Abstract
Pilocytic astrocytoma (PA) is the most common glioma in the pediatric population. PAs can exhibit variable behavior that does not always correlate with location. Although oncogenic rearrangements of the BRAF gene have recently been described in PAs, it is not clear whether such alterations have an impact on outcome. An institutional cohort of 147 PAs (118 with outcome data) from both cerebellar and non-cerebellar locations (spine, diencephalon, midbrain, brainstem, and cortex) was utilized in this study. Parameters included quantification of characteristic morphologic variables as well as genes and molecular loci previously shown to be of relevance in high-grade gliomas, including 1p, 9p, 10q, 17p, 19q, and BRAF. Neither 1p, 9p, and 10q nor 19q showed significant association with outcome in PAs, although p16 deletion was more common in PAs of the midbrain, brainstem, and spinal cord. Loss of heterozygosity on 17p13 correlated with increased risk of recurrence in cerebellar tumors. BRAF gene rearrangements were more common in cerebellar tumors than non-cerebellar tumors and associated with classic biphasic histology in the cerebellum. However, clinical outcome was independent of BRAF status. The molecular biology of PAs differs according to location, yet BRAF rearrangements do not appear to produce PAs with different behavior. Nevertheless, such tumors may have altered sensitivity to pathway-specific adjuvant therapy. Additionally, deletion on 17p13 may be an adverse prognostic biomarker in cerebellar tumors.
Keywords: Pilocytic astrocytoma, BRAF, p16, p53, 17p
Introduction
Pilocytic astrocytomas (PAs) are the most common primary brain tumors in children. While many patients with cerebellar and superficial cerebral lesions are cured with gross total resection as befitting their WHO grade 1 status [6], lesions in deep sites, such as the hypothalamus and brainstem, rarely can be removed and carry high risks for recurrence and morbidity. Even some superficial tumors that appear to have a good prognosis based on histology often behave in an unexpectedly aggressive manner [9, 10]. Partly because it is difficult to acquire sufficient numbers of pediatric low-grade gliomas (particularly those from deep-seated, unresectable locations), no consistent panel of markers has been identified that facilitates prognostic or therapeutic stratification, although some histologic features, like oligodendroglial-type morphology, suggest a higher risk of tumor recurrence [18, 45].
Studies focusing on the molecular biology of PAs have shown that these tumors are indeed distinct from higher-grade gliomas. Early cytogenetic work indicated that most PAs had normal or near-normal karyotypes without any consistent abnormalities [2, 4, 38], and DNA ploidy had no correlation with outcome [15]. Furthermore, while P53 overexpression, 17p loss of heterozygosity (LOH), and occasional TP53 mutations have been described in some PAs, p16 deletions and PTEN mutations/10q23 LOH are much less common [7, 13, 16, 47].
Array-based technologies have shed additional light on PA molecular biology. While conventional comparative genomic hybridization confirmed the absence of large cytogenetic abnormalities in most of these tumors [39], array comparative genomic hybridization identified a biologically active, low-level copy number gain of the BRAF gene on 7q34 in a large proportion of PAs [3, 31]. Subsequent work showed that the copy gain is due to a tandem duplication producing a KIAA1549:BRAF fusion protein with constitutive BRAF activity [14, 20, 42], although a minority of cases can involve SRGAP:RAF1 fusion or have other activating BRAF mutations. While such rearrangements have been shown to be more common in cerebellar versus non-cerebellar tumors [3, 14, 21, 22], it is not yet known whether BRAF status is associated with outcome, with other molecular alterations, or with a particular histologic pattern.
In an effort to answer these questions, we describe the results from analysis of 147 PAs, most with matched outcome data extending in some cases for more than 20 years.
Materials and methods
Cohort
This study used formalin-fixed paraffin-embedded tissue (FFPE) from an institutional Neuropathology Brain Tumor Bank. Institutional Review Board approval for a retrospective analysis of archival excess tissue was obtained before initiating the study. The cohort consisted of 147 PAs, including 97 cerebellar PAs and 50 tumors from other sites (Table 1). Of the 147 cases, 118 had outcome data available; median follow-up time was 5.2 years. Material was reviewed by 2 neuropathologists (CH and RLH), verifying that the original diagnosis was accurate. Other low-grade pediatric tumors, such as pilomyxoid astrocytomas, were excluded from this study. Over 75% of cerebellar and cortical cases were judged to have had gross total resection by the neurosurgeons at the time of initial resection, whereas over 90% of midline tumors were judged by the neurosurgeons to have been subtotally resected. Because precise information regarding degree of resection was not available in each case, biomarkers were evaluated controlling for location as a surrogate for extent of resection. Any case that demonstrated recurrence, progression, neuraxis spread, or death was considered an “adverse” outcome. All histologic, immunohistochemical, and molecular analyses were performed while blinded to outcome and, when possible, location.
Table 1.
Distribution of PAs and outcomes by location in cohort
| Location | Total no. | No. with outcome data | No. with adverse outcome (%) | No. with only local recurrence | No. of disseminated/metastatic | No. DoD |
|---|---|---|---|---|---|---|
| Cerebellum | 97 | 71 | 12 (16.9) | 10 | 2 | 0 |
| Brainstem/midbrain | 12 | 12 | 6 (50.0) | 6 | 0 | 0 |
| Hypothalamus | 11 | 9 | 4 (44.4) | 1 | 1 | 2 |
| Thalamus | 10 | 9 | 4 (44.4) | 2 | 1 | 1 |
| Spinal | 9 | 9 | 5 (55.6) | 3 | 2 | 1 |
| Cortex | 7 | 7 | 1 (14.3) | 0 | 1 | 1 |
| Basal ganglia | 1 | 1 | 0 (0.0) | 0 | 0 | 0 |
| Total | 147 | 118 | 32 (27.1) | 22 | 7 | 5 |
147 cases of PA were collected since 1980, the majority of which had corresponding outcome data available. Pooled together, cerebellar and cortical tumors had a lower rate of adverse outcomes compared to deep-seated, midline tumors (P = 0.006 by Mann–Whitney test)
DoD died of disease
PAs were grouped according to anatomic and surgical criteria. In particular, midbrain, brainstem, and spinal lesions were analyzed together because the operative goal is at most debulking rather than full excision at these sites, and these regions blend into each other anatomically. Moreover, both midbrain tumors also involved the brainstem, and the nine spinal tumors had similar poor outcomes and genetic changes as more rostral tumors in the brainstem (see “Results”). “Cerebral” tumors included those of the cortex, basal ganglia, and diencephalon (thalamus and hypothalamus).
