Abstract
Purpose:
To report endoscope-assisted fascia lata harvest (EAFH) as a minimally-invasive technique for correction of severe blepharoptosis.
Methods:
This was a retrospective case series between January 2013 and April 2017. Medical records of all consecutive patients who underwent frontalis suspension by EAFH in the study period were reviewed and outcome was analyzed.
Results:
Fourteen patients (10 males) were included in the study. Mean age of the group was 18.14 + 17.03 years (range 4-65 years) and 11 patients had simple congenital blepharoptosis. Blepharophimosis syndrome was seen in 3 patients. Eleven patients had bilateral blepharoptosis. The mean preoperative and postoperative MRD1 was –1.60 ± 0.87 mm and +2.12 ± 1.37 mm respectively. Mean lengths of the incision and fascial harvest were 2.25 ± 0.43 cm and 13.0 ± 2.35 cm (range 10-17 cm) respectively. The median follow-up of patients was 4.57 + 4.03 months (range 1-15 months). Complications included a wound dehiscence in two patients and these were resutured. The donor sites healed well in all patients leaving a small thigh scar and none needed scar revision.
Conclusion:
EAFH is a promising minimally-invasive technique performed with a small incision and achieved adequate length of fascial harvest.
Keywords: Autogenous fascia lata, frontalis suspension, minimally invasive
Frontalis suspension is the preferred surgical technique for correction of blepharoptosis with poor levator function.[1] In simple terms, frontalis suspension establishes a link between the frontalis muscle and the tarsus of the eyelid, thus correcting the eyelid position in primary gaze.[2] A variety of materials find mention in the literature - chromic gut, collagen, polypropylene, silicone, silk, nylon monofilament, polyester, polytetrafluoroethylene, and fascia lata (autogenous or banked) as effective choices of suspension material.[2] Even today, autogenous fascia lata remains the material of choice to a large section of ophthalmologists and many of them prefer the Crawford fasciotome (stripper) that allows retrieval of autogenous fascia lata through a small skin incision.[2]
Several authors have described innovative minimally invasive harvesting techniques exemplified by the kite-tail fascia lata strip technique by Evereklioglu and twin small-incision techniques by Kashkouli, Tay et al., and Bhatti et al.[3,4,5,6] A rigid endoscope-assisted fascial harvest technique was first described by Tucker et al. for repair of recurrent ventral hernia and later by Malhotra et al. for periocular surgery in three patients.[7,8] The purpose of our study was to revisit the minimally-invasive technique of endoscope-assisted fascia lata harvest (EAFH) and compare it with the other minimally invasive techniques for harvesting fascia lata.
Methods
This retrospective, interventional study was conducted at a tertiary care center in India between January 2013 and April 2017, and all surgeries were performed by experienced oculoplastic surgeons. The study was carried out in accordance with the ethical guidelines of the Declaration of Helsinki and Institutional Review Board approval was obtained. All patients underwent frontalis suspension for severe blepharoptosis with poor levator function (<4 mm). Data retrieved included demographic details, etiology of blepharoptosis, prior surgical interventions, length of the skin incision(s) and fascia lata harvested, outcome at final follow-up, and donor site complications.
