Abstract
In a 1989 paper, Marchbanks et al. (Am J Epidemiol. 1989;130(2):259–267) noted inconsistent definitions of infertility across research and clinical practice and examined differences in prevalence estimates across definitions. Since their study, there have been substantial changes in society, technology, and clinical practice related to female reproductive health. In response, we revisited the original paper using data from a recent study among reproductive-aged women. Internal comparisons across various definitions of infertility were made by assessing how many and which women were classified as infertile, their age at infertility, and the probability of spontaneous pregnancy after infertility. Results were also compared with Marchbanks et al. Black women were more likely to be classified as infertile than white women based on the definition “12 months of unprotected intercourse” (40.1% vs. 33.7%) but less likely by “12 months of attempting pregnancy” (14.3% vs. 21.8%) and “visiting a doctor for help getting pregnant” (8.4% vs. 19.7%). After unprotected intercourse for 12 months, 36.1% of women who were attempting pregnancy spontaneously conceived by 6 months compared with 13.5% of women who were not attempting pregnancy. While our results for most infertility definitions were similar to those of Marchbanks et al., prevalence estimates continued to differ across demographic groups by definition.
Keywords: attempting pregnancy, demography, diagnosis, infertility, reproduction, unprotected intercourse, women’s health
In their 1989 paper “Research on Infertility: Definition Makes a Difference,” Marchbanks et al. (1) noted that the lack of a standard definition for infertility has limited the study of this condition. Infertility is not only a quality-of-life issue but also a disease of the reproductive system (2–4) that may be a risk factor for other diseases over the life course, such as cardiovascular disease, cancer, and metabolic dysfunction (5–7). The authors compared the way different definitions of infertility affected the estimated prevalence of infertility overall and within demographic subgroups (1). Over 25 years later, multiple definitions of infertility are still being used. Although different definitions may be appropriate for different study goals, this variability likely contributes to the wide range of prevalence estimates reported for lifetime infertility (1.8%–47.4%) (8).
Since the publication of the original paper, there have been many changes in society, technology, and clinical practice related to female reproductive health. First, women are delaying childbirth. The average age at first birth increased from 21.4 years of age in 1970 (9) to 26.3 in 2014 (10), while the percentage of women giving birth to their first child at age 35 years or older has increased from 1% to 9%. Second, there have been dramatic developments in medical technology to assist women in achieving pregnancy. These advancements have led to greater success and availability of fertility treatment (11, 12). Further, some insurance policies now cover related services (13). Thus, more women are using infertility treatment such as assisted reproductive technology (ART) (e.g., in vitro fertilization) than ever before (14). Further, with the rise in age at first birth, women increasingly visit a doctor for fertility counseling and testing before trying to get pregnant (15). Finally, in 2013, the American Society for Reproductive Medicine revised their definition of infertility to be the failure to achieve a successful pregnancy (ultrasound evidence of pregnancy in the first trimester) after having appropriately timed unprotected intercourse over a period lasting 12 months or longer, for women of ages 20–34 years, or 6 months or longer for women aged 35 years or older (16). When the study by Marchbanks et al. (1) was published, they defined infertility based on 2 years without a pregnancy.
Changes in society, technology, and clinical practice provide the motivation for revisiting the findings from the original paper. Similar to Marchbanks et al., our objective was to compare various metrics of infertility. Specifically, we examined how different definitions changed estimates of: 1) the prevalence of lifetime infertility, overall and within sociodemographic subgroups; 2) the age at infertility; and 3) the cumulative incidence of spontaneous pregnancy after infertility.
METHODS
Study population
The Furthering Understanding of Cancer, Health, and Survivorship in Adult Women Study (FUCHSIA Women’s Study) is a population-based study of fertility outcomes among female cancer survivors and their cancer-free counterparts in Georgia. Cancer survivors were recruited from the Georgia Cancer Registry, a statewide population-based registry of all reportable cancers in Georgia. This analysis was restricted to the cancer-free women (i.e., the comparison group), who were recruited between 2012 and 2013 to represent the general population in Georgia. These women were identified using a list purchased from InfoUSA (Papillion, NE). Cancer-free women were frequency-matched to cancer survivors according to 5-year age groups and Georgia region of residence. This design is similar to the Marchbanks et al. study, which used the control group of the Cancer and Steroid Hormone Study, a population-based study of female reproductive cancers, for their study population.
For this study, women were eligible to participate if they were 22–45 years of age at recruitment, had a working telephone, and spoke English. They were invited to participate in a study of women’s health to avoid differentially attracting women with fertility problems. Informed consent and interviews were completed by telephone. The interview, described previously (17), contained detailed questions on reproductive and medical history, desire for children, demographic information, lifestyle choices, and use of contraceptives and medical services. The Emory University and Georgia Department of Public Health institutional review boards approved this study.
We derived 11 definitions of infertility, which were based on answers to interview questions (Table 1). Most definitions were based on the following series of questions: “Has there ever been a period of time during which you had regular (≥3 times per month) unprotected sex with a male partner for 6 months or longer but did not get pregnant? If so, for how long? Were you actively trying to get pregnant at this time?” Women were able to report multiple periods of time during which they had unprotected sex or were attempting pregnancy. Women were also asked whether they visited a doctor for help getting pregnant and, if so, whether they received an infertility diagnosis (as well as whether this diagnosis was due to female-related factors).
Table 1.
