Abstract
Background
Recent hypotheses have suggested the pathophysiological role of catecholamines in the evolution of the Takotsubo syndrome (TTS). The extent of cardiac and circulatory compromise dictates the use of some form of supportive therapy. This study was designed to investigate the clinical outcomes associated with catecholamine use in TTS patients.
Methods
Our institutional database constituted a collective of 114 patients diagnosed with TTS between 2003 and 2015. The study-patients were subsequently classified into two groups based on the need for catecholamine support during hospital stay (catecholamine group n = 93; 81%, non-catecholamine group = 21; 19%). The primary end-point of our study was all-cause mortality.
Results
Patients receiving catecholamine support showed higher grades of circulatory and cardiac compromise (left ventricular ejection fraction (LVEF) 39.6% vs. 32.7%, p-value < 0.01) and the course of disease was often complicated by the occurrence of different TTS-associated complications. The in-hospital mortality (3.2% vs. 28.5%, p < 0.01), 30-day mortality (17.2% vs. 51.4%, p < 0.01) as well as long-term mortality (38.7% vs. 80.9%, p < 0.01) was significantly higher in the group of patients receiving catecholamine support. A multivariate Cox regression analysis attributed EF ≤ 35% (HR 3.6, 95% CI 1.6–8.1; p < 0.01) and use of positive inotropic agents (HR 2.2, 95% CI 1.0–4.8; p 0.04) as independent predictors of the adverse outcome.
Conclusion
Rates of in-hospital events and short- as well as long-term mortality were significantly higher in TTS patients receiving catecholamine support as compared to the other study-patients. These results need further evaluation in pre-clinical and clinical trials to determine if external catecholamines contribute to an adverse clinical outcome already compromised by the initial insult.
Keywords: Takotsubo cardiomyopathy, Cardiogenic shock, Heart failure, Catecholamines
Background
The Takotsubo Syndrome (TTS) is as an acute and usually reversible from of heart failure characterized by a transient dysfunction of the left ventricle [1, 2]. The TTS patient presents with clinical features such as acute chest pain and dyspnea, bearing some similarity to the patient presenting with an acute myocardial infarction or an acute coronary syndrome (ACS) [3]. An increase in cardiac troponin and creatine kinase levels as well as electrocardiogram (ECG) changes on admission suggesting ST-segment elevation in precordial leads adds to the confusion in early diagnosis. The absence of significant coronary stenosis on coronary angiography, which could correlate with this presentation, and the history of an emotional or physical trigger, leads to the potential diagnosis of TTS [3, 4]. This non-ischemic syndrome has also alternatively been labeled as a stress- or stress-induced cardiomyopathy, an apical ballooning syndrome, or ‘broken heart syndrome’ [4–8].
The classical pattern of left ventricular (LV) morphology in TTS, present in almost 50–80% of all patients, is the apical variant, which is characterized by apical ballooning of the LV at end-systole. Other morphological presentations include those defined by a predominantly hypokinetic circumferential base (inverted Takotsubo variant), or a hypokinetic circumferential mid ventricle (mid LV variant), or demonstrating focal variations [9–13].
The pathophysiology of TTS has been well-debated, however is still poorly described. The influence of an acute catecholaminergic surge contributing to some form of myocardial stunning has been hypothesized by several researchers [14]. Stressful triggers could potentially contribute to an increased hypothalamic-pituitary-adrenal axis (HPA) gain and catecholamine release. This resulting catecholamine surge possibly directs a pathological response from the cardiovascular as well the sympathetic nervous system and serves as the basis for the evolution of TTS [15, 16].
This interesting correlate, naturally, has far-reaching clinical implications. The therapeutic use of catecholamines has been routinely advocated in cases of circulatory compromise, however, its use in the setting of TTS could have potential drawbacks. Extrapolating this thought, our study attempts to explore the hither to poorly understood pathophysiological mechanisms involved in the TTS and determine if external catecholamines contribute to an adverse clinical outcome already compromised by the initial insult.
Methods
Study design and population characteristics
This study incorporated a population subset derived from a patient collective diagnosed with TTS at the University Medical Centre Mannheim, Germany between January 2003 and September 2015. A total of 114 patients were included consecutively to this mono-centric and observational study designed for retrospective data analysis. All these patients were essentially diagnosed with the TTS on hospital admission, and their presenting features met the conditions set out by the modified Mayo Clinic Criteria [17]. These criteria essentially highlight the transient wall motion abnormality in the LV mid-segments with or without apical involvement; describe regional wall motion abnormalities that extend beyond a single epicardial vascular distribution; and define an event that occurs frequently, but not always in the wake of a successful trigger. Additionally, these salient criteria mandate the effective rule-out of occlusive coronary disease; focuses on the appearance of new ECG pathologies, which mimic ACS or modest elevations in cardiac troponin levels; and underlines the prerequisite absence of diseases like pheochromocytoma and myocarditis in the patient.