Surgical technique: Endoscope-assisted fascia lata harvest
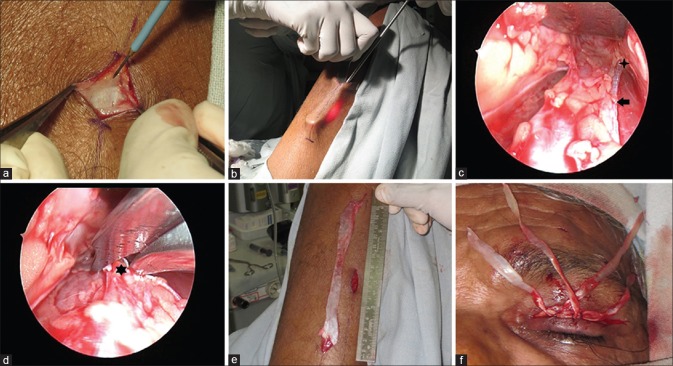
Under aseptic conditions, the face and donor site (lower thigh region) were prepared. Positioning of the leg was done with 30° knee flexion and a single 2 cm longitudinal incision was marked on the lower thigh at the junction of upper two-thirds and lower third on the imaginary line (Langer's) joining the fibular head with the anterior superior iliac spine. Care was taken to keep the incision 5 cm away from the knee and the targeted 15 cm of fascia lata was correspondingly marked over the skin. The incision was placed at the central 2 cm of 15 cm mark with a 15 no. Bard-Parker blade and subcutaneous tissue was separated. Further dissection through the fat and Scarpa's fascia helped in delineating the glistening avascular white fascia lata [Fig. 1a]. Depending on the width of fascia required, two parallel longitudinal incisions about 1 cm in length, 5 or 10 mm apart (depending on whether the surgery was for single or both eyes) were made using 11 no. blade under direct visualization on the glistening fascia. Under visualization of a rigid 4 mm, 0° or 30° endoscope, the subcutaneous and subfascial planes were dissected with the help of a curved Steven's scissors while an assistant used a malleable retractor to elevate tissues anterior to the fascia lata. The fascia was then cut longitudinally extending the 1 cm initial incisions on the fascia on either side. The illumination of the endoscope could be seen through the intact skin as a transcutaneous glow [Fig. 1b]. The incised longitudinal margins of the fascia were clearly visualized [Fig. 1c] with the endoscope. When the transcutaneous glow of the endoscope corresponded to the superior and inferior markings made on the skin, a curved nasal scissors (Rhinoforce II Nasal Scissors, Karl Storz) was used to make the horizontal incisions [Fig. 1d and e] to harvest fascia measuring 5–10 mm in width and 12–15 cm in length. The fascial defect was left open and harvested fascia was divided into 2 mm wide strips and placed in normal saline. The thigh wound was closed in layers with 5-0 polyglactin for subcutaneous tissue and 4-0 silk for skin.
Figure 1.
(a) Clinical photograph shows the skin incision measuring 2 cm and the glistening white band of fascia lata. The fibers of the fascia have a parallel arrangement and are aligned to the long axis of the thigh. (b) Clinical photograph shows the nonsheathed 30° 4 mm rigid endoscope aided by a malleable retractor. The glow through intact skin shows the position of the tip of the telescope. (c) Endoscopic view shows the broad white band of the fascia inferiorly while the malleable retractor is placed superiorly. The incised margin of the white glistening fascia is shown as black arrow and extent of the incised fascia is shown with a four-point star. Also seen are goblets of fat adhering to the anterior fascial surface. (d) Endoscopic view shows that a curved nasal scissors is used to cut the distal end of the fascia lata shown by a black 6-point star. (e) Clinical photograph shows the longitudinally placed skin incision (2 cm) and fascia lata (14 cm) after harvest. (f) Clinical photograph shows the 2 mm strips of fascia lata are fixed to the tarsal plate before they are tunneled to the preplaced forehead incisions
Frontalis suspension surgery
Forehead and eyelid incisions were marked either as a fox pentagon or a Crawford's double triangle. The eyelid crease incisions were made, and orbicularis was dissected to expose the anterior surface of the tarsus in upper eyelid. After making the forehead stab incisions, a Wright's needle was used to pass the fascia lata strips [Fig. 1f] and anchored to the tarsus with the help of 5/0 polyglactin sutures. The eyelid height and contour were adjusted before the forehead and eyelid incisions were closed. Frost sutures were taken and bandage contact lens was placed.
Standard postoperative medications and pressure stockings were prescribed in all patients. Planned follow-up visits included 2 and 6 weeks, 3, 6, and 12 months from the surgery. Primary outcome measures were the incision size at the donor site and length of fascia lata harvested. Secondary outcome measures include donor site complications and outcome of blepharoptosis correction.
