Abstract
Background
We sought to develop an objective implant selection guideline based on the ratio of patient body mass index (BMI) to age in order to select implants preoperatively and reduce cost while maintaining quality. The BMI-to-age ratio can be used to distinguish patient demand and select those patients who may benefit from newer technology and higher cost implants and those who would do well with standard-demand implants.
Methods
A retrospective analysis investigated the types of implants received by patients undergoing total knee arthroplasty from January 2012 to August 2014. Patients with a BMI-to-age ratio >0.60 were categorized as high demand and were eligible for either a high-demand implant or a standard-demand implant. Patients with a BMI-to-age ratio ≤0.60 were recognized as standard demand and would be eligible for only standard-demand implants. The actual implant received was identified and compared with the implant as predicted by the BMI-to-age ratio and potential cost savings were identified.
Results
A total of 1507 operative knees were identified. The high-demand implant carries a 31% greater cost than that of a standard-demand implant. Thirty-eight of 1084 high-demand implants were placed in standard-demand knees. An additional 1.1% cost was realized with 38 standard-demand knees receiving high-demand implants and 28.6% if high-demand knees had been used in all standard-demand patients.
Conclusions
Limiting the use of high-demand implants to high-functional-demand patients based on the BMI-to-age ratio may guide the surgeon's choice in optimizing implant selection while providing value-based purchasing criteria to the selection of total knee arthroplasty implants.
Keywords: TKA, Implant, BMI, Demand, Matching, Knee
Introduction
Total knee arthroplasty (TKA) is one of the most common and cost-effective orthopaedic procedures, and carries a high patient satisfaction. Over 700,000 TKAs are performed annually in the United States and the procedure is increasing in prevalence [1]. The number of TKAs performed annually in the United States is expected to grow by 673% to 3.48 million procedures by 2030 [2]. A variety of pathologic conditions affecting the knee can be treated with TKA, leading to pain relief, restoration of function, and increased mobility [3].
A high percentage of the hospital cost of TKA may be attributed to the cost of the prosthetic implant. Implant prices have grown at a much faster rate than any other aspect of the surgical procedure [4]. The American Academy of Orthopaedic Surgeons published a statement in 1992 with 3 major points; orthopaedic surgeons should make decisions relating to the selection of implants, they should establish reasonable criteria for implant selection based on patient's need, and that cost-containment strategies should be developed [4]. The institutional response to restricting the rising cost of implants has taken 3 major forms: competitive bidding, ceiling pricing, and implant selection guidelines based on demand matching. Implant selection guidelines are based on a demand-matching system of stratifying patients into levels of functional stress that is expected to be placed on the prosthesis [4].
It is still being investigated whether more costly implants have an overall higher survivorship in the general population [5]. However, certain implants may be indicated for specific patient populations, depending on demand. Surgeons take into consideration multiple factors including weight, age, expected activity after replacement, general health, and bone stock when deciding the appropriate implant to use for a particular patient [6]. Generally, younger, heavier patients who are more active may require a high-demand implant. Moreover, high-demand implants historically have incurred a greater price, and is only beneficial if placed in a high-demand patient. If proper demand matching is not used, high-demand implants may be used in standard-demand patients leading to increased cost and inadvertent allocation of implant capability to a patient who may not benefit from it. This scenario would not be cost-effective.
Implant selection guidelines based on demand are an effective approach in predicting patient functional status post-TKA. Because patient activity is correlated with wear, implant selection and resource allocation can be targeted to those patients who may benefit from presumed improvements in implant technology [7]. Preoperative implant selection guidelines based on demand matching or standardization for TKA were developed to provide objective standards for knee implant selection. Guidelines for knee implant selection are based on the demand a patient is expected to place on the knee prosthesis after TKA. The process of demand matching also has been used by hospitals to control and reduce the cost of joint replacement implants [7].
