J, Cox NJ, Paulson JC, Raman R, Sasisekharan R, Katz JM, Donis RO. Effect of receptor binding domain mutations on receptor binding and transmissibility of avian influenza H5N1 viruses. Virology. 2011b;413(1):139–147. doi: 10.1016/j.virol.2011.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maines TR, Lu XH, Erb SM, Edwards L, Guarner J, Greer PW, Nguyen DC, Szretter KJ, Chen LM, Thawatsupha P, Chittaganpitch M, Waicharoen S, Nguyen DT, Nguyen T, Nguyen HH, Kim JH, Hoang LT, Kang C, Phuong LS, Lim W, Zaki S, Donis RO, Cox NJ, Katz JM, Tumpey TM. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. Journal of Virology. 2005;79(18):11788–11800. doi: 10.1128/JVI.79.18.11788-11800.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maines TR, Szretter KJ, Perrone L, Belser JA, Bright RA, Zeng H, Tumpey TM, Katz JM. Pathogenesis of emerging avian influenza viruses in mammals and the host innate immune response. Immunological Reviews. 2008;225:68–84. doi: 10.1111/j.1600-065X.2008.00690.x. [DOI] [PubMed] [Google Scholar]
- Manz B, Gotz V, Wunderlich K, Eisel J, Kirchmair J, Stech J, Stech O, Chase G, Frank R, Schwemmle M. Disruption of the viral polymerase complex assembly as a novel approach to attenuate influenza A virus. Journal of Biological Chemistry. 2011;286(10):8414–8424. doi: 10.1074/jbc.M110.205534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manz B, Matrosovich M, Bovin N, Schwemmle M. A polymorphism in the hemagglutinin of the human isolate of a highly pathogenic H5N1 influenza virus determines organ tropism in mice. Journal of Virology. 2010;84(16):8316–8321. doi: 10.1128/JVI.00850-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massin P, van der Werf S, Naffakh N. Residue 627 of PB2 is a determinant of cold sensitivity in RNA replication of avian influenza viruses. Journal of Virology. 2001;75(11):5398–5404. doi: 10.1128/JVI.75.11.5398-5404.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matrosovich M, Tuzikov A, Bovin N, Gambaryan A, Klimov A, Castrucci MR, Donatelli I, Kawaoka Y. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. Journal of Virology. 2000;74(18):8502–8512. doi: 10.1128/jvi.74.18.8502-8512.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuoka Y, Swayne DE, Thomas C, Rameix-Welti MA, Naffakh N, Warnes C, Altholtz M, Donis R, Subbarao K. Neuraminidase stalk length and additional glycosylation of the hemagglutinin influence the virulence of influenza H5N1 viruses for mice. Journal of Virology. 2009;83(9):4704–4708. doi: 10.1128/JVI.01987-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley JL, Chipuk JE, Boyd KL, Van De Velde N, Green DR, McCullers JA. PB1-F2 proteins from H5N1 and 20 century pandemic influenza viruses cause immunopathology. PLoS Pathogens. 2010;6(7):e1001014. doi: 10.1371/journal.ppat.1001014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAuley JL, Hornung F, Boyd KL, Smith AM, McKeon R, Bennink J, Yewdell JW, McCullers JA. Expression of the 1918 influenza A virus PB1-F2 enhances the pathogenesis of viral and secondary bacterial pneumonia. Cell Host Microbe. 2007;2(4):240–249. doi: 10.1016/j.chom.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullers JA, Hoffmann E, Huber VC, Nickerson AD. A single amino acid change in the C-terminal domain of the matrix protein M1 of influenza B virus confers mouse adaptation and virulence. Virology. 2005;336(2):318–326. doi: 10.1016/j.virol.2005.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermott JE, Shankaran H, Eisfeld AJ, Belisle SE, Neuman G, Li C, McWeeney S, Sabourin C, Kawaoka Y, Katze MG, Waters KM. Conserved host response to highly pathogenic avian influenza virus infection in human cell culture, mouse and macaque model systems. BMC Systems Biology. 2011;5:190. doi: 10.1186/1752-0509-5-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munster VJ, de Wit E, van Riel D, Beyer WE, Rimmelzwaan GF, Osterhaus AD, Kuiken T, Fouchier RA. The molecular basis of the pathogenicity of the Dutch highly pathogenic human influenza A H7N7 viruses. Journal of Infectious Diseases. 2007;196(2):258–265. doi: 10.1086/518792. [DOI] [PubMed] [Google Scholar]
