Abstract
Bipolar disorder refers to a group of affective disorders, which together are characterised by depressive and manic or hypomanic episodes. These disorders include: bipolar disorder type I (depressive and manic episodes: this disorder can be diagnosed on the basis of one manic episode); bipolar disorder type II (depressive and hypomanic episodes); cyclothymic disorder (hypomanic and depressive symptoms that do not meet criteria for depressive episodes); and bipolar disorder not otherwise specified (depressive and hypomanic-like symptoms that do not meet the diagnostic criteria for any of the aforementioned disorders). Bipolar disorder type II is especially difficult to diagnose accurately because of the difficulty in differentiation of this disorder from recurrent unipolar depression (recurrent depressive episodes) in depressed patients. The identification of objective biomarkers that represent pathophysiologic processes that differ between bipolar disorder and unipolar depression can both inform bipolar disorder diagnosis and provide biological targets for the development of new and personalised treatments. Neuroimaging studies could help the identification of biomarkers that differentiate bipolar disorder from unipolar depression, but the problem in detection of a clear boundary between these disorders suggests that they might be better represented as a continuum of affective disorders. Innovative combinations of neuroimaging and pattern recognition approaches can identify individual patterns of neural structure and function that accurately ascertain where a patient might lie on a behavioural scale. Ultimately, an integrative approach, with several biological measurements using different scales, could yield patterns of biomarkers (biosignatures) to help identify biological targets for personalised and new treatments for all affective disorders.
Introduction
Psychiatric illnesses are usually primarily diagnosed by careful assessment of behaviour combined with subjective reports of abnormal experiences to group patients into disease categories. However, these categories mask substantial heterogeneity. For example, a diagnosis of schizoaffective disorder is often given to people with episodes of both affective and psychotic symptoms, either alternating or occurring together, which casts some doubt on the traditional dichotomy delineating affective and psychotic disorders into discrete illness categories.1 In the absence of definitive and objective biomarkers of pathophysiological processes underlying behaviours associated with conventionally defined psychiatric illness categories, and because of the heterogeneity within, and considerable overlap between, these behaviours, appropriate diagnosis and treatment are difficult for many psychiatric illnesses. Bipolar disorder is an especially good example of a group of psychiatric illnesses that are difficult to diagnose accurately. For example, although this disorder, along with other psychiatric illnesses, is one of the ten most debilitating of all non-communicable diseases,2,3 misdiagnosis of the illness as recurrent unipolar depression occurs in 60% of patients seeking treatment for depression.4,5 We emphasise the main reasons for the challenges in diagnosis of bipolar disorder in clinical practice, describe future clinical and biological directions for improving the accuracy of diagnosis, and discuss novel approaches that are moving towards a conceptualisation of bipolar disorder and unipolar depression along an affective disorders continuum.
Bipolar disorder definitions
The origins of the categorical approach to psychiatric illness lie in the classic work of the founders of modern psychiatry, such as Emil Kraepelin. Kraepelin proposed a dichotomy between psychiatric illnesses characterised by regularly recurring episodes of notable changes in affect; and illnesses characterised by abnormal cognitions, beliefs, and experiences (ie, psychotic symptoms), which usually manifested in early adulthood and persisted throughout life.6 Kraepelin referred to the first category as “manic—depressive psychosis”, including illnesses that we now refer to as affective disorders (eg, bipolar disorder), and the second as ”dementia praecox” (premature dementia), encompassing diseases that we now refer to as psychotic disorders (eg, schizophrenia). The term bipolar was first used in 1957 by Leonhard7 for disorders comprising both manic and depressive symptoms. In 1980, the name bipolar disorder was adopted by the Diagnostic and Statistical Manual for Mental Disorders (DSM) to replace the term manic depression.
In present classification systems, bipolar disorder now refers to a group of affective disorders in which patients experience episodes of depression, characterised by low mood and related symptoms (eg, loss of pleasure and reduced energy), and episodes of either mania, characterised by elated or irritable mood or both, and related symptoms such as increased energy and reduced need for sleep, or hypomania, whose symptoms are less severe or less protracted than are those of mania. The fourth edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-IV)8 contains four main subtypes of bipolar disorder: bipolar disorder type I (episodes of depression and at least one episode of full-blown mania); bipolar disorder type II (several protracted episodes of depression and at least one hypomanic episode but no manic episodes); cyclothymic disorder (many periods of hypomanic and depressive symptoms, in which the depressive symptoms do not meet the criteria for depressive episodes); and bipolar disorder not otherwise specified (depressive and hypomanic-like symptoms and episodes that might alternate rapidly, but do not meet the full diagnostic criteria for any of the aforementioned illnesses; panel 1). The tenth edition of the International Classification of Diseases (ICD-10)9 does not discriminate between bipolar disorder types I and II. ICD-10 also requires two discrete mood episodes, at least one of which must be manic or hypomanic, for a bipolar disorder diagnosis. However, in DSM-IV, one episode of mania (or mixed mood), or one episode of hypomania plus one major depressive episode, is sufficient for a diagnosis.
Panel 1. Bipolar disorder subtypes.
Diagnostic and Statistical Manual for Mental Disorders fourth edition (DSM-IV) criteria
-
Bipolar disorder type I
At least one episode of full-blown mania or mixed episode (manic and depressive symptoms). Usually has at least one depressive episode
-
Bipolar disorder type II
Several protracted depressive episodes and at least one hypomanic episode, but no manic episodes
-
Cyclothymic disorder
Several periods of hypomanic and depressive symptoms. Depressive symptoms do not meet criteria for depressive episodes
-
Bipolar disorder not otherwise specified
Depressive and hypomanic-like symptoms and episodes that might alternate rapidly, but do not meet the full diagnostic criteria for any of the above disorders
International Classification of Diseases 10th edition (ICD-10) criteria: differences from DSM-IV
ICD-10 does not discriminate between bipolar disorder types I and II
ICD-10 requires two discrete mood episodes, at least one of which must be manic, for a bipolar disorder diagnosis. In DSM-IV, one episode of mania (or mixed mood), or one episode of hypomania plus a major depressive episode, suffice for a BD diagnosis
Why is bipolar disorder so difficult to diagnose accurately?