Results
A total of 14 patients (25 eyes) underwent EAFH for blepharoptosis correction in the study period, of which 10 were male [Table 1]. Mean age of the group was 18.14 ± 17.03 years (range 4–65 years). Etiologically, 11 patients had simple congenital blepharoptosis and 3 had blepharophimosis syndrome. Most (n = 11) had bilateral blepharoptosis. The mean preoperative margin reflex distance-1 (MRD1) was − 1.60 ± 0.87 mm and postoperative MRD1 was + 2.12 ± 1.37 mm, and the difference was statistically significant (P < 0.0001, two-tailed t-test).
Table 1.
Demographics, etiology and outcome of Blepharoptosis after frontalis suspension with endoscope-assisted fascia lata harvest
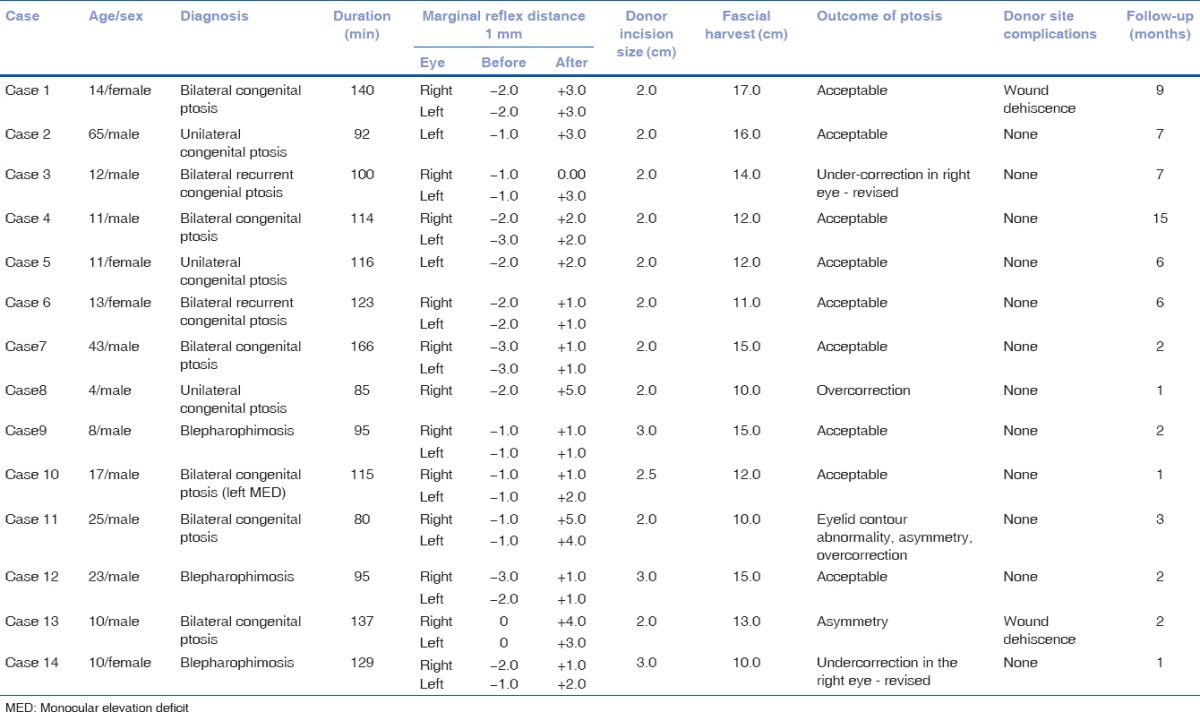
Mean size of the skin incision at donor site was 2.25 ± 0.43 cm and mean length of the harvested fascia lata was 13.0 ± 2.35 cm (range: 10–17 cm). The mean duration of the frontalis suspension surgery including harvesting fascia lata from donor site was 117.64 ± 24.79 min for 11 bilateral surgeries and 97.67 ± 16.26 min for remaining unilateral cases. The median follow-up of the EAFH group was 4.57 ± 4.03 months (range: 1–15 months). Donor site complications included wound dehiscence in two patients and these were sutured. All patients healed well with a small thigh scar and none needed scar revision.