- Munster VJ, Fouchier RA. Avian influenza virus: of virus and bird ecology. Vaccine. 2009;27(45):6340–6344. doi: 10.1016/j.vaccine.2009.02.082. [DOI] [PubMed] [Google Scholar]
- Naffakh N, Tomoiu A, Rameix-Welti MA, van der Werf S. Host restriction of avian influenza viruses at the level of the ribonucleoproteins. Annual Review of Microbiology. 2008;62:403–424. doi: 10.1146/annurev.micro.62.081307.162746. [DOI] [PubMed] [Google Scholar]
- O’Brien KB, Morrison TE, Dundore DY, Heise MT, Schultz-Cherry S. A protective role for complement C3 protein during pandemic 2009 H1N1 and H5N1 influenza A virus infection. PLoS One. 2011a;6(3):e17377. doi: 10.1371/journal.pone.0017377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien KB, Schultz-Cherry S, Knoll LJ. Parasite-mediated upregulation of NK cell-derived gamma interferon protects against severe highly pathogenic H5N1 influenza virus infection. Journal of Virology. 2011b;85(17):8680–8688. doi: 10.1128/JVI.05142-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsen SJ, Ungchusak K, Sovann L, Uyeki TM, Dowell SF, Cox NJ, Aldis W, Chunsuttiwat S. Family clustering of avian influenza A (H5N1) Emerging Infectious Diseases. 2005;11(11):1799–1801. doi: 10.3201/eid1111.050646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oner AF, Bay A, Arslan S, Akdeniz H, Sahin HA, Cesur Y, Epcacan S, Yilmaz N, Deger I, Kizilyildiz B, Karsen H, Ceyhan M. Avian influenza A (H5N1) infection in eastern Turkey in 2006. New England Journal of Medicine. 2006;355(21):2179–2185. doi: 10.1056/NEJMoa060601. [DOI] [PubMed] [Google Scholar]
- Opitz B, Rejaibi A, Dauber B, Eckhard J, Vinzing M, Schmeck B, Hippenstiel S, Suttorp N, Wolff T. IFNbeta induction by influenza A virus is mediated by RIG-I which is regulated by the viral NS1 protein. Cellular Microbiology. 2007;9(4):930–938. doi: 10.1111/j.1462-5822.2006.00841.x. [DOI] [PubMed] [Google Scholar]
- Park CH, Ishinaka M, Takada A, Kida H, Kimura T, Ochiai K, Umemura T. The invasion routes of neurovirulent A/Hong Kong/483/97 (H5N1) influenza virus into the central nervous system after respiratory infection in mice. Archives of Virology. 2002;147(7):1425–1436. doi: 10.1007/s00705-001-0750-x. [DOI] [PubMed] [Google Scholar]
- Peiris JS, Yu WC, Leung CW, Cheung CY, Ng WF, Nicholls JM, Ng TK, Chan KH, Lai ST, Lim WL, Yuen KY, Guan Y. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet. 2004;363(9409):617–619. doi: 10.1016/S0140-6736(04)15595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris M, Yuen KY, Leung CW, Chan KH, Ip PL, Lai RW, Orr WK, Short-ridge KF. Human infection with influenza H9N2. Lancet. 1999;354(9182):916–917. doi: 10.1016/s0140-6736(99)03311-5. [DOI] [PubMed] [Google Scholar]
- Peng BH, Yun N, Chumakova O, Zacks M, Campbell G, Smith J, Smith J, Linde S, Linde J, Paessler S. Neuropathology of H5N1 virus infection in ferrets. Veterinary Microbiology. 2012;156(3/4):294–304. doi: 10.1016/j.vetmic.2011.11.025. [DOI] [PubMed] [Google Scholar]
