Abstract
Non-alcoholic fatty liver disease (NAFLD) is an example of pathological fat accumulation in the liver and one of the major health conditions in the world. This study aimed to examine the independent role of dietary patterns in the development of NAFLD. In a cross-sectional study, 1500 individuals referred to a nutrition clinic were randomly selected, their demographic, anthropometric and blood metabolic indices were obtained, and food frequency questionnaires were completed for them. Liver stiffness was calculated using the NAFLD score formula and fibroscan. The two dominant dietary patterns identified were the “healthy” and “unhealthy dietary patterns”. A significant percentage of those with NAFLD (45%) were in the upper quartile of the unhealthy model; however, only 10% had the healthy pattern (p < 0.001). In this study, 32.9 and 13.9% of the healthy and unhealthy participants were in the upper quartile of the healthy diet pattern. Also, it was shown that waist circumference is a strong mediator of dietary patterns and NAFLD relationship, and the indirect effect of diet through abdominal circumference is 28 times greater than the direct effect on NAFLD. The results suggested that healthy and unhealthy dietary patterns are respectively associated with lower- and higher-risk of NAFLD but the role of waist circumference as a mediator deserves more consideration.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is a type of chronic liver disease characterized by oxidative stress, inflammation and fibrosis in the hepatocytes. It is an example of pathological fat accumulation (mainly triglyceride) in the liver, which shows no symptom of liver disease1. Fat constitutes over 5–10% of the liver weight in patients with NAFLD2. The disease ranges from simple steatosis to non-alcoholic steatohepatitis and occasionally cirrhosis and hepatocellular carcinoma. It is mainly associated with obesity, dyslipidemia, hypertension, type 2 diabetes and metabolic syndrome3,4.
NAFLD is one of the major health conditions worldwide, as 30% of the adult population and 60–80% of diabetic and obese patients are affected by it5,6. The prevalence of NAFLD in terms of variables such as age, gender, place of residence and race is between 12–24% in Asia. The overall prevalence of fatty liver in the general Iranian population has been estimated to be 33.9%, a relatively high figure7 which reaches 55.6% among those with type 2 diabetes8.
The etiology of NAFLD seems to be multicausal. Nutrition has been suggested as a potential environmental factor affecting the risk of NAFLD9,10. Recently, considerable attention has been focused on the associations between dietary patterns and the risk of NAFLD. In particular, it has been reported that the Mediterranean diet has a positive impact on NAFLD prevention and treatment11.
In recent years, with regards to the relationship between diet and disease, and especially, chronic disease-related diet, researchers investigated the relationships between dietary aspects and health outcomes by analyzing “diet patterns”. With such an analysis, questions on the confounding nutritional factors and the interactions between foods and nutrients were somewhat overcome. On the other hand, dietary patterns reflect the overall dietary intake and thus provide a perspective beyond the effects of nutrients or foods alone because nutrients are not consumed solely and nutrients in different foods can interact with each other or have synergistic effects12.
Due to the significance of this issue, the high prevalence of NAFLD and the fact that the onset and development of this disease are closely related to dietary pattern and lifestyle, attempts were made to examine the direct and mediated relationship between dietary patterns and NAFLD by comparing the dietary habits of those with/without NAFLD, in order to take a step towards combating and preventing the disease.
Results
Of the total sample size of 1500 individuals included in the study, 624 suffered from NAFLD (41.6%) and 876 were healthy (58.4%). Table 1 shows the baseline information of the participants of the study with/without NAFLD. Taking the relatively large sample size into account, all the study variables showed a significant difference between the two groups. No significant difference was observed between the two groups in terms of gender and smoking. The odds ratio for all the variables was calculated for NAFLD with all playing a part in its development.
Table 1.
Demographic and basic information of the participants in healthy and patient groups.
| Healthy people (N = 876) | NAFLD patient (N = 624) | P-value | OR | 95% C.I. | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Lower | Upper | ||||
| Age (years) | 34.09 | 10.26 | 57.24 | 8.69 | <0.001 | 1.243 | 1.216 | 1.27 | |
| Weight (Kg) | 79.88 | 11.90 | 98.88 | 10.05 | <0.001 | 1.148 | 1.132 | 1.163 | |
| BMI | 25.16 | 3.63 | 31.73 | 3.17 | <0.001 | 1.659 | 1.58 | 1.743 | |
| Waist circumference (cm) | 94.90 | 15.21 | 120.24 | 11.35 | <0.001 | 1.133 | 1.119 | 1.147 | |
| FBS (mg/dL) | 97.80 | 12.36 | 120.81 | 11.71 | <0.001 | 1.15 | 1.135 | 1.165 | |
| Fast Insulin (µU/mL) | 7.67 | 3.30 | 14.71 | 3.00 | <0.001 | 1.834 | 1.73 | 1.946 | |
