Abstract
Ocular bee stings are known to cause corneal melts, corneal infiltrates, cataracts, and secondary glaucoma. Our patient presented with scleritis, corneal infiltrates, and endophthalmitis after a ocular bee sting. Topical treatment led to resolution of anterior segment inflammation, but the scleritis and vitreous inflammation worsened. Vitrectomy with intravitreal antibiotics was done and scrapings from the scleral abscess showed growth of Aspergillus fumigatus on culture. Repeat vitrectomy with silicone oil was needed for retinal detachment. Oral and intravitreal antifungals led to resolution of inflammation with attached retina. This is the first reported case of bee sting-induced fungal endophthalmitis with scleritis.
Keywords: Aspergillus fumigatus, endophthalmitis, ocular bee sting, scleritis
Ocular bee stings are commonly associated with toxic reaction to the injected venom and result in manifestations such as corneal epithelial breakdown, corneal infiltrates, anterior chamber (AC) exudates, secondary glaucoma, and cataract.[1,2] We report a case of Aspergillus fumigatus fungal endophthalmitis and scleritis following ocular bee sting, which was successfully managed with pars plana vitrectomy (PPV) along with topical and systemic antifungals.
Case Report
A 25-year-old man presented with complaints of decrease in vision, pain, redness, and watering from his right eye (RE) 3 days after sting injury by a honey bee. He claimed to have removed the bee on his own. On presentation, his best-corrected visual acuity (BCVA) in the RE was hand motions close to face. His RE had circumcorneal congestion and showed a patch of necrotizing scleritis extending from 1 o’clock to 3 o’clock at the limbus. A brownish microperforation plugged with iris tissue was noted within the scleritis lesion. Cornea showed full-thickness infiltrates with surrounding edema. AC was regular in depth and contained a convex hypopyon. His pupil was up drawn toward the area of scleral perforation [Fig. 1]. Crystalline lens and posterior segment were not visible. Examination of the left eye was unremarkable.
Figure 1.
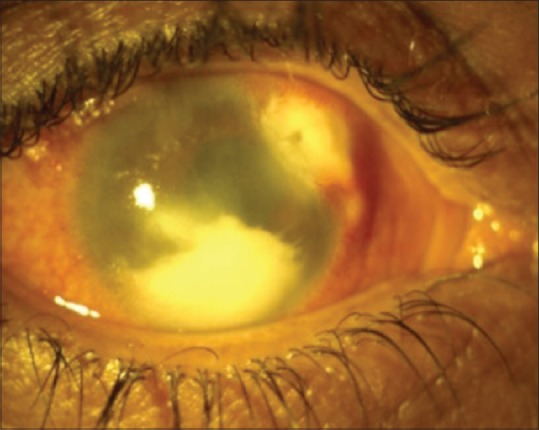
Circumcorneal congestion with area of scleral necrosis extending from 1:30 to 3 o’clock. Cornea is edematous and anterior chamber has a convex hypopyon
Working diagnosis of bee sting-induced toxic keratosclerouveitis was made, and the patient was started on oral prednisolone 60 mg OD, topical fortified antibiotics (cefazolin 5%, six times/day and tobramycin 1.4%, six times/day), and atropine (1%) eye drops. AC inflammation decreased considerably by the next day when an ultrasonography was done. It revealed multiple point-like moderate intensity echoes suggestive of exudates in the vitreous cavity [Fig. 2]. Diagnosis was revised to bee sting-induced exogenous endophthalmitis with necrotizing scleritis, and the patient was subjected to vitreous tap and intravitreal injection of antibiotics (vancomycin 1 mg/0.1 ml + ceftazidime 2.25 mg/0.1 ml). Intravenous levofloxacin was added. Vitreous aspirate was sent for Gram stain, potassium hydroxide (KOH) mount, and bacterial and fungal cultures. While the corneal infiltrates and AC inflammation resolved, there was no improvement of scleritis and vitreous exudates. Hence, the patient underwent PPV with intravitreal vancomycin (1 mg/0.1 ml) and ceftazidime (2.25 mg/0.1 ml). Vitreous tap and scrapings from the scleritis area were sent for Gram-stain, KOH mount, and bacterial and fungal cultures. KOH mount of scleral scraping and vitreous aspirate revealed the presence of branching hyphae with multiple conidia, suggestive of mycelial fungus [Fig. 3]. Fungus was identified as A. fumigatus on culture. The patient was started on oral itraconazole (200 mg BD); topical amphotericin B (15 μg/0.1 ml) and intravitreal amphotericin B (5 μg/0.1 ml) + dexamethasone (400 μg/0.1 ml) were injected. Five days after PPV, ultrasound revealed total retinal detachment with few vitreous exudates. Pars plana lensectomy along with revised vitrectomy with silicone oil tamponade was done. Three months following repeat vitrectomy, the eye was quiescent and the oral and topical antifungals were stopped. At 4-month follow-up, the patient had a BCVA of finger counting at 1 m. The scleritis had healed and the retina was attached under silicone oil [Fig. 4].
