Abstract
Introduction
In low-income and middle-income countries, it is estimated that one in every three preschool-age children are failing to meet cognitive or socioemotional developmental milestones. Thailand has implemented a universal national developmental screening programme (DSPM) for young children to enable detection of developmental disorders and early intervention that can improve child health outcomes. DSPM implementation is being hampered by low attendance at follow-up appointments when children fail the initial screening.
Methods
Action research, using qualitative methods was conducted with 19 caregivers, 5 health workers and 1 chief at two Health Promotion Hospitals to explore the factors affecting attendance at follow-up appointments. Transcripts and notes were analysed using descriptive content analysis. Findings were then discussed with 48 health workers, managers, researchers and policymakers.
Results
The high workload of health workers during busy vaccination clinics, and inadequate materials prevented clear communication with caregivers about the screening, how to stimulate child development and the screening result. Caregivers, particularly grandparents, had a lack of understanding about how to stimulate child development, and did not fully understand failed screening results. Caregivers felt blamed for not stimulating their child’s development, and were either worried that their child was severely disabled, or they did not believe the screening result and therefore questioned its usefulness. This led to a lack of attendance at follow-up appointments.
Conclusion
Task-sharing, mobile health (mhealth), community outreach and targeted interventions for grandparent caregivers might increase awareness about child development and screening, and allow health workers more time to communicate effectively. Sharing best practices, communication training and mentoring of DSPM workers coupled with mhealth job aids could also improve caregiver attendance at follow-up. Engagement of caregivers in understanding the barriers to attendance at follow-up and engagement of stakeholders in the design and implementation of interventions is important to ensure their effectiveness.
Keywords: developmental disabilities, preschool children, caregivers, child development, community-institutional relations
Key questions.
What is already known about this topic?
Early detection of children with developmental disorders and early stimulation of children with typical development can have lasting health benefits if caregivers are able to access interventions and follow advice.
What are the new findings?
The success of a national universal developmental screening programme in Thailand was hampered by low rates of follow-up among children failing initial screening.
Miscommunication between health workers and caregivers led to caregivers either being worried that their child was severely disabled, or they felt that the screening was not useful, which led to a lack of attendance at follow-up visits.
Many children were cared for by grandparent caregivers who found it more difficult to understand the screening process, health worker advice and the manual which was given to caregivers of children who failed the screening.
Recommendations for policy
Better communication about child development, the screening process and screening result could be enabled by mobile health interventions, task-sharing and engaging caregivers, particularly grandparents, in addressing barriers to attending follow-up appointments.
Introduction
Global estimates suggest that approximately 5% of children have a moderate to severe disability,1 of which an estimated 18.75/10 000 have a pervasive developmental disorder.2 Developmental disorder and delay is an umbrella term covering intellectual disability/mental retardation and pervasive developmental disorders, including autism. Prevalence estimates differ substantially between countries, with up to 15% of children in the USA reported to have developmental disorders.3 A study using data from 2010 of 35 low- and middle-income countries (LMIC) suggests that one in every three preschool-age children are failing to meet cognitive or socioemotional developmental milestones.4 Accurate data are difficult to find, especially in LMICs where most of the world’s children reside.5
Research has shown that 85% of people with developmental disorders in LMICs do not receive adequate treatment.6 Developmental disorders usually have a childhood onset and persist into adulthood. People with developmental disorders are more vulnerable to physical illness7 and, if left untreated, children with developmental disorders are two or three times more likely than other children to develop behavioural problems,8 which can become more severe in adolescence and into adulthood.9 10 Caregivers of children with developmental disorders are often psychologically distressed,11 12 and families often suffer a high emotional and financial burden13 which has knock-on effects on the child’s behaviour.
Research shows that early detection and intervention can have lasting benefits.14 15 Developmental screening programmes in primary care settings that engage caregivers and non-specialists can improve the identification and referral of children who have possible delays.16–19 This is particularly important in LMICs with a shortage of mental health workers.20 The usefulness of screening is partly dependent on caregiver ability to act on advice and, although sociodemographic and socioeconomic risk factors can be identified and measured, these are not necessarily amenable to change. There is a need to engage with those who do not follow advice to understand their reasons and work together with service providers, caregivers and policymakers to enable optimal service delivery, and facilitate increased uptake of screening and follow-up. In this paper, we present findings from an action research project which sought to address the factors affecting the implementation of the national child developmental screening programme (DSPM) in Thailand. In particular, we focus on the nationally reported problem of high numbers of caregivers who do not return for follow-up visits if their child failed the screening.
Theoretical framework
It was particularly important to use an action research approach to tackle this issue, as it enables critical reflection on the social reality by those experiencing that reality.21 It enables those experiencing the ‘problem’ to reflect and use their knowledge and experience to generate solutions,22 and starts with a premise that a full understanding of a situation from different perspectives is needed in order to change it.23 It uses a cyclical approach of problem definition, data collection, reflection and action, building on people’s own motivations to change.24 We engaged informally with policymakers and programme implementers to frame research questions, and then collaborated with caregivers, policymakers and programme implementers to develop an understanding of the problem through qualitative research and reflective discussion. We then discussed what action should be taken on the basis of this research to improve screening implementation and uptake with stakeholders. One of the strengths of this collaborative or cocreative approach is that it can enable the design of interventions that are responsive and context specific, and can increase uptake of research findings.25 26
The developmental screening programme
In Thailand, 0.33% of children aged 0–14 years had a disability, and 1.2% of deaths per 100 000 population were attributed to mental or behavioural disorders.27 A hospital-based study found that 3.8% of children receiving routine health check-ups had developmental or behavioural problems.28 The Thai Pediatric Society produced guidelines for developmental surveillance at well-child visits in 201329 and a national universal DSPM was initiated by 2015 (http://thaichilddevelopment.com). Its objectives were to improve early identification of developmental disorders and to enable early stimulation of child development in households through advice and referral. The DSPM is implemented by trained nurses or primary care workers at subdistrict Health Promoting Hospitals (HPH), and also at well-baby clinics of local, provincial and university hospitals.