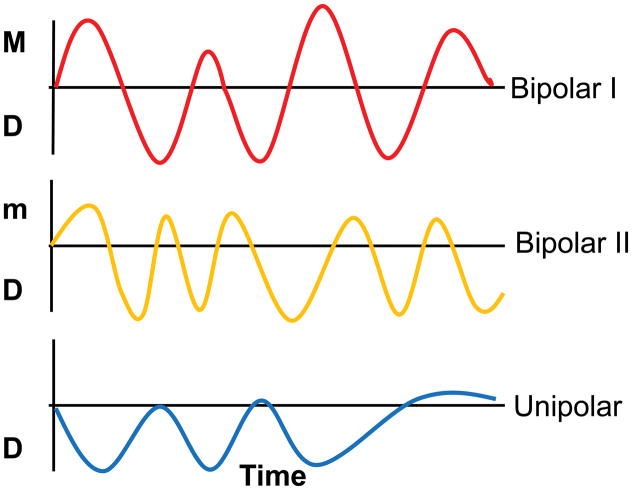
Bipolar disorder types I and II are especially difficult to diagnose accurately in clinical practice, particularly in their early stages. Only 20% of patients with bipolar disorder who are experiencing a depressive episode are diagnosed with the disorder within the first year of seeking treatment,5 and the mean delay between illness onset and diagnosis is 5–10 years.10 A major reason for the difficult diagnosis is the challenge of differentiating bipolar disorder type I or II from unipolar depression—an illness characterised by recurrent depressive episodes— especially in patients who present during a depressive episode and in those with no clear history of mania or hypomania.4,5 Unipolar depression is reportedly the most frequent misdiagnosis in patients with bipolar disorder,5 especially in bipolar disorder type II, because patients with this illness, by definition, never experience an episode of mania (figure 1).
Figure 1. Mood changes over time in bipolar disorder type I, bipolar disorder type II, and recurrent unipolar depressive disorder.
M=mania. m=hypomania. D=depression.
Another reason for the difficulty in distinction of bipolar disorder type I or II from unipolar depression is that the prevalence of depressive symptoms is higher than that of hypomanic or manic symptoms during the course of bipolar disorder type I or II, and these disorders often start with a depressive episode. People with bipolar disorder type II in particular spend much of their lives in a depressed state,5,11–13 and more time in depressive than hypomanic or manic episodes, which compounds the diagnostic problem.14 For ex ample, in two studies, people with bipolar disorder type I experienced hypomanic or manic symptoms only 9% of the time (9% of follow-up weeks),15 and individuals with bipolar disorder type II experienced hypomanic symptoms only 1% of the time (1% of follow-up weeks).16 Patients with bipolar disorder type II seek treatment for depressive symptoms much more frequently than they do for hypomanic or manic symptoms, and often do not recognise the consequences of, and thus fail to seek help for, the latter symptoms, which makes identification and treatment of these symptoms by clinicians especially difficult.
Mixed mood episodes, which are characterised by the presence of both depressive and hypomanic or manic symptoms, or a rapid alternation of the three symptom types, are being increasingly recognised as more common in people with bipolar disorder than was previously thought.17 This idea challenges the traditional view of bipolar disorder as a group of illnesses characterised by discrete depressive, hypomanic, or manic episodes. The identification of hypomanic and manic symptoms in bipolar disorder patients with a history of mixed episodes is made even more difficult, especially for less experienced clinicians, by both the reporting bias towards depressive symptoms and the absence of discrete hypomanic or manic episodes in these patients. Furthermore, increasing evidence suggests that sub threshold symptoms of bipolar disorder (ie, depressive-like, hypomanic-like, or manic-like symptoms that do not meet diagnostic thresholds for depressive, hypomanic, manic, or mixed episodes) in patients with bipolar disorder are associated with shorter time to future relapse into full-blown illness episodes than in patients without such subthreshold symptoms.18 This finding emphasises the significance of the effects of subthreshold symptoms of bipolar disorder on the future disease course.
In parallel, increasing evidence suggests that many patients diagnosed with unipolar depression might actually have a misdiagnosed bipolar disorder subtype. For example, in patients with a unipolar depression diagnosis, the 11-year rate for conversion to bipolar disorder type II is 9%,19 and the 5-year rate for development of a manic or hypomanic episode is 20%.20 Furthermore, results from antidepressant treatment trials for patients with unipolar depression indicate that up to two-thirds of these patients do not respond to first-line antidepressants, a third do not achieve full remission from symptoms after four treatments, and the rate of depression recurrence is very high, even in those who achieve remission after treatment with antidepressants.21,22
Together, these studies suggest that the boundary between bipolar disorder, particularly type II, and unipolar depression is not clear cut (panel 2), and that many people with treatment-resistant unipolar depression could have undiagnosed bipolar disorder.23 Misdiagnosis of bipolar disorder type I or II as unipolar depression has many potentially deleterious consequences, including prescription of inappropriate drugs, such as antidepressants in the absence of a mood-stabilising drug, which might lead to switching to mania, and, ultimately, poor clinical and functional outcome and high health-care costs.24–27 Accurate diagnosis of bipolar disorder in its early stages, ideally before the first episode of hypomania or mania, or when there is no clear history of hypomania or mania, could therefore help to prevent the long-term detrimental effects of misdiagnosis.
Panel 2. Challenges and clinical strategies in the diagnosis of bipolar disorder.
Reasons for the difficulty in bipolar disorder diagnosis
Diagnostic criteria for depressive episodes: are identical in bipolar disorder and unipolar depression. Bipolar disorder is thus often misdiagnosed as unipolar depression.
Many different bipolar disorder subtypes exist. Bipolar disorder type II is especially difficult to distinguish from unipolar depression, because of frequent depressive episodes and the absence of full-blown mania.
Depressive symptoms are common in bipolar disorder and their prevalence is higher than that of hypomanic or manic symptoms.
Mixed mood episodes are more common than was previously thought in bipolar disorder. These episodes might obscure detection of mania and hypomania, in view of the reporting bias towards depressive symptoms in people with bipolar disorder seeking treatment.
Subthreshold symptoms of hypomania are common in unipolar depression. These symptoms might be more common than was previously thought; they are present in 30–55% of people during a depressive episode and are common in unipolar depression. At least a subset of patients with treatment-resistant unipolar depression might have misdiagnosed bipolar disorder.
Clinical strategies to improve bipolar disorder diagnosis
Additional clinical rating scales help to detect subthreshold hypomanic symptoms in depressed people.