- Perrone LA, Plowden JK, Garcia-Sastre A, Katz JM, Tumpey TM. H5N1 and 1918 pandemic influenza virus infection results in early and excessive infiltration of macrophages and neutrophils in the lungs of mice. PLoS Pathogens. 2008;4(8):e1000115. doi: 10.1371/journal.ppat.1000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perrone LA, Szretter KJ, Katz JM, Mizgerd JP, Tumpey TM. Mice lacking both TNF and IL-1 receptors exhibit reduced lung inflammation and delay in onset of death following infection with a highly virulent H5N1 virus. Journal of Infectious Diseases. 2010;202(8):1161–1170. doi: 10.1086/656365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed ML, Yen HL, DuBois RM, Bridges OA, Salomon R, Webster RG, Russell CJ. Amino acid residues in the fusion peptide pocket regulate the pH of activation of the H5N1 influenza virus hemagglutinin protein. Journal of Virology. 2009;83(8):3568–3580. doi: 10.1128/JVI.02238-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimmelzwaan GF, Kuiken T, van Amerongen G, Bestebroer TM, Fouchier RA, Osterhaus AD. Pathogenesis of influenza A (H5N1) virus infection in a primate model. Journal of Virology. 2001;75(14):6687–6691. doi: 10.1128/JVI.75.14.6687-6691.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimmelzwaan GF, van Riel D, Baars M, Bestebroer TM, van Amerongen G, Fouchier RA, Osterhaus AD, Kuiken T. Influenza A virus (H5N1) infection in cats causes systemic disease with potential novel routes of virus spread within and between hosts. American Journal of Pathology. 2006;168(1):176–183. doi: 10.2353/ajpath.2006.050466. quiz 364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossman JS, Lamb RA. Influenza virus assembly and budding. Virology. 2011;411(2):229–236. doi: 10.1016/j.virol.2010.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe T, Cho DS, Bright RA, Zitzow LA, Katz JM. Neurological manifestations of avian influenza viruses in mammals. Avian Diseases. 2003;47(3 Suppl):1122–1126. doi: 10.1637/0005-2086-47.s3.1122. [DOI] [PubMed] [Google Scholar]
- Ruat C, Caillet C, Bidaut A, Simon J, Osterhaus AD. Vaccination of macaques with adjuvanted formalin-inactivated influenza A virus (H5N1) vaccines: protection against H5N1 challenge without disease enhancement. Journal of Virology. 2008;82(5):2565–2569. doi: 10.1128/JVI.01928-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon R, Franks J, Govorkova EA, Ilyushina NA, Yen HL, Hulse-Post DJ, Humberd J, Trichet M, Rehg JE, Webby RJ, Webster RG, Hoffmann E. The polymerase complex genes contribute to the high virulence of the human H5N1 influenza virus isolate A/Vietnam/1203/04. Journal of Experimental Medicine. 2006;203(3):689–697. doi: 10.1084/jem.20051938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon R, Hoffmann E, Webster RG. Inhibition of the cytokine response does not protect against lethal H5N1 influenza infection. Proceedings of the National Academy of Sciences of the United States of America. 2007a;104(30):12479–12481. doi: 10.1073/pnas.0705289104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon R, Staeheli P, Kochs G, Yen HL, Franks J, Rehg JE, Webster RG, Hoffmann E. Mx1 gene protects mice against the highly lethal human H5N1 influenza virus. Cell Cycle. 2007b;6(19):2417–2421. doi: 10.4161/cc.6.19.4779. [DOI] [PubMed] [Google Scholar]
- Schmolke M, Manicassamy B, Pena L, Sutton T, Hai R, Varga ZT, Hale BG, Steel J, Perez DR, Garcia-Sastre A. Differential contribution of PB1-F2 to the virulence of highly pathogenic H5N1 influenza A virus in mammalian and avian species. PLoS Pathogens. 2011;7(8):e1002186. doi: 10.1371/journal.ppat.1002186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo SH, Hoffmann E, Webster RG. Lethal H5N1 influenza viruses escape host anti-viral cytokine responses. Nature Medicine. 2002;8(9):950–954. doi: 10.1038/nm757. [DOI] [PubMed] [Google Scholar]