Eleven Possible Definitions of Infertility From the Furthering Understanding of Cancer, Health, and Survivorship in Adult Women Study, 2012–2015
| Infertility Definition | Explanation |
|---|---|
| Unprotected intercourse for 6 months | Did not get pregnant after 6 months of regulara unprotected intercourse |
| Attempting pregnancy for 6 months | Did not get pregnant after 6 months of regular unprotected intercourse while actively trying to become pregnant |
| Unprotected intercourse for 12 months | Did not get pregnant after 12 months of regular unprotected intercourse |
| Attempting pregnancy for 12 months | Did not get pregnant after 12 months of regular unprotected intercourse while actively trying to become pregnant |
| Unprotected intercourse for 24 months | Did not get pregnant after 24 months of regular unprotected intercourse |
| Attempting pregnancy for 24 months | Did not get pregnant after 24 months of regular unprotected intercourse while actively trying to become pregnant |
| Unprotected intercourse using 2013 ASRM age cutpoints | Did not get pregnant after 12 months of regular unprotected intercourse for those <35 years old or after 6 months for those ≥35 years old |
| Attempting pregnancy according to 2013 ASRM definition | Did not get pregnant after 12 months of regular unprotected intercourse for those <35 years old or after 6 months for those ≥35 years old while actively trying to become pregnant |
| Visited a doctor for help getting pregnant | Visited a doctor or other health professional for help becoming pregnant |
| Physician diagnosis of infertility at fertility care visitb | At doctor visit, was told there was a problem with her or her partner’s fertility |
| Physician diagnosis of infertility at fertility care visit due to female-related factorsb,c | At doctor visit, was told there was a problem with her fertility |
Abbreviation: ASRM, American Society for Reproductive Medicine.
a Regular intercourse defined as ≥3 times per month.
b Measured only among women who visited a doctor for help getting pregnant.
c Reason given by doctor for cause of infertility was a female-related factor (e.g., poor ovulation, low ovarian reserve, fibroids, blocked tubes, endometriosis, cervical problem, or menopause).
Statistical analysis
We estimated the lifetime prevalence of infertility for each definition among women who were at risk of becoming pregnant. Women who specified that they had never had sex with a man were excluded. Because cancer-free study participants were frequency-matched to the cancer survivors, and cancer incidence increases with age, prevalence estimates were standardized to the age distribution of women aged 22–45 years from 2014 US Census data to improve generalizability (18, 19).
We estimated the prevalence of lifetime infertility (censored at age at interview) based on different definitions of infertility within demographic subgroups of women. Characteristics included age, race/ethnicity, education, household income, and residential location based on the 2013 National Center for Health Statistics Urban-Rural Classification Scheme (20). We also examined differences in the age when first classified as infertile by definition.
We constructed Kaplan-Meier curves to compare time to pregnancy by pregnancy intention (attempting pregnancy vs. not) following 3 different-duration periods of unprotected intercourse. Time at risk began when women first reported meeting the criteria for each infertility definition and ended when they reported getting pregnant or were censored, either at the time of study interview or when they were no longer at risk of becoming pregnant (e.g., surgical menopause or hormonal contraceptive initiation) or no longer at risk of spontaneous conception (e.g., became pregnant using ART or another infertility treatment). We also constructed curves stratified by primary versus secondary infertility. Primary infertility includes nulliparous women who experience infertility and secondary infertility is limited to women who had had at least 1 child at the time of infertility (21).
We then compared our results to those of Marchbanks et al. Because the original study population included older women (aged 46–54 years) than those in our study, we restricted the age range of their study population to be comparable to ours. Then we calculated crude prevalences of infertility for their study based on the restricted population. Finally, we standardized our results to the age, education, and race distributions of their study population (see Table 2 in Marchbanks et al. (1)). We standardized our results to each distribution separately because the joint distribution of the covariates was not available.
RESULTS
Among the 1,073 cancer-free women who completed the interview, 33 women (3.1%) who reported never having sex with a man and 26 women (2.4%) who were missing information on whether they ever experienced a period of infertility were excluded. The final study population was 1,014.
The estimated prevalence of infertility varied widely across definitions, with the lowest being doctor diagnosis of female infertility (6.3%) and the highest being unprotected intercourse for at least 6 months (42.6%) (Table 2). The prevalence of infertility was 40%–50% lower for definitions of infertility based on attempting pregnancy in a given time period versus definitions based on any unprotected intercourse for each respective timeframe. Approximately one-fifth of the women were infertile using the 2013 American Society for Reproductive Medicine definition, and over a third (35.9%) were infertile when pregnancy intention was ignored and all unprotected intercourse was considered using the 2013 American Society for Reproductive Medicine age and time cutpoints. Age-adjustment resulted in similar prevalence estimates across infertility definitions based on unprotected intercourse. However, the age-adjusted prevalence of infertility based on attempting pregnancy decreased compared with the crude estimates. Similarly, the prevalence of “visiting a doctor for help getting pregnant” and “receiving an infertility diagnosis” decreased after age-adjustment.
Table 2.
Crude and Age-Adjusted Prevalence of Lifetime (Prior or Current) Infertility by 11 Different Definitions of Infertility (n = 1,014), Furthering Understanding of Cancer, Health, and Survivorship in Adult Women Study, 2012–2015
| Infertility Definition | Crude Prevalence, %a | Age-Adjusted Prevalence, %b |
|---|---|---|
| Unprotected intercourse for 6 months | 42.6 | 43.4 |
| Attempting pregnancy for 6 months | 25.5 | 19.1 |
| Unprotected intercourse for 12 months | 35.3 | 35.3 |
| Attempting pregnancy for 12 months | 19.7 | 14.9 |
| Unprotected intercourse for 24 months | 23.5 | 23.8 |
| Attempting pregnancy for 24 months | 11.2 | 8.9 |
| Unprotected intercourse using 2013 ASRM age cutpointsc | 35.9 | 35.6 |
| Attempting pregnancy according to 2013 ASRM definitionc | 20.5 | 15.3 |
| Visited a doctor for help getting pregnant | 16.6 | 11.8 |
| Physician diagnosis of infertilityd | 9.7 | 7.0 |
| Physician diagnosis of infertility due to female-related factorsd–f | 6.3 | 3.8 |
Abbreviation: ASRM, American Society for Reproductive Medicine.
a Percentage of women ever meeting given definition of infertility.
b Percentage of women ever meeting given definition of infertility, age-adjusted to the US population using the 2014 US Census estimates for women aged 22–45 years.
c Did not get pregnant after 12 months of appropriately timed unprotected intercourse (for those <35 years of age) or after 6 months (for those ≥35 years old).
d Measured only among women who visited a doctor for help getting pregnant.
e Reason given by doctor for cause of infertility was a female-related factor (poor ovulation, low ovarian reserve, fibroids, blocked tubes, endometriosis, cervical problem, or menopause).
f Denominators exclude 8 people missing this outcome.
