Abstract
Background
In 2009, the Benin government introduced a user fee exemption policy for caesarean sections. We analyse this policy with regard to how the existing ideas and institutions related to user fees influenced key steps of the policy cycle and draw lessons that could inform the policy dialogue for universal health coverage in the West African region.
Methods
Following the policy stages model, we analyse the agenda setting, policy formulation and legitimation phase, and assess the implementation fidelity and policy results. We adopted an embedded case study design, using quantitative and qualitative data collected with 13 tools at the national level and in seven hospitals implementing the policy.
Results
We found that the initial political goal of the policy was not to reduce maternal mortality but to eliminate the detention in hospitals of mothers and newborns who cannot pay the user fees by exempting a comprehensive package of maternal health services. We found that the policy development process suffered from inadequate uptake of evidence and that the policy content and process were not completely in harmony with political and public health goals. The initial policy intention clashed with the neoliberal orientation of the political system, the fee recovery principles institutionalised since the Bamako Initiative and the prevailing ideas in favour of user fees. The policymakers did not take these entrenched factors into account. The resulting tension contributed to a benefit package covering only caesarean sections and to the variable implementation and effectiveness of the policy.
Conclusion
The influence of organisational culture in the decision-making processes in the health sector is often ignored but must be considered in the design and implementation of any policy aimed at achieving universal health coverage in West African countries.
Keywords: maternal health, health policies and all other topics, health services research, health systems, child health
Key questions.
What is already known about this topic?
The implementation of user fee exemption policies in West Africa is variable and has led to mixed results in terms of equitable utilisation of quality health services. The main known reasons for the implementation gap are poor planning, inadequate financing and limited control of the discretionary power of providers. Such policies are developed in contexts where the user fee recovery culture has prevailed for decades. Little is known about how this context influences the policy process of user fee exemption policies.
What are the new findings?
This study analyses key steps of the policy cycle using a wide range of quantitative and qualitative data. It describes how policy actors and context shape the policy content and process. It shows that the current ideas and institutions in Benin related to user fees create a pro-user fee organisational culture within the health system that negatively influences policy formulation and its implementation.
Recommendations for policy
This study calls attention to the importance of organisational culture in the decision-making processes in the health sector. This often-ignored dimension of health systems must be considered in the design and implementation of any policy aimed at achieving universal health coverage in West African countries.
Background
In April 2009, the Benin government introduced a user fee exemption policy (UFEP) for caesarean section (CS) for all pregnant women who require this surgical procedure. The government created a national agency (hereafter referred to as the Implementing Agency) to implement this policy in 48 accredited facilities (including 18 non-state-owned facilities). Under this policy, the Implementing Agency pays facilities a fixed sum of XOF100 000 (€152) for each CS, regardless of the socioeconomic status of the woman, the reason for performing the CS, the facility level (primary, secondary or tertiary) or the facility ownership (state owned or non-state owned). The package only includes coverage for the actual CS. Women pay user fees for antenatal care, uncomplicated deliveries and other obstetric and neonatal complications.1
The user fee strategy is ‘a financing mechanism that has two main characteristics: payment is made at the point of service use and there is no risk sharing’.2 User fees were introduced in West Africa by the Bamako Initiative in 1987 and were underpinned by the following assumptions: (1) the strategy increases economic efficiency because scarce resources are allocated to their most valuable use; (2) it enhances accountability of the public sector and makes it more responsive to fluctuating preferences and demands; (3) it allows for cost recovery and increased equity; and (4) it is based on the principle of ‘fairness’ as the user pays only for the goods and services he or she uses.3
User fees still prevail in West Africa: out-of-pocket payments represented between 30%–72% of the total health expenditure in 13 countries in 2014.4 However, international donors and the scientific community are no longer in favour of user fees5 6: user fees constitute a regressive form of healthcare financing, imposing an unaffordable burden on poor households.7 They hinder vulnerable people from the timely use of life-saving health services and contribute to sustaining a vicious cycle of impoverishment.3 8
UFEPs address financial barriers and have the potential to improve access to healthcare. They are being applied to immunisation, contraception, care for HIV and tuberculosis,9 cholera treatment during outbreaks10 and to mother and child healthcare.11 Benin, Burkina Faso, Mali,1 Ghana, Sierra Leone, Senegal12 and Niger13 have all introduced such policies. From Sen’s capability perspective, a UFEP in theory provides ‘additional resources in people’s wallets: free healthcare at the point of delivery. This resource gives them the opportunity to use public health services whenever they feel the need, without being dissuaded by cost’.14 There is growing evidence that UFEPs increase the utilisation of services6 15 and reduce the economic burden of diseases on households.6 16 17 However, several authors called for careful action7 and specific measures to overcome social exclusion and to ensure that the most vulnerable groups have equitable access to resources provided by UFEPs through better policy formulation and policy implementation.18–20 Indeed, in certain cases, UFEPs are poorly implemented, with facilities running out of resources and forced to stop providing services. In other cases, health providers continue charging (partial) user fees.21 22
The challenges related to implementation of policies in general,23 and of UFEPs specifically, are insufficiently documented. Scholars have identified factors at the national level, including poor planning, insufficient allocation of resources, delays in distribution of resources and insufficient communication.21 24 At the operational level, the concept of ‘street level bureaucracy’ has been used to explain persistent charging of fees.25 26 However, little is known about the ideas and institutions that inform the choices of policy actors. Rarely studied have been the role of shared values, beliefs and assumptions within the dominant organisational culture, nor the role of trust or power dynamics27 28 in shaping the different stages of the policy cycle.
This paper contributes to filling this gap by analysing the agenda setting, the formulation and the legitimation of the UFEP for CS in Benin (hereafter called the Policy). Second, it assesses the extent to which the Policy was implemented and, third, it evaluates the results.
This study was part of the FEMHealth research programme, which ran from January 2011 to December 2013 in Mali, Benin, Burkina Faso and Morocco. FEMHealth adopted a multicountry case study design.29 It used 13 data collection tools to capture a wide range of qualitative and quantitative data on the policymaking process, the implementation and the effects of fee exemption policies at national, regional and district level. Other results and lessons from FEMHealth are published elsewhere.1 30 31
Methods
Study design, context and analytical framework
We adopted a case study design32 as this allowed us to explore different aspects of the ‘natural history’ of the UFEP, from the agenda-setting phase to the results, including the underlying processes.29 We defined the case as the policy cycle related to the UFEP for CS in Benin. The study sites were health districts. Benin is subdivided into 34 health districts, of which we purposively selected five in order to ensure maximum variation in terms of population wealth, availability and utilisation of health facilities prior to the Policy. To do so, we grouped the health districts using Ward’s method of hierarchical clustering33 34 in three categories according to the characteristics defined in table 1. In each category, we selected one or two health districts with characteristics closest to the mean value of the category. The five health districts have seven health facilities that implement the Policy.
Table 1.
