Abstract
Bone cement spacers loaded with antibiotic are the gold standard in septic revision. However, the management of massive bone defects constitutes a surgical challenge, requiring the use of different nails, expensive long stems, or cement-coated tumor prostheses for preparing the spacer. In most cases, the knee joint must be sacrificed. We describe a novel technique for preparing a biarticular total femur spacer with the help of a trochanteric nail coated with antibiotic loaded cement, allowing mobility of the hip and knee joints and assisted partial loading until second step surgery. This technique is helpful to maintain the length of the leg, prevent soft tissue contracture, and help eradicate the infection preserving the patient comfort and autonomy while waiting to receive total femoral replacement.
Keywords: Periprosthetic joint infection, Femoral spacer, Massive bone loss, Two stages revision, Biarticular spacer
Introduction
Prosthetic joint infection is a potentially devastating complication, although the different available surgical options (revision in 1 or 2 steps) have allowed healing rates of close to 90% [1]. However, the dramatic increase in the use of revision stems; the presence of multiresistant microorganisms; and the increase in patients with implants in contiguous joints constitute a genuine cause for concern among orthopaedic surgeons.
Two-step revision surgery is the standard treatment for prosthetic joint infection associated to important bone loss. Such bone loss due to infection, osteolysis, stress shielding, or fractures constitutes a genuine surgical challenge [2]. During the first step, it is essential to remove all the implants and devitalized tissues, and to perform extensive surgical debridement as in tumor cases. Posteriorly, the placement of a spacer with cement mixed with different antibiotics is common practice to maintain the joint space and correct soft tissue tension. Articulating spacers are currently preferred to offer the patient moderate function, walking with support, and a range of mobility allowing increased comfort in the interval between the first and second step, as well as to ensure better soft tissue management in the second step. However, implantation of these spacers is often difficult and depends on the amount of remaining bone.
Although there are number of alternatives for preparing these articulating spacers, eg, manually, using silicon/metal molds, commercial spacers, or directly implanting a cemented prosthesis on a temporary basis, very little information is available on the use of such spacers in massive bone defects or defects affecting the entire femur [3]. To our knowledge, there are only 2 reports in the literature on the preparation of femur spacers using a cemented intramedullary nail with a hip stem [3] or PROSTALAC type spacer [4]. In both publications, the knee joint was “sacrificed,” affixing the distal zone of the nail in the proximal tibia.
We present a new surgical technique to create a massive hand-made biarticulating spacer. After complete removal of the femur due to a septic nonunion of a supracondylar fracture and a proximal septic total hip arthroplasty in the same femur, a massive hand-made biarticulating spacer was built to preserve function and mobility of the hip and knee.
Surgical technique
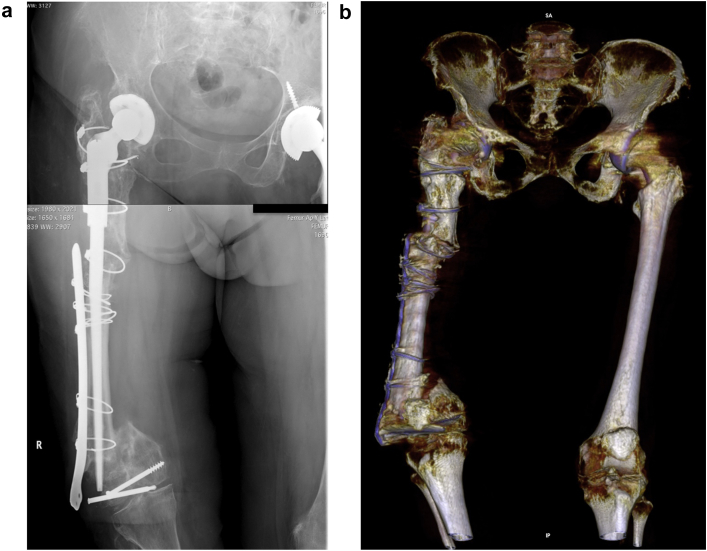
Under general anesthesia, the patient is placed in lateral decubitus allowing access to the hip and knee. At proximal level, a posterolateral access is chosen, because this is the approach commonly used by the authors in primary and revision surgery—extending it at distal level over the lateral thigh to the anterolateral zone of the knee, after removal of the previous scar tissue, and adopting a deep approach at distal level between the vastus lateralis muscle and the intermuscular septum. Special care is taken to leave enough proximal space for possible expansion of the approach at proximal level, and to leave the inguinal zone free at the location of the neurovascular bundle, in case any vascular complications are to occur during surgery (Fig. 1).
