Abstract
We investigated how often HIV-positive MSM (n=177) decide to engage in unprotected anal intercourse (UAI) because they have an undetectable viral load (UVL). We found that 20–57% of the UAI acts were related to having UVL, varying by partner type and partner HIV status. Among HIV-concordant partners, consideration of UVL before engaging in UAI was more prevalent with sex buddies (55%) than with casual partners (20%), although marginally significant (p=0.051). Among HIV-discordant partners, no significant difference was found in the frequency of UVL considerations before engaging in UAI: 40% with sex buddies versus 57% with casual partners. Interestingly, while the decision to engage in UAI based on UVL was frequently discussed with HIV-concordant partners (>91%), it was only discussed with HIV-discordant partners in 13–25% of the UAI cases (according to partner type), suggesting that the decision was mostly unilateral.
Keywords: undetectable viral load, men who have sex with men, sexual behavior, unprotected anal intercourse
INTRODUCTION
Studies conducted since the introduction of combination antiretroviral therapy (cART) indicate that some men who have sex with men (MSM) perceive that having an undetectable HIV load reduces the risk of HIV transmission [1–3]. Other studies reported that MSM were more likely to engage in unprotected anal intercourse (UAI) with their HIV-positive regular partner when they believed he had an undetectable rather than a detectable viral load [4, 5].
In 2008, the Swiss National AIDS Commission was the first to take a clear stance on the relationship between viral load and infectiousness and declared that sexual transmission of HIV is very unlikely within a monogamous HIV-discordant relationship under the following conditions: the HIV-positive individual has an undetectable viral load (i.e., HIV RNA <40 copies/ml), receives effective cART, tests regularly for viral load, and has no other sexually transmitted disease [6]. This statement was primarily based on data regarding vaginal sex among heterosexual steady couples. While the implications of the Swiss statement for MSM could be significant, relatively little is still known of the extent to which HIV-positive MSM base their decision to engage in UAI on the knowledge that their viral load is undetectable.
The purpose of this study was to investigate how often the decision to engage in UAI with casual partners is based on knowledge of undetectable viral load (UVL) among HIV-positive MSM in the Netherlands. We distinguished between HIV-positive and HIV-negative sex partners because we assume that the consideration of UVL could have different underlying motivations related to the partner’s HIV-status. With HIV-positive partners, consideration of UVL could be, for example, related to the perception of men that the risk for becoming super-infected with an additional (resistant) HIV strain is lower [7, 8]. With HIV-negative partners, having an UVL when engaging in UAI could be perceived as a condition in which the risk of transmitting the virus to the negative partner is negligible. Furthermore, we chose to investigate two different sex partner types (i.e., casual partner versus sex buddy) as they have been shown to be associated with different risk behavior patterns in the past [9]: MSM were more likely to engage in serosorting (i.e., having unprotected sex only with HIV concordant partners) with sex buddies than with casual sex partners. This was understood as a consequence of increased familiarity with the sex partner, which could facilitate serosorting negotiations. We wanted to examine whether a similar pattern will exist in our study: men will engage in UAI more often with sex buddies than casual partners when having UVL, presumably because of the facilitating effect of familiarity with the sex partner on discussing such a matter. Therefore, among those who engaged in UAI based on the consideration of UVL, we additionally examined how often this decision was discussed in advance by both sex partners. Finally, we studied the association between perceived protective value of UVL against transmission of HIV and the decision to engage in UAI based on viral load knowledge.
METHODS
Procedure and study sample
In early 2010, all members of an open online panel of the Netherlands HIV Association were invited by e-mail to participate in a cross-sectional study by filling out an online questionnaire. People can register for the panel via the Association’s website. Requirements for participation in the panel are: (1) being 16 years or older, (2) being HIV-positive or directly involved with someone who is HIV-positive, and (3) living in the Netherlands. The panel is contacted on a regular basis to ask for opinions on different topics relevant for people living with HIV and for participation in research, and consists of 517 HIV-positive men and women. Only HIV-positive men were invited to participate in this study.
In total, 212 HIV-positive men filled out our questionnaire and all reported having had sex with men. Of these men, self-reported viral load was undetectable in 177 (83%), detectable in 31 (15%), and unknown in 4 (2%) cases. As our primary interest was to study the consideration of UVL in the decision to engage in UAI, we included only those men with an UVL, resulting in a study sample of 177 HIV-positive MSM.