Facilities selected in Benin as subunits of analysis for the FEMHealth research project
| Category 1 | Category 2 | Category 3 | |
| Wealth index (100—mean index of poverty, %) |
Low 54.4 |
Moderate 67 |
High 75 |
| Availability of health facilities (mean radius of coverage of health centres, km) |
Moderate (5.1) |
Low (12.4) |
High (2.1) |
| Utilisation of health services (proportion of institutional deliveries, %) |
Moderate (72.1) |
Low (56.3) |
High (85.5) |
| Health district selected | Health District of Come-Grand-Popo-Houéyogbe-Bopa Health District of Dassa-Zoume-Glazoué |
Health District of Nikki-Kalalé-Pèrèrè Health District of Bembèrèkè-Sinendé |
Health district of Porto-Novo-Aguegue-Seme-Kpodji |
| Hospitals implementing the user fee exemption for caesarean sections policy within the health districts selected | District hospital of Come-Grand-Popo-Houeyogbe-Bopa District hospital of Dassa-Zoume-Glazoué |
District hospital of Nikki-Kalalé-Pèrèrè District hospital of Bembèrèkè |
Regional hospital of Ouémé-Plateau Hospital El-Fatheh Hospital Bon Samaritain |
The population of Benin is 10 million, and in 2011, the total fertility rate was 4.9.35 In 2011, 87% of deliveries took place in health facilities, and 5.4% of all deliveries were by CS.35 The maternal mortality ratio in 2015 was estimated at 405 deaths per 100 000 live births.36 There are about 2600 state-owned and non-state-owned health centres that provide maternal healthcare and about 40 state-owned and non-state-owned hospitals.37
To describe the Policy in general, we adopted the policy-making stages model.38 We used Kingdon’s multiple stream model39 to analyse the agenda-setting phase of the Policy. We applied the policy triangle framework with its four components (policy context, actors, process and content)40 to analyse the policy formulation and the policy legitimisation phase. We then assessed the actual policy implementation and the implementation fidelity (defined as ‘the degree to which an intervention was implemented as it was designed in an original protocol, plan, or policy’).41 For the latter, we used two variables: (1) the number of CS items provided for free (in accordance to the Policy) and (2) the remaining fees related to a CS. Finally, we assessed the effectiveness of the Policy using three methods:
analysis of the trends in the CS rate, using routine health data from 2001 to 2015
assessment of financial protection against catastrophic health expenditure under the free CS policy, using as proxy the fees charged for women who delivered by CS as a proportion of gross domestic product (GDP) per capita
assessment of equity in access to care under the Policy, for which we analysed the trends in CS rates for the different socioeconomic groups.
Data collection methods
The qualitative data collection methods included document review (policy documents, contemporary history documents and media publications) and in-depth semistructured interviews. Interviewees were purposively selected to include policy makers and implementers at all levels of the health system, as well as patients and community representatives. The above described models and frameworks guided the initial selection of documents that was expanded based on the preliminary findings. All qualitative data were collected in 2012 and 2013 by four researchers with a medical and/or socioanthropological background.
The quantitative data collection methods included structured data extraction from routine medical records of the seven selected facilities and from annual health statistics reports, which we used to assess national CS rates from 2001 to 2015. Data from four consecutive Demographic and Health Surveys (1996, 2001, 2006 and 2011–2012) were analysed to measure the population-based CS rates, stratified by relative wealth. A financial flow tracking study documented the budgets allocated to the Policy, the actual expenditure and the adequacy of the payments to the health facilities. We also carried out a costing study at facility level to assess the cost of performing a CS, for which we used interviews with facility managers and data extraction from medical records of a sample of 30 CS at each facility. The 30 files were selected by applying a systematic sampling technique to the list of the 150 most recent CS performed in each facility. We conducted exit interviews (EIs) with a total of 294 women who delivered by CS to collect data on the actual user fees they paid during their hospitalisation.
Data analysis methods
We conducted an iterative qualitative analysis that started during the data collection, whereby new findings and analytical insights were used to adapt the data collection tools. All interviews were recorded and transcribed verbatim. Qualitative data were entered in a NVIVO V.10 database to facilitate data management. We adopted a thematic analysis approach, inspired but not constrained by the models and frameworks presented above.
The CS rate was estimated by dividing the number of CS by the expected total number of deliveries per year, providing a proxy of the population-based CS rate nationwide. A segmented linear regression model using the Prais-Winsten method was used to examine these rates before and after the implementation of the Policy in Stata V.14, controlling for secular trends and adjusting for autocorrelation.42 We used Microsoft Excel 2011 (V.14.6.7) for all other quantitative analysis. Table 2 presents a summary of objectives, key research questions, data sources, data collection methods and analytical approaches. A more detailed description of the different methods used within the FEMHealth study has been presented elsewhere.43
Table 2.
Summary of objectives, key research questions, data collection techniques, data sources and analytical approaches used
| Subparts of the objectives | Key research question Key themes |
Data collection techniques/tools | Level, data source and sample | Analysis |
| Analysing the policy agenda setting | How did user fee for CSs get the government’s attention, as a priority problem to address? Problem stream, policy stream and political stream |
Semistructured interviews with policymakers Observation in meetings using an observation grid Document review |
Actors at the national, regional and international levels 1 conference and 10 agency meetings observed 24 informants interviewed 32 online media publications screened |
Thematic analysis |
| Analysing the policy formulation and legitimation | How were the objectives of the policy defined? How was the cost calculated? What effects were anticipated? How were the policy instruments selected? How did policy makers ensure support for the policy and its instruments? Context, actors, process and content of the policy |
Observation in meetings using an observation grid Structured discussion with key informants Document review Observation of implementing facilities |
Actors at the national, regional and international levels 1 conference and 10 agency meetings observed 24 informants interviewed 7 implementing hospitals observed |
Thematic analysis |
| Assessing the policy implementation fidelity | To what extent was the Policy implemented as it was designed in the original policy decree? Number of CS elements provided for free (in accordance with the policy)
Remaining charge for households for a CS |
Document review Semistructured interview with key informants Exit surveys Routine data extraction |
Policy documents at national, regional and local levels Facility health routine data supports Regional and district medical officers, health workers, facility users and community representatives |
Triangulation of the data from the different sources and transformation of qualitative data into quantitative data to compute the number of CSs elements provided for free (in accordance with the policy). A descriptive statistical analysis has been conducted to compute the remaining charge for households for a CS. |
| Assessing the policy results | To what extent was the policy successful in relation to its desired and expected effects? Impact on CS utilisation Remaining fees charged for women who delivered by CS as a proportion of GDP per capita Equity of utilisation: trends in CS rates for different socioeconomic groups |
Document review and data extraction Exit interviews (EI) |
Routine data in national health statistics from 2001 to 2015 Demographic and Health Survey (DHS) data for Benin from 1993 to 2011 (n=36 375) EI conducted with 294 with a CS |
Interrupted Time Series particularly the Segmented regression analysis41, of data from routine annual statistics and DHS data The model was specified as: Yt=β0 + β1*time + β2*policy + β3*postslope + εt Yt=outcome variable (caesarean delivery) at time t; time is a continuous variable; policy is a dummy variable indicating whether or not the policy has been implemented at time t; and postslope is coded 0 up to the last point before the introduction of the policy and coded sequentially from 1 thereafter. Analysis of the EI extracted specific data related to costs for a CS delivery for families, inside and outside hospitals. The expenditures have been computed as a proportion of the GDP per capita in Benin in 2012. The GDP per capita data in local current unit are extracted from the World Bank Open Data website. We used Microsoft Excel 2011 (V.14.6.7) for these analyses. |
CS, caesarean section; GDP, gross domestic product.
Results
How was the Policy put on the agenda?
In December 2008, Thomas Boni Yayi, president of Benin, signed the decree that institutionalised the Policy. Framed in the model of Kingdon,39 this ended a 3-year process in which the problem stream, the policy stream and the political stream were pulled together in a window of opportunity.
Problem stream: detention of women and their newborn babies in hospitals
User fees were formally introduced in Benin in 1988 in line with the cost-sharing principle of the Bamako Initiative.44 It soon became apparent, however, that many patients were unable to pay their bills. In response, facility managers frequently detained patients (including women and their newborns) after discharge until the bills were settled. They justified the recovery of fees on financial grounds. Patient detention therefore remained a component of the problem stream for a considerable period, though it was only sporadically documented45 before 2006, when Thomas Boni Yayi was elected as president. While visiting a hospital in northern Benin, he met women who had been detained in the hospital for several weeks. The president drew attention to this problem and newspapers began reporting on the issue.