| Two Hour Glucose (mg/dL) | 113.72 | 18.14 | 131.55 | 20.26 | <0.001 | 1.048 | 1.042 | 1.055 | |
| Two Hour Insulin (µU/mL) | 39.05 | 11.59 | 55.29 | 12.15 | <0.001 | 1.116 | 1.103 | 1.129 | |
| HOMA_IR | 0.92 | 0.23 | 1.18 | 0.22 | <0.001 | 143.4 | 81.70 | 251.8 | |
| HOMA_B | 67.77 | 16.04 | 79.54 | 18.55 | <0.001 | 1.04 | 1.034 | 1.047 | |
| LDL (mg/dL) | 92.04 | 15.00 | 114.52 | 15.88 | <0.001 | 1.095 | 1.085 | 1.105 | |
| HDL (mg/dL) | 49.48 | 7.69 | 38.44 | 6.52 | <0.001 | 0.823 | 0.807 | 0.839 | |
| TG (mg/dL) | 185.07 | 23.84 | 216.91 | 23.93 | <0.001 | 1.054 | 1.048 | 1.06 | |
| Total Cholesterol (mg/dL) | 176.59 | 14.93 | 196.55 | 15.62 | <0.001 | 1.086 | 1.076 | 1.095 | |
| Systolic Blood Pressure(mmHg) | 12.41 | 1.66 | 13.04 | 1.66 | <0.001 | 1.256 | 1.179 | 1.338 | |
| Diastolic Blood Pressure(mmHg) | 7.97 | 1.00 | 8.92 | 0.93 | <0.001 | 2.676 | 2.361 | 3.033 | |
| ALT (IU/L) | 38.93 | 12.66 | 60.46 | 12.46 | <0.001 | 1.132 | 1.119 | 1.146 | |
| AST (IU/L) | 30.99 | 12.94 | 50.72 | 11.43 | <0.001 | 1.126 | 1.113 | 1.14 | |
| GGT (IU/L) | 22.85 | 9.55 | 37.34 | 13.04 | <0.001 | 1.117 | 1.104 | 1.13 | |
| n | % | n | % | ||||||
| Sex | Female | 534 | 61.0% | 396 | 63.5% | 0.325 | 1.112 | 0.900 | 1.375 |
| Smoking | Yes | 107 | 12.2% | 71 | 11.4% | 0.622 | 0.923 | 0.671 | 1.270 |
ALT, alanine aminotransferase; AST, Aspartate Aminotransferase; BMI, body mass index; FBS, Fasting Blood Sugar; GGT, gamma-glutamyl transferase; HDL, high-density lipoprotein; HOMA-IR, homeostasis model of insulin resistance; HOMA-β, Homeostatic model assessment of β cell function; LDL, low-density lipoprotein; TG, Triglyceride.
In the next step, using factor analysis method, two dominant food patterns were identified for the participants. The foods in each group were labeled “healthy food pattern” and “unhealthy food patterns” (Table 2). The labeling is due to the considerable presence of ready-made, fried and industrial foods in one food pattern and the presence of vegetables, fruits and whole grains in the other. Table 2 shows the score of each food item in both food patterns. For simplification purposes, scores below 0.2 were deleted.
Table 2.
Load factors of food groups in the two main dietary patterns.
| Unhealthy diet | Healthy diet | |
|---|---|---|
| Processed meat | 0.522 | |
| Mayonnaise | 0.510 | |
| Egg | 0.452 | |
| Snacks | 0.422 | |
| Cereals | 0.408 | −0.250 |
| Solid. Oils | 0.392 | |
| Red Meat | 0.389 | −0.262 |
| Sweets | 0.373 | |
| Carbonated Drinks | 0.372 | |
| Fried. Potato | 0.366 | |
| Visceral Meat | 0.322 | |
| Fruit. Juice | 0.293 | |
| Industrial Fruit Juice | 0.279 | |
| High. fat. dairy | 0.276 | |
| Nuts | 0.229 | |
| salt | 0.222 | |
| Garlic | 0.221 | |
| Legumes | 0.221 | 0.210 |
| sugars | 0.210 | |
| seasoning | ||
| Margarine | ||
| Olive | ||
| Pickles | ||
| Liquid. Oils | ||
| Dried fruit | ||
| Other. Vegtables | 0.737 | |
| Yellow. Vegetables | 0.572 | |
| Dough | 0.489 | |
| Low. fat. Dairy | 0.479 | |
| Vegetables. Cabbages | 0.414 | |
| Tomato | 0.285 | 0.386 |
| poultry | 0.348 | |
| coffee | 0.326 | |
| butter | 0.227 | −0.268 |
| Potato | 0.252 | |
| Tea | ||
| fruit | ||
| Whole. wheat. bread | ||
| Fish | ||
| Green.Vegtables |
Coefficients smaller than 0.2 excluded.
Attempts were made to show the relationship between NAFLD and healthy or unhealthy diets (Table 3). Table 3 shows that although a healthy/unhealthy diet has a direct effect on NAFLD, the significance disappeared after optimization, which suggests the probability of strong mediators. A significant percentage of those with fatty liver (45%) were in the upper quartile of the unhealthy model; however, the percentage for the healthy individuals was about 10%, showing a statistically significant difference (P < 0.001). In terms of following a healthy diet, a significant percentage of healthy individuals was in the upper quartile of healthy diet (32.9%); whereas, this figure for those with fatty liver was about 13.9%. Tables 4 and 5 supplementary file shows similar results by FLI Score (43.10% of those with NAFLD was in quartile 4 of unhealthy dietary pattern vs 43.90% of healthy people was in quartile 4 of healthy dietary pattern).
Table 3.
Prevalence of fatty liver in healthy and unhealthy dietary pattern quartiles (according to NAFLD Score13).
| Fatty Liver | Crude | Adjusted* | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | P-value | OR | 95%CI | P-value | OR | 95%CI | ||||||
| N | % | N | % | lower | upper | lower | upper | ||||||
| Unhealty Diet | Q1 | 267 | 30.5% | 108 | 17.3% | ||||||||
| Q2 | 265 | 30.3% | 110 | 17.6% | 0.872 | 1.026 | 0.749 | 1.407 | 0.111 | 1.571 | 0.901 | 2.739 | |
| Q3 | 249 | 28.4% | 125 | 20.0% | 0.172 | 1.241 | 0.910 | 1.692 | 0.524 | 1.272 | 0.607 | 2.664 | |
| Q4 | 95 | 10.8% | 281 | 45.0% | <0.001 | 7.313 | 5.296 | 10.096 | 0.015 | 2.730 | 1.211 | 6.155 | |
| Healty Diet | Q1 | 160 | 18.3% | 215 | 34.5% | ||||||||
| Q2 | 208 | 23.7% | 166 | 26.6% | <0.001 | 0.594 | 0.445 | 0.793 | 0.269 | 0.764 | 0.473 | 1.232 | |
| Q3 | 220 | 25.1% | 156 | 25.0% | <0.001 | 0.528 | 0.395 | 0.705 | 0.463 | 0.829 | 0.503 | 1.367 | |
| Q4 | 288 | 32.9% | 87 | 13.9% | <0.001 | 0.225 | 0.164 | 0.308 | 0.087 | 0.614 | 0.351 | 1.074 | |
*Adjusted for Age, sex.