Figure 1.
(a) Radiograph view showing right distal femoral pseudoarthrosis. (b) Three-dimensional computed tomography reconstruction.
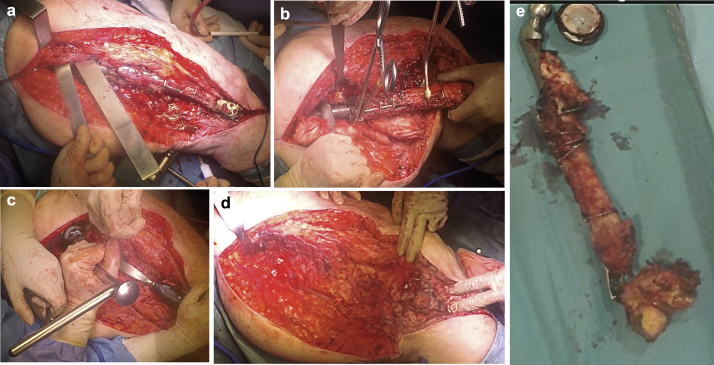
Proximally, and after dividing the fascia lata, en bloc dissection is carried out of the remnant short rotator cuffs, together with an L-shaped capsulotomy curved posteriorly at the limit of the greater trochanter—mobilizing the tissues posteriorly and palpating and protecting the sciatic nerve, without dissecting the latter. After confirming the good macroscopic appearance, a sliding trochanteric osteotomy is performed (Fig. 2a), leaving most of the insertion of the gluteus medius and vastus lateralis muscles for later reanchoring. In the thigh, the vastus lateralis is reflected anteriorly using blunt Hohmann type retractors for leverage. It is important to ensure careful hemostasis of the perforating vessels crossing at this level between the vastus lateralis and the biceps femoris muscle. At distal level, an anterolateral access to the knee is used, first resecting the menisci and external collateral ligaments, thereby allowing rotation of the joint and resection of the remaining meniscal tissue, cruciate and medial collateral ligaments, and the rest of muscle insertions. The prosthesis and distal femur are removed in block (Fig. 2b). Six samples are collected for microbiological study, in accordance with the usual protocol. In this case, because of the history of infection in the proximal zone, sampling was performed in the proximal and distal femur, sending the extracted implant for sonication. Special care is required during dissection of the posterior femoral surface at knee level and medial in the femoral diaphysis, to avoid neurovascular damage. An Explant extractor (Zimmer, Warsaw, IN) is used to remove the acetabular component, preserving as much acetabular bone as possible (Fig. 2c).
Figure 2.
Intraoperative views during femoral extraction. (a) Trochanteric osteotomy; (b) femoral extraction; (c) acetabular extraction; (d) massive defect after femoral extraction; and (e) resected femur.
After explantation of both components and the rest of the femur, radical debridement of all the devitalized tissues is carried out until a healthy bleeding bed is obtained for positioning of the spacer (Fig. 2d).