Patients with co-existing occlusive coronary artery disease as well as those exhibiting wall-motion abnormalities corresponding to any single coronary vessel territory were excluded from this study. A total of 18 patients with uncertain TTS, with no record of coronary angiography or echocardiography results, were excluded from this study. The relevant clinical data of each study-patient was ascertained and compiled in a database with significant aspects of their medical history, laboratory work-up and medical/surgical therapy efficiently earmarked for future reference. Additional parameters outlined for evaluation included duration of hospital stay, need for monitoring and care in the ICU (intensive care unit), use of invasive or non-invasive ventilation, inotropic support, temporary pacing, and demand for renal replacement therapy. Essential diagnostic workup including a routine ECG, echocardiography (to evaluate LV, RV function and wall-motion abnormalities), and a coronary and LV angiography (to rule out occlusive coronary artery disease) was performed on all patients. A consolidated review of this data was conducted by two independent cardiologists and once the diagnosis of TTS was reaffirmed, the study-patients were subsequently classified into two groups based on the need for catecholamine support during hospital stay. A consortium diagram to explain the population recruitment has been outlined in Fig. 1.
Fig. 1.
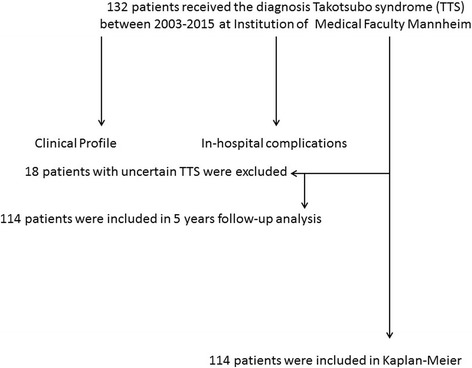
Flow Diagram of study
The primary end-point of our study was all-cause mortality as assessed by chart review and/or telephonic review. If medical records, treating physicians or relatives were unable to provide further information concerning the circumstances of death, it was defined as death due to unknown cause.
The research conduct corresponded to the principles outlined in the declaration of Helsinki and was approved by the medical ethics committee of the Faculty of Medicine in Mannheim, University of Heidelberg, Germany.
Statistics
Statistical analyses were performed using SPSS Version 22 (SPSS Inc., Chicago, Illinois). Data is presented here as means ± SD for continuous variables with a normal distribution, median (interquartile range) for continuous variables with a non-normal distribution, and as frequency (%) for categorical variables. The Kolmogorov–Smirnov test was used to assess normal distribution. Student’s t-test and the Mann–Whitney U-test were used to compare continuous variables with normal and non-normal distributions, respectively. The chi-squared-test or Fisher’s exact test was used to compare categorical variables. The log-rank test was used to compare the survival curves between the two patient groups classified as per catecholamine use. p-values < 0.10 on univariate analysis were further evaluated via the Cox multivariate regression to define independent risk factors for the respective end-point. A two-tailed p-value of < 0.05 was considered statistically significant.
Results
Baseline characteristics
The baseline characteristics of the 114 patients included in this study have been referenced in Table 1.
Table 1.
Baseline characteristics of 114 patients initially presenting with TTC
| Variables | No catecholamines (n = 93) | catecholamines(n = 21) | p value* |
|---|---|---|---|
| Demographics | |||
| Age, mean ± SD | 67.65 ± 11.00 | 65.00 ± 12.30 | 0.33 |
| Male, n (%) | 13 (13.97) | 6 (28.57) | 0.11 |
| Symptoms, n (%) | |||
| Dyspnoe | 34 (36.55) | 9 (42.85) | 0.62 |
| Chest pain | 52 (55.91) | 6 (28.57) | 0.03 |
| Clinic parameter | |||
| Systolic BP, mmHg | 134.96 ± 28.41 | 116.25 ± 42.32 | 0.01 |
| Diastolic BP, mmHg | 78.41 ± 13.67 | 66.55 ± 31.22 | 0.03 |
| Heart rate, bpm | 98.17 ± 27.64 | 110.95 ± 22.79 | 0.05 |
| ECG Data, n (%) | |||
| ST-segment elevation | 27 (29.03) | 7 (33.33) | 0.79 |
| Inversed T-Waves | 83 (89.24) | 19 (90.47) | 0.74 |
| PQ-interval | 160.67 ± 27.97 | 160.00 ± 34.38 | 0.92 |
| QTc (ms), mean ± SD | 484.49 ± 50.83 | 455.30 ± 52.82 | 0.02 |
| Stress factor, n (%) | |||
| Emotional sress | 28 (30.10) | 2 (9.52) | 0.05 |
| Physical stress | 50 (53.76) | 14 (66.66) | 0.33 |
| Laboratory values, mean ± SD | |||
| Troponin I (U/L) | 3.20 ± 4.41 | 6.57 ± 8.46 | 0.01 |