Children are screened at routine vaccination visits at 9, 18, 30 and 42 months by health workers in HPHs. Health workers use a DSPM manual to guide the screening process which is designed for health workers and caregivers. The manual gives guidance to the health worker and caregiver about which exercises the child should be able to do within their age range within the developmental domains, and has pictorial and written instructions about how to practise the exercises with the child. Health workers take children to a separate room and choose 8–10 exercises from the DSPM manual to test physical, social, emotional and cognitive developmental domains. For example, an 18-month-old child could be asked to walk while holding a ball; stack two blocks; point to a body part; say at least four words; and hold and drink from a cup. If a child fails to perform one of the exercises, the caregiver is counselled, given the DSPM manual and asked to return to the HPH on a non-vaccination day for a repeat DSPM screening after 1 month. If a child fails the screening a second time they are referred to the community or general hospital.
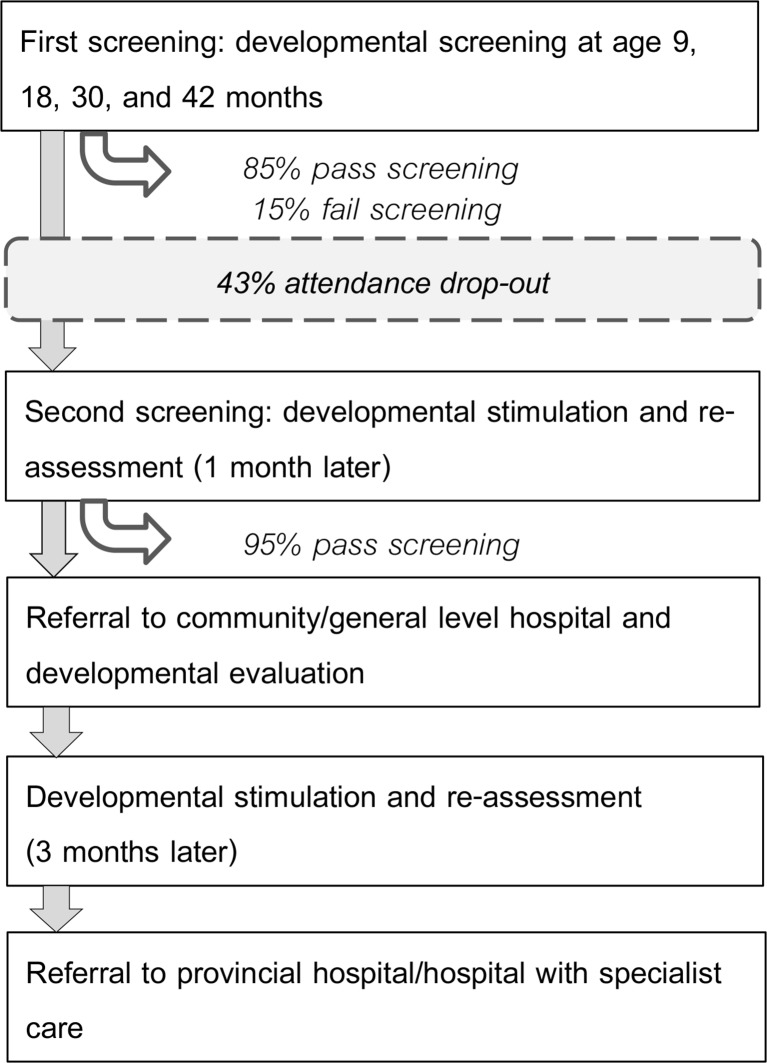
National evaluation data from April 2015 to February 2017 show that 15% of children failed the first screening but only 57% of these children returned for the second screening. Of these 57%, 95% passed the screening and did not require further follow-up (figure 1) (http://www.thaichilddevelopment.com/new_etc.php). Both policymakers and programme implementers were keen to understand the reasons for children not attending follow-up appointments. IC presented the problem at a mental health research workshop in Bangkok, and subsequently worked with the DSPM national evaluation team and researchers from Thammasat University, University College London and King’s College London to design and implement action research to understand the reasons for non-attendance at follow-up appointments and work on ways to address them.
Figure 1.
Developmental screening and referral process.
Methods
Setting and problem definition
The research took place in urban Pathum Thani Province, north Bangkok, in central Thailand. The province is divided into seven districts and 60 subdistricts with a total population of 1.074 million. Pathum Thani is similar to the rest of Thailand in that the populations are mainly Buddhist (95%) and most of the populations can read and write (95%), but distinct from other provinces in that manufacturing is the largest employment sector, as opposed to agriculture, and migration is common. Twenty-four per cent of the populations migrated in the last 5 years, mostly to work in industrial estates, and 30% of the populations are also registered as living in other provinces. 0.6% of the populations are registered as disabled.30
Government health services in Thailand are operated by the Ministry of Public Health (MOPH) and delivered through public sector universal healthcare which covers 99.5% of the population. Antenatal care and vaccination uptake is high at around 90%, with only small differences across socioeconomic groups.31
Specialist care is provided at regional hospitals in provincial centres. Below this, there are general hospitals in provincial capitals or major districts, and community hospitals at the district level.32 A subdistrict HPH is a primary care clinic for preventive medicine, health promotion and treatment for minor trauma or non-serious illnesses. It provides prescriptions from the national essential drugs list, and is usually run by nurses and health promotion staff.33 In Pathum Thani there are 84 HPHs that provide care for around 8000 population with seven members of staff.34 The vaccination clinic is usually held once a week or once every 2 weeks, seeing 30–80 children in a 3-hour clinic.
Sampling and data collection
We purposively selected two HPHs that had low rates of follow-up. These HPHs were similar, serving a similar population with one having slightly higher patient load of 50–60 children at a clinic as opposed to 30–40 in the other. One HPH was slightly more easily to access than the other, as it was on a larger road. We focused data collection on caregivers of children who had received screening at 9, 18 and 30 months old to maintain a relatively homogeneous sample of home care as opposed to older children who may attend kindergarten. We sought to explore the experience of the screening process from caregivers whose children had different screening results (ie, suspected developmental delay or typical development), and who had responded to these results in different ways (ie, caregivers who had returned for a follow-up visit and those who had not). Given our interest in exploring why many caregivers did not return for follow-up visits, we sampled slightly more caregivers from this category. From each HPH, we purposively sampled: (1) caregivers whose children had been screened and did not require a follow-up visit (n=4); (2) caregivers whose children required a follow-up visit that they had attended (n=4); and (3) caregivers whose children required a follow-up visit which they had not attended (n=6). Health workers and researchers made a list of all children meeting each sampling criterion, using clinic records. To minimise bias in selection, researchers phoned every third caregiver to ask if they were interested in participating in the study. No caregiver refused to participate. Two researchers visited each caregiver in their home, explained the study, took written consent to participate and conducted semistructured interviews using topic guides. Each caregiver was given an educational toy for their child to thank them for their time. We developed topic guides considering issues raised at a National Institute of Child Health DSPM workshop in May 2016. IC and JM piloted a topic guide with one caregiver whose child did not require a follow-up, and adjusted it. Interviews discussed child care and perceptions of child development, caregivers’ experience of the screening and follow-up process, and the reasons for attending or not attending follow-up. Data were collected in two phases (table 1). We collected data in two phases to enable all members of the research team—including the non-Thai-speaking members of the team—to review the data. After the first phase of data collection, data were transcribed, translated and reviewed, enabling the team to reflect on the findings and adjust topic guides between phases.