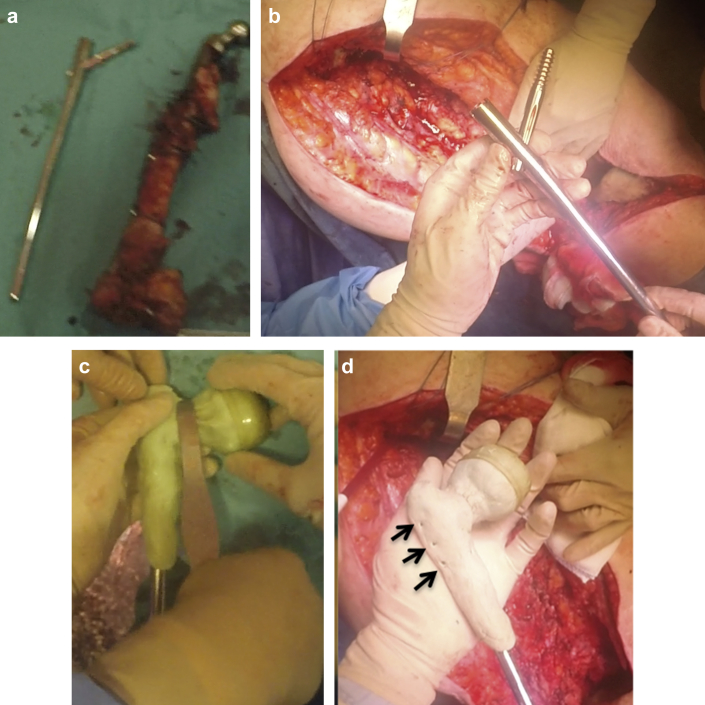
Before surgery, a calibrated radiograph of both extremities was obtained to determine the required spacer length. In this specific case, the spacer was prepared using a long 280 mm nail (Gamma nail, Stryker, Mahwah, NJ), leaving at least 6 cm of length for posterior preparation of the distal joint (Fig. 3a). The nail is initially presented with the screw, and the latter is blocked on the nail with the selected offset (Fig. 3b). The future femoral head is then created using the mold of a washing syringe, which is inverted to use the smooth part on the cephalic screw. Then, after confirming adequate acetabular congruency, the nail is coated with cement, taking special care not to generate too much material on the trochanteric zone to avoid complicating subsequent closure (Fig. 3c). Although the cement polymerized, small perforations are made in the cement layer at trochanteric level for posterior re-anchoring of the abductor and psoas muscles (Fig. 3d). After setting, the nail is completely covered with cement, leaving its distal orifice free and taking special care not to block the internal canal of the nail (Fig. 3e and f). Lastly, two bent Rush pins are used as support for the distal joint, creating a ball and socket type joint and using as mold another washing syringe similar to that previously used. At this point, it is important to ensure that there is a degree of “anteversion” between the femoral neck of the spacer and the curved shape of the distal joint, to minimize possible luxation of either joint (Fig. 3g). Before spacer implantation, the tibial metaphysis is reamed a few millimeters with acetabular reamers to house the spherical femoral head of the spacer (Fig. 4a). After reaming, the spacer is inserted, reducing it within the acetabulum and reanchoring the proximal muscles (gluteus and psoas) in the holes prepared for this purpose (Fig. 4b). Then, after abundant washing and the placement of 2 drains, closure is carried out, taking special care in closing of the distal arthrotomy to contain the new joint (Fig. 4c). Four packs of cement were used for preparing this spacer: 2 for the body and 1 for each joint. The cement used was Copal G+C (Heraeus Medical GmbH, Wehrheim, Germany), with the manual addition of antibiotic depending on the culture result 3 g vancomycin to each pack in this case).
Figure 3.
Biarticular femur spacer preparation process. (a) Nail measurement; (b) measurement of cephalic nail offset; (c and d) preparation of the proximal part: note the perforations made (arrows) for anchoring the abductor muscles; (e and f) nail coating; and (g) preparation of the distal ball and socket joint with washing. Note the reanchoring of the abductor muscles (arrows).
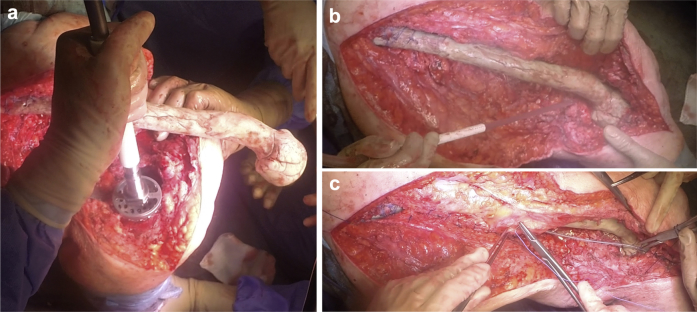
Figure 4.
(a) Final preparation of the tibial bed using acetabular drills; (b) definitive reduction; and (c) closing and covering of the spacer with vastus lateralis muscle.
After 24 hours, a postoperative radiograph controls are obtained. If they show that the spacer is in correctly position, immediate patient sitting is allowed, with flexion-extension exercises of the knee and assisted partial loading (Fig. 5). No hip abduction orthosis is placed; an articulated orthosis is used at knee level just for partial loading to control knee instability after soft tissues resection.