Political stream, policy stream and window of opportunity
The issue entered the political stream when the president committed himself to addressing the problem in front of the media, proposing to exempt user fees for children under 5 years of age. At that moment, UFEP was an option in the policy stream in Benin and across the West African region, where it was already applied to preventive and curative care within HIV, tuberculosis and immunisation programmes.46 The newly elected president created a window of opportunity to deliver on his electoral promises when he proposed UFEP for children under 5 years. To assist in the formulation of the Policy, he instigated a process of evidence gathering and a participatory approach, which included a series of workshops and a feasibility study conducted by a private consultancy agency.
Emergence of the focus on CS
During one of the workshops, it was decided that pregnant women should be exempted from fees as well: ‘Child health starts from conception and necessarily entails antenatal care, emergency obstetric and neonatal care, and post-natal care to ensure the survival of the child’.47 The report presented a cost estimation for a comprehensive UFEP that included mothers and newborns,47 based on the tariffs of the different services to be exempted. However, it considered only state-owned facilities and took into account only the direct costs paid for a CS by users, not costs incurred by the facilities, based on the assumption that the government already supported the latter through subsidies. The policy’s cost was estimated at €61 million per year, of which about €3 million was for a UFEP for CS only. At the end of this process, the government decided to focus on exempting costs for CS only for financial reasons.
How was the Policy formulated and legitimised?
To analyse the process of policy formulation and legitimisation, we applied the policy triangle framework of Walt and Gilson,40 which includes the policy context, content, process and actors.
The policy context
The political context
The Policy emerged in a specific political context. As an independent newcomer in politics, Thomas Boni Yayi won the second round of elections in 2016 with 75% of the votes.48 His political discourse focused on radical change in governance and created high expectations among the population. At the start of his mandate, he engaged in a wave of ‘strong acts’, of which the introduction of the fee exemption policy was one. In 2009, households contributed 43% of the total health expenditure through out-of-pocket payment (OOP), representing about €12.70 per capita.4 In this context, the Policy would translate to a savings of €152 for households (previously paid as OOP) in the case of a CS. The Policy was considered a political ‘winner’ and a key strategy for consolidating the president’s popularity. Furthermore, it was thought to be a relatively simple policy, which would be easy to communicate and finance.
A clash with the pro-user fee organisational culture of Benin’s health system
The political commitment of the President occurred against the background of a health system with a strong bureaucratic organisational structure49 and what we call in this paper a pro-user fee organisational culture. The latter was founded on a set of ideas and institutions coherently aligned in favour of user fees with four themes, which we will analyse below: (1) a dominant neoliberal ideology; (2) user fees as the main health financing mechanism; (3) institutionalised fee recovery practices; and (4) strongly shared ideas about user fees.
A dominant neoliberal ideology: the current constitution of Benin was developed at the national conference of February 1990, which formally shifted the country from a Marxist-Leninist regime (adopted in November 1974) to a liberal economy.48 50 The conference adopted the first structural adjustment programme, signed by national authorities in June 1989, as the new approach to rebuild the economy of the country.48 51 52 Under the new political regime, individual citizens were to assume the responsibility for health and welfare, and the state accordingly reduced its engagement in the economy and its expenditure through social programmes.53
User fees as the main health financing mechanism: in Benin, fee recovery mechanisms have been piloted since the 1980s,54 for instance through the health development project of Pahou. User fees were introduced formally and nationwide in 1988.55 In 2008, the feasibility report of the Policy requested ‘the preservation of the Bamako Initiative’, stating that ‘Despite this fee exemption policy, the Bamako Initiative must be respected in its form and spirit, and must function as in the past. (…) Care and care inputs are always to be charged and community funding can continue. (…) The State pays all or part of the cost on behalf of users’.47 The State would assume a third party payer role and this was expected to create ‘no disruption to the current system of cost recovery’.47
Institutionalised fee recovery practices: through observations in our study sites and from the document review, we identified several institutionalised fee recovery practices. First, fee payment is a systematic prerequisite for a patient’s access to health facilities, even in case of emergency (‘no cash, no care’). Second, user fee recovery agents, locally called ‘cols verts’ (green collars), use specific procedures to calculate inpatient user fees, trace users and prevent them from not paying. Third, the national annual health statistics reports include an assessment of performance in terms of fee recovery by health districts. Fourth, we found that hospital managers are supposed to meet recurrent expenses related to drugs, consumables and certain payroll elements with user fee revenue. Both healthcare providers and health managers are trained and socialised into developing, implementing and monitoring strategies to recover user fees.
Strongly shared ideas on cost recovery: our analysis shows that there is a widely shared set of ideas related to cost recovery among stakeholders. We found that patients tend to normalise the idea that finding resources to seek care is the responsibility of individuals as illustrated by a pregnant woman saying, ‘if you seek (care) and you don’t have money, you will die and it is your loss’. The blame is rarely put on the State, which is perceived as incapable of financing free care for all. A leader of the midwives’ association referred to this when she expressed her regrets that the population does not have a money-saving culture to face user fees for pregnancy: ‘Normally, we need that culture. A man needs to know that when his wife is pregnant, he has to start a ‘tontine’ (community savings group), for example. And if the woman has a job, and she is pregnant and she is active, she has to start putting money aside’.
We found that policymakers consider user fees as a form of community participation that ‘guarantees the income of health facilities’. They see user fees as an ‘essential complement to public funding, used to compensate for insufficient public funding and to ensure the day-to-day operation of health facilities’. Another view is that free healthcare will be abused and taken advantage of by the population. For instance, an academic leader in maternal health stated that, in the reasoning of the population ‘It is free’ means ‘I can make profit out of it’, which induces a risk of wastage.
The mother and child health context
In 2006, the maternal mortality ratio was 397 deaths per 100 000 live births and the neonatal mortality rate was 32 per 1000 live births. The institutional birth attendance rate was 78% and the CS rate was 4%.56 In 2009, nationwide efforts were initiated to improve access to family planning, insecticide-treated bed nets, immunisation, vitamin A supplementation, antenatal care, institutional delivery and emergency obstetric and newborn care. Efforts to reduce financial hardship for mothers and newborns included mutual health insurance initiatives, an indigent fund and the free referral of emergencies within a district. However, these initiatives were poorly implemented.47 57
Legitimisation of the policy
Communication played a key role in the process of legitimising the Policy vis-à-vis the (inter)national stakeholders. Two decrees (Decree N° 2008–730 of the 22 December 2008 and Decree N°2009–096 of the 30 March 2009) signed by the president provided legitimacy to the Policy as well as some implementation guidance. Other decrees (Decree 2009–146 of the 30 April 2009 and Decree 2009–455 of the 7 September 2009) allocated responsibilities of leadership for the Policy. However, the Policy was not enacted in law and therefore remains vulnerable to political change. We found that the government extensively involved the media to inform the population about the Policy. The president engaged himself and high-level government officials in promoting the Policy with regular visits to implementing facilities. Several providers reported being surprised and put under pressure to comply with the Policy, since the population was informed and was expecting immediate benefits.
While the politicians’ discourse focused on improvement of social protection with this policy, some technical policy actors from the Ministry of Health (MoH) described this policy as a means to reduce maternal and neonatal morbidity and mortality. Their argument was that despite a high proportion of institutional deliveries, the CS rate (3.7%) was very low. The MoH staff assumed that removing financial barriers would lead to a higher utilisation of CS among women needing this life-saving intervention. Benin’s international partners are influential in health decision-making processes and can legitimise national policies by means of their technical or financial support. For example, the share of external resources in the total health expenditure amounted to 24% in 2008 and 2009 and increased to 30% in 2011.4 We found that these actors were quite sceptical of the MoH staff’s argument, questioning the potential of the Policy to improve mother and child health outcomes and doubting the need for a separate Implementing Agency. The international agencies were poorly involved in the policy formulation. They did not provide substantial financial support to the Policy, with the exception of one bilateral partner, which started a 5-year project in 2013 to complement the Policy with other specific interventions to improve quality of CS and neonatal reanimation in accredited hospitals.58
The policy content
As indicated by the official name of the Policy, césarienne gratuite (free CS), the Policy aimed to exempt women from paying any fees for a CS. The decree defines the exempted fees to include the referral of pregnant women from a health centre to the hospital, an intravenous infusion, the consultation fee, the cost of the surgical procedure, the cost of drugs and medical consumables, other hospital expenses and the postoperative check-up.