Table 1.
Data collection with caregivers and Health Promotion Hospital (HPH) staff
| Sampling criteria | First-phase n semistructured interviews (translated to English) | Second-phase n semistructured interviews (translated to English) | Feedback focus group discussion |
| Carers of children with typical development (TD) | 2 (1) | 2 (1) | |
| Carers of children who failed first screening and were not followed-up (NFU) | 4 (2) | 2 (1) | 1 |
| Carers of children who failed first screening who were followed-up (FU) | – | 4 (1) | |
| Health workers (HW) | 2 (1) | 3 (1) | |
| Chief (C) | 1 (1) | – | |
| Total | 9 (5) | 11 (4) | 1 |
We also interviewed one chief of an HPH, to explore health systems issues in implementing DSPM, and five health workers who conducted DSPM screening. We explored the factors affecting the screening process and lack of attendance at follow-up appointments. Data were collected by two trained female fourth year community psychology students, who had had some prior experience of collecting qualitative data.
Data management and analysis
Data were recorded and transcribed in Thai. Half of the transcripts were translated to English by a Thai translator. Two paragraphs from the middle of two transcripts were back-translated by IC to check the accuracy of translation. IC wrote reports in English for each non-translated transcript, using broad topic guide headings. After the first phase of data collection, transcription and translation, JM, IC, PB, GLE and PCG discussed the findings, made adjustments to the topic guide and briefed the researchers. At the end of the second phase, all data were analysed using descriptive content analysis.35 GLE and JM made a list of themes emerging from the data and grouped these to make ‘higher-level’ codes. In a separate coding process, PCG and IC also developed higher level codes, and differences in the coding structures were discussed before coming to a consensus on the main themes. All Thai and English transcripts were coded by the research team. English-speaking researchers analysed translations and English reports of the Thai data, using deviant case analysis to check for bias. JM compiled a description of the findings which was reviewed and discussed before designing a discussion guide which PB and IC translated to Thai. This was used to feedback and discuss the main findings and interpretations in a focus group discussion (FGD) with five caregivers of children who had failed screenings at HPH 2 in the past week. The discussion took place in a closed room in the HPH and we paid participant travel expenses. PB conducted the discussion and IC made notes. These notes were discussed and used to distil the main findings.
Developing recommendations for action
We presented our findings and recommendations at a consultative meeting at Thammasat University Faculty of Medicine, inviting health workers from Pathum Thani Province, national DSPM team members and people involved in research and community child health work at the hospital (table 2). After the presentation, there was an open discussion about what actions were needed to improve screening and follow-up. We also discussed our results in two smaller meetings with researchers and paediatricians working in different areas of Thailand, who had experience in child development and were interested in the interaction between health services and communities. Notes from these meetings were consolidated by the research team into final recommendations.
Table 2.
Participants in consultative meetings
| Participants | n |
| Ministry of Public Health | |
| Director of the Department of Child Health | 1 |
| Pathum Thani Health Services | |
| Chief of the Department of Child and Maternal Health | 1 |
| Health workers from HPHs | 13 |
| Well-child clinic nurse | 1 |
| Thammasat University | |
| Vice Dean of the Faculty of Medicine | 1 |
| Researchers from the Department of Epidemiology | 2 |
| Faculty doctors | 6 |
| Social workers | 2 |
| Trainee social workers | 5 |
| Neonatologist | 1 |
| Paediatricians | 2 |
| Family medicine doctors | 2 |
| Child psychologist | 1 |
| Speech therapist | 1 |
| Child disability health worker | 1 |
| Research nurses | 3 |
| Mahidol University | |
| Researchers | 4 |
| Independent social work consultant | 1 |
| Total | 48 |
HPH, Health Promotion Hospital.
Results
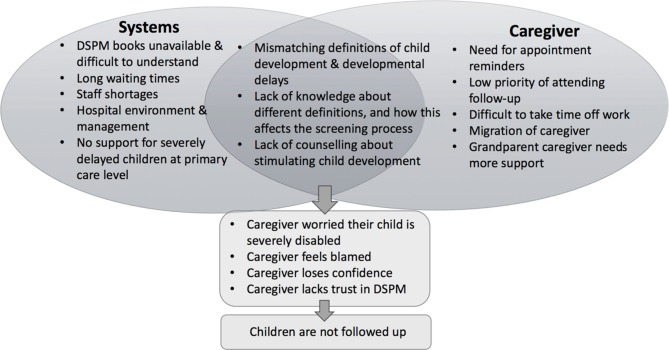
First, we present our findings from data collection with caregivers and HPH staff (table 3), then we present findings from consultative meetings. We found that health systems, community and communication barriers discouraged caregivers from bringing children who failed the screening to a follow-up appointment (figure 2).
Table 3.
Characteristics of caregivers and HPH staff
| n | Mean | |
| Caregiver characteristics | ||
| Relationship to child | ||
| Mother | 14 | |
| Grandmother | 5 | |
| Child characteristics | ||
| Sex | ||
| Female | 4 | |
| Male | 15 | |
| Age at initial DSPM screening (months) | ||
| 9 | 5 | |
| 18 | 5 | |
| 30 | 6 | |
| 32 | 2 | |
| 42 | 1 | |
| HPH staff characteristics | ||
| Age (years) | 41.3 | |
| Gender | ||
| Female | 6 | |
| Qualification (bachelor’s degree) | ||
| Nursing | 3 | |
| Public health | 2 | |
| Public healthcare | 1 | |
| Years as a health worker* | 10.2 | |
| Time since DSPM training* | ||
| Last year | 4 | |
| 1–2 years ago | 1 | |
*Only collected from health workers, not the chief.
DSPM, developmental screening programme; HPH, Health Promotion Hospital.
Figure 2.