In DSM-5, diagnostic criteria for bipolar disorder now include both changes in mood and changes in activity or energy; the mixed mood episode definition has been changed to acknowledge the coexistence of up to three manic symptoms within a major depressive episode; and short duration hypomania is now acknowledged. Diagnostic criteria in ICD-11 and DSM-5 will be standardised.
Careful assessment for previous mania or hypomania should be done in all depressed patients, alongside collateral information from carers.
Dimensional approaches to definitions of affective disorders
In the spectrum approach, clinical measures of dimensions of lifetime affective pathology are assessed, including manic and depressive symptoms, traits, and lifestyles that comprise both fully syndromal and subthreshold mood disturbances.57
Multidimensional Assessment of Thymic States assesses state-like emotional reactivity.58,59
Research Domain Criteria propose a reclassification of psychiatric disorders on the basis of domains of information processing that include dimensions of underlying pathophysiological processes, rather than by phenomenological observations.60
Clinical strategies to improve diagnosis of bipolar disorder in depressed patients
Several changes have been recommended for the bipolar disorder section in DSM-5. First, bipolar disorder and related disorders have their own chapter. Second, the diagnostic criteria for bipolar disorder now include both changes in mood and changes in activity or energy. Previously, the diagnosis of a mixed mood episode required a patient to simultaneously meet the full criteria for both mania and major depression. A new specifier with mixed features has replaced the earlier criteria, and thus acknowledges the coexistence of up to three manic symptoms within a major depressive episode. Other amendments that acknowledge short duration hypomania will now be included in section III of DSM-5 as a mental health condition requiring further study. The recent DSM-5 field trials indicate good test–retest reliability of adult bipolar disorder type I,28 suggesting that DSM-5 could be a positive step towards improved accuracy of bipolar disorder diagnosis. Additionally, DSM-5 acknowledges that more dimensional measures should be used in research settings for the measurement of psychopathology and to better define the continuum of both manic and depressive bipolar features. Efforts are also underway to harmonise the definitions of many psychiatric illnesses in the new ICD-11 with those in DSM-5.29
New self-administered and clinician-administered rating scales have been developed to help improve early detection of clinical features suggestive of a bipolar disorder diagnosis in people with a history of depressive episodes who might otherwise be diagnosed with unipolar depression. These clinical features include subthreshold hypomania, recurrence of mood episodes, and a positive family history of bipolar disorder. Examples of these rating scales include the Bipolar Inventory Symptoms Scale,30 the Screening Assessment of Depression Polarity,31 the Hypomania Checklist,32 and the Probabilistic Approach for Bipolar Depression.33 Finally, careful assessment for previous mania or hypomania in all depressed patients, combined with collateral information from carers, can help to improve the diagnostic accuracy of bipolar disorder.
Biological approaches to identification of bipolar disorder: use of neuroimaging to identify neural circuit biomarkers of the disease
The aforementioned approaches could detect clinical features suggestive of a bipolar disorder diagnosis that might have otherwise been undetected during standard clinical assessment (panel 2). However, these clinical approaches alone cannot identify objective biomarkers that represent the underlying pathophysiologic processes that vary between bipolar disorder and unipolar depression. The identification of such biomarkers could provide biological measures to inform diagnosis of bipolar disorder in the context of a depressive episode and, perhaps even more importantly, provide biological targets for personalised treatment and for the development of new interventions for bipolar disorder depression. More studies are emphasising the importance of genetic factors that confer susceptibility to the disorder.34 Neuroimaging techniques, through analysis of abnormalities in white matter connectivity, abnormalities in grey matter, and functional abnormalities in neural circuitry subserving cognitive and emotional processes that might be aberrant in bipolar disorder and unipolar depression, show particular promise to help identify neural circuit biomarkers that could aid diagnosis of, and provide treatment targets for, bipolar disorder.35
A suitable focus for analysis in neuroimaging studies of bipolar disorder and unipolar depression is the neural circuitry that supports emotion and reward processing, and emotion regulation, since these are key processes that are abnormal in all affective disorders. These neural circuitries include subcortical systems involved in emotion and reward processing (eg, amygdala and ventral striatum); ventromedial and dorsomedial prefrontal and anterior cingulate cortical regions with roles in automatic or implicit regulation of emotion; and lateral prefrontal cortical systems (eg, ventrolateral prefrontal and dorsolateral prefrontal cortices) implicated in cognitive control and voluntary or explicit top-down regulation of emotion (appendix p 1).36,37 Patterns of mainly raised subcortical activity and reduced prefrontal cortical activity during emotion processing in depressed patients with bipolar disorder and unipolar depression have been increasingly reported,38 which suggests that functional impairments in top-down emotion regulation circuitry are present across these illnesses.
Neural circuitry abnormalities that differentiate bipolar disorder depression from unipolar depression
Surprisingly, the extent to which functional and structural abnormalities in emotion, reward, and emotion regulation neural circuitries can distinguish bipolar disorder from unipolar depression has not been well studied.38 Thus, whether objective neuroimaging biomarkers can be identified in these circuitries to distinguish these illnesses is unclear.
Nevertheless, some evidence from a few neuroimaging studies comparing patients with bipolar disorder (predominantly type I) depression versus those with unipolar depression, suggests that some neuroimaging measures could help to distinguish the two disorders, at least in patients experiencing a depressive episode. For example, more substantial abnormalities in white matter connecting key prefrontal and subcortical neural regions in emotion processing and regulation neural circuitry,39,40 and more white matter hyperintensities,41 are reported in depressed patients with bipolar disorder than in those with unipolar depression. In parallel, findings from functional neuroimaging studies indicate differential patterns of amygdala activity and prefrontal cortical–amygdala connectivity during emotion processing42 and emotion regulation in bipolar and unipolar depression,42–45 suggesting either different underlying pathophysiological processes, or varying magnitudes of similar pathophysiological processes, in these disorders.
More neuroimaging studies are clearly needed to compare patients with different bipolar disorder depression subtypes versus those with unipolar depression, since almost no such studies have made these comparisons. Existing neuroimaging studies of bipolar versus unipolar depression have several limitations. For example, many of these studies included bipolar disorder depressed and unipolar de pressed groups that were not well matched in terms of illness duration and prescribed drugs, which are potentially confounding factors on neuroimaging measures.39,42,44,46 In view of the many limitations of existing clinical measures for accurate and early diagnosis of bipolar disorder, especially for patients in a depressive episode, objective biomarkers of bipolar disorder must be identified to improve functional and clinical outcomes for people with the disease. Neuroimaging approaches are at least starting to show promise as methods to help the identification of such biomarkers. Large-scale replication and prospective longitudinal studies are the next stage for this research pathway.
