Abstract
We investigated the association between dairy product consumption and all-cause, cardiovascular disease (CVD), and cancer mortality in the Golestan Cohort Study, a prospective cohort study launched in January 2004 in Golestan Province, northeastern Iran. A total of 42,403 men and women participated in the study and completed a diet questionnaire at enrollment. Cox proportional hazards models were used to estimate hazard ratios and 95% confidence intervals. We documented 3,291 deaths (1,467 from CVD and 859 from cancer) during 11 years of follow-up (2004–2015). The highest quintile of total dairy product consumption (versus the lowest) was associated with 19% lower all-cause mortality risk (hazard ratio (HR) = 0.81, 95% confidence interval (CI): 0.72, 0.91; Ptrend = 0.006) and 28% lower CVD mortality risk (HR = 0.72, 95% CI: 0.60, 0.86; Ptrend = 0.005). High consumption of low-fat dairy food was associated with lower risk of all-cause (HR = 0.83, 95% CI: 0.73, 0.94; Ptrend = 0.002) and CVD (HR = 0.74, 95% CI: 0.61, 0.89; Ptrend = 0.001) mortality. We noted 11% lower all-cause mortality and 16% lower CVD mortality risk with high yogurt intake. Cheese intake was associated with 16% lower all-cause mortality and 26% lower CVD mortality risk. Higher intake of high-fat dairy food and milk was not associated with all-cause or CVD mortality. Neither intake of individual dairy products nor intake of total dairy products was significantly associated with overall cancer mortality. High consumption of dairy products, especially yogurt and cheese, may reduce the risk of overall and CVD mortality.
Keywords: cancer, cardiovascular disease, cheese, dairy products, Golestan Cohort Study, milk, mortality, yogurt
An estimate for the year 2012 indicated that mortality from cardiovascular disease (CVD) comprised more than 46% of all deaths that occurred in Iran (1). Cancer is the third leading cause of death in Iran and accounts for 13% of all Iranian deaths (1). Dairy foods are major sources of vitamins and minerals that can play a protective role in CVD and cancer risk factors (2–6), whereas saturated fats (7, 8) and anabolic hormones (9) in some dairy products might affect the health benefit aspects of dairy foods. Previous studies have investigated the associations of milk and total dairy product consumption with the risk of all-cause, CVD, and cancer mortality, with inconsistent findings (10–29). Whereas meta-analyses of prospective cohort studies found a null association between milk intake and all-cause mortality risk (30, 31), more recently Michaëlsson et al. (20) reported a higher risk of CVD, cancer, and all-cause mortality with high milk consumption in Sweden. The roles of other dairy foods, such as yogurt or cheese, in mortality risk are less clear (20, 21, 23–25). Notably, most prior evidence on the association between dairy food consumption and mortality risk has been from studies carried out in Western countries with high dairy food consumption, especially high milk intake; the relationships of dairy foods to mortality risk in countries with lower dairy food consumption have been minimally studied. To address the role of dairy product consumption in mortality risk, we examined the association between dairy food consumption and CVD, cancer, and all-cause mortality in a generally healthy population in Iran, using data from the Golestan Cohort Study.
METHODS
Study population
The Golestan Cohort Study is a prospective population-based cohort study of 50,045 participants (21,234 men and 28,811 women) aged 36–85 years. It was launched in January 2004 in northeastern Iran (Golestan Province). Study participants were selected using random sampling of persons without a history of upper gastrointestinal cancer who lived in Gonbad City and 326 villages in Golestan Province. Further details have been provided elsewhere (32). Our analyses included men and women who completed a food frequency questionnaire (n = 49,112) at baseline. Among those participants, we excluded men and women who were lost to follow-up (n = 63), had an implausible total energy intake (<600 kcal/day or >4,200 kcal/day) (n = 436), or had reported a prior diagnosis of cancer, diabetes, heart disease, or stroke (n = 6,210). After these exclusions, data from 42,403 participants (18,261 men (43%) and 24,142 women (57%)) aged 36–83 years (mean age = 51.6 (standard deviation (SD), 8.8) years) were available for analysis.
This study was approved by the institutional review boards of the Digestive Disease Research Center of Tehran University of Medical Sciences, the US National Cancer Institute, the World Health Organization's International Agency for Research on Cancer, and the Harvard T.H. Chan School of Public Health. All participants gave written informed consent before enrollment.
Dietary assessment
At enrollment, nutritional data were collected by face-to-face interview using a 116-item food frequency questionnaire that was specifically designed and validated for this population (33). The validity of the questionnaire to assess dietary intake was evaluated by comparison with 12 24-hour diet recalls; the correlation for dietary protein intake was 0.76 (33). Total dairy product items listed in the food frequency questionnaire included milk, cheese, yogurt, liquid yogurt (doogh), dried yogurt paste (kashk), and cream (see Web Table 1, available at http://aje.oxfordjournals.org/). Responses were given for commonly used portion sizes and frequency of intake per day, week, month, or year. The standard serving sizes for these food items were 230 g for milk and yogurt, 350 g for doogh, 28 g for cheese, 72 g for kashk, and 15 g for cream. The reported frequencies and portion sizes for each food item were then converted to average daily intake. To determine energy intake, we multiplied the amount of each food item consumed (g/day) by the energy composition of each item using Iranian (34) and US Department of Agriculture (35) databases.
Assessment of covariates
At enrollment, face-to-face interviews were conducted to collect data on lifestyle variables and medical history using a general questionnaire. This questionnaire included detailed queries on sex, age, ethnicity, marital status, residential history, occupation, education, smoking habits, opium use, alcohol drinking, indicators of socioeconomic status, and medical history, including self-reports of medically diagnosed diabetes mellitus, heart disease, stroke, and cancer (36). Occupational physical activities were reported in 4 levels. Level 1 activities were defined as sedentary work, mostly done while sitting (e.g., driving); level 2 activities involved standing or occasional walking (e.g., teaching); level 3 activities were defined as mainly indoor activities causing a mild increase in heart rate and sweating (e.g., housekeeping); and level 4 activities involved those causing a significant increase in heart rate and sweating, and were usually performed outdoors (e.g., farming) (36). Height and weight were measured by the trained research staff. Systolic and diastolic blood pressures for each participant were also measured twice on both arms, with 10-minute intervals, in the sitting position. A wealth score was calculated as described in detail elsewhere (37). Briefly, to build a composite score for wealth, multiple correspondence analysis was used on the variables house ownership, house structure, house size, having a bath in the residence, and occupation, as well as possession of a personal automobile, a motorbike, a black-and-white television, a color television, a refrigerator, a freezer, a vacuum cleaner, and a washing machine.
Ascertainment of cause of death
All participants are being followed up annually by means of telephone calls. Deaths are reported by family members, friends, or local health workers through annual telephone calls, followed by a physician visit and completion of a verbal autopsy questionnaire, which has been validated for this population (38). For the current study, all available and relevant medical documents, including medical charts, radiographs, pathology reports, hospital discharge documents, etc., were gathered from the appropriate hospitals or pathology centers, either within the province or in neighboring provinces. All collected documents were reviewed, and the primary cause of death was documented on the basis of the International Classification of Diseases, Tenth Revision (ICD-10). The cause of death was coded as “unknown” if a final diagnosis could not be determined for any reason. In this analysis, we also specifically considered deaths due to CVD (ICD-10 codes I00–I99), coronary heart disease (CHD) (ICD-10 codes I20–I52), stroke (ICD-10 codes I60–I69), total cancer (ICD-10 codes C00–C97 and D00–D48), gastrointestinal cancer (ICD-10 codes C15–C26), and other types of cancer (ICD-10 codes C00–C14, C30–C97, and D00–D48).
Statistical analysis
The participants contributed person-years to the study from the date of completed questionnaires to the date of death or the last date of follow-up (June 1, 2015), whichever came first. Participants were divided into 5 categories (quintiles) according to food group. For high-fat dairy foods, milk, and cheese, participants who did not eat high-fat dairy foods, milk, or cheese were assigned to the lowest group and others were divided into 4 categories. Cox proportional hazards models were used to estimate unadjusted and adjusted hazard ratios and 95% confidence intervals for risk of all-cause and disease-specific mortality in a given quintile of consumption of total dairy products, low-fat dairy foods, high-fat dairy foods, milk, yogurt, and cheese, compared with persons in the lowest quintile. In multivariate models, we controlled for measured known confounders (36, 39–41), including age, sex, ethnicity, educational level, marital status, place of residence, cigarette smoking, opium use, alcohol intake, body mass index (BMI; weight (kg)/height (m)2), systolic blood pressure, occupational physical activity, family history of cancer, wealth score, medication use, and total energy intake (see table footnotes for their categorizations). The median value for each quintile was modeled as a continuous variable and used to estimate the hazard ratios and 95% confidence intervals for a 1-serving/day increase in intake, as well as for tests for trend. We replaced missing covariate data, which comprised 5 participants for BMI and 8 participants for systolic blood pressure, with median values. To examine whether the observed associations were independent of other dietary intake, we further adjusted for consumption of fruits and vegetables, grains, and total red meat (including the sum of unprocessed and processed red meat). Smoking and obesity are leading causes of death, and mortality risk differs by age and sex (1, 40, 41). Therefore, we examined whether the association of dairy product consumption with all-cause mortality risk differed by sex, age, BMI, or smoking. Interactions between dairy product consumption and these factors were examined by including appropriate interaction terms in the Cox proportional hazards models. STATA, version 12 (StataCorp LP, College Station, Texas), was used for all analyses. All P values were 2-sided. P values less than 0.05 were considered statistically significant.