Histology and immunohistochemistry
Histologic preparation and immunohistochemical studies for p53, MGMT, and MIB-1 were performed and quantified as previously described [32, 35, 36]. To ensure consistency of grading, all immunohistochemical assessments were done by a single neuropathologist (RLH).
The following histologic parameters were semiquantified for each case: primary pattern (see “Results”); percent area with oligodendroglial-like morphology; sharpness of tumor border (ranging from sharp to widely infiltrative); cellularity; degree of nuclear atypia; presence of degenerative-type nuclear atypia; mitoses per 0.5 cm2; and relative amounts of Rosenthal fibres, eosinophilic granular bodies, hyalinized vessels (on an arbitrary scale of 0–3), micro-vascular proliferation, calcification, inflammation, and necrosis. All histological assessments were done by a single neuropathologist (CH) to ensure consistency.
Tissue microarray (TMA) construction
A manual tissue arrayer [MTA-1, Beecher Instruments (Sun Prairie, WI)] was used to select 0.6 mm cores from paraffin blocks to a blank recipient paraffin block destined for FISH analysis; each case was arrayed in duplicate. Cases in which tissue was inadequate for coring were sectioned and analyzed for FISH separately.
Fluorescence in situ hybridization (FISH)
Formalin-fixed paraffin-embedded blocks, including TMA blocks, were analyzed via FISH using probes for 1p36, 9p21, and 19q13 (Abbott Molecular, Des Plaines, IL). BRAF probe consisted of 3 PAC clones: RP4-726N20, RP5-839B19, and RP4-813F11, previously used to detect BRAF rearrangements in thyroid carcinomas [8]. In particular, RP4-726N20 covers the centromeric end of BRAF, which is the segment that participates in rearrangements identified by FISH in PAs [22, 31]. For ploidy control, centromeric enumeration probes were used for chromosomes 1 (1q25), 7 (CEP7), 9 (CEP9), and 19 (19p13). Approximately 50 cells were analyzed in the targeted region per case. Deletion was scored for 1p36 and 19q13 if the target:ploidy control ratio was less than 0.8, with at least 20% of nuclei showing deletion. Deletion for 9p21 was scored if both signals were lost (homozygous deletion) in at least 20% of nuclei. BRAF abnormality was scored if BRAF:CEP7 was greater or equal to 1.15 and over 20% of cells showed relative BRAF gain. These cutoff points were derived using non-neoplastic brain tissue as controls.
PCR-based microsatellite LOH analysis
DNA was isolated from formalin-fixed paraffin-embedded blocks using standard laboratory procedures. The assay utilized seven microsatellite markers on chromosome 1p22—36.32 (D1S171, D1S162, D1S199, D1S1172, D1S1161, D1S407, and D1S226); 3 on 9p21-22 (D9S251, D9S1679, and D9S1748), 2 on 10q23 (D10S520 and D10S1173); 3 on 17p13 (D17S516, D17S786, and D17S1844); 3 on 19q13.31—19q13.32 (D19S112, D19S206, and D19S559). PCR was performed and the PCR products were analyzed using capillary gel electrophoresis on GeneMapper ABI 3730 (Foster City, CA). As normal tissue was not available, peak height ratios falling outside of 2 standard deviations beyond the mean of previously validated normal values for each polymorphic allele paring were assessed as showing loss of heterozygosity. None of the tumors showed complete deletion of either 1p or 19q.
Image acquisition
Images were acquired using Olympus microscopes (Olympus America, Inc., Center Valley, PA) and SPOT camera software (Diagnostic Instruments, Inc., Sterling Heights, MI). Images and composites were processed with Photoshop CS3 version 10.0.1 (Adobe Systems, Inc., San Jose, CA).
Statistical analysis
Fisher’s exact test was used to compare relative risk of adverse outcome between two groups. Means were compared between multiple groups by Kruskal–Wallis test (non-parametric ANOVA and Dunn’s post hoc) or between two groups by Mann–Whitney test where appropriate. Linear regression was used to assess trends between various quantified molecular and morphologic parameters and risk of adverse outcome. Statistical analysis was performed using GraphPad software (La Jolla, CA) and Microsoft Excel (Redmond, WA).
Results
Cohort characteristics
A total of 147 PAs were collected over 3 decades from 1980 through 2007. Median patient age was 7.7 years (range 1 month–18.8 years). 80.3% had available outcome data, including 73.2% of cerebellar cases and 94.0% of non-cerebellar cases (Table 1). 66% of all PAs were located in the cerebellum, 15.0% were in the diencephalon (thalamus and hypothalamus) or basal ganglia, 14.3% arose in the midbrain, brainstem, or spinal cord, and 4.8% were located in the cortex. 27.1% had adverse outcomes, 68.8% of which consisted strictly of local recurrence or progression. Consistent with prior studies, tumors in superficial locations (cortex and cerebellum) had a lower rate of adverse outcomes compared to deep-seated midline tumors of the diencephalon, midbrain/brainstem, and spinal cord (P = 0.006 by Mann–Whitney test). The median time from initial surgery to an adverse outcome was 1.5 years (range 4 months–16.2 years).
For all biomarkers described below, expression of markers of interest was not significantly different in tumors amenable to outcome analysis versus those that were not.
