Abstract
Understanding how the temperature-mortality association worldwide changes over time is crucial to addressing questions of human adaptation under climate change. Previous studies investigated the temporal changes in the association over a few discrete time frames or assumed a linear change. Also, most studies focused on attenuation of heat-related mortality and studied the United States or Europe. This research examined continuous temporal changes (potentially nonlinear) in mortality related to extreme temperature (both heat and cold) for 15 cities in Northeast Asia (1972–2009). We used a generalized linear model with splines to simultaneously capture 2 types of nonlinearity: nonlinear association between temperature and mortality and nonlinear change over time in the association. We combined city-specific results to generate country-specific results using Bayesian hierarchical modeling. Cold-related mortality remained roughly constant over decades and slightly increased in the late 2000s, with a larger increase for cardiorespiratory deaths than for deaths from other causes. Heat-related mortality rates have decreased continuously over time, with more substantial decrease in earlier decades, for older populations and for cardiorespiratory deaths. Our findings suggest that future assessment of health effects of climate change should account for the continuous changes in temperature-related health risk and variations by factors such as age, cause of death, and location.
Keywords: adaptation, climate change, heat and cold, temperature-mortality association; temporal change
Over the last decade, public concern has increased regarding temperature-related mortality worldwide, and numerous studies have found that extreme temperatures are related to increased mortality (1–5). More recently, as climate change is observed and projected, the focus has moved to the temporal changes in the temperature-mortality association (6–17). The degree to which populations change their health response to temperature is a crucial research question with respect to climate change. Some previous studies investigated the temporal change by dividing the study period into a few blocks of time (9–12), which limits the ability to examine a continuous pattern of change over time. Alternatively, other studies assumed linearity in the change over time (6–8), although the change could be nonlinear. In the context of climate change, investigating the potentially nonlinear change pattern in temperature-related mortality continuously is crucial because it allows for more accurate projections of the health effects of climate change.
Moreover, most previous literature addressing temporal change focused on the attenuation of the heat-related mortality (6, 9, 11–13). Fewer studies examined how populations’ response to cold weather has changed over time (10, 14–17). This may be partly because previous literature reported that cold-related mortality will be of less concern—that climate change would reduce excess winter death with global warming (18–20). However, in more recent studies, investigators have found that the association between cold and mortality has changed over time, and there will be little impact of climate change on cold-related mortality (21–25). In addition, the majority of previous studies were conducted in the United States (6, 8–10, 12) or Europe (13–17). Results in Western countries may not be applicable to Asian regions because of numerous factors (e.g., climate, economic status, housing condition, activity patterns, nutrition, and healthcare systems) that could vary the association between weather stressors and mortality.
The present study examines how weather-related mortality has varied over time. We estimated the time-varying mortality associated with extreme (both cold and hot) temperature for 15 cities in 3 high-income countries in Northeast Asia. To capture the time-varying change (potentially nonlinear), we used a generalized linear model with splines. This method allows for a nonlinear association between temperature and mortality and simultaneously a nonlinear change in this association over time. We estimated the time-varying association between extreme temperatures and mortality for each city and then combine these estimates to generate country-specific estimates using a Bayesian hierarchical approach. We examined how the cold- and heat-related mortality changed over time by age group (<65 years, 65–75 years, and >75 years) and cause of death (cardiovascular (CVD), respiratory, and other causes).