Measures
We measured general characteristics, sexual behavior, the consideration of UVL in the decision to engage in UAI and the discussion thereof with the partner, knowledge of the participant’s and partner’s viral load level, and risk perceptions.
Sample characteristics
We measured the participants’ age, nationality (Dutch versus non-Dutch), use of cART (yes/no), and level of education. Educational level was considered high with completion of higher vocational education or university, and middle to low with completion of secondary vocational education, high school, basic vocational education or primary school.
Type of sex partner
We distinguished two types of sex partners: casual (defined as “someone you have met by chance and had sex with”) and sex buddy (defined as “someone you regularly contact in order to have sex with”).
Unprotected anal intercourse (UAI)
We defined UAI as never or not always using condoms during insertive anal intercourse and/or receptive anal intercourse. If participants reported any incident of anal intercourse (insertive and/or receptive) in the preceding six months, they were asked about the frequency of condom use for those incidents (measured on a 5-point scale ranging from “never” to “always”). Participants who reported UAI were asked in more detail about the last time UAI occurred and the type of sex partner it occurred with.
HIV & viral load status of the partner
Participants were asked whether they knew the sex partner’s HIV status (positive/negative/unknown) before engaging in UAI. Regarding HIV-positive partners, participants were asked whether they knew the partner’s viral load level (undetectable/detectable/unknown) before they engaged in sex. Partners for whom status was reportedly negative or unknown will be henceforth referred to as “(potentially) HIV-negative”. The participants were also asked whether their partners knew the viral load status of the participant (yes/no).
Consideration of UVL in the decision to engage in UAI
We defined the consideration of UVL in deciding to engage in UAI as follows: (1) the decision made by the participant to have UAI with another HIV-positive man because that person’s viral load was undetectable, or (2) the decision made by the HIV-positive participant to have UAI with a (potentially) HIV-negative man because the HIV-positive participant’s viral load was undetectable. In case of UAI with an HIV-positive partner, we asked, “Did you decide to have anal intercourse without a condom with this [infected] partner because you knew that his viral load was undetectable?” (yes/no). In case of UAI with a (potentially) HIV-negative partner, we asked, “Did you decide to have anal intercourse without a condom with this [uninfected] partner because you knew that your own viral load was undetectable?” (yes/no). We measured the consideration of UVL, (1) ever since HIV diagnosis; and (2) during the last UAI contact (with either a casual partner or a sex buddy).
The discussion of the decision to engage in UAI based on an UVL
If participants reported they had considered their own or their partner’s UVL in the decision to engage in UAI, they were asked whether they had discussed this with their partner before the engagement in UAI (yes/no).
Perceived protective value of UVL
Participants evaluated the risk of HIV transmission in two different sexual scenarios in which two partners decide against condom use based on their viral load knowledge. The first scenario involved UAI between two HIV-positive partners who both had UVL levels, and the second one involved UAI between an HIV-positive man with UVL level and an HIV-negative partner. For each scenario, participants rated the perceived protective value of having UVL on a 7-point scale ranging from (1) “absolutely no risk” to (7) “absolute risk”. Responses were dichotomized as: “no to low risk” (values 1–2) and “moderate to absolute risk” (values 3–7).
Statistical analyses
We first described the characteristics of the study population: demographics, the perceived protective value of UVL, the proportions of UAI per sex partner type, and the proportion of men who ever considered their UVL in the decision to engage in UAI since HIV diagnosis. We then described how often men considered their UVL in the decision to engage in their most recent UAI incident with HIV-positive and HIV-negative casual partners and/or sex buddies and whether they discussed UVL considerations with these partners. The modified Wald method was used to compute 95% confidence intervals for the proportions of consideration of UVL [10].
Logistic regression analyses were used to explore whether the consideration of UVL in the decision to engage in UAI was associated with type of sex partner and perceived protective value of UVL. The logistic regression analyses included only those men who reported UAI during their last contact with a casual partner or a sex buddy (n=73). Two models were tested using the consideration of UVL as the dependent variable: one for HIV-positive partners and one for (potentially) HIV-negative partners, with the type of sex partner as the main determinant of interest. Nationality and educational level were included in order to explore whether these demographic factors might also have influenced the consideration of UVL in the decision to engage in UAI.