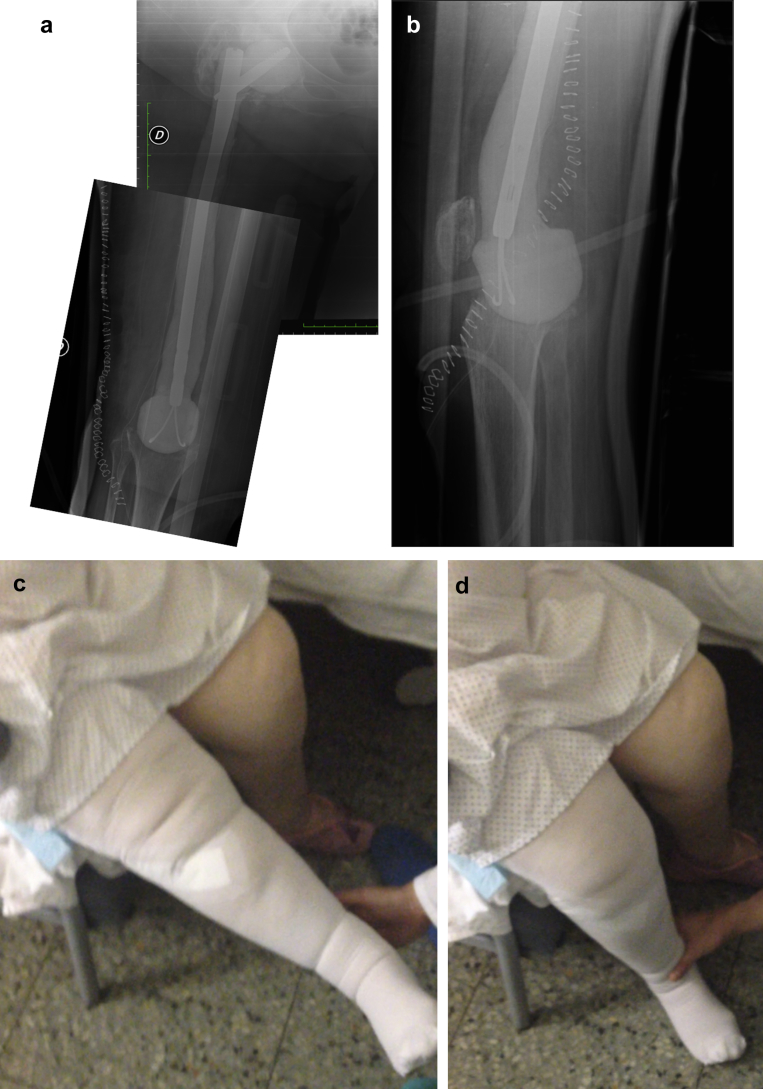
Figure 5.
Postoperative evaluation 48 hours after surgery. Radiograph control in (a) anteroposterior projection; (b) Lateral projection; and (c and d) Passive joint range.
Discussion
Infection after joint arthroplasty remains a genuine challenge for patients and surgeons alike. At present, 2-step revision surgery is regarded as the standard management in infections after total hip and total knee arthroplasties [5], although a growing number of authors are questioning this treatment and recommend 1-step revision, because of the potential economical savings and benefits for the patient [6]. However, to our knowledge, no studies have defended single-step replacement in massive defects that would require tumor implants for reconstruction.
Many studies have demonstrated the importance of using spacers with antibiotic-loaded cement to eradicate infection, facilitate subsequent reimplantation of the definitive implant, and improve patient mobility [7]. Despite these advantages, however, there are number of complications inherent to the use of spacers, such as luxation and fractures.
A favorable head/neck ratio is one of the important factors, together with adequate anchoring within the canal [8], to prevent these complications. By using a cephalomedullary nail as in our spacer, we can prepare cement heads as large as needed by the acetabular cavity, with a large difference between the diameter of the head and neck. This allows the avoidance of impingement and luxation, because another parameter that may be responsible for spacer luxation is a reduction of femoral offset—this being particularly important in cases characterized by massive bone defects. Another important advantage of this implant in preparing the spacer is that by modifying the position of the cephalic screw we can choose the offset needed to secure adequate tension of the periarticular soft tissues. Anagnostakos et al. [7] reported good results with manual hip spacers using a DHS type plate to restore the necessary offset. However, this technique cannot be used in proximal massive bone defects.