METHODS
Data
This study included data from 1994–2007 from 3 cities in Taiwan (Taipei, Taichung, and Kaohsiung), data from 1992–2010 from 6 cities in Korea (Seoul, Incheon, Daejeon, Daegu, Gwangju, and Busan), and data from 1972–2009 from 6 cities in Japan (Sapporo, Sendai, Tokyo, Nagoya, Osaka, and Kitakyushu). Daily mortality counts for each city were obtained from the National Death Registry of Taiwan, Statistics Korea, and the Ministry of Health, Labor, and Welfare of Japan. We defined all-cause mortality with the exclusion of accidental causes. We counted 2 cause-specific mortalities (CVD and respiratory) and noncardiorespiratory mortality. CVD mortality was defined by International Classification of Diseases, Eighth Revision (ICD-8), codes 390–458; International Classification of Diseases, Ninth Revision (ICD-9), codes 390–459; and International Classification of Diseases, Tenth Revision (ICD-10), codes I00–I99. Respiratory mortality was defined by ICD-8 codes 460–519, ICD-9 codes 460–519, and ICD-10 codes J00–J99. Mortality counts were also stratified into 3 age groups (<65 years, 65–75 years, and >75 years). Weather variables were obtained from Taiwan Environmental Protection Administration, Korea Meteorological Administration, and Japan Meteorological Agency. They include daily mean temperature (°C), daily mean pressure in hectopascals (hPa), and daily mean relative humidity (%). Hourly data were originally measured at various monitoring sites in each city, and 24-hour averages were calculated across all monitors for each city. Finally, a daily indicator variable for influenza epidemics was created, taking the value 1 if the moving average of the daily number of influenza deaths per 1,000 all-cause deaths over the previous week was ≥1 and 0 otherwise.
Statistical analysis
First, we examined the change over time in extreme temperature-related mortality sequentially by dividing the data of the whole study period into 5-year time frames with the starting year increased by 1. For each city in Japan, the first subperiod is 1972–1976, the second is 1973–1977, and so on, and the last is 2005–2009 (i.e., 34 serial subperiod data sets). Similarly, we obtained 15 and 10 serial subperiod data sets for each city in Korea and Taiwan, respectively. For each city and each 5-year subperiod, we estimated the cold- and heat-related mortality with the following generalized linear model (model 1) with splines as used in previous work (4):
| (1) |
where Yt is the death count on day t, is the expected death count on day t, β0 is an intercept, Tempt is a temperature metric on day t, Timet is a variable representing time on day t, Humt is the daily mean relative humidity on day t, Presst is the daily mean air pressure on day t, and ns( ) stands for natural cubic splines to model nonlinear associations with covariates. For the temperature metric, we used 7-day (for cold) and 2-day (for heat) moving averages of daily mean temperature, as in a previous study (4), in each of the separate models for cold- and heat-related mortality. Using results from model 1, we defined the cold-related mortality risk as the ratio of mortality (i.e., the relative risk) at the 1st and 10th percentiles of temperature and the heat-related mortality risk as the ratio of mortality at the 99th vs 90th temperature percentiles. The reference percentiles were obtained using the whole-period data specific to each city (Web Table 1, available at http://aje.oxfordjournals.org/) and then used to quantify the risk in all serial subperiods. As a sensitivity analysis, we also applied the reference percentiles specific to each subperiod and each city. Once we obtained serial sequences of city-specific cold- and heat-related risk estimates, we combined them and obtained country-specific estimates using a Bayesian hierarchical model.
Next, we investigated the time-varying cold- and heat-related mortality using the whole-period data simultaneously for each city by advancing model 1 as follows.
| (2) |
where the difference from model 1 is that temperature interacts with time. Model 2 (equation 2) allows for nonlinear associations between temperature and mortality and nonlinear interaction of temperature with time, thereby allowing for the association between temperature and mortality to nonlinearly change over time. The degrees of freedom value in the time term in ns(Temp) × ns(Time) was initially chosen as 3 for all 15 cities based on the results of the sequential subperiod analysis obtained from model 1. Further, the chosen degrees of freedom were justified by F tests for series of model comparisons. Fitting model 2 separately for cold- and heat- related mortality, we defined the cold-related mortality risk as the relative risk comparing the 1st and 10th percentiles of temperature and the heat-related mortality risk as the relative risk for the 99th versus 90th percentiles. Because of the interaction, the cold- and heat-related risks were obtained as functions of time (i.e., smooth curves over time), which we called time-varying cold- and heat-related risk. Once we obtained the time-varying cold- and heat-related mortality risk estimates for each city, we combined them to produce city-specific and country-specific estimates by applying a Bayesian hierarchical approach. In this second stage, we again examined whether the time-varying risks were supported against time-constant risks by checking whether the 95% posterior interval excluded 0 for any of the coefficients corresponding to the time-varying cold- and heat-related risk. More details for the second-stage modeling are found in Web Appendix 1.
