Abstract
Oral health status is correlated with socioeconomic status. However, the causal nature of the relationship is not established. Here we describe a natural experiment involving deteriorating socioeconomic circumstances following exposure to the 2011 Great East Japan Earthquake and Tsunami. We investigated the relationship between subjective economic deterioration and housing damage due to the disaster and tooth loss in a cohort of community-dwelling residents (n = 3,039), from whom we obtained information about socioeconomic status and health status in 2010 (i.e., predating the disaster). A follow-up survey was performed in 2013 (postdisaster), and 82.1% of the 4,380 eligible survivors responded. We estimated the impact of subjective economic deterioration and housing damage due to the disaster on tooth loss by fitting an instrumental variable probit model. Subjective economic deterioration and housing damage due to the disaster were significantly associated with 8.1% and 1.7% increases in the probability of tooth loss (probit coefficients were 0.469 (95% confidence interval: 0.065, 0.872) and 0.103 (95% confidence interval: 0.011, 0.196), respectively). In this natural experiment, we confirmed the causal relationship between deteriorating socioeconomic circumstances and tooth loss.
Keywords: change in economic status, instrumental variable analyses, natural disaster, natural experiment, oral health, tooth loss
Oral diseases are highly prevalent, and they pose a substantial health burden throughout the world (1, 2). For example, dental caries was the most prevalent disease in the Global Burden of Disease Study 2010 (1). Furthermore, the burden of oral disease, as expressed using disability-adjusted life years, is increasing with the recent growth and aging of the global population (1). The high prevalence of oral diseases was estimated to impose direct treatment costs amounting to US$298 billion (4.6% of global health expenditures) in 2010 (3). Accordingly, understanding the determinants of oral health and preventing oral diseases remain high priorities (4, 5).
Oral health is considered an exquisite mirror of social conditions (4, 6, 7), and an increasing number of studies have found that oral health problems are associated with low socioeconomic status (SES) (8–13). However, there is insufficient evidence to infer a causal relationship between SES and oral health, given the absence of evidence from interventions. Indeed, some studies have suggested the possibility of reverse causation, whereby poor oral health results in lower socioeconomic mobility—for example, as a result of people with poor teeth experiencing difficulties in the labor market (success in job interviews) (14, 15). Randomized controlled trials would be useful for examining this relationship. However, randomizing SES is difficult, for reasons of both ethics and feasibility. Accordingly, an alternative is to find natural experiments that cause an exogenous change in socioeconomic circumstances.
Natural experiment studies can provide strong causal evidence, as the independent variable of interest (in our example, deterioration of socioeconomic circumstances) happens semirandomly and independently of the outcome (16). Therefore, this design can be useful for evaluating whether socioeconomic circumstances causally affect oral health. Researchers have investigated the causal relationship between socioeconomic circumstances and general health in several natural experiments (17, 18), although we are not aware of any natural experiment study that has investigated oral health.
In this context, Japan experienced the Great East Japan Earthquake and Tsunami on March 11, 2011. This natural disaster created a suitable setting for a natural experiment study, as many people experienced financial loss due to the disaster (e.g., job loss, housing loss, and other property damage). For example, 51% of the survivors in a severely affected area reported experiencing economic hardship afterwards (19). Therefore, in this natural experiment study, we aimed to investigate the associations between change in oral health and worsened socioeconomic circumstances, which were naturally assigned by the earthquake.
METHODS
Study population
The present study was performed as a part of an ongoing nationwide prospective cohort study, the Japan Gerontological Evaluation Study (JAGES). The JAGES cohort was originally established to evaluate the social determinants of healthy aging in a nationwide sample of community-dwelling seniors (20). In the present study, we used data from one of the field sites of the JAGES cohort: Iwanuma City, on the northeastern coast of Japan. The baseline survey was conducted in Iwanuma in August 2010 (i.e., 7 months before the disaster), using self-administered questionnaires that were mailed to all residents of the city aged ≥65 years. On March 11, 2011, Iwanuma was just 80 km west of the earthquake epicenter, and the disaster killed 186 persons and destroyed 5,428 houses (21). A second survey was subsequently conducted in October 2013 (31 months after the disaster), and the investigators visited the survivors’ homes to gather information about postdisaster economic circumstances and oral health.
Exposure: subjective economic deterioration and housing damage by the disaster
We used 2 exposure measures: 1) self-rated economic change after the disaster (a subjective indicator) and 2) severity of housing damage, which was determined by local government inspectors (an objective indicator used for the purposes of survivor compensation). All participants in the present study were aged ≥65 years; 82% were retired or not engaged in paid work and were supported by their pension. In this context, exposure to the disaster is likely to have worsened the economic circumstances of the survivors via property damage (e.g., loss of housing, cars) and the financial costs of rebuilding lives, as opposed to direct loss of earnings stemming from job loss. Self-rated economic change was evaluated by asking the participants, “Was your economic situation affected by the disaster?”, with possible responses ranging from: “became worse,” “became partially worse,” “no change,” “partially improved,” or “improved.” We combined “no change,” “partially improved,” and “improved” into a single category because the numbers of participants in these categories were low. Government-assessed housing damage was evaluated by asking the participants, “What was the official classification of the damage to your house?”, which could be answered with the possible responses “destroyed,” “major,” “minor,” “partial,” or “no damage.” Damage level details are shown in Web Table 1 (available at http://aje.oxfordjournals.org/).