Since we had limited power, we chose to include only those covariates in the final multivariate model that were univariately associated with the consideration of UVL at p<0.10. As age was considered a potential confounder, it was always included in the final model. Our two main determinants, type of sex partner and perceived protective value of UVL, were forced into the final model to allow for comparability between the two models.
All analyses were performed with the SPSS 18 statistical package (SPSS Inc., Chicago, IL, USA).
RESULTS
The median age of the participants was 48 (IQR=42–55); 91% (161/177) had a Dutch nationality; 99% (175/177) of the participants used cART; 60.5% (107/177) had high educational levels and 39.5% (70/177) had middle to low educational levels; the median score of the perceived protective value of UVL regarding UAI between two HIV-positive partners who both had UVL levels was 2 (IQR=2–4); the median score of the perceived protective value of UVL regarding UAI between an HIV-positive man with UVL level and an HIV-negative partner was 3 (IQR=2–5) (Table 1). Of the participants who had practiced UAI with a casual partner in the preceding 6 months, 64% (43/67) also had their last UAI contact with this type of sex partner. Of the participants who had UAI with a sex buddy in the preceding 6 months, 58% (30/52) also had their last UAI contact with this type of sex partner. In total, 73 men had had their most recent UAI contact in the preceding 6 months with either a casual sex partner or a sex buddy.
Table 1.
General characteristics, consideration of UVL since HIV diagnosis, and proportions of UAI with two types of sex partners among 177 HIV-positive MSM with an undetectable viral load, 2010.
| N | % | |
|---|---|---|
|
| ||
| Total sample size | 177 | |
| Age (median; IQR) | 48 (42–55) | |
| Nationality | ||
| Dutch | 161 | 91.0 |
| Non-Dutch | 16 | 9.0 |
| cART | ||
| Yes | 175 | 98.9 |
| No | 2 | 1.1 |
| Educational level | ||
| High | 107 | 60.5 |
| Middle & Low | 70 | 39.5 |
| Perceived protective value of UVL (median; IQR) | ||
| UAI between two HIV-positive partners with UVL levels | 2 (2–4) | |
| UAI between an HIV-positive man with UVL level and an HIV-negative partner | 3 (2–5) | |
| Ever had UAI since HIV diagnosis | 120/177 | 67.8 |
| Consideration of UVL with partners of any HIV status | 75/120 | 62.5 |
| Consideration of UVL with an HIV-positive partner | 53/120 | 44.2 |
| Consideration of UVL with an HIV-negative or status unknown partner | 46/120 | 38.2 |
| Insertive and/or receptive anal intercourse with a casual partner in the preceding six months | 79/177 | 44.6 |
| Unprotected | 67/79 | 84.4 |
| Last UAI contact was with a casual partner | 43/67 | 64.2 |
| Insertive and/or receptive anal intercourse with a sex buddy in the preceding six months | 63/177 | 35.6 |
| Unprotected | 52/63 | 82.5 |
| Last UAI contact was with a sex buddy | 30/52 | 57.7 |
IQR=inter quartile range; cART=combination antiretroviral therapy; UAI=Unprotected Anal Intercourse; UVL=undetectable viral load
Consideration of UVL in the decision to engage in UAI since HIV diagnosis
A majority of the participants (68%; 120/177) reported having UAI at least once since being diagnosed HIV-positive (Table 1). Of those, 63% (75/120) had ever considered UVL in the decision to engage in UAI with either HIV-positive or (potentially) HIV-negative partners; 44% (53/120) with an HIV-positive partner, and 38% (46/120) with a (potentially) HIV-negative partner.
Consideration of UVL during the last UAI contact according to partner’s HIV status and type of sex partner
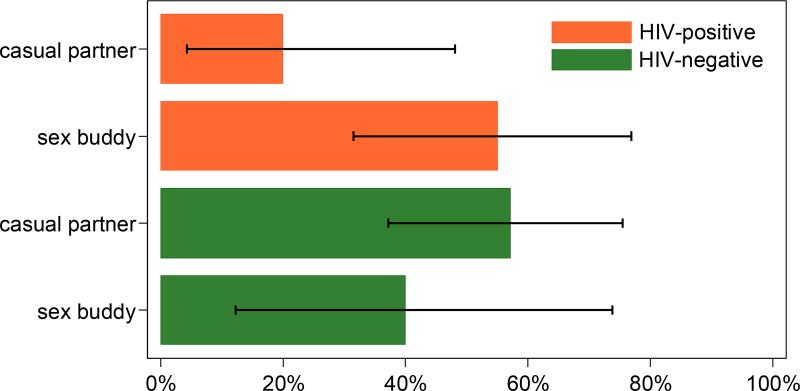
Among participants who had UAI with an HIV-positive partner (n=35), 20% (3/15) considered their partner’s UVL in the decision to engage in UAI with a casual partner and 55% (11/20) with a sex buddy (Figure 1). Among participants who had UAI with a (potentially) HIV-negative partner (n=38), 57% (16/28) considered their own UVL in the decision to engage in UAI with a casual partner and 40% (4/10) with a sex buddy.