Table 4.
Mediators for unhealthy dietary pattern on fatty liver.
| Indirect effect | Direct effect | Indirect/direct effect | Mediator tests | |||
|---|---|---|---|---|---|---|
| Aroian | Goodman | Sobel | ||||
| Systolic Blood Pressure(mmHg) | 0.02 | 0.43 | 0.06 | 3.27 | 3.30 | 3.29 |
| HOMA_B | 0.27 | 0.41 | 0.65 | 5.42 | 5.45 | 5.43 |
| HOMA_IR | 0.01 | 0.41 | 0.03 | 5.48 | 5.50 | 5.49 |
| Two Hour Insulin (µU/mL) | 0.49 | 0.37 | 1.32 | 7.26 | 7.28 | 7.27 |
| GGT (IU/L) | 0.47 | 0.35 | 1.36 | 8.41 | 8.43 | 8.42 |
| Total Cholesterol (mg/dL) | 0.52 | 0.34 | 1.54 | 8.88 | 8.90 | 8.89 |
| Two Hour Glucose (mg/dL) | 0.35 | 0.34 | 1.06 | 8.95 | 8.98 | 8.96 |
| HDL (mg/dL) | 0.49 | 0.34 | 1.44 | 9.04 | 9.06 | 9.05 |
| Diastolic Blood Pressure(mmHg) | 0.07 | 0.34 | 0.22 | 9.05 | 9.08 | 9.06 |
| LDL (mg/dL) | 0.57 | 0.28 | 2.01 | 10.25 | 10.28 | 10.27 |
| TG (mg/dL) | 0.54 | 0.22 | 2.48 | 12.11 | 12.13 | 12.12 |
| Weight (Kg) | 0.64 | 0.18 | 3.58 | 12.65 | 12.67 | 12.66 |
| FBS (mg/dL) | 0.69 | 0.18 | 3.95 | 12.76 | 12.78 | 12.77 |
| Age (years) | 0.79 | 0.13 | 6.31 | 13.07 | 13.09 | 13.08 |
| AST (IU/L) | 0.63 | 0.15 | 4.30 | 13.50 | 13.52 | 13.51 |
| ALT (IU/L) | 0.67 | 0.14 | 4.93 | 13.51 | 13.53 | 13.52 |
| BMI | 0.56 | 0.15 | 3.73 | 13.55 | 13.57 | 13.56 |
| Fast Insulin (µU/mL) | 0.60 | 0.12 | 5.09 | 13.78 | 13.80 | 13.79 |
| Waist (cm) | 0.79 | 0.03 | 28.25 | 14.64 | 14.66 | 14.65 |
ALT, alanine aminotransferase; AST, Aspartate Aminotransferase; BMI, body mass index; FBS, Fasting Blood Sugar; GGT, gamma-glutamyl transferase; HDL, high-density lipoprotein; HOMA-IR, homeostasis model of insulin resistance; HOMA-β, Homeostatic model assessment of β cell function; LDL, low-density lipoprotein; TG, Triglyceride.
Table 5.
Mediators for healthy dietary pattern on fatty liver.
| Indirect effect | Direct effect | Indirect/direct effect | Mediator tests | |||
|---|---|---|---|---|---|---|
| Aroian | Goodman | Sobel | ||||
| Systolic Blood Pressure(mmHg) | −0.02 | −0.36 | 0.07 | −4.20 | −4.26 | −4.23 |
| HOMA_B | −0.27 | −0.34 | 0.78 | −5.07 | −5.10 | −5.08 |
| Diastolic Blood Pressure(mmHg) | −0.05 | −0.31 | 0.17 | −6.94 | −6.97 | −6.95 |
| GGT (IU/L) | −0.47 | −0.27 | 1.74 | −7.43 | −7.45 | −7.44 |
| Two Hour Insulin (µU/mL) | −0.50 | −0.28 | 1.78 | −7.52 | −7.54 | −7.53 |
| HOMA_IR | −0.02 | −0.29 | 0.06 | −7.73 | −7.75 | −7.74 |
| Two Hour Glucose (mg/dL) | −0.39 | −0.28 | 1.38 | −8.37 | −8.40 | −8.39 |
| Total Cholesterol (mg/dL) | −0.53 | −0.26 | 2.02 | −8.69 | −8.71 | −8.70 |
| HDL (mg/dL) | −0.50 | −0.25 | 1.96 | −8.78 | −8.80 | −8.79 |
| LDL (mg/dL) | −0.59 | −0.23 | 2.57 | −9.87 | −9.90 | −9.88 |
| TG (mg/dL) | −0.57 | −0.18 | 3.16 | −10.99 | −11.01 | −11.00 |
| FBS (mg/dL) | −0.71 | −0.13 | 5.35 | −11.12 | −11.13 | −11.12 |
| ALT (IU/L) | −0.67 | −0.15 | 4.32 | −11.40 | −11.42 | −11.41 |
| Weight (Kg) | −0.65 | −0.16 | 4.02 | −11.64 | −11.66 | −11.65 |
| AST (IU/L) | −0.64 | −0.14 | 4.45 | −12.00 | −12.02 | −12.01 |
| Age (years) | −0.80 | −0.08 | 9.71 | −12.01 | −12.03 | −12.02 |
| Fast Insulin (µU/mL) | −0.58 | −0.09 | 6.41 | −12.51 | −12.53 | −12.52 |
| BMI | −0.54 | −0.11 | 4.74 | −12.55 | −12.57 | −12.56 |
| Waist (cm) | −0.75 | −0.05 | 14.34 | −12.64 | −12.66 | −12.65 |
ALT, alanine aminotransferase; AST, Aspartate Aminotransferase; BMI, body mass index; FBS, Fasting Blood Sugar; GGT, gamma-glutamyl transferase; HDL, high-density lipoprotein; HOMA-IR, homeostasis model of insulin resistance; HOMA-β, Homeostatic model assessment of β cell function; LDL, low-density lipoprotein; TG, Triglyceride.