Model 2 was fitted for all-cause mortality pooling all age groups, for cause-specific mortality pooling all age groups, and for all-cause mortality according to the 3 age groups. Sensitivity analysis was carried out to investigate the appropriate degrees of freedom in the time term in the interaction. All computations were performed using the statistical software R (R Foundation for Statistical Computing, Vienna, Austria). R code and example data are available in the Web Material for reproducing the results for South Korea.
RESULTS
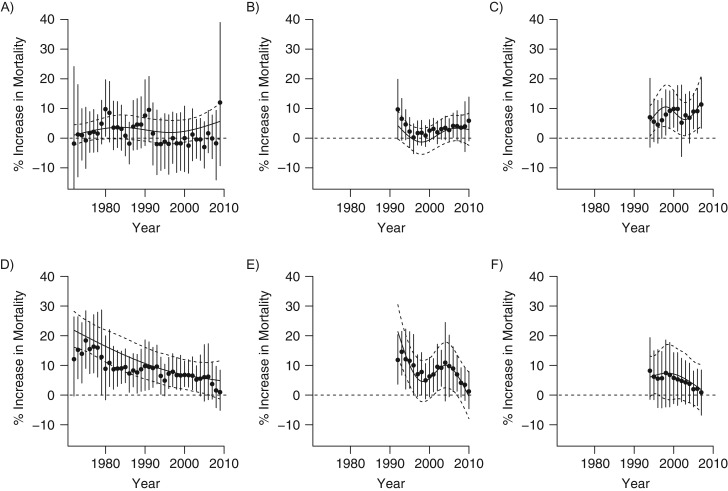
Figure 1 shows country-specific estimates for time-varying cold- and heat-related mortality risk. These results show the % change in mortality comparing the 1st and 10th percentiles of the moving 7-day average (lag 0–7) of temperature for the cold-related risk and the 99th and 90th percentiles of the moving 2-day average (lag 0–2) for the heat-related risk, and how these risk estimates change over time. In all 3 countries, cold-related risk remained roughly constant over the study period, although some decrease was observed for Korea in the mid-1990s, and slight increases were observed for Japan and Taiwan in the late 2000s. Decreases were observed in heat-related risk over the most of the study period in all 3 countries. In Japan, heat-related risk dramatically decreased in the 1970s and 1980s, and the decrease slowed down in the mid-1990s through 2000s. Korea showed a rapid decrease in heat-related risk in the 1990s and small fluctuations in the mid-2000s, followed by a strong decrease again in the late 2000s. Taiwan showed a smaller decrease in heat-related risk from the mid-1990s through 2000s. City-specific results are displayed in Web Figures 1–3; overall similar patterns are observed among cities in each country.
Figure 1.
Country-specific temporal changes in cold- and heat-related mortality risks (1972–2009 for Japan, 1992–2010 for Korea, and 1994–2007 for Taiwan). Cold-related risk for Japan (A), Korea (B), and Taiwan (C). Heat-related risk for Japan (D), Korea (E), and Taiwan (F). Circles represent the central estimates of risk with vertical lines as the 95% posterior intervals obtained from the time-constant models using subsets of data (5-year subsets with results presented at the corresponding midpoint year and 3- and 4-year subsets for the earliest and latest 2-year periods, due to data availability). The solid and dashed horizontal lines represent the central estimates of risk with 95% posterior intervals obtained from the nonlinear time-varying models using the whole data set.
Web Figure 4 shows country-specific estimates for time-varying cold- and heat-related mortality risk among different age groups. For cold-related risk, the changing pattern across time is similar among the 3 age groups in all 3 countries, although the risk estimates tended to be slightly higher for older populations. However, the changing pattern of heat-related risk over time substantially differs among the 3 age groups in all 3 countries. In Japan, heat-related risk was much larger for older populations early in the study period and converged to become similar among the 3 age groups in later years. In Korea and Taiwan, findings were similar in that, for older populations, heat-related risk was larger and the decrease in risk across time was larger.
