Abstract
We estimated associations between neighborhood supermarket gain or loss and glycemic control (assessed by glycated hemoglobin (HbA1c) values) in patients from the Kaiser Permanente Northern California Diabetes Registry (n = 434,806 person-years; 2007–2010). Annual clinical measures were linked to metrics from a geographic information system for each patient's address of longest residence. We estimated the association between change in supermarket presence (gain, loss, or no change) and change in HbA1c value, adjusting for individual- and area-level attributes and according to baseline glycemic control (near normal, <6.5%; good, 6.5%–7.9%; moderate, 8.0%–8.9%; and poor, ≥9.0%). Supermarket loss was associated with worse HbA1c trajectories for those with good, moderate, and poor glycemic control at baseline, while supermarket gain was associated with marginally better HbA1c outcomes only among patients with near normal HbA1c values at baseline. Patients with the poorest baseline HbA1c values (≥9.0%) had the worst associated changes in glycemic control following either supermarket loss or gain. Differences were not clinically meaningful relative to no change in supermarket presence. For patients with type 2 diabetes mellitus, gaining neighborhood supermarket presence did not benefit glycemic control in a substantive way. The significance of supermarket changes on health depends on a complex interaction of resident, neighborhood, and store characteristics.
Keywords: diabetes management, food availability, neighborhood characteristics
The prevalence of type 2 diabetes mellitus is a major public health concern (1, 2). This chronic condition is characterized by insulin resistance and elevated blood sugar (hyperglycemia), which can lead to serious complications, including heart disease, stroke, blindness, kidney failure, and loss of digits or limbs. Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins—and limited in sugar and refined carbohydrates—can help improve glycemic control and prevent or delay these complications (3).
The food retail options available where an individual lives may shape daily dietary choices and support or hinder individual efforts to self-manage this chronic condition (4). A growing number of governmental and nonprofit institutions are funding policy initiatives to subsidize the development of supermarkets and other fresh food retail in underserved neighborhoods (5–8). Such policies were developed under the assumption that the introduction of supermarket retail would deliver positive health benefits for area residents; however, this assumption is largely untested. Research on the health effects of community food retail interventions is still in nascent stages, with few longitudinal analyses to date. In recent years, a handful of studies examined diet and weight outcomes before and after neighborhood changes in supermarket retail but found no associations (9–12).
Virtually nothing is known about how neighborhood food retail changes affect disease management outcomes among the most clinically vulnerable residents who already have a chronic condition. Given that eating a nutritious diet is critical for glycemic control, the opening of the first supermarket in a food desert or the closure of the last remaining neighborhood supermarket could have a glycemic result on diabetic residents. Moreover, among residents with diabetes, those with worse glycemic control may be differentially affected by supermarket development and closure, because they may have the most to gain from new access and the most to lose from a loss of local fresh food retail.
Using data from the Kaiser Permanente Northern California (KPNC) Diabetes Registry for a period of 4 years (2007–2010), we estimated the associations between a gain or loss of neighborhood supermarket presence with changes in glycemic control (based on glycated hemoglobin (HbA1c) values) among patients with type 2 diabetes, stratified by baseline HbA1c levels. Relative to no change in neighborhood supermarket presence, we hypothesized that the opening of the first supermarket in a neighborhood (hereafter referred to as “supermarket gain”) would be associated with better HbA1c trajectories (i.e., larger HbA1c reductions or smaller HbA1c gains) and that the closure of the last supermarket in a neighborhood (here termed “supermarket loss”) would be associated with worse HbA1c trajectories (i.e., smaller HbA1c reductions or greater HbA1c gains) in all strata. Moreover, we hypothesized that patients with worse HbA1c levels at baseline would have the greatest relative HbA1c reduction from supermarket gain and the greatest relative HbA1c increase from supermarket loss.
