Abstract
We report a case of anterior megalophthalmos and complicated cataract, with apparently smaller lens in both eyes. The right eye had spontaneous retinal detachment. The child underwent cataract surgery in both the eyes with retinal detachment surgery in the right eye. Due to small size of the lenticular bag, a downsized customized intraocular lens (IOL) was implanted. Postoperatively, the IOL was well centered with ambulatory vision till 3 years of follow-up. This case describes this rare disorder and its association with apparently small-sized lens and discusses the course of its management, highlighting the visual rehabilitation with customization of IOLs.
Keywords: Anterior megalophthalmos, apparently small lens, downsized intraocular lens
Vail[1] used the phrase “anterior megalophthalmos” for the first time to describe bilateral anterior segment enlargements not accompanied by increased intraocular pressure. It is a rare X-linked recessive condition[2] characterized by the presence of megalocornea (horizontal corneal diameter more than 13 mm) in association with enlarged lens iris diaphragm and ciliary ring.[3] Other associated features are central mosaic corneal dystrophy, iridodonesis, iris stromal hypoplasia, phacodonesis caused by zonular stretching, ciliary body dysplasia, ectopia lentis, cataract, posterior embryotoxon, excessive mesenchymal tissue in the angle, glaucoma (not congenital),[3,4,5] and vitreoretinopathy predisposing to retinal detachment.[6] The lens in anterior megalophthalmos is of normal size.[7,8] Our case presented with megalocornea, deep anterior chamber, hypoplasia of iris stroma, complicated cataract in both eyes, and spontaneous retinal detachment in the right eye fitting into the diagnosis of anterior megalophthalmos, and we describe its successful management.
Case Report
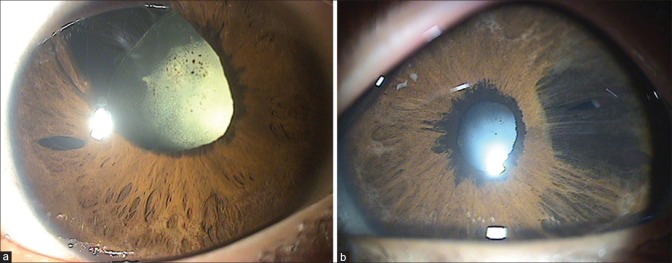
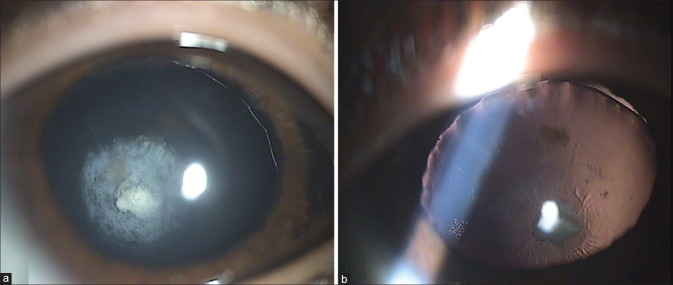
A 7-year-old male child, born out of consanguineous marriage, presented with poor vision in both eyes since birth. The vision was only light perception in the right eye and finger counting 3 m in the left eye. Anterior segment examination revealed megalocornea with horizontal diameter of 14.5 mm. The anterior chamber was deep in both eyes. Iris showed corectopia and iris atrophy in the right eye and ectropion uvea and iris hole in both the eyes [Fig. 1a and b]. Lens evaluation revealed posterior subcapsular with polar cataract in both eyes with crenated edges [Fig. 2a and b]. Lens overall diameter measured using the Zeiss eyepiece with graticule with a normal retina was 9 mm. Zonules were found to be intact. Intraocular pressure was normal in both the eyes. Optic nerve hypoplasia with a normal retina was noted in the left eye on fundus examination. There was a yellow hue to the right eye fundus, but no details were evident and B-scan examination revealed retinal detachment. Table 1 summarizes the clinical profile of the patient. He underwent surgery in the left eye first in view of the better prognosis in that eye and to allow early visual rehabilitation. Lens aspiration with a rigid customized posterior chamber intraocular lens (PCIOL) implantation through a scleral tunnel was planned. Since the crystalline lens was 9 mm, a downsized customized IOL was ordered. Lens diameter of 9 mm was confirmed intraoperatively. The biometric data of the patient are given in Table 1. A relatively small capsulorrhexis was made keeping in mind the smaller optic size and more chances of IOL subluxation from the bag in these cases. This was followed by hydrodelineation and aspiration of the cortical material using a bimanual technique. A posterior capsular plaque was noted at the center. Attempt was made to peel it off but in vain. However, in view of the spontaneous retinal detachment in the other eye and enlarged axial length in the left eye, primary posterior capsulotomy was deferred and a decision was taken to do Nd: YAG capsulotomy after 6 months. A single-piece rigid poly methyl metha acrylate (PMMA) PCIOL of + 15.00 D power with overall 9 mm diameter and 5 mm optic size (Intra Ocular Care Pvt. Ltd., Care Group India, ISO 9001:2000) was implanted in the bag with minimal manipulation. PCIOL was well centered at the end of the procedure.
