Abstract
Background
registered Nurses (RNs) working in UK care homes receive most of their training in acute hospitals. At present the role of care home nursing is underdeveloped and it is seen as a low status career. We describe here research to define core competencies for RNs working in UK care homes.
Methods
a two-stage process was adopted. A systematic literature review and focus groups with stakeholders provided an initial list of competencies. The competency list was modified over three rounds of a Delphi process with a multi-disciplinary expert panel of 28 members.
Results
twenty-two competencies entered the consensus process, all competencies were amended and six split. Thirty-one competencies were scored in round two, eight were agreed as essential, one competency was split into two. Twenty-four competencies were submitted for scoring in round three. In total, 22 competencies were agreed as essential for RNs working in care homes. A further 10 competencies did not reach consensus.
Conclusion
the output of this study is an expert-consensus list of competencies for RNs working in care homes. This would be a firm basis on which to build a curriculum for this staff group.
Keywords: Care homes, Nursing, Competencies, Older people
Background
Due to the ageing population there is increased use of residential and nursing homes – collectively referred to as care homes – to support the growing proportion of older people with more complex care needs. In the UK, care homes provide 465,000 beds, compared with 132,000 in acute hospitals [1].
The Registered Nurses (RNs) who work in care homes have usually received most of their training in acute hospitals [2]. Acute hospital work however, requires different skills and competencies from work in long-term care. There has been a call by many in nursing education to raise students’ understanding of gerontological and care home nursing as specialties that represent demanding and rewarding careers [3].
The role of nursing in long-term care is underdeveloped and working with older people is viewed by students as a low status career choice with lack of opportunities for professional development [4]. The Care Quality Commission (CQC) stated concerns about the shortage of nurses within nursing homes, many having insufficient staff on duty to ensure residents receive safe and dignified care. They reported 8% vacancy rates for RNs and the highest turnover rate of any job role in social care settings at 32% [1]. There is a concern that RNs are employed to earn a home its nursing home status and are not enabled to make full use of their competencies. It is also apparent that many RNs working in care homes are overseas workers and, due to changes in regulations, there are worries over their language/communication skills, competence and supervision [2].
There is a likely relationship between high turnover rates and nurses’ perceptions of low competency in core skill areas for long-term care [5]. In one survey, 50% of RNs in care homes rated their knowledge as insufficient in areas such as psychiatric illness, dealing with threat and violence, dementia, computer skills and healthcare and social welfare law [6]. Other research has suggested that current competencies do not correspond with the tasks required in nursing homes [7].
Competency development is known to predict work satisfaction and lower turnover rates [8]. Developing competencies in this workforce will facilitate professional development, more clearly define a career pathway in care home nursing and increase the status of work in this area.
This study set out to develop a competency framework for RNs working in care homes using the Delphi method.
Methods
The Delphi process is a consensus method aiming to determine the extent of agreement about an issue [9]. It allows everyone in the process to give opinions without being affected by group dynamics of assertiveness, politics or status, as can happen in face-to-face meetings. This study used a modified Delphi method where an initial list of competencies was compiled from a systematic literature search and supplemented by the views of stakeholders ascertained from focus groups. This set of competencies then underwent three rounds of consensus with an expert panel.