Barriers to implementing developmental screening programme (DSPM).
Health systems barriers
Staff shortages
The DSPM is a universal screening programme, but it was not feasible to screen all children who came for vaccination. Usually, there is only one trained DSPM health worker per facility, with one set of equipment. Screening occurred before or after vaccination and took from 20 min to 1 hour to complete. Health workers only screened children who were within 4 weeks of being 9, 18, 30 or 42 months of age at their vaccination visit: ‘When children come for a vaccination, if they are within certain age range in which screening is to be done, we will separate this group of children out… we have difficulty regarding manpower, we do not have enough staff (and) sometimes the screening takes a long time’ (HW 01). A few health workers felt that the facility environment was distracting for children, which added to the time needed for the assessment. Caregivers described the vaccination clinic as ‘chaotic’ and ‘busy’ (TD 03).
Appointments and follow-up
Health workers felt that they needed to work as fast as possible: ‘The key is fast service…The clinic opens at 7.30 am because we know that parents must go to their office in the morning. We try not to let them wait too long.’ A parent in the FGD told us that she came at 05:00 to take a ticket, and most caregivers said that waiting times were long. Health workers were aware that this affected their ability to give general advice about child development and explain in detail about the screening. Some caregivers were told in advance that their child would also be screened, while others found out about the screening when they were at the HPH. When a child failed the screening, follow-up appointment cards were sometimes given, but not routinely, and caregivers who had not attended the follow-up had expected to be informed about the appointment: ‘No one has informed me yet to make the second appointment. Usually a member of staff from the clinic tells me directly to make a vaccination appointment’ (NFU 05). Health workers in HPH 2 mentioned having to call caregivers to remind them about appointments. Health workers had no time to do community outreach, although several said that home visits would be beneficial. One health worker from HPH 2 had asked community health volunteers to follow-up with the caregiver, although she did not discuss the effectiveness of this strategy.
Referral process
When a child was identified with a severe developmental delay, health workers were meant to follow the protocol of counselling caregivers and asking them to come for a follow-up visit at the HPH, and they should not refer them immediately. Some suspected that caregivers of children with severe delays did not attend a follow-up visit because they had taken their child to a private hospital or public referral centre. One health worker stated that caregivers were recommended to do this: ‘When we find some problems (with the child) we always recommend parents to take their child to a hospital directly. If we follow the referral procedures, this takes time. Then after they have done this, they can come back to us to get a formal patient referral letter’ (HW 3).
Supporting materials
Although all caregivers were meant to be given a DSPM manual at the screening, there were insufficient manuals and, at HPH 1, only caregivers of children who failed two or more components of the screening received the manual. Health workers at HPH 2 prioritised giving the manual to caregivers who lived within the catchment area of the facility:
We made copies of selected pages and gave them to parents. We do not have the colour version of the manual. We decided to give the manual to children who are from our area. However, we gave the manual to the children who must be reassessed regardless if they are from our area or not. (HW 03)
When the manual was received by caregivers, it was unclear whether it had been used. One caregiver preferred to use a mobile phone application (app), one grandparent could not read, and health workers reported that some caregivers found the writing too small and the content too dense to comprehend: ‘(there is) too much content in the manual. For older people, maybe they don’t like the small font size in the manual’ (HW 03). These findings about the manual were also triangulated in our discussion with caregivers.
Communication barriers between caregivers and health workers
Defining child development
Caregivers from all three groups mentioned observing their child’s developmental progress by comparing them with other neighbourhood children and a few compared their child to the guidance in the vaccination booklet given by the HPH. Caregivers usually tracked the progress of their child’s development through their ability to talk, to identify and memorise the names of objects, and to socialise with other children. One respondent used a mobile phone app which contained information about child development. Gross and fine motor skills were not mentioned by caregivers as an indication of child development. Most children watched television and cartoons, which allowed caregivers to do housework and was considered useful for memorising objects and learning behaviours. Watching TV was often considered ‘play’. Although caregivers did have some knowledge that play could benefit child development, understanding of how it could do so was limited: ‘Playing with toys can help. This can help my son to memorise surrounding objects. I tell him what the objects are and let him memorise them’ (NFU 05). This finding was triangulated by health workers: ‘Most parents think that playing can support child development. However, they are still lacking knowledge on child development. Usually, they let their child play with some normal toys which make sounds. However, parents aren’t aware of which aspects of child development can be enhanced by those toys’ (HW 01).
Several health workers noted that caregivers were stressed about the assessment, and one told us, ‘Parents are worried. We can tell from their reaction. Then we promise we will try our best, and when we tell them that their child passed the assessment they are happy’ (HW 02). There was also evidence that some caregivers, particularly grandparents, did not feel confident in knowing how to stimulate their child’s development: ‘If they say it’s good then I just believe it. I do not know much about child development’ (TD 03). A negative screening result was also difficult for older caregivers to understand: ‘I don’t know how his development is, I don’t go outside, so I don’t know… I want to know, but I don’t know how to ask. I didn’t study. The world moves very fast and I just can’t keep up’ (NFU 01).
Communicating failure at initial screening
Health workers did not routinely try to increase caregivers’ knowledge about the five domains of gross motor, fine motor, expressive language, receptive language and personal and social development. Caregivers of children who passed the screening and who were not followed-up were not given advice by health workers about child development, beyond saying that their child’s development was normal: ‘Mostly we do not tell parents about (child development) because we have limited time… We do not provide an explanation immediately. We only explain when a child cannot do things’ (HW 03). However, caregivers who were followed-up, and some caregivers in the feedback FGD, who were all from HPH 2, said they were not given advice by health workers, but just told to focus more on the area where the child had failed the assessment: ‘They just mentioned that my son’s development is good. However, my son must practice more on picking-up things’ (FU 01). It is possible that caregivers did not perceive this as advice because they did not view these activities as developmental milestones. The style of counselling used by health workers—not talking in terms of the child’s delays or developmental domains, but more about practical advice—could be an easier way to communicate about failing the screening. On the other hand, this indirect communication about child stimulation led some caregivers to believe that no further action was required: ‘The health worker didn’t say anything. So, I think my grandson is normal. If there is something unusual, the doctor should have told me already’ (NFU 01).
Some health workers were more direct in communicating a failed screening result: “We explain to the parent like this… ‘your child’s development is not normal in these aspects. It is possible that your child’s development has never been stimulated before. I would like you to find some time to play with your child’” (HW 01). Although a few health workers discussed the need to be positive in counselling caregivers, this did not occur in all cases, causing stress to caregivers. Those whose child failed the screening and who believed the results were worried that their child was severely disabled: ‘The mother of my grandson is quite worried about whether he is mentally retarded’ (TD 03).
