Abstract
We report concurrent management of rhegmatogenous retinal detachment and myopic choroidal neovascularization in the left eye of a 24-year-old female who presented with sudden dimness of vision due to retinal detachment and choroidal neovascularization. Intravitreal antivascular endothelial growth factor was injected during primary vitrectomy for retinal detachment. At final follow-up, the retina was attached with scarring of choroidal neovascularization. Ours is the first report of the use of intravitreal antivascular endothelial growth factor during vitrectomy for retinal detachment.
Keywords: Anti-VEGF, vitrectomy, myopic choroidal neovascularization, retinal detachment
Rhegmatogenous retinal detachment (RRD) and choroidal neovascularization (CNV) are known causes of visual loss in myopic eyes. These conditions require early intervention to prevent increasing visual morbidity. We hereby report a case with concurrent existence and management of RRD and CNV in a single myopic eye.
Case Report
A 24-year-old female presented with sudden dimness of vision in her left eye for last 20 days. She was high myopic with best-corrected visual acuity of 20/30, N6 with −19 D spherical in the right eye and counting finger at two meter with −13 D spherical in the left eye. The anterior segment was unremarkable in both eyes. The right eye had attached retina with myopic macular degeneration. Left eye showed RRD involving entire retina except a narrow strip of the attached retina at the macula [Fig. 1a]. The causative retinal break was present inferiorly, and it was a posterior break. There was no shifting of subretinal fluid. Slit lamp biomicroscopy of the right eye revealed myopic macular degeneration. Left eye showed yellowish-black lesion at the fovea within the strip of the attached retina at the macula [Fig. 1a]. A clinical diagnosis of RRD with myopic CNV in the left eye was made.
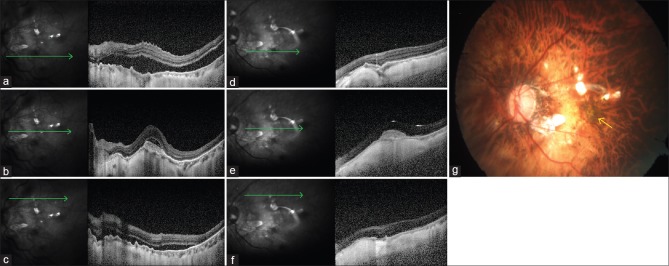
Figure 1.
(a) Color fundus photo of the left eye shows retinal detachment involving superior and inferior retina. Myopic choroidal neovascularization (yellow arrow) is present at fovea within the strip of the attached retina. (b) Fluorescein angiogram image of the left eye shows leakage from the subfoveal choroidal neovascularization (yellow blank arrow). Inferior retina shows bullous detachment. (c) Wide-field fluorescein angiogram image of the left eye shows edges of detached retina (yellow arrowheads) sparing an attached narrow strip of retina at the macula and temporally
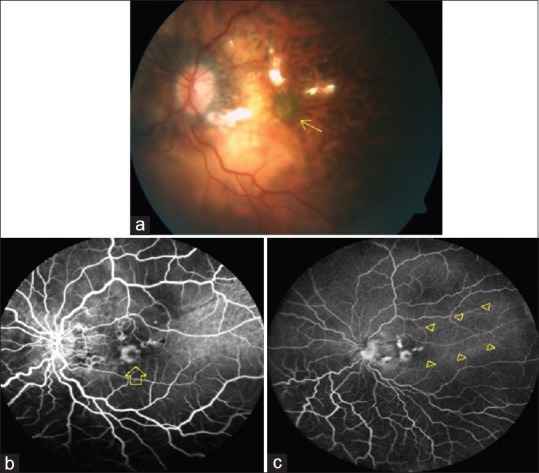
Fluorescein angiogram (FA) of the right eye revealed window defects at the macula. Left eye revealed hyperfluorescence with late leakage from the subfoveal CNV [Fig. 1b and c]. Spectral domain optical coherence tomography (SDOCT Spectralis, Heidelberg Engineering, Heidelberg, Germany) of the right eye showed thinning at fovea. Line scans through the macula in the left eye demonstrated separation between neurosensory retina and retinal pigment epithelium at superior and inferior temporal vascular arcades near the macula [Fig. 2a and c]. The center of the macula was attached. There was a hyperreflective thickening at beneath the fovea with backshadowing [Fig. 2b]. There was localized subretinal fluid overlying the subfoveal thickening with immediate adjacent retina being attached. The FA and SDOCT findings confirmed the CNV.
Figure 2.