Development of initial competencies
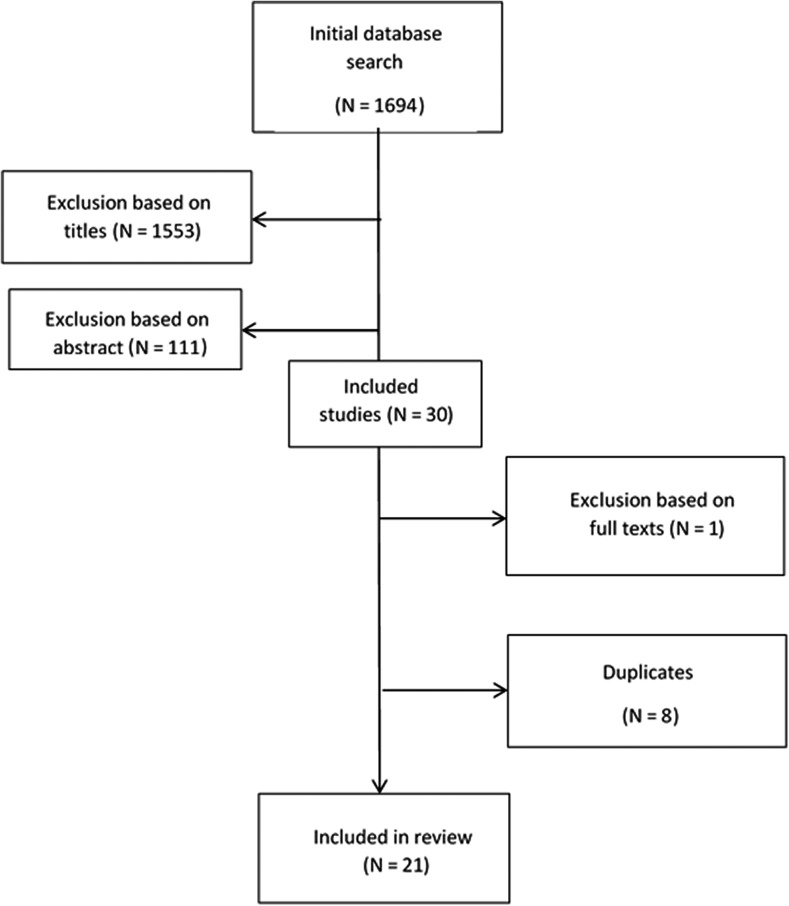
A systematic literature search was carried out in January 2016. This aimed to identify all relevant sources regardless of publication status. Search terms were ‘nursing’, ‘care home’ and ‘competencies’ and were mapped to relevant MeSH terms where relevant. The following databases were searched from inception to 15/10/2016: PsychInfo, Embase, Medline, Web of Science, Google Scholar, AgeInfo, OpenGrey; as well as the Royal College of Nursing and CQC websites. Screening of article titles was completed by the chief investigator (M.S.) and references not relevant to nursing home care, RNs, competencies and professional development of staff were excluded. The abstracts of remaining articles were screened for relevance and those not meeting the inclusion criteria were discarded. The remaining studies, after discarding duplicates, were read independently in full by two reviewers to identify all possible competencies for RNs working in care homes. Disagreement was resolved through discussion between the two reviewers (see Figure 1). Fifty-two competencies were identified from 21 studies [2, 10–28].
Figure 1.
Flowchart of systematic search and review process.
Quality assessment criteria were not used to rate methodological quality of articles as these are not routinely used in scoping reviews. Words or phrases extracted from the papers were categorised into topics, e.g. nutrition, dementia. Competency statements were written encompassing all individual phrases and words originally extracted from the articles. These were written and independently reviewed by two researchers (M.S. and S.G.) to ensure all data were included, resulting in a list of 51 competencies.
To supplement and provide expert content validation for the competency list, five focus groups were held. Focus groups included care workers (N = 3), RNs working in care homes (N = 3), care home managers (N = 2), family members of care home residents (N = 2) and healthcare professionals regularly liaising with care homes (N = 6). Focus groups lasted approximately one hour and were facilitated by two researchers. Discussion began by asking participants to describe the role of RNs working in care homes and the competencies required. After participants had stated their initial ideas, they were shown the list of competencies from the literature review and asked to comment on competencies they thought to be missing or particularly important. Participants were also asked how the role of care home RNs had changed in the last 5 years and how the role may change in future. Focus groups were audio-recorded and anonymised on transcription. Transcripts were analysed for competencies not already included in the competency list generated from the literature review. Nine competencies were added to the list following the focus groups.
The competency list was revised by the research team so that language and layout reflected that usually found in competency frameworks for nursing. Some competencies were combined into single statements and others divided so that competencies seen as more essential by participants were given greater emphasis. An audit trail referenced all competencies back to the literature and focus groups. The list taken into the Delphi process consisted of 22 competency statements.
The Delphi process
The expert panel was chosen on the basis of their experience of care home nursing. For experts from the medical and nursing professions, contributors to the British Geriatrics Society Fit for Frailty document [29], a consensus best practice document for the care of older people living with frailty in community and outpatient settings, were invited to participate. All contributors were experienced clinicians in the field of geriatrics. Out of the 20 invited, 14 agreed to participate. To represent the allied professions who work in care homes the Chartered Society of Physiotherapy Older People AGILE network was contacted and six volunteers responded. To include the care home staff perspective, the Enabling Research in Care Homes (EnRiCH) network for the East Midlands was contacted and nine responded. For a patient/resident perspective, the Patient and Public Leadership section of the East Midlands Academic Health Science Network were contacted, however no volunteers responded. In total, the panel numbered 29 in the first round. Nine had a medical background including one GP and one psychiatrist, 11 had a nursing background, five were physiotherapists and four were occupational therapists experienced in care home working.
