Abstract
The knee adduction moment (KAM) is a surrogate measure for medial compartment knee loading and is related to the progression of knee osteoarthritis. Toe-in and toe-out gait modifications typically reduce the first and second KAM peaks, respectively. We investigated whether assigning a subject-specific foot progression angle (FPA) modification reduces the peak KAM by more than assigning the same modification to everyone. To explore the effects of motor learning on muscle coordination and kinetics, we also evaluated the peak knee flexion moment and quadriceps-hamstring co-contraction during normal walking, when subjects first learned their subject-specific FPA, and following 20 min of training. Using vibrotactile feedback, we trained 20 healthy adults to toe-in and toe-out by 5° and 10° relative to their natural FPA, then identified the subject-specific FPA as the angle where each subject maximally reduced their larger KAM peak. When walking at their subject-specific FPA, 18 subjects significantly reduced their larger KAM peak; 8 by toeing-in and 10 by toeing-out. On average, subjects reduced their larger KAM peak by 18.6 ± 16.2% when walking at their subject-specific FPA, which was more than the reductions achieved when all subjects toed-in by 10° (10.0 ± 17.1%, p = .013) or toed-out by 10° (11.0 ± 18.3%, p = .002). Quadriceps-hamstring co-contraction and the peak knee flexion moment increased when subjects first learned their subject-specific FPA, but only co-contraction returned to baseline levels following training. These findings demonstrate that subject-specific gait modifications reduce the peak KAM more than uniformly assigned modifications and have the potential to slow the progression of medial compartment knee osteoarthritis.
Keywords: Knee osteoarthritis, Gait retraining, Real-time biofeedback, Knee adduction moment, Co-contraction
1. Introduction
Knee osteoarthritis affects roughly 10% of people over the age of 60 (Quintana et al., 2008). Over 90% of individuals with early stage knee osteoarthritis have symptoms isolated to the medial compartment (Hernborg and Nilsson, 1977). The external knee adduction moment (KAM) is correlated with the proportion of load transmitted through the medial compartment during the stance phase of gait (Kutzner et al., 2013) and is related to the presence (Hurwitz et al., 2002), severity (Sharma et al., 1998), and progression (Miyazaki et al., 2002) of medial compartment knee osteoarthritis. As a result, reducing the KAM is often the target of conservative interventions.
Several gait modifications such as increasing trunk sway, medial knee thrust, and changing the foot progression angle (FPA) have been shown to reduce the KAM (Fregly et al., 2007; Guo et al., 2007; Mündermann et al., 2008; Richards et al., 2017; Shull et al., 2013a). Many studies assign the same intervention to all subjects, yet not all subjects reduce their peak KAM, and some even increase it (Erhart et al., 2010; Hinman et al., 2012; Hunt and Takacs, 2014). Due to subject-to-subject variability in the effectiveness of different gait modifications, it has been suggested that the subject-specific selection of these modifications may enhance their effectiveness (Favre et al., 2016; Gerbrands et al., 2014, 2017; Shull et al., 2015; van den Noort et al., 2015).
FPA modification is amenable to a personalized approach. During the stance phase of walking, the KAM has two peaks, and in general, toeing-in reduces the first peak while toeing-out reduces the second peak. These modifications reduce the moment arm of the KAM by lateralizing the center-of-pressure during early and late stance, respectively (Guo et al., 2007; Lin et al., 2001; Shull et al., 2013a). Both toeing-in and toeing-out have been shown to reduce medial knee pain following 10 weeks of adoption (Hunt and Takacs, 2014; Shull et al., 2013b). Most people exhibit a larger first KAM peak during walking (Mündermann et al., 2005; Simic et al., 2013) and could likely reduce this peak by toeing-in; however, between 18% and 35% of people exhibit a larger second peak (Jenkyn et al., 2008; Ogaya et al., 2015) and would likely benefit more from toeing-out. Therefore, compared to assigning all subjects a toe-in or toe-out modification (Hunt and Takacs, 2014; Shull et al., 2013b), the effectiveness of FPA modification on alleviating medial compartment osteoarthritis symptoms could likely be improved by assigning subject-specific modifications aimed at reducing each subject’s larger KAM peak.
The external knee flexion moment (KFM) and knee flexor/extensor muscle activity also affect medial compartment loading (DeMers et al., 2014; Walter et al., 2010; Winby et al., 2009). The peak KFM is related to increased quadriceps activity, which increases knee loads (Tsai et al., 2013), and is moderately correlated with the rate of medial cartilage thickness loss (Chehab et al., 2014). Regression models that use both the KAM and KFM to predict medial contact force are more strongly correlated to medial contact force (r2 = 0.85–0.93) than those that use the KAM alone (r2 = 0.63–0.68) (Manal et al., 2015; Walter et al., 2010). Quadriceps-hamstring co-contraction also increases knee loads (Tsai et al., 2012), is related to the rate of cartilage volume loss (Hodges et al., 2016), but is not captured by either the KAM or KFM. Both the KFM and co-contraction can increase while adapting to new movement patterns (Bernshteĭn, 1967; Gribble et al., 2003; Voloshina et al., 2013). Although the KFM has been shown to increase when initially altering the FPA (Jenkyn et al., 2008; Simic et al., 2013), the effect of changing FPA on quadriceps-hamstring co-contraction is unknown. It is therefore important to discern which changes in the KFM and co-contraction are due to the learning of a novel task and which can be attributed to the gait modification itself.
The purpose of our study was to investigate if the selection of a subject-specific FPA enhances an individual’s ability to reduce their peak KAM. We hypothesized that subjects would achieve a greater reduction in their larger KAM peak by adopting a subject-specific FPA than if all subjects were assigned a uniform toe-in or toe-out gait. We also assessed the effect of training on the KFM and quadriceps-hamstring co-contraction and hypothesized that these measures would increase when subjects initially learn their new subject-specific FPA but return to baseline levels after a 20-min training period.
2. Methods
2.1. Participants
Twenty healthy adults (26 ± 5 y.o.) participated after giving informed consent to a Stanford University Institutional Review Board approved protocol. Individuals were excluded if they were currently experiencing lower extremity pain or if they had any lower extremity surgery or injury during the past year.