Fracturing is another important complication associated to the use of cement spacers. Biring et al. [9] recorded a spacer fracture rate of 2%, associated to a bone fracture rate of 10%. None of these cases involved massive defects, however. In our opinion, the use of a cephalomedullary nail for the spacer affords sufficient stability to avoid this kind of complication (Table 1). Moreover, the fact that we do not need to mold the implant, as in an isolated cement spacer or a spacer with a thinner nail such as an Ender or Rush pin, implies that no new points of fatigue appear in the material.
Table 1.
Advantages of biarticular total femur spacer for massive femoral bone loss.
| Advantages |
|---|
|
The use of articulating spacers for massive femoral bone defects has been described before [3] (Table 2). However, the use of Rush or Kirschner pins is associated to a high pin fracture rate. Richard et al. [3] and Sherman et al. [10] have described different spacer preparation techniques using a cement-loaded Kuntscher nail with an Exeter stem or a long antibiotic loaded bone cement-coated stem for proximal massive bone defects, with good results, although these defects did not include the distal part of the femur where the 2 spacers were affixed. Other authors have described prosthesis-spacer systems, coating the temporary prosthesis with large amounts of antibiotic-loaded cement, in application to certain femoral defects [12].
Table 2.
Different surgical techniques described for massive femoral spacer.
| Author | Material used | Hip articulation | Knee articulation | Disadvantage |
|---|---|---|---|---|
| Richards et al. [9] | Kuntscher nail with an Exeter stem | Cemented Exeter hip arthroplasty (polyethylene liner + stem). No proximal implant coating | Fixed with Kuntscher nail |
|
| Sherman et al. [10] | Unipolar trial long stem femoral component | Unipolar polar head coated with antibiotic PMMA | NO. Cemented implant in a minimal distal femoral bone |
|
| Cassar Gheiti et al. [11] | Femoral intramedullary nail with a CPCS stem | Unipolar head. No proximal implant coating | Fixed with femoral intramedullary nail |
|
| Kamath et al. [4] | Femoral intramedullary nail with PROSTALAC spacer | PROSTALAC spacer. Partial proximal implant coating | Fixed with femoral intramedullary nail modified |
|
| Current paper | Trochanteric long nail with 2 Rush pins | Handmade hemiarthroplasty (over cephalic screw). All implant is coated with antibiotic PMMA | Handmade ball and socket articulation (over Rush pins) |
|
PMMA, poly methyl methacrylate.
The absence of distal bone for affixing the spacer and knee joint implies a great difference between a massive and total bone defect. To our knowledge, only Kamath et al. [4] and Cassar Gheiti et al. [11] have previously described the use of a manual spacer for total femoral defects. Although the authors used different components for preparing an articulating spacer at proximal level (PROSTALAC vs a poly methyl methacrylate-coated stem), both of them inserted a femoral nail at distal level into the tibial endomedullary canal and secured fixation at this level with a lock or simply by applying pressure—sacrificing mobility of the knee joint. Although the patients operated on with these techniques were allowed to walk with partial loading using a walker, we consider that the risk of peri-implant fracture is high, because of the great leverage to which the proximal tibia is subjected. In addition, in many cases, the patients that undergo such surgery must be managed in a wheelchair, and the stabilization of the knee in extension makes this difficult. The use of a biarticular total femur spacer allows us to maintain a knee joint range of 0°-90°, with lesser retraction of the periarticular structures at knee level, favoring the recovery of mobility after implantation of the definitive component in the second step, and reducing muscle loss (mainly referred to the quadriceps muscle). No less important is the fact that a biarticular spacer allows these patients to maintain a normal sitting position during the period in which they carry the spacer, allowing flexion-extension exercises of the knee and partial loading with the help of an articulating knee pad. This undoubtedly results in improved patient quality of life.