Web Figure 5 shows country-specific estimates for time-varying cold- and heat-related mortality risk for different causes of death. The change in risk over time varies by cause of death for both cold- and heat-related risk in all 3 countries. The increase in cold-related risk in the late 2000s is largest for respiratory deaths and smallest for noncardiorespiratory deaths in Japan and Taiwan. The decrease in heat-related risk in 1970s and 1980s is much more dramatic for respiratory deaths than for CVD or noncardiorespiratory deaths in Japan. In Korea, the decrease in heat-related risk was largest for CVD death and larger for respiratory death than for noncardiorespiratory deaths. In Taiwan, the heat-related risk increased in the 1990s and decreased in the 2000s for CVD and respiratory deaths, while noncardiorespiratory risk decreased throughout the study period.
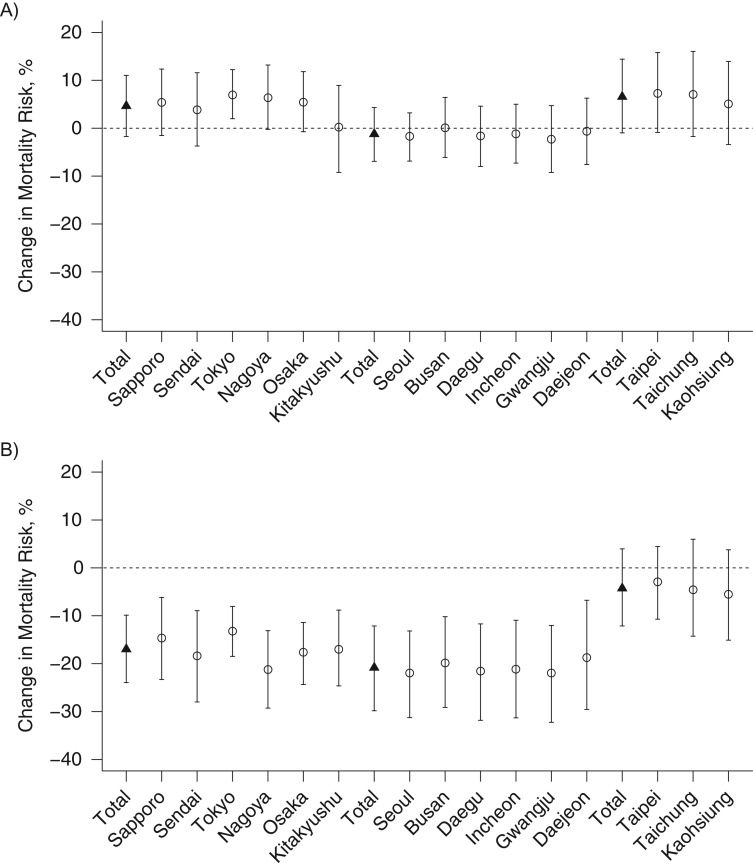
Figure 2 shows the changes in cold- and heat-related mortality risk (% increase in mortality) from the first to the last years of the study period for each city and for each country (i.e., 1972 vs. 2009 for Japan, 1992 vs. 2010 for Korea, and 1994 vs. 2007 for Taiwan). Cold-related risk increased between the first and last years of the study period in all cities in Japan and Taiwan except for Kitakyushu, although results were not statistically different for most cities. Larger increases were observed for cold-related risk in Taiwan, and changes in cold-related risk are negligible in cities of Korea. Meanwhile, heat-related risk decreased in all the cities analyzed in all 3 countries, with larger decreases in Japan and Korea than in Taiwan. Heat-related risks in the most recent year were statistically lower than in the first year of the study period for all the cities in Japan and Korea. Because the study period differs among countries, we additionally estimated changes in cold- and heat-related risk between 1994 and 2007, which is the largest time interval with data for all 3 countries (Web Figure 6). Results were generally similar, although attenuated in this shorter time frame.