RESULTS
During a maximum of 11 years (average = 8 years) of follow-up from January 2004 through June 1, 2015, among men and women in the Golestan Cohort Study, we documented 3,291 deaths (1,938 deaths among men and 1,353 deaths among women). A total of 1,467 deaths were due to CVD, and 859 deaths were caused by cancer. Mean total dairy product consumption was 1.3 (SD, 0.9) servings/day (range, 0–11.7 servings/day) at enrollment. A total of 123 participants did not consume any kind of dairy products, 342 consumed no low-fat dairy food, 4,255 consumed no high-fat dairy food, 6,183 consumed no milk, 662 consumed no yogurt, and 3,405 consumed no cheese. The main dairy products consumed were yogurt (38%, of which 89% was low/medium-fat); cheese (33%, of which 97% was low/medium-fat), and milk (20%, of which 12% was low/medium-fat). As compared with participants who consumed dairy products less frequently, those who consumed dairy products more frequently were more likely to be male, married, smokers, and Turkmen, more likely to have a greater BMI, less likely to engage in higher levels of activity during work, and less likely to live in a rural area (Table 1).
Table 1.
Characteristics of Participants in the Golestan Cohort Study According to Quintile of Total Dairy Product Consumption at Baseline, Iran, 2004
| Characteristic | Quintile of Total Dairy Product Consumption | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 (n = 8,480) | 2 (n = 8,481) | 3 (n = 8,480) | 4 (n = 8,481) | 5 (n = 8,481) | ||||||
| Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | |
| Dietary intake, servings/day | ||||||||||
| Dairy products | ||||||||||
| Total dairy products | 0.35 (0.16) | 0.79 (0.11) | 1.16 (0.11) | 1.59 (0.15) | 2.64 (0.83) | |||||
| Low-fat dairy products | 0.26 (0.16) | 0.58 (0.20) | 0.81 (0.28) | 1.07 (0.38) | 1.49 (0.72) | |||||
| High-fat dairy products | 0.09 (0.11) | 0.21 (0.19) | 0.34 (0.27) | 0.52 (0.38) | 1.15 (0.90) | |||||
| Milk | 0.06 (0.08) | 0.14 (0.14) | 0.23 (0.20) | 0.34 (0.26) | 0.57 (0.42) | |||||
| Yogurt | 0.15 (0.12) | 0.32 (0.16) | 0.43 (0.20) | 0.57 (0.24) | 0.88 (0.55) | |||||
| Cheese | 0.12 (0.12) | 0.29 (0.19) | 0.41 (0.25) | 0.52 (0.32) | 0.67 (0.47) | |||||
| Total red meat | 0.11 (0.17) | 0.17 (0.20) | 0.20 (0.19) | 0.23 (0.23) | 0.27 (0.26) | |||||
| Grains | 12.2 (5.1) | 12.5 (4.7) | 12.7 (4.7) | 12.8 (4.8) | 13.2 (4.9) | |||||
| Total fruits | 1.12 (1.12) | 1.50 (1.18) | 1.80 (1.35) | 2.14 (1.56) | 2.78 (2.05) | |||||
| Total vegetables | 1.09 (0.68) | 1.28 (0.75) | 1.43 (0.82) | 1.60 (0.93) | 1.83 (1.15) | |||||
| Total energy intake, kcal/day | 1,839 (534) | 2,030 (498) | 2,158 (497) | 2,295 (512) | 2,539 (557) | |||||
| Age, years | 52.1 (9.0) | 51.4 (8.7) | 51.3 (8.7) | 51.3 (8.6) | 51.9 (8.9) | |||||
| Body mass indexa | 25.5 (5.4) | 26.3 (5.6) | 26.6 (5.3) | 26.9 (5.3) | 27.0 (5.2) | |||||
| Male sex | 36 | 39 | 42 | 45 | 53 | |||||
| Ethnicity (Turkmen) | 64 | 74 | 77 | 79 | 83 | |||||
| Married | 84 | 87 | 88 | 91 | 92 | |||||
| Current smoker | 13 | 13 | 14 | 14 | 16 | |||||
| Opium user | 20 | 16 | 16 | 15 | 15 | |||||
| Rural residence | 91 | 86 | 82 | 76 | 68 | |||||
| Occupational physical activityb | ||||||||||
| Level 1 | 3 | 3 | 2 | 2 | 3 | |||||
| Level 2 | 2 | 3 | 5 | 7 | 10 | |||||
| Level 3 | 53 | 56 | 56 | 57 | 51 | |||||
| Level 4 | 42 | 38 | 37 | 34 | 36 | |||||
Abbreviation: SD, standard deviation.
a Weight (kg)/height (m)2.
b Level 1 activities were defined as sedentary work, mostly done while sitting (e.g., driving); level 2 activities involved standing or occasional walking (e.g., teaching); level 3 activities were defined as mainly indoor activities causing a mild increase in heart rate and sweating (e.g., housekeeping); and level 4 activities involved those causing a significant increase in heart rate and sweating, and were usually performed outdoors (e.g., farming) (36).
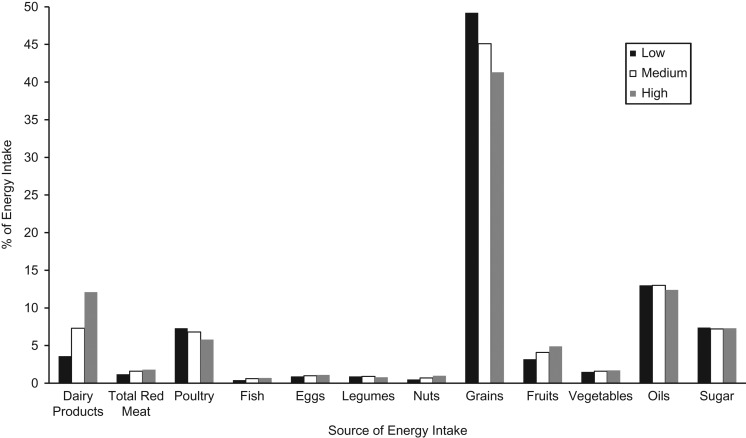
To describe and visualize changes in dietary habits according to increasing total dairy product consumption, we calculated the percentage of energy intake from each food group according to tertile of total dairy product consumption. An increase in dairy product intake was mainly associated with a decrease in the percentage of energy intake from grains (Figure 1).
Figure 1.
Percentage of energy intake derived from various food groups according to intake of total dairy products (low (<0.9 servings/day), medium (0.9–1.5 servings/day), or high (>1.5 servings/day)) among men and women at baseline in the Golestan Cohort Study, Iran, 2004. Sources of energy intake from sugar included sugar and sugared foods and beverages.
Dairy products and all-cause mortality
Age-adjusted and multivariate-adjusted analyses showed a significant inverse association between frequency of dairy product consumption and all-cause mortality risk. Comparing the highest quintile of total dairy product consumption with the lowest, the multivariate hazard ratio for all-cause mortality risk was 0.81 (95% confidence interval (CI): 0.72, 0.91; Ptrend = 0.006). Having the highest intake of low-fat dairy food versus the lowest was associated with a 17% lower death risk (hazard ratio for highest quintile vs. lowest (HRHvL) = 0.83, 95% CI: 0.73, 0.94; Ptrend = 0.002) (Table 2). The inverse association between low-fat dairy products was still significant after additional adjustment for intake of fruits and vegetables (HRHvL = 0.85, 95% CI: 0.75, 0.97; Ptrend = 0.01), grains (HRHvL = 0.84, 95% CI: 0.74, 0.95; Ptrend = 0.005), or total red meat (HRHvL = 0.82, 95% CI: 0.73, 0.93; Ptrend = 0.001). Further adjustment for high-fat dairy food consumption did not change the association (HRHvL = 0.83, 95% CI: 0.74, 0.94; Ptrend = 0.003). Yogurt was associated with lower all-cause mortality risk (HRHvL = 0.89, 95% CI: 0.79, 1.00; Ptrend = 0.03), as was cheese intake (HRHvL = 0.84, 95% CI: 0.73, 0.96; Ptrend = 0.02) (Table 2). A similar association was observed for low/medium-fat yogurt (data not shown). Since the participants in this cohort usually consumed low/medium-fat cheese and only 3% of them consumed high-fat cheese, this association was mainly due to low/medium-fat cheese intake. We did not observe a significant association between intake of high-fat dairy foods or milk and all-cause mortality risk. Since the majority of milk intake was high-fat (88%) and the mean intake of low/medium-fat milk was 0.04 (SD, 0.16) servings/day, we could not evaluate the association between low/medium-fat milk consumption and mortality risk. Among the covariates, wealth score accounted for most of the difference in hazard ratios for dairy foods between the age-adjusted models and the multivariate-adjusted models. We observed stronger associations between dairy food consumption and all-cause mortality risk when we used multivariate-adjusted models that excluded wealth score. However, the associations were still nonsignificant for milk and high-fat dairy foods (Web Table 2).