Figure 1.
Proportions of consideration of undetectable viral load (UVL) among 73 HIV-positive MSM engaging in UAI, according to partner’s HIV status and partner type, 2010. UAI=unprotected anal intercourse; Note. Error bars represent 95% confidence intervals.
The discussion of the decision to engage in UAI based on an UVL and viral load knowledge
Among the participants who had considered UVL in the decision to engage in UAI with an HIV-positive partner, 100% (3/3) had discussed this with a casual partner and 91% (10/11) with a sex buddy. Accordingly, knowledge of the partner’s UVL was reported by 100% (3/3) of the participants with a casual partner and by 91% (10/11) of the participants with a sex buddy. Among the participants who had considered UVL in the decision to engage in UAI with a (potentially) HIV-negative partner, only 13% (2/16) had discussed this with the casual partner and 25% (1/4) with the sex buddy. The partner’s knowledge of the participant’s UVL was reported by 25% (4/16) of the participants with a casual partner and by 50% (2/4) of the participants with a sex buddy.
Association between type of sex partner and consideration of UVL during the last UAI contact
Univariate analyses revealed that only type of sex partner and perceived protective value of UVL were associated with the consideration of UVL at p<0.10, for HIV-positive and HIV-negative partners, respectively. Multivariate analyses (see Table 2) revealed that for sex with HIV-positive partners, type of partner was (marginally) significantly associated with the consideration of UVL: men were more likely to consider their partner’s UVL in the decision to engage in UAI with a sex buddy than with a casual partner (OR=5.02; 95%CI=0.99–25.31; p=0.051). For (potentially) HIV-negative partners, only perceived protective value of UVL was significantly associated with the consideration of UVL: men who perceived having UVL to be less protective were less likely to consider UVL in the decision to engage in UAI (OR=0.23; 95%CI=0.06–0.96; p=0.044).
Table 2.
Multivariate determinants of the consideration of UVL among 73 MSM who had had UAI during the last contact with either an HIV-positive or a (potentially) HIV-negative casual partner or an HIV-positive or a (potentially) HIV-negative sex buddy, 2010.
| HIV-positive partner | (potentially) HIV-negative partner | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| n/N (%) | ORadj (95%CI) | p-value | n/N (%) | ORadj (95%CI) | p-value | |
|
|
||||||
| Type of sex partner | ||||||
| Casual partner | 3/15 (20%) | 1 | 0.051 | 16/28 (57%) | 1 | 0.170 |
| Sex Buddy | 11/20 (55%) | 5.02 (0.99–25.31) | 4/10 (40%) | 0.28 (0.05–1.73) | ||
| Age (per 10 years increment) | 1.15 (0.94–1.42) | 0.170 | 1.08 (0.92–1.28) | 0.346 | ||
| Perceived protective value of UVL against HIV transmission | ||||||
| HIV-positive partners | ||||||
| No to low risk | 12/28 (43%) | 1 | 0.764 | |||
| Moderate to absolute risk | 2/7 (29%) | 0.74 (0.10–5.42) | ||||
| (potentially) HIV-negative partners | ||||||
| No to low risk | 14/21 (67%) | 1 | 0.044 | |||
| Moderate to absolute risk | 6/17 (35%) | 0.23 (0.06–0.96) | ||||
OR=odds ratio; adj=adjusted; 95%CI=95% Confidence Interval; UVL=undetectable viral load
DISCUSSION
In our sample of HIV-positive MSM, we found relatively high proportions of men who considered their own and their HIV-positive partner’s current UVL in the decision to engage in UAI with various types of sex partners.
