Abstract
This paper examines the association between alcohol consumption and sexual risk behaviors (unprotected sex, multiple sex partners, sex under influence of drugs or alcohol and commercial sex) in a sample of Central Asian migrant and non-migrant laborers in the largest marketplace in Kazakhstan. We used data from The Silk Road Health Project, conducted from 2010 to 2013 with 1342 male migrant and non-migrant market workers. Participants were selected through respondent driven sampling at the Baraholka Market in Almaty, Kazakhstan. We used regression analyses adjusting for potential confounders to examine the relationship between alcohol consumption and sexual risk behavior. We found that hazardous drinking was associated with an increase in the odds of sex under the influence of drugs (aOR = 6.09, 95% CI 3.48, 10.65; p < .001) and purchasing commercial sex (aOR = 2.02, 95% CI 1.02, 4.02; p < .05). We identified potential targets for HIV interventions to reduce sexual risk behaviors among this key population.
Keywords: Sexual behaviors, Migrants, Alcohol, Central Asia
Introduction
HIV and alcohol use disorders (AUD) are serious epidemics in Kazakhstan, and Eastern Europe. Unlike many parts of the world, the HIV epidemic in Kazakhstan and Eastern Europe has continued to accelerate [1, 2]. Kazakhstan is one of nine countries worldwide that has experienced a precipitous rise in HIV incidence (> 25%) during the past decade [3]. As in other Central Asian counties (Kyrgyzstan, Tajikistan, Uzbekistan, and Turkmenistan), Kazakhstan’s rapidly growing HIV rate is largely driven by injection drug use [4, 5] and sexual risk behaviors [6, 7]. Both transmission routes are exacerbated by the extremely high prevalence of Alcohol Use Disorders (AUD) in this region where it was estimated in 2010 that 15% of Kazakh men were heavy episodic drinkers and 8.9% had AUD [8]. Studies among adult general populations in Central Asia and Eastern Europe suggest that Kazakhstan is among the countries with the highest rates of heavy episodic drinking in the region [8, 9]. There is mounting empirical literature from Eastern Europe and Central Asia suggesting that alcohol use heightens HIV risk behaviors among non-migrant market laborers, people who inject drugs and other populations [10–12]. Globally, dangerous patterns of alcohol consumption constitute a major cause of morbidity and mortality from accidents, injuries, liver damage, and other physical and psychiatric illnesses [13–16]. Research suggests that AUD heightens transmission of HIV [17], accelerates HIV disease progression through a decline in CD4 count [18, 19], reduces linkages to HIV care [18, 20], increases mortality [21] and increases sexual risk behaviors including unprotected sex, sex under the influence of drugs and alcohol, multiple sex partners and purchasing sex [21–31].
A number of studies conducted around the world have shown that alcohol use among migrant workers is a major risk factor for engaging in sexual behaviors that puts one at risk for HIV [32–35]. Few studies have examined this topic among migrant workers in Central Asia, despite the growing population of labor migrants in Kazakhstan from surrounding countries [36, 37]. Labor migrants in Central Asia including Kazakhstan are among the world’s most vulnerable populations to HIV infection [33, 38, 39]. The collapse of the Soviet Union in 1991 led to an economic crisis in the region that increased unemployment, poverty and mass emigration of foreign workers from other Central Asian countries into Kazakhstan in search of greater economic opportunities [36, 37, 40, 41]. Each year, an estimated one million labor migrants enter Kazakhstan, the majority of whom obtain employment at the Baraholka Marketplace in Almaty, the largest marketplace in Central Asia [36]. Prior research on this population found that mobility patterns heightened the risk for biologically confirmed STIs, commercial sex and unprotected sex among internal migrants and non-migrants [10]. External male migrants reported the lowest rates of STIs and sexual risk behaviors [10]. Studies in Russia have found that Central Asian male migrant workers have a high prevalence of alcohol, drug use and sexual risk compared to other migrant groups [32, 33]. External migrants are individuals who cross international borders to enter a foreign country. Internal migrants are individuals who travel within a country to new places of residence, typically for labor-related reasons [40].
HIV sexual risk behaviors among mobile labor migrants and other key HIV-affected populations have also been associated with several structural social, economic and policy risk factors such as poverty, unstable housing, poor living conditions, adverse employment situations, negligible access to health care services, lack of social support, strict migration policies, policing, incarceration and isolation from national and non-governmental AIDS organizations [42–46]. The structural risk framework suggests that factors exogenous to the individual play a crucial role in shaping explosive social contexts conducive to HIV transmission among key affected populations including migrant workers [47, 48]. An understudied risk faced by migrant workers is the relationship between imprisonment, harsh policing behaviors and HIV risk outcomes including sexual behaviors and alcohol use. Research suggests that incarceration in Kazakhstan increases risk of HIV and estimates more than 25% of all registered cases of HIV infection occur within prison settings [43, 46]. In Kazakhstan, the incoming migratory flow from surrounding Central Asian countries is regulated by legal authorities along national borders and in the marketplace by stopping migrants for questioning, examining paperwork to ensure legal and residency status, and enforcing migration laws [37, 49]. Qualitative interviews and focus groups with Uzbek labor migrants in Kazakhstan identified harsh policing practices that included frequent questioning, harassment, physical beatings, and arrest by migration police and market officials [50]. However, no studies have examined the association between these risks, alcohol and policing or other structural factors among labor migrants in Central Asia or globally. To understand the relationship between alcohol and other drug use, and sexual behaviors, we must consider the role of structural risk factors such as poverty, homelessness, criminal justice involvement and access to medical care and mobility. Research has yet to examine the relationship between AUD and sexual risks among labor migrants in Central Asia, after controlling for risk and mobility factors. Additionally, relationships between alcohol and sexual risk behaviors are understudied among non-migrant populations in Kazakhstan and other parts of Central Asia and Eastern Europe. To address this dearth in the literature, this study examines relationships between alcohol and sexual risk in a sample of migrant and non-migrant market laborers in Almaty, Kazakhstan.