Molecular profiling of glioma-relevant genes in PAs
1p and 19q codeletion is a well-known biomarker of oligodendrogliomas (albeit only in adult tumors) and is associated with improved chemosensitivity and survival. In this cohort of PAs, none had whole-arm deletion of either 1p or 19q by PCR-based microsatellite LOH analysis, and only one tumor had codeletion via FISH. Neither 1p nor 19q loss correlated with location or outcome in PAs (Table 2). Partial 1p LOH also showed no correlation with oligodendroglial morphology (not shown).
Table 2.
LOH at key genetic loci in PAs according to location and outcome
| Genetic locus | Location | Any LOH (%) | No. of adverse outcomes/total (%) | P |
|---|---|---|---|---|
| 1p | Cerebellum | Yes (56.9) | 4/33 (12.1) | 0.7152 |
| No (43.1) | 4/25 (16.0) | |||
| Cerebrum | Yes (60.0) | 5/12 (41.7) | 0.3246 | |
| No (40.0) | 1/8 (12.5) | |||
| MB/BS/SC | Yes (80.0) | 9/16 (56.3) | 1.0000 | |
| No (20.0) | 2/4 (50.0) | |||
| 19q | Cerebellum | Yes (35.1) | 3/20 (15.0) | 1.0000 |
| No (64.9) | 5/37 (13.5) | |||
| Cerebrum | Yes (27.8) | 2/5 (40.0) | 0.5827 | |
| No (72.2) | 3/13 (23.1) | |||
| MB/BS/SC | Yes (63.2) | 6/12 (50.0) | 0.6332 | |
| No (36.8) | 5/7 (71.4) | |||
| 9p21 (CDKN2A/p16) | Cerebellum | Yes (33.9) | 4/19 (21.1) | 0.1652 |
| No (66.1) | 2/37 (5.4) | |||
| Cerebrum | Yes (38.9) | 2/7 (28.6) | 1.0000 | |
| No (61.1) | 4/11 (36.4) | |||
| MB/BS/SC | Yes (31.6) | 2/6 (33.3) | 0.3189 | |
| No (68.4) | 9/13 (69.2) | |||
| 10q23 (PTEN) | Cerebellum | Yes (50.0) | 2/23 (50.0) | 1.0000 |
| No (50.0) | 2/23 (50.0) | |||
| Cerebrum | Yes (57.1) | 3/8 (37.5) | 0.2088 | |
| No (42.9) | 0/6 (0.0) | |||
| MB/BS/SC | Yes (50.0) | 5/7 (71.4) | 1.0000 | |
| No (50.0) | 4/7 (57.1) | |||
| 17p13 (TP53) | Cerebellum | Yes (33.3) | 5/18 (27.8) | 0.0344* |
| No (66.7) | 2/36 (5.6) | |||
| Cerebrum | Yes (31.3) | 1/5 (20.0) | 1.0000 | |
| No (68.8) | 3/11 (27.3) | |||
| MB/BS/SC | Yes (41.2) | 5/7 (71.4) | 0.6221 | |
| No (58.8) | 5/10 (50.0) |
PAs with outcome data were assessed for loss of heterozygosity (LOH) via PCR (see “Methods”) at genetic loci known to be of biological and/or prognostic significance in higher-grade pediatric and adult gliomas. LOH at 17p13, containing the TP53 gene, showed significant correlation with adverse outcome via Fisher’s exact test, but only in cerebellar tumors (this table includes only the 118 PAs with outcome data; in some cases, DNA was inadequate for assessment in one or more loci)
MB/BS/SC midbrain, brainstem, and spinal cord
P < 0.05 via Kruskal–Wallis
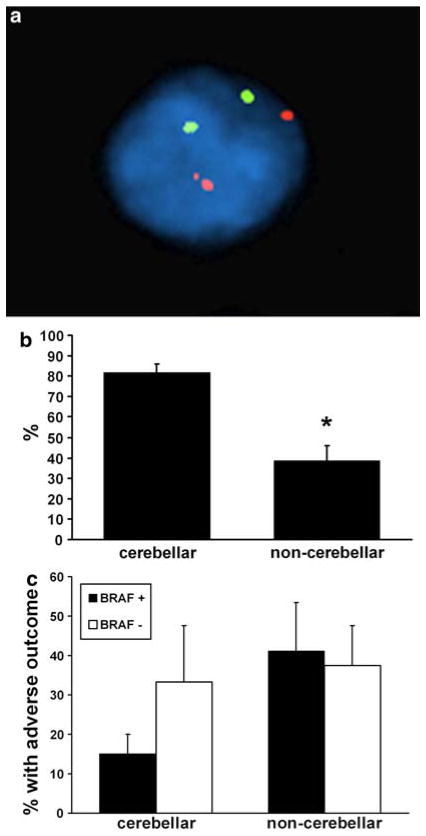
9p21 contains the CDKN2A gene which encodes the p16 tumor suppressor protein; homozygous deletion is often seen in a variety of neoplasms, including higher-grade gliomas [29]. 38.5% of all PAs (including those without outcome data) showed LOH on 9p21, but only 6.4% had homozygous deletion via FISH. However, specific homozygous deletion of p16 was significantly more frequent in tumors of the midbrain, brainstem, and spinal cord than of the cerebrum or cerebellum (20 vs. 4 and 3.6%, respectively; Fig. 1). However, neither p16 homozygous deletion (not shown) nor 9p21 LOH (Table 2) was significantly associated with outcome in any location, and LOH on 9p21 was not more frequent in tumors of the midbrain, brainstem, and spinal cord.
Fig. 1.