Demographic characteristics of our study population are listed in Table 3. The estimated prevalences of infertility were similar across age groups for definitions based on unprotected intercourse but were lower for women aged 22–29 years compared with older women for definitions based on attempting pregnancy (Table 4). Young women were also less likely to be categorized as infertile as defined by “visiting a doctor for help getting pregnant” or “receiving an infertility diagnosis” (Table 3). The estimated prevalences of infertility for black women were greater than the estimates for white women for 12 and 24 months of unprotected intercourse but were lower for definitions based on attempting pregnancy (Table 4). Black women were also less likely to be classified as infertile based on visiting a doctor for help getting pregnant. Women with household incomes of less than $50,000 had a lower estimated prevalence of infertility than wealthier women based on definitions restricted to women attempting pregnancy or based on visiting a doctor for help getting pregnant (Tables 3 and 4). Similarly, women with less than a college degree were less likely than more educated women to be classified as infertile by visiting a doctor for help getting pregnant. However, more-educated women were less likely to be classified as infertile by 6, 12, and 24 months of attempting pregnancy (as well as by all unprotected intercourse) compared with less-educated women. Finally, women living in large central metropolitan areas were the least likely to be classified as infertile for definitions based on unprotected intercourse and attempting pregnancy compared with women who lived in less urban areas.
Table 3.
Demographic Characteristics of the Study Population, Stratified by Definitions of Infertility Related to Visiting a Doctor and Clinical Diagnoses, Furthering Understanding of Cancer, Health, and Survivorship in Adult Women Study, 2012–2015
| Characteristic | Total Population (n = 1,014)a | Visited a Doctor (n = 168) | Doctor Diagnosis of Infertilityb (n = 98) | Doctor Diagnosis of Female Infertilityb (n = 63) | ||||
|---|---|---|---|---|---|---|---|---|
| No. | %c | No. | %c | No. | %c | No. | %c | |
| Age at interview, years | ||||||||
| 22–29 | 60 | 5.9 | 2 | 3.3 | 1 | 1.7 | 0 | 0.0 |
| 30–39 | 546 | 53.9 | 89 | 16.3 | 50 | 9.2 | 31 | 5.7 |
| 40–45 | 408 | 40.2 | 77 | 18.9 | 47 | 11.5 | 32 | 7.8 |
| Race/ethnicity | ||||||||
| White | 679 | 67.4 | 134 | 19.7 | 81 | 11.9 | 53 | 7.8 |
| Black | 287 | 28.5 | 24 | 8.4 | 13 | 4.5 | 8 | 2.8 |
| Other | 42 | 4.2 | 9 | 21.4 | 4 | 9.5 | 2 | 4.8 |
| Missing | 6 | 1 | 0 | 0 | ||||
| Education | ||||||||
| Up to high school graduation | 45 | 4.4 | 5 | 11.1 | 3 | 6.7 | 3 | 6.7 |
| Some college | 246 | 24.3 | 32 | 13.0 | 21 | 8.5 | 15 | 6.1 |
| College | 371 | 36.6 | 60 | 16.2 | 32 | 8.6 | 22 | 5.9 |
| Graduate school or beyond | 352 | 34.7 | 71 | 20.2 | 42 | 11.9 | 23 | 6.5 |
| Annual income, $ | ||||||||
| <50,000 | 268 | 26.9 | 22 | 8.2 | 14 | 5.2 | 10 | 3.7 |
| 50,000–100,000 | 388 | 38.9 | 62 | 16.0 | 38 | 9.8 | 26 | 6.7 |
| >100,000 | 342 | 34.3 | 80 | 23.4 | 45 | 13.2 | 26 | 7.6 |
| Missing | 16 | 4 | 0 | 0 | ||||
| Residence | ||||||||
| Nonmetro | 106 | 10.5 | 15 | 14.2 | 10 | 9.4 | 10 | 9.4 |
| Small metro | 164 | 16.2 | 24 | 14.6 | 16 | 9.8 | 8 | 4.9 |
| Large fringe metro | 617 | 60.9 | 110 | 17.8 | 62 | 10.0 | 40 | 6.5 |
| Large central metro | 127 | 12.5 | 19 | 15.0 | 10 | 7.9 | 5 | 3.9 |
a Included women without a history of cancer, who had reported sexual intercourse with a male partner and were not missing information on amount of time having unprotected intercourse for at least 6 months.
b Measured only among women who visited a doctor for help getting pregnant.
c Percentage calculated as the proportion of women in each sociodemographic subgroup that met each particular definition.
Table 4.
Demographic Characteristics of the Study Population, Stratified by Definitions of Infertility Related to Months of Unprotected Intercourse and Attempting Pregnancy, Furthering Understanding of Cancer, Health, and Survivorship in Adult Women Study, 2012–2015