Our institution, an academic, high volume, urban orthopaedic specialty hospital began a program to decrease the price of total joint replacement implants as part of an overall cost saving effort associated with value-based purchasing and the bundled payment for care improvement initiative. Before the implementation of this program, a body mass index (BMI) >40 kg/m2 and/or age <55 years was the only defining criteria for high-demand implant selection while taking into consideration qualitative analysis of activity level, and patient-specific factors including anatomy and bone quality [8]. Approval for higher cost implants in patients who did not meet the age and weight criteria for high-demand implants were made on a case-by-case basis by a surgeon committee.
In this study, as part of a TKA clinical pathway, we sought to develop a universally objective selection guideline based on the BMI-to-age ratio of patient to select implants preoperatively and reduce cost. The literature contains few validated tools that can accurately and reproducibly predict patient activity after TKA [7]. The BMI-to-age ratio can be used to distinguish patient demand and select those patients who would likely benefit from newer technology and higher cost implants and who will do well with the standard-demand implants. Inappropriate implant selection may effectively be reduced, and thus decrease the overall cost of arthroplasty for an institution. We hypothesize that the implementation of a BMI-to-age ratio as part as a standardized clinical pathway would decrease overall costs and enhance efficiency in implant selection. Rational selection of implants in a value-based health care system is critical to economic survivorship in the new health care paradigm.
Material and methods
Participants
Participants were identified after approval by the institutional review board. Data were collected on TKAs that have occurred over a 2.5-year period with 1363 patients with 1507 TKAs identified from the electronic medical record.
Study methodology
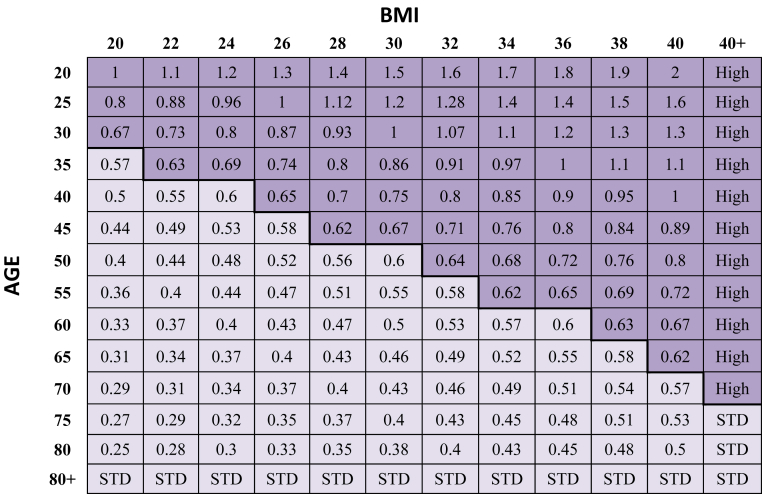
A retrospective review was conducted to assess the types of implants received by patients undergoing TKA from January 2012 to August 2014 under the former implant selection guideline criteria, which included age <55 years, BMI >40 kg/m2, as well as patient factors including activity level and anatomy. This left that previous guideline system open for interpretation. For our study, patients were stratified based on their BMI-to-age ratio. The BMI-to-age ratio cutoff was developed by a team of surgeons at our institution, taking into consideration the current literature, the previous implant-matching guidelines, and a retrospective analysis of patient outcomes and historical demand-matching patterns. Demand refers to patient requirements in the context of wear rates based on age and BMI, rather than physical-activity demand. Patients with a BMI-to-age ratio >0.60 were categorized as high-demand patients and were eligible for either a high-demand implant or a standard-demand implant. Patients with a BMI-to-age ratio ≤0.60 are recognized as a standard-demand patient and should only be eligible for standard-demand implants. Under the ration, standard-demand implants may be placed in both standard-demand patients and high-demand patients, based on several factors the surgeon considers while evaluating what is best fit for the patient's needs. High-demand implants placed in standard-demand patients were considered to be not cost-effective. The actual implant received was identified and compared with the implant as predicted by the BMI-to-age ratio and potential cost savings were identified. Retrospectively, we determined how much cost would have been saved if the BMI-to-age ratio implant selection guidelines had been implemented during this period. In addition, we calculated the maximum potential savings that could be achieved under this model (Fig. 1; Tables 1 and 2).