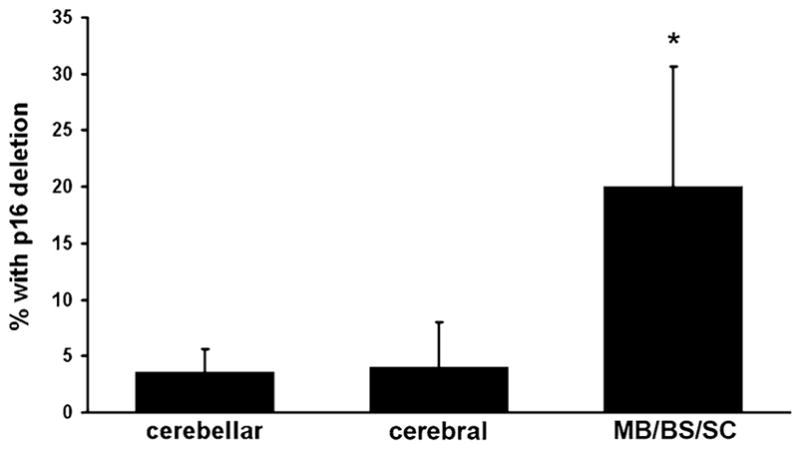
Homozygous p16 deletion is more common in PAs of the midbrain/brainstem and spine (MB/BS/SC) than elsewhere. *P < 0.05 versus cerebral or cerebellar PAs
The PTEN gene is a critical negative regulator of the pro-oncogenic epidermal growth factor signaling pathway and is frequently deleted in high-grade gliomas [29]. LOH of at least 1 microsatellite on 10q23 was seen in 53.1% of all PAs, but showed no association with location or outcome (Table 2).
17p13 contains the TP53 gene, which frequently undergoes LOH and portends a more aggressive clinical course in high-grade pediatric gliomas [33–35]. In this cohort of PAs, LOH on 17p13 was also associated with a significantly elevated rate of adverse outcomes, but only in cerebellar tumors (Table 2). In PAs of all locations, there was a significant correlation between increasing number of LOH loci on 17p13 and decreased p53 immunostaining (P = 0.02 via linear regression); in particular, tumors with any LOH on 17p13 had lower p53 immunoreactivity (0.68 ± 0.1) compared to tumors with intact 17p13 (1.14 ± 0.1, P < 0.01 via Mann–Whitney test). However, even restricted to just cerebellar PAs, no link between p53 expression and outcome was identified (P = 0.96 via Spearman correlation).
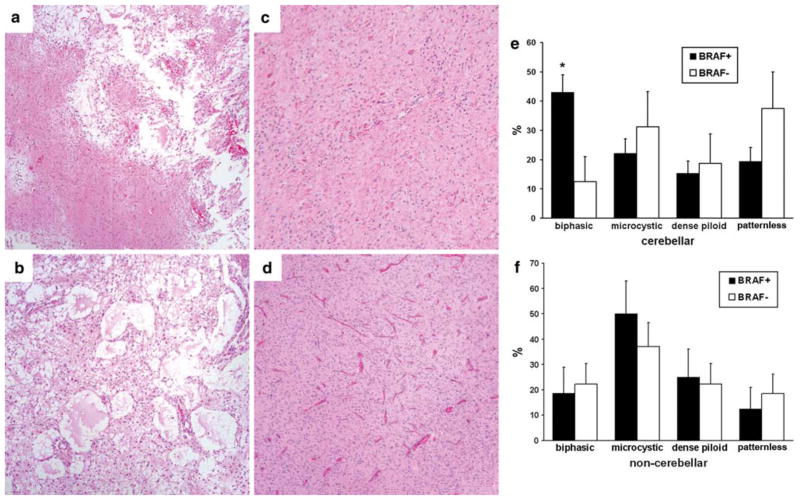
BRAF status and association with location and outcome
Recent studies have identified a rearrangement of the BRAF gene on 7q34, producing constitutively active oncogenic signal [3, 14, 20, 31, 42]. To assess the presence of abnormal BRAF signal, a FISH probe composed of 3 PAC clones covering the entire gene was utilized; this same probe identified analogous BRAF rearrangements in thyroid carcinomas [8], with the typical pattern being two large orange signals plus a third smaller orange signal near one of the larger signals (Fig. 2a). In good agreement with prior work [14, 22], there was a marked difference in BRAF rearrangement pattern by location, with 81.8% of cerebellar PAs showing BRAF rearrangement while only 38.6% of PAs in all other locations had BRAF rearrangement (Fig. 2b, P = 0.006 via Fisher’s exact test). No significant difference existed between tumors of the cerebrum and midbrain, brainstem, and spine (not shown).
Fig. 2.
BRAF rearrangement does not alter clinical outcome in PAs. a Orange-labeled FISH probe using three clones covering the entire BRAF gene (see “Methods”) identifies an abnormal smaller third signal adjacent to one of the larger signals, consistent with duplication and rearrangement of BRAF. b Cerebellar PAs are more likely to show BRAF rearrangement compared to non-cerebellar PAs (*P = 0.006). c Controlling for location, PAs with BRAF rearrangement (BRAF+) do not have significantly different outcomes than those without (BRAF−, P = 0.15 in cerebellar tumors)
Adjusting for location, PAs with BRAF rearrangement showed no significant difference in outcome compared to those without rearrangement (Fig. 2c). Of note, BRAF-negative cerebellar tumors had a mean adverse outcome rate of 33.3 versus 15.1% in BRAF-rearranged cerebellar tumors, but this was not significant because so few cerebellar tumors were BRAF-negative.
The four main histologic patterns of PAs are (1) classic biphasic, alternating between areas of dense and loose architecture (Fig. 3a); (2) microcystic, featuring loose architecture with large spaces often filled with proteinaceous fluid (Fig. 3b); (3) dense piloid, often with many Rosenthal fibres (Fig. 3c); and “patternless growth”, which can be difficult to distinguish from a grade 2 diffuse astrocytoma (Fig. 3d). Cerebellar PAs with BRAF rearrangement tended to produce a biphasic histologic pattern, whereas cerebellar tumors without BRAF showed no significant enrichment of a specific pattern (Fig. 3e). Outside the cerebellum, BRAF-positive and BRAF-negative PAs showed similar distribution of histotypes (Fig. 3f).
Fig. 3.