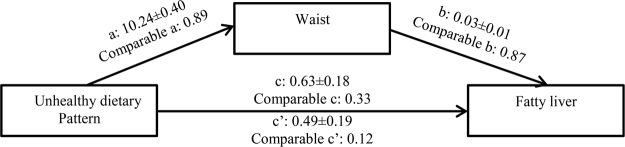
Table 4 was obtained after performing a statistical test and drawing a relationship triangle for each risk factor. This table presents a comparison of the statistic value of the Sobel test and the normal table. If the value is greater than 1.96, a significant mediator exists. The strongest mediator is the one with the greater Sobel statistic. Waist circumference is the strongest mediator. The indirect effect is the effect that a diet has on fatty liver through a mediator. The direct effect is the amount of effect exerted directly on fatty liver irrespective of a mediator. The ratio showed that the indirect diet effect through waist circumference is 28 times greater than the effect exerted on fatty liver directly. The obvious conclusion is that the nullification of this relationship through a mediator is more effective than that of a direct relationship. Waist circumference also showed the strongest relationship in the healthy diet tests (Table 5 and Fig. 1). Adjusting for age and sex showed that indirect effect of unhealthy dietary pattern on fatty liver through waist was 7.2 times more than its direct effect.
Figure 1.
Waist as the most important mediators for unhealthy dietary pattern in fatty liver.
A comparison of the quantitative characteristics of the participants among the dominant food patterns quartiles is shown in Tables 6 and 7 supplementary file correlation of each characteristics with healthy and unhealthy dietary pattern have been shown.
Discussion
The results of the current study showed the prevalence of NAFLD among an urban Iranian sample population, which indicated that 40% of males and 42% of females suffered from the disease. Meanwhile, the study of Moghaddasifar et al.7, which is a meta-analysis of 23 previous studies in Iran, indicated an onset of about 33.9% among the Iranian population, which is seen more prevalently in males. The higher prevalence of fatty liver in the current study samples may be due to various factors such as the participants’ place of residence (residency in metropolitan areas and the capital of the country) and their greater BMIs, which was about 27.8 ± 4.7, clearly showing that the participants were overweight.
Two popular scales were used to define fatty liver: the Fatty Liver Score13 and the FLI Score14, which of course, had similar results. The results of the comparison of the two methods are shown in Tables 2 and 3 of the supplementary file. The results of the Fatty Liver Score are shown in the Table 3a,b.
This study compared the nutritional behaviors of a 1500-individual sample with/without NAFLD. The extracted patterns, as the dominant food patterns used in the society, are similar to the food patterns in other studies on the Iranian society15,16. The unhealthy diet which manifested in the current study due to the high consumption of items such as processed meat, mayonnaise, eggs, red meat, carbonated beverages and sweets, had a direct and positive relationship with fatty liver disease. The participants in the highest quartile of this food pattern were more likely to develop fatty liver than those in the lowest quartile. With items such as vegetables, yellow vegetables, low-fat dairy, cabbage, tomatoes and chicken meat, the healthy food pattern stood on the opposite side of the previous pattern. This study indicates a negative relationship between fatty liver and healthy food pattern. Those who are in the highest quartile of the healthy diet demonstrated the lowest probability of developing NAFLD when compared with those in the lowest quartile. Various studies that either used the general terms “healthy and unhealthy food patterns” as a combination of foods in a pattern or described some specific food items in this type of pattern and their relationship with fatty liver, reported similar results.
The food pattern in the study of Attica, which included potatoes, red and white meat, and meat products, was associated with increased risk of metabolic syndrome, abdominal obesity and dyslipidemia17. By studying four food patterns among the Chinese people, Yang et al.18 demonstrated that those who consumed the highest amounts of animal source foods had a higher chance of developing fatty livers than those with the lowest levels of consumption (prevalence ratio (PR = 1.354; 95% Cl: 1.063–1.724). However, consumers following the cereal-vegetable pattern had a lower chance of developing fatty liver in the highest quartile when compared with the lowest one (PR = 0.777; 95% Cl:0.618–0.977). In a study on adolescents, Oddy et al.19 showed that adopting a food pattern known as the “Western Food Pattern” at the age of 14 is more prevalently associated with fatty liver at the age of 17 (odds ratio = 1.59; 95% Cl: 1.17–2.14). Their study emphasized that the use of a healthy diet at the age of 14 may prevent the development of fatty liver at the age of 17 (OR = 0.63; 95% Cl: 0.41–0.96). Jia et al.20 showed a significant relationship between NAFLD and food pattern in females only, demonstrating 2.19 times greater probability of suffering from fatty liver for those in the highest quartile of the high-carbohydrate intake food pattern (95% Cl: 1.40–3.46).