2.2. Data collection
Subjects performed 7 different trials during a single data collection session: a static calibration trial, a baseline walking trial, 4 FPA evaluation trials, and a 20 min training trial.
Nineteen retroreflective markers were placed bilaterally on the 2nd and 5th metatarsal heads, calcanei, malleoli, femoral epicondyles, anterior and posterior superior iliac spines, and the C7 vertebrae. Fourteen additional markers were used to aid in limb tracking. Marker data were collected with an optical motion capture system at 80 Hz (Motion Analysis Corporation, Santa Rosa, CA, USA). Ground reaction forces from a split-belt treadmill (Bertec Corporation, Columbus, OH, USA) and electromyograms (Delysis Inc., Boston, MA, USA) from the vastus lateralis and biceps femoris were collected at 1600 Hz. Force and marker data were streamed into MATLAB R2015b (MathWorks Corporation, Natick, MA, USA) for real-time estimation of FPA. FPA was calculated as the average angle between the line connecting the markers on the calcaneus and second metatarsal head and the forward direction of the treadmill (Rutherford et al., 2008) during 15–40% of stance phase.
Subjects first performed a static calibration trial, which we used to estimate joint center locations, joint axes of rotation, and tracking marker reference locations. The knee joint center and axis of rotation were estimated as the mid-point between the medial and lateral femoral epicondyle markers and the line connecting the markers, respectively. The ankle joint center was defined as the mid-point between the medial and lateral malleoli markers. After choosing a comfortable walking speed (mean ± SD; 1.15 ± 0.10 m/s), subjects practiced treadmill walking for 5 min, then performed a 2-min baseline walking trial. The final 20 steps of this trial were used to determine their baseline FPA, the larger of their two KAM peaks, and to estimate baseline kinematics, kinetics, and muscle activity (see Section 2.3).
To determine their subject-specific FPA, subjects performed four 2-min FPA evaluation trials targeting each of 5° and 10° of toe-in and toe-out relative to their baseline FPA. Two C2 vibrotactile motors (Engineering Acoustics, Inc., Casselberry, FL, USA) affixed to the medial and lateral aspects of the proximal tibia provided vibrotactile feedback following an unsuccessful step when the FPA was not within 2° of each trial’s target angle. A single limb was chosen randomly for feedback and kinematic, kinetic, and electromyographic analysis. The final 20 successful steps of each evaluation trial were used for analysis (see Section 2.3). The subject-specific FPA was selected as the 5° or 10° change in FPA that reduced each subject’s larger baseline KAM peak by the greatest amount. One subject (subject 10) found 10° toe-into be excessively uncomfortable, so their subject-specific FPA was selected as 5° toe-in, which also reduced their larger KAM peak. If there was not a significant difference in magnitude between the KAM peaks at baseline, the peak that was maximally reduced from a change in FPA, without an increase in the other peak, was analyzed. We defined the evaluation trial corresponding to the subject-specific FPA as the subject-specific FPA evaluation trial.
Following the evaluation trials, subjects trained at their subject-specific FPA with feedback for 20 min, taking breaks every 5 min. Feedback was given for unsuccessful steps, and the final 20 successful steps of the training were analyzed.
2.3. Data processing
Motion and force data were low-pass filtered at 15 Hz using a 4th order, zero-phase Butterworth filter. Knee moments were calculated as the moment of the ground reaction force about the knee joint center (Shull et al., 2011). Knee moments are reported in the tibial reference frame with the mediolateral (y) axis parallel to the knee rotation axis, the anterior-posterior (x) axis perpendicular to the y-axis and the line connecting the knee and ankle joint centers, and a mutually perpendicular z-axis. To report positive values for both the early and late stance KFM peaks, the absolute value of the moment was identified as the KFMabs. The first and second KAM and KFMabs peaks were identified as the maxima during 0–50% and 51–100% of the stance phase. To identify each subject’s larger KAM peak at baseline, the percent difference in KAM peaks was calculated for each step by subtracting the second peak from the first peak, then dividing by the larger of the peaks. Unless otherwise noted, reported changes in the KFMabs are from the same half of stance phase as each subject’s larger KAM peak. Peak knee moments, percent difference in KAM peaks, and FPA were averaged over 20 steps.
To further assess the efficacy of the FPA modifications, we used a linear regression of the form
| (1) |
to estimate the first and second medial contact force peaks from the KAM and KFMabs peaks. For a single subject with an instrumented knee implant, Walter et al. (2010) reported c1, c2, c3 values of 0.38, 0.13, and 0.50. Manal et al. (2015) reported coefficients of 0.34, 0.13, and 0.83 for a study of ten subjects following ACL reconstruction, where medial contact force was estimated from an electromyogram-driven model. We estimate medial contact force with an average of the aforementioned coefficients: 0.36, 0.13, and 0.67.
Electromyography was used to estimate the magnitude of muscle activity and co-contraction during 4 phases of the gait cycle: load acceptance (0–10% gait cycle), midstance (10–30%), terminal stance (30–50%), and terminal swing (88–100%) (Perry, 1992). Electromyograms were bandpass filtered (30–500 Hz), rectified, and passed through a critically damped, lowpass filter (20 Hz). Each muscle’s signal was averaged over 20 steps, then normalized to the muscle’s maximum average signal during the baseline trial. We computed the average activation during the aforementioned phases of the gait cycle to assess changes in muscle activity between trials (Fridlund and Cacioppo, 1986). We also computed the quadriceps-hamstring co-contraction index as the average value of the overlapping envelope created by the vastus lateralis and biceps femoris signals during the gait phases (Damiano et al., 2000).
To further study the mechanism by which FPA modifications affect the KAM, we evaluated the frontal plane ground reaction force magnitude and KAM moment arm (Shull et al., 2013a). To further investigate changes in the KAM moment arm, we evaluated the mediolateral distance between right and left centers-of-pressure and knee joint centers during consecutive steps (Shull et al., 2013a). Because modifying the FPA can change the mediolateral positions of the heel and forefoot without changing step width, we calculated step width as the distance between the right and left centers-of-pressure (Donelan et al., 2001) at 50% stance. All measurements were averaged over 20 steps.