| Characteristic | 6 Months of Unprotected Intercourse (n = 432) | 6 Months of Attempting Pregnancy (n = 259) | 12 Months of Unprotected Intercourse (n = 358) | 12 Months of Attempting Pregnancy (n = 200) | 24 Months of Unprotected Intercourse (n = 238) | 24 Months of Attempting Pregnancy (n = 114) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | %a | No. | %a | No. | %a | No. | %a | No. | %a | No. | %a | |
| Age at interview, years | ||||||||||||
| 22–29 | 27 | 45.0 | 6 | 10.0 | 23 | 38.3 | 5 | 8.3 | 17 | 28.3 | 4 | 6.7 |
| 30–39 | 230 | 42.1 | 140 | 25.6 | 182 | 33.3 | 100 | 18.3 | 118 | 21.6 | 52 | 9.5 |
| 40–45 | 175 | 42.9 | 113 | 27.7 | 153 | 37.5 | 95 | 23.3 | 103 | 25.2 | 58 | 14.2 |
| Race/ethnicity | ||||||||||||
| White | 287 | 42.3 | 195 | 28.7 | 229 | 33.7 | 148 | 21.8 | 145 | 21.4 | 83 | 12.2 |
| Black | 126 | 43.9 | 49 | 17.1 | 115 | 40.1 | 41 | 14.3 | 81 | 28.2 | 23 | 8.0 |
| Other | 16 | 38.1 | 12 | 28.6 | 11 | 26.2 | 8 | 19.0 | 9 | 21.4 | 6 | 14.3 |
| Missing | 3 | 3 | 3 | 3 | 3 | 2 | ||||||
| Education | ||||||||||||
| Up to high school graduation | 27 | 60.0 | 13 | 28.9 | 23 | 51.1 | 11 | 24.4 | 18 | 40.0 | 7 | 15.6 |
| Some college | 121 | 49.2 | 60 | 24.4 | 109 | 44.3 | 49 | 19.9 | 76 | 30.9 | 31 | 12.6 |
| College | 150 | 40.4 | 95 | 25.6 | 122 | 32.9 | 75 | 20.2 | 76 | 20.5 | 43 | 11.6 |
| Graduate school or beyond | 134 | 38.1 | 91 | 25.9 | 104 | 29.5 | 65 | 18.5 | 68 | 19.3 | 33 | 9.4 |
| Annual income, $ | ||||||||||||
| <50,000 | 126 | 47.0 | 53 | 19.8 | 107 | 39.9 | 42 | 15.7 | 80 | 29.9 | 29 | 10.8 |
| 50,000–100,000 | 171 | 44.1 | 105 | 27.1 | 138 | 35.6 | 77 | 19.8 | 88 | 22.7 | 41 | 10.6 |
| >100,000 | 126 | 36.8 | 96 | 28.1 | 105 | 30.7 | 77 | 22.5 | 64 | 18.7 | 41 | 12.0 |
| Missing | 9 | 5 | 8 | 4 | 6 | 3 | ||||||
| Residence | ||||||||||||
| Nonmetro | 56 | 52.8 | 36 | 34.0 | 47 | 44.3 | 28 | 26.4 | 37 | 34.9 | 21 | 19.8 |
| Small metro | 72 | 43.9 | 41 | 25.0 | 61 | 37.2 | 32 | 19.5 | 43 | 26.2 | 20 | 12.2 |
| Large fringe metro | 266 | 43.1 | 156 | 25.3 | 222 | 36.0 | 121 | 19.6 | 140 | 22.7 | 65 | 10.5 |
| Large central metro | 38 | 29.9 | 26 | 20.5 | 28 | 22.0 | 19 | 15.0 | 18 | 14.2 | 8 | 6.3 |
a Percentages calculated as the proportion of women in each sociodemographic subgroup that met each particular definition. Denominators shown in Table 3.
Among women classified as infertile, a higher percentage first experienced infertility during the ages of 18–29 years than during ages 30–45 years for most definitions (Web Table 1, available at https://academic.oup.com/aje). However, the percentage reporting infertility at ages 18–29 years was smaller based on attempting pregnancy compared with unprotected intercourse (e.g., 24 months: 81.1% for unprotected intercourse vs. 71.9% for attempting pregnancy). Women were the least likely to first experience infertility at ages of 18–29 years based on visited a doctor for help getting pregnant.
We also calculated the percentage of women aged 30 years or older at interview who reported infertility during the ages of 18–29 years and the percentage of women aged 40 years or older who experienced infertility during the ages of 30–39 (Web Table 2). Women were more likely to be classified as infertile during ages 18–29 years compared with ages 30–39 years based on the unprotected intercourse definitions, whereas the age groups had more similar frequencies based on attempting pregnancy.
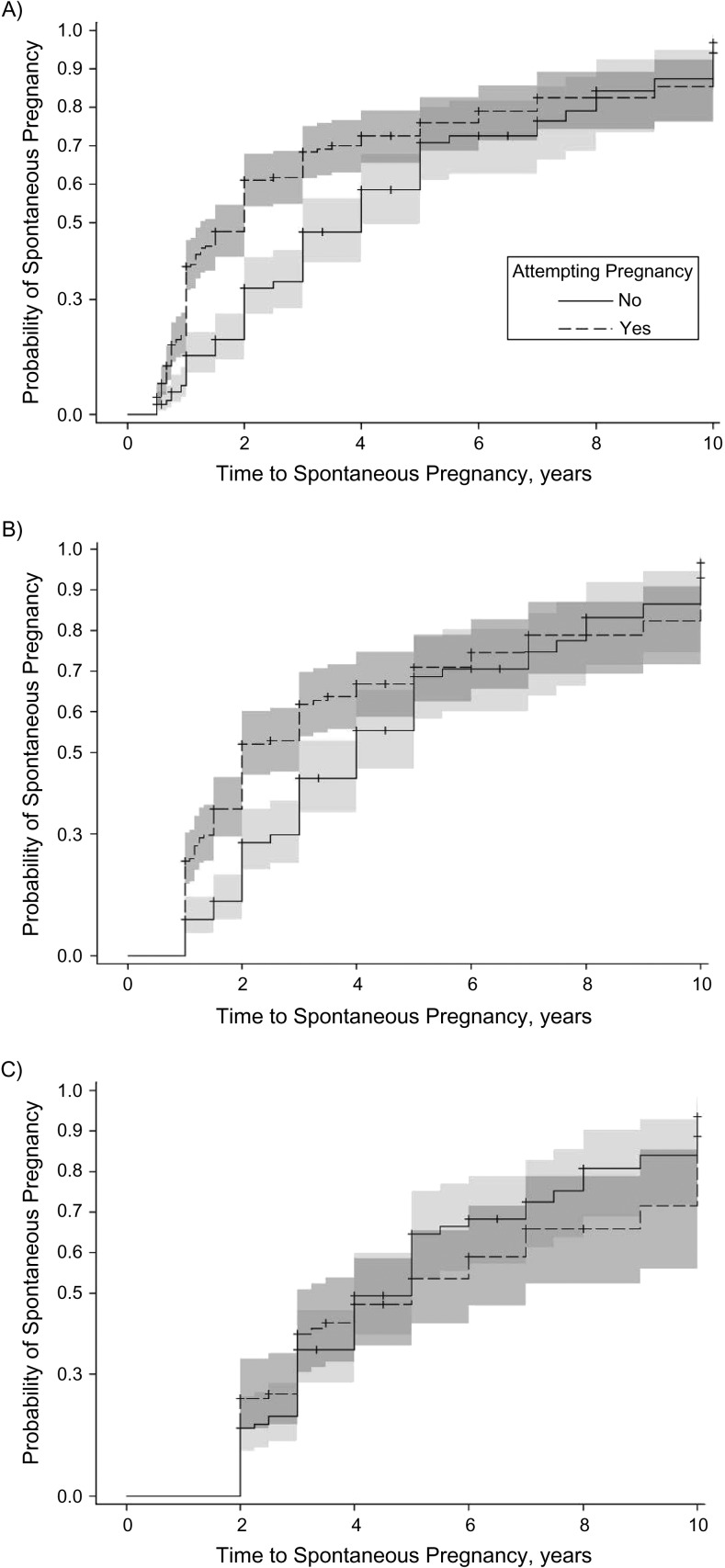
Although most women achieved pregnancy after an infertile period, the probability of pregnancy after infertility varied across definitions (Figure 1). Women attempting pregnancy were more likely to become pregnant than those who were not attempting pregnancy in the first 5 years after meeting infertility definitions based on 6 or 12 months of unprotected intercourse (P < 0.0005; Wilcoxon and log-rank tests; Figure 1A and 1B). However, this pattern was not observed using the definition of 24 months of unprotected intercourse (Figure 1C). Across unprotected-intercourse definitions, women experiencing secondary infertility were more likely to become pregnant compared with those experiencing primary infertility, although confidence intervals overlapped substantially (Table 5 and Web Figure 1). Women experiencing secondary infertility were more likely to be attempting pregnancy compared with those experiencing primary infertility (57.1% with secondary infertility vs. 45.9% with primary infertility; P = 0.04 using χ2 test).