Outcome: tooth loss
Number of remaining teeth was obtained in categories: 0, 1–9, 10–19, or ≥20 teeth in the baseline survey and 0, 1–4, 5–9, 10–19, or ≥20 teeth in the follow-up survey. We combined the follow-up survey categories of 1–4 teeth and 5–9 teeth into a single category of 1–9 teeth and then compared the responses with those of the baseline survey. A response of a low number of teeth at follow-up compared with the number given at baseline was defined as tooth loss.
Covariates
The following baseline variables were considered as covariates: age (65–69, 70–74, 75–79, 80–84, or ≥85 years), sex (male or female), equivalized annual household income (tertiles: low, middle, and high), years of education (≤9, 10–12, or ≥13), and comorbidity (any of the following self-reported comorbid conditions: cancer, heart disease, stroke, hypertension, diabetes mellitus, hyperlipidemia, osteoporosis, mental illness, or sleep disorder). We also considered the following variables in the follow-up survey: loss of loved ones because of the disaster (lost or not lost) and psychological distress at follow-up, measured using the Kessler Psychological Distress Scale, truncated version (K6 scale) (none: <5; moderate: 5–12; severe: ≥13) (22).
Analyses
To overcome residual confounding due to unmeasured confounders, we conducted instrumental variable (IV) analyses. The goal of IV estimation is to mimic a randomized trial by finding variable(s) in the data set which exogenously affect the exposure (i.e., subjective economic deterioration and housing damage) without directly affecting the outcome (tooth loss).
A valid IV must satisfy 3 conditions: It must be 1) independent of all confounders, 2) associated with the exposure of interest, and 3) independent of outcomes given the exposure of interest and all confounders (23). In our study, we used distance from the coastline as our instrument. Distance of each participant's residence from the coast was a powerful predictor of tsunami damage (and hence, property destruction and loss of wealth)—yet it ought not to have been directly correlated with tooth loss. We calculated the inverse of the distance from the coastline to each resident's address at baseline using geographic information systems and used this as an IV for subjective economic deterioration and housing damage. The covariate balance was evaluated using balancing plots (24). The IV probit analysis was carried out in 2 stages. In the first stage, “disaster damage” is instrumented by the distance variable. In the second stage, the instrumented values for disaster damage are then plugged into the equation predicting the outcome (tooth loss). Our causal parameter of interest is therefore β1:
| (1) |
| (2) |
We fitted this model by employing the conditional maximum likelihood, which simultaneously estimates equations 1 and 2 with equation 1 as the probit function form. Conditional maximum likelihood has an advantage compared with 2-stage least-squares estimation because conditional maximum likelihood can estimate average partial effects without retransformation (25, 26). The strength of the correlation between distance from the coastline (inverse distance) and damage from the disaster (disaster damage)—that is, subjective economic deterioration or housing damage—was evaluated by means of the F statistic, testing for the significance of π1 in equation 2. It is suggested that the F statistic should exceed 10. There was a significant correlation between subjective economic deterioration and housing damage (Spearman's ρ = 0.36, P < 0.001). Therefore, we constructed models with either subjective economic deterioration or housing damage. As sensitivity analyses, we conducted IV analyses with 2-stage least squares and conducted multivariable probit regression analyses in which subjective economic deterioration and housing damage were treated as categorical variables.
Complete-case analyses and analyses with multiple imputation were conducted. In the multiple imputation procedure, we created 20 multiply imputed data sets by imputing missing information on explanatory variables, assuming that data were missing at random and using the multivariate normal imputation method. These estimated parameters were then combined using Rubin's combination methods (27, 28). The prevalence of missing information for each variable is shown in Web Table 2. All analyses were performed using Stata software (version 13.1; StataCorp LP, College Station, Texas), with the specific programs “ivprobit” (29) and “margins” for postestimation (30) at a significance level of 0.05.
Ethical considerations
Ethical approval for this study was obtained from the Human Subjects Committee of the Harvard T. H. Chan School of Public Health, the Ethics Committee of the Tohoku University Graduate School of Medicine, the Research Ethics Committee of the Graduate School of Medicine of Chiba University, and the Research Ethics Committee involving Human Participants of Nihon Fukushi University. Informed consent was obtained from the participants via mail for the baseline survey and was obtained in person for the follow-up survey.