| Creatine phosphatkinase (U/L) | 721.11 ± 2900.64 | 323.74 ± 469.71 | 0.55 |
| CKMB | 37.44 ± 65.08 | 31.00 ± 23.56 | 0.77 |
| C-Reactive protein (mg/l) | 42.63 ± 64.25 | 80.30 ± 126.15 | 0.06 |
| Hemoglobin | 12.10 ± 1.99 | 12.29 ± 2.08 | 0.70 |
| Creatinine (mg/dl) | 1.14 ± 0.76 | 1.19 ± 0.50 | 0.79 |
| GFR < 60 ml/min | 25 (26.88) | 7 (33.33) | 0.59 |
| Echocardiography data, n (%) | |||
| LV EF % | 39.67 ± 9.12 | 32.76 ± 9.09 | < 0.01 |
| Follow-up LV EF % | 55.23 ± 7.54 | 48.63 ± 14.90 | < 0.01 |
| Apical ballooning | 64 (68.81) | 18 (85.71) | 0.15 |
| Mitral regurgation | 50 (53.76) | 10 (47.61) | 0.63 |
| Tricspid regurgation | 42 (45.16) | 7 (33.33) | 0.46 |
| RV-Involvement | 17 (18.27) | 9 (42.85) | 0.02 |
| Medical history, n (%) | |||
| Smoking | 30 (32.25) | 6 (28.57) | 0.80 |
| Diabetes mellitus | 22 (23.65) | 4 (19.04) | 0.64 |
| Obesity (BMI > 25 kg/m2) | 27 (29.03) | 4 (19.04) | 0.75 |
| Hypertension | 54 (58.06) | 12 (57.14) | 1.00 |
| COPD | 19 (20.43) | 7 (33.33) | 0.25 |
| Atrial fibrillation | 15 (16.12) | 6 (28.57) | 0.21 |
| Coronary artery disease | 16 (17.20) | 6 (28.57) | 0.23 |
| History of malignancy | 13 (13.97) | 3 (14.28) | 0.97 |
| Drugs on admission, n (%) | |||
| Beta-blocker | 32 (34.40) | 3 (14.28) | 0.06 |
| ACE inhibitor | 30 (32.25) | 5 (23.80) | 0.45 |
| ASS | 24 (25.80) | 5 (23.80) | 0.87 |
| Anticoagulation | 7 (7.52) | 0 (0) | 0.19 |
*p values for the comparison between group 1 and group 2; SD Standard deviation, ECG Electrocardiogram, EF Ejection fraction, BMI body-mass-index, COPD Chronic obstructive pulmonary disease, ACE Angiotensin-convetring-enzyme
EFhochversusnichthoch*Katecholaminpflichtigkeit: 0.000
The bolded indication highlight significant values
A detailed analysis of available data revealed an insignificant demographic distribution, with age and gender variables expressed almost similarly in both patient groups. Chest pain was interestingly more pronounced in the hemodynamically stable patient (55.9%, n = 52, vs. 28.5%, n = 6, p = 0.03) as compared to those requiring some form of catecholamine support. The clinical parameters used to ascertain patient status, such as systolic blood pressure (134.96 ± 28.41 mmHg vs. 116.25 ± 42.3 mmHg, p = 0.01) and heart rate (98.1 ± 27.6 bpm vs. 110.9 ± 22.7 bpm, p = 0.03), expectedly showed variation between the two groups, wherein lower blood pressure values and mild tachycardia was frequently observed among patients requiring catecholamine support.
Diagnostic parameters
The initial diagnostic work-up, detailed with an electrocardiogram, suggested catecholamine-support-free patients recorded significantly longer QTc-Interval’s as opposed to the hemodynamically unstable catecholamine therapy-dependent patient (484.49 ± 50.83 ms vs. 455.30 ± 52.82 ms, p = 0.02). Other diagnostic parameters like echocardiographic estimates of left-ventricular ejection fraction revealed a comparatively lower degree of compromise in cardiac function among patients not requiring external catecholamines (index LVEF measurements 39.67 ± 9.12% vs. 32.76 ± 9.09%, p < 0.01). Similarly, lower index troponin-I levels were documented in this group (3.20 ± 4.41 U/l vs. 6.57 ± 8.46 U/l, p = 0.01). Right ventricular involvement was less pronounced in the non-catecholamine support patient-group (18.2%, n = 17 vs. 42.85%, n = 9, p = 0.02).
In-hospital outcome
Data detailing in-hospital events and treatment strategies adopted for our study population suggested that patients suffering from hemodynamic compromise and requiring catecholamine support had a significantly increased incidence of life-threatening arrhythmias (33.3%, n = 7 vs. 6.4%, n = 6, p < 0.01) as well as cardiogenic shock (85.7%, n = 18 vs. 4.3%, n = 4, p < 0.01) and often required admission to an intensive care unit with longer stays (9.5 ± 11.3 days vs. 3.2 ± 3.5 days, p < 0.01). Rates of in-hospital death were higher among patients receiving catecholamine support (28.5%, n = 6 vs. 3.2%, n = 3, p < 0.01). Non-invasive positive pressure ventilation, endotracheal intubation and cardiopulmonary resuscitation procedures were practised significantly more often in patients constituting this group, Table 2.
Table 2.