Figure 1.
Kaplan-Meier curves of time to spontaneous pregnancy after periods of unprotected intercourse, truncated at 10 years and stratified by pregnancy intent, among Georgia women aged 22–45 years, Furthering Understanding of Cancer, Health, and Survivorship in Adult Women Study, 2012–2015. A) After 6 months of unprotected intercourse (n = 432); B) after 12 months of unprotected intercourse (n = 358); C) after 24 months of unprotected intercourse (n = 238).
Table 5.
Cumulative Incidence of Spontaneous Pregnancy (%) After a Period of Infertility, Stratified by Primary and Secondary Infertilitya, Furthering Understanding of Cancer, Health, and Survivorship in Adult Women Study 2012–2015
| No. of Months After Infertility Period | Unprotected Intercourse for 6 Months | Unprotected Intercourse for 12 Months | Unprotected Intercourse for 24 Months | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total (n = 432)b | Primary (n = 255) | Secondary (n = 176) | Total (n = 358)b | Primary (n = 209) | Secondary (n = 148) | Total (n = 238)b | Primary (n = 142) | Secondary (n = 95) | |
| 6 | 27.0 | 24.5 | 30.7 | 24.2 | 20.6 | 29.4 | 20.5 | 17.8 | 24.6 |
| 12 | 33.7 | 31.2 | 37.5 | 38.6 | 33.9 | 45.8 | 35.9 | 33.4 | 40.0 |
| 24 | 47.5 | 43.8 | 53.5 | 50.7 | 47.4 | 56.0 | 45.3 | 42.1 | 50.2 |
| 72 | 71.6 | 68.5 | 76.5 | 70.6 | 68.2 | 74.7 | 66.0 | 63.5 | 70.2 |
| 120 | 84.7 | 82.4 | 88.1 | 85.8 | 84.2 | 88.2 | 81.5 | 79.7 | 84.1 |
| >120 | 89.7 | 86.3 | 95.5 | 87.6 | 84.2 | 94.1 | 83.8 | 79.7 | 92.1 |
a Primary infertility included nulliparous women who experienced infertility, and secondary infertility referred to women who had had at least 1 child at the time of infertility.
b One woman was missing age at pregnancy so type of infertility (primary vs. secondary) was unknown.
Our study population was younger than that of Marchbanks et al. (1), with 40.2% over 40 years of age compared with 72.6% for Marchbanks et al. Further, 28.5% of our participants were black compared with their 10.4%, and 34.7% of our population had graduate-level education compared with 13.0% for Marchbanks et al. The prevalences of infertility in the Marchbanks et al. study were similar to ours across definitions, except that a slightly smaller percentage of women in our study were classified as infertile based on 24 months of attempting pregnancy and visiting a doctor for help getting pregnant (Table 6). These differences persisted after adjustment for age, although they were slightly attenuated after adjustment for race and education.
Table 6.
Prevalence of Infertility Comparisons Using Data From the Populations of the Cancer and Hormone Study (1980–1983) and the Furthering Understanding of Cancer, Health, and Survivorship in Adult Women Study (2012–2015)
| Infertility Definition | Cancer and Hormone Study | FUCHSIA Women’s Study | ||||
|---|---|---|---|---|---|---|
| Crude Prevalence | Crude Prevalence (Age-Restricted)a | Crude Prevalence | Age-Adjusteda,b | Race/Ethnicity-Adjustedb,c | Education-Adjustedb | |
| 12 months of unprotected intercourse | 38.6 | 34.4 | 35.3 | 35.6 | 34.2 | 43.1 |
| 24 months of unprotected intercourse | 27.0 | 21.6 | 23.5 | 23.9 | 22.1 | 31.4 |
| 24 months of attempting pregnancy | 16.1 | 14.9 | 11.2 | 10.9 | 11.9 | 13.4 |
| Visited a doctord | 12.2 | 11.3 | 7.5 | 7.1 | 8.3 | 8.1 |
| Doctor diagnosise | 6.8 | 6.7 | 4.9 | 4.6 | 5.6 | 5.7 |
a Based only on data from women aged 20–44 years, calculated from proportions presented in Marchbanks et al. (1, Table 2).
b Adjusted to the distributions of demographic characteristics (age, race, education) in the Marchbanks et al. study population.
c Denominator excludes 6 people missing information on race/ethnicity.
d No conception after 24 months of trying to conceive, and couple consulted physician for help getting pregnant.
e No conception after 24 months of trying to conceive, couple consulted physician for help, and physician diagnosed problem in woman, partner, or both.
Marchbanks et al. only considered visiting a doctor for help getting pregnant after 24 months of attempting pregnancy (1). When we added this condition, the estimated prevalence of infertility based on the physician-related definitions decreased in our study (e.g., visited a doctor for help getting pregnant: 16.6 vs. 7.5%; physician diagnosis of infertility: 9.7 vs. 4.9%). These estimates were also lower than those reported in Marchbanks et al. (visited a doctor for help getting pregnant: 11.3%; physician diagnosis of infertility: 6.7%). Finally, time to pregnancy after infertility based on unprotected intercourse differed slightly between Marchbanks et al. and our study. The estimated cumulative incidence of pregnancy at 6, 12, 24, and 72 months after 12 months of unprotected intercourse was about 5%–10% less in our study compared with Marchbanks et al. However, our estimates were similar by 120 months (85.8% vs. 83.8%, respectively). Last, our estimates of cumulative incidence of pregnancy after having had unprotected intercourse for 24 months were almost identical to those of Marchbanks et al. for all time points.