2.4. Statistics
One-sample t-tests were used to assess if the baseline percent difference between the KAM peaks, the percent reductions in peak knee moments, and percent reductions in medial contact forces were different than zero. Paired t-tests were used to compare peak knee moments, medial contact forces, co-contraction, muscle activity, and secondary kinematic measures between different trials. Prior to analysis, the normality of the data was assessed with a Shapiro-Wilk test. For comparisons involving non-normally distributed data, a Wilcoxon signed rank test was used instead of a t-test. All tests were conducted using SPSS v21.0 (IBM Corp, Chicago, IL, USA). Significance was set at p < .05. All values are reported as mean ± standard deviation.
3. Results
During the baseline trial, 17 of 20 subjects had a significantly larger first KAM peak than second peak. Fifteen of these subjects significantly reduced their first KAM peak by changing their FPA (Fig. 1). Of these, 8 maximally reduced their first KAM peak by toeing-in and 7 by toeing-out. One subject (subject 18) did not have a significant difference between the magnitudes of their first and second KAM peaks (Table 1). For this subject, the second KAM peak was reduced the most; this was achieved by toeing-out by 10°. The remaining 2 subjects who walked with a larger second KAM peak significantly reduced it by toeing-out. As a group, 18 subjects reduced their larger KAM peak by walking at their subject-specific FPA, 8 by toeing-in and 10 by toeing-out (Table 1).
Fig. 1.
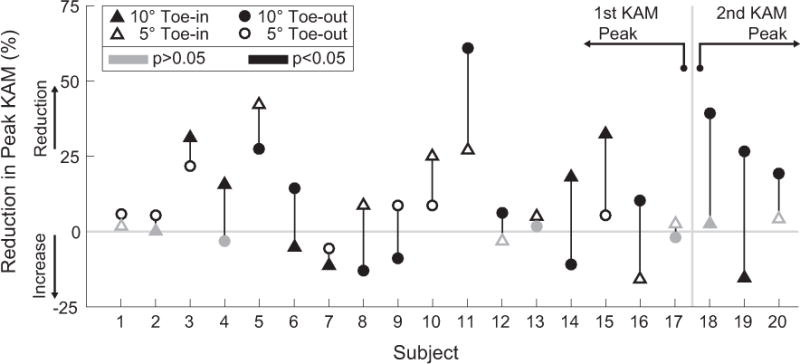
The reduction in the peak knee adduction moment (KAM) for each subject from a select two of the four foot progression angle (FPA) modifications; the two FPAs shown for each subject represent the FPA that yielded the greatest and least reduction in that subject’s peak KAM. Significant (p < .05) changes relative to baseline are represented with black markers, while non-significant changes are shown as gray markers. Subjects are ordered from left to right based on the percent difference between their first and second KAM peaks at baseline (Table 1) with subject 1 having the largest first KAM peak relative to their second peak. The reduction in the first KAM peak is shown for subjects 1–17 and the reduction in the second peak for subjects 18–20. Fifteen of 17 subjects with a larger first KAM peak at baseline were able to significantly reduce this peak, 8 by toeing-in and 7 by toeing-out. Subjects 18–20 reduced their second KAM peak the most by toeing-out. It is important to note that 7 of the 20 subjects could have significantly increased in their peak KAM had the wrong FPA modification been assigned to them.
Table 1.
Reductions in the peak knee adduction moment (KAM), knee flexion moment (KFMabs), and estimated medical contact force when all subjects walked at their subject-specific FPA. When walking at this FPA, 18 of 20 subjects significantly reduced their KAM peak and 13 significantly reduced their estimated medial contact force compared to baseline. For subjects 18–20, all reported values are for the second peak of each parameter. (bold: p < .05).
| Subject | Baseline difference in KAM peaks (%) | Subject-specific FPA (deg)
|
Reduction in peak KAM (%) | Reduction in peak KFMabs (%) | Reduction in estimated medial contact force (%) | |
|---|---|---|---|---|---|---|
| Toe-in | Toe-out | |||||
| 1 | 60.0 ± 5.4 | 5 | 6.0 ± 8.2 | 10.3 ± 11.9 | 5.4 ± 6.4 | |
| 2 | 52.5 ± 6.4 | 5 | 5.6 ± 7.4 | −5.8 ± 7.1 | 1.1 ± 4.3 | |
| 3 | 50.7 ± 13.6 | 10 | 31.2 ± 6.6 | −15.6 ± 10.8 | 6.7 ± 3.8 | |
| 4 | 45.5 ± 7.0 | 10 | 15.8 ± 6.5 | − 12.4 ± 16.9 | 8.0 ± 5.0 | |
| 5 | 39.9 ± 6.1 | 5 | 42.0 ± 6.9 | −37.8 ± 13.3 | 11.0 ± 3.2 | |
| 6 | 39.2 ± 14.3 | 10 | 14.3 ± 16.1 | −23.1 ± 20.2 | −1.0 ± 6.0 | |
| 7 | 39.1 ± 4.8 | 5 | −5.6 ± 9.8 | 22.1 ± 14.7 | 0.5 ± 6.5 | |
| 8 | 37.7 ± 5.4 | 5 | 8.6 ± 8.9 | −26.4 ± 18.4 | 1.1 ± 4.6 | |
| 9 | 36.1 ± 8.9 | 5 | 8.8 ± 9.7 | −12.5 ± 9.8 | 0.4 ± 6.0 | |