Innovative approaches to the study of bipolar disorder and unipolar depression
Dimensional approaches
The clinical challenges in differentiation between bipolar disorder and unipolar depression have led to substantial debate about the phenomenological and pathophysiological associations between them. Discussion continues about whether these illnesses might be better represented as an affective disorders continuum, with variable expressions of vulnerability to hypomania or mania contributing to different phenotypes and various types of recurrent illness.47–51 For example, recent reanalyses of two epidemiological studies, the Early Developmental Stages of Psychopathology study52 and the National Comorbidity Survey Replication study,53 showed that the bipolar disorder–unipolar depression dichotomy might be questionable, since hypomanic syndromes that do not meet DSM-IV criteria for bipolar disorder type II are present in about 40% of patients with recurrent unipolar depression.
Similar findings of high rates of hypomania in patients who had otherwise received a unipolar depression diagnosis have been reported in other studies. For example, in the BRIDGE study,54,55 investigators reported that 16·1% of depressed patients with unipolar depression actually met criteria for either bipolar disorder type I or type II. Furthermore, when the strict DSM-IV criteria for bipolar disorder (manic episode) were relaxed to include increased activity or energy (ie, removal of the sole emphasis on changes in mood), and the duration cut-off for hypomanic symptoms was reduced, the percentage of people meeting criteria for type I or II bipolar disorder increased to 47%. Similarly, in a UK study, investigators reported that 17% of adults with a diagnosis of unipolar depression endorsed subthreshold hypomania.56
In view of these difficulties in categorisation of bipolar disorder and unipolar depression, some studies have now adopted dimensional criteria, such as the spectrum approach,47 in which clinical measures of dimensions of lifetime affective pathology are assessed. These measures focus on manic and depressive symptoms, traits, and lifestyles that characterise the temperamental affective dysregulations that comprise both fully syndromal and subthreshold mood disturbances.57 With the MOODS-SR (a series of self-report rating scales assessing lifetime spectra of affective symptoms), patients with unipolar depression were shown to present with many hypomanic or manic symptoms, although fewer than those reported by patients with bipolar disorder type I.47 Another example of a dimensional approach to the study of affective disorders is the Multidimensional Assessment of Thymic States,58,59 a scale that assesses state-like emotional reactivity in people with bipolar disorder.
These dimensional approaches also parallel the approach advocated by the Research Domain Criteria (RDoC) of the US National Institute of Mental Health, which proposes that psychiatric illnesses should be reclassified on the basis of information processing domains (including dimensions of underlying pathophysiological processes) rather than phenomenological observations.60 The rationale is that these dimensional measures might be more closely linked to biomarkers of pathophysiologic processes in various psychiatric illnesses than are conventional categories of disorders such as bipolar disorder and unipolar depression.
Adoption of a dimensional approach to the study of affective disorders (panel 2) could therefore potentially redefine bipolarity in terms of different underlying pathophysiological processes, including abnormalities in neural circuitry supporting emotion and reward processing, and emotion regulation. Recent neuroimaging studies have begun to use such approaches in the study of bipolar disorder and unipolar depression. In one study, investigators reported that increased right amygdala activity in response to happy emotional faces in de pressed patients with unipolar depression was associated with more MOODS sub threshold manic symptoms experienced throughout life.61 Importantly, this study was the first to show that even within the unipolar depression diagnostic category, a range of activity in key neural regions important for processing emotional stimuli, especially positive emotional stimuli, seems to exist, and is associated with the extent of subthreshold manic symptoms. In another study, investigators reported a positive correlation between activity in the ventral striatum (a key region for reward processing) during reward anticipation, and reward sensitivity in patients with bipolar disorder type I, bipolar disorder type II, and healthy people.62 This finding not only emphasises how a specific dimensional personality trait— reward sensitivity—is associated with activity in underlying reward circuitry, but also shows that this positive association is applicable to different diagnostic categories, and thus supports the RDoC approach (appendix p 2).
Pattern recognition approaches and neuroimaging
Pattern recognition approaches are an example of machine learning—a branch of artificial intelligence that develops algorithms to allow computers to automatically learn and recognise complex patterns and to use large amounts of data to make intelligent decisions. Pattern recognition approaches have been used to classify pat terns of neural activity elicited by sensory or cognitive processes63—ie, so-called mind-reading devices to predict an individual’s brain state. These approaches are now being applied in the clinic to classify groups of patients on the basis of neuroimaging data64,65 and therefore have enormous potential to help classify patients with different affective disorders into diagnostic categories. In recent studies, investigators used combinations of pattern recognition approaches and various neuroimaging techniques to discriminate among bipolar disorder type I depressed, unipolar depressed, and healthy people on the basis of whole brain activity in response to emotional and neutral faces;66 to distinguish healthy adolescents who are at high genetic risk for future bipolar disorder (because they have a parent with the disorder) from their healthy, low-risk counterparts;67 and to classify patients as bipolar disorder type I depressed versus unipolar depressed on the basis of patterns of resting blood flow in the anterior cingulate cortex.68 However, because of the dimensional approach that is being advocated, an important new development in the application of pattern recognition approaches to neuroimaging studies is their ability to place a patient at a point along a dimensional behavioural scale, on the basis of their patterns of neuroimaging data.69 This exciting development has huge potential to integrate dimensional and individualised approaches to the identification of biomarkers of affective pathology that might cut across conventionally defined diagnostic categories of illness.
Integrative biological systems approaches
To move beyond a focus on one unit of measurement can ultimately yield patterns of biomarkers representing pathology at several biological measurement levels,70 which has been emphasised in the National Institute of Mental Health RDoC, which could encompass genetic, molecular, cellular, neural circuitry, and behavioural measures. Integration across these scales could thus yield different biosignatures that represent dimensions of underlying pathophysiological processes in bipolar disorder and other affective disorders.