Figure 1.
The BMI-to-age ratio demand matching. High-function-demand patient: BMI:age >0.60 (eligible for high-demand implant or standard-demand implant). Standard-function-demand patient: BMI:age ≤0.60 (should receive only standard-demand implant).
Table 1.
Types of implants received by patients from January 2012 to August 2014.
| Type of implant | Standard-demand knees | High-demand knees | Total |
|---|---|---|---|
| Standard-demand implants | 1046 | 375 | 1421 |
| High-demand implants | 38 | 48 | 86 |
| Total | 1084 | 423 | 1507 |
Table 2.
Patient demographics.
| Age:BMI category | Standard demand | High demand | Total |
|---|---|---|---|
| Age, y | 67.7 | 56.0 | 64.2 |
| BMI, kg/m2 | 31 | 40.8 | 34 |
| Gender | Male: 53 Female: 912 |
Male: 17 Female: 378 |
Male: 70 Female: 1290 |
At our institution, the high-demand implant choices were of newer design and included features such as high flexion, enhanced fixation, more kinematic design, oxidized zirconium, robotic-assisted compatibility and mobile-bearing as well as additional sizing and enhanced instrumentation. The insert choices include standard polyethylene, highly cross-linked polyethylene, and vitamin E–enhanced polyethylene. Previous implant selection guidelines at our institution were determined by the operating surgeon. Selection criteria included weight >300 lbs and/or age <55 years. Cost analysis was performed based on current implant pricing to determine how much cost would have been saved if high-demand implants were limited to use in only high-demand patients with a BMI-to-age ratio >0.60. All high-demand implants used in standard-demand groups were considered to be not cost-effective.
Results
A total of 1363 patients were identified as undergoing TKA between January 2012 and August 2014 with 1507 operative knees. The mean age and standard deviation at the time of surgery was 64.2 years ±10.2, with 4.8% of patients being men and 95.2% of patients being women. One thousand eighty-four TKAs were categorized as standard-demand patients (BMI:age ≤0.60), and 423 TKAs were categorized as high-demand patients (BMI:age >0.60). Of the patients categorized as standard-demand, the average age was 67.4 years; and of the patients categorized as high-demand, the average age was 56.0 years.
Under the ratio, high-demand implants may only be placed in high-demand patients, whereas standard-demand implants may be placed in standard-demand or high-demand patients per the surgeon's discretion. Thirty-eight high-demand implants and 1046 standard-demand implants were used in 1084 standard-function-demand patients. Forty-eight high-demand implants and 375 standard-demand implants were used in 423 high-demand patients based on the BMI-to-age ratio.
At our institution, the high-demand implant carries a 31% greater cost than a standard-demand implant. Thirty-eight high-demand implants were placed in standard-demand patients. We calculated that 1.1% of the total cost of all implants used in standard-demand patients undergoing TKA could have been saved if standard-demand implants were used in the 38 standard-demand knees that had received high-demand implants. If high-demand implants had been placed in all standard-demand and high-demand patients, the total cost would have been 31% greater than if they had received the less costly standard-demand implants, and 28.6% greater than the cost of the actual implants used in our patient sample.
Discussion
Total joint arthroplasty volumes have increased in the last 2 decades; and because of financial constraints, Medicare reimbursements have not kept pace with inflation [8]. The Medicare hospital payment for primary total joint arthroplasty has increased at 50% of the rate of inflation over the last 2 decades while hospital cost and implant cost have continued to increase [14]. Rising implant prices are a major driver of hospital spending on these procedures. As the aging US population creates a growing demand for joint replacement, controlling implant costs is becoming a top priority for healthcare institutions. Some hospitals have sought to control implant costs through an implant selection guideline criteria strategy—carefully delineating which patients can receive which implants.