| 10 | 35.1 ± 9.7 | 5 | 24.4 ± 9.7 | −16.3 ± 15.3 | 6.6 ± 5.0 | |
| 11 | 34.4 ± 7.2 | 10 | 60.9 ± 7.4 | −19.3 ± 9.9 | 13.7 ± 2.3 | |
| 12 | 31.1 ± 6.2 | 10 | 6.3 ± 8.1 | −3.2 ± 8.5 | 2.0 ± 4.4 | |
| 13 | 29.2 ± 6.9 | 5 | 7.5 ± 6.9 | −11.4 ± 20.8 | 2.6 ± 5.2 | |
| 14 | 27.5 ± 6.6 | 10 | 18.0 ± 5.4 | 2.9 ± 12.2 | 10.5 ± 3.6 | |
| 15 | 21.7 ± 5.5 | 10 | 32.4 ± 10.5 | −85.3 ± 54.8 | 12.2 ± 8.3 | |
| 16 | 17.2 ± 9.2 | 10 | 10.2 ± 10.7 | 19.8 ± 8.8 | 9.0 ± 4.6 | |
| 17 | 17.0 ± 6.4 | 5 | 2.7 ± 6.0 | −17.6 ± 21.5 | −0.3 ± 4.7 | |
| 18 | −0.8 ± 9.3 | 10 | 39.2 ± 4.5 | 10.7 ± 13.1 | 23.9 ± 3.9 | |
| 19 | −14.6 ± 7.8 | 10 | 26.6 ± 7.9 | −20.9 ± 14.5 | 11.1 ± 5.5 | |
| 20 | −26.6 ± 6.6 | 10 | 19.3 ± 6.8 | −6.5 ± 20.8 | 10.4 ± 4.7 | |
On average, when walking at their subject-specific FPA, subjects reduced their larger KAM peak by 18.6 ± 16.2% compared to baseline, which was greater than the reductions observed when everyone toed-in by 5° (7.7 ± 14.1%, p < .001), toed-in by 10° (10.0 ± 17.1%, p = .013), toed-out by 5° (8.7 ± 11.9%, p < .001), or toed-out by 10° (11.0 ± 18.3%, p = .002) (Fig. 2). This result is significant using a Benjamini-Hochberg procedure with a false discovery rate of 0.05 (Benjamini and Hochberg, 1995).
Fig. 2.
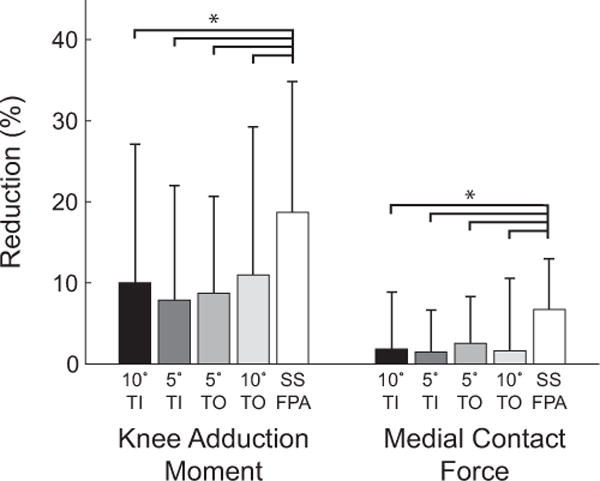
The percent reduction in the peak knee adduction moment and peak estimated medial contact force for 5° and 10° toe-in (TI) and toe-out (TO) gaits as well as at the subject-specific foot progression angle (SS FPA). When walking at their subject-specific foot progression angle, subjects achieved a greater reduction in both the knee adduction moment and medial contact force compared to when all subjects walked at any of the 5° or 10° foot progression angles. (* p < .05) All results are significant using a Benjamini-Hochberg procedure with false discovery rate of 0.05.
During the subject-specific FPA evaluation trial, the peak KFMabs increased by 12.4 ± 23.1% (p = .023) compared to baseline. After 20 min of training, the peak KFMabs remained 24.0 ± 25.5% greater than baseline (p < .001). Despite the increase in the KFMabs, 13 of the 20 subjects reduced their estimated medial contact force when walking at their subject-specific FPA compared to baseline (Table 1), with an average reduction among all subjects of 6.7 ± 6.3%. This reduction was significantly greater than the reductions observed when all subjects toed-in by 5° (1.4 ± 5.1%, p < .001), toed-in by 10° (1.8 ± 7.0%, p = .013), toed-out by 5° (2.6 ± 5.8%, p = .003), or toed-out by 10° (1.6 ± 8.9%, p < .001) (Fig. 2).
Quadriceps-hamstring co-contraction was greater than baseline during the FPA evaluation trial for loading response (p = .009), midstance (p = .025), terminal stance (p < .001), and terminal swing (p = .006) phases of gait. Co-contraction was no longer significantly different from baseline during any of the phases after 20 min of training (Fig. 3c). Compared to baseline, vastus lateralis activity significantly increased during the subject-specific FPA evaluation trial for all 4 phases of gait; this activity remained elevated after 20 min of training for all phases except terminal swing (Fig. 3a). In contrast, during the subject-specific FPA evaluation trial, biceps femoris activity was significantly greater than baseline during the loading response, midstance, and terminal stance phases but returned to baseline levels after 20 min of training (Fig. 3b).
Fig. 3.
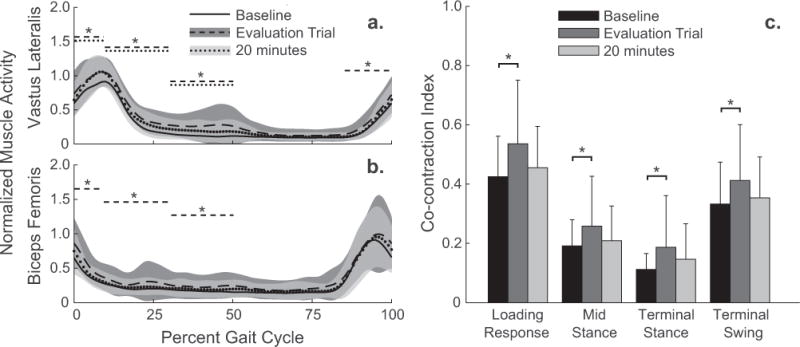
(a) Vastus lateralis and (b) biceps femoris normalized muscle activity and (c) co-contraction during four phases of the gait cycle. Muscle activity and co-contraction increased from baseline to the subject-specific FPA evaluation trial. Following 20 min of training, co-contraction and biceps femoris activity reduced to baseline levels, while vastus lateralis activity remained elevated. (* p < .05; dashed line: evaluation trial vs. baseline, dotted line: following 20 min of training vs. baseline).