- Shinya K, Gao Y, Cilloniz C, Suzuki Y, Fujie M, Deng G, Zhu Q, Fan S, Makino A, Muramoto Y, Fukuyama S, Tamura D, Noda T, Eisfeld AJ, Katze MG, Chen H, Kawaoka Y. Integrated clinical, pathologic, virologic, and transcriptomic analysis of H5N1 influenza virus-induced viral pneumonia in the rhesus macaque. Journal of Virology. 2012a;86(11):6055–6066. doi: 10.1128/JVI.00365-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinya K, Hamm S, Hatta M, Ito H, Ito T, Kawaoka Y. PB2 amino acid at position 627 affects replicative efficiency, but not cell tropism, of Hong Kong H5N1 influenza A viruses in mice. Virology. 2004;320(2):258–266. doi: 10.1016/j.virol.2003.11.030. [DOI] [PubMed] [Google Scholar]
- Shinya K, Hatta M, Yamada S, Takada A, Watanabe S, Halfmann P, Horimoto T, Neumann G, Kim JH, Lim W, Guan Y, Peiris M, Kiso M, Suzuki T, Suzuki Y, Kawaoka Y. Characterization of a human H5N1 influenza A virus isolated in 2003. Journal of Virology. 2005;79(15):9926–9932. doi: 10.1128/JVI.79.15.9926-9932.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinya K, Ito M, Makino A, Tanaka M, Miyake K, Eisfeld AJ, Kawaoka Y. The TLR4-TRIF pathway protects against H5N1 influenza virus infection. Journal of Virology. 2012b;86(1):19–24. doi: 10.1128/JVI.06168-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinya K, Makino A, Hatta M, Watanabe S, Kim JH, Hatta Y, Gao P, Ozawa M, Le QM, Kawaoka Y. Subclinical brain injury caused by H5N1 influenza virus infection. Journal of Virology. 2011a;85(10):5202–5207. doi: 10.1128/JVI.00239-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinya K, Makino A, Tanaka H, Hatta M, Watanabe T, Le MQ, Imai H, Kawaoka Y. Systemic dissemination of H5N1 influenza A viruses in ferrets and hamsters after direct intragastric inoculation. Journal of Virology. 2011b;85(10):4673–4678. doi: 10.1128/JVI.00148-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinya K, Okamura T, Sueta S, Kasai N, Tanaka M, Ginting TE, Makino A, Eisfeld AJ, Kawaoka Y. Toll-like receptor pre-stimulation protects mice against lethal infection with highly pathogenic influenza viruses. Virology Journal. 2011c;8:97. doi: 10.1186/1743-422X-8-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shope RE. The infection of ferrets with Swine influenza virus. Journal of Experimental Medicine. 1934;60(1):49–61. doi: 10.1084/jem.60.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith H, Sweet C. Lessons for human influenza from pathogenicity studies with ferrets. Reviews of Infectious Diseases. 1988;10(1):56–75. doi: 10.1093/clinids/10.1.56. [DOI] [PubMed] [Google Scholar]
- Song MS, Oh TK, Pascua PN, Moon HJ, Lee JH, Baek YH, Woo KJ, Yoon Y, Sung MH, Poo H, Kim CJ, Choi YK. Investigation of the biological indicator for vaccine efficacy against highly pathogenic avian influenza (HPAI) H5N1 virus challenge in mice and ferrets. Vaccine. 2009;27(24):3145–3152. doi: 10.1016/j.vaccine.2009.03.061. [DOI] [PubMed] [Google Scholar]
- Songserm T, Amonsin A, Jam-on R, Sae-Heng N, Pariyothorn N, Payungporn S, Theamboonlers A, Chutinimitkul S, Thanawongnuwech R, Poovorawan Y. Fatal avian influenza A H5N1 in a dog. Emerging Infectious Diseases. 2006;12(11):1744–1747. doi: 10.3201/eid1211.060542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soubies SM, Volmer C, Croville G, Loupias J, Peralta B, Costes P, Lacroux C, Guerin JL, Volmer R. Species-specific contribution of the four C-terminal amino acids of influenza A virus NS1 protein to virulence. Journal of Virology. 2010;84(13):6733–6747. doi: 10.1128/JVI.02427-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spesock A, Malur M, Hossain MJ, Chen LM, Njaa BL, Davis CT, Lipatov AS, York IA, Krug RM, Donis RO. The virulence of 1997 H5N1 influenza viruses in the mouse model is increased by correcting a defect in their NS1 proteins. Journal of Virology. 2011;85(14):7048–7058. doi: 10.1128/JVI.00417-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steel J. New strategies for the development of H5N1 subtype influenza vaccines: progress and challenges. BioDrugs. 2011;25(5):285–298. doi: 10.1007/BF03256169. [DOI] [PubMed] [Google Scholar]