The healthy diet in the current study which is due to the high consumption of vegetables, low-fat dairy and legumes, is remarkably similar to the Mediterranean diet, which has been shown to have a preventive effect on NAFLD21–23. For example, a recent study by Baratta et al. showed that the Mediterranean diet reduces the risk of NAFLD (OR: 0.801, P = 0.018)23. With regards to the probable mechanism associated with a healthy diet and NAFLD, its effect on improving cardiometabolic profiles (such as reducing TG or blood sugar)24 or the antioxidant effects25 of diet high in vegetable content, can be pointed to. On the other hand, the recommendations of the American Heart Association, which emphasizes on dietary patterns (such as the DASH or Mediterranean diet) rather than specific food items26 can be referred to.
Other studies have discussed the relationship between food intake and fatty liver or its related conditions. In a cross-sectional study, Williams et al. reported that a balanced diet accompanied by frequent consumption of raw vegetables, salad, fruit, fish, pasta, rice, and a low consumption of fried foods, sausages, fried fish and potatoes is negatively related to abdominal obesity, glucose, plasma triglyceride and positively related to HDL levels27. Recent studies have shown that increased consumption of fruits and vegetables reduces the risk of heart attacks, ischemic heart diseases, hypertension and type 2 diabetes, and contributes to weight loss28,29.
There was a significant difference between the affected and unaffected groups in terms of fatty food (such as butter, mayonnaise, high-fat dairy products) and fast food (such as fried potatoes) consumption. Seo et al. demonstrated that fast foods have high levels of calorie and fat, thus leading to high intake of energy, fat, salt, inadequate absorption of vitamins and reluctance to consume fruits and vegetables. The high consumption of such foods is associated with weight gain, obesity and/or the risk of chronic diseases such as diabetes30,31. Another study on mice showed that fast food diets (with high levels of cholesterol, saturated fat and fructose) were associated with progressive fibrosis32,33. Other studies showed that increased fat intake and the Western Diet are associated with insulin resistance, post-meal fat metabolism and progression of NAFLD34–36.
This study showed that the consumption of sweet and soft drinks, as well as juices by the affected individuals was higher than the healthy ones. The consumption of sweet drinks is associated with the risk of obesity, metabolic syndrome, fatty liver and heart diseases, which is due to higher calories, as well as rapid and high increase of absorbable sugars37–39. These data suggest that high intake of fructose and glucose in the form of sweetened beverages may lead to changes in energy balance regulation at the central nervous system level, or maybe factors other than energy content favor increased calorie consumption and weight gain2.
In the current study, the healthy individuals consumed poultry meat more than those with NAFLD. The consumption of fish in the healthy group exceeded that in the unhealthy group. In this regard, it can be asserted from earlier studies that different types of fat might have a protective effect on NAFLD, and the most important one is omega-3 fat40. Other laboratory studies have shown that a diet rich in omega-3 fatty acids increases insulin sensitivity in rats, reduces triglyceride contents in the liver and improves fatty liver41,42.
In this study, the consumption of cereals by individuals with fatty liver exceeded that of healthy individuals. In a case-control study in China, Shi et al. reported no significant difference between the two groups in terms of intake of cereals, carbohydrates and fish in the two groups. However, the intake of fruits, vegetables and dairies in the case group was lower than that in the control group and meat intake in the case group exceeded that in the control group43.
It is noteworthy that the affected individuals used natural juices more than the healthy ones. Regarding NAFLD, studies on rodents and humans have shown that high fructose-rich diets result to liver steatosis44 and it has been reported that simple carbohydrates such as fructose increase lipogenesis in liver and prevent the oxidation of lipids45.
Finally, this hypothesis was examined to determine whether the relationship between food patterns and fatty liver is a direct one or if it interacts with other variables. Tables 4 and 5 show that waist circumference is a strong mediator in the relationship between food patterns and fatty liver. Numerous studies have discussed the relationship between waist circumference and the risk of developing fatty liver. In a meta-analysis study, Qing Pang et al.46 examined 20 well-structured studies and concluded that waist circumference is the strongest anthropometric variable in predicting fatty liver (OR = 3.14, 95%Cl: 2.07–4.77), an even stronger variable than BMI. There are evidences that insulin resistance in NAFLD is more related to waist girth than BMI, and fatty liver is a liver manifestation of metabolic syndrome46–48.
To the best of the researchers’ knowledge, no other study has considered waist circumference as a mediator of the relationship between food pattern and fatty liver in such a clear and strong relationship. It can be assumed that food patterns affect fatty liver by changing waist circumference size, which is an indication of abdominal fat accumulation. The relationship power indicates that keeping waist circumference in a normal range may prevent fatty liver, even if a proper diet is not followed.
The limitations of this study include lack of a biopsy, the most accurate method of assessing the extent of liver damage in NAFLD, which could not be performed on the outpatients, as well as the cross-sectional nature of the study which prevented it from showing causal relationships, and/or even reverse relationships.
In general, the research results suggested that a healthy diet is associated with a lower risk and an unhealthy diet pattern is associated with a higher risk of developing fatty liver. In case the study results are confirmed in prospective studies, the healthy dietary pattern can be used for the development of suitable training policies to promote nutritional awareness, to encourage individuals to follow a healthier dietary pattern and avoid following unhealthy dietary patterns, to control and prevent the development of fatty liver. Abdominal obesity should be considered as a strong mediator affecting dietary patterns and fatty liver, and international recommendations on reducing abdominal obesity should be taken seriously. It is hoped that some steps are taken to prevent NAFLD with more education on the significance of observing a healthy diet plan and reducing abdominal obesity.