On average, the first KAM peak was reduced when subjects toed-in by 10° (p = .012) and trended towards being reduced (p = .061) when subjects toed-out by 10° (Table 2). The frontal plane ground reaction force magnitude at the time of the first KAM peak trended towards being larger than baseline for 10° toe-in gait (p = .057) and was not greater than baseline for 10° toe-out gait (p = .526). The KAM moment arm (Fig. 4a) at the time of the first KAM peak was smaller than baseline for 10° toe-in gait (p < .001) and trended towards being smaller for 10° toe-out gait (p = .071). The mediolateral distance between centers-of-pressure (Fig. 4c) at the time of the first KAM peak was greater than baseline for both 10° toe-in (p = .042) and 10° toe-out (p < .001) gaits; however, the mechanism for this increase was different for each gait. For 10° toe-in gait, the lateral shift in center-of-pressure during early stance was caused by lateralization of the heel when toeing-in, but not increasing step width. For toe-out gait, the lateral shift in center-of-pressure during early stance occurred due to an increase in step width (Fig. 4c, d, Table 2).
Table 2.
Changes in the foot progression angle (FPA), step width, knee adduction moment (KAM) peaks, and knee flexion moment (KFMabs) peaks during the baseline, 10° toe-in, and 10° toe-out trials. The FPA is reported as an absolute measure with respect to the forward direction. This is unlike the relative FPAs which we report elsewhere. Knee moments are normalized and reported as percent body-weight (BW) times height (ht). P-values compare baseline with toe-in or toe-out gait.
| Baseline | 10° Toe-in
|
10° Toe-out
|
|||
|---|---|---|---|---|---|
| p-value | p-value | ||||
| FPA (deg, absolute) | 2.6 ± 3.7 | −7.3 ± 3.6 | <.001 | 12.4 ± 3.7 | <.001 |
| Step Width at 50% Stance (cm) | 19.3 ± 3.0 | 19.1 ± 3.1 | .690 | 25.1 ± 5.3 | <.001 |
| KAM First Peak | |||||
| (%BW*ht) | 2.86 ± 0.92 | 2.59 ± 1.00 | 2.74 ± 1.12 | ||
| Reduction (%) | 10.5 ± 16.8 | .012 | 7.4 ± 16.6 | .061 | |
| KAM Second Peak | |||||
| (%BW*ht) | 2.04 ± 0.88 | 2.00 ± 0.85 | 1.51 ± 0.73 | ||
| Reduction (%) | 1.1 ± 14.5 | .737 | 27.6 ± 17.0 | <.001 | |
| KFMabs First Peak | |||||
| (%BW*ht) | 3.12 ± 1.08 | 3.36 ± 1.30 | 3.54 ± 1.12 | ||
| Reduction (%) | −10.9 ± 29.2 | .112 | −18.7 ± 28.6 | .009 | |
| KFMabs Second Peak | |||||
| (%BW*ht) | 1.90 ± 0.63 | 1.73 ± 0.77 | 1.84 ± 0.70 | ||
| Reduction (%) | 6.0 ± 32.3 | .417 | 1.5 ± 26.0 | .797 | |
Fig. 4.
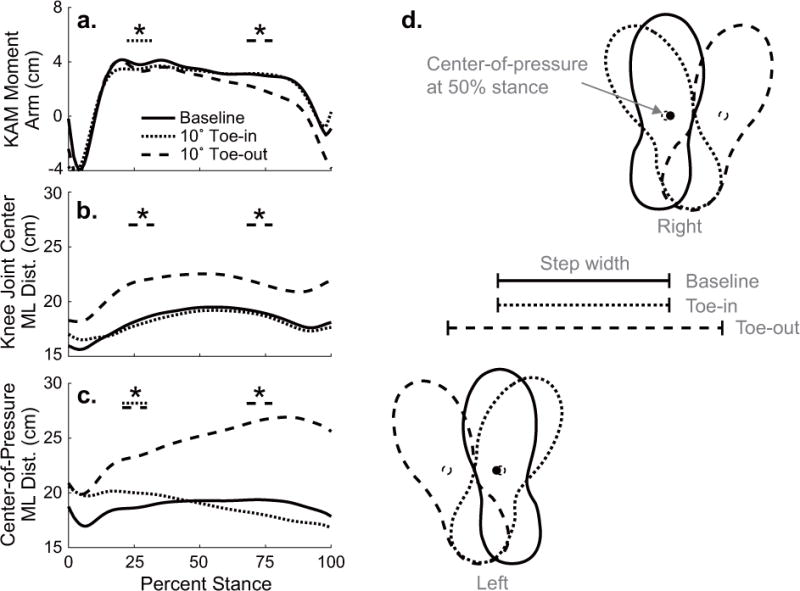
(a) The knee adduction moment (KAM) moment arm, (b) mediolateral (ML) distance between knee joint centers, and (c) mediolateral distance between centers-of-pressure during the baseline (solid), 10° toe-in (dotted), and 10° toe-out (dashed) trials. Toe-in and toe-out gaits are compared to baseline (* p < .05) at the time of the first and second KAM peaks. (d) A schematic of foot placement for consecutive left and right steps illustrates the average center-of-pressure trajectories from c. At the time of the first KAM peak, the KAM moment arm was smaller when subjects toed-in (p < .001) and trended towards being smaller when subjects toed-out (p = .071). For both FPAs, subjects lateralized their heels during early stance. When toeing-in, this lateralization was achieved by internally rotating the foot about the midfoot. When toeing-out, however, subjects lateralized their heels by increasing their step width (Table 2).