DISCUSSION
Significant changes in society, technology, and clinical practice related to reproductive health provided the motivation for revisiting the objectives of Marchbanks et al. (1). Our study confirms that a history of infertility is common, although it often spontaneously resolves. Although the original Marchbanks et al. study was conducted over 25 years ago, our reported prevalences of infertility based on 12 and 24 months of unprotected intercourse were very similar. However, fewer women were classified as infertile by 24 months of attempting pregnancy in our study, compared with Marchbanks et al. This difference may have been due to women in our study seeking care before 24 months of attempting pregnancy, which is consistent with the American Society for Reproductive Medicine recommendation that women seek care after 6 or 12 months of attempting pregnancy, depending on their age. Similarly, we found that women in our study were less likely than women described in Marchbanks et al. to be classified as infertile as a result of visiting a doctor for help getting pregnant or doctor diagnosis of infertility, but only after restricting analysis to women who attempted pregnancy for 24 months first. Although this restriction applied by Marchbanks et al. may be outdated in the United States, we note that in certain countries that offer free ART, 2 years of attempting pregnancy is often required (22). Overall, as in the original study, we found that the estimated prevalence of infertility varied widely across definitions, with the lowest proportion of women meeting the definition of doctor diagnosis of female infertility and the greatest proportion being based on unprotected intercourse for at least 6 months. Further, the prevalence of infertility differed by demographic characteristics. There was a high cumulative incidence of pregnancy after infertility across definitions. However, women who were attempting pregnancy were more likely to become pregnant compared with those who were not, and those experiencing secondary infertility were more likely to become pregnant than those with primary infertility.
As in the original paper, women who were black (vs. white) and less educated (vs. more educated) were more likely to be classified as infertile by definitions based on unprotected intercourse and less likely to be classified as infertile based on visiting a doctor for help getting pregnant or on receiving a diagnosis of infertility. The finding that black women were less likely to visit a doctor for help becoming pregnant has been previously reported in this cohort (23) and in others, including Marchbanks et al. (1, 24, 25). Barriers to seeking medical attention for help becoming pregnant may include an inability to afford infertility treatments or a general lack of access to care (24). This disparity may also be affected in part by comfort with ART. In this cohort, black women were less comfortable with ART than were white women (23).
The estimated prevalences of infertility based on attempting pregnancy were about half the prevalences based on unprotected intercourse across all time periods. Many women experience infertility during prolonged periods of unprotected sex without conceiving when they are not attempting pregnancy (26, 27), but these women are excluded from definitions based on attempting pregnancy. Further, among those having unprotected intercourse, there are differences by race and income in pregnancy intention (27, 28). Our results support these reports, and we were able to quantify differences in the prevalence of infertility based on unprotected intercourse and attempting pregnancy across various demographic strata. However, we note that pregnancy intentions represent a complex construct that is difficult to measure. For example, it is possible that during a single period of unprotected intercourse, couples may change from not attempting pregnancy to attempting pregnancy and perhaps back to not attempting pregnancy. Our study would not have been able to capture that level of detail, other related practices, or couple-level nuances.
Most women achieved pregnancy after being classified as infertile, which suggests that most infertility was resolved. This is consistent with other reports of subfertile couples (29, 30). However, among women who did not conceive within 6 or 12 months of having unprotected intercourse, those who were attempting pregnancy were more likely to eventually become pregnant, which is likely due to a combination of knowledge and behavior (31). In contrast, attempting pregnancy was not associated with an increased probability of pregnancy for women who had 24 months of unprotected intercourse, which may indicate a biologic problem that cannot be improved by appropriately timing intercourse. Our findings of an increased probability of pregnancy among women experiencing secondary versus primary infertility have been reported elsewhere (29, 32, 33) but were not reported by Marchbanks et al. Getting pregnant may be more likely among women who have conceived in the past, but in our study, a greater proportion of women experiencing secondary infertility were also attempting pregnancy. Thus, variability in the proportion of women attempting pregnancy may partially explain differences across studies in the probability of pregnancy for women with primary versus secondary infertility.
Our study has several strengths. First, we asked women detailed questions about their fertility history. The importance of collecting the length of infertility without an upper limit, instead of asking women about precategorized periods of infertility, has been previously noted (34). Our questions allowed us to derive various definitions of infertility as well as calculate the cumulative incidence of pregnancy after infertility based on these definitions. Although we were able to address the definitions explored by Marchbanks et al., we were unable to explore other approaches, such as the current-duration approach, which estimates the distribution of time to pregnancy among couples having unprotected intercourse using a cross-sectional design (35, 36). We were unable to implement this approach because we did not ask women if they were currently having unprotected sex.
Another strength of our study is that our denominator was not restricted to those who were trying to get pregnant. This has been noted as a limitation of other studies (35). Our results show how many and which women are excluded from definitions that restrict to couples that are attempting pregnancy. Not only does this restriction likely result in an underestimate of infertility, but we observed that certain demographic groups, such as black women and women with lower income, were less likely to be categorized as infertile with this restriction. Thus, studies of women attempting pregnancy may have limited generalizability. Although including all women having unprotected intercourse regardless of pregnancy intent may decrease false negatives, it may increase false positives because it will include couples who may not be timing intercourse appropriately for pregnancy because they are not actively trying to achieve pregnancy.
A final strength was that in our analysis of the cumulative incidence of pregnancy, we were able to censor women who achieved pregnancy through infertility treatment (n = 23) (31). Our estimates of the cumulative incidence of pregnancy were similar to the estimates of Marchbanks et al. By censoring women at the time of fertility treatment initiation, we were able to focus on “spontaneous” pregnancies, and this likely made our results comparable to Marchbanks et al., which was conducted when fertility treatment was more limited. When we considered all pregnancies, our estimates increased by about 3%–5%. We were also able to censor women because of surgical menopause and sterilization, which is important because the use of surgical sterilization procedures has increased since the 1980s (37).