Summary
Total femoral bone loss after periprosthetic infection currently does not justify disarticulation of the hip. The temporary use of a total femur spacer allows us to maintain the length of the leg, prevent soft tissue contracture, and help eradicate the infection. The technique we have described offers a possible solution to number of complications observed with the use of spacers in massive defects, affording greater patient comfort and autonomy while waiting to receive total femoral replacement.
Footnotes
No author associated with this paper has disclosed any potential or pertinent conflicts which may be perceived to have impending conflict with this work. For full disclosure statements refer to http://dx.doi.org/10.1016/j.artd.2017.02.007.
Appendix A. Supplementary data
References
- 1.Jacobs C., Christensen C.P., Berend M.E. Static and mobile antibiotic-impregnated cement spacers for the management of prosthetic joint infection. J Am Acad Orthop Surg. 2009;17(6):356. doi: 10.5435/00124635-200906000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Takahira N., Itoman M., Higashi K. Treatment outcome of two-stage revision total hip arthroplasty for infected hip arthroplasty using antibiotic-impregnated cement spacer. J Orthop Sci. 2003;8(1):26. doi: 10.1007/s007760300004. [DOI] [PubMed] [Google Scholar]
- 3.Richards C., Bell C.J., Viswanathan S., English H., Crawford R.W. Use of a cement-loaded Kuntscher nail in first-stage revision hip arthroplasty for massive femoral bone loss secondary to infection: a report of four cases. J Orthop Surg (Hong Kong) 2010;18(1):107. doi: 10.1177/230949901001800124. [DOI] [PubMed] [Google Scholar]
- 4.Kamath A.F., Austin D., Lee G.C. Mating of a PROSTALAC spacer with an intramedullary nail for reconstruction of an infected interprosthetic femoral shaft fracture: a case report. J Orthop Surg (Hong Kong) 2012;20(2):263. doi: 10.1177/230949901202000228. [DOI] [PubMed] [Google Scholar]
- 5.Garvin K.L., Backstein D., Pellegrini V.D., Jr., Kim R.H., Lewallen D.G. Dealing with complications. J Bone Joint Surg Am. 2009;91(Suppl 5):18. doi: 10.2106/JBJS.I.00347. [DOI] [PubMed] [Google Scholar]
- 6.Winkler H., Stoiber A., Kaudela K., Winter F., Menschik F. One stage uncemented revision of infected total hip replacement using cancellous allograft bone impregnated with antibiotics. J Bone Joint Surg Br. 2008;90(12):1580. doi: 10.1302/0301-620X.90B12.20742. [DOI] [PubMed] [Google Scholar]
- 7.Anagnostakos K., Jung J., Schmid N.V., Schmitt E., Kelm J. Mechanical complications and reconstruction strategies at the site of hip spacer implantation. Int J Med Sci. 2009;6(5):274. doi: 10.7150/ijms.6.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leunig M., Chosa E., Speck M., Ganz R. A cement spacer for two-stage revision of infected implants of the hip joint. Int Orthop. 1998;22(4):209. doi: 10.1007/s002640050244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Biring G.S., Kostamo T., Garbuz D.S., Masri B.A., Duncan C.P. Two-stage revision arthroplasty of the hip for infection using an interim articulated Prostalac hip spacer: a 10- to 15-year follow-up study. J Bone Joint Surg Br. 2009;91(11):1431. doi: 10.1302/0301-620X.91B11.22026. [DOI] [PubMed] [Google Scholar]
- 10.Sherman S.L., Cunneen K.P., Walcott-Sapp S., Brause B., Westrich G.H. Custom total femur spacer and second-stage total femur arthroplasty as a novel approach to infection and periprosthetic fracture. J Arthroplasty. 2008;23(5):781. doi: 10.1016/j.arth.2007.05.027. [DOI] [PubMed] [Google Scholar]
- 11.Cassar Gheiti A.J., Baker J.F., Brown T.E., Mulhall K.J. Management of total femoral bone loss using a hybrid cement spacer surgical technique. J Arthroplasty. 2013;28(2):347. doi: 10.1016/j.arth.2012.04.033. [DOI] [PubMed] [Google Scholar]
- 12.Macmull S., Bartlett W., Miles J. Custom-made hinged spacers in revision knee surgery for patients with infection, bone loss and instability. Knee. 2010;17(6):403. doi: 10.1016/j.knee.2009.11.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.