The feasibility study noticed some variation in the provision of CS and user fee practices in facilities of similar levels across the health system. For instance, the user fee paid in 2008 in district hospitals ranged between €94 and €116. In regional hospitals, it ranged from €90 to €153, and the range was higher still in national university hospitals, from €189 to €317.47 Based on this study, the policymakers considered two options to reimburse the facilities: an actual cost-based reimbursement or a lump sum reimbursement option of €152 for each CS. The latter was perceived as a straightforward method to achieve the political target while addressing the technocrats’ concerns of implementation failure due to high costs. The amount of €152 was estimated as sufficient to cover the costs of a CS in state-owned district and regional hospitals. The same rate was applied to non-state-owned facilities, whose cost structure was not examined in the feasibility study.
How policy actors shaped the content
We found that several actors played key roles in shaping the Policy. As already described, the president placed the issue on the agenda and supported the implementation of the Policy. The MoH’s Directorate of Mother and Child Health played a major technical role during the initial stages of policy formulation. This role was subsequently taken over by the Implementing Agency, headed by a former general secretary of the MoH. His personal experience and influence were critical in aligning the technocrats of the MoH with the political process. A leader of the University Clinic of Gynaecology and Obstetrics represented obstetricians in the process and provided clinical evidence. He was also instrumental in creating support for the adoption of the Policy by the practitioners and, as a relative of the president, yielded considerable influence. The president of the national association of midwives (Association des Sages-Femmes du Bénin) was also involved. Through their technical, political and social networks, these two actors held powerful positions, more so because later they supervised the implementation process as members of the Implementing Agency’s administrative board. Other key actors included the health economists of the private consultancy agency that shaped the policy formulation. Hospital managers were involved to different degrees during all phases of the policy formulation and implementation phases. An association of non-state-owned facilities, namely Association des Œuvres Médicales Privées, Confessionnelles et Sociales au Bénin, was representing 14 of non-state-owned facilities initially selected to implement the Policy. The hospitals belonging to this association negotiated the approval to systematically charge their patients €30 for each CS. As mentioned above, the international partners were sceptical of the Policy and little involved.
Implementation of the policy
The implementation actors and processes
We found that the Implementing Agency played, and still plays, a central role in communication, financial management and support. The agency operates as a vertical structure, with an executive and an administrative board. The former acts as a third-party payer, the latter supervises the providers and managers of the hospitals. The functions assigned to the Implementing Agency do not include monitoring the quality of CS nor ensuring equity. The feasibility report stated that ‘The guarantee of equity derives from the fact that all women seeking care will benefit from the same care, regardless of their socio-economic level or origin’.
Our analysis shows that the agency informed the facility managers about the Policy and the procedures through letters and directives. It organised training sessions for management teams covering the financial and general reimbursement procedures. However, no specific guidelines or procedure manuals were provided to health providers and managers. As we described above, the decree is clear about the services that the Policy covers. However, we found that the Implementing Agency interprets the term ‘caesarean section’ in its strict clinical sense as ‘one or more incisions made through a mother’s abdomen and uterus to deliver one or more babies’. Strictly following this definition, for instance, surgical procedures for ruptured uterus are not reimbursed.
The Implementing Agency set up relatively simple reimbursement procedures. For each CS, providers must fill a form with the identification details of the beneficiary and some clinical details of the service provided. The hospital management team compiles all information to prepare the claim submitted to the Implementing Agency. During their field visits, the executive board members use these documents for verification. The Implementing Agency staff carries out spot controls of the prescriptions and bills paid by users in the facilities. Since the government allowed direct payment to facilities, the reimbursements are faster than other disbursements. From the beginning of the Policy in 2009 up to December 2011, the analysis of the financial flow tracking data shows that the Implementing Agency reimbursed all 51 913 CS carried out in the 44 facilities implementing the Policy at this date for a cumulated amount of XOF 5 191 300 000 (€7 914 086).
Finally, the Implementing Agency is intended to support the providers in carrying out the Policy. We found, however, that the initial supervisory visits were inflexible and failed to address practical challenges faced by providers:
Doctors, when they treat women who have been referred with meconium stained fluid, prescribe strong antibiotics to avoid infection, but they (the Implementing Agency supervisors) said: ‘No, nothing other than ampicillin should be prescribed (the antibiotic provided for free within the Policy)’. Now that we do not prescribe anything else, we see surgical wounds become infected. (Midwife, regional hospital)
Implementation fidelity
The policy was initially implemented in 44 health facilities (figure 1). The facilities were accredited on the basis of two criteria: not-for-profit status and being capable of providing CS. Over time, four more facilities were accredited, including one private-for-profit facility. All seven facilities included in this study started implementing the Policy in April 2009.
Figure 1.
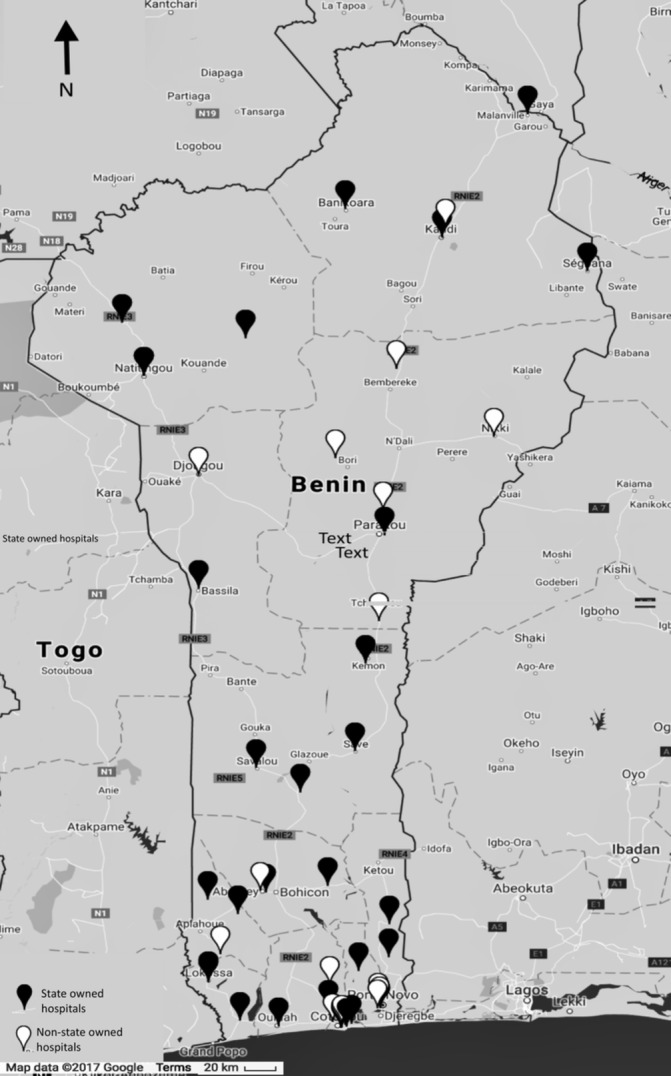
Map of the hospitals implementing the fee exemption for caesarean section policy in Benin.