- Steel J, Lowen AC, Mubareka S, Palese P. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathogens. 2009a;5(1):e1000252. doi: 10.1371/journal.ppat.1000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steel J, Lowen AC, Pena L, Angel M, Solorzano A, Albrecht R, Perez DR, Garcia-Sastre A, Palese P. Live attenuated influenza viruses containing NS1 truncations as vaccine candidates against H5N1 highly pathogenic avian influenza. Journal of Virology. 2009b;83(4):1742–1753. doi: 10.1128/JVI.01920-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinhauer DA. Role of hemagglutinin cleavage for the pathogenicity of influenza virus. Virology. 1999;258(1):1–20. doi: 10.1006/viro.1999.9716. [DOI] [PubMed] [Google Scholar]
- Subbarao EK, London W, Murphy BR. A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. Journal of Virology. 1993;67(4):1761–1764. doi: 10.1128/jvi.67.4.1761-1764.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suguitan AL, Jr, Matsuoka Y, Lau YF, Santos CP, Vogel L, Cheng LI, Orandle M, Subbarao K. The multibasic cleavage site of the hemagglutinin of highly pathogenic A/Vietnam/1203/2004 (H5N1) avian influenza virus acts as a virulence factor in a host-specific manner in mammals. Journal of Virology. 2012;86(5):2706–2714. doi: 10.1128/JVI.05546-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun R, Luo J, Gao Y, He H. Different infection routes of avian influenza A (H5N1) virus in mice. Integrative Zoology. 2009;4(4):402–408. doi: 10.1111/j.1749-4877.2009.00178.x. [DOI] [PubMed] [Google Scholar]
- Sun Y, Li C, Shu Y, Ju X, Zou Z, Wang H, Rao S, Guo F, Liu H, Nan W, Zhao Y, Yan Y, Tang J, Zhao C, Yang P, Liu K, Wang S, Lu H, Li X, Tan L, Gao R, Song J, Gao X, Tian X, Qin Y, Xu KF, Li D, Jin N, Jiang C. Inhibition of autophagy ameliorates acute lung injury caused by avian influenza A H5N1 infection. Science Signaling. 2012;5(212):ra16. doi: 10.1126/scisignal.2001931. [DOI] [PubMed] [Google Scholar]
- Swayne DE. Occupational and consumer risks from avian influenza viruses. Developmental Biology (Basel) 2006;124:85–90. [PubMed] [Google Scholar]
- Szretter KJ, Gangappa S, Belser JA, Zeng H, Chen H, Matsuoka Y, Sambhara S, Swayne DE, Tumpey TM, Katz JM. Early control of H5N1 influenza virus replication by the type I interferon response in mice. Journal of Virology. 2009;83(11):5825–5834. doi: 10.1128/JVI.02144-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szretter KJ, Gangappa S, Lu X, Smith C, Shieh WJ, Zaki SR, Sambhara S, Tumpey TM, Katz JM. Role of host cytokine responses in the pathogenesis of avian H5N1 influenza viruses in mice. Journal of Virology. 2007;81(6):2736–2744. doi: 10.1128/JVI.02336-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka H, Park CH, Ninomiya A, Ozaki H, Takada A, Umemura T, Kida H. Neurotropism of the 1997 Hong Kong H5N1 influenza virus in mice. Veterinary Microbiology. 2003;95(1/2):1–13. doi: 10.1016/s0378-1135(03)00132-9. [DOI] [PubMed] [Google Scholar]
- Taubenberger JK, Reid AH, Lourens RM, Wang R, Jin G, Fanning TG. Characterization of the 1918 influenza virus polymerase genes. Nature. 2005;437(7060):889–893. doi: 10.1038/nature04230. [DOI] [PubMed] [Google Scholar]