Discussion
Frontalis suspension is the surgery of choice for correction of severe blepharoptosis with poor levator function.[1] Fascia lata is often the preferred sling material owing to its excellent biocompatibility and long-term outcomes.[1,2] Our experience with EAFH showed that it was a minimally invasive technique with small incision size and adequate fascial harvest, resulting in good outcome of blepharoptosis surgery. The visualization of the fascial tissues in EAFH improved surgical dissection with the added advantage in training as compared to the Crawford's stripper which is a blind procedure with unpredictable outcomes.
The “kite tail” technique described by Evereklioglu uses 5 cm × 1 cm fascial harvest which is then cut like a “Z” and sutured to give the final suspension material.[3] This technique is promising, especially in that it tends to leave large sections of the fascia intact which can then be used in recurrent blepharoptosis.[3]
Other innovative minimally invasive techniques [Table 2] have been described in the literature to harvest autogenous fascia lata without using a fasciotome.[4,5,6] Kashkouli, Tay et al., and Bhatti et al. have individually described twin-incision techniques where the proximal and distal incisions were placed at the lower third of the line joining the lateral condyle of tibia with anterior superior iliac spine. All of these techniques allow harvest of large sheets of fascia lata which are utilized in a variety of surgical specialties given the versatility of autogenous fascia lata graft.[4,5,6] The twin incisions leave two small scars on the lateral thigh.[4,5,6]
Table 2.
Minimally-Invasive techniques used to harvest autogenous fascia lata reported in literature
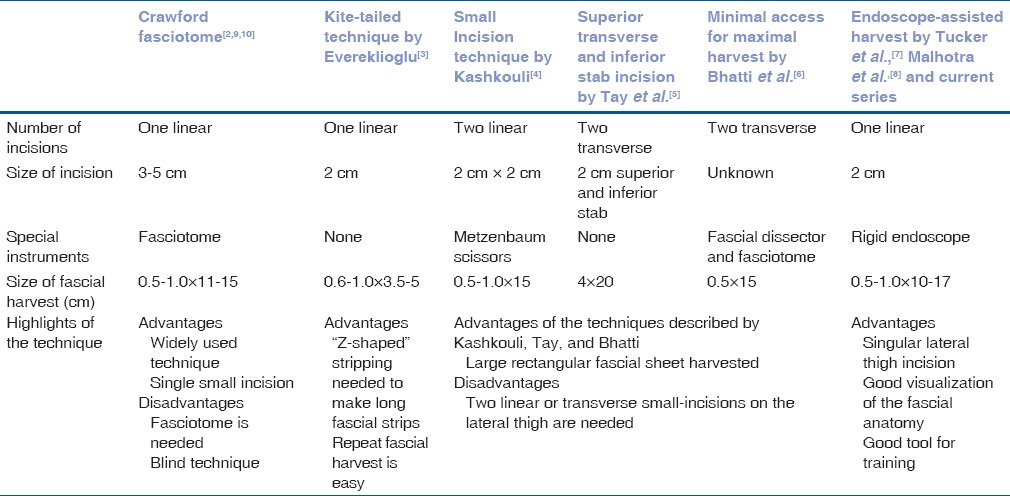
Use of a video endoscope to retrieve fascia lata for recurrent ventral hernia repair was first described by Tucker et al. in 1997.[7] Video endoscopically harvested fascia lata was applied in periocular region in three patients (2 blepharoptosis) by Malhotra et al. in 2007.[8] The authors used both low-thigh (one patient) and high-thigh (two patients) incisions to good effect with cosmetically acceptable outcome.[8] Malhotra et al. acknowledged that the time taken was twice as long as the traditional harvest.[8] This may be because the incision was placed at one end of the intended length of fascial dissection necessitating the endoscope to travel the entire length of the incision.[8] Our technique of placing the 2 cm incision at the center facilitated the surgery allowing dissection on either side and gave an optimal fascial harvest in all cases. Almost two decades after, it was first described EAFH appears to be a forgotten technique without a single report describing use in the periocular region in recent times. We performed EAFH at our institution as a minimally invasive technique for harvesting autogenous fascia lata in a select group of patients and found satisfactory outcomes. The mean length of the incision in our series was 2.25 cm and the mean length of the fascia harvested was 13.0 cm. All patients in our series underwent lower thigh incision for EAFH. While the high-thigh incision may be aesthetically superior, we preferred the lower thigh incision as it was easier to maneuver the telescope from the lower thigh incision. A Crawford's fasciotome, the preferred instrument used to harvest fascia lata, needs a 3–5 cm vertical incision and resulted in a mean scar size of 3.6 cm in thirty patients of congenital blepharoptosis.[2,9] EAFH scores over the Crawford fasciotome in its ability to allow clear visualization of the anatomy. This not only helps in harvesting a fascia of adequate size and width but also minimizes collateral damage to the underlying muscle and prevents hematoma and muscle hernia, improving precision of the length and width of fascia lata harvest.[9,10] In addition, EAFH technique can be demonstrated to trainees and helps in teaching.