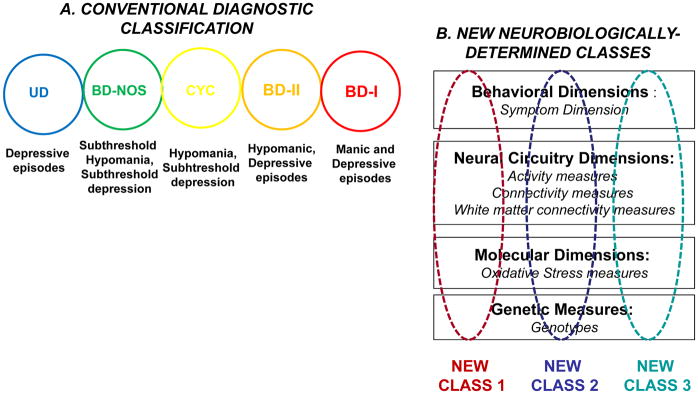
A key example of this idea is the integration of peripheral measures of oxidative stress and measures of white matter pathology in bipolar disorder. Oxidative stress is defined as an imbalance between oxidant–antioxidant systems that can ultimately lead to oxidative damage to protein, lipids, and DNA.71 Increasing evidence suggests that oxidative stress could be implicated in the pathophysiology of mood disorders, particularly bipolar disorder type I.72,73 Oxidative stress can be detected peripherally by analysis of serum measures of this factor. For example, abnormally high serum amounts of oxidative damage to lipids, proteins, and DNA have been recorded in people with bipolar disorder.74–77 Additional evidence is available from postmortem brain studies of raised amounts of lipid oxidative stress in the anterior cingulate cortex,78 and of a specific mitochondrial oxidative cascade enzymal impairment in the prefrontal cortex, probably leading to increased protein oxidation, in patients with bipolar disorder.79 In an integrated analysis of peripheral measures of oxidative stress and white matter integrity in bipolar disorder, investigators showed both substantially reduced integrity (reduced fractional anisotropy) of major white matter tracts, mainly in the prefrontal cortex, and substantially increased serum measures of lipid oxidative stress, in patients with bipolar disorder compared with healthy people.77 Furthermore, these measures correlated significantly and variance in serum measures of lipid oxidation explained nearly 60% of the variance in fractional anisotropy in these tracts. These results are similar to other findings of lower densities of oligodendroglial and glial cells in the pre frontal cortex of patients with bipolar disorder than in healthy people,80,81 and suggest that lipid oxidative stress could be a pathophysiological mechanism that underlies white matter abnormalities in bipolar disorder. These findings thereby draw attention to the potential of a combination of neuroimaging measures and serum markers of affective disorder pathology, which are also expressed at the neural circuit level, to elucidate pathophysiologic processes. This elucidation would help to identify bio signatures of dimensions of affective disorder pathology that might be applicable to a range of different affective disorders. Ultimately, this integrative approach has the potential to redefine bipolar disorder and all illnesses across the affective disorders spectrum in terms of new, neurobiologically established subgroups based on these biosignatures (figure 2).
Figure 2. Conventional diagnostic classification criteria for affective disorders compared with neurobiologically defined classes of illness.
(A) Conventional and overlapping diagnostic categories of affective disorders: bipolar disorder type I, bipolar disorder type II, cyclothymia, bipolar disorder not otherwise specified, and recurrent unipolar depressive disorder. The diagnostic criteria for these disorders are based on observable symptoms and mood episodes. (B) Examples of an integrated biological systems approach to affective disorders. New neurobiologically defined classes of affective disorders could be based on biosignatures of dimensions of pathology expressed at genetic, molecular, neural circuitry, and behavioural levels.
Conclusions
Recent evidence from field trials indicates that DSM-5 criteria might help to increase the accuracy of bipolar disorder type I diagnosis, one reason for which could be the less stringent criteria for mixed episodes. However, bipolar disorder, and bipolar disorder type II in particular, remains difficult to diagnose accurately in clinical practice, largely because of its frequent misdiagnosis as unipolar depression in depressed patients, since the diagnostic criteria for depressive episodes are identical for the two disorders. This challenge is compounded by higher prevalence of depressive than hypomanic or manic symptoms in bipolar disorder, and high rates of subthreshold manic symptoms in people diagnosed with unipolar depression. Although clinical approaches to improve the diagnosis of bipolar disorder include rating scales designed to detect subthreshold hypomanic or manic symptoms, these approaches alone cannot identify objective biomarkers that represent underlying pathophysiological processes. Promising findings from studies with different neuroimaging modalities indicate that neuroimaging measures might help to identify biomarkers to differentiate bipolar disorder from unipolar depression. However, the difficulty in identification of a clear boundary between the two disorders suggests that they might be better represented as an affective disorders continuum, with variable expressions of bipolarity representing dimensions of underlying pathophysiologic processes. Neuroimaging studies are starting to adopt this approach. Furthermore, exciting new combinations of neuroimaging and pattern recognition approaches have potential to identify individual patterns of neural circuitry structure and function that can help to both classify a patient into different categories, and place an individual at a point on a behavioural scale. Moving forward, however, the use of biological measurements across genetic, molecular, cellular, neural circuitry, and behavioural levels is imperative to yield patterns of biomarkers (bio signatures) that represent dimensions of underlying pathophysiological processes in bipolar disorder and other affective disorders. Ultimately, this integrative approach has the greatest potential to identify biological targets for personalised treatment and new treatment developments for all such illnesses (panel 3).
Panel 3. Priority unanswered questions for the diagnosis of bipolar disorder.
Can objective biomarkers be identified to discriminate between bipolar disorder and unipolar depression, and between bipolar disorder subtypes?
Do biomarkers exist that represent dimensions of pathology that cut across different diagnostic categories in the affective disorders spectrum?
Can an integrated biological systems approach identify biosignatures, which comprise biomarkers of affective disorders at different biological levels (eg, genes, cells, and neural circuitries)?
Can individual biomarkers and biosignatures be identified to improve diagnosis of, and treatment options for, affective disorders in clinical practice?
Supplementary Material
Footnotes
Contributors
MLP and DJK wrote and revised the first and final versions of the report. MLP and DJK did the literature searches and interpreted the data.
Conflicts of interest
We declare that we have no conflicts of interest.