In-hospital events and treatment strategy
| Variables |
No catecholamines
(n = 93) |
catecholamines
(n = 21) |
p value* |
|---|---|---|---|
| Life-threatening arrhythmia | 6 (6.45) | 7 (33.33) | < 0.01 |
| NPPV and intubation | 21 (22.5) | 18 (85.7) | < 0.01 |
| Resuscitation | 3 (3.22) | 6 (28.57) | < 0.01 |
| Defibrillator-Implantation | 1 (1.0) | 1 (4.7) | 0.33 |
| VA-ECMO | 0 (0) | 1 (4.7) | 0.18 |
| Admission to ICU, length of stay | 3.24 ± 3.59 | 9.57 ± 11.32 | < 0.01 |
| In-hospital death | 3 (3.2) | 6 (28.5) | < 0.01 |
| Thromboembolic events | 10 (10.75) | 4 (19.04) | 0.29 |
| Acquired Long QTs | 61 (65.59) | 12 (57.14) | 0.41 |
| Cardiogenic Shock | 4 (4.30) | 18 (85.71) | < 0.01 |
*p values for the comparison between no catecholamines and catecholamines; NPPV Noninvasive positive pressure ventilation, VA-ECMO Veno-arterial extracorporal membrane oxygenation, ICU Intermediate care unit
The bolded indication highlight significant values
Long-term follow-up
TTS patients receiving catecholamine support registered significantly higher 30-day mortality rates as compared to the clinically stable patient (57.14%, n = 12 vs.17.2%, n = 16, p < 0.01). Furthermore, these patients showed an ongoing increased risk of death beyond the first 30-days after hospital admission resulting in considerably higher long-term mortality-rates (80.95%, n = 17 vs. 38.70%, n = 36, p < 0.01); Table 3, Fig. 2. In a Cox univariate analysis EF ≤35% (HR 4.8, 95% CI 2.2–104; p < 0.01), male gender (HR 2.6, 95% CI 1.2–5.7; p 0.01) and use of positive inotropic agents (HR 3.9, 95% CI 1.9–7.9; p < 0.01) were associated with an adverse outcome. In comparison, a multivariate Cox regression analysis attributed EF ≤ 35% (HR 3.6, 95% CI 1.6–8.1; p < 0.01) and use of positive inotropic agents (HR 2.2, 95% CI 1.0–4.8; p 0.04) as independent predictors of the adverse outcome, Table 4. The various causes of death have been illustrated in Table 5.
Table 3.
Outcome (mortality) in TTS patients
| Variables | No catecholamines (n = 93) |
catecholamines
(n = 21) |
Relative risk (95% CI) | p value * |
|---|---|---|---|---|
| In-hospital mortality | 3 (3.22) | 6 (28.57) | (1.0–6.5) | < 0.01 |
| 30-day mortality | 3 (2.15) | 6 (28.57) | (1.0–6.5) | < 0.01 |
| 1-year mortality | 6 (6.45) | 8 (38.09) | (1.1–3.7) | < 0.01 |
| 2-year mortality | 11 (11.82) | 10 (47.61) | (1.1–2.5) | < 0.01 |
| 3-year mortality | 12 (12.90) | 11 (52.38) | (1.1–2.5) | < 0.01 |
| 4-year mortality | 18 (19.35) | 11 (52.38) | (1.0–1.9) | < 0.01 |
| Long-term mortality | 20 (21.50) | 13 (61.90) | (1.1–2.0) | < 0.01 |
*p values for the comparison between no catecholamines and catecholamines
Fig. 2.
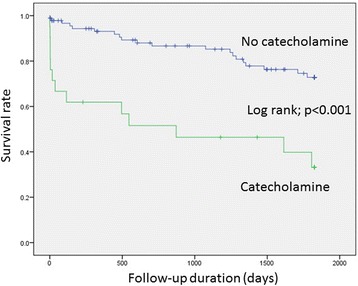
Log-rank and survival rates of patients treated and not treated with catecholamines
Table 4.
Multivariate analysis for the end point (all-cause mortality)
| Univariate analysis | Multivariate analysisa) | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P-value | HR | 95% CI | P-value | |
| Male | 2.6 | 1.2–5.7 | 0.01 | 1.8 | 0.8–4.0 | 0.14 |
| EF ≤ 35% | 4.8 | 2.2–104 | < 0.01 | 3.6 | 1.6–8.1 | < 0.01 |
| Emotionalerstress | 0.4 | 0.1–1.1 | 0.10 | |||
| Inotropic drugs | 3.9 | 1.9–7.9 | < 0.01 | 2.2 | 1.0–4.8 | 0.04 |
| Diabetes mellitus Typ II | 1.0 | 0.7–1.4 | 0.81 | |||
| Hypertension | 0.9 | 0.7–1.2 | 0.64 | |||
| Apical ballooning | 1.1 | 0.8–1.4 | 0.39 | |||
| History of cancer | 1.7 | 0.7–4.2 | 0.21 | |||
| Smoking | 0.7 | 0.3–1.6 | 0.49 | |||
HR hazard ratio, EF ejection fraction, CRP c-reactive protein, GFR glomerular filtration rate
aOnly the following variables with significant effects in univariate analysis were analyzed by multivariate Cox regression: Male, EF ≤ 35%, Inotropic drugs
The bolded indication highlight significant values
Table 5.