Figure 1.
Slit lamp image of the right eye (a) and left eye (b) with iris showing corectopia and iris atrophy in the right eye and ectropion uvea and iris hole in both eyes
Figure 2.
Slit lamp image of the left eye after dilatation with oblique illumination (a) and retroillumination (b) with lens showing posterior subcapsular with polar cataract with crenated edges
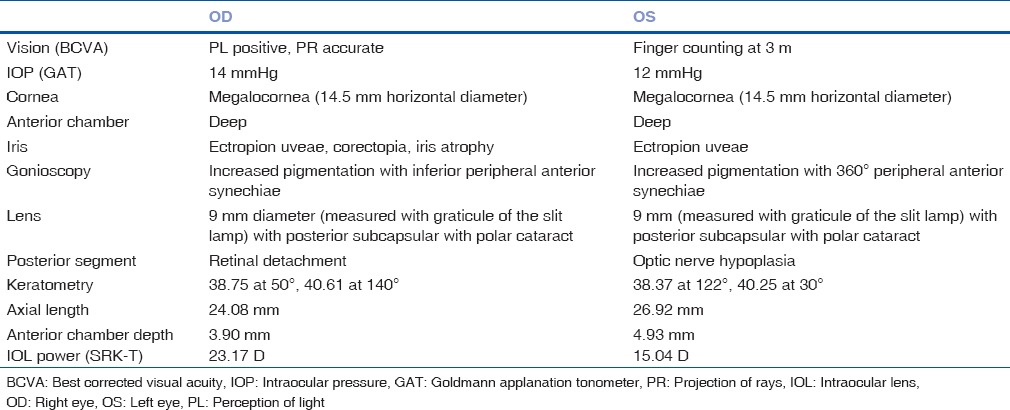
Table 1.
Clinical profile of the patient
In the immediate postoperative period, the best-corrected visual acuity was 20/125 in the left eye. The possibility of amblyopia in the left eye could not be ruled out in view of longstanding cataract of congenital origin and optic nerve hypoplasia. Eight months later, anterior capsular phimosis was noted again and Nd: YAG laser was used to release phimosis and perform a posterior capsulotomy for the preexisting posterior capsular opacification [Fig. 3a–c]. At the last follow-up, 3 years later, a trial of low vision was given and he improved from 20/125 to 20/40 with telescopic aid for distance and from N12 for near to N6 with stand magnifier.
Figure 3.
Slit lamp image of the left eye showing anterior capsular phimosis pre Nd: YAG laser (a) and postlaser treatment (b). Note that the Nd: YAG capsulotomy has been done for posterior capsular opacification (c) Retroillumination after Nd: YAG capsulotomy showing the opening in the posterior capsule
The right eye underwent lens aspiration with customized PCIOL implantation with pars plana vitrectomy, belt buckling, and silicone oil exchange 10 days after left eye cataract surgery under very guarded visual prognosis but with unfavorable outcome. The eye eventually underwent phthisical changes a year after the surgery.