When caregivers felt that their child could achieve the activities that they failed in the screening, they did not believe in the screening process, and one caregiver was angry with the insinuation that her child was severely disabled. This led some caregivers to believe that it was not useful to attend a follow-up appointment: ‘Some caregivers think it is a waste of time. They do not like the screening’ (HW 05). A few caregivers felt blamed by health workers for not stimulating their child’s development sufficiently: ‘She told me that my son’s development is slow. She also asked why I didn’t stimulate his development. That’s why I am stressed’ (NFU 02).
Caregiver barriers
Interpretation of the screening result
Although most caregivers thought the screening process was broadly beneficial and ‘better than nothing’ (FGD caregivers), if they thought it was not relevant to them they did not believe it was very important. One caregiver said: ‘parents blindly believe that their child is normal, and so do not take them to the assessment’ (TD 03). Health workers corroborated this and said that this parental confidence often meant that they did not attend the follow-up appointment: ‘Sometimes, parents are confident that their child’s development is normal… So they do not understand why they must bring their child back to us’ (HW 03). Some caregivers believed their child to be capable, or felt that they would improve as they grew up: ‘I accepted that my son’s development is a bit slow in socialisation aspect… once he is three years old, I will take him to a kindergarten. At that time, he should be socialising with other children without any problems’ (NFU 05). While grandparents often cared for children, health workers said that it was usually mothers who brought them for vaccination and screening. Therefore, any explanation given after a screening may not have reached a grandparent. This is particularly important as grandparents found the process more difficult to understand than mothers.
Conflicting priorities
Health workers and caregivers all felt that it was difficult for caregivers to manage the time for child development activities suggested in the manual. They also said that follow-up visits were not prioritised, particularly for busy working caregivers: ‘Sometimes parents are busy and do not have time for the follow-up appointment’ (NFU 05). Health workers found that a phone call would help motivate caregivers, but with high workloads it was unfeasible for them to call every caregiver: ‘if we call them, most of them will come back to us. But if we just made an appointment without calling, they rarely come back on the appointment date’ (HW 03). Migration of caregivers also made follow-up challenging: ‘Some children have already moved to other places. This makes following-up difficult’ (HW 05).
Policymaker and practitioner engagement
Health workers were invited to comment on a presentation of our findings and a one-page briefing (in Thai). They generally concurred with our results regarding the communication gap between health workers and caregivers, acknowledging that both caregivers and health workers needed to communicate better, particularly when a child failed the screening. They were aware that caregivers understood that a failed screening indicated a severe disability, which affected their likelihood of coming for a follow-up appointment.
Health workers concurred that they were under a lot of time pressure, with too many children to screen, and it was unfeasible to telephone caregivers for follow-up visits. They recommended screening tasks be shared with community health volunteers and other cadres, which was also mentioned by health workers that we interviewed: ‘In my opinion this task (DSPM screening) should not be limited to being done only by a nurse. It is possible that we can train village health volunteers, technical officers, and other healthcare staff to do this assessment’ (HW 02).
Health workers at the consultation felt that the DSPM manual needed to be simplified, and the toys used were often unfamiliar to caregivers and children, which may have led some children to fail the screening. They suggested using examples of low-cost household materials (such as old milk cartons instead of building blocks) in the manual. Health workers felt that increased awareness among caregivers could be promoted through postnatal training, videos, mobile phone apps and a comprehensive manual about child development instead of several books with different guidance.
The policymaker also concurred with our results and gave an update on new interventions or additions by MOPH which addressed some issues. There is a revised and simplified manual, with more pictures, and a freely available app of the screening process for caregivers to download and use whenever they want. The manual also has Quick Response Codes which link to videos that caregivers can watch. He encouraged health workers not to wait for policy changes and to implement change in their own HPH, and suggested some financial resources that HPHs could access if necessary. There was no on-the-job observation of health worker implementation of DSPM and health workers were only supported through an annual regional ‘empowerment workshop’ where provincial public health office representatives joined health workers to receive updates and refresher training, and present and discuss data on screening and referral rates. Some felt that this forum was an opportunity to share communication skills best practice, but stressed the need for dissemination and follow-up. In particular, it was important not to use the terminology ‘developmental delay’ and use a clear but positive communication approach. There was also some discussion about adding communication skills training and a communication test to the DSPM training where health workers would have to prove both technical and communication ability before passing the training and implementing DSPM.
Discussion
Our study found that health systems, community and communication barriers discouraged caregivers from bringing children who failed the screening to a follow-up appointment. We describe the recommendations resulting from our consultative process and discuss the potential for these strategies to be effective.
Increasing awareness of benefits and need for screening
When caregivers are more aware of the benefits of early child development, research has shown that they are more likely to effectively interact with their children.36 37 Broad health promotion strategies combined with targeted activity to those at increased risk, including migrants, could better prepare caregivers for the screening test and increase awareness about the need to stimulate child development. Public awareness campaigns could be implemented through television, video screening in the waiting room at the HPH and at day care centres. In addition, targeted training for teachers, day care workers and community health volunteers to increase awareness about developmental stimulation and the DSPM might encourage caregivers to act on recommended advice. Health promotion strategies are likely to be more effective if they are part of an integrated package of community-based interventions.38
Task-sharing for universal coverage and follow-up
Health workers only screened children who came for their vaccinations on time, and it is likely that those who were not screened or failed to return for screening were among the most vulnerable. Pathum Thani has a high number of internal migrants, and data suggest that, although they are eligible to access the Thai health system, outpatient utilisation is lower among internal migrants than among non-migrants.39 Data from 2004 to 2006 showed that half of internal migrants failed to collect the health cards which allow them to access the health system.40 41 A targeted community outreach strategy could improve access to screening and follow-up among migrant populations, implementing task-sharing to increase the availability of those able to screen. More research is needed to understand the feasibility and acceptability of task-sharing in this setting,42 but evidence suggests that lay health worker and parent interventions improve child development among typically developing children and those with developmental disorders in low-resource settings.43 44 In order to train, supervise and maintain the skills of village health workers, lay health workers and DSPM trained health workers, it is recommended to upgrade an existing health worker to be a DSPM champion. This individual could give initial and refresher training locally and facilitate sharing of practical and communication skills between DSPM workers, particularly about how to effectively engage caregivers, and encourage caregivers to communicate with each other about the child’s developmental progress. These champions could also lobby local authorities to ensure that adequate resources are invested in procuring DSPM materials. DSPM workers could be supported by mobile health (mhealth) interventions, modifying the MOPH app to add a module for DSPM workers, integrating communication and counselling skills that are based on experiential learning and best practices.