RESULTS
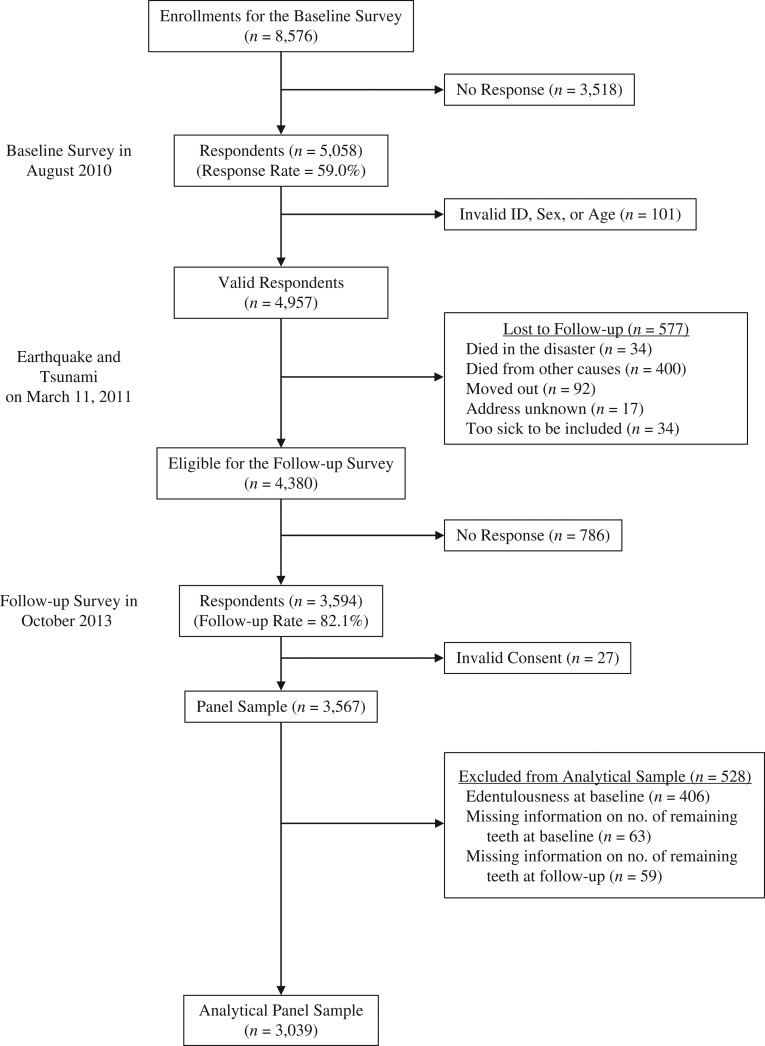
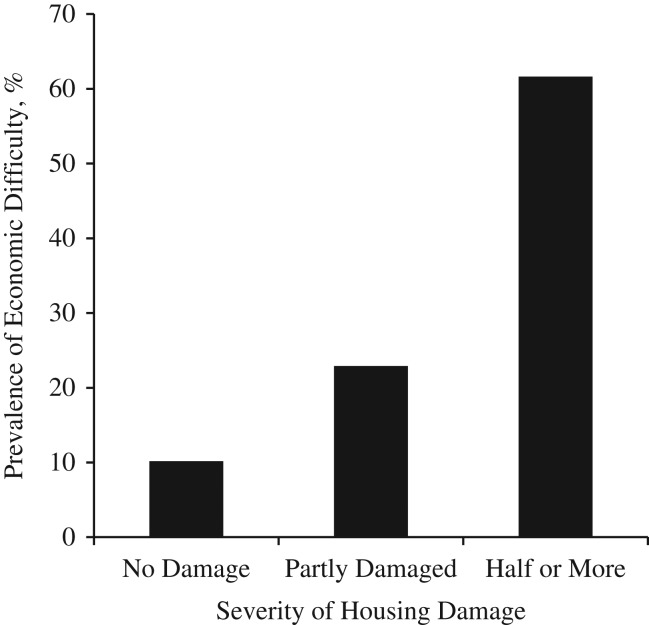
Figure 1 shows the flow of participants in the present study. The baseline survey in 2010 was completed by 5,058 participants (response rate = 59.0%). Among the 4,380 eligible survivors, 82.1% completed the follow-up survey, although we excluded cases with invalid informed consent responses, which provided us with 3,567 records. We included 3,039 participants in the analyses after excluding participants who had no teeth at baseline or were missing information on their number of teeth either at baseline or in the follow-up survey. Respondents with more severe housing damage exhibited a significantly higher prevalence of subjective economic difficulty (Figure 2; P < 0.001). The analytical sample comprised 3,039 individuals (mean age at baseline = 72.9 years; 45.1% were men).
Figure 1.
Selection of participants for a study of lowered socioeconomic circumstances and tooth loss after the 2011 Great East Japan Earthquake and Tsunami, Iwanuma, Japan, 2010–2013. ID, identification.
Figure 2.
Correlation between economic difficulty and severity of housing damage after the 2011 Great East Japan Earthquake and Tsunami (n = 3,428), Iwanuma, Japan, 2010–2013. The government-assessed level of housing damage was evaluated by asking the participants, “What was the official classification of the damage to your house?”. Possible responses were “destroyed,” “major,” “minor,” “partial,” or “no damage.” Participants with missing information on either subjective deterioration of economic circumstances or housing damage were excluded. χ2 test: P < 0.001.
Table 1 shows the participants’ characteristics and their associations with tooth loss. The incidence rate for tooth loss was 8.2%. Survivors with subjective economic difficulty or housing damage due to the disaster exhibited higher incidences of tooth loss.
Table 1.