Table 2.
Hazard Ratios for All-Cause Mortality According to Quintile of Dairy Product Consumption Among Men and Women in the Golestan Cohort Study, Iran, 2004–2015
| Quintile of DairyProduct Intake | Median Intake, servings/day | All-Cause Mortality | |||||
|---|---|---|---|---|---|---|---|
| No. of Deaths | Person-Years of Follow-up | Age-Adjusted HR | 95% CI | Multivariate-Adjusted HRa | 95% CI | ||
| Total Dairy Products | |||||||
| 1 | 0.4 | 838 | 65,618 | 1 | Referent | 1 | Referent |
| 2 | 0.8 | 613 | 66,887 | 0.77 | 0.69, 0.85 | 0.85 | 0.76, 0.95 |
| 3 | 1.2 | 595 | 67,270 | 0.74 | 0.67, 0.83 | 0.87 | 0.78, 0.97 |
| 4 | 1.6 | 615 | 68,590 | 0.75 | 0.68, 0.84 | 0.90 | 0.81, 1.01 |
| 5 | 2.4 | 630 | 71,501 | 0.68 | 0.61, 0.75 | 0.81 | 0.72, 0.91 |
| Ptrend | <0.0001 | 0.006 | |||||
| Per serving/day | 0.85 | 0.81, 0.89 | 0.92 | 0.87, 0.98 | |||
| Low-Fat Dairy Products | |||||||
| 1 | 0.2 | 857 | 66,541 | 1 | Referent | 1 | Referent |
| 2 | 0.5 | 670 | 66,808 | 0.84 | 0.76, 0.93 | 0.92 | 0.83, 1.02 |
| 3 | 0.8 | 639 | 67,289 | 0.80 | 0.73, 0.89 | 0.92 | 0.83, 1.02 |
| 4 | 1.0 | 575 | 67,961 | 0.74 | 0.66, 0.82 | 0.86 | 0.77, 0.96 |
| 5 | 1.6 | 550 | 71,268 | 0.67 | 0.60, 0.74 | 0.83 | 0.73, 0.94 |
| Ptrend | <0.0001 | 0.002 | |||||
| Per serving/day | 0.75 | 0.70, 0.81 | 0.88 | 0.81, 0.95 | |||
| High-Fat Dairy Products | |||||||
| 1 | 0 | 330 | 33,291 | 1 | Referent | 1 | Referent |
| 2 | 0.05 | 747 | 76,224 | 1.11 | 0.98, 1.27 | 1.06 | 0.93, 1.21 |
| 3 | 0.2 | 728 | 74,365 | 1.10 | 0.96, 1.25 | 1.05 | 0.92, 1.20 |
| 4 | 0.5 | 685 | 77,484 | 0.96 | 0.84, 1.10 | 0.97 | 0.84, 1.11 |
| 5 | 1.1 | 801 | 78,504 | 1.01 | 0.89, 1.15 | 1.01 | 0.88, 1.16 |
| Ptrend | 0.08 | 0.43 | |||||
| Per serving/day | 0.93 | 0.85, 1.01 | 0.96 | 0.88, 1.06 | |||
| Milk | |||||||
| 1 | 0 | 479 | 48,304 | 1 | Referent | 1 | Referent |
| 2 | 0.04 | 730 | 70,988 | 1.07 | 0.96, 1.20 | 1.00 | 0.89, 1.13 |
| 3 | 0.1 | 647 | 66,404 | 0.96 | 0.85, 1.08 | 0.98 | 0.87, 1.11 |
| 4 | 0.3 | 616 | 72,901 | 0.84 | 0.74, 0.94 | 0.89 | 0.79, 1.01 |
| 5 | 0.6 | 819 | 81,271 | 0.88 | 0.78, 0.98 | 1.00 | 0.89, 1.13 |
| Ptrend | <0.0001 | 0.98 | |||||
| Per serving/day | 0.76 | 0.65, 0.87 | 1.00 | 0.86, 1.16 | |||
| Yogurt | |||||||
| 1 | 0.1 | 784 | 65,749 | 1 | Referent | 1 | Referent |
| 2 | 0.3 | 669 | 66,603 | 0.86 | 0.78, 0.96 | 0.94 | 0.85, 1.05 |
| 3 | 0.4 | 625 | 67,047 | 0.83 | 0.75, 0.92 | 0.95 | 0.85, 1.06 |
| 4 | 0.6 | 583 | 68,889 | 0.71 | 0.64, 0.79 | 0.86 | 0.77, 0.97 |
| 5 | 0.9 | 630 | 71,579 | 0.75 | 0.68, 0.84 | 0.89 | 0.79, 1.00 |
| Ptrend | <0.0001 | 0.03 | |||||
| Per serving/day | 0.67 | 0.59, 0.77 | 0.85 | 0.73, 0.98 | |||
| Cheese | |||||||
| 1 | 0 | 382 | 26,394 | 1 | Referent | 1 | Referent |
| 2 | 0.1 | 872 | 79,955 | 0.94 | 0.84, 1.06 | 0.91 | 0.80, 1.03 |
| 3 | 0.3 | 664 | 68,829 | 0.85 | 0.75, 0.97 | 0.91 | 0.80, 1.03 |
| 4 | 0.5 | 745 | 85,901 | 0.80 | 0.71, 0.91 | 0.86 | 0.76, 0.98 |
| 5 | 0.8 | 628 | 78,789 | 0.74 | 0.66, 0.85 | 0.84 | 0.73, 0.96 |
| Ptrend | <0.0001 | 0.02 | |||||
| Per serving/day | 0.71 | 0.63, 0.81 | 0.85 | 0.75, 0.97 | |||
Abbreviations: CI, confidence interval; HR, hazard ratio.
a The multivariate model adjusted for sex, age (years), ethnicity (Turkmen, Persian, other), education (illiterate, ≤5 years, 6–8 years, high school, college), marital status (married, other), residency (rural, urban), smoking (never smoker, former smoker, current smoker of <20 packs/year, current smoker of 20–29 packs/year, current smoker of ≥30 packs/year), opium use (user, nonuser), alcohol use (user, nonuser), body mass index (weight (kg)/height (m)2; <18.5, 18.5–<20.0, 20.0–<22.5, 22.5–<25.0, 25.0–<30.0, 30–<35.0, ≥35.0), systolic blood pressure (mm Hg; quintiles), occupational physical activity (sedentary; standing or occasional walking; activity causing a mild increase in heart rate and sweating; activity causing a significant increase in heart rate and sweating), family history of cancer (yes, no), wealth scoreb (quintiles), medication use, and energy intake (kcal/day; quintiles).
b The wealth score is described in detail elsewhere (37). Briefly, to build a composite score for wealth, multiple correspondence analysis was used on the variables house ownership, house structure, house size, having a bath in the residence, and occupation, as well as possession of a personal automobile, a motorbike, a black-and-white television, a color television, a refrigerator, a freezer, a vacuum cleaner, and a washing machine.
Dairy products and CVD mortality
In multivariate analysis, total dairy product consumption was associated with lower risk of CVD mortality (HRHvL = 0.72, 95% CI: 0.60, 0.86; Ptrend = 0.005) (Table 3), CHD mortality (HRHvL = 0.73, 95% CI: 0.57, 0.93; Ptrend = 0.03) (Web Table 3), and stroke mortality (HRHvL = 0.63, 95% CI: 0.46, 0.86; Ptrend = 0.01) (Web Table 3). Being in the highest quintile of low-fat dairy product consumption (versus the lowest) was associated with a 26% lower risk of CVD mortality, a 34% lower risk of CHD mortality, and a 32% lower risk of stroke mortality. Similar associations were observed when we additionally adjusted for fruit and vegetable intake (for total CVD mortality, HRHvL = 0.73, 95% CI: 0.60, 0.88 (Ptrend = 0.001); for CHD mortality, HRHvL = 0.66, 95% CI: 0.51, 0.86 (Ptrend = 0.003); and for stroke mortality, HRHvL = 0.66, 95% CI: 0.48, 0.93 (Ptrend = 0.005)). In addition, these associations were independent of total red meat or grain intake (data not shown). Comparing the highest quintile with the lowest, yogurt intake was associated with a lower CVD mortality risk (HRHvL = 0.84, 95% CI: 0.70, 1.00; Ptrend = 0.03) (Table 3) and a lower CHD mortality risk (HRHvL = 0.73, 95% CI: 0.57, 0.93; Ptrend = 0.01) (Web Table 3) but not a lower stroke mortality risk (HRHvL = 0.89, 95% CI: 0.66, 1.21; Ptrend = 0.24) (Web Table 3). Similar point estimates were noted for low/medium-fat yogurt (data not shown). We also observed an inverse association between cheese intake and CVD mortality risk (HRHvL = 0.74, 95% CI: 0.61, 0.91; Ptrend = 0.02), as well as for CHD mortality risk. We did not observe any significant association between either high-fat dairy product intake or milk intake and CVD, CHD, or stroke mortality risk (Table 3 and Web Table 3). Stronger associations were observed in multivariate models without adjustment for wealth score (Web Table 4).