The Delphi study was administered according to published guidelines [9, 30]. Each questionnaire was administered to panel members via email. Reminder emails were sent after 7 and 10 days. After 2 weeks, if no response was received, the panel member was removed from further rounds. The entire Delphi process took place via email. The panel members never met face-to-face and were not aware of the identity of other panel members.
The final competency list, agreed by the research team, was converted into a questionnaire allowing each panel member to rate a competency statement as ‘essential’ or ‘non-essential’ to care home nursing or ‘needs further development’. In the second and third round the option of ‘desirable’ was included in response to panel comments. For each competency statement the panel member could provide free-text comments or suggest alterations to the wording.
Free-text comments made by the panel were discussed by the research team to decide on their inclusion in future iterations of the questionnaire. Comments adding clarity and detail to competency statements were included where multiple panel members made similar comments. Where comments were contradictory they were rejected, however in the third round contradictory comments were summarised and sent to the expert panel for comment. In addition, at every round the panel was informed of the percentage of the panel who rated each competency as ‘essential’, ‘desirable’, ‘non-essential’ or ‘needs further development’. Where amendments to competencies were made, competency statements were re-scored by the panel in the following round, even if the original statement had achieved consensus. Consensus was defined as 80% of panel members agreeing on a rating of ‘essential’, ‘desirable’ or ‘non-essential’ [9]. There is no established threshold for consensus in the literature. The median threshold for Delphi studies in a recent review was 75% [9]. As this study initially included only three options in the Delphi questionnaire, ’essential’, ‘non-essential’ or ‘needs further development’, the consensus threshold was raised to minimise the likelihood of agreement by chance. Statements where 80% or more of the panel agreed were removed from future rounds.
Ethical approval for this study was granted by the UK Social Care Research Ethics Committee (Ref: 16/IEC08/0002).
Results
Round 1
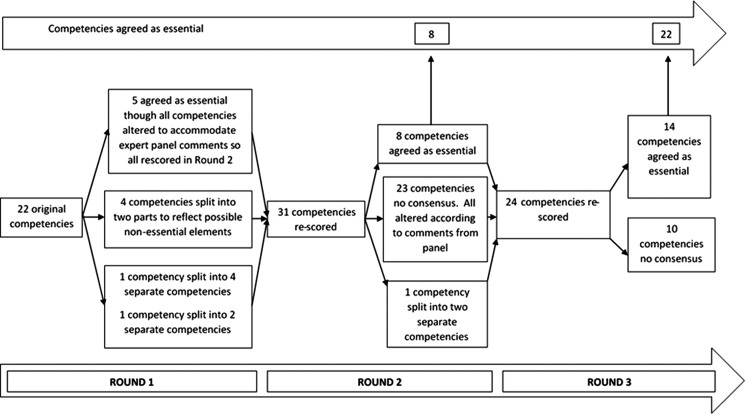
Questionnaire 1 was distributed to panel members in April 2016. Twenty-six of 29 panel members responded. In the first round 5/22 competencies were rated essential, however, due to the panel's comments, the research team thought all competencies required amendment. There was no consensus on 17/22 competencies. From the panel comments, five competencies were split into two and one competency was split into four competencies. This resulted in 31 competencies requiring re-scoring in the second round. See Figure 2.
Figure 2.
Flowchart representing the consensus process.
Round 2
Questionnaire 2, consisting of 31 competencies, was sent to the 26 panel members who had responded to the first questionnaire in May 2016. Twenty-four of 26 responded. In the second round, 8/31 competencies were rated essential by over 80% of the panel. Twenty-three competencies did not reach consensus. All 23 remaining competencies were amended according to panel comments and one competency was split into two competencies. Twenty-four competencies required re-scoring in the third round.