Figure 2.
City-specific and country-specific changes in cold- and heat-related mortality risk, comparing risks at the first and last years of the study period in each country (1972–2009 for Japan, 1992–2010 for Korea, and 1994–2007 for Taiwan). A) Changes in cold-related mortality risk. B) Changes in heat-related mortality risk. Circles and triangles represent city-specific and country-specific central estimates of risk change with bars indicating 95% posterior intervals.
We conducted a sensitivity analysis to examine whether the nonlinear temporal change in cold/heat-related mortality was favored against linear change or no change. Web Figures 7–9 show time-varying cold- and heat-related mortality risk estimated with varying degrees of freedom for each city in Taiwan, Korea, and Japan. We observed that the fits seem to be improved with degrees of freedom up to 3 (i.e., with nonlinear interaction) but not as much for degrees of freedom greater than 3. This visual observation was also supported by quantitative evidence in model comparisons conducted at the first stage for each city. Web Table 2 reports the P values from the F tests. In modeling cold/heat-related mortality, the nonlinear change was favored against linear change in about half of the cities in all 3 countries. These results justify the specification of the nonlinear interaction between temperature and time in all cities at the first stage for pooling the results in the second stage. In addition, the 95% posterior interval–based testing procedure in the second stage also revealed that the nonlinear change was supported against no change in our study data (Web Table 3).
DISCUSSION
The present study found that the temperature-mortality association has changed over the last few decades in 15 major cities in 3 high-income countries in Northeast Asia. Cold-related mortality remained similar over most of the study periods and increased slightly in the late 2000s. Heat-related mortality has generally decreased over the study periods. The increasing trend in cold-related mortality differed for 3 causes of death, with the sharpest increase in risk for respiratory deaths and little change for noncardiorespiratory deaths. The pattern of decreasing heat-related mortality over time differed by cause of death and age; the largest decrease was for respiratory deaths and the oldest population. These results generally applied to all 3 countries with some variations.
Cold-related mortality did not vary over most of the study period and increased slightly in the late 2000s in Japan and Taiwan. This nondecreasing cold-related mortality was observed both with time-constant percentiles and with time-dependent percentiles used to quantify the cold-related risk (Web Figure 10). One possible explanation for the nondecreasing cold-related mortality may be physiological or behavioral change in vulnerable populations, perhaps in response to climate change. As shown in Web Figure 11, temperature generally increased across the study period in all cities. Earlier research shows that people in warmer climates are generally more sensitive to cold weather (1, 3, 4). Likewise, the general trend of warming weather may result in people becoming more vulnerable to cold temperatures, which could relate to our observed results of a lack of a decrease in the cold-related mortality over time. Some research reported that cold-related mortality may be of less concern in the future as the climate becomes warmer and cold weather becomes less frequent (18–20); however, our findings suggest that as climate warms, people's susceptibility to cold may increase, and cold-related mortality could still be of concern although there may be reduced frequency of cold weather. Because data are not available after 2007 in Taiwan and 2009 in Japan, additional research is needed to fully interpret the temporal trends in the cold-related mortality in these regions.