Methodology
The study protocol was in accordance with the Declaration of Helsinki guidelines and was approved by the Institutional Review Board (IRB) of Fasa University of Medical Sciences (Code: IR.FUMS.REC.1396.230). Written informed consent was obtained from all the participants. It was confirmed that all the methods were performed in accordance with the relevant guidelines and regulations.
This cross-sectional study was conducted on 1500 individuals living in Tehran between April 1, 2016 and the end of February, 2017. The participants were selected using random cluster sampling among those visiting a nutrition counseling center in Tehran. The exclusion criteria included alcohol consumption >40 g/day for males, >20 g/day for females, and lack of informed consent. The Ethics Committee of Fasa University of Medical Sciences approved the research protocol with No. 96061. The purpose of the study was explained to the participants and they completed written consent forms before entering the study.
Demographic information including gender, age and menopausal status were obtained. The participants’ heights and weights were measured and recorded by a trained individual. The heights were measured using a stadiometer with a 1.0 cm precision while the weights were determined using a digital scale with a 1.0 kg precision (Seca 767, Japan). The body mass index (BMI) was calculated by dividing weight in kilograms by the square of height in meters.
Blood pressure was measured twice in a sitting position from the right arm after 15 min of rest and the mean of the two figures was considered as the final blood pressure.
The common dietary intake of the participants was obtained using a semi-quantitative food frequency questionnaire (FFQ) over the past year. The questionnaire included a list of 168 food items with a standard amount of each item specified. The validity and reliability of this questionnaire have been previously investigated49. The participants expressed the frequency with which they consumed each item with respect to the standard amount in the past year. The values specified for each item were converted to grams per day using the manual for household measures. A comparison of the risk factors in individuals with/without fatty livers was done using the Chi-square test and was demonstrated by the odds ratio and a 95% confidence interval. Two main components of the diet were extracted using principal component analysis (PCA) and varymax rotations.
This method is determined by weight for each of the categories of food in the specified component, which indicates the presence of that food in the target component, and by this, the foods that make up the particular component (factor) is understood and based on the presence of these foods, the component can be named.
The components were labeled “healthy food pattern” and “unhealthy food pattern” in terms of nutrients. Food patterns were categorized into four quartiles, compared using logistic regression in those affected and unaffected, and demonstrated by the odds ratio and a 95% confidence interval. The analysis was performed once using raw data and again after age and gender optimization. The relationship between the two main components of food pattern and risk factors was shown using correlation and regression coefficients.
Variables might play a role, and associated risk factors as the mediator of the role of diet were examined. The mediator is an intermediate variable responsible for the relationship between two other variables.
The following should be considered when examining a mediator:
-
A.
Is the independent variable relates to the mediator? Route a
-
B.
Is the mediator relates to the dependent variable? Route b
-
C.
Is the independent variable relates to the dependent variable? Route c
-
D.
Does the simultaneous examination of the relationship between the independent variable and mediator with the dependent variable reveal the extent to which the relationship between the independent and the dependent variable decreases? Route c’
If Route c’ is adequately smaller than Route c, the mediator has been found.
It is necessary for the mediator to have a biological justification as well. Due to the dichotomous state of the dependent variable, the correction proposed by Nathaniel R50 based on the Sobel test51 was used to find the mediators. The strongest mediator was determined based on the greater value of the Sobel statistic and was optimized in terms of age and gender.
The i-ntravenous blood sample was taken in a 12-h fasting state to measure the condition of serum lipids. Blood samples were transferred to a laboratory for biochemical testing. Blood sugar (FBS), high-density lipoprotein (HDL), triacylglycerol (TG), total cholesterol (TC) and liver enzymes (ALT, AST and GGT) were measured by an enzymatic method using Pars Azmoon Commercial kits. The Friedewald formula was used to calculate low-density lipoprotein (LDL)52. The serum lipid values were reported based on mg/dl.
The homeostatic model (HOMA) is a method used to determine and quantify insulin resistance and beta cell function (equations 1 and 2). IR is used for insulin resistance and %β for the β-cell function.
| 1 |
| 2 |
Liver stiffness was measured by the NAFLD Score formula (equation 3) which was used to determine the extent of liver fat13 and confirmed by an experienced specialist using a fibroscan device.
| 3 |
Another powerful indicator of fatty liver diagnosis is the fatty liver index (FLI) which is calculated using the equation 414.
| 4 |
The data were analyzed in SPSS ver. 23. The descriptive data for the main variables were reported as mean ± standard deviation. The independent t-test was used to compare the variables between the two groups. Linear regression test was used to determine the linear relationship of the variables used in the study. P < 0.05 was considered as the significance level.
Implication for health policy makers/practice/research/medical education
Determining the relationship between dietary pattern and other risk factors with NAFLD can help policy makers or other researchers for designing preventive programs for Fatty liver that accounts for 1.3–2.6 deaths per 100,000 per year. The results of present study shows dietary pattern is significant determinant of NAFLD but waist circumference is an mediator of its effect on NAFLD that must be under more control.
Electronic supplementary material
Author Contributions
Conceptualization: R.H., E.E. Methodology: R.H., Software: M.M.N., A.D. Validation: R.H. M.M.N. Formal analysis: M.M.N., A.D. Investigation: N.H., A.G., R.H. Resources: SO, RH Data curation: MMN, RH Writing (original draft preparation): N.H., R.H. Writing (review and editing): A.G., R.H. Visualization: R.H., B.H. Supervision: R.H. Project administration: R.H. Funding acquisition: R.H.