Demographic Characteristics of Participants and Their Association With Tooth Loss After the 2011 Great East Japan Earthquake and Tsunami (n = 2,332), Iwanuma, Japan, 2010–2013
| Characteristic | Tooth Loss | Total No. of Persons | |||
|---|---|---|---|---|---|
| No | Yes | ||||
| No. | % | No. | % | ||
| Subjective deterioration of economic circumstances | |||||
| No change/improved | 1,672 | 92.6 | 133 | 7.4 | 1,805 |
| Became partially worse | 342 | 89.5 | 40 | 10.5 | 382 |
| Became worse | 127 | 87.6 | 18 | 12.4 | 145 |
| Housing damage | |||||
| No damage | 897 | 92.1 | 77 | 7.9 | 974 |
| Partial | 946 | 92.4 | 78 | 7.6 | 1,024 |
| Minor | 151 | 91.0 | 15 | 9.0 | 166 |
| Major | 76 | 90.5 | 8 | 9.5 | 84 |
| Destroyed | 71 | 84.5 | 13 | 15.5 | 84 |
| Sex | |||||
| Male | 1,032 | 90.7 | 106 | 9.3 | 1,138 |
| Female | 1,109 | 92.9 | 85 | 7.1 | 1,194 |
| Age group, years | |||||
| 65–69 | 846 | 93.7 | 57 | 6.3 | 903 |
| 70–74 | 620 | 90.9 | 62 | 9.1 | 682 |
| 75–79 | 408 | 91.9 | 36 | 8.1 | 444 |
| 80–84 | 194 | 90.7 | 20 | 9.3 | 214 |
| ≥85 | 73 | 82.0 | 16 | 18.0 | 89 |
| Tertile of predisaster income | |||||
| Low | 718 | 89.8 | 82 | 10.3 | 800 |
| Middle | 716 | 92.7 | 56 | 7.3 | 772 |
| High | 707 | 93.0 | 53 | 7.0 | 760 |
| Years of education | |||||
| ≤9 | 634 | 90.2 | 69 | 9.8 | 703 |
| 10–12 | 1,008 | 92.8 | 78 | 7.2 | 1,086 |
| ≥13 | 499 | 91.9 | 44 | 8.1 | 543 |
| Comorbid conditions before disaster | |||||
| No | 743 | 91.6 | 68 | 8.4 | 811 |
| Yes | 1,398 | 91.9 | 123 | 8.1 | 1,521 |
| Loss of loved ones in disaster | |||||
| Lost | 824 | 92.0 | 72 | 8.0 | 896 |
| Not lost | 1,317 | 91.7 | 119 | 8.3 | 1,436 |
| Psychological distress after disaster | |||||
| None | 1,323 | 93.0 | 100 | 7.0 | 1,423 |
| Moderate | 732 | 90.3 | 79 | 9.7 | 811 |
| Severe | 86 | 87.8 | 12 | 12.2 | 98 |
| Total | 2,141 | 91.8 | 191 | 8.2 | 2,332 |
Web Table 3 and Web Figure 1 show the covariate distribution and covariate balance plot (24) according to instrument and actual disaster damage. The covariate balance was improved in IV analyses.
Tables 2 and 3 show the association between tooth loss and subjective economic deterioration or housing damage obtained from IV probit analyses after applying multiple imputations. A significant association between subjective economic deterioration and tooth loss was observed. The average partial effect was 0.081, which translates to an 8.1% increase in the probability of tooth loss per increment in subjective economic deterioration (Table 2). The F statistic was 144.33, suggesting a sufficient correlation between the IV and the exposure variable (Table 2). A significant association was observed between housing damage due to the disaster and tooth loss. The average partial effect was 0.017, which translates to a 1.7% increase in the probability of tooth loss per increment in housing damage (Table 3). The F statistic was 1,622.93, suggesting a sufficient correlation between the IV and the exposure variable (Table 3). Loss of a loved one was not significantly associated with tooth loss (Tables 2 and 3).
Table 2.