METHODS
Study sample
The sample was drawn from the KPNC Diabetes Registry (13), a dynamic cohort of KPNC health-plan members with a history of diabetes ascertained from clinical and laboratory-based diagnoses. KPNC is a large, integrated not-for-profit health-care delivery system that provides care for approximately one-third of the residents in its service area in Northern California. A unique medical record number assigned to each member was used to link comprehensive clinical records with geospatial measures at each member's geocoded address at the census block centroid of record. The study period spanned 4 years from January 1, 2007, to December 31, 2010, with clinical measurements in each calendar year. Each subject's baseline was defined as his or her first year in the study. Data collection methods were approved by the KPNC Ethics Review Board, and written informed consent was waived.
Inclusion/exclusion criteria
Of all Registry members with type 2 diabetes mellitus, no end-stage renal disease, and at least 1 HbA1c record (n = 229,778 subjects), we excluded members with invalid address data (n = 11,579 subjects) as well as members with evidence of bariatric surgery, positive pregnancy test, or cancer diagnosis within 1 year before or after the study period (n = 33,676 subjects). Additionally, we restricted the sample of observations to limit residential mobility by retaining observations that corresponded to years at each subject's longest address of residence (excluded n = 76,204 person-years). Thus, for example, if a subject moved in the fourth year of the study period, we retained the first 3 years of observations, and if a subject moved in the first year, we retained the last 3 years of observations. Finally, we excluded subjects with less than 2 years of observations (after imputation) and removed potential outliers by dropping observations with extreme annual HbA1c change in the top or bottom 0.5% of the frequency distribution (n = 24,523). This left a final analytical sample of 160,000 subjects who contributed a total of 434,806 person-years.
Outcome: change in HbA1c
Individual-level change in annual average HbA1c (calculated as the average of all available HbA1c measures over the course of the calendar year) was the primary outcome of this study. HbA1c assays were ordered over the natural course of patient medical care and were conducted using high-performance liquid chromatography at a single KPNC central laboratory.
Exposure: change in supermarket neighborhood presence
In each year of the study period, we mapped updated retail locations of supermarkets and large grocery stores (with more than $2 million in sales annually and >2,499 square feet in floor area) based on InfoUSA (Papillion, Nebraska) business establishment data as of January 1st of each year, as distributed through ESRI Inc. (Redlands, California) (14). Store type designations in the commercial list were cleaned and reclassified based on Standard Industrial Codes (SIC) of businesses as well as by keyword searches and name recognition (Web Appendix 1, available at http://aje.oxfordjournals.org/). We created an indicator for supermarket presence in a subject's neighborhood, defined as a within-1-mile street network buffer around the census block centroid of each member's residential address, using ArcGIS 10.1 (ESRI Inc.) (15). Change in neighborhood presence of supermarkets compared with the previous year was then transformed into 3 mutually exclusive indicator variables: supermarket gain, no change, and supermarket loss.
Supermarket gain refers to the development of the first supermarket in a neighborhood without any supermarkets in the previous year. Similarly, supermarket loss refers to the closure of the last neighborhood supermarket, such that no neighborhood supermarkets are open in the current year. No change refers to the absence of both of these conditions. We developed these definitions under the assumption that, with respect to neighborhood health, the marginal benefit provided by each new supermarket is greatest with the first neighborhood supermarket and the marginal health cost of each neighborhood supermarket closure is greatest with the last supermarket closure.
Covariates: change in individual and neighborhood characteristics
Using InfoUSA business establishment data (Web Appendix 1), the physical activity kernel density (e.g., parks, camps, gyms, and recreation centers) and unhealthful food outlet kernel density (fast food outlets and convenience stores) within a mile of each member's census block centroid were estimated using a quadratic function for inverse distance weighting. Additionally, census-block group measures of population density, percent of population under the federal poverty level, and median self-reported home value were obtained from the 2005–2009, 2006–2010, 2007–2011, and 2008–2012 5-year aggregate American Community Survey (ACS) releases. Aggregate estimates were assigned to the middle year of the 5-year period in panel data (16).