Discussion
The lens in anterior megalophthalmos is of normal size,[7] but the ciliary ring is enlarged, which is responsible for weakened zonules and subluxation of lens needing customized IOLs of larger size. In our patient, as the capsular bag was small, we decided against implantation of a standard IOL that would have stretched the bag relaxing the zonules, leading to further subluxation of the lens. The lens with its crenated edges was clearly seen on slit lamp examination, and it was measured with a Zeiss eyepiece (×10) with measuring graticule at ×8 magnification. The size of the capsular bag was confirmed intraoperatively using a graded spatula and was found to be 9 mm. It was important to customize the IOL to place it in that capsular bag. The IOL power was calculated using SRK-T formula. Very few companies in India customize IOL and the lenses available are made of PMMA. Considering the safety profile of PMMA lenses,[9,10] customized PMMA IOLs of + 15.0 D were ordered with an overall diameter of 9 mm and optic size of 5 mm. Implantation of a rigid lens demands a larger incision as against a foldable IOL implantation, preferably a scleral tunnel that offers better wound integrity and less surgically induced astigmatism. Considering the small size of the lens in our case and increased chances of IOL decentration in cases of anterior megalophthalmos, an appropriate capsulorrhexis for the relatively small bag was made. IOL dislocation did not appear any time during the follow-ups.
Conclusion
This is the first case report of rare association of anterior megalophthalmos with apparently smaller sized lens. Although cataract surgery in a patient with megalophthalmos is a challenging one, this case highlights that good visual rehabilitation is possible with the help of customized downsized IOLs.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Vail DT. Adult hereditary anterior megalophthalmos sine glaucoma: A definite disease entity, with special reference to extraction of the cataract. Arch Ophthalmol. 1931;6:39–62. [Google Scholar]
- 2.Meire FM, Delleman JW. Biometry in X linked megalocornea: Pathognomonic findings. Br J Ophthalmol. 1994;78:781–5. doi: 10.1136/bjo.78.10.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duke-Elder S, editor . In: Congenital Deformities. Vol. 3. St Louis, MO: CV Mosby; 1964. Anomalies of the size of the cornea: Anterior megalophthalmos; pp. 498–505. [Google Scholar]
- 4.Kuchenbecker J, Behrens-Baumann W. Ciliary body dysplasia in megalophthalmos anterior diagnosed using ultrasound biomicroscopy. Eye (Lond) 2002;16:638–9. doi: 10.1038/sj.eye.6700156. [DOI] [PubMed] [Google Scholar]
- 5.Turaçli ME, Tekeli O. Anterior megalophthalmos with pigmentary glaucoma. Graefes Arch Clin Exp Ophthalmol. 2005;243:1066–8. doi: 10.1007/s00417-005-1157-2. [DOI] [PubMed] [Google Scholar]
- 6.Ahmadieh H, Banaee T, Javadi MA, Jafarinasab MR, Yazdani S, Sajjadi H, et al. Vitreoretinal disorders in anterior megalophthalmos. Jpn J Ophthalmol. 2006;50:515–23. doi: 10.1007/s10384-006-0370-9. [DOI] [PubMed] [Google Scholar]
- 7.Sharan S, Billson FA. Anterior megalophthalmos in a family with 3 female siblings. J Cataract Refract Surg. 2005;31:1433–6. doi: 10.1016/j.jcrs.2004.11.057. [DOI] [PubMed] [Google Scholar]
- 8.Hegde V, Jain R, Bappal A. Successful visual rehabilitation in a case of anterior megalophthalmos. Middle East Afr J Ophthalmol. 2012;19:413–5. doi: 10.4103/0974-9233.102763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panahi-Bazaz MR, Zamani M, Abazar B. Hydrophilic acrylic versus PMMA intraocular lens implantation in pediatric cataract surgery. J Ophthalmic Vis Res. 2009;4:201–7. [PMC free article] [PubMed] [Google Scholar]
- 10.Sukhija J, Ram J, Gupta N, Sawhney A, Kaur S. Long-term results after primary intraocular lens implantation in children operated less than 2 years of age for congenital cataract. Indian J Ophthalmol. 2014;62:1132–5. doi: 10.4103/0301-4738.149131. [DOI] [PMC free article] [PubMed] [Google Scholar]