Association Between Subjective Deterioration of Economic Circumstances and Tooth Loss Following the 2011 Earthquake in an Instrumental Variable Analysis With Conditional Maximum Likelihood, After Application of Multiple Imputation (n = 3,039), Iwanuma, Japan, 2010–2013
| Variable | Multivariable Probit Regression (Without IV) | Conditional Maximum Likelihood | Average Partial Effect | |||||
|---|---|---|---|---|---|---|---|---|
| First Stage | Second Stage | |||||||
| B | 95% CI | B | 95% CI | B | 95% CI | Probability | 95% CI | |
| Subjective economic deterioration (ranging from “no change/improved” (1) to “became worse” (3)) | 0.082 | −0.027, 0.191 | 0.469 | 0.065, 0.872 | 0.081 | 0.005, 0.157 | ||
| Distance from coastline, km−1a | 0.314 | 0.263, 0.365 | ||||||
| Sex | ||||||||
| Male | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| Female | −0.114 | −0.242, 0.013 | −0.051 | −0.090, −0.012 | −0.092 | −0.221, 0.036 | −0.016 | −0.038, 0.006 |
| Age group, years | ||||||||
| 65–69 | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| 70–74 | 0.162 | −0.001, 0.325 | −0.044 | −0.092, 0.004 | 0.175 | 0.015, 0.336 | 0.030 | 0.002, 0.058 |
| 75–79 | 0.192 | 0.012, 0.372 | −0.101 | −0.156, −0.047 | 0.231 | 0.050, 0.411 | 0.040 | 0.008, 0.072 |
| 80–84 | 0.248 | 0.029, 0.467 | −0.122 | −0.192, −0.053 | 0.295 | 0.075, 0.514 | 0.051 | 0.012, 0.090 |
| ≥85 | 0.560 | 0.279, 0.842 | −0.135 | −0.235, −0.034 | 0.601 | 0.322, 0.880 | 0.104 | 0.054, 0.154 |
| Tertile of predisaster income | ||||||||
| Low | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| Middle | −0.182 | −0.356, −0.008 | −0.159 | −0.210, −0.108 | −0.110 | −0.299, 0.079 | −0.019 | −0.051, 0.013 |
| High | −0.161 | −0.334, 0.012 | −0.180 | −0.233, −0.127 | −0.081 | −0.271, 0.108 | −0.014 | −0.046, 0.018 |
| Years of education | ||||||||
| ≤9 | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| 10–12 | −0.110 | −0.260, 0.039 | −0.083 | −0.131, −0.036 | −0.059 | −0.217, 0.100 | −0.010 | −0.037, 0.017 |
| ≥13 | −0.054 | −0.237, 0.129 | −0.119 | −0.176, −0.062 | 0.011 | −0.182, 0.204 | 0.002 | −0.032, 0.035 |
| Comorbid conditions before disaster | ||||||||
| No | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| Yes | −0.096 | −0.232, 0.039 | 0.021 | −0.021, 0.063 | −0.105 | −0.238, 0.029 | −0.018 | −0.041, 0.005 |
| Loss of loved ones in disaster | ||||||||
| Not lost | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| Lost | −0.063 | −0.196, 0.071 | 0.133 | 0.092, 0.174 | −0.130 | −0.278, 0.018 | −0.023 | −0.049, 0.004 |
| Psychological distress after disaster | ||||||||
| None | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| Moderate | 0.174 | 0.038, 0.310 | 0.188 | 0.147, 0.230 | 0.090 | −0.070, 0.251 | 0.016 | −0.011, 0.043 |
| Severe | 0.165 | −0.136, 0.466 | 0.394 | 0.295, 0.493 | −0.006 | −0.352, 0.340 | −0.001 | −0.061, 0.059 |
Abbreviations: CI, confidence interval; IV, instrumental variable.
aF statistic in first stage of IV analysis = 144.33.
Table 3.
Association Between Housing Damage and Tooth Loss Following the 2011 Earthquake in an Instrumental Variable Analysis With Conditional Maximum Likelihood, After Application of Multiple Imputation (n = 3,039), Iwanuma, Japan, 2010–2013
| Variable | Multivariable Probit Regression (Without IV) | Conditional Maximum Likelihood | Average Partial Effect | |||||
|---|---|---|---|---|---|---|---|---|
| First Stage | Second Stage | |||||||
| B | 95% CI | B | 95% CI | B | 95% CI | Probability | 95% CI | |
| Housing damage (ranging from “no damage” (1) to “destroyed” (5)) | 0.060 | −0.003, 0.123 | 0.103 | 0.011, 0.196 | 0.017 | 0.002, 0.033 | ||
| Distance from coastline, km−1a | 1.463 | 1.392, 1.534 | ||||||
| Sex | ||||||||
| Male | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| Female | −0.119 | −0.247, 0.009 | −0.003 | −0.058, 0.053 | −0.119 | −0.247, 0.008 | −0.020 | −0.041, 0.001 |
| Age group, years | ||||||||
| 65–69 | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| 70–74 | 0.164 | 0.001, 0.326 | −0.083 | −0.152, −0.014 | 0.167 | 0.004, 0.329 | 0.028 | 0.001, 0.055 |
| 75–79 | 0.187 | 0.007, 0.366 | −0.025 | −0.101, 0.052 | 0.190 | 0.010, 0.369 | 0.031 | 0.002, 0.061 |
| 80–84 | 0.243 | 0.024, 0.462 | −0.078 | −0.175, 0.020 | 0.250 | 0.031, 0.469 | 0.041 | 0.005, 0.078 |
| ≥85 | 0.557 | 0.276, 0.838 | −0.138 | −0.279, 0.004 | 0.564 | 0.283, 0.845 | 0.094 | 0.047, 0.140 |
| Tertile of predisaster income | ||||||||
| Low | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| Middle | −0.191 | −0.364, −0.018 | −0.030 | −0.100, 0.039 | −0.186 | −0.359, −0.013 | −0.031 | −0.060, −0.002 |
| High | −0.174 | −0.346, −0.003 | 0.022 | −0.048, 0.093 | −0.172 | −0.344, −0.001 | −0.029 | −0.057, −0.000 |
| Years of education | ||||||||
| ≤9 | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| 10–12 | −0.105 | −0.255, 0.046 | −0.071 | −0.138, −0.005 | −0.092 | −0.244, 0.060 | −0.015 | −0.040, 0.010 |
| ≥13 | −0.054 | −0.236, 0.129 | −0.043 | −0.124, 0.037 | −0.042 | −0.226, 0.142 | −0.007 | −0.037, 0.024 |
| Comorbid conditions before disaster | ||||||||
| No | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| Yes | −0.096 | −0.232, 0.039 | 0.025 | −0.034, 0.085 | −0.099 | −0.235, 0.036 | −0.016 | −0.039, 0.006 |
| Loss of loved ones in disaster | ||||||||
| Not lost | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| Lost | −0.072 | −0.207, 0.063 | 0.197 | 0.140, 0.255 | −0.089 | −0.227, 0.048 | −0.015 | −0.038, 0.008 |
| Psychological distress after disaster | ||||||||
| None | 0 | Referent | 0 | Referent | 0 | Referent | 0 | Referent |
| Moderate | 0.180 | 0.046, 0.314 | 0.153 | 0.094, 0.212 | 0.169 | 0.033, 0.304 | 0.028 | 0.006, 0.050 |
| Severe | 0.181 | −0.118, 0.480 | 0.205 | 0.066, 0.343 | 0.163 | −0.138, 0.464 | 0.027 | −0.023, 0.077 |
Abbreviations: CI, confidence interval; IV, instrumental variable.
