Abstract
We describe a case illustrating a new technique of using intraoperative optical coherence tomography (IOCT) for foreign body removal from the limbus and cornea. In this case, fragments of a fish hook in the temporal limbus and cornea were identified on the OCT. The residual pieces were then removed, assisted by high-resolution, real-time cross-sectional imaging, IOCT. While this technique involves steep learning curve, we believe that it is safe for the patient and helps surgeon with instant decision making and reduce orbital manipulation.
Keywords: Cornea, Foreign body, Fish hook, Intraoperative OCT
Case report
A 20-year-old male with a history of open globe injury with a fish hook presented as a referral to the cornea clinic. The open globe was repaired and the bulk of the fish hook had been removed two months before the presentation. However, follow-up CT scan showed a retained residual metallic foreign body.
At the cornea clinic the patient denied ocular pain and recent vision change but complained of inability to wear his contact lens. Uncorrected visual acuity (UCVA) in the left eye was 20/200; IOP was unavailable. He had no ocular motility limitations or afferent pupillary defects. Slit lamp exam showed healed and epithelialized corneal laceration with posterior scar extending to anterior cornea along inferior pupillary margin with 1 × 1 mm microcystic edema overlying the corneal scar. No infiltrate or signs of infection noted. Gonioscopy was normal with intact trabecular meshwork.
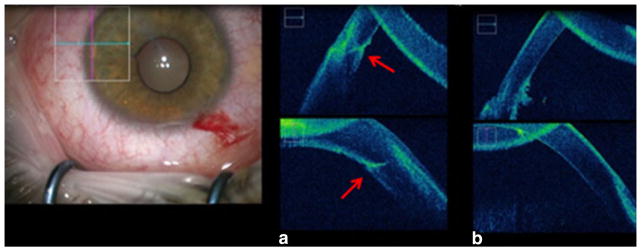
Anterior segment OCT (Fig. 1) and ultrasound revealed that the foreign body was captured anterior to the lens, in the posterior stroma with intrusion into the anterior chamber from the angle near the temporal limbus of the left eye.
Fig. 1.
Anterior segment optical coherence tomography (OCT) image of the affected cornea. The red arrow is pointing at the foreign body in the temporal limbus of the left eye
Surgical technique
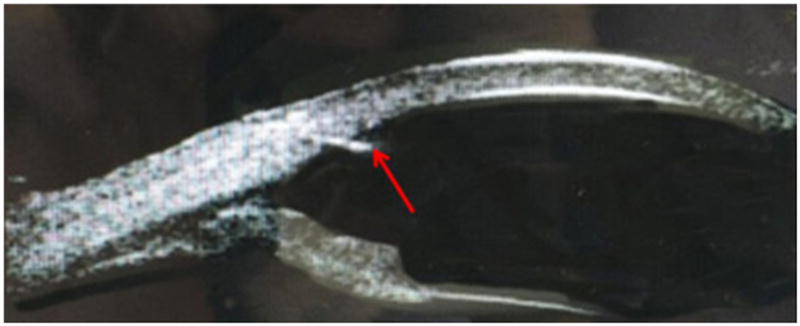
After informed consent, the left eye was prepped and draped in standard sterile fashion for ophthalmic surgery. The procedure was performed under retrobulbar block. A stab wound was created at 10:30 and 1 % Lidocaine was instilled in the anterior chamber. The anterior chamber was filled with viscoelastic. A light pipe was held at the temporal limbus outside of the eye to illuminate the small metallic foreign body using scleral scatter. This foreign body was located in Descemet’s membrane about 1 mm from the angle at 3 o’clock using IOCT. A second stab wound was created at 9 o’clock. Microsurgical technology (MST) 23-gauge microforceps, 25gauge MaxGrip microforceps (Alcon-Grieshaber), and 25gauge (Inner limiting membrane) ILM forceps (Alcon-Grieshaber) were all used to remove the foreign body. The initial piece of the foreign body came out cleanly and was <1 × <1 mm. The second piece of the foreign body came out in small pieces. Intraoperative OCT was used to ensure that there was no remaining foreign body, additionally the transilluminator revealed no remaining refractile bodies. The area was inspected carefully for other residual foreign body particles (Fig. 2). A third stab wound was created at about 1:30; bimanual irrigation aspiration was used to remove all of the viscoelastic. Miostat was placed in the eye. The wounds were hydrated and found to be water tight. Antibiotic and steroid drops were placed in the eye. The patient was transported to the PACU in stable condition.
Fig. 2.
Intraoperative photograph from the operating microscope (surgeon’s view). The OCT images (a, b) correspond to the cornea and limbus focused in the rectangular box shown. a Intraoperative OCT image of the affected cornea before the surgical removal of the foreign body. Horizontal cross-sectional image (top) and vertical cross-sectional image (bottom) with the red arrows pointing at the foreign body. b Intraoperative OCT image of the affected cornea confirming the complete removal of the foreign body from the temporal limbus. Horizontal cross-sectional image (top) and vertical cross-sectional image (bottom)
Outcome
One week after the surgery, patient was seen by a local ophthalmologist. As per the report, the patient was symptom free with no signs of infection. Visual acuity improved to 20/20 with contact lens and intraocular pressure was normal. Good functional improvement with uncomplicated recovery and absence of clinical signs made the requirement of postoperative Anterior segment OCT less important. Patient refused follow-up CT scan due to scheduling conflicts with college and for financial reasons. A three-week phone call to patient’s mother revealed that the patient is doing fine and headed to college.