Round 3
Questionnaire 3, consisting of 24 competencies, was sent to the 24 panel members who had responded to the second questionnaire in June 2016. Twenty of 24 responded. In the third round, 14/24 competencies were rated essential by over 80% of the panel. Ten competencies did not reach consensus. Nine of the remaining 10 competencies were agreed by more than half the panel as essential but did not reach the 80% consensus threshold. One competency was rated by more than half of the panel as ‘desirable’ but did not reach the 80% threshold. The final list of competencies and their ratings can be seen in Table 1. (The full competency statements can be found in Appendix 1..
Table 1.
Final list of competencies and their ratings.
| No. | Competency | % E | % D | % I | % FD | |
|---|---|---|---|---|---|---|
| 1 | Attitudes and relationship-centred care | 83 | 4 | 0 | 12 | |
| 2 | Enhancing well-being and maintaining ability | 80 | 0 | 0 | 25 | |
| 3 | Communication | 75 | 0 | 0 | 25 | |
| 4 | Knowledge and understanding of old age | 80 | 5 | 0 | 15 | |
| 5 | Assessment and care planning | a) | 80 | 10 | 0 | 10 |
| b) | 95 | 0 | 0 | 5 | ||
| 6 | Administering procedures and interventions | a) | 55 | 30 | 0 | 15 |
| b) | 15 | 60 | 10 | 15 | ||
| 7 | Hygiene | 92 | 0 | 0 | 8 | |
| 8 | Urinary continence | 88 | 4 | 0 | 8 | |
| 9 | Bowel care | 96 | 0 | 0 | 4 | |
| 10 | Nutrition and hydration | 70 | 10 | 0 | 20 | |
| 11 | Pain management | 100 | 0 | 0 | 0 | |
| 12 | Skin viability | 83 | 4 | 0 | 13 | |
| 13 | Pharmacology | 85 | 0 | 0 | 15 | |
| 14 | Dementia care | a) | 85 | 0 | 0 | 15 |
| b) | 60 | 30 | 0 | 10 | ||
| 15 | Cultural, spiritual and sexual needs of residents | 85 | 0 | 0 | 15 | |
| 16 | Sleep | 80 | 5 | 5 | 10 | |
| 17 | Long-term conditions and comorbidities | 70 | 10 | 0 | 20 | |
| 18 | Managing acute Ill health | 90 | 5 | 0 | 5 | |
| 19 | End of life care | 85 | 5 | 0 | 10 | |
| 20 | Moving and handling | 95 | 0 | 0 | 5 | |
| 21 | Resident safety | 80 | 5 | 0 | 15 | |
| 22 | Team working | 92 | 0 | 0 | 8 | |
| 23 | Management and leadership | 75 | 20 | 0 | 5 | |
| 24 | Teaching | 55 | 30 | 0 | 15 | |
| 25 | Quality improvement and evidence based practice | a) | 80 | 15 | 0 | 5 |
| b) | 75 | 15 | 0 | 10 | ||
| 26 | Policy and procedures | a) | 80 | 15 | 0 | 5 |
| b) | 92 | 0 | 0 | 8 | ||
| 27 | Reflective practice | 92 | 0 | 0 | 8 | |
E, essential; D, desirable; I, irrelevant; FD, further development required; bold, consensus over 80% threshold.
Discussion
By the end of the third round the panel reached consensus on 22 of 32 competencies, indicating they were essential for RNs working in care homes. Ten statements had not reached the 80% threshold, though for nine of these over 50% of the panel agreed the competencies were essential. For one competency, over 50% agreed the competency was desirable.
The panel raised a number of contentious points which prevented consensus on some competencies. Some panel members indicated that the competency list should reflect what is achievable for the present workforce and that certain competencies would not be expected of a newly qualified nurse. Other panel members were more aspirational, commenting on the necessity to set a ‘gold standard’ in care home nursing, raise the skill level of all nurses considering care home work and build future capacity in care home nursing by encouraging skills that, although little utilised at present, may be necessary in the future as long-term care changes with the needs of the population. These views were demonstrated in discussion of the use of intravenous injections and syringe drivers.
Another difficulty was accommodating the heterogeneity of care home contexts, and differing nursing obligations, within a single set of competencies. Respondents noted a nurse could be the only qualified healthcare professional on shift, or one of a team of RNs. A curriculum could differentiate between these roles by considering a two-tiered approach to a care home nursing qualification. Competency in dementia care was controversial as some claimed this knowledge was only essential for dementia specialist homes. Others quoted the expected rise in care home residents with dementia as an incentive for all nurses to be skilled in dementia care.