Competing Interests
The authors declare no competing interests.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-23192-x.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McCullough AJ. The clinical features, diagnosis and natural history of nonalcoholic fatty liver disease. Clinics in liver disease. 2004;8:521–533. doi: 10.1016/j.cld.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 2.Zivkovic AM, German JB, Sanyal AJ. Comparative review of diets for the metabolic syndrome: implications for nonalcoholic fatty liver disease. The American journal of clinical nutrition. 2007;86:285–300. doi: 10.1093/ajcn/86.2.285. [DOI] [PubMed] [Google Scholar]
- 3.Chalasani N, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592–1609. doi: 10.1053/j.gastro.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Zand H, et al. Obesity-induced p53 activation in insulin-dependent and independent tissues is inhibited by beta-adrenergic agonist in diet-induced obese rats. Life sciences. 2016;147:103–109. doi: 10.1016/j.lfs.2016.01.040. [DOI] [PubMed] [Google Scholar]
- 5.Ratziu, V., Bellentani, S., Cortez-Pinto, H., Day, C. & Marchesini, G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. Journal of hepatology53, 372–384 (2010). [DOI] [PubMed]
- 6.Younossi, Z. M. et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clinical Gastroenterology and Hepatology9, 524-530. e521 (2011). [DOI] [PubMed]
- 7.Moghaddasifar I, et al. Prevalence of non-alcoholic fatty liver disease and its related factors in Iran. International journal of organ transplantation medicine. 2016;7:149. [PMC free article] [PubMed] [Google Scholar]
- 8.Lankarani, K. B. et al. Non alcoholic fatty liver disease in southern Iran: a population based study. Hepatitis monthly13 (2013). [DOI] [PMC free article] [PubMed]
- 9.Alavian, S. M., Esmaillzadeh, A., Adibi, P. & Azadbakht, L. Dietary quality indices and biochemical parameters among patients with non alcoholic fatty liver disease (NAFLD). Hepatitis monthly13 (2013). [DOI] [PMC free article] [PubMed]
- 10.Kontogianni MD, et al. Adherence to the Mediterranean diet is associated with the severity of non-alcoholic fatty liver disease. Clinical Nutrition. 2014;33:678–683. doi: 10.1016/j.clnu.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 11.Abenavoli L, et al. Alimentary regimen in non-alcoholic fatty liver disease: Mediterranean diet. World Journal of Gastroenterology: WJG. 2014;20:16831. doi: 10.3748/wjg.v20.i45.16831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Current opinion in lipidology. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Angulo P, et al. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007;45:846–854. doi: 10.1002/hep.21496. [DOI] [PubMed] [Google Scholar]
- 14.Bedogni G, et al. The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC gastroenterology. 2006;6:33. doi: 10.1186/1471-230X-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Esmaillzadeh A, Azadbakht L. Major dietary patterns in relation to general obesity and central adiposity among Iranian women. The Journal of nutrition. 2008;138:358–363. doi: 10.1093/jn/138.2.358. [DOI] [PubMed] [Google Scholar]
- 16.Rezazadeh A, Rashidkhani B, Omidvar N. Association of major dietary patterns with socioeconomic and lifestyle factors of adult women living in Tehran, Iran. Nutrition. 2010;26:337–341. doi: 10.1016/j.nut.2009.06.019. [DOI] [PubMed] [Google Scholar]
- 17.Panagiotakos DB, Pitsavos C, Skoumas Y, Stefanadis C. The association between food patterns and the metabolic syndrome using principal components analysis: The ATTICA Study. Journal of the American Dietetic Association. 2007;107:979–987. doi: 10.1016/j.jada.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 18.Yang C-Q, et al. Dietary patterns modulate the risk of non-alcoholic fatty liver disease in Chinese adults. Nutrients. 2015;7:4778–4791. doi: 10.3390/nu7064778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oddy WH, et al. The Western dietary pattern is prospectively associated with nonalcoholic fatty liver disease in adolescence. The American journal of gastroenterology. 2013;108:778. doi: 10.1038/ajg.2013.95. [DOI] [PubMed] [Google Scholar]
- 20.Jia Q, et al. Dietary patterns are associated with prevalence of fatty liver disease in adults. European journal of clinical nutrition. 2015;69:914. doi: 10.1038/ejcn.2014.297. [DOI] [PubMed] [Google Scholar]
- 21.Sofi F, Casini A. Mediterranean diet and non-alcoholic fatty liver disease: New therapeutic option around the corner? World journal of gastroenterology: WJG. 2014;20:7339. doi: 10.3748/wjg.v20.i23.7339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Trovato FM, Catalano D, Martines GF, Pace P, Trovato GM. Mediterranean diet and non-alcoholic fatty liver disease: the need of extended and comprehensive interventions. Clinical Nutrition. 2015;34:86–88. doi: 10.1016/j.clnu.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 23.Baratta F, et al. Adherence to Mediterranean Diet and Non-Alcoholic Fatty Liver Disease: Effect on Insulin Resistance. The American Journal Of Gastroenterology. 2017;112:1832. doi: 10.1038/ajg.2017.371. [DOI] [PubMed] [Google Scholar]
- 24.Garcia M, et al. The effect of the traditional Mediterranean-style diet on metabolic risk factors: A meta-analysis. Nutrients. 2016;8:168. doi: 10.3390/nu8030168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zamora-Ros R, et al. Mediterranean diet and non enzymatic antioxidant capacity in the PREDIMED study: evidence for a mechanism of antioxidant tuning. Nutrition, Metabolism and Cardiovascular Diseases. 2013;23:1167–1174. doi: 10.1016/j.numecd.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 26.Eckel RH, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014;63:2960–2984. doi: 10.1016/j.jacc.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 27.Williams DE, et al. A cross-sectional study of dietary patterns with glucose intolerance and other features of the metabolic syndrome. British Journal of Nutrition. 2000;83:257–266. doi: 10.1017/S0007114500000337. [DOI] [PubMed] [Google Scholar]