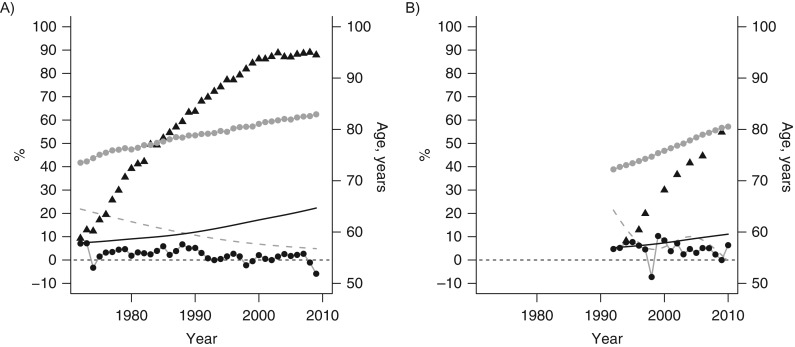
Our results indicated that heat-related mortality continuously declined over the past several decades in all 3 countries, with different rates of change over time and different patterns among countries. In Japan, the decline in heat-related mortality was more dramatic at earlier years and became slower at later periods, with a turning point in the mid-1990s. In Korea, heat-related mortality has generally declined, with some fluctuations in the mid-2000s. One plausible hypothesis is that this may relate to the country's economic growth pattern. Figure 3 shows that the gross national product growth rate (%) was positive in Japan in the 1970s and 1980s and negative since early 1990s, which is roughly when the heat-related mortality began to decline less rapidly. Similarly, except for the financial crisis in 1997, Korea achieved positive growth rates over most of the study period. Figure 3 also shows that the air-conditioning prevalence rate increases and the heat-related mortality risk decreases overtime in both countries. Although we find that these socioeconomic factors covary, the temporal trends in the temperature-mortality association are complex and could be driven by many other factors. A complex and quantitative analysis would be required in order to disentangle these intricate systems and identify what contributed to the observed temporal trends.
Figure 3.
Factors that may covary with the temporal trend in heat-related mortality risks in Japan (1972–2009) (A) and Korea (1992–2010) (B). Dashed line: estimated heat-related risk (% increase in mortality); triangle: air conditioning prevalence rate (%); black circle: Gross National Product growth rate (%); solid line: older population (% ≥65 years); and grey circle: life expectancy (years).
Within all 3 countries analyzed, the temporal trends in cold-related mortality are similar by age group, although the decreasing pattern in heat-related mortality was sharper in older populations. One possible explanation may be that the baseline health status of older people has improved in recent decades through the benefits of economic growth. Life expectancy has continually increased in recent decades in Japan and Korea (Figure 3). Our results imply that the contribution by older persons to heat-related mortality in the total population fell and become more similar to that of the general population. Some studies have reported that aging in a society may increase the heat-related mortality burden because older populations are more vulnerable to heat; however, our results do not support this hypothesis for this region. Differential adaptations to heat among age groups were also found in a previous US study (6).
Our findings have important implications for assessing the health impacts of climate change. First, predictions of future temperature-related mortality depend on various factors (26–28), among which the temperature-mortality association and potential temporal changes are critical. Most previous studies on climate and health used estimates from time-constant models, and our results suggest that the time-constant assumption may not be appropriate. Second, recent studies investigating the temporal change with linear change assumed may not have fully captured the temporal patterns. For instance, Gasparrini et al. (7) investigated a linear change in heat-related mortality in multiple cities from different parts of the world, including Korea and Japan. They did not identify a significant attenuation using a model with linear trend in Korea, while we found some significant evidence for a nonlinear temporal change. Third, our results suggest that changes in heat-related health responses over time can differ by age, cause of death, and region.
Several methodological issues should be pointed out regarding our study. First, we used a moving average of daily mean temperature over lags as a temperature metric. Distributed lag nonlinear models (3, 5, 7, 29) may alternatively be used, but the extension to incorporate a nonlinear interaction with time would increase the complexity in estimation. Second, we quantified the cold- and heat-related mortality risk using the 1st versus 10th and 90th versus 99th percentiles of temperature metric, as in many other studies (1, 3, 4). This may be limited to summarizing the total risk over the whole range of temperature. There exists no universal metric to summarize the cold- and heat-related risk in nonlinear modeling. Various studies use different measures; the overall results are generally consistent among different risk quantifications (3). Third, it should be cautioned that nonlinear models may characterize random fluctuations as true changes because of their flexibility. For example, the time-varying heat-related mortality risk in Taiwan and Korea was estimated as nonlinear curves with fluctuations. Although supported by statistical tests, these curves are hard to interpret and may include random noise which may be misidentified as actual changes. As nonlinear modeling becomes more popular in this field, further research is merited into statistical methods for distinguishing true nonlinearity from random fluctuation.