Despite these strengths, our study had some limitations. Our study population is likely different from the general female US population. We recruited women without a history of cancer from a purchased list to serve as the comparison group for female cancer survivors in the FUCHSIA Women’s Study. Women in the comparison group had distributions of race, education, income, and relationship status similar to those of the cancer survivors who were recruited from a population-based registry, which provides some reassurance that our study population shared sociodemographic characteristics with the cancer survivors. In this study, we provided prevalence estimates standardized to the age distribution of women aged 22–45 years in the United States to further improve representativeness, and our estimates changed minimally. We compared our results to those of Marchbanks et al., and this comparison was affected by selection factors for both studies. Differences in study populations are always of concern when comparing across studies. However, our study and that of Marchbanks et al. share several common attributes. Both infertility studies used the comparison group from studies where the comparison group was matched to female cancer survivors recruited from population-based registries. Thus, our study is well suited to be compared with the original study and provides a unique opportunity to evaluate temporal changes in female infertility.
Due to the retrospective cohort study design, our estimates of infertility based on months of unprotected intercourse or attempting pregnancy were subject to error in recall. However, a previous study indicated that retrospective report of time to pregnancy had good accuracy (38). This is corroborated by our estimate of infertility based on 12 months of attempting pregnancy (19.7%) being similar to estimates of infertility after 12 months in preconception cohorts in the United States with prospective follow-up, ranging from 13%–18% (39, 40).
Last, our estimation of the prevalence of infertility was affected by many factors. We estimated the prevalence of infertility in women, but fertility is affected by the health of 2 people. Some women may have been classified as infertile because of their partner’s reproductive health rather than their own. Further, these definitions do not exclusively reflect an underlying biological capacity to have children and may be affected by access to healthcare, lifestyle choices, and comfort with the use of ART and/or adoption, among other factors. In fact, some definitions apply directly to the woman’s actions (i.e., visited a doctor for help getting pregnant) or her attitudes and beliefs (i.e., attempting pregnancy). Accordingly, some definitions may be better suited than others depending on the goal of the study. For example, definitions based on attempting pregnancy may underestimate the prevalence of underlying infertility and the need for care in certain populations, and definitions based on visiting a doctor for help getting pregnant may not be appropriate in studies estimating subclinical effects on time to pregnancy. Despite this, our study provides a comprehensive overview of ways to measure female reproductive capacity that have been used in previous research and how estimates vary by definition.
The present study illustrates that in order to better understand the burden of infertility, evaluating the strengths and limitations of different definitions is paramount. This is particularly true when comparing definitions of self-reported infertility versus clinical evaluations of infertility. Given our findings that the definition (continues to) make a difference overall and within demographic subgroups, future studies should carefully consider which definition best aligns with their study aims and understand the ramifications of their choice for both internal and external validity. Moreover, investigators may consider collecting data on different definitions and comparing results across them. By using multiple definitions and evaluating any differences between them, we may be able to assess which results are robust across definitions and which may vary. This may allow us to better understand variation across studies and lead us to improve the overall characterization and study of infertility.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Rollins School of Public Health, Emory University, Atlanta, Georgia (Melanie H. Jacobson, Helen B. Chin, Amy Fothergill, Penelope P. Howards); Epidemiology Branch, National Institute of Environmental Health Sciences, National Institutes of Health, Department of Health and Human Services, Research Triangle Park, North Carolina (Helen B. Chin); Aflac Cancer and Blood Disorders Center, Department of Pediatrics, Emory University School of Medicine, Atlanta, Georgia (Ann C. Mertens); and Department of Gynecology and Obstetrics, Emory University School of Medicine, Atlanta, Georgia (Jessica B. Spencer).
Funding provided by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grants 1R01HD066059 and T32HD052460). This research was supported in part by the Intramural Research Program of the National Institutes of Health, National Institute of Environmental Health Sciences.
We thank Dr. Polly Marchbanks for inspiring this work.
A preliminary version of this work was presented at the Society for Epidemiologic Research 48th Annual Meeting, June 16–19, 2015, Denver, Colorado.
Conflict of interest: none declared.
Abbreviations
- ART
assisted reproductive technology
- FUCHSIA Women’s Study
Furthering Understanding of Cancer, Health, and Survivorship in Adult Women Study
REFERENCES
- 1. Marchbanks PA, Peterson HB, Rubin GL, et al. The Cancer and Steroid Hormone Study Group Research on infertility: definition makes a difference. Am J Epidemiol. 1989;130(2):259–267. [DOI] [PubMed] [Google Scholar]
- 2. Zegers-Hochschild F, Adamson GD, de Mouzon J, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92(5):1520–1524. [DOI] [PubMed] [Google Scholar]
- 3. Mascarenhas MN, Cheung H, Mathers CD, et al. Measuring infertility in populations: constructing a standard definition for use with demographic and reproductive health surveys. Popul Health Metr. 2012;10(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Speroff L, Fritz MA. Clinical Gynecologic Endocrinology and Infertility. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 5. Solomon CG, Hu FB, Dunaif A, et al. Menstrual cycle irregularity and risk for future cardiovascular disease. J Clin Endocrinol Metab. 2002;87(5):2013–2017. [DOI] [PubMed] [Google Scholar]
- 6. Berkowitz GS, Lapinski RH, Wein R, et al. Race/ethnicity and other risk factors for gestational diabetes. Am J Epidemiol. 1992;135(9):965–973. [DOI] [PubMed] [Google Scholar]
- 7. Brinton LA, Berman ML, Mortel R, et al. Reproductive, menstrual, and medical risk factors for endometrial cancer: results from a case-control study. Am J Obstet Gynecol. 1992;167(5):1317–1325. [DOI] [PubMed] [Google Scholar]
- 8. Gurunath S, Pandian Z, Anderson RA, et al. Defining infertility—a systematic review of prevalence studies. Hum Reprod Update. 2011;17(5):575–588. [DOI] [PubMed] [Google Scholar]
- 9. Mathews TJ, Hamilton BE. Delayed childbearing: more women are having their first child later in life. NCHS Data Brief. 2009;(21):1–8. [PubMed] [Google Scholar]
- 10. Mathews TJ, Hamilton BE. Mean age of mothers is on the rise: United States, 2000–2014. NCHS Data Brief. 2016;(232):1–8. [PubMed] [Google Scholar]
- 11. Jain T, Missmer SA, Hornstein MD. Trends in embryo-transfer practice and in outcomes of the use of assisted reproductive technology in the United States. N Engl J Med. 2004;350(16):1639–1645. [DOI] [PubMed] [Google Scholar]
- 12. Chandra A, Copen CE, Stephen EH. Infertility service use in the United States: data from the National Survey of Family Growth, 1982–2010. Natl Health Stat Report. 2014;(73):1–21. [PubMed] [Google Scholar]
- 13. Henne MB, Bundorf MK. Insurance mandates and trends in infertility treatments. Fertil Steril. 2008;89(1):66–73. [DOI] [PubMed] [Google Scholar]
- 14. Sunderam S, Kissin DM, Crawford SB, et al. Assisted reproductive technology surveillance—United States, 2011. MMWR Surveill Summ. 2014;63(10):1–28. [PubMed] [Google Scholar]
- 15. Wright VC, Shah S. Assisted Reproductive Technology Surveillance: United States, 2001 Washington, DC: US Department of Health and Human Services; 2004. [PubMed]
- 16. Practice Committee of American Society for Reproductive Medicine Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril. 2013;99(1):63. [DOI] [PubMed] [Google Scholar]
- 17. Chin HB, Johnson CY, Kim KH, et al. Piloting a computer assisted telephone interview: the FUCHSIA Women’s Study. BMC Womens Health. 2014;14:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. US Census Bureau Population Division Annual Estimates of the Resident Population by Single Year of Age and Sex for the United States: April 1, 2010 to July 1, 2014 Washington, DC: US Department of Commerce; 2014.