A recent systematic review on global migration and HIV transmission underscores that empirical literature has used non-probabilistic samples, qualitative data, or a limited range of structural risks that drive HIV risk and alcohol and drug use among labor migrants [34]. This paper addresses some of these methodological shortcomings and research gaps in prior studies by examining the extent to which AUD is associated with increased sexual risk among a large respondent-driven sample (RDS) of three groups of male market workers in Kazakhstan (external migrants, internal migrants, non-migrants) after adjusting for potentially confounding risk characteristics, migration status and mobility. We first describe the sociodemographic, drug use, sexual risk, HIV and STI status, structural risks (homelessness, poverty, criminal justice, access to care, mobility and migration status and mobility characteristics) by alcohol use (hazardous drinking). Next, we examine associations between hazardous drinking and sexual risk behaviors, after adjusting for socio-demographic characteristics and structural risk covariates. We hypothesize that, after adjusting for socio-demographic and structural risk confounders (homelessness, criminal justice, access to care, mobility and migration status), hazardous drinking will be associated with multiple sex partners, unprotected sex, commercial sex, and sex under the influence of drugs or alcohol.
Methods
Data and Sample
We used cross-sectional data from The Silk Road Health Project, which recruited participants from the Baraholka Market. The purpose of the Silk Road Study was to examine the relationship between mobility, structural risk environments, sexually transmitted infections, HIV risk behaviors (e.g., commercial sex, multiple sex partners, unprotected sex), drug use, trauma, mental health, physical health and social welfare and other factors among internal, external and non-migrant market vendors in Almaty Kazakhstan [39].
The participants for the Silk Road study were recruited using Respondent Driven Sampling in which two seeds were selected from each of the five groups (Kazakh non-migrant, Kazakh internal migrant, Kyrgz migrant, Tajik migrant, and Uzbek migrant) [39]. Internal migrant workers were defined as Kazakh citizens who lived beyond a 2 h commute to Almaty City at the time of the study and non-migrants were defined as workers who maintained a primary residence that was within 2 h commuting distance to the city. Recruitment in waves of seeds eventually results in a representative sample that is independent of the initial seeds and provides an incentive system to reach hidden populations [51, 52]. External and internal migrants were considered a hidden population by virtue of their often stigmatized and socially marginalized status in the marketplace and broader Kazakh society [39].
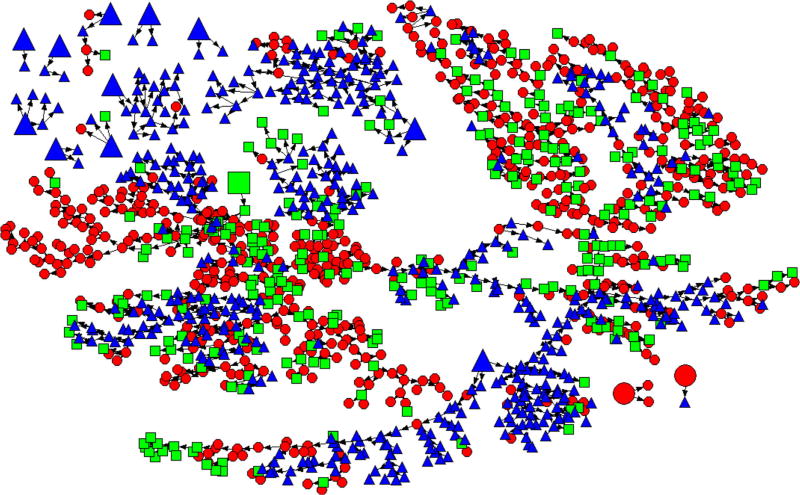
In RDS sampling techniques, each time a seed recruits a new group of participants is considered a recruitment wave. Seeds were selected from the marketplace to recruit male migrants from Kyrgyzstan, Tajikistan and Uzbekistan and a comparison group of internal and non-migrants from Kazakhstan. Any individual was eligible to be a seed who met the eligibility criteria. Coupons were provided to each seed upon enrollment into the study with instructions to recruit three additional potential subjects for screening into the study. Trained research staff recruited 14 participants using Respondent Driving Sampling (RDS) methods who assumed the role of “seeds” (two non-migrants, one internal migrant, and eleven external migrants) to recruit additional eligible participants for screening and enrollment into the study. The 14 participants selected as seeds generated 14 isolated recruitment chains of which two chains accounted for 90% of the sample. Equilibrium was attained after 6 waves accounting for 88% of the sample. The longest chain consisted of 36 recruitment waves. The remaining waves repeated until a representative sample was attained which was measured using a homiphily index. A homiphily index measures the tendency of participants to recruit from their own group rather than at random [51, 52]. Homiphily indices were .72 for non-migrants, .69 for external migrants and .20 for internal migrants [10]. There was a 72% probability that non-migrant seeds recruited new participants at random indicating that a large percentage of random mixing occurred across migrant groups. Additional information on recruitment procedures, network sizes, and RDS characteristics are provided elsewhere [10]. Fig. 1 presents the RDS design used in this study to recruit a representative sample of external, internal and non-migrants [10].
Fig. 1.
RDS sample from 14 seeds (red circle non-migrant, green square internal migrant, blue triangle external migrant, large shape seed)
Eligibility and Inclusion Criteria
Eligibility for men to participate in the study included, (1) selection as a seed or a valid recruitment coupon, (2) between the ages of 18 and 60, (3) valid citizenship of Kazakhstan, Kyrgyzstan, or Uzbekistan, (4) Employed in the Baraholka Market in Almaty during the past week, (5) Fluency in Russian, Tajik, or Kazakh, (6) and ability to provide informed consent. Assessments collected data from eligible participants on socio-demographics, alcohol consumption, illicit drug use, migration and mobility variables, criminal justice involvement, access to health, and sexual risk behaviors using Audio Computer-Assisted Self-Interview (ACASI). Biological assays tested for the presence of HIV, syphilis, gonorrhea, and chlamydia. Participants who consented and completed biological assays and the assessments received $10USD in addition to $1USD for completing the screening instrument and $5USD for each referred participant in the case of seeds. Research staff provided pre-test counseling at the time of testing and posttest counseling at the time of notification. Referrals for HIV/STI treatment were provided.