BRAF correlation with primary histologic pattern in PAs. 147 PAs were scored as to the primary histologic pattern on microscopic examination, including biphasic (a), microcystic (b), dense piloid (c), and patternless growth (d). Cerebellar PAs showing BRAF rearrangement (BRAF+) tended to be biphasic (e), whereas tumors without BRAF rearrangement (BRAF−) showed no significant enrichment for a specific histotype. Outside the cerebellum, BRAF-positive and BRAF-negative PAs showed similar histologic distributions (f). *P < 0.05 compared to BRAF+ dense piloid and patternless tumors. Of note, the eosinophilic structures in d are blood vessels, not Rosenthal fibres
Despite the proliferative effects of constitutively active BRAF, no correlation was identified between BRAF status and MIB-1 PI or p53; MIB-1 PI was 6.8 ± 0.7% in BRAF-positive cases and 6.3 ± 0.9% in BRAF-negative cases, while p53 score was 0.83 ± 0.09 in BRAF-positive cases and 0.86 ± 0.1 in BRAF-negative cases. However, there was a trend toward reduced MGMT expression in BRAF-negative PAs (0.79 ± 0.2 vs. 1.2 ± 0.1 in BRAF-positive tumors, P = 0.06). There was also a significant positive association between BRAF rearrangement and a well-defined tumor border, as well as trends toward younger patients (7.7 vs. 9.3 years) and toward tumors with intact 1p. No associations were present with 9p, 10q, 17p, or 19q status (Table 3).
Table 3.
Associations between BRAF status and age, other genetic alterations, and histological features
| Variable | P |
|---|---|
| Younger age | 0.0584 |
| 1p | 0.0666 |
| 19q | 0.6174 |
| 9p21 | 0.7798 |
| 10q23 | 0.7531 |
| 17p13 | 0.2143 |
| Oligodendroglial morphology | 0.6704 |
| Leptomeningeal spread | 0.1188 |
| Sharp tumor border | 0.0296* |
| High cellularity | 0.8128 |
| Nuclear atypia | 0.9610 |
| Mitoses | 0.5208 |
| Rosenthal fibres | 0.4099 |
| EGBs | 0.9641 |
Multiple regression analysis identified a well-defined tumor border as significantly associated with BRAF rearrangement, plus trends toward rearrangements in younger patients as well as in tumors with intact 1p. Younger age and absence of 1p LOH showed a trend toward association with BRAF rearrangement
EGBs eosinophilic granular bodies
P < 0.05
Discussion
Studies exploring outcome in PAs are few, in part, because these tumors are relatively uncommon, but also because PAs are indolent and require longer follow-up intervals. While mostly curable through complete excision, PAs do have variable outcomes, particularly when located in sites where gross total resection is not possible. Until recently, the molecular biology of PAs has been ambiguous, with no clear patterns of alterations described. These results show that genetic loci characteristic of higher-grade gliomas do not play a significant role in the biological behavior of PAs. BRAF gene rearrangement, however, has recently been observed to be a common event in PAs [3, 14, 20, 31, 42].
Braf is a part of the Raf family of serine/threonine kinases, and is the principal downstream target of Ras in the pro-oncogenic MAPK pathway [12]. Although a relatively new finding in PAs, BRAF abnormalities have been described in a variety of other neoplasms, including melanomas [12], thyroid carcinomas [28], and colonic adenocarcinomas [19]. Most of these neoplasms involve activating point mutations, with the presence of such alterations correlating with adverse outcomes in thyroid and colorectal carcinomas [11, 43] but not melanomas [41].
The results of the current study are consistent with other recent reports suggesting that BRAF rearrangement is more common in PAs of the cerebellum than elsewhere [14, 22]. Adjusting for location, however, BRAF rearrangement does not produce PAs with different biological behavior than tumors arising by different pathways. Specifically, such tumors have no difference in mitotic index, MIB-1 PI, p53 expression, or outcome, although MGMT trends toward being reduced in tumors without BRAF rearrangement and there are some region-specific differences in histology. The lack of an apparent association between BRAF abnormalities and tumor outcome is in some ways unexpected, considering that BRAF rearrangement produces a fusion protein that no longer requires Ras binding and thus has constitutive Braf activity [14, 31, 42]. In this cohort, such rearrangements were significantly associated with a sharp, non-infiltrative tumor border. Increased activity of other proteins, such as TGF-β and Pten, may be required in conjunction with Braf to promote invasion, as has been shown in melanocytes [25].
Despite the fact that not all PAs appear to have specific alterations of BRAF, MAPK pathway activation occurs in the vast majority of these tumors [3, 40], although activation may be increased in those with BRAF rearrangements [42]. These results have clinical relevance, as ongoing phase I and II trials with small molecule MEK inhibitors have shown encouraging results in a variety of neoplasms [1, 5, 26, 37]. Moreover, melanomas and thyroid carcinomas are more sensitive in vitro to small molecule RAF inhibitors if they carry BRAF mutations [17, 24]. In theory, then, PAs with BRAF rearrangement should also be more sensitive to such inhibitors, although downstream MAPK signaling in these tumors may be stimulated by factors other than BRAF activation. Accordingly, BRAF mutation status may not be the sole determinant of sensitivity to agents targeting the Raf/MEK/MAPK signaling cascade.
The frequency of LOH in 1p and 19q in this cohort is higher than that reported previously [44, 46]. Some of the discrepancies may be related to the use of more and different microsatellite markers in this study. Also, the necessity of using unrelated normal samples as controls may have had an impact in some cases. This method of interpreting LOH data has nevertheless proven reliable, when necessary, in analyzing clinical specimens for 1p19q codeletion. Furthermore, tissue blocks were selected that, on H&E, had little admixed non-neoplastic tissue. If the best tumor block contained a region of non-neoplastic tissue, the tumor was isolated via microdissection; thus, “dilution” with admixed non-neoplastic tissue was minimized in these cases. In addition, although some PAs do have whole chromosome copy number gain which could skew LOH results, prior cytogenetic studies (in particular, karyotyping studies) have shown that chromosomes 1 and 19 are not commonly gained in PAs [2, 4, 38, 39]. Consistent with such prior work, only five of the tumors in the current cohort showed hyperploidy of either chromosome 1 or 19 via FISH analysis. Despite the increased frequency of LOH in our study, there was no consistent pattern of LOH loss at specific loci on 1p or 19q, and none of the 1p19q microsatellite markers showed any association with outcome, histology, or location. Thus, these losses are likely small, random deletions intrinsic to neoplastic status and of no particular biological significance.