Figure 2.
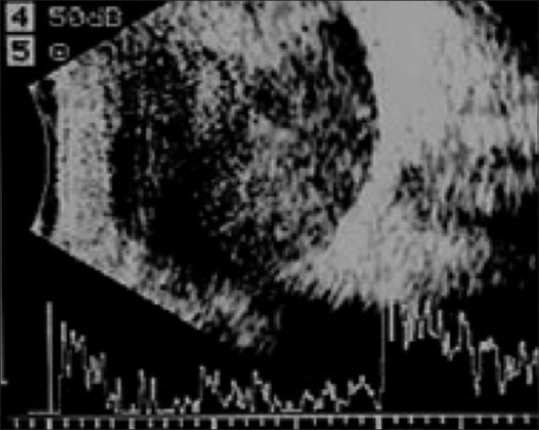
Ocular ultrasound showing the presence of multiple point-like echoes in the vitreous, suggestive of exudates
Figure 3.
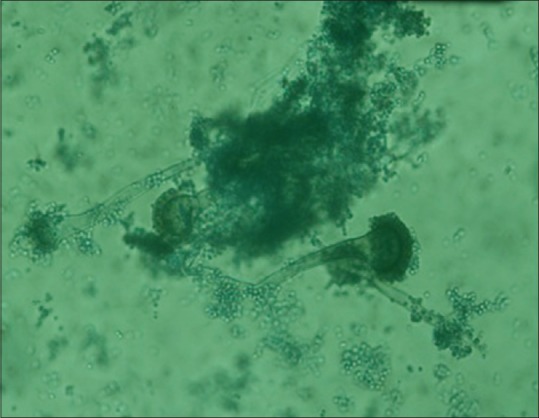
Multiple septate branching hyphae with conidiophores, suggestive of Aspergillus fumigatus
Figure 4.
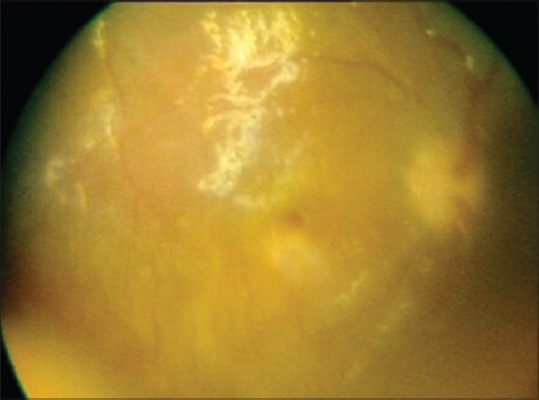
Three months postpars plana lensectomy and vitrectomy-quiet anterior chamber and attached retina with silicone oil
Discussion
A number of ocular complications have been reported following ocular stings from bees or wasps.[1,2] Corneal complications are the most frequent following bee sting injury.[2] Bee venom is a complex toxin which causes activation of the complement cascade, leading to the production of chemotactic factors and anaphylatoxins which result in cell death and ocular inflammation.[3]
Our patient developed a microperforation at the probable site of bee sting. The iris tissue plugging the site of microperforation could have been inoculated with the fungus carried by the bee. Ocular inflammation could be due to reaction to the bee venom, inoculation of the fungus, or a combination of both these factors. Anterior segment inflammation was most likely a consequence of bee venom as it responded to anti-inflammatory treatment. Scleritis and vitreous inflammation were possibly caused by A. fumigatus, and thus, they responded to topical and oral antifungal agents.