- To KF, Chan PK, Chan KF, Lee WK, Lam WY, Wong KF, Tang NL, Tsang DN, Sung RY, Buckley TA, Tam JS, Cheng AF. Pathology of fatal human infection associated with avian influenza A H5N1 virus. Journal of Medical Virology. 2001;63(3):242–246. doi: 10.1002/1096-9071(200103)63:3<242::aid-jmv1007>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Tolnay AE, Baskin CR, Tumpey TM, Sabourin PJ, Sabourin CL, Long JP, Pyles JA, Albrecht RA, Garcia-Sastre A, Katze MG, Bielefeldt-Ohmann H. Extrapulmonary tissue responses in cynomolgus macaques (Macaca fascicularis) infected with highly pathogenic avian influenza A (H5N1) virus. Archives of Virology. 2010;155(6):905–914. doi: 10.1007/s00705-010-0662-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tompkins SM, Zhao ZS, Lo CY, Misplon JA, Liu T, Ye Z, Hogan RJ, Wu Z, Benton KA, Tumpey TM, Epstein SL. Matrix protein 2 vaccination and protection against influenza viruses, including subtype H5N1. Emerging Infectious Diseases. 2007;13(3):426–435. doi: 10.3201/eid1303.061125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumpey TM, Lu X, Morken T, Zaki SR, Katz JM. Depletion of lymphocytes and diminished cytokine production in mice infected with a highly virulent influenza A (H5N1) virus isolated from humans. Journal of Virology. 2000;74(13):6105–6116. doi: 10.1128/jvi.74.13.6105-6116.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumpey TM, Maines TR, Van Hoeven N, Glaser L, Solorzano A, Pappas C, Cox NJ, Swayne DE, Palese P, Katz JM, Garcia-Sastre A. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science. 2007a;315(5812):655–659. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- Tumpey TM, Suarez DL, Perkins LE, Senne DA, Lee JG, Lee YJ, Mo IP, Sung HW, Swayne DE. Characterization of a highly pathogenic H5N1 avian influenza A virus isolated from duck meat. Journal of Virology. 2002;76(12):6344–6355. doi: 10.1128/JVI.76.12.6344-6355.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tumpey TM, Szretter KJ, Van Hoeven N, Katz JM, Kochs G, Haller O, Garcia-Sastre A, Staeheli P. The Mx1 gene protects mice against the pandemic 1918 and highly lethal human H5N1 influenza viruses. Journal of Virology. 2007b;81(19):10818–10821. doi: 10.1128/JVI.01116-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahlenkamp TW, Teifke JP, Harder TC, Beer M, Mettenleiter TC. Systemic influenza virus H5N1 infection in cats after gastrointestinal exposure. Influenza and Other Respiratory Viruses. 2010;4(6):379–386. doi: 10.1111/j.1750-2659.2010.00173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Brand JM, Stittelaar KJ, van Amerongen G, Rimmelzwaan GF, Simon J, de Wit E, Munster V, Bestebroer T, Fouchier RA, Kuiken T, Osterhaus AD. Severity of pneumonia due to new H1N1 influenza virus in ferrets is intermediate between that due to seasonal H1N1 virus and highly pathogenic avian influenza H5N1 virus. Journal of Infectious Diseases. 2010;201(7):993–999. doi: 10.1086/651132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hoeven N, Belser JA, Szretter KJ, Zeng H, Staeheli P, Swayne DE, Katz JM, Tumpey TM. Pathogenesis of 1918 pandemic and H5N1 influenza virus infections in a guinea pig model: antiviral potential of exogenous alpha interferon to reduce virus shedding. Journal of Virology. 2009;83(7):2851–2861. doi: 10.1128/JVI.02174-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Riel D, Munster VJ, de Wit E, Rimmelzwaan GF, Fouchier RA, Osterhaus AD, Kuiken T. H5N1 virus attachment to lower respiratory tract. Science. 2006;312(5772):399. doi: 10.1126/science.1125548. [DOI] [PubMed] [Google Scholar]