Mhealth strategies
Text message appointment reminders could be effective at increasing attendance at follow-up appointments in settings with high literacy and mobile phone coverage. There is some evidence to suggest that text message appointment reminders increase attendance at health appointments, and have the same impact on attendance as phone call reminders, while being more cost-effective.45–48 Combining education and outreach about DSPM with reminders may be more effective than messaging alone,49 especially among migrant populations and older grandparent caregivers with sight difficulties or low mobile phone literacy.50 51 HPHs could also explore the use of text and voice message reminders for older grandparent caregivers, which have been shown to be effective at increasing uptake of screening.52 The effectiveness of mhealth strategies such as message reminders or the DSPM app should be piloted and adjusted in consultation with users to optimise their effectiveness.
Targeting elder caregivers
The percentage of children under 18 living with grandparents and without both parents has increased in Thailand in the past two decades, from 2% in 1986 to 8% in 2006,53 driven largely by increased internal migration. Studies suggest that this shift in caretaking to the older generation may cause some stress, despite often being of economic benefit.53 54 In Thailand, 87% of persons over 60 years old only have a basic primary education, with older women being less educated than men.55 This helps to explain our findings that grandmothers were least likely to understand the advice given by health workers and found the DSPM manual difficult to follow. It will be important to pilot-test the revised manual with grandmothers to understand its effectiveness. A study in Thailand with children aged 6–12 years old found that those cared for by grandparents were more likely to have developmental delays, indicating the importance of engaging all caregivers to increase awareness of the importance of early child stimulation.56 Developing interventions targeted to grandparents would benefit from specifically engaging these groups in intervention design.57 For example, interventions could target elderly clubs which have a monthly meeting and exist in every subdistrict as a centre for activities which the club themselves decide upon.58 One study found that those who attend the clubs and those who visit young children have better social support networks.59 Around one-third of people over 60 participate in an elderly club, and membership is skewed to those living nearby.55 Before recommending elderly clubs as an intervention delivery mechanism, it is important to explore with older caregivers whether they are regular attenders, and the feasibility and acceptability of taking young children to these clubs.
Study limitations
Time and budget restrictions meant it was not feasible for us to interview a larger sample of stakeholders. However, while our current sample was small it provided valid data that enabled us to address the research question and data were triangulated between different stakeholders. Our discussions with policymakers and practitioners indicated that our findings and recommendations were likely to be of relevance beyond the immediate study context.
We were unable to engage caregivers adequately in discussing intervention options. The project was funded by a small grant, which meant that researchers could only be employed on a short-term basis to conduct interviews, instead of facilitating an entire iterative cycle of evaluation, taking action and re-evaluating. In the research and healthcare context of this study it was uncommon for users, health workers and policymakers to participate in a discussion of research findings together. Our approach of engaging caregivers separately from health workers and policymakers enabled each group to speak more freely. We anticipate the ongoing engagement of caregivers, health workers and policymakers in the development and evaluation of one or more of the suggested interventions.
Conclusion
Universal child developmental screening programmes can increase early detection and intervention to support caregivers and children with developmental disorders. The success of screening programmes is dependent on the ability of caregivers to follow advice after screening. Studies examining risk factors for lack of attendance at follow-up or lack of compliance to advice may enable targeting of programmes to at-risk groups, but unless there is meaningful engagement with caregivers to understand and address the barriers to following advice, even targeted programmes may not be effective.
We took an action research approach to explore the factors affecting the success of the Thai national universal DSPM and make recommendations for action. The DSPM has been integrated into routine vaccination visits at community HPHs, which is beneficial in a context of high vaccination coverage. However, implementing DSPM in this setting also meant that health workers were often too busy to counsel caregivers about the reasons for the screening, the meaning of the result and how to stimulate child development. When a failed screening was communicated as ‘developmental delay’, caregivers took it to mean ‘mental retardation’ which resulted in caregivers feeling worried at a failed screening, or feeling that the screening was irrelevant and not useful. This then led to a lack of attendance at follow-up visits. The lack of clear communication was particularly an issue for grandparent caregivers, who were more likely to have difficulty understanding advice and reading support materials if they were available. Our engagement process led to the proposition of mhealth interventions, interventions to target older caregivers and task-sharing to increase coverage and reach at-risk groups. Further engagement of caregivers in the development of these interventions will be necessary in order to improve follow-up rates after screening and improve the effectiveness of the programme.
Acknowledgments
We thank Dr Kanittha Buranapansak at Thammasat University, and all the study participants.
Footnotes
PCG and GLE contributed equally.
Contributors: All authors conceived the study during a workshop, and participated in study design, data analysis, participant engagement and write-up. JM wrote the first draft of the manuscript, and IC, PB, PCG and GLE commented, added to and edited the manuscript.
Funding: This research was funded by the Naughton/Clift Matthews Global Health Fund. University College London Global Engagement Funds provided additional support for JM’s travel, and the King’s College London Global Research Grant supported travel for PCG and GLE. Initial networking between the authors was facilitated by the Newton Fund in partnership with the British Council and Thailand Research Fund.
Competing interests: None declared.
Ethics approval: University College London Research Ethics Committee and Thammasat University Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available on application to the corresponding author. Participants gave informed consent for data sharing.