The methodology of this study facilitated experts from disparate backgrounds to state their opinion, without the dynamics of a face-to-face group situation. The method of feedback in each round prevented the research process from getting mired in certain topics as can be the case with a consensus conference. The nature of the Delphi process yields results that are dependent on the opinions of the panel. Although the research team attempted to form a panel that represented many stakeholder groups, we had no representatives from care home residents or their family members.
It must be taken into account that this process has not resulted in a complete set of competencies. The number of rounds was capped to encourage retention of the panel and the rounds necessary to reach consensus on each competency would not have been feasible. Face-to-face discussion of the wording of these competencies, and the sharing of reasons for ratings among panel members, might have resulted in a more informed consensus between panel members. In addition the threshold of consensus was placed relatively high at 80%. If this threshold had been set lower, e.g. at 70% as in other studies [31], another five competencies would have reached consensus.
The competencies produced through the consensus exercise are an important reminder of the broad contribution that RNs can make to high quality care in a care home setting. This extends beyond task-oriented aspects of care which mandatorily require RN input, such as drug administration and injections. Thus these competencies provide an opportunity to revisit the role of nurses, ensuring that their full potential contribution to care in care homes is explored and realised.
Conclusion
We propose that we have identified competencies that are agreed to be sufficiently broad and comprehensive to form the basis of a curriculum for nurses wanting to practise in care homes. We suggest that it would be reasonable for authors of such curricula to choose, in addition, to incorporate some of those domains where the pooled consensus across the ‘essential’ and ‘needs further development’ columns equals greater than or equal to 80%. Those areas where the balance of consensus hangs in the ‘further development’ column, we contest, are those areas where the competency statements require further evaluation by experts in the field in order to appropriately capture the skills required on this topic. These points notwithstanding, given the paucity of structured education specific to care home nurses in general, it would perhaps be best to start in areas where the greatest consensus was achieved. These domains should be seen as educational priorities.
Key points.
The role of care home nursing is underdeveloped and it is seen as a low status career.
Competency development will define a career pathway in care home nursing and increase the status of work in this area
A modified Delphi study enables experts to come to consensus on a competency framework for RNs working in care homes
Consensus was reached on the necessity of 22/32 competencies to form the basis of a curriculum for RNs working in care homes
Supplementary Material
Acknowledgements
The authors would like to thank Optimum Workforce Development (Nottinghamshire County Council) for funding this project. We would also like to thank Emily Cousins (Institute of Mental Health) for her work on the literature review process. Many thanks to the participants in the focus groups and to all involved in the expert panel. The panel were: Jane Balmbra (OT, Falls Lead for Rushcliffe), Sharon Blackburn (RGN RMN, Policy & Communications Director, National Care Forum), Susan Briggs (Physiotherapist, Care Home Advisory Service for Derbyshire Community Health Services NHS Foundation Trust), Andrew Clegg (Clinical Senior Lecturer & Honorary Consultant Geriatrician, Deputy Lead for NIHR CLAHRC Older People's Theme, Academic Unit of Elderly Care and Rehabilitation, Bradford Institute for Health Research), Cheryl Crocker (Regional Lead Patient Safety Collaborative, East Midlands Academic Health Science Network), Tom Dening (Professor of Dementia Research, Faculty of Medicine & Health Sciences, University