Table 3.
Hazard Ratios for Cardiovascular Disease Mortality According to Quintile of Dairy Product Consumption Among Men and Women in the Golestan Cohort Study, Iran, 2004–2015
| Quintile of Dairy Product Intake | Median Intake, servings/day | Cardiovascular Disease Mortality | |||||
|---|---|---|---|---|---|---|---|
| No. of Deaths | Person-Years of Follow-up | Age-Adjusted HR | 95% CI | Multivariate-Adjusted HRa | 95% CI | ||
| Total Dairy Products | |||||||
| 1 | 0.4 | 396 | 65,618 | 1 | Referent | 1 | Referent |
| 2 | 0.8 | 254 | 66,887 | 0.68 | 0.58, 0.79 | 0.74 | 0.63, 0.87 |
| 3 | 1.2 | 271 | 67,270 | 0.72 | 0.62, 0.84 | 0.81 | 0.69, 0.96 |
| 4 | 1.6 | 272 | 68,590 | 0.71 | 0.61, 0.83 | 0.82 | 0.69, 0.97 |
| 5 | 2.4 | 274 | 71,501 | 0.63 | 0.54, 0.74 | 0.72 | 0.60, 0.86 |
| Ptrend | <0.0001 | 0.005 | |||||
| Per serving/day | 0.83 | 0.77, 0.89 | 0.88 | 0.81, 0.96 | |||
| Low-Fat Dairy Products | |||||||
| 1 | 0.2 | 389 | 66,541 | 1 | Referent | 1 | Referent |
| 2 | 0.5 | 304 | 66,808 | 0.84 | 0.72, 0.98 | 0.91 | 0.78, 1.06 |
| 3 | 0.8 | 271 | 67,289 | 0.76 | 0.65, 0.88 | 0.84 | 0.71, 0.98 |
| 4 | 1.0 | 266 | 67,961 | 0.76 | 0.65, 0.89 | 0.84 | 0.71, 0.99 |
| 5 | 1.6 | 237 | 71,268 | 0.64 | 0.55, 0.76 | 0.74 | 0.61, 0.89 |
| Ptrend | <0.0001 | 0.001 | |||||
| Per serving/day | 0.74 | 0.66, 0.83 | 0.81 | 0.71, 0.92 | |||
| High-Fat Dairy Products | |||||||
| 1 | 0 | 135 | 33,291 | 1 | Referent | 1 | Referent |
| 2 | 0.05 | 348 | 76,224 | 1.28 | 1.05, 1.57 | 1.26 | 1.03, 1.54 |
| 3 | 0.2 | 348 | 74,365 | 1.29 | 1.06, 1.57 | 1.30 | 1.06, 1.59 |
| 4 | 0.5 | 289 | 77,484 | 1.00 | 0.82, 1.23 | 1.06 | 0.86, 1.31 |
| 5 | 1.1 | 347 | 78,504 | 1.07 | 0.88, 1.31 | 1.14 | 0.92, 1.40 |
| Ptrend | 0.045 | 0.32 | |||||
| Per serving/day | 0.88 | 0.77, 1.00 | 0.93 | 0.81, 1.07 | |||
| Milk | |||||||
| 1 | 0 | 210 | 48,304 | 1 | Referent | 1 | Referent |
| 2 | 0.04 | 343 | 70,988 | 1.15 | 0.97, 1.37 | 1.10 | 0.92, 1.30 |
| 3 | 0.1 | 288 | 66,404 | 0.98 | 0.82, 1.17 | 1.00 | 0.84, 1.20 |
| 4 | 0.3 | 264 | 72,901 | 0.82 | 0.68, 0.98 | 0.89 | 0.74, 1.07 |
| 5 | 0.6 | 362 | 81,271 | 0.88 | 0.74, 1.04 | 1.00 | 0.84, 1.20 |
| Ptrend | 0.002 | 0.46 | |||||
| Per serving/day | 0.71 | 0.57, 0.88 | 0.92 | 0.73, 1.15 | |||
| Yogurt | |||||||
| 1 | 0.1 | 351 | 65,749 | 1 | Referent | 1 | Referent |
| 2 | 0.3 | 307 | 66,603 | 0.89 | 0.76, 1.04 | 0.96 | 0.82, 1.12 |
| 3 | 0.4 | 270 | 67,047 | 0.81 | 0.69, 0.95 | 0.90 | 0.76, 1.06 |
| 4 | 0.6 | 264 | 68,889 | 0.72 | 0.62, 0.85 | 0.84 | 0.71, 0.99 |
| 5 | 0.9 | 275 | 71,579 | 0.75 | 0.64, 0.87 | 0.84 | 0.70, 1.00 |
| Ptrend | <0.0001 | 0.03 | |||||
| Per serving/day | 0.66 | 0.54, 0.81 | 0.78 | 0.62, 0.97 | |||
| Cheese | |||||||
| 1 | 0 | 185 | 26,394 | 1 | Referent | 1 | Referent |
| 2 | 0.1 | 383 | 79,955 | 0.87 | 0.73, 1.04 | 0.85 | 0.71, 1.02 |
| 3 | 0.3 | 284 | 68,829 | 0.77 | 0.64, 0.92 | 0.82 | 0.68, 0.99 |
| 4 | 0.5 | 344 | 85,901 | 0.78 | 0.65, 0.93 | 0.84 | 0.70, 1.01 |
| 5 | 0.8 | 271 | 78,789 | 0.68 | 0.56, 0.82 | 0.74 | 0.61, 0.91 |
| Ptrend | <0.0001 | 0.02 | |||||
| Per serving/day | 0.69 | 0.58, 0.83 | 0.79 | 0.66, 0.96 | |||
Abbreviations: CI, confidence interval; HR, hazard ratio.
a The multivariate model adjusted for sex, age (years), ethnicity (Turkmen, Persian, other), education (illiterate, ≤5 years, 6–8 years, high school, college), marital status (married, other), residency (rural, urban), smoking (never smoker, former smoker, current smoker of <20 packs/year, current smoker of 20–29 packs/year, current smoker of ≥30 packs/year), opium use (user, nonuser), alcohol use (user, nonuser), body mass index (weight (kg)/height (m)2; <18.5, 18.5–<20.0, 20.0–<22.5, 22.5–<25.0, 25.0–<30.0, 30–<35.0, ≥35.0), systolic blood pressure (mm Hg; quintiles), occupational physical activity (sedentary; standing or occasional walking; activity causing a mild increase in heart rate and sweating; activity causing a significant increase in heart rate and sweating), family history of cancer (yes, no), wealth score (quintiles; see Table 2), medication use, and energy intake (kcal/day; quintiles).
Dairy products and cancer mortality
After adjustment for confounding variables, total dairy product consumption was not associated with risk of total cancer mortality (HRHvL = 0.81, 95% CI: 0.64, 1.02; Ptrend = 0.23) (Table 4), gastrointestinal cancer mortality (HRHvL = 0.88, 95% CI: 0.65, 1.19; Ptrend = 0.77) (Web Table 5), or other cancer mortality (HRHvL = 0.71, 95% CI: 0.50, 1.02; Ptrend = 0.12) (Web Table 5). However, the association was significant for total cancer mortality risk in the multivariate model without adjustment for wealth score (Web Table 6). Neither low-fat dairy product consumption nor high-fat dairy product consumption was associated with cancer mortality risk. Consumption of milk, yogurt, and cheese was not associated with risk of total cancer, gastrointestinal cancer, or other cancer mortality (Table 4 and Web Table 5). However, we found a significant inverse association between yogurt intake and risk of total cancer and gastrointestinal cancer mortality without adjusting for wealth score (Web Table 6).
Table 4.