References
- 1.Black RE, Cousens S, Johnson HL, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 2010;375:1969–87. 10.1016/S0140-6736(10)60549-1 [DOI] [PubMed] [Google Scholar]
- 2.Elsabbagh M, Divan G, Koh YJ, et al. Global prevalence of autism and other pervasive developmental disorders. Autism Res 2012;5:160–79. 10.1002/aur.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boyle CA, Boulet S, Schieve LA, et al. Trends in the prevalence of developmental disabilities in US children, 1997-2008. Pediatrics 2011;127:1034–42. 10.1542/peds.2010-2989 [DOI] [PubMed] [Google Scholar]
- 4.McCoy DC, Peet ED, Ezzati M, et al. Early childhood developmental status in low- and middle-income countries: national, regional, and global prevalence estimates using predictive modeling. PLoS Med 2016;13:e1002034 10.1371/journal.pmed.1002034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collins PY, Pringle B, Alexander C, et al. Global services and support for children with developmental delays and disabilities: Bridging research and policy gaps. PLoS Med 2017;14:e1002393 10.1371/journal.pmed.1002393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA 2004;291:2581–90. 10.1001/jama.291.21.2581 [DOI] [PubMed] [Google Scholar]
- 7.WHO. mhGAP Intervention Guide. Geneva: WHO, 2010. [Google Scholar]
- 8.Emerson E, Einfeld S. Emotional and behavioural difficulties in young children with and without developmental delay: a bi-national perspective. J Child Psychol Psychiatry 2010;51:583–93. 10.1111/j.1469-7610.2009.02179.x [DOI] [PubMed] [Google Scholar]
- 9.Einfeld SL, Tonge BJ. Population prevalence of psychopathology in children and adolescents with intellectual disability: II. Epidemiological findings. J Intellect Disabil Res 1996;40:99–109. 10.1111/j.1365-2788.1996.tb00611.x [DOI] [PubMed] [Google Scholar]
- 10.Einfeld SL, Piccinin AM, Mackinnon A, et al. Psychopathology in young people with intellectual disability. JAMA 2006;296:1981–9. 10.1001/jama.296.16.1981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lecavalier L, Leone S, Wiltz J. The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. J Intellect Disabil Res 2006;50:172–83. 10.1111/j.1365-2788.2005.00732.x [DOI] [PubMed] [Google Scholar]
- 12.Lerthattasilp T, Charernboon T, Chunsuwan I, et al. Depression and burden among caregivers of children with autistic spectrum disorder. J Med Assoc Thai 2015;98(Suppl 2):S45–52. [PubMed] [Google Scholar]
- 13.Newacheck PW, Kim SE. A national profile of health care utilization and expenditures for children with special health care needs. Arch Pediatr Adolesc Med 2005;159:10–17. 10.1001/archpedi.159.1.10 [DOI] [PubMed] [Google Scholar]
- 14.Manning M, Homel R, Smith C. A meta-analysis of the effects of early developmental prevention programs in at-risk populations on non-health outcomes in adolescence. Child Youth Serv Rev 2010;32:506–19. 10.1016/j.childyouth.2009.11.003 [DOI] [Google Scholar]
- 15.Anderson LM, Shinn C, Fullilove MT, et al. The effectiveness of early childhood development programs. A systematic review. Am J Prev Med 2003;24:32–46. [DOI] [PubMed] [Google Scholar]
- 16.Schonwald A, Huntington N, Chan E, et al. Routine developmental screening implemented in urban primary care settings: more evidence of feasibility and effectiveness. Pediatrics 2009;123:660–8. 10.1542/peds.2007-2798 [DOI] [PubMed] [Google Scholar]
- 17.Guevara JP, Gerdes M, Localio R, et al. Effectiveness of developmental screening in an urban setting. Pediatrics 2013;131:30–7. 10.1542/peds.2012-0765 [DOI] [PubMed] [Google Scholar]
- 18.Rahman A, Divan G, Hamdani SU, et al. Effectiveness of the parent-mediated intervention for children with autism spectrum disorder in south Asia in India and Pakistan (PASS): a randomised controlled trial. Lancet Psychiatry 2016;3:128–36. 10.1016/S2215-0366(15)00388-0 [DOI] [PubMed] [Google Scholar]
- 19.Green J, Charman T, McConachie H, et al. Parent-mediated communication-focused treatment in children with autism (PACT): a randomised controlled trial. Lancet 2010;375:2152–60. 10.1016/S0140-6736(10)60587-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kakuma R, Minas H, van Ginneken N, et al. Human resources for mental health care: current situation and strategies for action. Lancet 2011;378:1654–63. 10.1016/S0140-6736(11)61093-3 [DOI] [PubMed] [Google Scholar]
- 21.Baum F, MacDougall C, Smith D. Participatory action research. J Epidemiol Community Health 2006;60:854–7. 10.1136/jech.2004.028662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hart E, Bond M. Action research for health and social care: a guide to practice. Buckingham: Open University Press, 1995. [Google Scholar]
- 23.McNiff J, Whitehead J. All you need to know about action research. New Delhi: Sage Publications, 2006. [Google Scholar]
- 24.Meyer J. Using qualitative methods in health related action research. BMJ 2000;320:178 10.1136/bmj.320.7228.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jagosh J, Macaulay AC, Pluye P, et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q 2012;90:311–46. 10.1111/j.1468-0009.2012.00665.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goodyear-Smith F, Jackson C, Greenhalgh T. Co-design and implementation research: challenges and solutions for ethics committees. BMC Med Ethics 2015;16:16 10.1186/s12910-015-0072-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. WHO. WHO mortality database 1980–2005. 2012. http://apps.who.int/healthinfo/statistics/mortality/whodpms/
- 28.Waitchaporn C, Theeranate C. Parents evaluation of developmental status (PEDS) to detect developmental and behavioural problems in well-baby clinic at Phramongkutklao Hospital. Thai J Pediatr 2011:50–7. [Google Scholar]
- 29.Royal College of Pediatricians of Thailand. Guideline in child health supervision. Bangkok: Sapphasarn, 2013. [Google Scholar]
- 30.Office NS. The 2012 disability survey. Bangkok: National Statistics Office, Ministry of information and communication technology, 2014. [Google Scholar]
- 31.Lindelow M, Hawkins L O. Government spending and central-local relations in Thailand’s health sector. Washington: World Bank, 2011. [Google Scholar]
- 32.Government of Thailand. Management framework of health facility in Thailand.Health MoP; https://phdb.moph.go.th/phdb2017/admin/files/userfiles/files/8-article_20130904140619.pdf (accessed 17 Sep 2017). [Google Scholar]