We found that men considered their partner’s UVL before engaging in UAI more often with HIV-positive sex buddies than with HIV-positive casual partners. It could be that for men to engage in UAI based on UVL knowledge they need to disclose their viral load status and discuss such a relative complex issue with their sex partners. Knowing the sex partner well can facilitate such disclosure and discussion.
On the other hand, among the HIV-positive participants who had UAI with a (potentially) HIV-negative partner, the consideration of one’s UVL was not related to partner type. The relatively high proportions of men who considered their UVL with (potentially) HIV-negative partners raise the question whether the viral load status was shared with the (potentially) HIV-negative partners and whether the latter have participated in the decision to engage in UAI based on the UVL of their partner. We have shown that only a small number of the (potentially) HIV-negative partners knew the participants’ UVL status before engaging in UAI, and even a smaller number discussed the decision to engage in UAI based on their UVL levels. This suggests that the decision to engage in UAI based on the UVL status was mostly a unilateral decision taken by our participants and was not mutually discussed in advance. Discussion of viral load levels with the (potentially) HIV-negative partner would require to disclose the positive HIV-status, a known barrier because of possible stigma and fear of rejection [11]. In addition, if HIV-positive men disclose their status, they might prefer to avoid viral load information as a too complex subject to discuss because their (potentially) HIV-negative partners might be unaware of viral load issues. Since we collected data only from the HIV-positive participants, future investigations should include the perspectives of HIV-negative MSM in the communication around UVL and UAI.
As for the perceived protective value of UVL, this perception had a significant effect only with respect to UAI with (potentially) HIV-negative partners. If men believed an undetectable viral load would prevent infection during UAI, they were more likely to engage in UAI. The lack of such an association when deciding to engage in UAI with HIV-positive partners might raise the question why HIV-positive men choose to consider UVL when engaging in UAI with HIV-concordant partners and what the perceived added value of such a strategy is in their view. Further qualitative studies should shed more light on this question.
Some limitations of our study should be noticed. We obtained data only from MSM participating in an ongoing online panel of the Netherlands HIV Association. As our panel is a self-selected group of people it may not be representative of other HIV-positive MSM in the Netherlands. Also, as our data on viral load and sexual risk behavior are self-reported, they may be skewed by social desirability. Furthermore, differences in proportions of consideration of UVL between types of (potentially) HIV-negative partners were not statistically significant, probably due to limited power. However, with a larger sample this effect could have been significant and therefore we suggest to repeat this study with a larger sample to be able to confirm our results.
For future research, we recommend to study in more detail the conditions under which MSM consider UVL in the decision to engage in UAI. For example, the Swiss National AIDS Commission stated that having an UVL can potentially eliminate the risk of HIV infection if certain other conditions (e.g., no concurrent STI) are also fulfilled [6]. Whether our participants considered such conditions was not studied here. In addition, other limitations to the consideration of UVL as a risk-reduction strategy also exist. For example, the viral load level in blood is not always perfectly associated with load levels in semen, especially in concurrence with other STIs [12, 13]. Therefore, when appraising their own levels of infectiousness, HIV-positive MSM who engage in insertive UAI cannot completely rely on measurements of the viral load levels in their blood. Furthermore, the Swiss statement is supported by studies among heterosexuals (i.e., vaginal transmission route) [14, 15], but evidence for its validity for MSM (i.e., the anal transmission route) is still lacking. It is therefore necessary that clear clinical and epidemiological evidence will be provided that supports the assumed protective value of having UVL against anal transmission of HIV among MSM. HIV prevention campaigners need such evidence to take an informed stance in the debate around viral load considerations and urgently so, in the light of the already frequent use by MSM.