Measures
Exposure
Alcohol consumption
We measured participants’ alcohol consumption using the Alcohol Use Disorders Identification test (AUDIT) and a score of eight or higher indicated hazardous drinking behavior in the past year [53, 54].
Outcome
Sexual Risk Behaviors
We measured four sexual risk behaviors with primary and other partners within the past 90 days using the risk behavior assessment (RBA). Unprotected sex included a dichotomous variable of unprotected vaginal or anal sex with any sexual partner in the past 90 days. Multiple sexual partners consisted of a dichotomized variable measuring vaginal or anal sex with more than one partner in the past 90 days. Questions measured engaging in commercial sex by asking participants if in the past 90 days whether the participant had exchanged money, goods, or drugs for sex with a woman. Participants were asked to report engaging in sex while under the influence of alcohol or drugs in the past 90 days.
Control Covariates
Confounders of interest were selected based upon review of recent global literature emphasizing the impact of structural and sociodemographic variables on sexual risk behaviors with both migrant and non-migrant populations.
Socio-Demographic Characteristics
Participants provided self-reported information on age (years), education (high school degree/greater or less than high school) coresidence (live with spouse or girlfriend) and marital status. Employment included whether participants’ job responsibilities included roles as an owner, vendor, carrier, transporter of goods, or other.
Illicit Drug Use
We assessed participants’ lifetime and past month use of marijuana or hashish, club drugs, amphetamines, heroin, tranquilizers and other illicit drugs. We created dichotomous variables for types of drugs and combined to measure any lifetime illicit drug use. We combined all drugs used in the past 30 days to provide a dichotomous indicator measuring any recent drug use.
Biologically Confirmed Cases of Sexually Transmitted Infections
We assessed for HIV, syphilis, gonorrhea, and chlamydia through biological assay. The methods for biological specimen collection are detailed in a prior publication by El-Bassel et al. [39].
Structural Risk Factors
Criminal Justice Involvement. We assessed involvement with the criminal justice system through measuring the number of times participants experienced questioning by market officials, questioning by migration police, arrest by migration police and incarceration in the past 90 days. Each criminal justice variable was dichotomized to reflect any involvement. Access to health care was categorized as whether a participant had needed to see a doctor in the past 90 days and did not go. Homelessness: Participants were asked if in the past 90 days they had been without a place to sleep. Poverty was measured by categorizing a participant’s income as above or below the living wage in Kazakhstan (15,999 tenge per month in 2011) [55]. Mobility and migration status. Mobility included a dichotomous variable measuring if the participant traveled anywhere outside of Almaty in the past 90 days. Dichotomous variables provided indicators of migration status as either non-migrant, internal migrant from Kazakhstan or external migrants from Tajikistan, Kyrgyzstan, or Uzbekistan.
Data Analysis
RDS weights were calculated using RDSAT and analyzed using the statistical computing software STATA version 14 for analysis (STATA 2015) [56]. Weighted population proportions and means for sexual risk behaviors, alcohol consumption, drug use, sociodemographic, structural and criminal justice variables were calculated and reported in Table 1 (numbers and percentages relative to totals do not add up because of RDS weighting). We also stratified characteristics of the sample by alcohol consumption patterns and performed bivariate Wald tests that adjusted for the RDS study design to assess for statistically significant differences between participants with and without hazardous drinking patterns [57]. To examine our central hypothesis, we performed multivariate logistic regressions to assess if alcohol consumption patterns predicted increased odds of sexual risk behaviors (unprotected sex, more than one sexual partner, sex under the influence of drugs or alcohol and commercial sex) after adjusting for potential confounders and RDS weights. We fit logistic regression models for hazardous alcohol consumption that adjusted for drug use, impoverishment, homelessness, access to health care and criminal justice involvement, mobility and external migration status [58, 59].
Table 1.
Descriptive characteristics and bivariate tests stratified by alcohol use (n = 1342)
| Overall % (n) | Yes % (n) | No % (n) | |
|---|---|---|---|
| Total sample | 13.07 (184) | 86.93 (1158) | |
| Sexual risk variables | |||
| Commercial sex | 8.53 (119) | 15.96 (33)* | 7.41 (86)* |
| Multiple sexual partners | 28.81 (355) | 34.73 (66) | 27.92 (289) |
| Had unprotected vaginal/anal sex with any female partner last 90 days | 28.89 (441) | 39.48 (91)* | 27.30 (350)* |
| Sex under influence of drugs/alcohol | 10.03 (167) | 28.92 (72)*** | 6.81 (95)*** |