Discussion
The surgical management of foreign body removal is challenging as it varies according to the location, depth, and relation to other ocular structures. It is imperative to prevent further structural damage of the ocular tissues which may lead to functional damage in future. Nonetheless, penetrating ocular fish hook injuries with prompt attention and appropriate surgical intervention results in excellent long-term prognosis [1].
Fish hook injuries commonly exist as anterior segment damage [1–3]. In the present case, the status of anterior segment at the time of injury was unclear as patient was presented as a referral to the cornea clinic two months after trauma. The residual fish hook as shown on preoperative CT scan was removed safely from the temporal limbus using a new technique with the assistance of IOCT.
Intraoperative OCT is gaining popularity in the treatment of retinal diseases and for cataract removal with microincision technique and Femtosecond laser-assisted extraction [4, 5]. However, the literature is lacking with regard to foreign body removal from ocular tissues using intraoperative imaging. Literature on fish hook injuries is limited to case reports and a case series by Aiello et al. In the series, authors reported four different techniques for surgical management of these injuries [1]. In our case, a modified surgical technique different from those reported was used because the presentation of the patient was unusual, with metal fragments remaining in the limbus and the cornea after bulk removal of the fish hook.
A surgical approach was planned to remove the metal fragments using IOCT, light pipe, MST, MaxGrip forceps, and ILM forceps preventing further damage to the nearby ocular tissues. The first wound was created for paracentesis and viscoelastic injection. The second stab wound at 9 o’clock was performed for easy access of the FB and simultaneous visualization on the OCT. The purpose of the light pipe was to create scleral scatter from the metal to aid with surgical maneuvers. The ILM and max grip forceps were used for gentle removal of the FB. The third stab wound was created for irrigation aspiration and removal of viscoelastic. At the end, patient received moxifloxacin 0.5 % eye drops to prevent infection. Fish hooks are usually made out of high carbon steel or stainless steel to protect them from corrosion, hence broad spectrum antibiotics were not considered necessary posto peratively.
Craig et al. reported removal of intraocular foreign body (IOFB) from anterior segment via limbal incision and foreign body forceps and/or scratch-down sclerotomy [6]. Previous studies narrated techniques transitioning from use of rare-earth magnets to pars plana vitrectomy for penetrating IOFB removal from the posterior segment [7]. Manjunatha et al. highlighted the aid of Gonioscopy under operating microscope for anterior segment FB removal which would have been less expensive in our patient [8]. The FB in this case is also in the anterior segment but the visualization was challenging with Gonio lens as the object was present as unusually small residual fragments. Hence, different approach with different equipment was tried for efficient removal. Intraoperative OCT provided the surgeon with real-time cross-sectional imaging of the structural anatomy which helped with flexibility in intraoperative management from the incision to the wound closure.
The current approach achieved good anatomical and functional results with no intraoperative and postoperative complications. The present technique may be considered as a safe, reliable, and new approach for the removal of small ocular penetrating foreign bodies.
Acknowledgments
This work was supported in part by an Unrestricted Grant from Research to Prevent Blindness, Inc., New York, NY, to the Department of Ophthalmology and Visual Sciences, University of Utah.
Footnotes
Compliance with ethical standards
Conflict of interest This report has no potential financial conflicts of interest.
Contributor Information
Sailaja Bondalapati, John A. Moran Eye Center, University of Utah, 647 S, 1200 E, Salt Lake City, UT 84102, USA.
Bala Ambati, John A. Moran Eye Center, University of Utah, 65 Mario Capecchi Dr, Salt Lake City, UT 84132, USA.
References
- 1.Aiello LP, Iwamoto M, Guyer DR. Penetrating ocular fish-hook injuries. surgical management and long-term visual outcome. Ophthalmology. 1992;99(6):862–866. doi: 10.1016/s0161-6420(92)31881-0. [DOI] [PubMed] [Google Scholar]
- 2.Agrawal R, Laude A, Taneja M. Fish-hook injury of the eye. Int Ophthalmol. 2012;32(3):269–271. doi: 10.1007/s10792-012-9551-3. [DOI] [PubMed] [Google Scholar]
- 3.Iannetti L, Tortorella P. Penetrating fish-hook ocular injury: management of an unusual intraocular foreign body. Case Rep Med. 2014;2014:901285. doi: 10.1155/2014/901285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Das S, Kummelil MK, Kharbanda V, et al. Microscope integrated intraoperative spectral domain optical coherence tomography for cataract surgery: Uses and applications. Curr Eye Res. 2015;45:1–10. doi: 10.3109/02713683.2015.1050742. [DOI] [PubMed] [Google Scholar]
- 5.Jayadev C, Dabir S, Vinekar A, Shah U, Vaid T, Yadav NK. Microscope-integrated optical coherence tomography: a new surgical tool in vitreoretinal surgery. Indian J Ophthalmol. 2015;63(5):399–403. doi: 10.4103/0301-4738.159865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greven CM, Engelbrecht NE, Slusher MM, Nagy SS. Intraocular foreign bodies: management, prognostic factors, and visual outcomes. Ophthalmology. 2000;107(3):608–612. doi: 10.1016/s0161-6420(99)00134-7. [DOI] [PubMed] [Google Scholar]
- 7.Mester V, Kuhn F. Ferrous intraocular foreign bodies retained in the posterior segment: management options and results. Int Ophthalmol. 1998;22(6):355–362. doi: 10.1023/a:1006487313380. [DOI] [PubMed] [Google Scholar]
- 8.Manjunatha NP, Deshmukh RR, Kayarkar VV. Large metallic fragment found in the angle of anterior chamber after phacoemulsification, and its removal. Eye. 2007;21:295–296. doi: 10.1038/sj.eye.6702549. [DOI] [PubMed] [Google Scholar]