Finally, we acknowledge several limitations in our study. One is that study periods differ among countries because of data availability. Second, limited data are available for potential risk factors that could explain the temporal change in temperature-related mortality. Using country-specific data for some socioeconomic variables (as presented in Figure 3), we observed that these variables tend to covary with the temporal trend over time in heat-related mortality. However, future studies could conduct more in-depth analysis regarding the numerous complex factors that could contribute to temporal change in heat- or cold-related mortality and how they differ by population and location. Without knowing the driving factors for the temporal change, future prediction for the health effects of climate change will still be limited. In addition, the categorization of causes of mortality and age groups is broad, and future studies could apply more refined categories of population susceptible to extreme temperature.
In conclusion, we examined nonlinearly time-varying mortality associated with extreme temperature (both cold and hot) for 15 cities in 3 high-income countries in Northeast Asia. We proposed a flexible analytical framework to capture the nonlinear time-varying trend smoothly. The cold-related mortality remained relatively constant over the decades and increased slightly in late 2000s, particularly for cardiorespiratory deaths. Heat-related mortality has continuously and nonlinearly decreased over the last decades, with more dramatic decreases estimated at earlier years, for older populations, and for cardiorespiratory deaths. These findings have important implications for the assessment of health consequences of climate change and indicate that such assessment should account for the nonlinear change over time in temperature-mortality association, the nondecreasing cold-related mortality, and variations in the temporal change among cause of deaths, age, and region.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Mathematical Sciences, Korea Advanced Institute of Science and Technology, Daejeon, South Korea (Yeonseung Chung, Heesang Noh); Faculty of Health and Sport Sciences, University of Tsukuba, Tsukuba, Japan (Yasushi Honda); Department of Pediatric Infectious Diseases, Institute of Tropical Medicine, Nagasaki University, Nagasaki, Japan (Masahiro Hashizume); School of Forestry and Environmental Studies, Yale University, New Haven, Connecticut (Michelle L. Bell); National Institute of Environmental Health Sciences, National Health Research Institutes, Zhunan, Taiwan (Yue-Liang Leon Guo); Institute of Health and Environment, Seoul National University, Seoul, South Korea (Ho Kim); and Department of Public Health Science, Graduate School of Public Health, Seoul National University, Seoul, South Korea (Ho Kim).
This study was supported by the Korean Ministry of Environment as research on impact assessment of climate change to support policy for the Korean peninsula (grant 900-20160057), the Global Research Laboratory Program (grant K21004000001-10A0500-00710) and the Senior Investigator Research Fund (grant 2016R1A2B1007082) supported by the National Research Foundation of Korea, Korean Ministry of Science, ICT, and Future Planning, the Environmental Research and Technology Development Fund (S-10 and S-14) of the Japanese Ministry of Environment, and the National Health Research Institutes, Taiwan (grant NHRI-EM-106-SP03).
Conflict of interest: none declared.
REFERENCES
- 1. Anderson BG, Bell ML. Weather-related mortality: how heat, cold, and heat waves affect mortality in the United States. Epidemiology. 2009;20(2):205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Basu R. High ambient temperature and mortality: a review of epidemiological studies from 2001 to 2008. Environ Health. 2009;8:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Guo Y, Gasparrini A, Armstrong B, et al. Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology. 2014;25(6):781–789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chung Y, Lim YH, Honda Y, et al. Mortality related to extreme temperature for 15 cities in northeast Asia. Epidemiology. 2015;26(2):255–262. [DOI] [PubMed] [Google Scholar]