The trend toward increased MGMT production in PAs with BRAF rearrangements is not easily explained, since Ras GTPase and activating BRAF mutations are positively correlated with high MGMT promoter methylation and reduced expression in other cancers [27, 30]. Non-epigenetic pathways of MGMT regulation are not well-described, although NF-κB may directly promote expression [23].
In this cohort, cerebellar PAs with LOH on 17p13 showed a higher rate of adverse outcomes compared to tumors with intact 17p13. Although the majority of cerebellar PAs were grossly excised (see “Methods”), specific data on extent of resection in each individual case were not available. Thus, it is not known whether the 17p13-deleted cerebellar tumors were more likely to be incompletely resected. Prior work has shown that PAs with LOH anywhere on 17p have higher rates of recurrence, whether the TP53 gene was involved or not [47]. Furthermore, p53 accumulation showed no direct correlation with biological behavior in PAs in this same cohort [18], though p53 protein expression was inversely related to 17p13 LOH (see “Results”). Thus, other genes on 17p besides TP53 may play a significant role in PA biology, although not as a prognostic factor independent of location.
In conclusion, many characteristics of PAs do vary according to location, including BRAF rearrangement. The worse outcomes seen in midline tumors may therefore be related to more than just extent of resection. BRAF rearrangement is more common in cerebellar tumors than elsewhere, yet PAs with this abnormality do not have different intrinsic biological behavior than those arising by other mechanisms. Nevertheless, pending MEK inhibitor clinical trials on PAs may need to take into account differential BRAF rearrangement, as it could prove to be a predictor of therapy response.
Acknowledgments
The authors thank Colleen Lovell and Judy Burnham for their histological expertise; Kathy Cieply, John Salvatore, and Carol Sherer for their assistance in fluorescence in situ hybridization; and Marianne Notaro and Michelle Bisceglia for TMA preparation. This study was funded by a Brain Tumor Society Award from the Pediatric Low Grade Glioma Foundation and NIH R01 NS37704. CH was supported by a Callie Rohr/American Brain Tumor Association Fellowship. Portions of this data were presented at the American Association of Neuropathologists 2009 Annual Meeting in San Antonio, TX.
Footnotes
Conflicts of interest statement The authors declare that they have no conflict of interest.
Contributor Information
Craig Horbinski, Department of Pathology, University of Kentucky, 800 Rose St., Lexington, KY 40536, USA.
Ronald L. Hamilton, Department of Pathology, University of Pittsburgh, 200 Lothrop Street, Pittsburgh, PA 15213, USA
Yuri Nikiforov, Department of Pathology, University of Pittsburgh, 200 Lothrop Street, Pittsburgh, PA 15213, USA.
Ian F. Pollack, Department of Pediatric Neurosurgery, Children’s Hospital of Pittsburgh, 45th Street and Penn Avenue, Pittsburgh, PA 15201, USA
References
- 1.Adjei AA, Cohen RB, Franklin W, et al. Phase I pharmacokinetic and pharmacodynamic study of the oral, small-molecule mitogen-activated protein kinase kinase 1/2 inhibitor AZD6244 (ARRY-142886) in patients with advanced cancers. J Clin Oncol. 2008;26(13):2139–2146. doi: 10.1200/JCO.2007.14.4956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agamanolis DP, Malone JM. Chromosomal abnormalities in 47 pediatric brain tumors. Cancer Genet Cytogenet. 1995;81(2):125–134. doi: 10.1016/0165-4608(94)00123-s. [DOI] [PubMed] [Google Scholar]
- 3.Bar EE, Lin A, Tihan T, Burger PC, Eberhart CG. Frequent gains at chromosome 7q34 involving BRAF in pilocytic astrocytoma. J Neuropathol Exp Neurol. 2008;67(9):878–887. doi: 10.1097/NEN.0b013e3181845622. [DOI] [PubMed] [Google Scholar]
- 4.Bhattacharjee MB, Armstrong DD, Vogel H, Cooley LD. Cytogenetic analysis of 120 primary pediatric brain tumors and literature review. Cancer Genet Cytogenet. 1997;97(1):39–53. doi: 10.1016/s0165-4608(96)00330-5. [DOI] [PubMed] [Google Scholar]
- 5.Blumenschein GR, Jr, Gatzemeier U, Fossella F, et al. Phase II, multicenter, uncontrolled trial of single-agent sorafenib in patients with relapsed or refractory, advanced non-small-cell lung cancer. J Clin Oncol. 2009;27(26):4274–4280. doi: 10.1200/JCO.2009.22.0541. [DOI] [PubMed] [Google Scholar]
- 6.Campbell JW, Pollack IF. Cerebellar astrocytomas in children. J Neurooncol. 1996;28(2–3):223–231. doi: 10.1007/BF00250201. [DOI] [PubMed] [Google Scholar]
- 7.Cheng Y, Pang JC, Ng HK, et al. Pilocytic astrocytomas do not show most of the genetic changes commonly seen in diffuse astrocytomas. Histopathology. 2000;37(5):437–444. doi: 10.1046/j.1365-2559.2000.01005.x. [DOI] [PubMed] [Google Scholar]