Hazard Ratios for Total Cancer Mortality According to Quintile of Dairy Product Consumption Among Men and Women in the Golestan Cohort Study, Iran, 2004–2015
| Quintile of Dairy Product Intake | Median Intake, servings/day | Total Cancer Mortality | |||||
|---|---|---|---|---|---|---|---|
| No. of Deaths | Person-Years of Follow-up | Age-Adjusted HR | 95% CI | Multivariate-Adjusted HRa | 95% CI | ||
| Total Dairy Products | |||||||
| 1 | 0.4 | 221 | 65,618 | 1 | Referent | 1 | Referent |
| 2 | 0.8 | 152 | 66,887 | 0.72 | 0.58, 0.88 | 0.77 | 0.63, 0.95 |
| 3 | 1.2 | 148 | 67,270 | 0.70 | 0.57, 0.86 | 0.79 | 0.64, 0.98 |
| 4 | 1.6 | 162 | 68,590 | 0.75 | 0.61, 0.92 | 0.87 | 0.70, 1.08 |
| 5 | 2.4 | 176 | 71,501 | 0.72 | 0.59, 0.88 | 0.81 | 0.64, 1.02 |
| Ptrend | 0.01 | 0.23 | |||||
| Per serving/day | 0.88 | 0.80, 0.97 | 0.93 | 0.84, 1.04 | |||
| Low-Fat Dairy Products | |||||||
| 1 | 0.2 | 214 | 66,541 | 1 | Referent | 1 | Referent |
| 2 | 0.5 | 173 | 66,808 | 0.86 | 0.70, 1.05 | 0.92 | 0.75, 1.12 |
| 3 | 0.8 | 176 | 67,289 | 0.88 | 0.72, 1.08 | 0.99 | 0.80, 1.22 |
| 4 | 1.0 | 148 | 67,961 | 0.76 | 0.61, 0.93 | 0.88 | 0.70, 1.10 |
| 5 | 1.6 | 148 | 71,268 | 0.72 | 0.58, 0.88 | 0.91 | 0.72, 1.16 |
| Ptrend | 0.001 | 0.44 | |||||
| Per serving/day | 0.79 | 0.68, 0.91 | 0.94 | 0.80, 1.10 | |||
| High-Fat Dairy Products | |||||||
| 1 | 0 | 99 | 33,291 | 1 | Referent | 1 | Referent |
| 2 | 0.05 | 179 | 76,224 | 0.88 | 0.69, 1.13 | 0.79 | 0.62, 1.02 |
| 3 | 0.2 | 194 | 74,365 | 0.96 | 0.76, 1.23 | 0.85 | 0.66, 1.09 |
| 4 | 0.5 | 172 | 77,484 | 0.80 | 0.63, 1.03 | 0.71 | 0.55, 0.92 |
| 5 | 1.1 | 215 | 78,504 | 0.90 | 0.71, 1.15 | 0.77 | 0.59, 0.99 |
| Ptrend | 0.61 | 0.20 | |||||
| Per serving/day | 0.96 | 0.81, 1.13 | 0.89 | 0.74, 1.06 | |||
| Milk | |||||||
| 1 | 0 | 137 | 48,304 | 1 | Referent | 1 | Referent |
| 2 | 0.04 | 170 | 70,988 | 0.87 | 0.70, 1.09 | 0.80 | 0.64, 1.00 |
| 3 | 0.1 | 178 | 66,404 | 0.93 | 0.74, 1.16 | 0.93 | 0.74, 1.17 |
| 4 | 0.3 | 162 | 72,901 | 0.77 | 0.61, 0.97 | 0.79 | 0.63, 0.99 |
| 5 | 0.6 | 212 | 81,271 | 0.80 | 0.65, 1.00 | 0.87 | 0.69, 1.09 |
| Ptrend | 0.06 | 0.65 | |||||
| Per serving/day | 0.76 | 0.58, 1.01 | 0.93 | 0.69, 1.26 | |||
| Yogurt | |||||||
| 1 | 0.1 | 207 | 65,749 | 1 | Referent | 1 | Referent |
| 2 | 0.3 | 172 | 66,603 | 0.84 | 0.69, 1.03 | 0.88 | 0.72, 1.08 |
| 3 | 0.4 | 162 | 67,047 | 0.81 | 0.66, 1.00 | 0.88 | 0.71, 1.09 |
| 4 | 0.6 | 147 | 68,889 | 0.68 | 0.55, 0.84 | 0.78 | 0.63, 0.98 |
| 5 | 0.9 | 171 | 71,579 | 0.78 | 0.64, 0.95 | 0.86 | 0.69, 1.08 |
| Ptrend | 0.006 | 0.18 | |||||
| Per serving/day | 0.70 | 0.54, 0.90 | 0.82 | 0.62, 1.09 | |||
| Cheese | |||||||
| 1 | 0 | 87 | 26,394 | 1 | Referent | 1 | Referent |
| 2 | 0.1 | 228 | 79,955 | 1.07 | 0.83, 1.37 | 0.99 | 0.77, 1.27 |
| 3 | 0.3 | 165 | 68,829 | 0.92 | 0.71, 1.19 | 0.92 | 0.71, 1.20 |
| 4 | 0.5 | 206 | 85,901 | 0.95 | 0.74, 1.23 | 0.99 | 0.77, 1.29 |
| 5 | 0.8 | 173 | 78,789 | 0.89 | 0.68, 1.15 | 0.98 | 0.75, 1.29 |
| Ptrend | 0.10 | 0.99 | |||||
| Per serving/day | 0.82 | 0.65, 1.04 | 1.00 | 0.78, 1.29 | |||
Abbreviations: CI, confidence interval; HR, hazard ratio.
a The multivariate model adjusted for sex, age (years), ethnicity (Turkmen, Persian, other), education (illiterate, ≤5 years, 6–8 years, high school, college), marital status (married, other), residency (rural, urban), smoking (never smoker, former smoker, current smoker of <20 packs/year, current smoker of 20–29 packs/year, current smoker of ≥30 packs/year), opium use (user, nonuser), alcohol use (user, nonuser), body mass index (weight (kg)/height (m)2; <18.5, 18.5–<20.0, 20.0–<22.5, 22.5–<25.0, 25.0–<30.0, 30–<35.0, ≥35.0), systolic blood pressure (mm Hg; quintiles), occupational physical activity (sedentary; standing or occasional walking; activity causing a mild increase in heart rate and sweating; activity causing a significant increase in heart rate and sweating), family history of cancer (yes, no), wealth score (quintiles; see Table 2), medication use, and energy intake (kcal/day; quintiles).
Sensitivity analysis
In sensitivity analyses, we excluded participants who died due to external events (i.e., accidents, intoxication, suicide, or other types of injury; n = 217) from all-cause mortality risk. The results were minimally changed: Comparing the highest quintile with the lowest, the hazard ratio was 0.82 (95% CI: 0.72, 0.93; Ptrend = 0.02) for total dairy products, 0.83 (95% CI: 0.73, 0.94; Ptrend = 0.003) for low-fat dairy products, 1.03 (95% CI: 0.89, 1.18; Ptrend = 0.63) for high-fat dairy products, 1.01 (95% CI: 0.90, 1.14; Ptrend = 0.80) for milk, 0.90 (95% CI: 0.80, 1.02) (Ptrend = 0.09) for yogurt, and 0.82 (95% CI: 0.71, 0.94; Ptrend = 0.01) for cheese.
Given that greater BMI was observed with higher dairy intake (Table 1), it could be that adjustment for BMI reflected overcontrol for confounders. Therefore, in sensitivity analysis, we used multivariate models that excluded measures of BMI. The associations were materially unchanged (data not shown).
We also examined whether the association between dairy product consumption and all-cause mortality risk differed according to levels of sex, age, BMI, and smoking. The association between total dairy products and all-cause mortality risk was modified by BMI. For the highest quintile of total dairy product consumption versus the lowest, the mortality risk was 22% lower among participants who had BMI <30 (HRHvL = 0.78, 95% CI: 0.68, 0.89; Ptrend = 0.001), with a nonsignificant association in participants with BMI ≥30 (HRHvL = 0.96, 95% CI: 0.72, 1.30; Ptrend = 0.74) (Pinteraction = 0.01) (Table 5). Similar interactions were observed for low-fat dairy foods and yogurt. On the other hand, high intake of milk was associated with higher risk of mortality among obese participants (Pinteraction = 0.01) (Table 5). We also examined whether the associations between dairy product consumption and CVD and cancer mortality risk were modified by BMI. High intake of yogurt was significantly associated with lower risk of CVD mortality among nonobese participants (Pinteraction = 0.045) (Web Table 7). In addition, a lower risk of total cancer mortality was observed with high intakes of low-fat dairy products and yogurt among nonobese participants but not obese ones (for low-fat dairy products, Pinteraction = 0.002; for yogurt, Pinteraction = 0.001) (Web Table 8).
Table 5.