- 5. Gasparrini A, Guo Y, Hashizume M, et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet. 2015;386(9991):369–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bobb JF, Peng RD, Bell ML, et al. Heat-related mortality and adaptation to heat in the United States. Environ Health Perspect. 2014;122(8):811–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gasparrini A, Guo Y, Hashizume M, et al. Temporal variation in heat-mortality associations: a multi-country study. Environ Health Perspect. 2015;123(11):1200–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Guo Y, Barnett AG, Tong S. High temperatures-related elderly mortality varied greatly from year to year: important information for heat-warning systems. Sci Rep. 2012;2:830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sheridan SC, Kalkstein AJ, Kalkstein LS. Trends in heat-related mortality in the United States, 1975–2004. Nat Hazards. 2009;50(1):145–160. [Google Scholar]
- 10. Barnett AG. Temperature and cardiovascular deaths in the US elderly: changes over time. Epidemiology. 2007;18(3):369–372. [DOI] [PubMed] [Google Scholar]
- 11. Ha J, Kim H. Changes in the association between summer temperature and mortality in Seoul, South Korea. Int J Biometeorol. 2013;57(4):535–544. [DOI] [PubMed] [Google Scholar]
- 12. Davis RE, Knappenberger PC, Michaels PJ, et al. Changing heat-related mortality in the United States. Environ Health Perspect. 2003;111(14):1712–1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Donaldson GC, Keatinge WR, Näyhä S. Changes in summer temperature and heat-related mortality since 1971 in North Carolina, South Finland, and Southeast England. Environ Res. 2003;91(1):1–7. [DOI] [PubMed] [Google Scholar]
- 14. Åström DO, Forsberg B, Edvinsson S, et al. Acute fatal effects of short-lasting extreme temperatures in Stockholm, Sweden: evidence across a century of change. Epidemiology. 2013;24(6):820–829. [DOI] [PubMed] [Google Scholar]
- 15. Christidis N, Donaldson GC, Stott PA. Causes for the recent changes in cold- and heat-related mortality in England and Wales. Clim Change. 2010;102(3-4):539–553. [Google Scholar]
- 16. Ekamper P, Duin G. 150 Years of temperature-related excess mortality in the Netherlands. Demogr Res. 2009;21(14):385–426. [Google Scholar]
- 17. Carson C, Hajat S, Armstrong B, et al. Declining vulnerability to temperature-related mortality in London over the 20th century. Am J Epidemiol. 2006;164(1):77–84. [DOI] [PubMed] [Google Scholar]
- 18. Kalkstein LS, Breene JS. An evaluation of climate/mortality relationships in large US cities and the possible impacts of a climate change. Environ Health Perspect. 1997;105(1):84–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kovats RS, Haines A, Stanwell-Smith R, et al. Climate change and human health in Europe. BMJ. 1999;318(7199):1682–1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Langford IH, Bentham G. The potential effects of climate change on winter mortality in England and Wales. Int J Biometeorol. 1995;38(3):141–147. [DOI] [PubMed] [Google Scholar]
- 21. Davis RE, Knappenberger PC, Michaels PJ, et al. Seasonality of climate-human mortality relationships in US cities and impacts of climate change. Clim Res. 2004;26:61–76. [Google Scholar]
- 22. Martin SL, Cakmak S, Hebbern CA, et al. Climate change and future temperature-related mortality in 15 Canadian cities. Int J Biometerorol. 2012;56(4):605–619. [DOI] [PubMed] [Google Scholar]
- 23. Morabito M, Crisci A, Moriondo M, et al. Air temperature-related human health outcomes: current impact and estimations of future risks in Central Italy. Sci Total Environ. 2012;441:28–40. [DOI] [PubMed] [Google Scholar]
- 24. Staddon PL, Montgomery HE, Depledge MH. Climate warming will not decrease winter mortality. Nat Clim Chang. 2014;4(3):190–194. [Google Scholar]
- 25. Huang C, Barnett A. Human impacts: winter weather and health. Nat Clim Chang. 2014;4(3):173–174. [Google Scholar]
- 26. Huang C, Barnett AG, Wang X, et al. Projecting future heat-related mortality under climate change scenarios: a systematic review. Environ Health Perspect. 2011;119(12):1681–1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Peng RD, Bobb JF, Tebaldi C, et al. Toward a quantitative estimate of future heat wave mortality under global climate change. Environ Health Perspect. 2011;119(5):701–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Linares C, Mirón IJ, Montero JC, et al. The time trend temperature-mortality as a factor of uncertainty analysis of impacts of future heat waves. Environ Health Perspect. 2014;122(5):A118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gasparrini A. Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw. 2011;43(8):1–20. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.