| Drug use | 11.46 (139) | 20.50 (34)** | 10.10 (105**) |
| Marijuana | 7.51 (88) | 15.61 (22)** | 6.29 (66)** |
| Recent drug use (any) | 4.36 (68) | 6.22 (14) | 4.08 (46) |
| Sexually transmitted infections | 8.73 (103) | 11.56 (23) | 8.31 (80) |
| HIV | .06 (3) | 0 | .07 (3) |
| Structural factors | |||
| Poverty | 20.15 (229) | 28.53 (35) | 18.89 (194) |
| Homeless | 16.45 (181) | 14.22 (23) | 16.78 (158) |
| Access to health care | 16.96 (248) | 27.54 (68)** | 15.37 (180)** |
| Criminal justice | |||
| Incarcerated | 3.90 (107) | 6.48 (18) | 3.50 (89) |
| Arrested by migration police | 15.88 (321) | 22.20 (50) | 14.80 (271) |
| Questioned by migration police | 18.18 (279) | 26.58 (60)* | 16.92 (219)* |
| Questioned by market police | 13.60 (226) | 18.89 (48) | 12.81 (178) |
| Mobility | |||
| Travel in past 90 days | 33.75 (87) | 38.58 (89) | 32.64 (386) |
| Migration Status | |||
| Non-migrant | 52.67 (562) | 52.98 (72) | 52.62 (490) |
| Internal migrant | 26.27 (278) | 17.78 (37) | 27.54 (241) |
| External migrant | 21.06 (502) | 29.23 (75)* | 19.83 (427)* |
| Kyrgz | 4.62 (79) | 5.15 (68)** | 1.50 (11)** |
| Tajik | 2.13 (203) | .76 (8) | 2.37 (195) |
| Ukzbek | 14.31 (220) | 26.35 (56)*** | 12.50 (164)*** |
| Sociodemographic characteristics | |||
| Age | 27.01 (.78) | 28.33 (.77)*** | 24.72 (.29)*** |
| Married/common law marriage | 37.08 (587) | 48.14 (99)* | 35.42 (488)* |
| Spouse/girlfriend live together | 24.89 (358) | 32.09 (66) | 23.67 (292) |
| Have child(ren) | 28.90 (461) | 42.15 (88)** | 26.91 (373)** |
| Less than high school (missing 67 cases) | 75.98 (925) | 78.51 (136) | 75.60 (789) |
| Work at Baraklholka Market | 61.66 (880) | 52.63 (93) | 63.02 (787) |
| As an owner | 4.72 (144) | 4.62 (13) | 4.73 (131) |
| As a vendor or sell goods | 30.81 (537) | 24.70 (51) | 31.73 (486) |
| As a carrier | 23.91 (258) | 19.87 (35) | 23.52 (223) |
< .05;
< .01;
< .001
Results
Descriptive Statistics
Table 1 provides descriptive statistics and bivariate tests of differences stratified by hazardous alcohol drinking patterns. The average age of participants who reported hazardous alcohol use (28.33 years vs. 24.72; p < .001) were older than their counterparts. A greater proportion of participants with hazardous drinking behaviors were married (48.14%, 99 vs. 35.42%, 488; p = .025) and had children (42.15%, 88 vs. 26.91%, 373; p = .004).
Biologically Confirmed Cases of HIV and STI
Only 3 cases of HIV were identified (.06%) and none were reported among people with hazardous alcohol consumption patterns. Overall 8.73% (103) of the sample tested positive for any STI and 11.53(23) % in the hazardous alcohol consumption category.
Mobility and Migration Status
A greater proportion of participants who reported hazardous drinking behavior were external migrants (29.23%, 75 vs. 19.83%, 427, p = .023) specifically from Tajikistan (5.15%, 68 vs. 1.50, 11) and Uzbekistan (26.35%, 56 vs. 12.50%, 164). Overall, more than a third of participants who reported hazardous drinking reported traveling outside of Almaty in the past 90 days (38.58%, 89).
Risk Environment Characteristics
A greater proportion of participants with hazardous drinking consumption patterns needed to see a doctor but did not go compared to participants without hazardous drinking (27.54%, 68 vs. 15.37% 180, p = .003). A significantly greater proportion of participants with hazardous alcohol use were questioned by the migration police (26.58%, 60 vs. 16.92%, 219, p < .015).
Exposure Variable
Overall, 13.07% (184) scored an 8 or greater on the AUDIT meeting the criteria for a pattern of hazardous drinking behaviors.
Outcome Variables
Sexual Risk Behaviors
Of the total sample, 8.53% (119) traded money, drugs or other goods for sex, 28.89% (441) had unprotected sex with any partner, 28.81% (355) multiple sexual partners, and 10.03%(167), sex under the influence of drugs and/or alcohol. Compared to their counterparts, a significantly greater proportion of participants with hazardous drinking consumption reported trading money or goods for commercial sex (15.96%, 33 vs. 7.41%, 86; p = .030). Sex under the influence of drugs or alcohol were significantly more common among participants who reported hazardous alcohol drinking patterns (28.92%, 72 vs. 6.81%, 95; p < .001).
Multivariate findings testing the main hypothesis on the relationship between risky sexual behaviors and hazardous drinking controlling for confounders.
Table 2 presents multivariate weighted logistic regressions of associations between alcohol use and sexual risk after adjusting for socio-demographic and structural risk characteristics, mobility and migration status. The adjusted odds ratio (aOR) of sex under the influence of drugs or alcohol for participants who engaged in hazardous drinking was 6.09 (aOR) times the odds (95% CI 3.48, 10.65, p < .001) of participants who did not engage in hazardous drinking. Hazardous drinking was also associated with increased odds of engaging in commercial sex after adjusting for potential confounders (aOR = 2.02 95% CI 1.02, 4.02, p = .023).
Table 2.