Multivariable-Adjusted Hazard Ratios for All-Cause Mortality According to Dairy Product Consumption and Body Mass Index Among Participants in the Golestan Cohort Study, Iran, 2004–2015
| Quintile of Dairy Product Intake | Median Intake, servings/day | Body Mass Indexa | |||||||
|---|---|---|---|---|---|---|---|---|---|
| <30 | ≥30 | ||||||||
| No. of Deaths | Person-Years of Follow-up | Multivariate-Adjusted HRb | 95% CI | No. of Deaths | Person-Years of Follow-up | Multivariate-Adjusted HRb | 95% CI | ||
| Total Dairy Products | |||||||||
| 1 | 0.4 | 733 | 52,644 | 1 | Referent | 105 | 12,974 | 1 | Referent |
| 2 | 0.8 | 522 | 50,415 | 0.86 | 0.77, 0.96 | 91 | 16,473 | 0.81 | 0.61, 1.08 |
| 3 | 1.2 | 490 | 50,342 | 0.86 | 0.76, 0.97 | 105 | 16,928 | 0.89 | 0.67, 1.18 |
| 4 | 1.6 | 508 | 50,536 | 0.90 | 0.80, 1.02 | 107 | 18,054 | 0.90 | 0.67, 1.20 |
| 5 | 2.4 | 493 | 52,165 | 0.78 | 0.68, 0.89 | 137 | 19,336 | 0.96 | 0.72, 1.30 |
| Ptrend | 0.001 | 0.74 | |||||||
| Pinteraction | 0.01 | ||||||||
| Low-Fat Dairy Products | |||||||||
| 1 | 0.2 | 749 | 53,943 | 1 | Referent | 108 | 12,598 | 1 | Referent |
| 2 | 0.5 | 592 | 51,854 | 0.96 | 0.86, 1.07 | 78 | 14,954 | 0.70 | 0.52, 0.94 |
| 3 | 0.8 | 526 | 50,520 | 0.91 | 0.81, 1.02 | 113 | 16,769 | 0.93 | 0.70, 1.22 |
| 4 | 1.0 | 466 | 50,128 | 0.84 | 0.74, 0.95 | 109 | 17,833 | 0.91 | 0.68, 1.21 |
| 5 | 1.6 | 413 | 49,656 | 0.81 | 0.71, 0.93 | 137 | 21,612 | 0.86 | 0.65, 1.15 |
| Ptrend | 0.001 | 0.78 | |||||||
| Pinteraction | 0.03 | ||||||||
| High-Fat Dairy Products | |||||||||
| 1 | 0 | 268 | 24,728 | 1 | Referent | 62 | 8,564 | 1 | Referent |
| 2 | 0.05 | 628 | 56,282 | 1.13 | 0.97, 1.30 | 119 | 19,941 | 0.82 | 0.60, 1.12 |
| 3 | 0.2 | 618 | 56,024 | 1.10 | 0.95, 1.28 | 110 | 18,341 | 0.85 | 0.61, 1.17 |
| 4 | 0.5 | 570 | 58,834 | 1.00 | 0.86, 1.16 | 115 | 18,649 | 0.83 | 0.60, 1.15 |
| 5 | 1.1 | 662 | 60,234 | 1.03 | 0.89, 1.20 | 139 | 18,270 | 0.95 | 0.69, 1.31 |
| Ptrend | 0.25 | 0.44 | |||||||
| Pinteraction | 0.09 | ||||||||
| Milk | |||||||||
| 1 | 0 | 420 | 36,850 | 1 | Referent | 59 | 11,453 | 1 | Referent |
| 2 | 0.04 | 621 | 54,286 | 0.98 | 0.86, 1.11 | 109 | 16,701 | 1.20 | 0.87, 1.65 |
| 3 | 0.1 | 529 | 49,590 | 0.93 | 0.82, 1.06 | 118 | 16,814 | 1.28 | 0.93, 1.75 |
| 4 | 0.3 | 521 | 55,123 | 0.88 | 0.77, 1.00 | 95 | 17,778 | 1.04 | 0.75, 1.44 |
| 5 | 0.6 | 655 | 60,252 | 0.95 | 0.83, 1.08 | 164 | 21,019 | 1.41 | 1.03, 1.92 |
| Ptrend | 0.45 | 0.07 | |||||||
| Pinteraction | 0.01 | ||||||||
| Yogurt | |||||||||
| 1 | 0.1 | 687 | 53,058 | 1 | Referent | 97 | 12,691 | 1 | Referent |
| 2 | 0.3 | 573 | 51,144 | 0.94 | 0.84, 1.06 | 96 | 15,459 | 0.92 | 0.69, 1.23 |
| 3 | 0.4 | 538 | 50,736 | 0.96 | 0.86, 1.08 | 87 | 16,311 | 0.80 | 0.59, 1.09 |
| 4 | 0.6 | 465 | 50,224 | 0.84 | 0.74, 0.95 | 118 | 18,665 | 0.94 | 0.70, 1.25 |
| 5 | 0.9 | 483 | 50,940 | 0.85 | 0.75, 0.97 | 147 | 20,639 | 1.00 | 0.75, 1.33 |
| Ptrend | 0.005 | 0.68 | |||||||
| Pinteraction | 0.01 | ||||||||
| Cheese | |||||||||
| 1 | 0 | 328 | 20,563 | 1 | Referent | 54 | 5,830 | 1 | Referent |
| 2 | 0.1 | 740 | 62,439 | 0.90 | 0.79, 1.03 | 132 | 17,516 | 0.95 | 0.69, 1.30 |
| 3 | 0.3 | 565 | 52,057 | 0.91 | 0.79, 1.05 | 99 | 16,771 | 0.89 | 0.64, 1.24 |
| 4 | 0.5 | 620 | 63,513 | 0.87 | 0.76, 1.00 | 125 | 22,388 | 0.84 | 0.61, 1.17 |
| 5 | 0.8 | 493 | 57,529 | 0.81 | 0.70, 0.94 | 135 | 21,259 | 0.97 | 0.70, 1.35 |
| Ptrend | 0.009 | 1.00 | |||||||
| Pinteraction | 0.11 | ||||||||
Abbreviations: CI, confidence interval; HR, hazard ratio.
a Weight (kg)/height (m)2.
b The multivariate model adjusted for sex, age (years), ethnicity (Turkmen, Persian, other), education (illiterate, ≤5 years, 6–8 years, high school, college), marital status (married, other), residency (rural, urban), smoking (never smoker, former smoker, current smoker of <20 packs/year, current smoker of 20–29 packs/year, current smoker of ≥30 packs/year), opium use (user, nonuser), alcohol use (user, nonuser), systolic blood pressure (mm Hg; quintiles), occupational physical activity (sedentary; standing or occasional walking; activity causing a mild increase in heart rate and sweating; activity causing a significant increase in heart rate and sweating), family history of cancer (yes, no), wealth score (quintiles; see Table 2), medication use, and energy intake (kcal/day; quintiles).
DISCUSSION
In this large cohort study in Iran, we found inverse associations between consumption of dairy products and CVD and all-cause mortality risk, after adjusting for potential confounders. The associations were more apparent for intakes of low-fat dairy products, yogurt, and cheese. Adjustment for red meat, grain, or fruit and vegetable intake did not appreciably change the associations. We did not observe significant associations between specific or total dairy product consumption and cancer mortality risk.
There is mixed evidence from prospective studies concerning a role of dairy food consumption in mortality risk (10–29). Consistent with our results, in the Whitehall II Study (21), higher consumption of dairy products was associated with reduced all-cause mortality risk in comparison with the lowest intake. Similar findings for total dairy products and mortality risk have been reported among men and women in Switzerland (22). Previous findings in the Whitehall II Study (21), the Rotterdam Study (23), the Hoorn Study (24), and the European Prospective Investigation into Cancer and Nutrition–Netherlands (EPIC-NL) cohort study (25) did not support a significant inverse association between yogurt consumption and CVD mortality risk. We observed that yogurt consumption was associated with lower risk of all-cause and CVD mortality. The amount of yogurt consumed was higher in the current study than in other studies, which may have led to significantly reduced CVD and all-cause mortality risk. We also found a suggestion that high cheese intake was inversely associated with all-cause and CVD mortality risk. Previous findings on cheese intake have been few and inconsistent (20, 21, 23–25). Among Swedish men and women, cheese intake decreased CVD, cancer, and all-cause mortality risk (20). However, cheese intake was not associated with mortality risk in the Whitehall II Study (21), the Rotterdam Study (23), the Hoorn Study (24), or EPIC-NL (25). This heterogeneity of results between studies and populations might be due to the different composition of dairy products and interactions with other dietary and nondietary factors. In nutrition, the effect of a food or nutrient is usually dependent on background diet. Dairy products are most likely to be beneficial if the background diet is poor and dairy foods are displacing starch intake. Further, our analysis found inverse associations between consumption of most dairy foods, especially low-fat versions, and mortality risk. It is possible that saturated fats in high-fat dairy products might dilute the beneficial health effects of dairy foods (8) and could explain the discrepant findings of prior studies with respect to dairy foods and mortality risk.
In the present study, milk consumption was not related to all-cause, CVD, or cancer mortality. In a systematic review and meta-analysis of prospective studies, Soedamah-Muthu et al. (31) found that milk consumption was not associated with all-cause mortality risk. Although more recently a study of a Japanese cohort showed a significant inverse association between milk intake and mortality risk in men (26), Michaëlsson et al. (20) analyzed data from 2 Swedish cohorts and reported higher risk of CVD, cancer, and all-cause mortality with high milk consumption. These differences are probably partly due to the far higher milk consumption in Sweden (240 g/day in women and 290 g/day in men) relative to Iran (57 g/day in women and 69 g/day in men) and Japan. Failure to exclude participants with diabetes, coronary heart disease, and other morbidity that could affect dietary intake at baseline in the Swedish study could also have resulted in confounding.
Dairy food consumption was not associated with gastrointestinal or total cancer mortality risk. Few epidemiologic studies have investigated whether a high dairy food intake is associated with cancer mortality risk (20, 27–29). While in the Michaëlsson et al. study high milk intake was associated with higher cancer mortality risk in Swedish women but not men, there were no significant associations between cheese or yogurt and cancer mortality risk (20). Lower fatal colorectal cancer risk (27) and higher fatal prostate cancer risk (29) have both been reported in conjunction with high milk consumption.