The Charlson Comorbidity Index was calculated from prior-year clinical records and serves as a validated measure of 10-year mortality risk based on the presence of 22 comorbid conditions (17, 18). Additionally, we created an indicator for the use of diabetes treatment medications that may lower HbA1c levels, including insulin, sulfonylurea, metformin, and thiazolidinediones.
Missing data
Missing values for both HbA1c and Charlson Comorbidity Index were imputed using chained equations as described in Web Table 1. Given that standard errors were estimated using bootstrapping, a single stochastic imputation was drawn for each missing value in each bootstrap iteration (19).
Statistical analyses
We estimated the association of change in neighborhood supermarket presence on individual-level HbA1c using a first-difference regression model (20) (model 1) in Stata, version 12 (StataCorp LP, College Station, Texas) (21).
Model 1:
In which i subscripts the individual, t subscripts the year, and is a vector of covariates including Charlson Comorbidity Index, diabetes medication use, physical activity venue density, unhealthful food outlet density, population density, percent under the federal poverty level, and median housing value. Based on the distribution of certain continuous variables (Charlson Comorbidity Index, physical activity venue density, unhealthful food outlet density, population density, percent under the federal poverty level, and median housing value), quadratic and cubic polynomials were included. β1 estimates the relationship between supermarket gain and change in HbA1c (compared with no supermarket-presence change), and β2 estimates the relationship between supermarket loss and change in HbA1c (compared with no supermarket-presence change).
Subjects were stratified by baseline HbA1c (categories: <6.5%, 6.5%–7.9%, 8.0%–8.9%, and ≥9.0%) and first-difference models were estimated for each stratum separately. Because all observations for each subject reflect time at a single address (the address of longest residence), within-subject changes in supermarket exposure from year to year can be attributed to supermarket developments and closures rather than to changes in residence.
Observations for each subject were inverse weighted by the subject's total contributed person-years of differenced observations to upweight subjects with fewer years of data. To account for a correlated error structure, empirical confidence intervals were calculated from 1,000 nonparametric bootstrap iterations of the data-imputation and model-fitting process. Sensitivity analyses (models 2–5) were conducted to test the robustness of estimates to more conservative model specifications that account for several potential sources of bias (details in Web Table 2).
RESULTS
There was no significant change in HbA1c over time, although comorbidity scores did increase over the course of the study (Table 1). Additionally, median home prices declined, and poverty rate and population density increased over time. Changes in neighborhood supermarket presence were rare. Over the 4-year period and for each baseline HbA1c stratum, approximately 7% of subjects experienced at least 1 annual gain in neighborhood supermarket presence where there had been no supermarkets in the previous year, and approximately 8% of subjects experienced at least 1 annual loss of neighborhood supermarket presence such that no supermarkets remained. Individual and neighborhood-level characteristics according to baseline HbA1c strata are presented in Web Table 3.