Multivariate weighted logistic regressions of associations between alcohol use and sexual risk showing adjusted odds ratios (aOR)
| Sex under influence of drugs aOR (95% CI) |
Commercial sex aOR (95% CI) |
Unprotected sex aOR (95% CI) |
More than one sexual partner aOR (95% CI) |
|
|---|---|---|---|---|
| Drug and alcohol use | ||||
| Hazardous alcohol use | 6.09*** (3.48, 10.65) | 2.02* (1.02, 4.02) | 1.60 (.98, 2.62) | 1.27 (.76,2.12) |
| Drug use | 1.77 (.84, 3.70) | 1.80 (.75, 4.30) | 1.40 (.76, 2.60) | 1.67 (.90, 3.07) |
| Structural factors | ||||
| Below poverty line | 1.45 (.68, 3.02) | .91 (.44, 1.92) | .91 (.55, 1.48) | 1.20 (.75, 1.92) |
| Homelessness | .63 (.20, 2.03) | 1.20 (.46, 2.95) | .49* (.26, .91) | .40** (.22, .72) |
| Access to health care | 1.87* (1.08, 3.23) | .82 (.36, 1.89) | 2.30*** (1.44, 3.70) | 1.22 (.72, 2.08) |
| Legal involvement | ||||
| Incarcerated | 1.59 (.70, 3.59) | 1.68 (.62, 4.54) | .78 (.36, 1.68) | 1.65 (.66, 4.14) |
| Migration police | 1.71 (.71, 4.10) | 2.13 (.75, 6.07) | .72 (.33, 1.57) | 1.08 (.41, 2.85) |
| Market police | .48 (.17, 1.36) | .37 (.12, 1.19) | 1.43 (.60, 3.40) | .62 (.21, 1.80) |
| Mobility and migration | ||||
| Mobility | 1.12 (.62, 2.02) | 2.48** (1.30, 4.73) | 1.32 (.88, 1.99) | 2.09** (1.39, 3.14) |
| External migrant | 1.26 (.67, 2.34) | 1.30 (.68, 2.43) | 1.25 (.83, 1.88) | .55 (.36, .86) |
< .05;
< .01;
< .01
Discussion
This study is one of the first to examine the relationship between alcohol misuse and sexual risk behaviors among male market laborers from Central Asia that includes both external and internal migrants as well as non-migrants. Overall, 13.07% of the sample met the criteria for a pattern of hazardous drinking behaviors. These findings are consistent with the prevalence rate of alcohol problems for the Kazakhstani population (15%) as reported by WHO [60]. The WHO and other literature has indicated that male episodic heavy drinking patterns in Kazakhstan are among the highest in the world [61, 62].
The findings also show that the greatest number of participants who reported hazardous drinking were external migrants specifically from Tajikistan and Uzbekistan, compared to internal migrants (Kazakhs) and non-migrant (Kazakhs). This finding is somewhat surprising, given that both Uzbeks and Tajiks come from more traditional Muslim countries where, under Islam, alcohol use goes against religious values [61]. Poor working conditions at the marketplace and specific migration characteristics such as mobility might foster a social environment conducive to developing alcohol use problems. Market vendors often conduct their work in an open space in the marketplace and work long hours in cold and inclement weather in winter [10]. These stark conditions may encourage the use of alcohol. In our in-depth interviews in the marketplace, participants reported demanding and stressful working conditions, which may lead some men to use alcohol to cope with the stress [9, 63]. In this study, we also found that those who traveled outside of Almaty in the past 90 days, compared to their counterparts, tended to have a higher prevalence of hazardous alcohol consumption. In the current study, the bivariate analysis found that a significantly greater proportion of participants with hazardous alcohol consumption compared to their counterparts were questioned by the migration police and market officials. This link may be related to misuse of alcohol as a coping mechanism by the market vendors before facing what they construe as harassment by the border police and market officials [37]. This finding is of substantial importance because Tajik and Uzbek migrants may be a specific subpopulation that is at particular risk of sexual risk behaviors due to hazardous drinking behavior. Additional research is in order to identify if disparities in working and living conditions may explain elevated rates in rates of drinking in this population. Given that cultural and religious norms often explain low rates of drinking alcohol and sexual risk behaviors among Tajik and Uzbek migrants additional research is in order to explain if there are certain aspects of the migration process that differentially heighten risk for this subpopulation compared to other migrant populations.
As in other studies, the multivariate models found strong support for our main hypothesis showing that alcohol misuse increases sexual risk behaviors among male market vendors. We found that hazardous drinking was associated with engaging in commercial sex and sex under the influence of drugs and alcohol. This link has been repeatedly found in a number of studies among different samples of men in different parts of the world [21–31]. We did not find a significant relationship between having STIs or HIV and hazardous alcohol use. This may be because of the low prevalence of HIV (3 cases) and STIs (8.73%) in this population.
Globally Migrants are at higher risk of HIV by virtue of greater rates of sexual risk behaviors and use of drugs that are also associated with heightened risk of HIV. In Kazakhstan, limited research supports higher rates of alcohol and sexual risk among migrants. Contrary to prior research this study found low rates of HIV. Potential explanations for low rates of HIV pertain to reasons for mobility for external migrants compared to internal and non-migrants provided in prior literature. As reported in prior literature external migrants most frequently return to sending countries to visit family and maintain social ties [10]. The protective effects of family members may diminish the occurrence of sexual risk behaviors of purchasing sex and multiple sex partners [10]. However while in the receiving country, external migrants may engage in much higher rates of alcohol use and purchasing of commercial sex to cope with challenges and hardship associated with prolonged time away from family. Qualitative research in Kazakhstan found that male external migrants were motivated to travel to earn a better income for remittance to families in sending countries. Factors associated with family ties in sending countries may be protective against HIV infection among external migrants despite the occurrence of sexual risk behaviors. The relationship between hazardous drinking and sex under the influence of drugs and purchasing sex are concerning particularly for a population that is marginalized and excluded from accessing health promotion and HIV prevention interventions.
Although rates of STI and HIV were low, the prevalence of sexual risk behaviors were high and provide a proxy indication of potential HIV risk in this population. Also, this study found that lack of access to care was associated with hazardous drinking behaviors. Given the large proportion of hazardous drinkers who were migrants from Tajikistan and Uzbekistan, it is possible that lack of knowledge of where to receive care for medical problems rather than lack of availability explains this relationship. Findings from this study call for future research that is more nuanced and differentiates between knowledge of services, barriers to health care, and availability of services to identify avenues of intervention with this population.
There are three major limitations to this study. First, the generalizability of study findings is limited to the Baraholka Market, which was the sole source of recruitment for the sample. Second, this paper utilizes cross-sectional data, which does not allow any causal interpretations of the findings. Finally, we assessed alcohol use only through self-reported measures. In addition to the three major limitations of this study, the dichotomized nature of the access to health care variable presents some limitations as a crude indicator because the variable does not differentiate between knowledge of services, access and barriers to receiving health care. Given the importance of access to health care for this population, these findings suggest future research with this population is necessary to measures more nuanced aspects of how migrant and non-migrant workers engage with health care services. Engaging workers in the marketplace with medical professionals when needed may provide an opportunity to address high rates of hazardous drinking and sexual risk behaviors.