4. Discussion
The purpose of our study was to test whether assigning a subject-specific FPA reduces the peak KAM by more than a uniformly assigned FPA. In support of this hypothesis, we found that subjects reduced their larger KAM peak by more when walking at their subject-specific FPA than when all subjects toed-in or toed-out by 5° or 10°. We also hypothesized that the peak KFMabs and quadriceps-hamstring co-contraction would increase initially, but return to baseline levels following 20 min of training. This hypothesis was only partially confirmed as the peak KFMabs and quadriceps-hamstring co-contraction increased when initially learning the subject-specific FPA, but only co-contraction returned to baseline levels after training.
Our results demonstrate the importance of assessing the kinetics of every subject at both baseline and when walking with a range of different gait modifications before selecting a new gait pattern. Toeing-out typically reduces the second KAM peak by more than toeing-in reduces the first peak (Simic et al., 2013); however, in our study, only 3 of 20 subjects walked with even peaks or a larger second peak at baseline, suggesting that the effectiveness of toe-out gait may only target the larger KAM peak for as few as 15% of the population (Table 1). Similarly, although toeing-in typically reduces the first KAM peak (Shull et al., 2013a), 7 of the 17 subjects in our study who had a larger first KAM peak maximally reduced this peak by toeing-out, not toeing-in (Fig. 1). Potentially of greatest importance, 35% (7 out of 20) of our subjects would have experienced an increase in their peak KAM had the wrong FPA modification been chosen.
On average, our subjects trended towards reducing their first KAM peak when toeing-out by 10° (Table 2). This finding is consistent with previously reported reductions in the first KAM peak when subjects toed-out by 7° (Hunt and Takacs, 2014), but is inconsistent with increases observed when subjects toed-out by 10–16° (Favre et al., 2016; Simic et al., 2013). These differences may be due to secondary kinematic changes that have been shown to impact the KAM peaks (Favre et al., 2016; van den Noort et al., 2015). For example, our subjects walked with a 5.9 cm greater step width while toeing-out by 10° compared to baseline, and increasing step width can reduce the KAM (Favre et al., 2016; Fregly et al., 2008) by lateralizing the center-of-pressure during the entire stance phase (Fig. 4). Simic et al. (2013) reported a 2 cm increase in step width when subjects toed-out by 16.3°; however, in this study, step width was defined as the mediolateral distance between ankle joint centers, which can be affected by FPA. Their reported increase in step width would likely be greater using our midfoot-oriented definition of step width, which reduces the effect that foot rotation has on step width estimations (Fig. 4d). The increase in step width that accompanied toe-out gait precludes us from comparing the direct effects of altering FPA on the KAM, but it nevertheless appears to be an advantageous secondary kinematic change.
Quadriceps-hamstring co-contraction and the peak KFMabs increased when subjects initially learned their new gait. Co-contraction subsequently decreased after 20 min of training (Fig. 3c), which corresponds with observations made when learning upper extremity reaching tasks (Gribble et al., 2003). Unlike co-contraction, the peak KFMabs remained elevated following 20 min of training. The increase in the peak KFMabs aligns with previously reported increases of 9–21% after FPA modification (Hunt and Takacs, 2014; Simic et al., 2013). Estimating medial contact force is a valuable way to differentiate between the opposing effects of gait modifications on the KAM and KFMabs peaks. Although 18 of 20 subjects reduced their larger KAM peak at their subject-specific FPA, 5 of these subjects did not reduce their estimated medial contact force because of a simultaneous increase in their peak KFMabs. Our regression-based estimation of medial contact force is less accurate than direct measurement, but it may provide a more holistic evaluation of changes in medial compartment loading that result from gait modifications that reduce the KAM but increase the KFM than assessing the KAM alone.
There were several limitations to our study. First, our cohort was composed of healthy individuals. Nevertheless, our subjects reduced their first KAM peak by 10.5% when toeing-in by 10°, which is similar to the 7–20% reductions in osteoarthritic cohorts who toed-in by relative angles of 5–14° (Shull et al., 2013a, 2013b; Simic et al., 2013). Similarly, our subjects reduced their second KAM peak by 27.6% when toeing out by 10°, which aligns with the 10–36% reductions in osteoarthritic cohorts who toed-in by 7–16° (Hunt and Takacs, 2014; Simic et al., 2013). Future studies are necessary to discern whether individuals with knee osteoarthritis will achieve similar KAM reductions by adopting a subject-specific FPA as healthy individuals and how these modifications affect other lower body joints after long term adoption. Additionally, we only report changes in muscle co-contraction and the KFMabs after training during a single laboratory visit. Different learning effects may be apparent in osteoarthritic individuals over the course of longer term gait retraining protocols. Finally, we estimated medial contact force from knee moments using previously published regressions based on contact force measurements in a single subject with an instrumented knee implant (Walter et al., 2010) and simulation-based estimates from ten ACL-reconstructed subjects (Manal et al., 2015). Due to the small sample size and differences in subject population from which these regressions were computed, caution should be exercised when interpreting our regression-based medial contact force estimates. A future study reporting a similar regression relating knee moments to simulated contact force in a large cohort of osteoarthritic patients would enhance the usefulness of this simple model for assessing gait modification efficacy.
Our study demonstrates the importance of selecting subject-specific gait modifications rather than assigning a uniform modification to everyone. We found that individualizing each subject’s FPA modification based on their baseline kinetics and kinetic response to different FPAs yielded greater KAM reductions than had a uniform modification been assigned to the entire cohort. Individualized gait retraining is a promising avenue for reducing loads in the medial compartment of the knee and potentially slowing the progression of medial compartment knee osteoarthritis.
Acknowledgments
We would like to thank Julie Kolesar, Andrea Finlay, and Cara Welker for their assistance in data collection and statistical analysis. This material is based upon work supported by the National Science Foundation Graduate Research Fellowship under Grant No. DGE-114747. This work was also supported in part by Merit Review Award Number I01 RX001811 from the United States (U. S.) Department of Veterans Affairs Rehabilitation R&D (Rehab RD) Service. The funding sources did not play a role in data analysis, manuscript preparation, or the decision to publish this work.
Footnotes
Conflict of Interest
We, the authors, do not have a conflict of interest related to this work.