(a) Preoperative line scan spectral domain optical coherence tomography image near inferior vascular arcade shows separation between retinal pigment epithelium and neurosensory retina suggestive of retinal detachment. (b) Preoperative line scan spectral domain optical coherence tomography image through the fovea shows choroidal neovascularization and overlying subretinal fluid suggestive of activity. Rest of the retina is attached. (c) Preoperative line scan spectral domain optical coherence tomography image near superior vascular arcade shows separation between retinal pigment epithelium and neurosensory retina suggestive of retinal detachment. (d) Postoperative line scan spectral domain optical coherence tomography image near inferior vascular arcade shows reattached retina. (e) Postoperative line scan spectral domain optical coherence tomography image through the fovea shows increased backscattering and reduced size of choroidal neovascularization suggestive of regression of choroidal neovascularization. Overlying subretinal fluid has resolved with regression. (f) Postoperative line scan spectral domain optical coherence tomography image near superior vascular arcade shows reattached retina. (g) Postoperative color fundus photograph of the left eye shows silicon oil-filled eye with attached retina and resolved choroidal neovascularization (yellow arrow)
Being faced with twin pathologies of RRD and CNV, both of which required early but different interventions, the patient was explained about her eye condition in detail. It was decided to tackle both RRD and CNV together. The patient underwent standard 23-gauge three-port pars plana vitrectomy with belt buckling using 240 band. Care was taken to prevent iatrogenic detachment of the macula, and posterior vitreous detachment was initially induced nasally from optic nerve head followed by extension to periphery in all directions. Fluid-gas exchange was performed through preexisting retinal break at 6 o’ clock position. Laser photocoagulation was done around the retinal break and at the belt buckle effect. Intravitreal ranibizumab (Accentrix 0.5mg/0.05 ml, Novartis Pharmaceutical Corp.) was injected in the air-filled vitreous cavity after fluid-air exchange and laser. Finally, silicon oil tamponade was used. The patient was advised to maintain prone position for 12–16 h per day for three weeks from the day of surgery.
Postoperatively, the patient was doing well with attached retina in the left eye. At 6-week follow–up, the best-corrected visual acuity was 20/30, N6 and 20/120, N10 in her right and left eye, respectively. The right eye was stable. Left eye revealed well-reattached retina with apparently scarred CNV [Fig. 2d–g]. The SDOCT of left eye revealed resolution of subretinal fluid overlying the CNV with increased backscattering and reduced size of the membrane suggestive of scarring of CNV [Fig. 2e]. The patient was prescribed refractive correction and advised to be on monthly follow-up. The vision in the left eye was maintained and there was no sign of reactivation of CNV at next follow-up at 1 month. She has been advised to monitor for increasing distortion of images using Amsler's chart and to review again after a month.
Discussion
While RRD needs surgical repair with oil or gas tamponade, CNV requires intravitreal antivascular endothelial growth factor (anti-VEGF) injection. Since both of them are visually devastating in their individual rights, treatment of one cannot wait for the treatment of other to complete. Therefore, in our case, it was decided to treat both RRD and CNV together.
Intravitreal anti-VEGF is known to be effective in oil-filled eyes in animal studies.[1] However, the peak concentration was found to be lower and achieved later than the eyes which had native vitreous. There have been reports of injection of anti-VEGF in oil-filled eyes for various retinal diseases.[2,3,4] Chhablani and Narayanan and Cascavilla et al. have used intravitreal anti-VEGF in silico n oil-filled eyes which had developed CNV following the previous vitrectomy for retinal detachment.[2,3] While they had injected anti-VEGF in oil-filled eyes, we had a different scenario where we had untreated CNV and RRD simultaneously and had to inject during the primary repair of RRD itself. To the best of our knowledge, there is no report in literature about concurrent management of myopic CNV and RRD with intravitreal anti-VEGF.
We had injected anti-VEGF after fluid-air exchange keeping in mind to let the drug reach the retinal surface directly and avoiding washout of the drug with the infusion fluid used during vitrectomy. However, it was also important to inject the drug before silicon oil injection to avoid the barrier which silicon oil bubble would have posed for the drug to reach the retinal surface. CNV regressed with one anti-VEGF injection in our case; however, the patient has been under follow-up to look for possible recurrence.
Conclusion
Our case highlights the concurrent management of myopic CNV and RRD during the primary vitrectomy. Timing of injection, following fluid-air exchange and before silicon oil injection, appears to be vital to have optimum treatment response.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Xu Y, You Y, Du W, Zhao C, Li J, Mao J, et al. Ocular pharmacokinetics of bevacizumab in vitrectomized eyes with silicone oil tamponade. Invest Ophthalmol Vis Sci. 2012;53:5221–6. doi: 10.1167/iovs.12-9702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chhablani J, Narayanan R. Anti-VEGF therapy in a silicone oil-filled myopic eye with choroidal neovascularisation. BMJ Case Rep 2015. 2015 doi: 10.1136/bcr-2014-208663. pii: bcr2014208663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cascavilla ML, Querques G, Querques L, Codenotti M, Bandello F. Intravitreal ranibizumab for myopic choroidal neovascularization after pars plana vitrectomy and silicone oil tamponade. Eur J Ophthalmol. 2013;23:913–6. doi: 10.5301/ejo.5000337. [DOI] [PubMed] [Google Scholar]
- 4.Salman AG. Intrasilicone bevacizumab injection for iris neovascularization after vitrectomy for proliferative diabetic retinopathy. Ophthalmic Res. 2013;49:20–4. doi: 10.1159/000341734. [DOI] [PubMed] [Google Scholar]