Acknowledgments
Funding: This study was supported by the ‘AIDS Fonds’, grant no. 2008025
References
- 1.Kalichman SC, Nachimson D, Cherry C, Williams E. AIDS treatment advances and behavioral prevention setbacks: preliminary assessment of reduced perceived threat of HIV-AIDS. Health Psychol. 1998;17(6):546–550. doi: 10.1037//0278-6133.17.6.546. [DOI] [PubMed] [Google Scholar]
- 2.Suarez TP, Kelly JA, Pinkerton SD, Stevenson YL, Hayat M, Smith MD, et al. Influence of a partner's HIV serostatus, use of highly active antiretroviral therapy, and viral load on perceptions of sexual risk behavior in a community sample of men who have sex with men. J Acquir Immune Defic Syndr. 2001;28(5):471–477. doi: 10.1097/00042560-200112150-00011. [DOI] [PubMed] [Google Scholar]
- 3.Vanable PA, Ostrow DG, McKirnan DJ, Taywaditep KJ, Hope BA. Impact of combination therapies on HIV risk perceptions and sexual risk among HIV-positive and HIV-negative gay and bisexual men. Health Psychol. 2000;19(2):134–145. doi: 10.1037//0278-6133.19.2.134. [DOI] [PubMed] [Google Scholar]
- 4.Prestage G, Mao L, Kippax S, Jin F, Hurley M, Grulich A, et al. Use of viral load to negotiate condom use among gay men in Sydney, Australia. AIDS Behav. 2009;13(4):645–651. doi: 10.1007/s10461-009-9527-0. [DOI] [PubMed] [Google Scholar]
- 5.Van de Ven P, Mao L, Fogarty A, Rawstorne P, Crawford J, Prestage G, et al. Undetectable viral load is associated with sexual risk taking in HIV serodiscordant gay couples in Sydney. AIDS. 2005;19(2):179–184. doi: 10.1097/00002030-200501280-00010. [DOI] [PubMed] [Google Scholar]
- 6.Vernazza P, Hirschel B, Bernasconi E, Flepp M. Les personnes séropositives nesouffrant d'aucune autre MST et suivant un traitement antirétroviral efficace ne transmettent pas le VIH par voie sexuelle. Bull Med Suisses. 2008;89:165–169. [Google Scholar]
- 7.Bourne A, Dodds C, Weatherburn P, Keogh P. Perceptions of superinfection risk among gay men with diagnosed HIV who have unprotected anal intercourse. Int J STD AIDS. 2011;22(4):190–193. doi: 10.1258/ijsa.2011.010116. [DOI] [PubMed] [Google Scholar]
- 8.Poudel KC, Poudel-Tandukar K, Yasuoka J, Jimba M. HIV superinfection: another reason to avoid serosorting practice. Lancet. 2007;370(9581):23. doi: 10.1016/S0140-6736(07)61033-2. [DOI] [PubMed] [Google Scholar]
- 9.van den Boom W, Stolte I, Sandfort T, Davidovich U. Serosorting and sexual risk behaviour according to different casual partnership types among MSM: the study of one-night stands and sex buddies. AIDS Care. 2012;24(2):167–173. doi: 10.1080/09540121.2011.603285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agresti A, Coull B. Approximate is better than 'exact' for interval estimation of binomial proportions. The Amercan Statistician. 1998;52:119–126. [Google Scholar]
- 11.Przybyla SM, Golin CE, Widman L, Grodensky CA, Earp JA, Suchindran C. Serostatus disclosure to sexual partners among people living with HIV: examining the roles of partner characteristics and stigma. AIDS Care. 2013;25(5):566–572. doi: 10.1080/09540121.2012.722601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kalichman SC, Cage M, Barnett T, Tharnish P, Rompa D, Austin J, et al. Human immunodeficiency virus in semen and plasma: investigation of sexual transmission risk behavioral correlates. AIDS Res Hum Retroviruses. 2001;17(18):1695–1703. doi: 10.1089/08892220152741397. [DOI] [PubMed] [Google Scholar]
- 13.Politch JA, Mayer KH, Welles SL, O'Brien WX, Xu C, Bowman FP, et al. Highly active antiretroviral therapy does not completely suppress HIV in semen of sexually active HIV-infected men who have sex with men. AIDS. 2012;26(12):1535–1543. doi: 10.1097/QAD.0b013e328353b11b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quinn TC, Wawer MJ, Sewankambo N, Serwadda D, Li C, Wabwire-Mangen F, et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project Study Group. N Engl J Med. 2000;342(13):921–929. doi: 10.1056/NEJM200003303421303. [DOI] [PubMed] [Google Scholar]
- 15.Reynolds SJ, Makumbi F, Nakigozi G, Kagaayi J, Gray RH, Wawer M, et al. HIV-1 transmission among HIV-1 discordant couples before and after the introduction of antiretroviral therapy. AIDS. 2011;25(4):473–477. doi: 10.1097/QAD.0b013e3283437c2b. [DOI] [PMC free article] [PubMed] [Google Scholar]