References
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57:289–300. [Google Scholar]
- Bernshteĭn N. The Co-ordination and Regulation of Movements. Permagon Press; Oxford: 1967. [Google Scholar]
- Chehab EF, Favre J, Erhart-Hledik JC, Andriacchi TP. Baseline knee adduction and flexion moments during walking are both associated with 5 year cartilage changes in patients with medial knee osteoarthritis. Osteoarthr Cartil. 2014;22:1833–1839. doi: 10.1016/j.joca.2014.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damiano DL, Martellotta TL, Sullivan DJ, Granata KP, Abel MF. Muscle force production and functional performance in spastic cerebral palsy: relationship of cocontraction. Arch Phys Med Rehabil. 2000;81:895–900. doi: 10.1053/apmr.2000.5579. [DOI] [PubMed] [Google Scholar]
- DeMers MS, Pal S, Delp SL. Changes in tibiofemoral forces due to variations in muscle activity during walking. J Orthop Res. 2014;32:769–776. doi: 10.1002/jor.22601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donelan JM, Kram R, Kuo AD. Mechanical and metabolic determinants of the preferred step width in human walking. Proc Biol Sci. 2001;268:1985–1992. doi: 10.1098/rspb.2001.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erhart JC, Mündermann A, Elspas B, Giori NJ, Andriacchi TP. Changes in knee adduction moment, pain, and functionality with a variable-stiffness walking shoe after 6 months. J Orthop Res. 2010;28:873–879. doi: 10.1002/jor.21077. [DOI] [PubMed] [Google Scholar]
- Favre J, Erhart-Hledik JC, Chehab EF, Andriacchi TP. General scheme to reduce the knee adduction moment by modifying a combination of gait variables. J Orthop Res. 2016;34:1547–1556. doi: 10.1002/jor.23151. [DOI] [PubMed] [Google Scholar]
- Fregly BJ, Reinbolt JA, Chmielewski TL. Evaluation of a patient-specific cost function to predict the influence of foot path on the knee adduction torque during gait. Comput Methods Biomech Biomed Engin. 2008;11:63–71. doi: 10.1080/10255840701552036. [DOI] [PubMed] [Google Scholar]
- Fregly BJ, Reinbolt JA, Rooney KL, Mitchell KH, Chmielewski TL. Design of patient-specific gait modifications for knee osteoarthritis rehabilitation. IEEE Trans Biomed Eng. 2007;54:1687–1695. doi: 10.1109/TBME.2007.891934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridlund AJ, Cacioppo JT. Guidelines for human electromyographic research. Psychophysiology. 1986;23:567–589. doi: 10.1111/j.1469-8986.1986.tb00676.x. [DOI] [PubMed] [Google Scholar]
- Gerbrands TA, Pisters MF, Theeven PJR, Verschueren S, Vanwanseele B. Lateral trunk lean and medializing the knee as gait strategies for knee osteoarthritis. Gait Posture. 2017;51:247–253. doi: 10.1016/j.gaitpost.2016.11.014. [DOI] [PubMed] [Google Scholar]
- Gerbrands TA, Pisters MF, Vanwanseele B. Individual selection of gait retraining strategies is essential to optimally reduce medial knee load during gait. Clin Biomech. 2014;29:828–834. doi: 10.1016/j.clinbiomech.2014.05.005. [DOI] [PubMed] [Google Scholar]
- Gribble PL, Mullin LI, Cothros N, Mattar A. Role of cocontraction in arm movement accuracy. J Neurophysiol. 2003;89:2396–2405. doi: 10.1152/jn.01020.2002. [DOI] [PubMed] [Google Scholar]
- Guo M, Axe MJ, Manal K. The influence of foot progression angle on the knee adduction moment during walking and stair climbing in pain free individuals with knee osteoarthritis. Gait Posture. 2007;26:436–441. doi: 10.1016/j.gaitpost.2006.10.008. [DOI] [PubMed] [Google Scholar]
- Hernborg JS, Nilsson BE. The natural course of untreated osteoarthritis of the knee. Clin Orthop Relat Res. 1977;123:130–137. [PubMed] [Google Scholar]
- Hinman RS, Bowles KA, Metcalf BB, Wrigley TV, Bennell KL. Lateral wedge insoles for medial knee osteoarthritis: Effects on lower limb frontal plane biomechanics. Clin Biomech. 2012;27:27–33. doi: 10.1016/j.clinbiomech.2011.07.010. [DOI] [PubMed] [Google Scholar]
- Hodges PW, van den Hoorn W, Wrigley TV, Hinman RS, Bowles K, Cicuttini F, Wang Y, Bennell K. Increased duration of co-contraction of medial knee muscles is associated with greater progression of knee osteoarthritis. Man Ther. 2016;21:151–158. doi: 10.1016/j.math.2015.07.004. [DOI] [PubMed] [Google Scholar]
- Hunt MA, Takacs J. Effects of a 10-week toe-out gait modification intervention in people with medial knee osteoarthritis: a pilot, feasibility study. Osteoarthr Cartil. 2014;22:904–911. doi: 10.1016/j.joca.2014.04.007. [DOI] [PubMed] [Google Scholar]
- Hurwitz DE, Ryals AB, Case JP, Block JA, Andriacchi TP. The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. J Orthop Res. 2002;20:101–107. doi: 10.1016/S0736-0266(01)00081-X. [DOI] [PubMed] [Google Scholar]
- Jenkyn TR, Hunt MA, Jones IC, Giffin JR, Birmingham TB. Toe-out gait in patients with knee osteoarthritis partially transforms external knee adduction moment into flexion moment during early stance phase of gait: a tri-planar kinetic mechanism. J Biomech. 2008;41:276–283. doi: 10.1016/j.jbiomech.2007.09.015. [DOI] [PubMed] [Google Scholar]
- Kutzner I, Trepczynski A, Heller MO, Bergmann G. Knee adduction moment and medial contact force – facts about their correlation during gait. PLoS One. 2013;8:1–8. doi: 10.1371/journal.pone.0081036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CJ, Lai KA, Chou YL, Ho CS. The effect of changing the foot progression angle on the knee adduction moment in normal teenagers. Gait Posture. 2001;14:85–91. doi: 10.1016/s0966-6362(01)00126-6. [DOI] [PubMed] [Google Scholar]