References
- 1.Craddock N, Owen MJ. The beginning of the end for the Kraepelinian dichotomy. Br J Psychiatry. 2005;186:364–66. doi: 10.1192/bjp.186.5.364. [DOI] [PubMed] [Google Scholar]
- 2.WHO. The global burden of disease: 2004 update. Geneva: World Health Organization; 2008. [Google Scholar]
- 3.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goodwin FK, Jamison KR, Ghaemi SN. Manic-depressive illness: bipolar disorders and recurrent depression. 2. New York: Oxford University Press; 2007. [Google Scholar]
- 5.Hirschfeld RM, Lewis L, Vornik LA. Perceptions and impact of bipolar disorder: how far have we really come?. Results of the national depressive and manic-depressive association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. 2003;64:161–74. [PubMed] [Google Scholar]
- 6.Kraepelin E. Manic-depressive insanity and paranoia. New York: E & S Livingstone; 1921. [Google Scholar]
- 7.Leonhard K, Beckmann H. Classification of endogenous psychoses and their differential etiology. 2. New York: Springer; 1999. [Google Scholar]
- 8.American Psychiatric Association. Diagnostic criteria from DSM-IV-TR. Washington: American Psychiatric Association; 2000. [Google Scholar]
- 9.WHO. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. Geneva: World Health Organization; 1993. [Google Scholar]
- 10.Baldessarini RJ, Tondo L, Baethge CJ, Lepri B, Bratti IM. Effects of treatment latency on response to maintenance treatment in manic-depressive disorders. Bipolar Disord. 2007;9:386–93. doi: 10.1111/j.1399-5618.2007.00385.x. [DOI] [PubMed] [Google Scholar]
- 11.Ghaemi SN, Ko JY, Goodwin FK. “Cade’s disease” and beyond: misdiagnosis, antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry. 2002;47:125–34. doi: 10.1177/070674370204700202. [DOI] [PubMed] [Google Scholar]
- 12.Lish JD, Dime-Meenan S, Whybrow PC, Price RA, Hirschfeld RM. The National Depressive and Manic-depressive Association (DMDA) survey of bipolar members. J Affect Disord. 1994;31:281–94. doi: 10.1016/0165-0327(94)90104-x. [DOI] [PubMed] [Google Scholar]
- 13.Manning JS. Bipolar disorder in primary care. J Fam Pract. 2003;(suppl):S6–9. [PubMed] [Google Scholar]
- 14.Judd LL, Schettler PJ, Akiskal HS, et al. Long-term symptomatic status of bipolar I vs. bipolar II disorders. Int J Neuropsychopharmacol. 2003;6:127–37. doi: 10.1017/S1461145703003341. [DOI] [PubMed] [Google Scholar]
- 15.Judd LL, Akiskal HS, Schettler PJ, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002;59:530–37. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- 16.Judd LL, Akiskal HS, Schettler PJ, et al. A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. Arch Gen Psychiatry. 2003;60:261–69. doi: 10.1001/archpsyc.60.3.261. [DOI] [PubMed] [Google Scholar]
- 17.Marneros A. Origin and development of concepts of bipolar mixed states. J Affect Disord. 2001;67:229–40. doi: 10.1016/s0165-0327(01)00437-2. [DOI] [PubMed] [Google Scholar]
- 18.DeDios C, Ezquiaga E, Agud JL, et al. Subthreshold symptoms and time to relapse/recurrence in a community cohort of bipolar disorder outpatients. J Affect Disord. 2012;143:160–65. doi: 10.1016/j.jad.2012.05.047. [DOI] [PubMed] [Google Scholar]
- 19.Akiskal HS, Maser JD, Zeller PJ, et al. Switching from ‘unipolar’ to bipolar II. An 11-year prospective study of clinical and temperamental predictors in 559 patients. Arch Gen Psychiatry. 1995;52:114–23. doi: 10.1001/archpsyc.1995.03950140032004. [DOI] [PubMed] [Google Scholar]
- 20.Goldberg JF, Harrow M, Whiteside JE. Risk for bipolar illness in patients initially hospitalized for unipolar depression. Am J Psychiatry. 2001;158:1265–70. doi: 10.1176/appi.ajp.158.8.1265. [DOI] [PubMed] [Google Scholar]
- 21.Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- 22.Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905–17. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- 23.Correa R, Akiskal H, Gilmer W, Nierenberg AA, Trivedi M, Zisook S. Is unrecognized bipolar disorder a frequent contributor to apparent treatment resistant depression? J Affect Disord. 2010;127:10–18. doi: 10.1016/j.jad.2010.06.036. [DOI] [PubMed] [Google Scholar]
- 24.Valenti M, Pacchiarotti I, Bonnin CM, et al. Risk factors for antidepressant-related switch to mania. J Clin Psychiatry. 2012;73:e271–76. doi: 10.4088/JCP.11m07166. [DOI] [PubMed] [Google Scholar]
- 25.Baldessarini RJ, Salvatore P, Khalsa HM, et al. Morbidity in 303 first-episode bipolar I disorder patients. Bipolar Disord. 2010;12:264–70. doi: 10.1111/j.1399-5618.2010.00812.x. [DOI] [PubMed] [Google Scholar]
- 26.Hirschfeld RM, Lewis L, Vornik LA. Perceptions and impact of bipolar disorder: how far have we really come? Results of the national depressive and manic-depressive association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. 2003;64:161–74. [PubMed] [Google Scholar]
- 27.Goodwin GM. Bipolar depression and treatment with antidepressants. Br J Psychiatry. 2012;200:5–6. doi: 10.1192/bjp.bp.111.095349. [DOI] [PubMed] [Google Scholar]
- 28.Regier D, Narrow W, Clarke D, et al. DSM-5 field trials in the United States and Canada, part II: test-retest reliability of selected categorical disorders. Am J Psychiatry. 2013;170:59–70. doi: 10.1176/appi.ajp.2012.12070999. [DOI] [PubMed] [Google Scholar]
- 29.First MB. Harmonisation of ICD-11 and DSM-V: opportunities and challenges. Br J Psychiatry. 2009;195:382–90. doi: 10.1192/bjp.bp.108.060822. [DOI] [PubMed] [Google Scholar]
- 30.Bowden CL, Singh V, Thompson P, et al. Development of the Bipolar Inventory of Symptoms Scale. Acta Psychiatr Scand. 2007;116:189–94. doi: 10.1111/j.1600-0447.2006.00955.x. [DOI] [PubMed] [Google Scholar]
- 31.Solomon DA, Leon AC, Maser JD, et al. Distinguishing bipolar major depression from unipolar major depression with the screening assessment of depression-polarity (SAD-P) J Clin Psychiatry. 2006;67:434–42. doi: 10.4088/jcp.v67n0315. [DOI] [PubMed] [Google Scholar]