- van Riel D, Munster VJ, de Wit E, Rimmelzwaan GF, Fouchier RA, Osterhaus AD, Kuiken T. Human and avian influenza viruses target different cells in the lower respiratory tract of humans and other mammals. American Journal of Pathology. 2007;171(4):1215–1223. doi: 10.2353/ajpath.2007.070248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varga ZT, Ramos I, Hai R, Schmolke M, Garcia-Sastre A, Fernandez-Sesma A, Palese P. The influenza virus protein PB1-F2 inhibits the induction of type I interferon at the level of the MAVS adaptor protein. PLoS Pathogens. 2011;7(6):e1002067. doi: 10.1371/journal.ppat.1002067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veits J, Weber S, Stech O, Breithaupt A, Graber M, Gohrbandt S, Bogs J, Hundt J, Teifke JP, Mettenleiter TC, Stech J. Avian influenza virus hemagglu-tinins H2, H4, H8, and H14 support a highly pathogenic phenotype. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(7):2579–2584. doi: 10.1073/pnas.1109397109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan H, Sorrell EM, Song H, Hossain MJ, Ramirez-Nieto G, Monne I, Stevens J, Cattoli G, Capua I, Chen LM, Donis RO, Busch J, Paulson JC, Brockwell C, Webby R, Blanco J, Al-Natour MQ, Perez DR. Replication and transmission of H9N2 influenza viruses in ferrets: evaluation of pandemic potential. PLoS One. 2008;3(8):e2923. doi: 10.1371/journal.pone.0002923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W, Lu B, Zhou H, Suguitan AL, Jr, Cheng X, Subbarao K, Kemble G, Jin H. Glycosylation at 158N of the hemagglutinin protein and receptor binding specificity synergistically affect the antigenicity and immunogenicity of a live attenuated H5N1 A/Vietnam/1203/2004 vaccine virus in ferrets. Journal of Virology. 2010;84(13):6570–6577. doi: 10.1128/JVI.00221-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Chan CC, Yang M, Deng J, Poon VK, Leung VH, Ko KH, Zhou J, Yuen KY, Zheng BJ, Lu L. A critical role of IL-17 in modulating the B-cell response during H5N1 influenza virus infection. Cellular & Molecular Immunology. 2011;8(6):462–468. doi: 10.1038/cmi.2011.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. WHO Manual on Animal Influenza Diagnosis and Surveillance. WHO; 2002. [Google Scholar]
- WHO. Cumulative Number of Confirmed Human Cases of Avian Influenza A(H5N1) Reported to WHO 2013 [Google Scholar]
- Wong JP, Christopher ME, Viswanathan S, Karpoff N, Dai X, Das D, Sun LQ, Wang M, Salazar AM. Activation of toll-like receptor signaling pathway for protection against influenza virus infection. Vaccine. 2009;27(25/26):3481–3483. doi: 10.1016/j.vaccine.2009.01.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu C, Hu WB, Xu K, He YX, Wang TY, Chen Z, Li TX, Liu JH, Buchy P, Sun B. Amino acids 473V and 598P of PB1 from an avian-origin influenza A virus contribute to polymerase activity, especially in mammalian cells. Journal of General Virology. 2012;93(Pt 3):531–540. doi: 10.1099/vir.0.036434-0. [DOI] [PubMed] [Google Scholar]
- Xu T, Qiao J, Zhao L, He G, Li K, Wang J, Tian Y, Wang H. Effect of dexamethasone on acute respiratory distress syndrome induced by the H5N1 virus in mice. European Respiratory Journal. 2009;33(4):852–860. doi: 10.1183/09031936.00130507. [DOI] [PubMed] [Google Scholar]
- Yamada M, Bingham J, Payne J, Rookes J, Lowther S, Haining J, Robinson R, Johnson D, Middleton D. Multiple routes of invasion of wild-type Clade 1 highly pathogenic avian influenza H5N1 virus into the central nervous system (CNS) after intranasal exposure in ferrets. Acta Neuropathologica. 2012;124(4):505–516. doi: 10.1007/s00401-012-1010-8. [DOI] [PubMed] [Google Scholar]