All-Cause of death
| In-hospital mortality | |
| 1. Cardiac cause including cardiogenic shock and life-threatening arrhythmia (n = 6) 2. Malignoma (n = 1) 3. Neurological cause (n = 2) | |
| Out of hospital mortality | |
| 1. Cardiac cause including cardiogenic shock and life-threatening arrhythmia (n = 4) 2. Malignoma (n = 6) 3. Sepsis (n = 4) 4. Kidney failure (n = 2) 5. Pulmonary cause (n = 2) 6. Unknown cause (n = 6) |
Discussion
The principal foundation of this study was to determine the role and influence of catecholamine therapy in the treatment of the hemodynamically unstable TTS patient. At the outset, patients receiving catecholamine support showed higher degrees of circulatory and cardiac compromise, and the course of disease was often complicated by the occurrence of different TTS-associated complications. This group of patients also demonstrated poorer in-hospital outcomes and had higher long-term mortality rates as compared to the group of patients not receiving any catecholamine support therapy. It could therefore be inferred that circulatory support in the form of catecholamines entails a poorer outcome for the TTS patient. A pertinent question arises when debating the role of catecholamines exacerbating the mortality risk in such a clinical scenario solely on the basis of the pathophysiology of the syndrome. All patients, irrelevant of diagnosis, requiring catecholamine support constitute a clinically compromised group, however, do TTS patients in circulatory or cardiac shock suffer from additional drawbacks due to this line of management? Our results indicate that contemporary circulatory support drugs like catecholamines additionally exacerbates the risk of mortality in a TTS patient. This study is probably the first of many to follow, that has attempted to express this distinct correlation. Although, many studies have attributed some form of catecholamine toxicity leading to the pathophysiological evolution of TTS, we shall explore this line of discussion further, considering the potential impact on current treatment strategies.
A detailed research of recently published literature highlights the several hypotheses which have been postulated to explain the pathogenesis of TTS. These mechanisms essentially entail the possibility of coronary microvascular dysfunction, coronary artery spasm, catecholamine-induced myocardial stunning, acute LV outflow obstruction, acute increased ventricular afterload, myocardial microinfarction or abnormalities in cardiac fatty acid metabolism influencing the development of TTS [15].
A common link serving these several theories can be construed with the consistent demonstration of some form of microvascular dysfunction among all TTS patients. The research work conducted by Uchida et al. could successfully exhibit the presence of extensive endothelial apoptosis in myocardial biopsies [18] while Afonso et al. demonstrated circulatory disturbances in myocardial contrast echocardiography [19]. Abnormalities associated with endothelium dependent vasodilatation, excessive vasoconstriction and impairment of myocardial perfusion have been associated with coronary microvascular dysfunction seen in TTS patients [20]. The additional demonstration of regional contraction band necrosis, inflammatory cell inflammation and localised fibrosis, all attributed to direct catecholamine toxicity, further corroborates this theory [17, 21]. Interesting results interpreted from the research of Morel et al. suggested that an increase in C-reactive protein levels and white blood cell counts corresponded to increased levels of catecholamines in TTS patients [22]. The raised levels could in theory initiate a systemic inflammation mediated by cytokines like TNF-alpha and interleukin-6, explaining the observation of myocardial oedema in cardiac MRI [23]. In animal models of TTS, as prepared by Paur et al., the use of high bolus doses of catecholamines has simulated LV apical ballooning [24]. Additional studies by Wittstein et al., proving increased levels of circulating catecholamines in TTS patients as compared to those with myocardial infarction, as well as the theory of “stimulus trafficking” (involving a switch in intracellular signal trafficking from Gs protein to Gi protein) proposed by Lyon et al. have all given credence to the hypothesised pathogenic role of catecholamines in the development of TTS [24–26].
Although, these above-mentioned studies effectively hint at a definitive pathophysiological role played by catecholamines in the evolution of the syndrome, they fall short of explaining the potential effects of exogenous catecholamines in exacerbating a case of existing TTS.
A detailed analysis of our published research in this respect revealed that in-hospital events as well as short- and long-term mortality rates among TTS patients diagnosed with a significantly reduced LVEF on admission were significantly higher [27, 28]. We also showed that rates of in-hospital events and short- as well as long-term mortality rates were significantly higher in TTS patients suffering from arrhythmias such as atrial fibrillation [29, 30]. Although, such clinical scenarios do place the TTS patient at the worse end of the spectrum, it does not effectively explain the additional deleterious effects observed when patients received exogenous catecholamines as a form of therapy. An extrapolation of our data suggests reduced LVEF and use of positive inotropic agents as independent predictors of adverse outcome. A plausible explanation for this observation is perhaps the reactivation of catecholamine receptors or their downstream molecular pathways in the acute phase of TTS, which exacerbates the effects of the syndrome.