of Nottingham), Jenny Fantom (Falls Lead, Falls Prevention Service), Dawne Garrett (Professional Lead for Care of Older People Royal College of Nursing), Claire Goodman (Professor of Health Care Research, Centre for Research in Primary and Community Care), Barbara Hanratty (Professor of Primary Care and Public Health), Hazel Heath (Independent Nurse Consultant), Steve Iliffe (Emeritus Professor of Primary care for Older People, University College London), Annabelle Long (Research Physiotherapist, Guide to Action for falls prevention in Care Homes (GtACH) project), Jane Machin (OT, Adult Social Care, Health & Public Protection), Finbarr Martin (Consultant Geriatrician, Department of Ageing and Health, Guys and St Thomas’ NHS Foundation Trust), Christine McAlpine (Consultant, Department of Medicine for the Elderly, Glasgow Royal Infirmary), Louise McGregor (Chair of the AGILE network), Julienne Meyer (Professor of Nursing, Care for Older People, City University London, Executive Director: My Home Life programme), Mandy Miles (Advanced Nurse Practitioner, Erewash Care Home Support Service), Hannah Needle (Physiotherapist, Derbyshire Care Home Advisory Service), William Peet (RN, Wren Hall nursing Home), Sam Pessoll (Interim Integrated Community Team Lead for Chesterfield and Care Home Advisory Services), Isabella Robbins (RN, Associate Research Fellow, Division of Rehabilitation and Ageing, University of Nottingham), Kate Robertson (Consultant Therapist in Falls Prevention), Louise Robinson (Director of Newcastle University Institute for Ageing, Professor of Primary Care and Ageing, RCGP National Champion for Dementia), Deborah Sturdy (Nurse Advisor for Older People), Sanja Thompson (Consultant Geriatrician, Foundation Training Programme Director, Senior Fellow HEA, Honorary Senior Clinical Lecturer University of Oxford), Iain Wilkinson (Honorary Clinical Senior Lecturer – BSMS, Consultant Orthogeriatrician) and Rebecca Wilson (Occupational Therapist, City Specialist Dementia Outreach Team). Lastly, the author would like to thank the AQUEDUCT project for allowing the time to prepare this article for publication.
Supplementary data
Conflicts of interest
None declared.
References
- 1. Care Quality Commission The State of Health Care and Adult Social Care in England. House of Commons; 2014. Retrieved from https://www.cqc.org.uk/sites/default/files/state-of-care-201314-full-report-1.1.pdf.
- 2. Spilsbury K, Hanratty B, McCaughan D Supporting Nursing in Care Homes. The RCN Foundation Patient Care and Professional Development for Nursing Staff in Care and Nursing Homes: A Research and Consultation Project, 2015.
- 3. Abbey J, Liddle J, Bridges P et al. Clinical placements in residential aged care facilities: the impact on nursing students’ perception of aged care and the effect on career plans. Aust J Adv Nurs 2006; 23: 14. [PubMed] [Google Scholar]
- 4. Xiao LD, Kelton M, Paterson J. Critical action research applied in critical placement development in aged care facilities. Nurs Inq 2012; 19: 322–33. [DOI] [PubMed] [Google Scholar]
- 5. Hayes LJ, O'Brien-Pallas L, Duffield C et al. Nurse turnover: a literature review. Int J Nurs Stud 2006; 43: 237–63. [DOI] [PubMed] [Google Scholar]
- 6. Hasson H, Arnetz JE. Nursing staff competence, work strain, stress and satisfaction in elderly care: a comparison of home‐based care and nursing homes. J Clin Nurs 2008; 17: 468–81. [DOI] [PubMed] [Google Scholar]
- 7. Brodaty H, Draper B, Low LF. Nursing home staff attitudes towards residents with dementia: strain and satisfaction with work. J Adv Nurs 2003; 44: 583–90. [DOI] [PubMed] [Google Scholar]
- 8. Hannan S, Norman IJ, Redfern SJ. Care work and quality of care for older people: a review of the research literature. Rev Clin Gerontol 2001; 11: 189–203. [Google Scholar]
- 9. Diamond IR, Grant RC, Feldman BM et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol 2014; 67: 401–9. [DOI] [PubMed] [Google Scholar]
- 10. Aud MA, Bostick JE, Marek KD, McDaniel RW. Introducing baccalaureate student nurses to gerontological nursing. J Prof Nurs 2006; 22: 73–8. [DOI] [PubMed] [Google Scholar]