Nonetheless, findings from this paper have important HIV and alcohol prevention implications and a potential to guide future research on the relationship between alcohol misuse and sexual risk behaviors among male market vendors in Central Asia, a key population at risk for HIV. To date, market laborers have no access to educational or prevention programs targeting the role that hazardous alcohol consumption plays in reducing inhibitions that may lead to risky sexual exposure to infectious diseases such as HIV, Hepatitis C (HCV) and B (HVB), and STIs or on how alcohol misuse leads to chronic debilitation and physical diseases. Both use of alcohol and sexual behaviors that put one at risk for HIV are taboo topics among Central Asian men, particularly among those actively engaged in commerce as these workers are in the largest international marketplace in Kazakhstan. Despite the scope of ostensibly hidden hazardous alcohol consumption in the region, this issue has not been addressed in the context of HIV prevention. Even if men in this marketplace recognize that their alcohol problems are treatable and desire to access help, they have no place to turn. Other than hospital admission for detoxification, there are no available prevention or treatment programs for alcohol misuse in Kazakhstan or throughout the Central Asian region. Moreover, most HIV prevention programs and policies aimed at key affected populations of mobile workers in Central Asia have largely focused on a curbing the threat of HIV or other infectious diseases posed by external migrants through mandatory HIV testing and referral of HIV positive migrants to their own countries for treatment. Obviously, this punitive approach often prevents labor migrants, who may fear deportation, from seeking medical care. Our findings underscore the urgent need for effective prevention strategies and policies to address widespread alcohol misuse issues facing over 15% of this mobile population
The findings from this research may help inform the design of programs and policies to more effectively target hazardous alcohol consumption and its consequences for this key mobile population affected by HIV. These programs must consider the characteristics, culture, and social vulnerabilities of this group. Men working in the marketplace and all migrants should have access to programs and information on the negative role of hazardous alcohol drinking on taking sexual risks that can result in HIV transmission and disease progression, and how alcohol misuse affects physical health long term and leads to increased disabilities over time.
Acknowledgments
Funding The study was funded by a grant from NIMH to Dr. El-Bassel. R01 NMH082684. Phillip L. Marotta received support from the National Institute on Drug Abuse Grant #: 1T32DA037801-01 PI: N. El-Bassel.
Footnotes
Compliance with Ethical Standards
Ethical Approval Research involved human participants and all procedures were approved by Columbia University Institutional Review Board.
Informed Consent Informed consent was obtained from all participants prior to participation in the study.
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.WHO. European status report on alcohol and health 2014. Copenhagen: WHO; 2014. [Google Scholar]
- 2.Boltaev AA, El-Bassel N, Deryabina AP, Terlikbaeva A, Gilbert L, Hunt T, Strathdee SA. Scaling up HIV prevention efforts targeting people who inject drugs in Central Asia: a review of key challenges and ways forward. Drug Alcohol Depend. 2013;132:S41–7. doi: 10.1016/j.drugalcdep.2013.07.033. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. 2015 [Google Scholar]
- 4.RAC. HIV Surveillance Update for Kazakhstan by Oblast and Risk Group. Unpublished Ministry of Health Statistics. Almaty, Kazakhstan: Republican AIDS Center (RAC), Ministry of Health; 2011. [Google Scholar]
- 5.UNAIDS. Global report: UNAIDS report on the global AIDS epidemic 2011. New York: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2012. [Google Scholar]
- 6.Abdala N, White E, Toussova OV, Krasnoselskikh TV, Verevochkin S, Kozlov AP, Heimer R. Comparing sexual risks and patterns of alcohol and drug use between injection drug users (IDUs) and non-IDUs who report sexual partnerships with IDUs in St Petersburg, Russia. BMC Public Health. 2010;10(1):676. doi: 10.1186/1471-2458-10-676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DeHovitz J, Uuskula A, El-Bassel N. The HIV epidemic in Eastern Europe and Central Asia. Curr HIV/AIDS Rep. 2014;11(2):168–76. doi: 10.1007/s11904-014-0202-3. [DOI] [PubMed] [Google Scholar]
- 8.WHO. Global alcohol report profiles. Kazakhstan: World Health Organization; 2014. [Google Scholar]
- 9.Mergenova G, Shaw SA, Terlikbayeva A, Gilbert L, Gensburg L, Primbetova S, El-Bassel N. Social support and HIV risks among migrant and non-migrant market workers in Almaty, Kazakhstan. J Immigr Minority Health. 2016:1–9. doi: 10.1007/s10903-016-0529-5. [DOI] [PubMed] [Google Scholar]
- 10.El-Bassel N, Gilbert L, Shaw SA, Mergenova G, Terlikbayeva A, Primbetova S, West B. The Silk Road Health Project: how mobility and migration status influence HIV risks among male migrant workers in Central Asia. PLoS ONE. 2016;11(3):e0151278. doi: 10.1371/journal.pone.0151278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pomerleau J, McKee M, Rose R, Haerpfer CW, Rotman D, Tumanov S. Hazardous alcohol drinking in the former Soviet Union: a cross-sectional study of eight countries. Alcohol Alcohol. 2008;43(3):351–9. doi: 10.1093/alcalc/agm167. [DOI] [PubMed] [Google Scholar]