Our study has significant clinical implications. The essential role of catecholamines in the treatment of circulatory compromise has been consistently validated in the past, however, its use in TTS patients is now certainly questionable. Considering the pathophysiology of the syndrome, it would be pertinent to avoid any sort of catecholamine therapy for such patients. The Heart Failure Association of the European Society of Cardiology has recommended the avoidance or withdrawal of exogenous catecholamines as they could probably prolong or exacerbate the acute phase of the syndrome by activation of catecholamine receptors or their downstream molecular pathways [31]. It is for this reason that experts have suggested the early use of left ventricular assist device (LVAD) or extracorporeal membrane oxygenation (ECMO) as a bridge to recovery in highly unstable patients. Although treatment with levosimendan in this scenario is controversial, the absence of mechanical support may necessitate its use in certain scenarios [15].
This study clearly highlights the pitfalls associated with catecholamine use in patients suffering from circulatory compromise. The observation that most patients did not noticeably profit from this line of management and consistently suffered from poorer clinical outcomes with higher long-term mortality rates cements further support to recently postulated hypotheses and current recommendations for clinical management.
Study limitations
This study was limited by its single-center retrospective observational study design, which included patients admitted over the period of 13 years. There was insufficient data detailing the proposed limits and quantified catecholamine doses used in these patients, furthermore, preventing the definitive assessment of the prognostic impact of different treatment strategies such as ECMO and intra-aortic balloon pump (IABP).
Conclusion
This study equivocally suggests that TTS patients receiving catecholamine therapy show higher grades of circulatory and cardiac compromise, have poorer in-hospital outcomes and demonstrate higher long-term mortality rates in comparison to patients not receiving any form of catecholamine support. Although, these patients could in effect be suffering from a severe form of TTS, the interplay between the several mechanisms involved in the pathogenesis of this syndrome dictates the planning of therapeutic strategies precluding exogenous catecholamine use.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
Data and Supplementary material is attached herewith.
Abbreviations
- ACS
Acute Coronary Syndrome
- ECMO
Extracorporeal membrane oxygenation
- HPA
Hypothalamic-pituitary-adrenal axis
- IABP
Intra-aortic balloon pump
- ICU
Intensive care unit
- LV
Left ventricle
- LVAD
Left ventricular assist device
- LVEF
Left ventricular ejection fraction
- RV
Right ventricle
- TTS
Takotsubo Syndrome
Authors’ contributions
UA and IEB conceived the study, participated in its design and coordination, participated in data analysis and interpretation and helped to draft and revise the manuscript for important intellectual content. CF participated in the study design and coordination, data acquisition and analysis and helped to draft the manuscript for important intellectual content. MBe participated in the study design and coordination, data acquisition and analysis and helped to draft the manuscript for important intellectual content. KS participated in the study design and coordination, as well as data analysis and revised the manuscript. SB helped to draft and revise the manuscript for important intellectual content after critically analysing and interpreting the data. AH helped to draft and revise the manuscript for important intellectual content after critically analysing and interpreting the data. ET participated in the study design and coordination, as well as data analysis and revised the manuscript. MBo participated in the study design and coordination, as well as data acquisition and revised the manuscript for important intellectual content. IA conceived the study, participated in its design and coordination, participated in data analysis and interpretation and helped to draft and revise the manuscript for important intellectual content. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Approved by the medical ethics committee of the Faculty of Medicine in Mannheim, University of Heidelberg, Germany. As this was a retrospective study, the ethics committee waivered the need for informed consent.
Consent for publication
As this was a retrospective study, consent from included patients was not required.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Uzair Ansari, Phone: (+49) 621 383 5229, Email: uzair.ansari@umm.de.
Ibrahim El-Battrawy, Email: ibrahim.el-battrawy@medma.uni-heidelberg.de.
Christian Fastner, Email: christian.fastner@umm.de.
Michael Behnes, Email: michael.behnes@umm.de.
Katherine Sattler, Email: katherine.sattler@umm.de.
Aydin Huseynov, Email: aydin.huseynov@umm.de.
Stefan Baumann, Email: stefan.baumann@umm.de.
Erol Tülümen, Email: erol.tueluemen@umm.de.
Martin Borggrefe, Email: martin.borggrefe@umm.de.
Ibrahim Akin, Email: ibrahim.akin@umm.de.