- 32.Angst J, Adolfsson R, Benazzi F, et al. The HCL-32: towards a self-assessment tool for hypomanic symptoms in outpatients. J Affect Disord. 2005;88:217–33. doi: 10.1016/j.jad.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 33.Mitchell PB, Goodwin GM, Johnson GF, Hirschfeld RMA. Diagnostic guidelines for bipolar depression: a probabilistic approach. Bipolar Disord. 2008;10:144–52. doi: 10.1111/j.1399-5618.2007.00559.x. [DOI] [PubMed] [Google Scholar]
- 34.Craddock N, Sklar P. Genetics of bipolar disorder. Lancet. 2013;381:1654–62. doi: 10.1016/S0140-6736(13)60855-7. [DOI] [PubMed] [Google Scholar]
- 35.Phillips ML, Vieta E. Identifying functional neuroimaging biomarkers of bipolar disorder: toward DSM-V. Schizophr Bull. 2007;33:893–904. doi: 10.1093/schbul/sbm060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Phillips ML, Ladouceur CD, Drevets WC. A neural model of voluntary and automatic emotion regulation: implications for understanding the pathophysiology and neurodevelopment of bipolar disorder. Mol Psychiatry. 2008;13:833–57. doi: 10.1038/mp.2008.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kupfer DJ, Frank E, Phillips ML. Major depressive disorder: new clinical, neurobiological, and treatment perspectives. Lancet. 2012;379:1045–55. doi: 10.1016/S0140-6736(11)60602-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.de Almeida JR, Phillips ML. Distinguishing between unipolar depression and bipolar depression: current and future clinical and neuroimaging perspectives. Biol Psychiatry. 2013;73:111–18. doi: 10.1016/j.biopsych.2012.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Versace A, Almeida JR, Quevedo K, et al. Right orbitofrontal corticolimbic and left corticocortical white matter connectivity differentiate bipolar and unipolar depression. Biol Psychiatry. 2010;68:560–67. doi: 10.1016/j.biopsych.2010.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Macritchie KAN, Lloyd AJ, Bastin ME, et al. White matter microstructural abnormalities in euthymic bipolar disorder. Br J Psychiatry. 2010;196:52–58. doi: 10.1192/bjp.bp.108.058586. [DOI] [PubMed] [Google Scholar]
- 41.Silverstone T, McPherson H, Li Q, Doyle T. Deep white matter hyperintensities in patients with bipolar depression, unipolar depression and age-matched control subjects. Bipolar Disord. 2003;5:53–57. doi: 10.1034/j.1399-5618.2003.01208.x. [DOI] [PubMed] [Google Scholar]
- 42.Almeida JR, Versace A, Mechelli A, et al. Abnormal amygdala-prefrontal effective connectivity to happy faces differentiates bipolar from major depression. Biol Psychiatry. 2009;66:451–59. doi: 10.1016/j.biopsych.2009.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Almeida JR, Versace A, Hassel S, Kupfer DJ, Phillips ML. Elevated amygdala activity to sad facial expressions: a state marker of bipolar but not unipolar depression. Biol Psychiatry. 2010;67:414–21. doi: 10.1016/j.biopsych.2009.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Taylor Tavares JV, Clark L, Furey ML, Williams GB, Sahakian BJ, Drevets WC. Neural basis of abnormal response to negative feedback in unmedicated mood disorders. Neuroimage. 2008;42:1118–26. doi: 10.1016/j.neuroimage.2008.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bertocci MA, Bebko GM, Mullin BC, et al. Abnormal anterior cingulate cortical activity during emotional n-back task performance distinguishes bipolar from unipolar depressed females. Psychol Med. 2012;42:1417–28. doi: 10.1017/S003329171100242X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Benedetti F, Absinta M, Rocca MA, et al. Tract-specific white matter structural disruption in patients with bipolar disorder. Bipolar Disord. 2011;13:414–24. doi: 10.1111/j.1399-5618.2011.00938.x. [DOI] [PubMed] [Google Scholar]
- 47.Cassano GB, Rucci P, Frank E, et al. The mood spectrum in unipolar and bipolar disorder: arguments for a unitary approach. Am J Psychiatry. 2004;161:1264–69. doi: 10.1176/appi.ajp.161.7.1264. [DOI] [PubMed] [Google Scholar]
- 48.Biondi M, Picardi A, Pasquini M, Gaetano P, Pancheri P. Dimensional psychopathology of depression: detection of an ‘activation’ dimension in unipolar depressed outpatients. J Affect Disord. 2005;84:133–39. doi: 10.1016/S0165-0327(02)00103-9. [DOI] [PubMed] [Google Scholar]
- 49.Akiskal HS, Mallya G. Criteria for the “soft” bipolar spectrum: treatment implications. Psychopharmacol Bull. 1987;23:68–73. [PubMed] [Google Scholar]
- 50.Angst J. The bipolar spectrum. Br J Psychiatry. 2007;190:189–91. doi: 10.1192/bjp.bp.106.030957. [DOI] [PubMed] [Google Scholar]
- 51.Vieta E, Phillips ML. Deconstructing bipolar disorder: a critical review of its diagnostic validity and a proposal for DSM-V and ICD-11. Schizophr Bull. 2007;33:886–92. doi: 10.1093/schbul/sbm057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zimmermann P, Bruckl T, Nocon A, et al. Heterogeneity of DSM-IV major depressive disorder as a consequence of subthreshold bipolarity. Arch Gen Psychiatry. 2009;66:1341–52. doi: 10.1001/archgenpsychiatry.2009.158. [DOI] [PubMed] [Google Scholar]
- 53.Angst J, Cui L, Swendsen J, et al. Major depressive disorder with subthreshold bipolarity in the National Comorbidity Survey Replication. Am J Psychiatry. 2010;167:1194–201. doi: 10.1176/appi.ajp.2010.09071011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Angst J, Azorin JM, Bowden CL, et al. Prevalence and characteristics of undiagnosed bipolar disorders in patients with a major depressive episode: the BRIDGE study. Arch Gen Psychiatry. 2011;68:791–98. doi: 10.1001/archgenpsychiatry.2011.87. [DOI] [PubMed] [Google Scholar]
- 55.Angst J, Gamma A, Bowden CL, et al. Diagnostic criteria for bipolarity based on an international sample of 5635 patients with DSM-IV major depressive episodes. Eur Arch Psychiatry Clin Neurosci. 2012;262:3–11. doi: 10.1007/s00406-011-0228-0. [DOI] [PubMed] [Google Scholar]