In terms of inputs, the government initially provided kits containing all the consumables and drugs required for a CS to the accredited facilities. The allocation was based on the expected number of CS and came on top of the fixed sum reimbursed by the government. However, we found that some facility managers interpreted the kits as a recurrent measure. The sudden interruption of their provision led the managers of some facilities to reduce the services in the package.
We found that policy adoption was highly variable (table 3). Hospital 2, for instance, provided only one of the eight items for free, while hospital 5 provided five. Patient transfer, intravenous infusion and the consultation were not provided for free in five out of seven facilities. When asked why, district and hospital managers explained that the operational procedures issued by the Implementing Agency did not cover these items. For instance, they mentioned that there was no procedure foreseen to reimburse users who themselves paid for their transfer to facilities. The surgical procedure, hospitalisation and the postoperative check-up were almost consistently provided for free. We found that drugs and medical consumables were partially provided for free. Only one hospital fully adopted the free drugs directive.
Table 3.
Services offered for free under the fee exemption for CS policy in seven hospitals in Benin in 2012
| Items | Hopsital 1 | Hospital 2 | Hospital 3 | Hospital 4 | Hospital 5 | Hospital 6 | Hospital 7 | Number of free items (across all hospitals) |
| Referral within the district | 0/7 | |||||||
| Starting intravenous infusion before referral | 0/7 | |||||||
| Consultation | 2/7 | |||||||
| Cost of surgery | 6/7 | |||||||
| Drugs | 1/7 | |||||||
| Supplies | 2/7 | |||||||
| Cost of hospitalisation | 5/7 | |||||||
| Postsurgery check-up | 6/7 | |||||||
| Free items out of total items | 3/8 | 1/8 | 2/8 | 3/8 | 5/8 | 4/8 | 4/8 |
Black, not free; grey, charged partially; white, free. Source: FEMHealth Report, Benin (19).
CS, caesarean section.
The policy outcomes
CS delivery rate
As shown in the table 4, 2.3% of all deliveries were by CS in 2001. Before the Policy was introduced, the CS rate was increasing by an average of 0.2% per year. When the Policy was introduced, there was no immediate change in the number of CS (P=0.424). However, from 2009 onwards, there was an average increase in the CS rate of 0.5% per year. By 2015, the CS rate was 7%. This represents an additional average increase of 0.3% per year over and above the pre-existing secular trend, which we can interpret as attributable to the Policy in the absence of other interventions that might have increased CS rates.
Table 4.
Change in CSs per 100 expected live births prepolicy and postpolicy, using national health information data from 2001 to 2015 in Benin
| Average caesarean rate | 95% CI | P value | |
| Constant | 2.3% | 1.5% to 3.0% | <0.001 |
| Annual trend before the policy (2009) | +0.2% | 0.07% to 0.4% | 0.009 |
| Immediate change in level (2009) | −0.4% | −1.3% to 0.6% | 0.424 |
| Annual trend after the policy (2009) | +0.5% | 0.3% to 0.7% | <0.001 |
| Change in trend before versus after the policy | +0.3% | 0.07% to 0.6% | 0.016 |
CSs, caesarean sections.
Actual fees related to CS
Our analysis indicated that since the initiation of the Policy, most women were still paying fees related to CS. The median fee paid in a facility ranged from €0 to €41.40. We found that across the seven study sites, the fees charged to women who underwent a CS were reduced by at least 47%–84%, as compared with the prepolicy tariff (table 5). Fees charged to women varied across hospitals but also within the same hospital. In one hospital, for example, some users received fully free CS, while others still paid up to €55.
Table 5.
Comparison of the tariff before the policy and user fee paid by users for CS under the fee exemption for CS policy in Benin in 2012
| Facility | Tariff before the policy in € (a) | Min charge after the policy in € (b) | Median charge after the policy in € (c) | Maximum charge after the policy in € (d) | Minimum charge reduction in € (d−a) | Minimum proportion of charge reduction in € (d*100/a) |
| Hospital 1 | 148.09 | 0.00 | 14.68 | 31.10 | −116.99 | −79% |
| Hospital 2 | 176.82 | 0.00 | 0.00 | 27.44 | −149.38 | −84% |
| Hospital 3 | 140.41 | 4.12 | 11.81 | 34.30 | −106.10 | −76% |
| Hospital 4 | 112.32 | 2.97 | 11.63 | 22.53 | −89.79 | −80% |
| Hospital 5 | 112.32 | 38.72 | 41.39 | 115.71 | 3.38 | 3% |
| Hospital 6 | 86.13 | 0.15 | 5.34 | 45.73 | −40.40 | −47% |
| Hospital 7 | 122.66 | 0.00 | 8.69 | 54.72 | −67.94 | −55% |
Source: FEMHealth exit interview data, Benin, 2012.
CS, caesarean section.
Financial protection provided by the Policy
We analysed the remaining user fees paid for a CS, proportional to the national GDP per capita for each included facility (table 6). The mean proportion ranged from 6.6% to 15.4%, with a maximum by hospital from 11.9% up to 50.1%. Further analysis reveals several patterns. Hospital 2 provided better protection: it provided all items related to CS for free and charged a maximum fee of 12.11% of the GDP per capita. At the opposite end, hospital 3 persistently charged fees, ranging from 11.7% up to 38.9% of GDP per capita.
Table 6.
User fees for a delivery by CS under the fee exemption for CS policy in seven hospitals as a proportion of the GDP per capita in Benin in 2012
| All facilities | Hospital 1 | Hospital 2 | Hospital 3 | Hospital 4 | Hospital 5 | Hospital 6 | Hospital 7 | |
| Mean (%) | 9.53 | 9.94 | 6.59 | 15.38 | 7.37 | 10.31 | 6.98 | 6.75 |
| Median (%) | 8.00 | 8.42 | 5.70 | 14.43 | 7.27 | 7.92 | 5.70 | 6.35 |
| Minimum (%) | 0.00 | 1.76 | 0.00 | 11.71 | 4.92 | 2.83 | 1.33 | 2.18 |
| Maximum (%) | 50.11 | 50.11 | 12.11 | 38.94 | 11.88 | 36.00 | 19.76 | 17.75 |
Source: FEMHealth exit interview data.
GDP per capita - 2012 LCU, Word Bank data.
CS, caesarean section; GDP, gross domestic product.
Equity analysis
Figure 2 presents the trends in the proportion of deliveries by CS stratified by relative wealth from 1993 to 2011. Using DHS data, this graph shows a persistent equity gap in utilisation of CS between the richest quintile of the population and the other groups in the period of 1995 to 2009. After the Policy was initiated, that gap actually widened: in 2011, more than 15% of women in the top quintile had a delivery by CS, compared with around 5% for the rest of the population.
Figure 2.
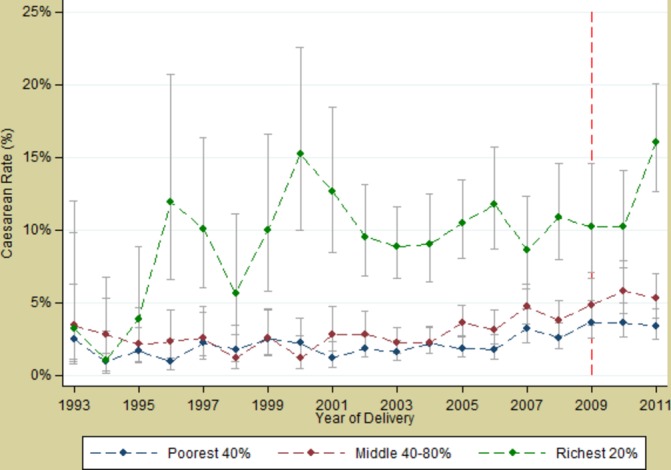
Trends in caesarean section rates by socioeconomic group from 1993 to 2011 in Benin from Demographic and Health Survey data.