References
- 1.Hurst RT, Prasad A, Askew JW, III, Sengupta PP, Tajik AJ. Takotsubo cardio- myopathy: a unique cardiomyopathy with variable ventricular morphology. JACC Cardiovasc Imaging. 2010;3:641–649. doi: 10.1016/j.jcmg.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 2.Medeiros K, O’Connor MJ, Baicu CF, et al. Systolic and diastolic mechanics in stress cardiomyopathy. Circulation. 2014;129:1659–1667. doi: 10.1161/CIRCULATIONAHA.113.002781. [DOI] [PubMed] [Google Scholar]
- 3.Prasad A. Apical ballooning syndrome: an important differential diagnosis of acute myocardial infarction. Circulation. 2007;115:e56–e59. doi: 10.1161/CIRCULATIONAHA.106.669341. [DOI] [PubMed] [Google Scholar]
- 4.Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, Moss AJ, Seidman CE, Young JB. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association scientific statement from the council on clinical cardiology, heart failure and transplantation committee; quality of care and outcomes research and functional genomics and translational biology interdisciplinary working groups; and council on epidemiology and prevention. Circulation. 2006;113:1807–1816. doi: 10.1161/CIRCULATIONAHA.106.174287. [DOI] [PubMed] [Google Scholar]
- 5.Sharkey SW, Lesser JR, Maron MS, Maron BJ. Why not just call it takotsubo cardiomyopathy: a discussion of nomenclature. J Am Coll Cardiol. 2011;57:1496–1497. doi: 10.1016/j.jacc.2010.11.029. [DOI] [PubMed] [Google Scholar]
- 6.El-Battrawy I, Behnes M, Ansari U, Hillenbrand D, Haghi D, Hoffmann U, Akin I. Comparison and outcome analysis of patients with apical and non-apical takotsubo cardiomyopathy. QJM: An International Journal of Medicine. 2016;1–6. [DOI] [PubMed]
- 7.Owa M, Aizawa K, Urasawa N, Ichinose H, Yamamoto K, Karasawa K, Kagoshima M, Koyama J, Ikeda S. Emotional stress-induced ‘ampulla cardiomyopathy’: discrepancy between the metabolic and sympathetic innervation imag- ing performed during the recovery course. Jpn Circ J. 2001;65:349–352. doi: 10.1253/jcj.65.349. [DOI] [PubMed] [Google Scholar]
- 8.Mukherjee A, Sunkel-Laing B, Dewhurst N. ‘Broken heart’ syndrome in Scotland: a case of Takotsubo cardiomyopathy in a recently widowed lady. Scott Med J. 2013;58:e15–e19. doi: 10.1177/0036933012474605. [DOI] [PubMed] [Google Scholar]
- 9.Haghi D, Athanasiadis A, Papavassiliu T, Suselbeck T, Fluechter S, Mahrholdt H, Borggrefe M, Sechtem U. Right ventricular involvement in Takotsubo cardiomyopathy. Eur Heart J. 2006;27:2433–2439. doi: 10.1093/eurheartj/ehl274. [DOI] [PubMed] [Google Scholar]
- 10.Kurowski V, Kaiser A, von Hof K, Killermann DP, Mayer B, Hartmann F, Schunkert H, Radke PW. Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest. 2007;132:809–816. doi: 10.1378/chest.07-0608. [DOI] [PubMed] [Google Scholar]
- 11.Ennezat PV, Pesenti-Rossi D, Aubert JM, Rachenne V, Bauchart JJ, Auffray JL, Logeart D, Cohen-Solal A, Asseman P. Transient left ventricular basal dysfunction without coronary stenosis in acute cerebral disorders: a novel heart syndrome (inverted Takotsubo) Echocardiography. 2005;22:599–602. doi: 10.1111/j.1540-8175.2005.40046.x. [DOI] [PubMed] [Google Scholar]
- 12.Van deWalle SO, Gevaert SA, Gheeraert PJ, De Pauw M, Gillebert TC. Transient stress-induced cardiomyopathy with an ‘inverted takotsubo’ contractile pattern. Mayo Clin Proc. 2006;81:1499–1502. doi: 10.4065/81.11.1499. [DOI] [PubMed] [Google Scholar]
- 13.Cacciotti L, Camastra GS, Beni S, Giannantoni P, Musaro S, Proietti I, De Angelis L, Semeraro R, Ansalone GA. New variant of Tako-tsubo cardiomyopathy: transient mid-ventricular ballooning. J Cardiovasc Med. 2007;8:1052–1054. doi: 10.2459/JCM.0b013e32803cab4a. [DOI] [PubMed] [Google Scholar]
- 14.Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, Lüscher TF. Clinical features and outcomes of Takotsubo (stress) cardiomyopathy. N Engl J Med. 2015;373(10):929–938. doi: 10.1056/NEJMoa1406761. [DOI] [PubMed] [Google Scholar]
- 15.Lyon AR, Bossone E, Schneider B, Sechtem U, Citro R, Underwood SR, Omerovic E. Current state of knowledge on Takotsubo syndrome: a position statement from the taskforce on Takotsubo syndrome of the heart failure Association of the European Society of cardiology. Eur J Heart Fail. 2016;18(1):8–27. doi: 10.1002/ejhf.424. [DOI] [PubMed] [Google Scholar]
- 16.Wittstein IS, Thiemann DR, Lima JAC, Baughman KL, Schulman SP, Gerstenblith G, Wu KC, Rade JJ, Bivalacqua TJ, Champion HC. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539–548. doi: 10.1056/NEJMoa043046. [DOI] [PubMed] [Google Scholar]