- 33.Kitreerawutiwong N, Jordan S, Hughes D. Facility type and primary care performance in sub-district health promotion hospitals in Northern Thailand. PLoS One 2017;12:e0174055 10.1371/journal.pone.0174055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ministry of Public Health. Framework of manpower planning: sub-district health promotion hospital. Strategy BoPa; http://cpho.moph.go.th/wp/wp-content/uploads/2013/12/6.%E0%B8%9A%E0%B8%97%E0%B8%97%E0%B8%B5%E0%B9%88-3-%E0%B8%9C%E0%B8%B1%E0%B8%87%E0%B9%82%E0%B8%84%E0%B8%A3%E0%B8%87%E0%B8%AA%E0%B8%A3%E0%B9%89%E0%B8%B2%E0%B8%87%E0%B8%AD%E0%B8%B1%E0%B8%95%E0%B8%A3%E0%B8%B2%E0%B8%81%E0%B8%B3%E0%B8%A5%E0%B8%B1%E0%B8%87.pdf (accessed on 17 Aug 2017). [Google Scholar]
- 35.Bos W, Tarnai C. Content analysis in empirical social research. Int J Educ Res 1999;31:659–71. 10.1016/S0883-0355(99)00032-4 [DOI] [Google Scholar]
- 36.Wacharasin C, Barnard K, Spieker S. Factors affecting toddler cognitive development in low-income families: implications for practitioners. Infants Young Child 2003;16:175–81. [Google Scholar]
- 37.Chivanon N, Wacharasin C. Factors influencing Thai parent-child interaction in a rapidly changing industrial environment. Int J Nurs Pract 2012;18(Suppl 2):8–17. 10.1111/j.1440-172X.2012.02024.x [DOI] [PubMed] [Google Scholar]
- 38.Kotchabhakdi NJ. Impact of a community-based program on early childhood development. J Pediatr Health Care 1999;13:S17–20. 10.1016/S0891-5245(99)90051-2 [DOI] [PubMed] [Google Scholar]
- 39.International Organisation for Migration. Thailand Migration Report. Bangkok: IOM, 2011. [Google Scholar]
- 40.Pearson E, Punpuing S, Jampaklay A, et al. The Mekong Challenge: underpaid, overworked and overlooked. Bangkok: International Labour Organisation, 2006. [Google Scholar]
- 41.Archavanitkul K, Thaweesit S, Suksinchai S, et al. The Thai State and Changes in AIDS and Reproductive health policies for undocumented migrants. Nakhon Pathom: Institute for Population and Social Research, Mahidol University, 2007. [Google Scholar]
- 42.Padmanathan P, De Silva MJ. The acceptability and feasibility of task-sharing for mental healthcare in low and middle income countries: a systematic review. Soc Sci Med 2013;97:82–6. 10.1016/j.socscimed.2013.08.004 [DOI] [PubMed] [Google Scholar]
- 43.Britto PR, Lye SJ, Proulx K, et al. Nurturing care: promoting early childhood development. Lancet 2017;389:91–102. 10.1016/S0140-6736(16)31390-3 [DOI] [PubMed] [Google Scholar]
- 44.Hamdani SU, Minhas FA, Iqbal Z, et al. Model for Service Delivery for Developmental Disorders in Low-Income Countries. Pediatrics 2015;136:1166–72. 10.1542/peds.2015-0861 [DOI] [PubMed] [Google Scholar]
- 45.Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, et al. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database Syst Rev 2013:CD007458 10.1002/14651858.CD007458.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lin H, Wu X. Intervention strategies for improving patient adherence to follow-up in the era of mobile information technology: a systematic review and meta-analysis. PLoS One 2014;9:e104266 10.1371/journal.pone.0104266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chen ZW, Fang LZ, Chen LY, et al. Comparison of an SMS text messaging and phone reminder to improve attendance at a health promotion center: a randomized controlled trial. J Zhejiang Univ Sci B 2008;9:34–8. 10.1631/jzus.B071464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Leong KC, Chen WS, Leong KW, et al. The use of text messaging to improve attendance in primary care: a randomized controlled trial. Fam Pract 2006;23:699–705. 10.1093/fampra/cml044 [DOI] [PubMed] [Google Scholar]
- 49.Bangure D, Chirundu D, Gombe N, et al. Effectiveness of short message services reminder on childhood immunization programme in Kadoma, Zimbabwe - a randomized controlled trial, 2013. BMC Public Health 2015;15:137 10.1186/s12889-015-1470-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen L, Du X, Zhang L, et al. Effectiveness of a smartphone app on improving immunization of children in rural Sichuan Province, China: a cluster randomized controlled trial. BMC Public Health 2016;16:909 10.1186/s12889-016-3549-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Uddin MJ, Shamsuzzaman M, Horng L, et al. Use of mobile phones for improving vaccination coverage among children living in rural hard-to-reach areas and urban streets of Bangladesh. Vaccine 2016;34:276–83. 10.1016/j.vaccine.2015.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Posadzki P, Mastellos N, Ryan R, et al. Automated telephone communication systems for preventive healthcare and management of long-term conditions. Cochrane Database Syst Rev 2016;12:CD009921 10.1002/14651858.CD009921.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jampaklay A, Vapattanawong P, Tangchonlatip K, et al. Children living apart from parents due to Internal Migration (CLAIM). Institute for Population and Social Research, Mahidol University, & UNICEF Thailand: Institute for Population and Social Research, Mahidol University, 2012. [Google Scholar]
- 54.Aree J. Growing up away from parents: children of migrants living with grandparents : Phodisita C, Taweesit S, Thai Family in Social and Demographic Transition. Nakhon Pathom, Thailand: IPSR, Mahidol University: IPSR, Mahidol University, 2009. [Google Scholar]
- 55.Knodel J, Terrawichitchainan B, Prachuabmoh V, et al. The situation of Thailand’s older population: an update based on the 2014 survey of older persons in Thailand. Singapore: Institutional knowledge at Singapore Management University, 2015. [Google Scholar]
- 56.Nanthamongkolchai S, Munsawaengsub C, Nanthamongkolchai C. Influence of child rearing by grandparent on the development of children aged six to twelve years. J Med Assoc Thai 2009;92:430–4. [PubMed] [Google Scholar]
- 57.Sullivan A, Winograd G, Verkuilen J, et al. Children on the autism spectrum: grandmother involvement and family functioning. J Appl Res Intellect Disabil 2012;25:484–94. 10.1111/j.1468-3148.2012.00695.x [DOI] [PubMed] [Google Scholar]
- 58.Torut B, Pongquan S. Impact of the Elderly Club on the Social Well-Being of the Rural Elderly in the Northeastern Region of Thailand. Poverty Public Policy 2012;4:58–78. 10.1002/pop4.6 [DOI] [Google Scholar]
- 59.Kuhirunyaratn P, Pongpanich S, Somrongthong R, et al. Social support among elderly in Khon Kean Province, Thailand. Southeast Asian J Trop Med Public Health 2007;38:936–46. [PubMed] [Google Scholar]