Discussion
In this study, we analysed key steps of the policy cycle using a wide range of quantitative and qualitative data. We found that the scope of the initially ambitious policy was reduced all along the stages of the policy cycle. Overall, our analysis showed an increase of the CS rate in Benin, from 2.3% in 2001 to 7% in 2015 according to the national facility-based statistics and from 3.7 in 2009 to 6.4 in 2012 if the DHS data are used. We thus found that there was a systematic increase in CS rate after the Policy was implemented. However, we cannot fully attribute this increase to the Policy, even if to the best of our knowledge, there were no other interventions or contextual factors that could explain this increase. The increase could also be due to better reporting, an indirect effect of the Policy, since the reimbursement of facilities was directly linked to good reporting. It should be noted that the CS rate of women in the richest quintile is still far higher than that of women in the lowest quintiles.
We argue that the development of the UFEP for CS in Benin can be seen as rowing a course against the current. The policy encountered resistance in the form of a dominant pro-user fee culture within the MoH and a neoliberal political regime that favoured user fees. Additional resistance was mounted by health technocrats who feared that the Policy would not be sustainable and put hospitals at risk. This fear may have been justified by previous failures,59 lessons from the other UFEPs in the region22 and the international literature calling for careful action for UFEP.7 The dominant scepticism about the sustainability of UFEP led to preserving the existing user fee recovery principles. Such scepticism about UFEP was also reported in Niger49 and reflects the lack of confidence in the State as a reliable partner.27 In Benin, this contributed to a UFEP package that is more restricted than in any other country in the region.1 The ‘business as usual’ logic may explain why the Implementing Agency was not given additional roles related to quality assurance or equity. This is a missed opportunity as the new resource allocation mechanism could have been framed by strategic purchasing arrangements60 to increase equity and quality. This strategic choice would probably have received more support from Benin’s international partners.
The policy did not attain its political goal of making CS fully free for all. In fact, it tends to benefit women in the top quintile more than any other group, thus paradoxically reinforcing existing inequities. The well-known risk of such policies reaching predominantly the richest due to prevalent social exclusion mechanisms was not taken into consideration by policymakers. Barriers to social inclusion, such as limited access to appropriate information and limited capacity to reach health services, are well known20 21 61 but were not tackled. Equity seems not to have been a major concern in the policy formulation phase and was not assessed by the monitoring system of the Policy. The development of the Policy would have been better if policymakers perceived the political commitment and the resources provided by the Policy as a means to effectively foster financial access to quality emergency obstetric and neonatal care for all while explicitly addressing social exclusion mechanisms. This, of course, would have required that the principles of the Bamako Initiative, which failed to address equity challenges for decades,62–64 were placed in question.
One could argue that this is a rather pessimistic view because the Policy succeeded in reducing user fees for CS at least by 47% (and up to 84% in some facilities) as compared with the prepolicy tariff. However, considering the resources allocated to this policy, this result is clearly suboptimal.31
To some readers, the limited effect of the Policy may not be a surprise. After all, one could argue that the potential of the Policy to reduce maternal and neonatal morbimortality was overestimated. There is, indeed, evidence showing that a narrowly defined policy intervention—like a UFEP for only CS—has only limited potential to reduce maternal and neonatal morbidity and mortality.65 Such a policy may even induce perverse effects by incentivising unnecessary CS and thus lead to significant complications, disability or death, particularly in settings that lack the facilities and/or capacity to properly conduct safe surgery and treat surgical complications.66
Our analysis found that the Policy is only partially implemented. We identified several factors, some of which are related to the Policy itself (narrow target and narrow focus), the policy context (with barriers at all levels) or the position of the different actors.
We found that international partners did not provide much support for the Policy, which is in contrast to recent study findings indicating that international donors are no longer in favour of user fees.5 6 The position of international partners in Benin is different from Ghana, where they have more prominently shaped the agenda setting of fee exemption for a comprehensive package of maternal health services.67 We surmise that the position of international actors in Benin was based on the poor evidence of the effectiveness of a narrowly focused policy (CS only) and concerns regarding the global increase of the CS rate and its adverse effects.66
The limited uptake by facility managers can be explained by several factors. First, the national strategic plan for improving maternal and neonatal health,68 which was in place when the Policy was being developed, did not explicitly consider fee exemption as a policy option. This, combined with the pro-user fee culture, led to resistance to the Policy by many technocrats. The way organisational culture and dominant ideas and institutions shape policy formulation as well as implementation of policies requires more attention.
At the implementation level, fees charged to women and financial protection varied across facilities and within a same hospital. Managers of non-state-owned facilities exploited their discretionary power69 in the absence of strong governance arrangements and only partially implemented the Policy. Managers found arguments to keep charging patients that ignored the effect of the Policy on the cost of implementation for non-state-owned facilities. Also, at state-run facilities, weak governance and regulation70 is a documented challenge that may have contributed to variable implementation. The pro-user fee culture prevalent at the central level in the MoH made it easier for facility managers and providers to continue charging user fees. However, we found that some facilities implemented the Policy better than others. Further exploration of the different dynamics at hospital level may enrich the debate and prevent similar mixed responses towards Universal Health Coverage interventions.31
The main limitation of this study is the lack of investigation into how the population was involved in the agenda-setting phase. Our interviews with community representatives in the local health committees, and patients and their families at different maternity wards, provided only indirect insights. We may have missed an opportunity by not investigating the only private-for-profit facility accredited to implement the Policy, which could have provided insights into other dynamics shaping the Policy.
Our methods to assess national population-based CS rates used data drawn from annual statistics reports, based largely on self-reported routine data from both state-owned and non-state-owned facilities. Such datasets may raise concerns about accuracy and completeness. However, CS is likely to be one of the indicators with the highest completeness since it is a major intervention carried out in a limited number of facilities that are closely monitored by the MoH. The Policy has indirectly incentivised facilities to produce quality CS data since 2009, which may also explain better reporting of CS in facilities and thus in the annual health statistic reports after 2009. Triangulating with DHS data may have reduced the impact of this limitation in our analysis, but DHS data are available only up to 2011.
Conclusion
In this study, we set out to analyse the key steps of the policy cycle related to the UFEP for CS in Benin. We uncovered how the policy actors and the context shape the policy content and process and found that dominant ideas and institutions related to user fees create a pro-user fee organisational culture within the health system that influenced both the formulation of the Policy as well as its implementation.
Policymakers did not address these entrenched elements, which led to a persistent tension that affected the key steps of the policy cycle. Weak governance arrangements allowed both state-owned and non-state-owned facility actors to continue charging fees related to CS. Unless a policy addresses all financial, geographical and cultural barriers to care, it will not ensure access of care for all. Financial protection and equity should be emphasised in the organisational culture of health systems in Benin and in West African countries at large, in tandem with multisectoral efforts for better governance. Without such efforts, the pathway toward UHC will be slow and challenging.
Acknowledgments
The authors would like to thank the European Commission and the Directorate-general Development Cooperation and Humanitarian Aid of Belgium for their financial support to the development of this manuscript. We would also like to thank the Ministry of Health of Benin for authorising and providing effective institutional support for the development and the implementation of this research programme.
Footnotes
Handling editor: Valery Ridde
Contributors: J-PD and BM conceptualise the structure and the goals of the current revised manuscript. J-PD and JAC conducted the necessary extra-analysis for the current manuscript. J-PD developed the first draft. All the authors contributed to its improvement. All approved the current revised version.
Funding: The authors received funding from Directorate-general Development Cooperation and Humanitarian Aid of Belgium to the development of this manuscript and from the Seventh Framework Programme (10.13039/100011102).
Competing interests: None declared.