- 19. Curtin LR, Klein RJ Direct Standardization (Age-Adjusted Death Rates). Washington, DC: US Department of Health and Human Services; 1995. [PubMed]
- 20. Ingram DD, Franco SJ. 2013 NCHS urban-rural classification scheme for counties. Vital Health Stat 2. 2014;(166):1–73. [PubMed] [Google Scholar]
- 21. Chandra A, Copen CE, Stephen EH. Infertility and impaired fecundity in the United States, 1982–2010: data from the National Survey of Family Growth. Natl Health Stat Rep. 2013(67):1–18. [PubMed] [Google Scholar]
- 22. Lintsen AM, Eijkemans MJ, Hunault CC, et al. Predicting ongoing pregnancy chances after IVF and ICSI: a national prospective study. Hum Reprod. 2007;22(9):2455–2462. [DOI] [PubMed] [Google Scholar]
- 23. Chin HB, Howards PP, Kramer MR, et al. Racial disparities in seeking care for help getting pregnant. Paediatr Perinat Epidemiol. 2015;29(5):416–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jain T. Socioeconomic and racial disparities among infertility patients seeking care. Fertil Steril. 2006;85(4):876–881. [DOI] [PubMed] [Google Scholar]
- 25. Seifer DB, Frazier LM, Grainger DA. Disparity in assisted reproductive technologies outcomes in black women compared with white women. Fertil Steril. 2008;90(5):1701–1710. [DOI] [PubMed] [Google Scholar]
- 26. Larsen U. Research on infertility: which definition should we use? Fertil Steril. 2005;83(4):846–852. [DOI] [PubMed] [Google Scholar]
- 27. Greil AL, McQuillan J, Johnson K, et al. The hidden infertile: infertile women without pregnancy intent in the United States. Fertil Steril. 2010;93(6):2080–2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Borrero S, Nikolajski C, Steinberg JR, et al. “It just happens”: a qualitative study exploring low-income women’s perspectives on pregnancy intention and planning. Contraception. 2015;91(2):150–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Snick HK, Snick TS, Evers JL, et al. The spontaneous pregnancy prognosis in untreated subfertile couples: the Walcheren primary care study. Hum Reprod. 1997;12(7):1582–1588. [DOI] [PubMed] [Google Scholar]
- 30. Gnoth C, Godehardt E, Frank-Herrmann P, et al. Definition and prevalence of subfertility and infertility. Hum Reprod. 2005;20(5):1144–1147. [DOI] [PubMed] [Google Scholar]
- 31. Joffe M, Key J, Best N, et al. Studying time to pregnancy by use of a retrospective design. Am J Epidemiol. 2005;162(2):115–124. [DOI] [PubMed] [Google Scholar]
- 32. Akande VA, Hunt LP, Cahill DJ, et al. Differences in time to natural conception between women with unexplained infertility and infertile women with minor endometriosis. Hum Reprod. 2004;19(1):96–103. [DOI] [PubMed] [Google Scholar]
- 33. Collins JA, Burrows EA, Wilan AR. The prognosis for live birth among untreated infertile couples. Fertil Steril. 1995;64(1):22–28. [PubMed] [Google Scholar]
- 34. Cabrera-León A, Lopez-Villaverde V, Rueda M, et al. Calibrated prevalence of infertility in 30- to 49-year-old women according to different approaches: a cross-sectional population-based study. Hum Reprod. 2015;30(11):2677–2685. [DOI] [PubMed] [Google Scholar]
- 35. Thoma ME, McLain AC, Louis JF, et al. Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil Steril. 2013;99(5):1324.e1–1331.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Slama R, Ducot B, Carstensen L, et al. Feasibility of the current-duration approach to studying human fecundity. Epidemiology. 2006;17(4):440–449. [DOI] [PubMed] [Google Scholar]
- 37. Chandra A. Surgical sterilization in the United States: prevalence and characteristics, 1965–95. Vital Health Stat 23. 1998(20):1–33. [PubMed] [Google Scholar]
- 38. Jukic AM, McConnaughey DR, Weinberg CR, et al. Long-term recall of time to pregnancy. Epidemiology. 2016;27(5):705–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Buck Louis GM, Sundaram R, Schisterman EF, et al. Heavy metals and couple fecundity, the LIFE Study. Chemosphere. 2012;87(11):1201–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zinaman MJ, Clegg ED, Brown CC, et al. Estimates of human fertility and pregnancy loss. Fertil Steril. 1996;65(3):503–509. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.