- 8.Ciampi R, Knauf JA, Kerler R, et al. Oncogenic AKAP9-BRAF fusion is a novel mechanism of MAPK pathway activation in thyroid cancer. J Clin Invest. 2005;115(1):94–101. doi: 10.1172/JCI23237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dirven CM, Mooij JJ, Molenaar WM. Cerebellar pilocytic astrocytoma: a treatment protocol based upon analysis of 73 cases and a review of the literature. Childs Nerv Syst. 1997;13(1):17–23. doi: 10.1007/s003810050033. [DOI] [PubMed] [Google Scholar]
- 10.Due-Tonnessen BJ, Helseth E, Scheie D, Skullerud K, Aamodt G, Lundar T. Long-term outcome after resection of benign cerebellar astrocytomas in children and young adults (0–19 years): report of 110 consecutive cases. Pediatr Neurosurg. 2002;37(2):71–80. doi: 10.1159/000065108. [DOI] [PubMed] [Google Scholar]
- 11.Elisei R, Ugolini C, Viola D, et al. BRAF(V600E) mutation and outcome of patients with papillary thyroid carcinoma: a 15-year median follow-up study. J Clin Endocrinol Metab. 2008;93(10):3943–3949. doi: 10.1210/jc.2008-0607. [DOI] [PubMed] [Google Scholar]
- 12.Fecher LA, Cummings SD, Keefe MJ, Alani RM. Toward a molecular classification of melanoma. J Clin Oncol. 2007;25(12):1606–1620. doi: 10.1200/JCO.2006.06.0442. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez C, Figarella-Branger D, Girard N, et al. Pilocytic astrocytomas in children: prognostic factors—a retrospective study of 80 cases. Neurosurgery. 2003;53(3):544–553. doi: 10.1227/01.neu.0000079330.01541.6e. (discussion 554–545) [DOI] [PubMed] [Google Scholar]
- 14.Forshew T, Tatevossian RG, Lawson AR, et al. Activation of the ERK/MAPK pathway: a signature genetic defect in posterior fossa pilocytic astrocytomas. J Pathol. 2009;218(2):172–181. doi: 10.1002/path.2558. [DOI] [PubMed] [Google Scholar]
- 15.Forsyth PA, Shaw EG, Scheithauer BW, O’Fallon JR, Layton DD, Jr, Katzmann JA. Supratentorial pilocytic astrocytomas. A clinicopathologic, prognostic, and flow cytometric study of 51 patients. Cancer. 1993;72(4):1335–1342. doi: 10.1002/1097-0142(19930815)72:4<1335::aid-cncr2820720431>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 16.Hayes VM, Dirven CM, Dam A, et al. High frequency of TP53 mutations in juvenile pilocytic astrocytomas indicates role of TP53 in the development of these tumors. Brain Pathol. 1999;9(3):463–467. doi: 10.1111/j.1750-3639.1999.tb00535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoeflich KP, Herter S, Tien J, et al. Antitumor efficacy of the novel RAF inhibitor GDC-0879 is predicted by BRAFV600E mutational status and sustained extracellular signal-regulated kinase/mitogen-activated protein kinase pathway suppression. Cancer Res. 2009;69(7):3042–3051. doi: 10.1158/0008-5472.CAN-08-3563. [DOI] [PubMed] [Google Scholar]
- 18.Horbinski C, Hamilton RL, Lovell C, Burnham J, Pollack IF. Impact of morphology, MIB-1, p53 and MGMT on outcome in pilocytic astrocytomas. Brain Pathol. 2009 doi: 10.1111/j.1750-3639.2009.00336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jass JR. Colorectal cancer: a multipathway disease. Crit Rev Oncog. 2006;12(3–4):273–287. doi: 10.1615/critrevoncog.v12.i3-4.50. [DOI] [PubMed] [Google Scholar]
- 20.Jones DT, Kocialkowski S, Liu L, et al. Tandem duplication producing a novel oncogenic BRAF fusion gene defines the majority of pilocytic astrocytomas. Cancer Res. 2008;68(21):8673–8677. doi: 10.1158/0008-5472.CAN-08-2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones DT, Kocialkowski S, Liu L, Pearson DM, Ichimura K, Collins VP. Oncogenic RAF1 rearrangement and a novel BRAF mutation as alternatives to KIAA1549:BRAF fusion in activating the MAPK pathway in pilocytic astrocytoma. Oncogene. 2009;28(20):2119–2123. doi: 10.1038/onc.2009.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Korshunov A, Meyer J, Capper D, et al. Combined molecular analysis of BRAF and IDH1 distinguishes pilocytic astrocytoma from diffuse astrocytoma. Acta Neuropathol. 2009;118(3):401–405. doi: 10.1007/s00401-009-0550-z. [DOI] [PubMed] [Google Scholar]
- 23.Lavon I, Fuchs D, Zrihan D, et al. Novel mechanism whereby nuclear factor kappaB mediates DNA damage repair through regulation of O(6)-methylguanine-DNA-methyltransferase. Cancer Res. 2007;67(18):8952–8959. doi: 10.1158/0008-5472.CAN-06-3820. [DOI] [PubMed] [Google Scholar]
- 24.Liu D, Liu Z, Jiang D, Dackiw AP, Xing M. Inhibitory effects of the mitogen-activated protein kinase kinase inhibitor CI-1040 on the proliferation and tumor growth of thyroid cancer cells with BRAF or RAS mutations. J Clin Endocrinol Metab. 2007;92(12):4686–4695. doi: 10.1210/jc.2007-0097. [DOI] [PubMed] [Google Scholar]
- 25.Lo RS, Witte ON. Transforming growth factor-beta activation promotes genetic context-dependent invasion of immortalized melanocytes. Cancer Res. 2008;68(11):4248–4257. doi: 10.1158/0008-5472.CAN-07-5671. [DOI] [PubMed] [Google Scholar]
- 26.Lorusso PM, Adjei AA, Varterasian M, et al. Phase I and pharmacodynamic study of the oral MEK inhibitor CI-1040 in patients with advanced malignancies. J Clin Oncol. 2005;23(23):5281–5293. doi: 10.1200/JCO.2005.14.415. [DOI] [PubMed] [Google Scholar]