- Yamada S, Hatta M, Staker BL, Watanabe S, Imai M, Shinya K, Sakai-Tagawa Y, Ito M, Ozawa M, Watanabe T, Sakabe S, Li C, Kim JH, Myler PJ, Phan I, Raymond A, Smith E, Stacy R, Nidom CA, Lank SM, Wiseman RW, Bimber BN, O’Connor DH, Neumann G, Stewart LJ, Kawaoka Y. Biological and structural characterization of a host-adapting amino acid in influenza virus. PLoS Pathogens. 2010;6(8):e1001034. doi: 10.1371/journal.ppat.1001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen HL, Ilyushina NA, Salomon R, Hoffmann E, Webster RG, Govorkova EA. Neuraminidase inhibitor-resistant recombinant A/Vietnam/1203/04 (H5N1) influenza viruses retain their replication efficiency and pathogenicity in vitro and in vivo. Journal of Virology. 2007a;81(22):12418–12426. doi: 10.1128/JVI.01067-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen HL, Lipatov AS, Ilyushina NA, Govorkova EA, Franks J, Yilmaz N, Douglas A, Hay A, Krauss S, Rehg JE, Hoffmann E, Webster RG. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. Journal of Virology. 2007b;81(13):6890–6898. doi: 10.1128/JVI.00170-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen KY, Chan PK, Peiris M, Tsang DN, Que TL, Shortridge KF, Cheung PT, To WK, Ho ET, Sung R, Cheng AF. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet. 1998;351(9101):467–471. doi: 10.1016/s0140-6736(98)01182-9. [DOI] [PubMed] [Google Scholar]
- Zamarin D, Garcia-Sastre A, Xiao X, Wang R, Palese P. Influenza virus PB1-F2 protein induces cell death through mitochondrial ANT3 and VDAC1. PLoS Pathogens. 2005;1(1):e4. doi: 10.1371/journal.ppat.0010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamarin D, Ortigoza MB, Palese P. Influenza A virus PB1-F2 protein contributes to viral pathogenesis in mice. Journal of Virology. 2006;80(16):7976–7983. doi: 10.1128/JVI.00415-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zell R, Krumbholz A, Eitner A, Krieg R, Halbhuber KJ, Wutzler P. Prevalence of PB1-F2 of influenza A viruses. Journal of General Virology. 2007;88(Pt 2):536–546. doi: 10.1099/vir.0.82378-0. [DOI] [PubMed] [Google Scholar]
- Zhou B, Li Y, Halpin R, Hine E, Spiro DJ, Wentworth DE. PB2 residue 158 is a pathogenic determinant of pandemic H1N1 and H5 influenza a viruses in mice. Journal of Virology. 2011;85(1):357–365. doi: 10.1128/JVI.01694-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou H, Zhu J, Tu J, Zou W, Hu Y, Yu Z, Yin W, Li Y, Zhang A, Wu Y, Yu Z, Chen H, Jin M. Effect on virulence and pathogenicity of H5N1 influenza A virus through truncations of NS1 eIF4GI binding domain. Journal of Infectious Diseases. 2010;202(9):1338–1346. doi: 10.1086/656536. [DOI] [PubMed] [Google Scholar]
- Zhou J, Sun W, Wang J, Guo J, Yin W, Wu N, Li L, Yan Y, Liao M, Huang Y, Luo K, Jiang X, Chen H. Characterization of the H5N1 highly pathogenic avian influenza virus derived from wild pikas in China. Journal of Virology. 2009;83(17):8957–8964. doi: 10.1128/JVI.00793-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu H, Ding X, Chen X, Yao P, Xu F, Xie R, Yang Z, Liang W, Zhang Y, Li Y, Shen J, He P, Guo Z, Su B, Sun S, Zhu Z. Neutralizing antibody but not hemagglutination antibody provides accurate evaluation for protective immune response to H5N1 avian influenza virus in vaccinated rabbits. Vaccine. 2011;29(33):5421–5423. doi: 10.1016/j.vaccine.2011.05.067. [DOI] [PubMed] [Google Scholar]
- Zielecki F, Semmler I, Kalthoff D, Voss D, Mauel S, Gruber AD, Beer M, Wolff T. Virulence determinants of avian H5N1 influenza A virus in mammalian and avian hosts: role of the C-terminal ESEV motif in the viral NS1 protein. Journal of Virology. 2010;84(20):10708–10718. doi: 10.1128/JVI.00610-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zitzow LA, Rowe T, Morken T, Shieh WJ, Zaki S, Katz JM. Pathogenesis of avian influenza A (H5N1) viruses in ferrets. Journal of Virology. 2002;76(9):4420–4429. doi: 10.1128/JVI.76.9.4420-4429.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]