- 12.Fritz K, Morojele N, Kalichman S. Alcohol: the forgotten drug in HIV/AIDS. Lancet. 2010;376(6739):398. doi: 10.1016/S0140-6736(10)60884-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, Wodak A, Panda S, Tyndall M, Toufik A, Mattick RP. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372:1733–45. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- 14.Arasteh K, Des Jarlais DC Group WHOPIDICS. Hazardous drinking and HIV sexual risk behaviors among injection drug users in developing and transitional countries. AIDS Behav. 2010;14(4):862–9. doi: 10.1007/s10461-008-9491-0. [DOI] [PubMed] [Google Scholar]
- 15.Baum MK, Rafie C, Lai S, Sales S, Page JB, Campa A. Alcohol use accelerates HIV disease progression. AIDS Res Hum Retroviruses. 2010;26(5):511–8. doi: 10.1089/aid.2009.0211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet. 2009;373(9682):2223–33. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 17.Baliunas D, Rehm J, Irving H, Shuper P. Alcohol consumption and risk of incident human immunodeficiency virus infection: a meta-analysis. Int J Public Health. 2010;55(3):159–66. doi: 10.1007/s00038-009-0095-x. [DOI] [PubMed] [Google Scholar]
- 18.Chander G, Lau B, Moore RD. Hazardous alcohol use: a risk factor for non-adherence and lack of suppression in HIV infection. J Acquir Immune Defic Syndr. 2006;43(4):411. doi: 10.1097/01.qai.0000243121.44659.a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Samet JH, Cheng DM, Libman H, Nunes DP, Alperen JK, Saitz R. Alcohol consumption and HIV disease progression. J Acquir Immune Defic Syndr. 2007;46(2):194. doi: 10.1097/QAI.0b013e318142aabb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conigliaro J, Gordon AJ, McGinnis KA, Rabeneck L, Justice AC. How harmful is hazardous alcohol use and abuse in HIV infection: do health care providers know who is at risk? J Acquir Immune Defic Syndr. 2003;33(4):521–5. doi: 10.1097/00126334-200308010-00014. [DOI] [PubMed] [Google Scholar]
- 21.Obel N, Omland LH, Kronborg G, Larsen CS, Pedersen G, Sørensen HT, Gerstoft J. Impact of non-HIV and HIV risk factors on survival in HIV-infected patients on HAART: a population-based nationwide cohort study. PLoS ONE. 2011;6(7):e22698. doi: 10.1371/journal.pone.0022698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li Q, Li X, Stanton B. Alcohol use and sexual risk behaviors and outcomes in China: a literature review. AIDS Behav. 2010;14(6):1227–36. doi: 10.1007/s10461-009-9648-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher JC, Cook PA, Kapiga SH. Alcohol use before sex and HIV risk: situational characteristics of protected and unprotected encounters among high-risk African women. Sex Transm Dis. 2010;37(9):571–8. doi: 10.1097/OLQ.0b013e3181dbafad. [DOI] [PubMed] [Google Scholar]
- 24.Carey KB, Senn TE, Walsh JL, Scott-Sheldon LA, Carey MP. Alcohol use predicts number of sexual partners for female but not male STI clinic patients. AIDS Behav. 2016;20(1):52–9. doi: 10.1007/s10461-015-1177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol use and sexual risks for HIV/AIDS in sub-Saharan Africa: systematic review of empirical findings. Prev Sci. 2007;8(2):141–51. doi: 10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- 26.Aicken CR, Nardone A, Mercer CH. Alcohol misuse, sexual risk behaviour and adverse sexual health outcomes: evidence from Britain’s national probability sexual behaviour surveys. J Public Health. 2010;33(2):262–71. doi: 10.1093/pubmed/fdq056. [DOI] [PubMed] [Google Scholar]
- 27.Arasteh K, Des Jarlais DC, Perlis TE. Alcohol and HIV sexual risk behaviors among injection drug users. Drug Alcohol Depend. 2008;95(1):54–61. doi: 10.1016/j.drugalcdep.2007.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Castilla J, Barrio G, Belza MJ, de la Fuente L. Drug and alcohol consumption and sexual risk behaviour among young adults: results from a national survey. Drug Alcohol Depend. 1999;56(1):47–53. doi: 10.1016/s0376-8716(99)00008-3. [DOI] [PubMed] [Google Scholar]
- 29.Fisher JC, Bang H, Kapiga SH. The association between HIV infection and alcohol use: a systematic review and meta-analysis of African studies. Sex Transm Dis. 2007;34(11):856–63. doi: 10.1097/OLQ.0b013e318067b4fd. [DOI] [PubMed] [Google Scholar]
- 30.Cho YH, Span SA. The effect of alcohol on sexual risk-taking among young men and women. Addict Behav. 2010;35(8):779–85. doi: 10.1016/j.addbeh.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 31.Rees V, Saitz R, Horton NJ, Samet J. Association of alcohol consumption with HIV sex-and drug-risk behaviors among drug users. J Subst Abuse Treat. 2001;21(3):129–34. doi: 10.1016/s0740-5472(01)00190-8. [DOI] [PubMed] [Google Scholar]
- 32.Amirkhanian YA, Kuznetsova AV, Kelly JA, DiFranceisco WJ, Musatov VB, Avsukevich NA, McAuliffe TL. Male labor migrants in Russia: HIV risk behavior levels, contextual factors, and prevention needs. J Immigr Minor Health. 2011;13(5):919–28. doi: 10.1007/s10903-010-9376-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weine S, Bahromov M, Loue S, Owens L. HIV sexual risk behaviors and multilevel determinants among male labor migrants from Tajikistan. J Immigr Minor Health. 2013;15(4):700–10. doi: 10.1007/s10903-012-9718-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weine SM, Kashuba AB. Labor migration and HIV risk: a systematic review of the literature. AIDS Behav. 2012;16(6):1605–21. doi: 10.1007/s10461-012-0183-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Worby PA, Organista KC. Alcohol use and problem drinking among male Mexican and Central American im/migrant laborers a review of the literature. Hispanic J Behav Sci. 2007;29(4):413–55. [Google Scholar]