aF statistic in first stage of IV analysis = 1,622.93.
The sensitivity analyses produced similar results. Results from IV analyses with 2-stage least squares estimation are shown in Web Tables 4 and 5; results from multivariable probit regressions (without IV) treating disaster damage as a categorical variable (not statistically significant) are shown in Web Tables 6 and 7; and results from complete-case analyses are shown in Web Tables 8–13.
DISCUSSION
The present natural experiment provides evidence that worsened economic circumstances (measured by subjective economic deterioration or housing damage) are associated with tooth loss. IV analyses showed a significant association between worsened economic circumstances and tooth loss; however, multivariable analyses (without IV) did not. This suggests the existence of unmeasured confounding in the multivariable model. We were able to overcome this problem through the use of IV analyses taking advantage of an exogenous natural disaster situation. Our findings strengthen the causal interpretation of the effect of deteriorating socioeconomic circumstances on oral health. We also found that housing damage (an objective indicator of loss of wealth) was significantly associated with tooth loss.
The association between low SES and poor oral health has been amply documented in both cross-sectional and longitudinal studies (8, 31, 32). A meta-analysis of 2 cross-sectional studies and 10 cohort studies found a significant association between low income and tooth loss (12). However, those studies were observational, and hence it is difficult to infer causality. In contrast, the present natural experiment provided causal evidence regarding the relationship between deterioration of socioeconomic circumstances due to disaster damage and tooth loss.
The conceptual mediators of the effect of SES on oral health include material deprivation, psychosocial distress, and behavioral and biological factors, as well as health-care systems (33). In addition, there are some plausible biological pathways connecting SES and tooth loss. For example, experiencing economic difficulty is associated with increased psychological distress (34), and psychological distress can affect immune function (35), thereby raising the risk of periodontal disease (36), which is one of the biggest causes of tooth loss among older people (37). In the context of the present study, survivors of the 2011 Great East Japan Earthquake and Tsunami were likely to have encountered economic challenges, limited day-to-day resources, and stressors. Moreover, low SES status is a barrier to health-care access (38). Reduced access to dental care among survivors with worsened economic conditions might have contributed to tooth loss. This suggests that policies which ensure access to health care are needed for disaster survivors. After the 2011 earthquake and tsunami, the Japanese government provided free health care to survivors who were severely affected by the disaster; 1.4% of the present study's participants reported that they could not visit a dental clinic because of disaster damage (results are not shown). Oral health would have been even worse among the survivors if this policy had not been implemented.
Surprisingly, loss of loved ones in the disaster was not significantly associated with tooth loss. This result is consistent with previous studies performed after the earthquake which showed that loss of loved ones in the disaster was not associated with dementia onset or depressive symptoms (39, 40). There are 2 possible reasons for this result: 1) the difference between the 2 types of disaster damage—deterioration of economic circumstances and loss of a loved one—might suggest that survivors could get over psychological loss but economic difficulty might burden survivors long-term; and 2) lack of information on the frequency of social interaction between the respondent and the relatives/friends who were lost at baseline. If we had been able to consider the frequency of social interaction at baseline, loss of relatives/friends might have been associated with tooth loss.
Our study included several strengths, such as the availability of pre- and postdisaster data among survivors, as well as our ability to leverage the “natural experiment” of wealth and income loss stemming from the experience of disaster. We applied IV analyses to overcome the problem of unmeasured confounding. On the other hand, our study also had several limitations that warrant consideration. First, the data regarding economic status and oral health were self-reported, although a previous study found that self-reporting of number of teeth was validated by clinical dental examinations (41). Second, we did not measure dental caries and periodontal disease at baseline, which are risk factors for tooth loss at follow-up; however, our IV analysis enabled us to control for these unmeasured confounders. Third, the follow-up period might have been too short to detect tooth loss. However, in a US study, Gilbert et al. (42) performed clinical examinations of adults aged ≥45 years, and 24% of them lost 1 or more teeth within 2 years, which would indicate that the 3-year follow-up period in the present study was sufficient to detect tooth loss. Fourth, we did not simultaneously include subjective economic deterioration and housing damage because of collinearity between these two variables; it is also difficult to isolate the effects of 2 variables using only 1 instrument. Due to the model's design, the models with each exposure ignore the other exposure's effect on tooth loss. Fifth, this study only considered the effects of a single natural disaster. The external validity of these findings is limited.