Formerly at our institution, the implant selection guideline criteria include patient age, BMI, activity level, and anatomy, but exceptions were limited and not well-defined. For example, patients must be under 55 years of age and/or heavier than 300 lbs to be considered for a high-demand implant [9]. The BMI-to-age ratio was developed by a team of surgeons at our institution, based on current literature and a retrospective analysis of demand-matching patterns and outcomes of their patients. A BMI-to-age ratio of 0.60 was established as the cutoff because after considering the expected activity level and patient function, younger and heavier patients will theoretically maintain the highest benefit from high-demand implants, and historically have had the highest TKA failure rates. Young, low to average BMI patients historically have excellent survivorship with standard implants; there has been little added benefit for the application of a high-functional-demand, high-cost implant in these standard-demand patient groups [10], [11], [12], [13]. However, the utilization of a BMI-to-age ratio can objectively identify those patients who may benefit from the high-demand implants.
Our data indicated that with the implementation of BMI-to-age ratio implant selection guidelines, utilization of high-priced implants in standard-demand knees can be effectively avoided. A 1.1% decrease in cost of the total implant expenditures would have been realized over the 2.5-year review, if only standard-demand implants had been used in standard-demand patients. If high-demand implants were used for all standard-demand patients, the cost would have been an additional $679,900; 29.5% more than if we had used the BMI-to-age ratio criteria for implant selection.
In 88.9% of cases, the BMI-to-age ratio was highly correlated with the implant choices made by surgeon preference and previous guidelines. Objectifying implant selection guidelines improves the predictability of implant costs for health care institutions while allowing surgeon's choice for those patients where new technology may be indicated. Limiting the use of high-demand implants to high-demand patients based on the BMI-to-age ratio may guide the surgeon's choice in optimizing implant selection while providing value-based purchasing criteria to the selection of TKA implants.
There are several factors that influence the cost of implants. Patient-specific factors including age and comorbidities have a very small effect on the overall cost. Hospital characteristics and physician preference have the greatest effect [14]. In an economic analysis, Bozic et al. demonstrated that while implant cost was affected by hospital factors including volume, number of vendors present, and hospital bed size, there was a significant amount of cost variation among hospitals that could not be accounted for [14], [15]. The same study also found significant cost variation because of physician preference [14], [15].
Quality, value-based medicine is essential in the alternative payment model era of TKA now unfolding. In 2011, the bundled payment for care improvement initiative was introduced by Centers for Medicare and Medicaid Services to achieve the highest value medical care possible for TKA patients. Representing some of the highest Centers for Medicare and Medicaid Services expenditures, naturally TKA was a target. The model that was established at our institution includes services provided 72 hours before admission, the inpatient stay, and 90 days after discharge [16]. A threshold cost or target price is provided per episode of care and Medicare then retrospectively performs audits to determine whether the payments exceed or were less than the target price. Savings from the initial bundled payment that is achieved because of cost-effective care will be awarded to the episode initiators and gain shared with providers through previously negotiated quality and cost metric calculations. Physician reimbursement above standard Medicare rates are determined by a gain-sharing formula based on quality, cost-effectiveness, volume, and value agreed on with the hospital and is limited to 50% of the surgeon fee for a Medicare TKA [16]. The potential value generated is an incentive for quality and cost-effective care delivery, which can be achieved through the implementation of standardized clinical pathways and implant standardization programs.
Healy et al. [6] developed a cost-reduction and implant-selection program based on demand matching. This program offered guidelines for TKA implant selection that decreased the cost of knee implants for the hospital. Patients were assigned to demand groups based on 5 measures: age, weight, bone stock, general health, and the expected postoperative patient activity as determined by the surgeon. The implants were assigned to demand function categories based on an implant's expected capacity to manage the patient's predicted demand. This program was only used for use in primary TKA. The goals were to improve clinical efficiency, cost-effectiveness, and quality of care. It was demonstrated that the employment of a knee standardization program and clinical pathway post-TKA reduced hospital cost and length of stay without compromising patient outcomes, satisfaction, or complication rates. The utility of all-polyethylene tibial components in lower demand categories afforded the greatest cost savings [6].