- 56.Forty L, Smith D, Jones L, et al. Identifying hypomanic features in major depressive disorder using the hypomania checklist (HCL-32) J Affect Disord. 2009;114:68–73. doi: 10.1016/j.jad.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 57.Cassano GB, Mula M, Rucci P, et al. The structure of lifetime manic–hypomanic spectrum. J Affect Disord. 2009;112:59–70. doi: 10.1016/j.jad.2008.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Henry C, M’Bailara K, Mathieu F, Poinsot R, Falissard B. Construction and validation of a dimensional scale exploring mood disorders: MAThyS (Multidimensional Assessment of Thymic States) BMC Psychiatry. 2008;8:82. doi: 10.1186/1471-244X-8-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Henry C, M’Bailara K, Poinsot R, et al. Evidence for two types of bipolar depression using a dimensional approach. Psychother Psychosom. 2007;76:325–31. doi: 10.1159/000107559. [DOI] [PubMed] [Google Scholar]
- 60.Insel T, Cuthbert B, Garvey M, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167:748–51. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 61.Fournier JC, Keener MT, Mullin BC, et al. Heterogeneity of amygdala response in major depressive disorder: the impact of lifetime subthreshold mania. Psychol Med. 2013;43:293–302. doi: 10.1017/S0033291712000918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Caseras X, Lawrence NS, Murphy K, Wise RG, Phillips ML. Ventral striatum activity in response to reward: differences between bipolar I and II disorders. Am J Psychiatry. 2013 doi: 10.1176/appi.ajp.2012.12020169. published online Apr 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Haynes JD, Rees G. Decoding mental states from brain activity in humans. Nat Rev Neurosci. 2006;7:523–34. doi: 10.1038/nrn1931. [DOI] [PubMed] [Google Scholar]
- 64.Koutsouleris N, Meisenzahl EM, Davatzikos C, et al. Use of neuroanatomical pattern classification to identify subjects in at-risk mental states of psychosis and predict disease transition. Arch Gen Psychiatry. 2009;66:700–12. doi: 10.1001/archgenpsychiatry.2009.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nouretdinov I, Costafreda SG, Gammerman A, et al. Machine learning classification with confidence: application of transductive conformal predictors to MRI-based diagnostic and prognostic markers in depression. Neuroimage. 2011;56:809–13. doi: 10.1016/j.neuroimage.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 66.Mourão-Miranda J, Almeida JR, Hassel S, et al. Pattern recognition analyses of brain activation elicited by happy and neutral faces in unipolar and bipolar depression. Bipolar Disord. 2012;14:451–60. doi: 10.1111/j.1399-5618.2012.01019.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mourão-Miranda J, Oliveira L, Ladouceur CD, et al. Pattern recognition and functional neuroimaging help to discriminate healthy adolescents at risk for mood disorders from low risk adolescents. PLoS One. 2012;7:e29482. doi: 10.1371/journal.pone.0029482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Almeida JRC, Mourão-Miranda J, Aizenstein HJ, et al. Pattern recognition on anterior cingulate cortex blood flow classifies depressed females with bipolar vs. unipolar depression. Br J Psychiatry. doi: 10.1192/bjp.bp.112.122838. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cohen JR, Asarnow RF, Sabb FW, et al. Decoding continuous variables from neuroimaging data: basic and clinical applications. Front Neurosci. 2011;5:75. doi: 10.3389/fnins.2011.00075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.McIntosh AM. Toward a systems biology of mood disorder. Biol Psychiatry. 2013;73:107–08. doi: 10.1016/j.biopsych.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 71.Halliwell B, Gutteridge JMC. Free radicals in biology and medicine. 4. New York: Oxford University Press; 2007. [Google Scholar]
- 72.Young LT. Is bipolar disorder a mitochondrial disease? J Psychiatry Neurosci. 2007;32:160–61. [PMC free article] [PubMed] [Google Scholar]
- 73.Andreazza AC, Kauer-Sant’anna M, Frey BN, et al. Oxidative stress markers in bipolar disorder: a meta-analysis. J Affect Disord. 2008;111:135–44. doi: 10.1016/j.jad.2008.04.013. [DOI] [PubMed] [Google Scholar]
- 74.Andreazza AC, Cassini C, Rosa AR, et al. Serum S100B and antioxidant enzymes in bipolar patients. J Psychiatr Res. 2007;41:523–29. doi: 10.1016/j.jpsychires.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 75.Yumru M, Savas HA, Kalenderoglu A, Bulut M, Celik H, Erel O. Oxidative imbalance in bipolar disorder subtypes: a comparative study. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33:1070–74. doi: 10.1016/j.pnpbp.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 76.Magalhaes PV, Dean OM, Bush AI, et al. N-acetyl cysteine add-on treatment for bipolar II disorder: a subgroup analysis of a randomized placebo-controlled trial. J Affect Disord. 2011;129:317–20. doi: 10.1016/j.jad.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 77.Versace A, Andreazza AC, Young LT, et al. Elevated serum measures of lipid peroxidation and abnormal prefrontal white matter in euthymic bipolar adults: toward peripheral biomarkers of bipolar disorder. Mol Psychiatry. 2013 doi: 10.1038/mp.2012.188. published online Jan 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang JF, Shao L, Sun X, Young LT. Increased oxidative stress in the anterior cingulate cortex of subjects with bipolar disorder and schizophrenia. Bipolar Disord. 2009;11:523–29. doi: 10.1111/j.1399-5618.2009.00717.x. [DOI] [PubMed] [Google Scholar]
- 79.Andreazza AC, Shao L, Wang JF, Young LT. Mitochondrial complex I activity and oxidative damage to mitochondrial proteins in the prefrontal cortex of patients with bipolar disorder. Arch Gen Psychiatry. 2010;67:360–68. doi: 10.1001/archgenpsychiatry.2010.22. [DOI] [PubMed] [Google Scholar]
- 80.Rajkowska G, Halaris A, Selemon LD. Reductions in neuronal and glial density characterize the dorsolateral prefrontal cortex in bipolar disorder. Biol Psychiatry. 2001;49:741–52. doi: 10.1016/s0006-3223(01)01080-0. [DOI] [PubMed] [Google Scholar]
- 81.Tkachev D, Mimmack ML, Ryan MM, et al. Oligodendrocyte dysfunction in schizophrenia and bipolar disorder. Lancet. 2003;362:798–805. doi: 10.1016/S0140-6736(03)14289-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.