- Manal K, Gardinier E, Buchanan TS, Snyder-Mackler L. A more informed evaluation of medial compartment loading: the combined use of the knee adduction and flexor moments. Osteoarthr Cartil. 2015;23:1107–1111. doi: 10.1016/j.joca.2015.02.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mündermann A, Asay JL, Mündermann L, Andriacchi TP. Implications of increased medio-lateral trunk sway for ambulatory mechanics. J Biomech. 2008;41:165–170. doi: 10.1016/j.jbiomech.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Mündermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52:2835–2844. doi: 10.1002/art.21262. [DOI] [PubMed] [Google Scholar]
- Ogaya S, Naito H, Iwata A, Higuchi Y, Fuchioka S, Tanaka M. Toe-out gait decreases the second peak of the medial knee contact force. J Appl Biomech. 2015;31:275–280. doi: 10.1123/jab.2014-0310. [DOI] [PubMed] [Google Scholar]
- Perry J. Gait Analysis: Normal and Pathological Function. SLACK Incorporated; Thorofare, New Jersey: 1992. [Google Scholar]
- Quintana JM, Arostegui I, Escobar A, Azkarate J, Goenaga JI, Lafuente I. Prevalence of knee and hip osteoarthritis and the appropriateness of joint replacement in an older population. Arch Intern Med. 2008;168:1576–1584. doi: 10.1001/archinte.168.14.1576. [DOI] [PubMed] [Google Scholar]
- Richards R, van den Noort JC, Dekker J, Harlaar J. Gait retraining with real-rime biofeedback to reduce knee adduction moment: systematic review of effects and methods used. Arch Phys Med Rehabil. 2017;98:137–150. doi: 10.1016/j.apmr.2016.07.006. [DOI] [PubMed] [Google Scholar]
- Rutherford DJ, Hubley-Kozey CL, Deluzio KJ, Stanish WD, Dunbar M. Foot progression angle and the knee adduction moment: a cross-sectional investigation in knee osteoarthritis. Osteoarthr Cartil. 2008;16:883–889. doi: 10.1016/j.joca.2007.11.012. [DOI] [PubMed] [Google Scholar]
- Sharma L, Hurwitz DE, Thonar EJ, Sum JA, Lenz ME, Dunlop DD, Schnitzer TJ, Kirwan-Mellis G, Andriacchi TP. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis Rheum. 1998;41:1233–1240. doi: 10.1002/1529-0131(199807)41:7<1233::AID-ART14>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Shull PB, Huang Y, Schlotman T, Reinbolt JA. Muscle force modification strategies are not consistent for gait retraining to reduce the knee adduction moment in individuals with knee osteoarthritis. J Biomech. 2015;48:3163–3169. doi: 10.1016/j.jbiomech.2015.07.006. [DOI] [PubMed] [Google Scholar]
- Shull PB, Lurie KL, Cutkosky MR, Besier TF. Training multi-parameter gaits to reduce the knee adduction moment with data-driven models and haptic feedback. J Biomech. 2011;44:1605–1609. doi: 10.1016/j.jbiomech.2011.03.016. [DOI] [PubMed] [Google Scholar]
- Shull PB, Shultz R, Silder A, Dragoo JL, Besier TF, Cutkosky MR, Delp SL. Toe-in gait reduces the first peak knee adduction moment in patients with medial compartment knee osteoarthritis. J Biomech. 2013a;46:122–128. doi: 10.1016/j.jbiomech.2012.10.019. [DOI] [PubMed] [Google Scholar]
- Shull PB, Silder A, Shultz R, Dragoo JL, Besier TF, Delp SL, Cutkosky MR. Six-week gait retraining program reduces knee adduction moment, reduces pain, and improves function for individuals with medial compartment knee osteoarthritis. J Orthop Res. 2013b;31:1020–1025. doi: 10.1002/jor.22340. [DOI] [PubMed] [Google Scholar]
- Simic M, Wrigley TV, Hinman RS, Hunt MA, Bennell KL. Altering foot progression angle in people with medial knee osteoarthritis: the effects of varying toe-in and toe-out angles are mediated by pain and malalignment. Osteoarthr Cartil. 2013;21:1272–1280. doi: 10.1016/j.joca.2013.06.001. [DOI] [PubMed] [Google Scholar]
- Tsai LC, McLean S, Colletti PM, Powers CM. Greater muscle co-contraction results in increased tibiofemoral compressive forces in females who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012;30:2007–2014. doi: 10.1002/jor.22176. [DOI] [PubMed] [Google Scholar]
- Tsai LC, Scher IS, Powers CM. Quantification of tibiofemoral shear and compressive loads using an MRI-based EMG-driven knee model. J Appl Biomech. 2013;29:229–234. doi: 10.1123/jab.29.2.229. [DOI] [PubMed] [Google Scholar]
- van den Noort JC, Steenbrink F, Roeles S, Harlaar J. Real-time visual feedback for gait retraining: toward application in knee osteoarthritis. Med Biol Eng Comput. 2015;53:275–286. doi: 10.1007/s11517-014-1233-z. [DOI] [PubMed] [Google Scholar]
- Voloshina AS, Kuo AD, Daley MA, Ferris DP. Biomechanics and energetics of walking on uneven terrain. J Exp Biol. 2013;216:3963–3970. doi: 10.1242/jeb.081711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter JP, D’Lima DD, Colwell CW, Fregly BJ. Decreased knee adduction moment does not guarantee decreased medial contact force during gait. J Orthop Res. 2010;28:1348–1354. doi: 10.1002/jor.21142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winby CR, Lloyd DG, Besier TF, Kirk TB. Muscle and external load contribution to knee joint contact loads during normal gait. J Biomech. 2009;42:2294–2300. doi: 10.1016/j.jbiomech.2009.06.019. [DOI] [PubMed] [Google Scholar]