In conclusion, our results indicate that deteriorating economic circumstances were associated with poor oral health among survivors of the 2011 Japanese earthquake. The present findings from this natural experiment study strengthen causal inference about the effect of SES on oral health.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of International and Community Oral Health, Graduate School of Dentistry, Tohoku University, Sendai, Japan (Yusuke Matsuyama, Jun Aida, Toru Tsuboya, Ken Osaka); Department of Social and Behavioral Sciences, Harvard T.H. Chan School of Public Health, Boston, Massachusetts (Hiroyuki Hikichi, Ichiro Kawachi); Center for Preventive Medical Sciences, Chiba University, Chiba, Japan (Katsunori Kondo); and Center for Gerontology and Social Science, National Center for Geriatrics and Gerontology, Obu, Japan (Katsunori Kondo).
This study used data from the Japan Gerontological Evaluation Study (JAGES), which is conducted by the Center for Well-being and Society, Nihon Fukushi University. This study was supported by a grant from the National Institute on Aging, US National Institutes of Health (grant 1R01AG042463-01A1); several Health and Labour Sciences Research Grants (Comprehensive Research on Aging and Health) from the Japanese Ministry of Health, Labour and Welfare (grants H22-Choju-Shitei-008, H24-Choju-Wakate-009, H25-Choju-Ippan-003, and H28-Choju-Ippan-002); Grants-in-Aid for Scientific Research from the Japanese Society for the Promotion of Science (grants KAKENHI 23243070, 22390400, 24390469, and 15H01972); a grant from the Strategic Research Foundation Grant-Aided Project for Private Universities from the Japanese Ministry of Education, Culture, Sports, Science and Technology (grant S0991035); and Research and Development Grants for Longevity Science from the Japan Agency for Medical Research and Development.
We appreciate the support and cooperation of the Iwanuma mayor's office and the staff of the Department of Health and Welfare of the Iwanuma city government.
The funders played no role in the study design, data collection and analysis, or the decision to publish this report.
Conflict of interest: none declared.
REFERENCES
- 1. Marcenes W, Kassebaum NJ, Bernabé E, et al. Global burden of oral conditions in 1990–2010: a systematic analysis. J Dent Res. 2013;92(7):592–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kassebaum NJ, Bernabé E, Dahiya M, et al. Global burden of severe tooth loss: a systematic review and meta-analysis. J Dent Res. 2014;93(7 suppl):20S–28S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Listl S, Galloway J, Mossey PA, et al. Global economic impact of dental diseases. J Dent Res. 2015;94(10):1355–1361. [DOI] [PubMed] [Google Scholar]
- 4. Marshman Z, Robinson PG. Dental public health In: Detels R, Beaglehole R, Lansang MA, et al., eds. Oxford Textbook of Public Health. Oxford, United Kingdom: Oxford Medical Publications; 2011:1101–1116. [Google Scholar]
- 5. Daly B, Batchelor P, Treasure E, et al. Essential Dental Public Health. Oxford, United Kingdom: Oxford University Press; 2013. [Google Scholar]
- 6. Watt RG, Sheiham A. Integrating the common risk factor approach into a social determinants framework. Community Dent Oral Epidemiol. 2012;40(4):289–296. [DOI] [PubMed] [Google Scholar]
- 7. Petersen P, Yamamoto T. Improving the oral health of older people: the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2005;33(2):81–92. [DOI] [PubMed] [Google Scholar]
- 8. Matsuyama Y, Aida J, Takeuchi K, et al. Inequalities of dental prosthesis use under universal healthcare insurance. Community Dent Oral Epidemiol. 2014;42(2):122–128. [DOI] [PubMed] [Google Scholar]
- 9. Sabbah W, Tsakos G, Chandola T, et al. Social gradients in oral and general health. J Dent Res. 2007;86(10):992–996. [DOI] [PubMed] [Google Scholar]
- 10. Costa SM, Martins CC, de Bonfim ML, et al. A systematic review of socioeconomic indicators and dental caries in adults. Int J Environ Res Public Health. 2012;9(10):3540–3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kim DW, Park JC, Rim TT, et al. Socioeconomic disparities of periodontitis in Koreans based on the KNHANES IV. Oral Dis. 2014;20(6):551–559. [DOI] [PubMed] [Google Scholar]
- 12. Seerig LM, Nascimento GG, Peres MA, et al. Tooth loss in adults and income: systematic review and meta-analysis. J Dent. 2015;43(9):1051–1059. [DOI] [PubMed] [Google Scholar]
- 13. Japan Dental Association The Current Evidence of Dental Care and Oral Health for Achieving Healthy Longevity in an Aging Society 2015 Tokyo, Japan: Japan Dental Association; 2015. https://www.jda.or.jp/en/. Accessed February 15, 2017. [Google Scholar]
- 14. Pithon MM, Nascimento CC, Barbosa GC, et al. Do dental esthetics have any influence on finding a job. Am J Orthod Dentofacial Orthop. 2014;146(4):423–429. [DOI] [PubMed] [Google Scholar]
- 15. Glied S, Neidell M. The economic value of teeth. J Hum Resour. 2010;45(2):468–496. [Google Scholar]