Several explanations for our findings are possible. Clinical trials have shown that consumption of dairy foods has beneficial effects on levels of some cardiometabolic risk factors, including lipid profiles (42), hypertension (43, 44), and insulin resistance (45). In addition, fermented dairy products and probiotic bacteria may have beneficial health effects on blood cholesterol, blood pressure, and immune function (46, 47) and may provide prophylactic protection against heart disease (48), diabetes (49, 50), and stroke (51). Moreover, in prospective cohort studies, increased consumption of yogurt and other dairy foods was associated with less weight gain and lower waist circumference (52, 53). However, in the present study, higher dairy product consumption was associated with higher BMI (Table 1), and an interaction with BMI was observed. Health benefits of dairy foods in nonobese individuals could be explained by the fact that obesity, one of the leading causes of death, may attenuate the advantage of dairy products in increasing life expectancy or delaying death in persons with higher BMI. Milk fortified with vitamin D, which is consumed in some countries, may have additional cardioprotective benefits (6). Notably, because dairy foods are not fortified with vitamin D in Iran, the cardioprotective influence of dairy products would be independent of vitamin D.
Potential limitations of this study should be considered. Residual confounding is always of concern in any observational study. Our comprehensive adjustment for many potential confounders minimized residual confounding, although we could not rule out the influence of unmeasured or unknown confounders. Measurement error in the consumption of dairy products is another potential limitation. Dairy food consumption was evaluated by self-report at 1 point in time, and there is a possibility that men and women might have changed their dietary habits during the follow-up period. However, based on a report of the Food and Agriculture Organization, trends in the production, export, import, and consumption of dairy foods changed minimally from 2004 through 2014 in Iran (54, 55). Moreover, underreporting of food intake, particularly in obese participants, is likely. However, the effect of this would have biased the observed associations toward the null.
Our study had several strengths. The prospective and population-based study design and the high follow-up rate minimized the risk of potential selection bias. Dietary information was obtained from participants without preexisting diabetes, CVD, or cancer, minimizing the possibility of recall bias. The large number of deaths provided adequate statistical power to detect modest differences in risk, as well as the ability to examine disease-specific mortality risk. Furthermore, longitudinal studies regarding the relationship between dairy product consumption and mortality risk in Iran are lacking, and the Golestan Cohort Study is a unique cohort study in which we evaluated the role of dairy products in populations with different lifestyle patterns and socioeconomic backgrounds.
In summary, our results from a large-scale cohort study in Iran showed significant inverse associations of dairy food consumption, especially consumption of low-fat dairy foods, with all-cause and CVD mortality risk. We also noted that higher yogurt consumption and higher cheese consumption were specifically associated with lower risk of all-cause and CVD mortality in the present study. We observed that the relationship between dairy foods and all-cause mortality risk differed by body weight, with a lower risk in nonobese individuals, as was also seen for total cancer mortality. Further studies are warranted to investigate the health effects of dairy products and to identify biological mechanisms.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Nutrition, Harvard T.H. Chan School of Public Health, Boston, Massachusetts (Maryam S. Farvid, Walter C. Willett); Digestive Disease Research Center, Digestive Disease Research Institute, Tehran University of Medical Sciences, Tehran, Iran (Maryam S. Farvid, Akbar F. Malekshah, Akram Pourshams, Sadaf G. Sepanlou, Maryam Sharafkhah, Reza Malekzadeh); Digestive Oncology Research Center, Digestive Disease Research Institute, Tehran University of Medical Sciences, Tehran, Iran (Akbar F. Malekshah, Sadaf G. Sepanlou, Hossein Poustchi, Reza Malekzadeh); Liver and Pancreatobiliary Diseases Research Center, Digestive Disease Research Institute, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran (Akram Pourshams, Hossein Poustchi, Maryam Sharafkhah, Reza Malekzadeh); Golestan Research Center of Gastroenterology and Hepatology, Golestan University of Medical Sciences, Gorgan, Iran (Masoud Khoshnia); independent researcher, Växjö, Sweden (Mojtaba Farvid); Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, Maryland (Christian C. Abnet, Sanford M. Dawsey); Department of Public Health Analysis, School of Community Health and Policy, Morgan State University, Baltimore, Maryland (Farin Kamangar); Section of Genetics, International Agency for Research on Cancer, Lyon, France (Paul Brennan); Departments of Oncology and Public Health and Primary Care, School of Clinical Medicine, University of Cambridge, Cambridge, United Kingdom (Paul D. Pharoah); Tisch Cancer Institute and Institute for Translational Epidemiology, Icahn School of Medicine at Mount Sinai, New York, New York (Paolo Boffetta); Department of Epidemiology, Harvard T.H. Chan School of Public Health, Boston, Massachusetts (Walter C. Willett); and Channing Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston, Massachusetts (Walter C. Willett).
This work was supported by Tehran University of Medical Sciences (grant 82-603); Cancer Research UK (grant C20/A5860); the Intramural Research Program of the National Cancer Institute, US National Institutes of Health (grant Z01 CP000185-03); and various collaborative research agreements with the International Agency for Research on Cancer. M.F. was supported by a Takemi Fellowship from the Japan Pharmaceutical Manufacturers Association.
We thank the Behvarz’ working in the study areas for their help. We thank the directors of the public health districts of Gonbad and Kalaleh for their collaboration. We express our special thanks to the general physicians, nurses, and nutritionists on the enrollment teams for their collaboration and assistance. We received special support from the Social Security Organization of Iran, Golestan branch. We have enjoyed the close collaboration of the Golestan health deputies and the chief of the Gonbad health district.
Conflict of interest: none declared.
REFERENCES
- 1. World Health Organization Iran (Islamic Republic of). (Noncommunicable diseases country profiles 2014). http://www.who.int/nmh/countries/irn_en.pdf?ua=1. Published 2014. Accessed February 24, 2016.
- 2. Soedamah-Muthu SS, Verberne LD, Ding EL, et al. Dairy consumption and incidence of hypertension: a dose-response meta-analysis of prospective cohort studies. Hypertension. 2012;60(5):1131–1137. [DOI] [PubMed] [Google Scholar]
- 3. Elwood PC, Pickering JE, Fehily AM. Milk and dairy consumption, diabetes and the metabolic syndrome: the Caerphilly prospective study. J Epidemiol Community Health. 2007;61(8):695–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Krishnan AV, Feldman D. Mechanisms of the anti-cancer and anti-inflammatory actions of vitamin D. Annu Rev Pharmacol Toxicol. 2011;51:311–336. [DOI] [PubMed] [Google Scholar]
- 5. Mamede AC, Tavares SD, Abrantes AM, et al. The role of vitamins in cancer: a review. Nutr Cancer. 2011;63(4):479–494. [DOI] [PubMed] [Google Scholar]
- 6. Pérez-Hernández N, Aptilon-Duque G, Nostroza-Hernández MC, et al. Vitamin D and its effects on cardiovascular diseases: a comprehensive review. Korean J Intern Med. 2016;31(6):1018–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ohlsson L. Dairy products and plasma cholesterol levels. Food Nutr Res. 2010;54:10.3402/fnr.v54i0.5124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chien KL, Lin HJ, Hsu HC, et al. Comparison of predictive performance of various fatty acids for the risk of cardiovascular disease events and all-cause deaths in a community-based cohort. Atherosclerosis. 2013;230(1):140–147. [DOI] [PubMed] [Google Scholar]
- 9. Aune D, Navarro Rosenblatt DA, Chan DS, et al. Dairy products, calcium, and prostate cancer risk: a systematic review and meta-analysis of cohort studies. Am J Clin Nutr. 2015;101(1):87–117. [DOI] [PubMed] [Google Scholar]
- 10. Kahn HA, Phillips RL, Snowdon DA, et al. Association between reported diet and all-cause mortality. Twenty-one-year follow-up on 27,530 adult Seventh-Day Adventists. Am J Epidemiol. 1984;119(5):775–787. [DOI] [PubMed] [Google Scholar]
- 11. Mann JI, Appleby PN, Key TJ, et al. Dietary determinants of ischaemic heart disease in health conscious individuals. Heart. 1997;78(5):450–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fraser GE, Shavlik DJ. Risk factors for all-cause and coronary heart disease mortality in the oldest-old. The Adventist Health Study. Arch Intern Med. 1997;157(19):2249–2258. [PubMed] [Google Scholar]
- 13. Whiteman D, Muir J, Jones L, et al. Dietary questions as determinants of mortality: the OXCHECK experience. Public Health Nutr. 1999;2(4):477–487. [DOI] [PubMed] [Google Scholar]