Robinson et al. [17] investigated the costs associated with TKA in an analysis of 10,155 patients undergoing unilateral TKA across 61 hospitals and determined that the average implant cost per case ranged from $1797 to $12,093. Sixty-one percent of the total variation in implant costs can be attributed to hospital characteristics and only 2.5% attributable to patient characteristics; the remaining 36.5% of variance was attributable to within-hospital variation, but not because of patient or hospital characteristics [17]. The additional cost does not necessarily equate to an added benefit. These costs may translate to the expenses of using new technology without evidence of prolonged survivorship or improved functionality [17]. With rising hospital costs, in a value-based healthcare environment, it is in the provider's, the hospital's, and the patient's best interest to curb unnecessary costs while maintaining quality.
One problem with unstandardized implant selection is that surgeons are not fully aware of the costs of the implants that are being used. A study performed at Case Western Reserve and The University of Michigan distributed questionnaires to consultant attending orthopaedic surgeons and residents. Respondents were asked to estimate the costs of commonly used orthopaedic devices. Sixty-seven percent of responses were underestimations of implant cost and 33% were overestimations. The study concluded that the knowledge of orthopaedic implant cost among attendings and residents is poor [18]. This disparity between the perceived costs and actual costs is a contributing factor to prevent the use of cost-ineffective implants in TKA. An awareness of the cost of implants and a conscientious effort by physicians to account for cost vs benefit will help control the growing costs of TKA. Higher priced TKA implants (ie, oxidized zirconium, vitamin E polyethylene, mobile bearings) does not necessarily increase survivorship in all patients, especially if they do not need a high-demand implant [10], [11], [12].
As the demands of young, active patients with knee osteoarthritis increase, the demand for new technology will likely increase. A “high-function knee” will evolve with potential for greater range of motion, improved kinematics, and reduced bearing surface wear with a more natural feel under high loads. Evaluating new technology for appropriate use will be a challenge. Stratification of patients with different activity levels or demand is important for implementing and evaluating new technologies. Because new technology will likely be used for the patient groups already most at risk for failure with traditional technologies, it will be difficult to show superiority of new implants over traditional models. This is because a higher failure rate might be anticipated in these groups and since past outcomes of traditional models have been reported in lower demand groups. Orthopaedic surgeons will need an easily implemented patient activity measure for stratification of patient groups and results of treatment [7]. A BMI-to-age ratio with an activity score multiplier would be an ideal implant selection guideline. Perhaps with digital personal technology such a predictive tool will be more readily available in the future.
Implant selection guidelines based on demand matching in TKA have been proven to be a valid means to predict appropriate implant selection. Surgeons' implant selection was costlier than BMI-to-age ratio selection when analyzing the high-demand implants placed. However, with the surge of projected knee replacements in the future and the increasing prices of TKA implants, consistent proper implant selection and utilization based on patient functional demand consideration is essential. Implant selection guidelines based on a BMI-to-age ratio may provide the framework to make budgeting for implant costs more predictive in a value-based health care environment.
Conclusions
Transition to the BMI-to-age ratio has had little effect on surgeon's choice of TKA implants at our institution. Objectifying implant selection guidelines improves the predictability of implant costs for health care institutions while allowing surgeon's choice for those patients where new technology may be indicated. Limiting the use of high-demand implants to only high-demand patients based on the BMI-to-age ratio may guide the surgeon's choice in optimizing implant selection while providing value-based purchasing criteria to the selection of TKA implants [6], [7], [19].
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2017.08.001.