- 28.Alonso A, et al. Fruit and vegetable consumption is inversely associated with blood pressure in a Mediterranean population with a high vegetable-fat intake: the Seguimiento Universidad de Navarra (SUN) Study. British Journal of Nutrition. 2004;92:311–319. doi: 10.1079/BJN20041196. [DOI] [PubMed] [Google Scholar]
- 29.Rolls BJ, Ello-Martin JA, Tohill BC. What can intervention studies tell us about the relationship between fruit and vegetable consumption and weight management? Nutrition reviews. 2004;62:1–17. doi: 10.1111/j.1753-4887.2004.tb00001.x. [DOI] [PubMed] [Google Scholar]
- 30.Ehrampoush E, et al. Ability of dairy fat in inducing metabolic syndrome in rats. SpringerPlus. 2016;5:2020. doi: 10.1186/s40064-016-3716-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seo H-S, Lee S-K, Nam S. Factors influencing fast food consumption behaviors of middle-school students in Seoul: an application of theory of planned behaviors. Nutrition research and practice. 2011;5:169–178. doi: 10.4162/nrp.2011.5.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bakhtiyari M, et al. Anxiety as a consequence of modern dietary pattern in adults in Tehran—Iran. Eating behaviors. 2013;14:107–112. doi: 10.1016/j.eatbeh.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 33.Charlton M, et al. Fast food diet mouse: novel small animal model of NASH with ballooning, progressive fibrosis, and high physiological fidelity to the human condition. American Journal of Physiology-Gastrointestinal and Liver Physiology. 2011;301:G825–G834. doi: 10.1152/ajpgi.00145.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Babai MA, et al. Defining a BMI cut-off point for the Iranian population: the Shiraz Heart Study. PloS one. 2016;11:e0160639. doi: 10.1371/journal.pone.0160639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ehrampoush, E. et al. New anthropometric indices or old ones: Which is the better predictor of body fat? Diabetes & Metabolic Syndrome: Clinical Research & Reviews 11, 257–263 (2017). [DOI] [PubMed]
- 36.McCarthy EM, Rinella ME. The role of diet and nutrient composition in nonalcoholic fatty liver disease. Journal of the Academy of Nutrition and Dietetics. 2012;112:401–409. doi: 10.1016/j.jada.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 37.Fung TT, et al. Sweetened beverage consumption and risk of coronary heart disease in women. The American journal of clinical nutrition. 2009;89:1037–1042. doi: 10.3945/ajcn.2008.27140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Malik VS, et al. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes. Diabetes care. 2010;33:2477–2483. doi: 10.2337/dc10-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. American journal of public health. 2007;97:667–675. doi: 10.2105/AJPH.2005.083782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simopoulos AP. Dietary omega-3 fatty acid deficiency and high fructose intake in the development of metabolic syndrome, brain metabolic abnormalities, and non-alcoholic fatty liver disease. Nutrients. 2013;5:2901–2923. doi: 10.3390/nu5082901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Levy JR, Clore JN, Stevens W. Dietary n‐3 polyunsaturated fatty acids decrease hepatic triglycerides in Fischer 344 rats. Hepatology. 2004;39:608–616. doi: 10.1002/hep.20093. [DOI] [PubMed] [Google Scholar]
- 42.Sekiya M, et al. Polyunsaturated fatty acids ameliorate hepatic steatosis in obese mice by SREBP‐1 suppression. Hepatology. 2003;38:1529–1539. doi: 10.1016/j.hep.2003.09.028. [DOI] [PubMed] [Google Scholar]
- 43.Lei S, et al. The prevalence of nonalcoholic fatty liver disease and its association with lifestyle/dietary habits among university faculty and staff in Chengdu. Biomedical and environmental sciences. 2012;25:383–391. doi: 10.3967/0895-3988.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 44.Laguna JC, Alegret M, Roglans N. Simple sugar intake and hepatocellular carcinoma: epidemiological and mechanistic insight. Nutrients. 2014;6:5933–5954. doi: 10.3390/nu6125933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Spruss A, Bergheim I. Dietary fructose and intestinal barrier: potential risk factor in the pathogenesis of nonalcoholic fatty liver disease. The Journal of nutritional biochemistry. 2009;20:657–662. doi: 10.1016/j.jnutbio.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 46.Pang Q, et al. Central obesity and nonalcoholic fatty liver disease risk after adjusting for body mass index. World Journal of Gastroenterology: WJG. 2015;21:1650. doi: 10.3748/wjg.v21.i5.1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lonardo A, Caldwell SH, Loria P. Clinical physiology of NAFLD: a critical overview of pathogenesis and treatment. Expert Review of Endocrinology & Metabolism. 2010;5:403–423. doi: 10.1586/eem.10.5. [DOI] [Google Scholar]
- 48.Marchesini G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37:917–923. doi: 10.1053/jhep.2003.50161. [DOI] [PubMed] [Google Scholar]
- 49.Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran Lipid and Glucose Study. Public health nutrition. 2010;13:654–662. doi: 10.1017/S1368980009991698. [DOI] [PubMed] [Google Scholar]
- 50.Kenny, D. A. & Herr, N. R. Mediation with Dichotomous Outcomes, http://www.nrhpsych.com/mediation/logmed.html (1993).
- 51.Magni P, et al. Free and bound plasma leptin in normal weight and obese men and women: relationship with body composition, resting energy expenditure, insulin‐sensitivity, lipid profile and macronutrient preference. Clinical endocrinology. 2005;62:189–196. doi: 10.1111/j.1365-2265.2005.02195.x. [DOI] [PubMed] [Google Scholar]
- 52.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical chemistry. 1972;18:499–502. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.