- 17.Khullar M, Datta BN, Wahi PL, Chakravarti RN. Catecholamine-induced experimental cardiomyopathy - a histopathological, histochemical and ultrastructural study. Indian Heart J 1989; 41: 307–313 [PMID: 2599540]. [PubMed]
- 18.Uchida Y, Egami H, Uchida Y, Sakurai T, Kanai M, Shirai S, Nakagawa O, Oshima T. Possible participation of endothelial cell apoptosis of coronary microvessels in the genesis of Takotsubo cardiomyopathy. Clin Cardiol. 2010;33 [DOI] [PMC free article] [PubMed]
- 19.Afonso L, Bachour K, Awad K, Sandidge G. Takotsubo cardiomyopathy: pathogenetic insights and myocardial perfusion kinetics using myocardial contrast echocardiography. Eur J Echocardiogr. 2008;9:849–854. doi: 10.1093/ejechocard/jen192. [DOI] [PubMed] [Google Scholar]
- 20.Galiuto L, De Caterina AR, Porfidia A, Paraggio L, Barchetta S, Locorotondo G, Rebuzzi AG, Crea F. Reversible coronary microvascular dysfunction: a common pathogenetic mechanism in apical ballooning or Tako-Tsubo syndrome. Eur Heart J 2010; 31: 1319–1327 [PMID: 20215125 10.1093/%20eurheartj/ehq039. [DOI] [PubMed]
- 21.Nef HM, Möllmann H, Kostin S, Troidl C, Voss S, Weber M, Dill T, Rolf A, Brandt R, Hamm CW, Elsässer A. Takotsubo cardiomyopathy: intra-individual structural analysis in the acute phase and after functional recovery. Eur Heart J 2007; 28: 2456–2464 [PMID: 17395683 10.1093/eurheartj/%20ehl570]. [DOI] [PubMed]
- 22.Morel O, Sauer F, Imperiale A, Cimarelli S, Blondet C, Jesel L, Trinh A, De Poli F, Ohlmann P, Constantinesco A, Bareiss P. Importance of inflammation and neurohumoral activation in Takotsubo cardiomyopathy. J Card Fail 2009; 15: 206–213 [PMID: 19327622 10.1016/j.cardfail.2008.10.031]. [DOI] [PubMed]
- 23.Avegliano G, Huguet M, Costabel JP, Ronderos R, Bijnens B, Kuschnir P, Thierer J, Tobón-Gomez C, Martinez GO, Frangi A. Morphologic pattern of late gadolinium enhancement in Takotsubo cardiomyopathy detected by early cardiovascular magnetic resonance. Clin Cardiol 2011; 34: 178–182 [PMID: 21400545 10.1002/clc.20877. [DOI] [PMC free article] [PubMed]
- 24.Paur H, Wright PT, Sikkel MB, Tranter MH, Mansfield C, O’Gara P, et al. High levels of circulating epinephrine trigger apical cardiodepression in a β2- adrenergic receptor/Gi-dependent manner: a new model of Takotsubo cardiomyopathy. Circulation. 2012;126:697–706. doi: 10.1161/CIRCULATIONAHA.112.111591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lyon AR, Rees PSC, Prasad S, Poole-Wilson PA, Harding SE. Stress (Takotsubo) cardiomyopathy—a novel pathophysiological hypothesis to explain catecholamine-induced acute myocardial stunning. Nat Clin Pract CardiovascMed. 2008;5:22–29. doi: 10.1038/ncpcardio1066. [DOI] [PubMed] [Google Scholar]
- 26.Scantlebury D, Prasad A. Diagnosis of Takotsubo cardiomyopathy. Circ J. 2014;78(9):2129–2139. doi: 10.1253/circj.CJ-14-0859. [DOI] [PubMed] [Google Scholar]
- 27.El-Battrawy I, Ansari U, Lang S, Behnes M, Schramm K, Fastner C, Zhou X, Kuschyk J, Tülümen E, Röger S, et al. Impact and management of left ventricular function on the prognosis of Takotsubo syndrome. Eur J Clin Investig. 2017;47:477–485. doi: 10.1111/eci.12768. [DOI] [PubMed] [Google Scholar]
- 28.Becher T, El-Battrawy I, Baumann S, Fastner C, Behnes M, Loßnitzer D, Elmas E, Hoffmann U, Papavassiliu T, Kuschyk J, et al. Characteristics and long-term outcome of right ventricular involvement in Takotsubo cardiomyopathy. Int J Cardiol. 2016;220:371–375. doi: 10.1016/j.ijcard.2016.06.240. [DOI] [PubMed] [Google Scholar]
- 29.El-Battrawy I, Lang S, Ansari U, Tülümen E, Schramm K, Fastner C, Zhou X, Hoffmann U, Borggrefe M, Akin I. Prevalence of malignant arrhythmia and sudden cardiac death in takotsubo syndrome Borggrefe, M., Akin, I. Prevalence of malignant arrhythmia and sudden cardiac death in takotsubo syndrome and its management. EP Europace. 2017. https://doi.org/10.1093/europace/eux073 [DOI] [PubMed]
- 30.El-Battrawy I, Lang S, Ansari U, Tülümen E, Schramm K, Fastner C, Zhou X, Hoffmann U, Borggrefe M, Akin I. Prevalence of malignant arrhythmia and sudden cardiac death in takotsubo syndrome and its management. EP Europace. 2017; [DOI] [PubMed]
- 31.Redmond M, Knapp C, Salim M, Shanbhag S, Jaumdally R. Use of vasopressors in Takotsubo cardiomyopathy: a cautionary tale. Br J Anaesth. 2013;110:487–488. doi: 10.1093/bja/aes586. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and Supplementary material is attached herewith.