Ethics approval: The Benin National Committee for Health Ethics (ref. 0792/MS/DC/SGM/DFRS/SRAO/SA), the Institutional Review Board of the Institute of Tropical Medicine, Antwerp (ref. 114359799) and the ethical committee of the London School of Hygiene and Tropical Medicine (ref. 6103) approved this study protocol.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Witter S, Boukhalfa C, Cresswell JA, et al. Cost and impact of policies to remove and reduce fees for obstetric care in Benin, Burkina Faso, Mali and Morocco. Int J Equity Health 2016;15:123 10.1186/s12939-016-0412-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lagarde M, Palmer N. The impact of user fees on health service utilization in low- and middle-income countries: how strong is the evidence? Bull World Health Organ 2008;86:839–48. 10.2471/BLT.07.049197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Araoyinbo ID, Ataguba JE. User fees in Africa: from theory and evidence, what next? An essay submitted to the african Health Economics and Policy Association. Alliance for Health Policy and System Research, 2008.
- 4. WHO. National health account indicators, 2016.
- 5. Robert E, Ridde V. Global health actors no longer in favor of user fees: a documentary study. Global Health 2013;9:29 10.1186/1744-8603-9-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ridde V. From institutionalization of user fees to their abolition in West Africa: a story of pilot projects and public policies. BMC Health Serv Res 2015;15(Suppl 3):S6 10.1186/1472-6963-15-S3-S6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gilson L, McIntyre D. Removing user fees for primary care in Africa: the need for careful action. BMJ 2005;331:762–5. 10.1136/bmj.331.7519.762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Russell S, Gilson L. User fee policies to promote health service access for the poor: a wolf in sheep’ s clothing? Int J Health Serv 1997;27:359–79. 10.2190/YHL2-F0EA-JW1M-DHEJ [DOI] [PubMed] [Google Scholar]
- 9. Meessen B, Hercot D, Noirhomme M, et al. Removing user fees in the health sector in low-icome countries: a multi-country review. New York: United Nation Children’s Fund, 2009. [Google Scholar]
- 10. Gbary AR, Sossou RA, Dossou JP, et al. [The determinants of the low case fatality rate of the cholera epidemic in the Littoral department of Benin in 2008]. Sante Publique 2011;23:345–58. [PubMed] [Google Scholar]
- 11. Richard F, Antony M, Witter S, et al. Fee exemption for maternal care in sub-Saharan Africa: a review of 11 countries and lessons for the region. Glob Heal Gov 2013;6:1–21. [Google Scholar]
- 12. McKinnon B, Harper S, Kaufman JS. Who benefits from removing user fees for facility-based delivery services? Evidence on socioeconomic differences from Ghana, Senegal and Sierra Leone. Soc Sci Med 2015;135:117–23. 10.1016/j.socscimed.2015.05.003 [DOI] [PubMed] [Google Scholar]
- 13. Olivier de Sardan J-P, Ridde V. Une politique publique de santé et ses contradictions: la gratuité des soins au Burkina Faso, au Mali et au Niger. Paris: Éditions Karthala, 2014. [Google Scholar]
- 14. Robert E, Samb OM, Marchal B, et al. Building a middle-range theory of free public healthcare seeking in sub-Saharan Africa: a realist review. Health Policy Plan 2017;32:1002–14. 10.1093/heapol/czx035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zombré D, De Allegri M, Ridde V. Immediate and sustained effects of user fee exemption on healthcare utilization among children under five in Burkina Faso: a controlled interrupted time-series analysis. Soc Sci Med 2017;179:27–35. 10.1016/j.socscimed.2017.02.027 [DOI] [PubMed] [Google Scholar]
- 16. Abdou Illou MM, Haddad S, Agier I, et al. The elimination of healthcare user fees for children under five substantially alleviates the burden on household expenses in Burkina Faso. BMC Health Serv Res 2015;15:313 10.1186/s12913-015-0957-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. De Allegri M, Ridde V, Louis VR, et al. The impact of targeted subsidies for facility-based delivery on access to care and equity - evidence from a population-based study in rural Burkina Faso. J Public Health Policy 2012;33:439–53. 10.1057/jphp.2012.27 [DOI] [PubMed] [Google Scholar]
- 18. Atchessi N, Ridde V, Zunzunegui M -V. User fees exemptions alone are not enough to increase indigent use of healthcare services. Health Policy Plan 2016;31:674–81. 10.1093/heapol/czv135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mladovsky P, Ba M. Removing user fees for health services: a multi-epistemological perspective on access inequities in senegal. Soc Sci Med 2017;188:91–9. 10.1016/j.socscimed.2017.07.002 [DOI] [PubMed] [Google Scholar]
- 20. Soors W, Dkhimi F, Criel B. Lack of access to health care for African indigents: a social exclusion perspective. Int J Equity Health 2013;12:91 10.1186/1475-9276-12-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Agyepong IA, Nagai RA. “We charge them; otherwise we cannot run the hospital” front line workers, clients and health financing policy implementation gaps in Ghana. Health Policy 2011;99:226–33. 10.1016/j.healthpol.2010.09.018 [DOI] [PubMed] [Google Scholar]
- 22. Olivier de Sardan J-P, Ridde V. L’exemption de paiement des soins au Burkina Faso, Mali et Niger. Afr Contemp 2012;243:11 10.3917/afco.243.0011 [DOI] [Google Scholar]
- 23. Ridde V, Olivier de Sardan JP. The implementation of public health interventions in Africa: a neglected strategic theme. Med Sante Trop 2017;27:6–9. 10.1684/mst.2016.0605 [DOI] [PubMed] [Google Scholar]
- 24. Witter S, Adjei S, Armar-Klemesu M, et al. Providing free maternal health care: ten lessons from an evaluation of the national delivery exemption policy in Ghana. Glob Health Action 2009;2:1881 10.3402/gha.v2i0.1881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ridde V, Sombie I. Street-level workers’ criteria for identifying indigents to be exempted from user fees in Burkina Faso. Trop Med Int Health 2012;17:782–91. 10.1111/j.1365-3156.2012.02991.x [DOI] [PubMed] [Google Scholar]
- 26. Walker L, Gilson L. ’We are bitter but we are satisfied': nurses as street-level bureaucrats in South Africa. Soc Sci Med 2004;59:1251–61. 10.1016/j.socscimed.2003.12.020 [DOI] [PubMed] [Google Scholar]
- 27. Beland D, Ridde V. Ideas and Policy Implementation: Understanding the Resistance against Free Health Care in Africa. Glob Heal Gov 2016;10:9–23. [Google Scholar]
- 28. Erasmus E, Gilson L, Govender V, et al. Organisational culture and trust as influences over the implementation of equity-oriented policy in two South African case study hospitals. Int J Equity Health 2017;16:164 10.1186/s12939-017-0659-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Marchal B, Van Belle S, De Brouwere V, et al. Studying complex interventions: reflections from the FEMHealth project on evaluating fee exemption policies in West Africa and Morocco. BMC Health Serv Res 2013;13:469 10.1186/1472-6963-13-469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ganaba R, Ilboudo PGC, Cresswell JA, et al. The obstetric care subsidy policy in Burkina Faso: what are the effects after five years of implementation? Findings of a complex evaluation. BMC Pregnancy Childbirth 2016;16:84 10.1186/s12884-016-0875-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lange IL, Kanhonou L, Goufodji S, et al. The costs of ’free': experiences of facility-based childbirth after Benin’s caesarean section exemption policy. Soc Sci Med 2016;168:53–62. 10.1016/j.socscimed.2016.09.008 [DOI] [PubMed] [Google Scholar]
- 32. Yin RK. Case Study Research. Design and Methods. Vol. 4 Thousand Oaks, California: Sage Publications, 2009:264–7. [Google Scholar]
- 33. Everitt BS, Landau S, Leese M, et al. Cluster analysis. 5th edn London, UK: Wiley, 2011. [Google Scholar]
- 34. Joe H, Ward J. Hierarchical grouping to optimize an objective function. J Am Stat Assoc 1963;58:9. [Google Scholar]
- 35. Institut National de la Statistique et de l’Analyse Economique et Macro International Inc. Enquête Démographique et de Santé (EDSB-IV) - Bénin 2011-2012. Calverston, Maryland, USA, 2013. [Google Scholar]
- 36. WHO, UNICEF, UNFPA, World Bank Group, United Nations Population Division. Trends in maternal mortality: 1990 to 2015 Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: World Health Organization, 2015. [Google Scholar]
- 37. Health System 20/20. Evaluation du système de santé du Bénin. Besthesda: Abt Associates Inc, 2012. [Google Scholar]
- 38. Cairney P. Understand public policy: theories and issues. New York: Palgrave MacMillan, 2012. [Google Scholar]
- 39. Kingdon JW. Agendas, alternatives, and public policies. 2nd edn: Pearson Education Ltd, 1995. [Google Scholar]
- 40. Walt G, Gilson L. Reforming the health sector in developing countries: the central role of policy analysis. Health Policy Plan 1994;9:353–70. 10.1093/heapol/9.4.353 [DOI] [PubMed] [Google Scholar]
- 41. Peters DH, Tran TN, Adam T. Implementation research in health: a practical guide. Geneva, Switzerland: Alliance for Health Policy and Systems Research, World Health Organization, 2013. [Google Scholar]
- 42. Lagarde M. How to do (or not to do). Assessing the impact of a policy change with routine longitudinal data. Health Policy Plan 2012;27:76–83. 10.1093/heapol/czr004 [DOI] [PubMed] [Google Scholar]
- 43. Centre de Recherche en Reproduction Humaine et en Démographie. Rapport de synthèse: l’évaluation de la politique de gratuité de la césarienne dans cinq zones sanitaires au Bénin. Cotonou, Benin: University of Aberdeen, 2014. [Google Scholar]
- 44. Gbedonou P, Moussa Y, Floury B, et al. The Bamako initiative: hope or illusion? observations on the Benin experience. Cah Santé 1994;4:281–8. [PubMed] [Google Scholar]
- 45. Boko M. BENIN: humiliation, detention for failure to pay maternity bills. Inter Press Service. News Views Point from Global South. 1999, 2016.