Appendix A. Supplementary data
References
- 1.Watts C.D., Wagner E.R., Houdek M.T. Morbid obesity: a significant risk factor for failure of two-stage revision total knee arthroplasty for infection. J Bone Joint Surg Am. 2014;96(18):e154. doi: 10.2106/JBJS.M.01289. [DOI] [PubMed] [Google Scholar]
- 2.Kurtz S., Ong K., Lau E. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 3.Mahomed N.N., Barrett J., Katz J.N. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg Am. 2005;87:1222. doi: 10.2106/JBJS.D.02546. [DOI] [PubMed] [Google Scholar]
- 4.Barrack R. Implant matching has no clinical or scientific basis. J Arthroplasty. 1996;11(8):969. doi: 10.1016/s0883-5403(96)80140-9. discussion 971–972. [DOI] [PubMed] [Google Scholar]
- 5.Schwarzkopf R., Sagebin F.M., Karia R. Factors influencing patients' willingness to pay for new technologies in hip and knee implants. J Arthroplasty. 2013;28(3):390. doi: 10.1016/j.arth.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Healy W.L., Iorio R., Ko J., Appleby D., Lemos D.W. Impact of cost reduction programs on short-term patient outcome and hospital cost of total knee arthroplasty. J Bone Joint Surg Am. 2002;84-A(3):348. doi: 10.2106/00004623-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Iorio R., Healy W.L., Applegate T. Validity of preoperative demand matching as an indicator of activity after TKA. Clin Orthop Relat Res. 2006;452:44. doi: 10.1097/01.blo.0000229361.12244.2d. [DOI] [PubMed] [Google Scholar]
- 8.Alvarado C.M., Bosco J. Understanding and controlling cost in total joint arthroplasty. Bull Hosp Jt Dis (2013) 2015;73(2):70–77. [PubMed] [Google Scholar]
- 9.Orthopedic hospital uses ‘price point’ strategy to lower implant costs. OR Manager. 2014;30(9):22. 24-5. [PubMed] [Google Scholar]
- 10.Duffy G.P., Trousdale R.T., Stuart M.J. Total knee arthroplasty in patients 55 years old or younger. 10- to 17-year results. Clin Orthop Relat Res. 1998;(356):22. doi: 10.1097/00003086-199811000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Nunley R.M., Nam D., Berend K.R. New total knee arthroplasty designs: do young patients notice? Clin Orthop Relat Res. 2015;473(1):101. doi: 10.1007/s11999-014-3713-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Victor J., Ghijselings S., Tajdar F. Total knee arthroplasty at 15-17 years: does implant design affect outcome? Int Orthop. 2014;38(2):235. doi: 10.1007/s00264-013-2231-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Toman J., Iorio R., Healy W.L. All-polyethylene and metal-backed tibial components are equivalent with BMI of less than 37.5. Clin Orthop Relat Res. 2012;470(1):108. doi: 10.1007/s11999-011-2124-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bosco J.A., Alvarado C.M., Slover J.D., Iorio R., Hutzler L.H. Decreasing total joint implant costs and physician specific cost variation through negotiation. J Arthroplasty. 2014;29(4):678. doi: 10.1016/j.arth.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 15.Bozic K.J., Saleh K.J., Rosenberg A.G. Economic evaluation in total hip arthroplasty: analysis and review of the literature. J Arthroplasty. 2004;19:180. doi: 10.1016/s0883-5403(03)00456-x. [DOI] [PubMed] [Google Scholar]
- 16.Iorio R. Strategies and tactics for successful implementation of bundled payments: bundled payment for care improvement at a large, urban, academic medical center. J Arthroplasty. 2015;30(3):349. doi: 10.1016/j.arth.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 17.Robinson J.C., Pozen A., Tseng S., Bozic K.J. Variability in costs associated with total hip and knee replacement implants. J Bone Joint Surg Am. 2012;94(18):1693. doi: 10.2106/JBJS.K.00355. [DOI] [PubMed] [Google Scholar]
- 18.Streit J.J., Youssef A., Coale R.M., Carpenter J.E., Marcus R.E. Orthopaedic surgeons frequently underestimate the cost of orthopaedic implants. Clin Orthop Relat Res. 2013;471:1744. doi: 10.1007/s11999-012-2757-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bozic K.J., Morshed S., Silverstein M.D., Rubash H.E., Kahn J.G. Use of cost-effectiveness analysis to evaluate new technologies in orthopaedics. The case of alternative bearing surfaces in total hip arthroplasty. J Bone Joint Surg Am. 2006;88(4):706. doi: 10.2106/JBJS.E.00614. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.