- 11. Borson S, Reichman WE, Coyne AC, Rovner B, Sakauye K. Effectiveness of nursing home staff as managers of disruptive behavior: perceptions of nursing directors. Am J Geriatr Psychiatry 2000; 8: 251–3. [PubMed] [Google Scholar]
- 12. Bourbonniere M, Strumpf NE. Enhancing geriatric nursing competencies for RNs in nursing homes. Res Gerontol Nurs 2008; 1: 171–5. [DOI] [PubMed] [Google Scholar]
- 13. Bradway C, DiResta J, Miller E, Edmiston J, Fleshner I, Polomano RC. Caring for obese individuals in the longterm care setting. Ann Long Term Care 2009; 17: 17–21. [Google Scholar]
- 14. Crogan NL, Pasvogel A. The influence of protein-calorie malnutrition on quality of life in nursing homes. J Gerontol A Biol Sci Med Sci 2003; 58: M159–64. [DOI] [PubMed] [Google Scholar]
- 15. DeHart D, Webb J, Cornman C. Prevention of elder mistreatment in nursing homes: competencies for direct-care staff. J Elder Abuse Negl 2009; 21: 360–78. [DOI] [PubMed] [Google Scholar]
- 16. Ersek M, Grant MM, Kraybill BM. Enhancing end-of-life care in nursing homes: Palliative Care Educational Resource Team (PERT) program. J Palliat Med 2005; 8: 556–66. [DOI] [PubMed] [Google Scholar]
- 17. Glass JC Jr, Todd-Atkinson S. Continuing education needs of nurses employed in nursing facilities. J Contin Educ Nurs; 30: 219–28. [DOI] [PubMed] [Google Scholar]
- 18. Gould E, Reed P. Alzheimer's Association Quality Care Campaign and professional training initiatives: improving hands-on care for people with dementia in the USA. Int Psychogeriatr 2009; 21(S1):S25–33. [DOI] [PubMed] [Google Scholar]
- 19. Hasson H, Arnetz JE. Nursing staff competence, work strain, stress and satisfaction in elderly care: a comparison of home‐based care and nursing homes. J Clin Nurs 2008; 17: 468–81. [DOI] [PubMed] [Google Scholar]
- 20. Koivunen M, Välimäki M, Jakobsson T, Pitkänen A. Developing an evidence-based curriculum designed to help psychiatric nurses learn to use computers and the Internet. J Prof Nurs 2008; 24: 302–14. [DOI] [PubMed] [Google Scholar]
- 21. Lees L, Hill C, Coles T. Without prejudice: results and realisation of a training needs audit in nursing homes. Nurs Older People 2006; 18: 19–27. [DOI] [PubMed] [Google Scholar]
- 22. Marshall-Gray CBP, Laurence A, Green A, Valadez A, Scott-Tilley D, Merritt P. Geriatric Training Academy: innovative education for certified nurse aides and charge nurses. J Gerontol Nurs 2007; 33: 37–44. [DOI] [PubMed] [Google Scholar]
- 23. Mueller C, Burger S, Rader J, Carter D. Nurse competencies for person-directed care in nursing homes. Geriatr Nurs (Minneap) 2013; 34: 101–4. [DOI] [PubMed] [Google Scholar]
- 24. O'Rourke D. Enhanced orientation for nurses new to long-term care. Appl Workplace Sol Nurs 2012; 25: 64– 70. [DOI] [PubMed] [Google Scholar]
- 25. Smith M, Stolder ME, Jaggers B, Liu MF, Haedtke C. Depression training in nursing homes: Lessons learned from a pilot study. Issues Ment Health Nurs 2013; 34: 90–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Steel K, Ribbe M, Ahronheim J et al. Incorporating education on palliative care into the long‐term care setting. J Am Geriatr Soc 1999; 47: 904–7. [DOI] [PubMed] [Google Scholar]
- 27. Walker BL, Osgood NJ, Ephross PH, Richardson JP, Farrar B, Cole C. Developing a training curriculum on elderly sexuality for long term care facility staff. Gerontol Geriatr Educ 1998; 19: 3–22. [Google Scholar]
- 28. Wallace M, Greiner P, Lange J. Development, implementation, and evaluation of a geriatric nurse education program. J Contin Educ Nurs 2006; 37: 214. [DOI] [PubMed] [Google Scholar]
- 29. British Geriatrics Society Fit for Frailty: Consensus best practice guidance for the care of older people living with frailty in community and outpatient settings; 2014. Retrieved from http://www.bgs.org.uk/campaigns/fff/fff_full.pdf.
- 30. Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Pract Assess Res Eval 2007; 12: 1–8. [Google Scholar]
- 31. Goldberg SE, Cooper J, Blundell A, Gordon AL, Masud T, Moorchilot R. Development of a curriculum for advanced nurse practitioners working with older people with frailty in the acute hospital through a modified Delphi process. Age Ageing 2016; 45: 48–53. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.