- 46. Witter S. Federal Ministry of Health K. Removal of user fees for health care: a review of recent experiences in Africa. Khartoum: Federal Ministry of Health, 2010. [Google Scholar]
- 47. Scen-Afrik. Etude de l’offre gratuite des soins aux enfants de moins de cinq ans et aux femmes enceintes, y compris la césarienne. Cotonou, Bénin: Ministère de la Santé du Bénin, 2008. [Google Scholar]
- 48. Houngnikpo MC, Decalo S. Historical dictionary of Benin. Lanham, Maryland: Scarecrow Press, 2012. [Google Scholar]
- 49. Bierschenk T, Olivier de Sardan J-P. States at work: dynamics of African bureaucracies. Leiden, Boston: Brill, 2014. [Google Scholar]
- 50. Ronen D. Political dynamics in Benin. Washington, DC, 1984. Department of State of USA. [Google Scholar]
- 51. Koko JL. National conference as a strategy for conflict Transformation and peacemaking: the legacy of the Republic of Benin model. London: Adonis & Abbey Publishers Ltd, 2008. [Google Scholar]
- 52. Tévoedjrè A. Rapport général de synthèse de la conférence des forces vives de la nation - Nous avons vaincu la fatalité. Cotonou: Republique du Benin, 1990. [Google Scholar]
- 53. Bank W. 1989. Benin - Structural adjustment program. Washington, DC: World Bank. [Google Scholar]
- 54. Carrin G. Community financing of drugs in Sub-Saharan Africa. Int J Health Plann Manage 1987;2:125–45. 10.1002/hpm.4740020206 [DOI] [PubMed] [Google Scholar]
- 55. Kanji N. Charging for drugs in Africa: UNICEF’S ‘Bamako Initiative’. Health Policy Plan 1989;4:110–20. 10.1093/heapol/4.2.110 [DOI] [Google Scholar]
- 56. Institut National de la Statistique et de l’Analyse Economique et Macro International Inc. Enquête Démographique et de Santé (EDSB-III) - Bénin 2006. Calverston, Maryland, USA: Institut National de la Statistique et de l’Analyse Economique et Macro International Inc, 2007. [Google Scholar]
- 57. Jansen C, Lodi E, Lodenstein E, et al. Vers une couverture maladie universelle au Bénin. Amsterdam: KIT Publishers, 2013. [Google Scholar]
- 58. AEDES. Fiche projet - Programme d’appui à la santé maternelle et infantile. 2013. http://www.aedes.be/en/fiches_projet/benin/benin_pasmi_2013.html (accessed 1 Sep 2017).
- 59. Knippenberg R, Alihonou E, Soucat A, et al. Implementation of the Bamako Initiative: strategies in Benin and Guinea. Int J Health Plann Manage 1997;12(Suppl 1):S29–47. [DOI] [PubMed] [Google Scholar]
- 60. Terwindt F, Rajan D, Soucat A. Priority-setting for national health policies, strategies and plans In: Strategizing national health in the 21st century: a handbook. Vol. 71, 2016. [Google Scholar]
- 61. Michielsen JJ, Meulemans H, Soors W, et al. Social protection in health: the need for a transformative dimension. Trop Med Int Health 2010;15:654–8. 10.1111/j.1365-3156.2010.02529.x [DOI] [PubMed] [Google Scholar]
- 62. Soucat A, Gandaho T, Levy-Bruhl D, et al. Health seeking behaviour and household health expenditures in Benin and Guinea: the equity implications of the Bamako Initiative. Int J Health Plann Manage 1997;12(Suppl 1):S137–63. [DOI] [PubMed] [Google Scholar]
- 63. Gilson L, Kalyalya D, Kuchler F, et al. The equity impacts of community financing activities in three African countries. Int J Health Plann Manage 2000;15:291–317. 10.1002/hpm.599 [DOI] [PubMed] [Google Scholar]
- 64. Ridde V. Is the Bamako Initiative still relevant for West African health systems? Int J Health Serv 2011;41:175–84. 10.2190/HS.41.1.l [DOI] [PubMed] [Google Scholar]
- 65. Campbell OM, Graham WJ; Lancet Maternal Survival Series steering group. Strategies for reducing maternal mortality: getting on with what works. Lancet 2006;368:1284–99. 10.1016/S0140-6736(06)69381-1 [DOI] [PubMed] [Google Scholar]
- 66. Betrán AP, Ye J, Moller AB, et al. The increasing trend in caesarean section rates: Global, Regional and National Estimates: 1990-2014. PLoS One 2016;11:e0148343 10.1371/journal.pone.0148343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Koduah A, Agyepong IA, van Dijk H. ’The one with the purse makes policy': Power, problem definition, framing and maternal health policies and programmes evolution in national level institutionalised policy making processes in Ghana. Soc Sci Med 2016;167:79–87. 10.1016/j.socscimed.2016.08.051 [DOI] [PubMed] [Google Scholar]
- 68. Direction de la Santé Familiale. Document de stratégie nationalede réduction de la mortalité maternelle et néontale au Bénin 2006-2015. Cotonou, Benin: Ministère de la Santé du Bénin, 2006. [Google Scholar]
- 69. Lipsky M. Street-level bureaucracy: dilemmas of the individual in public services. New York: Russell Sage Foundation, 1980. [Google Scholar]
- 70. Project S, Inc AA. Benin private health sector assessment. Bethesda: USAID, 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Boko M. BENIN: humiliation, detention for failure to pay maternity bills. Inter Press Service. News Views Point from Global South. 1999, 2016.