We acknowledge that our study has limitations primarily arising from the retrospective design and small sample size. In addition, removal of autogenous fascia lata carries the risk of visible and/or palpable vastus lateralis muscle bulging as reported in half of pediatric cases.[9,10] However, we did not find the muscle bulge in our series of patients. EAFH increased the surgical time initially, but this improved over time. The authors believe that the limitations of EAFH are outweighed by the small incision, predictable fascial harvest, and minimal donor site morbidity.
Conclusion
EAFH offers promise as a minimally invasive technique with small incision, adequate fascial harvest, and esthetic outcome both in the correction of blepharoptosis and at the donor site. Further, EAFH is likely to be beneficial across specialties where autogenous fascia lata is the material of choice.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Beard C. Ptosis. 3rd ed. St Louis: Mosby; 1981. pp. 169–73. [Google Scholar]
- 2.Ben Simon GJ, Macedo AA, Schwartz RM, Wang DY, McCann JD, Goldberg RA. Frontalis suspension for upper eyelid ptosis: Evaluation of different surgical designs and material. Am J Ophthalmol. 2005;140:877–85. doi: 10.1016/j.ajo.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 3.Evereklioglu C. ‘Kite-tail’ fascia lata strips technique: Frontalis suspension using a non-endoscopic minimally invasive single-thigh incision approach. Br J Ophthalmol. 2012;96:570–5. doi: 10.1136/bjophthalmol-2011-300400. [DOI] [PubMed] [Google Scholar]
- 4.Kashkouli MB. A novel technique for small-incision fascia lata harvesting without a fasciatome for the frontalis suspension procedure. Orbit. 2007;26:203–6. doi: 10.1080/01676830701376122. [DOI] [PubMed] [Google Scholar]
- 5.Tay VS, Tan KS, Loh IC. Minimally invasive fascia lata harvest: A new method. Plast Reconstr Surg Glob Open. 2013 doi: 10.1097/GOX.0b013e31828c4406. pii: e7-e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhatti AF, Soueid A, Baden JM, Orlando A. Fascia lata harvesting: Minimal access for maximum harvest. A new technique. Plast Reconstr Surg. 2010;126:277e–8e. doi: 10.1097/PRS.0b013e3181ef82fa. [DOI] [PubMed] [Google Scholar]
- 7.Tucker JG, Choat D, Zubowicz VN. Videoscopically assisted fascia lata harvest for the correction of recurrent ventral hernia. South Med J. 1997;90:399–401. doi: 10.1097/00007611-199704000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Malhotra R, Selva D, Olver JM. Endoscopic harvesting of autogenous fascia lata. Ophthal Plast Reconstr Surg. 2007;23:372–5. doi: 10.1097/IOP.0b013e3181469cbd. [DOI] [PubMed] [Google Scholar]
- 9.Bleyen I, Hardy I, Codère F. Muscle prolapse after harvesting autogenous fascia lata used for frontalis suspension in children. Ophthal Plast Reconstr Surg. 2009;25:359–60. doi: 10.1097/IOP.0b013e3181b1e67a. [DOI] [PubMed] [Google Scholar]
- 10.Wheatcroft SM, Vardy SJ, Tyers AG. Complications of fascia lata harvesting for ptosis surgery. Br J Ophthalmol. 1997;81:581–3. doi: 10.1136/bjo.81.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]