- 36.Laruelle M. Central Asian Labor Migrants in Russia: the ‘Diasporization’of the Central Asian States? China Eurasia Forum Q. 2007;5(3):101–19. [Google Scholar]
- 37.Laruelle M. Kazakhstan, the new country of immigration for Central Asian workers. Central Asia-Caucasus Anal. 2008;10(9):6–8. [Google Scholar]
- 38.Thorne C, Ferencic N, Malyuta R, Mimica J, Niemiec T. Central Asia: hotspot in the worldwide HIV epidemic. Lancet Infect Dis. 2010;10(7):479–88. doi: 10.1016/S1473-3099(10)70118-3. [DOI] [PubMed] [Google Scholar]
- 39.Zhussupov B, McNutt LA, Gilbert L, Terlikbayeva A, El-Bassel N. Migrant workers in Kazakhstan: gender differences in HIV knowledge and sexual risk behaviors. AIDS Behav. 2015;19(7):1298–304. doi: 10.1007/s10461-014-0914-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.International Office of Migration IOM. 2006 [Google Scholar]
- 41.Marat E. Labor migration in Central Asia: Implications of the global economic crisis. Stockholm: Silk Road Studies Program, Institute for Security and Development Policy; 2009. [Google Scholar]
- 42.Azbel L, Wickersham JA, Grishaev Ymigra, Dvoryak S, Altice FL. Burden of infectious diseases, substance use disorders, and mental illness among Ukrainian prisoners transitioning to the community. PLoS ONE. 2013;8(3):e59643. doi: 10.1371/journal.pone.0059643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Altice FL, Azbel L, Stone J, Brooks-Pollock E, Smyrnov P, Dvoriak S, Stöver H. The perfect storm: incarceration and the high-risk environment perpetuating transmission of HIV, hepatitis C virus, and tuberculosis in Eastern Europe and Central Asia. The Lancet. 2016;388(10050):1228–48. doi: 10.1016/S0140-6736(16)30856-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rubenstein LS, Amon JJ, McLemore M, Eba P, Dolan K, Lines R, Beyrer C. HIV, prisoners, and human rights. The Lancet. 2016;388(10050):1202–14. doi: 10.1016/S0140-6736(16)30663-8. [DOI] [PubMed] [Google Scholar]
- 45.Vagenas P, Azbel L, Polonsky M, Kerimi N, Mamyrov M, Dvoryak S, Altice FL. A review of medical and substance use comorbidities in Central Asian prisons: implications for HIV prevention and treatment. Drug Alcohol Depend. 2013;132:S25–31. doi: 10.1016/j.drugalcdep.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kutsa O, Marcus R, Bojko MJ, Zelenev A, Mazhnaya A, Dvoriak S, Altice FL. Factors associated with physical and sexual violence by police among people who inject drugs in Ukraine: implications for retention on opioid agonist therapy. J Int AIDS Soc. 2016;19:20897. doi: 10.7448/IAS.19.4.20897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rhodes T. The ‘risk environment’: a framework for understanding and reducing drug-related harm. Int J drug Policy. 2002;13(2):85–94. [Google Scholar]
- 48.Strathdee SA, Hallett TB, Bobrova N, Rhodes T, Booth R, Abdool R, Hankins CA. HIV and risk environment for injecting drug users: the past, present, and future. The Lancet. 2010;376(9737):268–84. doi: 10.1016/S0140-6736(10)60743-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.El-Bassel N, Gilbert L, Terlikbayeva A, Beyrer C, Wu E, Shaw SA, Primbetova S. HIV risks among injecting and non-injecting female partners of men who inject drugs in Almaty, Kazakhstan: implications for HIV prevention, research, and policy. Int J drug Policy. 2014;25(6):1195–203. doi: 10.1016/j.drugpo.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huffman SA, Veen J, Hennink MM, McFarland DA. Exploitation, vulnerability to tuberculosis and access to treatment among Uzbek labor migrants in Kazakhstan. Soc Sci Med. 2012;74(6):864–72. doi: 10.1016/j.socscimed.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 51.Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Soc Probl. 1997;44(2):174–99. [Google Scholar]
- 52.Heckathorn DD. Extensions of respondent-driven sampling: analyzing continuous variables and controlling for differential recruitment. Sociol Methodol. 2007;37(1):151–207. [Google Scholar]
- 53.Saunders JB, Aasland OG, Babor TF, De la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 54.Schuckit MA. Alcohol-use disorders. The Lancet. 2009;373(9662):492–501. doi: 10.1016/S0140-6736(09)60009-X. [DOI] [PubMed] [Google Scholar]
- 55.Statistics MoNEotRoKCo. 2014 [Google Scholar]
- 56.STATA Corporation, 2016 STATA v14 [Google Scholar]
- 57.Rao JN, Scott AJ. The analysis of categorical data from complex sample surveys: Chi squared tests for goodness of fit and independence in two-way tables. J Am Stat Assoc. 1981;76(374):221–30. [Google Scholar]
- 58.Archer KJ, Lemeshow S. Goodness-of-fit test for a logistic regression model fitted using survey sample data. Stata Journal. 2006;6(1):97–105. [Google Scholar]
- 59.Lemeshow S, Sturdivant RX, Hosmer DW. Applied logistic regression (Wiley Series in probability and statistics) New York: Wiley; 2013. [Google Scholar]
- 60.World Health Organization. Global status report on alcohol and health 2014. Geneva: World Health Organization; 2014. [Google Scholar]
- 61.Rasanayagam J. Islam in post-Soviet Uzbekistan: the morality of experience. Cambridge: Cambridge University Press; 2010. [Google Scholar]
- 62.Pomerleau J, McKee M, Rose R, Haerpfer CW, Rotman D, Tumanov S. Hazardous alcohol drinking in the former Soviet Union: a cross-sectional study of eight countries. Alcohol Alcohol. 2008;43(3):351–9. doi: 10.1093/alcalc/agm167. [DOI] [PubMed] [Google Scholar]
- 63.Shaw SA, El-Bassel N, Gilbert L, Terlikbayeva A, Hunt T, Primbetova S, Chang M. Depression among people who inject drugs and their intimate partners in Kazakhstan. Community Ment Health J. 2016;52(8):1047–56. doi: 10.1007/s10597-015-9883-3. [DOI] [PMC free article] [PubMed] [Google Scholar]