Ocular infections with Aspergillus species are usually associated with keratitis and sporadically with endophthalmitis.[4] In addition, Aspergillus is an uncommon cause of infectious scleritis.[5] Rychener first described three principal causes of exogenous fungal endophthalmitis in 1933: contiguous spread from an external ocular infection, penetrating trauma, and intraocular surgery.[6] Trauma with vegetative matter is the usual cause for mycotic scleritis and endophthalmitis.[7]
In case of severe anterior segment inflammation, differentiation between sterile and infectious endophthalmitis becomes difficult. Vitreous samples should be sent for microbiological evaluation to rule out any infectious pathology. Fungal infections of eye usually have a delayed onset of inflammation after injury, but our patient presented within 3 days. A high index of suspicion for fungal infection must be kept in patients of ocular bee stings, irrespective of the duration of symptoms.
To the best of our knowledge, bee sting-induced fungal endophthalmitis with scleritis has not been reported. There is a recent case report of wasp sting-induced panuveitis which improved after vitrectomy.[8]
Conclusion
Bee sting ocular injuries can cause severe ocular inflammation and infectious complications. Hence, aggressive and timely management is needed for these cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chen CJ, Richardson CD. Bee sting-induced ocular changes. Ann Ophthalmol. 1986;18:285–6. [PubMed] [Google Scholar]
- 2.Teoh SC, Lee JJ, Fam HB. Corneal honeybee sting. Can J Ophthalmol. 2005;40:469–71. doi: 10.1016/S0008-4182(05)80008-0. [DOI] [PubMed] [Google Scholar]
- 3.Siddharthan KS, Raghavan A, Revathi R. Clinical features and management of ocular lesions after stings by hymenopteran insects. Indian J Ophthalmol. 2014;62:248–51. doi: 10.4103/0301-4738.128637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scott IU, Flynn HW, Jr, Feuer W, Pflugfelder SC, Alfonso EC, Forster RK, et al. Endophthalmitis associated with microbial keratitis. Ophthalmology. 1996;103:1864–70. doi: 10.1016/s0161-6420(96)30415-6. [DOI] [PubMed] [Google Scholar]
- 5.Ho YF, Yeh LK, Tan HY, Chen HC, Chen YF, Lin HC, et al. Infectious scleritis in Taiwan-a 10-year review in a tertiary-care hospital. Cornea. 2014;33:838–43. doi: 10.1097/ICO.0000000000000174. [DOI] [PubMed] [Google Scholar]
- 6.Rychener RO. Intra-ocular mycosis. Trans Am Ophthalmol Soc. 1933;31:477–96. [PMC free article] [PubMed] [Google Scholar]
- 7.Peyman GA, Carroll CP, Raichand M. Prevention and management of traumatic endophthalmitis. Ophthalmology. 1980;87:320–4. doi: 10.1016/s0161-6420(80)35240-8. [DOI] [PubMed] [Google Scholar]
- 8.Nakatani Y, Nishimura A, Sugiyama K. Successful treatment of corneal wasp sting-induced panuveitis with vitrectomy. J Ophthalmic Inflamm Infect. 2013;3:18. doi: 10.1186/1869-5760-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]