- 27.Nagasaka T, Sasamoto H, Notohara K, et al. Colorectal cancer with mutation in BRAF, KRAS, and wild-type with respect to both oncogenes showing different patterns of DNA methylation. J Clin Oncol. 2004;22(22):4584–4594. doi: 10.1200/JCO.2004.02.154. [DOI] [PubMed] [Google Scholar]
- 28.Nikiforov YE. Thyroid carcinoma: molecular pathways and therapeutic targets. Mod Pathol. 2008;21(Suppl 2):S37–S43. doi: 10.1038/modpathol.2008.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ohgaki H, Kleihues P. Genetic pathways to primary and secondary glioblastoma. Am J Pathol. 2007;170(5):1445–1453. doi: 10.2353/ajpath.2007.070011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patra SK. Ras regulation of DNA-methylation and cancer. Exp Cell Res. 2008;314(6):1193–1201. doi: 10.1016/j.yexcr.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 31.Pfister S, Janzarik WG, Remke M, et al. BRAF gene duplication constitutes a mechanism of MAPK pathway activation in low-grade astrocytomas. J Clin Invest. 2008;118(5):1739–1749. doi: 10.1172/JCI33656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pollack IF, Campbell JW, Hamilton RL, Martinez AJ, Bozik ME. Proliferation index as a predictor of prognosis in malignant gliomas of childhood. Cancer. 1997;79(4):849–856. [PubMed] [Google Scholar]
- 33.Pollack IF, Finkelstein SD, Burnham J, et al. Age and TP53 mutation frequency in childhood malignant gliomas: results in a multi-institutional cohort. Cancer Res. 2001;61(20):7404–7407. [PubMed] [Google Scholar]
- 34.Pollack IF, Finkelstein SD, Woods J, et al. Expression of p53 and prognosis in children with malignant gliomas. N Engl J Med. 2002;346(6):420–427. doi: 10.1056/NEJMoa012224. [DOI] [PubMed] [Google Scholar]
- 35.Pollack IF, Hamilton RL, Finkelstein SD, et al. The relationship between TP53 mutations and overexpression of p53 and prognosis in malignant gliomas of childhood. Cancer Res. 1997;57(2):304–309. [PubMed] [Google Scholar]
- 36.Pollack IF, Hamilton RL, Sobol RW, et al. O6-methyl-guanine-DNA methyltransferase expression strongly correlates with outcome in childhood malignant gliomas: results from the CCG-945 Cohort. J Clin Oncol. 2006;24(21):3431–3437. doi: 10.1200/JCO.2006.05.7265. [DOI] [PubMed] [Google Scholar]
- 37.Rinehart J, Adjei AA, Lorusso PM, et al. Multicenter phase II study of the oral MEK inhibitor, CI-1040, in patients with advanced non-small-cell lung, breast, colon, and pancreatic cancer. J Clin Oncol. 2004;22(22):4456–4462. doi: 10.1200/JCO.2004.01.185. [DOI] [PubMed] [Google Scholar]
- 38.Roberts P, Chumas PD, Picton S, Bridges L, Livingstone JH, Sheridan E. A review of the cytogenetics of 58 pediatric brain tumors. Cancer Genet Cytogenet. 2001;131(1):1–12. doi: 10.1016/s0165-4608(01)00483-6. [DOI] [PubMed] [Google Scholar]
- 39.Sanoudou D, Tingby O, Ferguson-Smith MA, Collins VP, Coleman N. Analysis of pilocytic astrocytoma by comparative genomic hybridization. Br J Cancer. 2000;82(6):1218–1222. doi: 10.1054/bjoc.1999.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sharma MK, Zehnbauer BA, Watson MA, Gutmann DH. RAS pathway activation and an oncogenic RAS mutation in sporadic pilocytic astrocytoma. Neurology. 2005;65(8):1335–1336. doi: 10.1212/01.wnl.0000180409.78098.d7. [DOI] [PubMed] [Google Scholar]
- 41.Shinozaki M, Fujimoto A, Morton DL, Hoon DS. Incidence of BRAF oncogene mutation and clinical relevance for primary cutaneous melanomas. Clin Cancer Res. 2004;10(5):1753–1757. doi: 10.1158/1078-0432.ccr-1169-3. [DOI] [PubMed] [Google Scholar]
- 42.Sievert AJ, Jackson EM, Gai X, et al. Duplication of 7q34 in pediatric low-grade astrocytomas detected by high-density single-nucleotide polymorphism-based genotype arrays results in a novel BRAF fusion gene. Brain Pathol. 2009;19(3):449–458. doi: 10.1111/j.1750-3639.2008.00225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Souglakos J, Philips J, Wang R, et al. Prognostic and predictive value of common mutations for treatment response and survival in patients with metastatic colorectal cancer. Br J Cancer. 2009;101(3):465–472. doi: 10.1038/sj.bjc.6605164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tada K, Kochi M, Saya H, et al. Preliminary observations on genetic alterations in pilocytic astrocytomas associated with neurofibromatosis 1. NeuroOncology. 2003;5(4):228–234. doi: 10.1215/s115285170300005x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tibbetts KM, Emnett RJ, Gao F, et al. Histopathologic predictors of pilocytic astrocytoma event-free survival. Acta Neuropathol. 2009;117(6):657–665. doi: 10.1007/s00401-009-0506-3. [DOI] [PubMed] [Google Scholar]
- 46.von Deimling A, Fimmers R, Schmidt MC, et al. Comprehensive allelotype and genetic analysis of 466 human nervous system tumors. J Neuropathol Exp Neurol. 2000;59(6):544–558. doi: 10.1093/jnen/59.6.544. [DOI] [PubMed] [Google Scholar]
- 47.Willert JR, Daneshvar L, Sheffield VC, Cogen PH. Deletion of chromosome arm 17p DNA sequences in pediatric high-grade and juvenile pilocytic astrocytomas. Genes Chrom Cancer. 1995;12(3):165–172. doi: 10.1002/gcc.2870120303. [DOI] [PubMed] [Google Scholar]