- 16. Remler DK, Van Ryzin GG. Research Methods in Practice: Strategies for Description and Causation. Thousand Oaks, CA: Sage Publications; 2014. [Google Scholar]
- 17. Hanandita W, Tampubolon G. Does poverty reduce mental health? An instrumental variable analysis. Soc Sci Med. 2014;113:59–67. [DOI] [PubMed] [Google Scholar]
- 18. Huang W, Zhou Y. Effects of education on cognition at older ages: evidence from China's Great Famine. Soc Sci Med. 2013;98:54–62. [DOI] [PubMed] [Google Scholar]
- 19. Yokoyama Y, Otsuka K, Kawakami N, et al. Mental health and related factors after the Great East Japan Earthquake and Tsunami. PLoS One. 2014;9(7):e102497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kondo K. Progress in aging epidemiology in Japan: the JAGES project. J Epidemiol. 2016;26(7):331–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Miyagi Prefectural Government Report of Damage by the Great East Japan Earthquake [in Japanese]. Sendai, Japan: Miyagi Prefectural Government; 2015. http://www.pref.miyagi.jp/uploaded/attachment/29,6031.pdf. Accessed March 30, 2015. [Google Scholar]
- 22. Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–976. [DOI] [PubMed] [Google Scholar]
- 23. Greenland S. An introduction to instrumental variables for epidemiologists. Int J Epidemiol. 2000;29(4):722–729. [DOI] [PubMed] [Google Scholar]
- 24. Jackson JW, Swanson SA. Toward a clearer portrayal of confounding bias in instrumental variable applications. Epidemiology. 2015;26(4):498–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. 2nd ed Cambridge, MA: The MIT Press; 2010. [Google Scholar]
- 26. Wehby G, Jugessur A, Murray JC, et al. Genes as instruments for studying risk behavior effects: an application to maternal smoking and orofacial clefts. Health Serv Outcomes Res Methodol. 2011;11(1-2):54–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Carpenter J, Kenward M. Multiple Imputation and Its Application. 1st ed Hoboken, NJ: John Wiley & Sons, Inc.; 2012. [Google Scholar]
- 28. Rubin DB. Multiple Imputation for Nonresponse in Surveys. Hoboken, NJ: John Wiley & Sons, Inc.; 1987. [Google Scholar]
- 29. StataCorp LP ivprobit—probit model with continuous endogenous regressors. http://www.stata.com/manuals13/rivprobit.pdf. Accessed February 16, 2017.
- 30. StataCorp LP ivprobit postestimation—postestimation tools for ivprobit. http://www.stata.com/manuals13/rivprobitpostestimation.pdf. Accessed February 16, 2017.
- 31. Ueno M, Ohara S, Inoue M, et al. Association between education level and dentition status in Japanese adults: Japan public health center-based oral health study. Community Dent Oral Epidemiol. 2012;40(6):481–487. [DOI] [PubMed] [Google Scholar]
- 32. Morita I, Nakagaki H, Yoshii S, et al. Is there a gradient by job classification in dental status in Japanese men. Eur J Oral Sci. 2007;115(4):275–279. [DOI] [PubMed] [Google Scholar]
- 33. Solar O, Irwin A. A Conceptual Framework for Action on the Social Determinants of Health (Social Determinants of Health Discussion Paper 2). Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 34. Korda RJ, Paige E, Yiengprugsawan V, et al. Income-related inequalities in chronic conditions, physical functioning and psychological distress among older people in Australia: cross-sectional findings from the 45 and Up Study. BMC Public Health. 2014;14(1):741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Segerstrom SC, Segerstrom SC, Miller GE, et al. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130(4):601–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Peruzzo DC, Benatti BB, Ambrosano GM, et al. A systematic review of stress and psychological factors as possible risk factors for periodontal disease. J Periodontol. 2007;78(8):1491–1504. [DOI] [PubMed] [Google Scholar]
- 37. Aida J, Ando Y, Akhter R, et al. Reasons for permanent tooth extractions in Japan. J Epidemiol. 2006;16(5):214–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Babazono A, Kuwabara K, Hagihara A, et al. Does income influence demand for medical services despite Japan's “health care for all” policy. Int J Technol Assess Health Care. 2008;24(1):125–130. [DOI] [PubMed] [Google Scholar]
- 39. Hikichi H, Aida J, Kondo K, et al. Increased risk of dementia in the aftermath of the 2011 Great East Japan Earthquake and Tsunami. Proc Natl Acad Sci USA. 2016;113(45):E6911–E6918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tsuboya T, Aida J, Hikichi H, et al. Predictors of depressive symptoms following the Great East Japan Earthquake: a prospective study. Soc Sci Med. 2016;161:47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yamamoto T, Kondo K, Fuchida S, et al. Validity of self-reported oral health variables: Aichi Gerontological Evaluation Study (AGES) project [in Japanese]. Health Sci Health Care. 2012;12(1):4–12. [Google Scholar]
- 42. Gilbert GH, Miller MK, Duncan RP, et al. Tooth-specific and person-level predictors of 24-month tooth loss among older adults. Community Dent Oral Epidemiol. 1999;27(5):372–385. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.