- 14. Fortes C, Forastiere F, Farchi S, et al. Diet and overall survival in a cohort of very elderly people. Epidemiology. 2000;11(4):440–445. [DOI] [PubMed] [Google Scholar]
- 15. Ness AR, Smith GD, Hart C. Milk, coronary heart disease and mortality. J Epidemiol Community Health. 2001;55(6):379–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Elwood PC, Pickering JE, Fehily AM, et al. Milk drinking, ischaemic heart disease and ischaemic stroke I. Evidence from the Caerphilly cohort. Eur J Clin Nutr. 2004;58(5):711–717. [DOI] [PubMed] [Google Scholar]
- 17. Knoops KT, Groot de LC, Fidanza F, et al. Comparison of three different dietary scores in relation to 10-year mortality in elderly European subjects: the HALE project. Eur J Clin Nutr. 2006;60(6):746–755. [DOI] [PubMed] [Google Scholar]
- 18. Paganini-Hill A, Kawas CH, Corrada MM. Non-alcoholic beverage and caffeine consumption and mortality: the Leisure World Cohort Study. Prev Med. 2007;44(4):305–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bonthuis M, Hughes MC, Ibiebele TI, et al. Dairy consumption and patterns of mortality of Australian adults. Eur J Clin Nutr. 2010;64(6):569–577. [DOI] [PubMed] [Google Scholar]
- 20. Michaëlsson K, Wolk A, Langenskiöld S, et al. Milk intake and risk of mortality and fractures in women and men: cohort studies. BMJ. 2014;349:g6015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Soedamah-Muthu SS, Masset G, Verberne L, et al. Consumption of dairy products and associations with incident diabetes, CHD and mortality in the Whitehall II study. Br J Nutr. 2013;109(4):718–726. [DOI] [PubMed] [Google Scholar]
- 22. Vormund K, Braun J, Rohrmann S, et al. Mediterranean diet and mortality in Switzerland: an alpine paradox. Eur J Nutr. 2015;54(1):139–148. [DOI] [PubMed] [Google Scholar]
- 23. Praagman J, Franco OH, Ikram MA, et al. Dairy products and the risk of stroke and coronary heart disease: the Rotterdam Study. Eur J Nutr. 2015;54(6):981–990. [DOI] [PubMed] [Google Scholar]
- 24. van Aerde MA, Soedamah-Muthu SS, Geleijnse JM, et al. Dairy intake in relation to cardiovascular disease mortality and all-cause mortality: the Hoorn Study. Eur J Nutr. 2013;52(2):609–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Praagman J, Dalmeijer GW, van der Schouw YT, et al. The relationship between fermented food intake and mortality risk in the European Prospective Investigation into Cancer and Nutrition-Netherlands cohort. Br J Nutr. 2015;113(3):498–506. [DOI] [PubMed] [Google Scholar]
- 26. Wang C, Yatsuya H, Tamakoshi K, et al. Milk drinking and mortality: findings from the Japan Collaborative Cohort Study. J Epidemiol. 2015;25(1):66–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yang B, McCullough ML, Gapstur SM, et al. Calcium, vitamin D, dairy products, and mortality among colorectal cancer survivors: the Cancer Prevention Study-II Nutrition Cohort. J Clin Oncol. 2014;32(22):2335–2343. [DOI] [PubMed] [Google Scholar]
- 28. Dik VK, Murphy N, Siersema PD, et al. Prediagnostic intake of dairy products and dietary calcium and colorectal cancer survival—results from the EPIC cohort study. Cancer Epidemiol Biomarkers Prev. 2014;23(9):1813–1823. [DOI] [PubMed] [Google Scholar]
- 29. Song Y, Chavarro JE, Cao Y, et al. Whole milk intake is associated with prostate cancer-specific mortality among US male physicians. J Nutr. 2013;143(2):189–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. O'Sullivan TA, Hafekost K, Mitrou F, et al. Food sources of saturated fat and the association with mortality: a meta-analysis. Am J Public Health. 2013;103(9):e31–e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Soedamah-Muthu SS, Ding EL, Al-Delaimy WK, et al. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: dose-response meta-analysis of prospective cohort studies. Am J Clin Nutr. 2011;93(1):158–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pourshams A, Khademi H, Malekshah AF, et al. Cohort profile: the Golestan Cohort Study—a prospective study of oesophageal cancer in northern Iran. Int J Epidemiol. 2010;39(1):52–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Malekshah AF, Kimiagar M, Saadatian-Elahi M, et al. Validity and reliability of a new food frequency questionnaire compared to 24 h recalls and biochemical measurements: pilot phase of Golestan cohort study of esophageal cancer. Eur J Clin Nutr. 2006;60(8):971–977. [DOI] [PubMed] [Google Scholar]
- 34. Azar M, Sarkisian E. Food Composition Table of Iran. Tehran, Iran: National Nutrition and Food Science Research Institute of Shaheed Beheshti University; 1981. [Google Scholar]
- 35. Agricultural Research Service, US Department of Agriculture USDA National Nutrient Database for Standard Reference, Release 17. Washington, DC: US Department of Agriculture;2004. http://www.ars.usda.gov/Services/docs.htm?docid=8964. Accessed February 24, 2016. [Google Scholar]
- 36. Etemadi A, Abnet CC, Kamangar F, et al. Impact of body size and physical activity during adolescence and adult life on overall and cause-specific mortality in a large cohort study from Iran. Eur J Epidemiol. 2014;29(2):95–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Islami F, Kamangar F, Nasrollahzadeh D, et al. Socio-economic status and oesophageal cancer: results from a population-based case-control study in a high-risk area. Int J Epidemiol. 2009;38(4):978–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Khademi H, Etemadi A, Kamangar F, et al. Verbal autopsy: reliability and validity estimates for causes of death in the Golestan Cohort Study in Iran. PLoS One. 2010;5(6):e11183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Khademi H, Malekzadeh R, Pourshams A, et al. Opium use and mortality in Golestan Cohort Study: prospective cohort study of 50,000 adults in Iran. BMJ. 2012;344:e2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Afshin A, Micha R, Khatibzadeh S, et al. The impact of dietary habits and metabolic risk factors on cardiovascular and diabetes mortality in countries of the Middle East and North Africa in 2010: a comparative risk assessment analysis. BMJ Open. 2015;5(5):e006385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Murray CJ, Atkinson C, Bhalla K, et al. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Huo Yung Kai S, Bongard V, Simon C, et al. Low-fat and high-fat dairy products are differently related to blood lipids and cardiovascular risk score. Eur J Prev Cardiol. 2014;21(12):1557–1567. [DOI] [PubMed] [Google Scholar]
- 43. Drouin-Chartier JP, Gagnon J, Labonté MÈ, et al. Impact of milk consumption on cardiometabolic risk in postmenopausal women with abdominal obesity. Nutr J. 2015;14:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Conway V, Couture P, Gauthier S, et al. Effect of buttermilk consumption on blood pressure in moderately hypercholesterolemic men and women. Nutrition. 2014;30(1):116–119. [DOI] [PubMed] [Google Scholar]
- 45. Tremblay A, Gilbert JA. Milk products, insulin resistance syndrome and type 2 diabetes. J Am Coll Nutr. 2009;28(suppl 1):91S–102S. [DOI] [PubMed] [Google Scholar]
- 46. Parvez S, Malik KA, Ah Kang S, et al. Probiotics and their fermented food products are beneficial for health. J Appl Microbiol. 2006;100(6):1171–1185. [DOI] [PubMed] [Google Scholar]
- 47. Biong AS, Müller H, Seljeflot I, et al. A comparison of the effects of cheese and butter on serum lipids, haemostatic variables and homocysteine. Br J Nutr. 2004;92(5):791–797. [DOI] [PubMed] [Google Scholar]
- 48. Nakamura Y, Yamamoto N, Sakai K, et al. Antihypertensive effect of sour milk and peptides isolated from it that are inhibitors to angiotensin I-converting enzyme. J Dairy Sci. 1995;78(6):1253–1257. [DOI] [PubMed] [Google Scholar]
- 49. Chen M, Sun Q, Giovannucci E, et al. Dairy consumption and risk of type 2 diabetes: 3 cohorts of US adults and an updated meta-analysis. BMC Med. 2014;12:215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sluijs I, Forouhi NG, Beulens JW, et al. The amount and type of dairy product intake and incident type 2 diabetes: results from the EPIC-InterAct Study. Am J Clin Nutr. 2012;96(2):382–390. [DOI] [PubMed] [Google Scholar]
- 51. Hu D, Huang J, Wang Y, et al. Dairy foods and risk of stroke: a meta-analysis of prospective cohort studies. Nutr Metab Cardiovasc Dis. 2014;24(5):460–469. [DOI] [PubMed] [Google Scholar]
- 52. Wang H, Troy LM, Rogers GT, et al. Longitudinal association between dairy consumption and changes of body weight and waist circumference: the Framingham Heart Study. Int J Obes (Lond). 2014;38(2):299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mozaffarian D, Hao T, Rimm EB, et al. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Food and Agriculture Organization of the United Nations FAO Statistical Pocketbook 2015. World Food and Agriculture. Rome, Italy: Food and Agriculture Organization of the United Nations; 2015. http://www.fao.org/3/a-i4691e.pdf. Accessed February 24, 2016. [Google Scholar]
- 55. Food and Agriculture Organization of the United Nations FAOSTAT. Food balance sheets. (Data on Iran, 2004 and 2014). http://faostat.fao.org/site/368/DesktopDefault.aspx?PageID=368#ancor. Accessed February 24, 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.