Table 1.
Individual- and Neighborhood-Level Characteristics of the Study Sample (After Imputation), Kaiser Permanente Northern California Diabetes Registry, 2007–2011
| Characteristic | 2007 (n = 143,152) |
2008 (n = 143,152) |
2009 (n = 146,324) |
2010 (n = 145,328) |
||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | Mean (SD) | % | |
| Individual-Level Variables | ||||||||
| Age | 61.9 (12.6) | 62.9 (12.6) | 63.7 (12.6) | 64.7 (12.6) | ||||
| Female sex | 47.0 | 46.8 | 46.9 | 46.8 | ||||
| Race | ||||||||
| Asian | 18.0 | 18.0 | 18.1 | 18.0 | ||||
| Black | 9.3 | 9.3 | 9.4 | 9.3 | ||||
| Hispanic (nonwhite) | 20.0 | 20.0 | 19.9 | 20.0 | ||||
| White | 46.2 | 46.2 | 46.0 | 46.1 | ||||
| Other | 6.5 | 6.5 | 6.5 | 6.5 | ||||
| BMIa | 31.6 (7.1) | 31.5 (7.2) | 31.5 (7.2) | 31.4 (7.2) | ||||
| HbA1c | ||||||||
| NGSP, % | 7.3% (1.4%) | 7.1% (1.4%) | 7.2% (1.4%) | 7.2% (1.4%) | ||||
| IFCC, mmol/mol | 56 (15.3) | 54 (15.3) | 55 (15.3) | 55 (15.3) | ||||
| Comorbidity score | 1.8 (1.2) | 2.0 (1.5) | 2.2 (1.6) | 2.3 (1.6) | ||||
| Using insulin, thiazolidinediones, metformin, or sulfonylureas | 66.0 | 67.9 | 67.4 | 66.7 | ||||
| Neighborhood-Level Variables | ||||||||
| Any supermarket presence | 54.0 | 54.0 | 52.6 | 52.2 | ||||
| Gained supermarket presence (vs. prior year) | 2.0 | 2.5 | 2.5 | |||||
| Lost supermarket presence (vs. prior year) | 2.0 | 3.8 | 2.7 | |||||
| Fast food and convenience store, no. in 1-mile network radius | 1.2 (1.2) | 1.1 (1.2) | 1.2 (1.2) | 1.2 (1.2) | ||||
| Physical activity venue, no. in 1-mile network radius | 1.5 (1.7) | 1.4 (1.7) | 1.4 (1.7) | 1.5 (1.7) | ||||
| Median home price, $ | 509,305 (216,743) | 483,864 (227,225) | 446,250 (232,101) | 413,092 (235,830) | ||||
| Poverty rate, % | 10.0 (9.7) | 10.4 (10.3) | 11.0 (10.6) | 11.7 (10.9) | ||||
| Population per square mile | 8,084 (8,396) | 8,298 (8,801) | 8,354 (8,866) | 8,396 (8,890) | ||||
Abbreviations: BMI, body mass index; HbA1c, glycated hemoglobin; IFCC, International Federation of Clinical Chemistry; NGSP, National Glycohemoglobin Standardization Program; SD, standard deviation.
a BMI was calculated as weight (kg)/height (m)2.
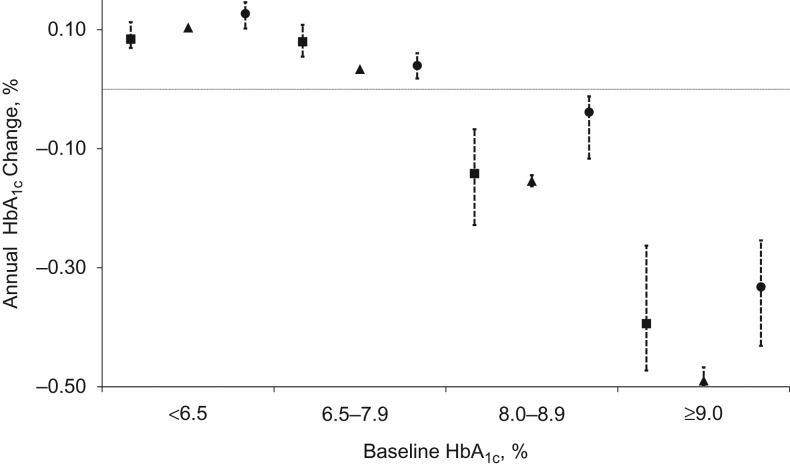
Overall, patients with the lowest HbA1c at baseline experienced the greatest annual increase in HbA1c and patients with the highest HbA1c at baseline experienced the greatest annual decrease in HbA1c (Figure 1). This pattern is not surprising and may reflect regression to the mean.
Figure 1.
Annual adjusted change in glycated hemoglobin (HbA1c) by baseline HbA1c values and change in neighborhood supermarket presence, Kaiser Permanente Northern California Diabetes Registry, 2007–2011. Annual HbA1c change for each category of change in supermarket presence (square: neighborhood supermarket presence gain; triangle: no change in neighborhood supermarket presence; circle: neighborhood supermarket presence loss), presented by baseline HbA1c. Estimates were adjusted for Charlson Comorbidity Index, diabetes medication use, physical activity venue density, unhealthful food outlet density, population density, poverty rate, and median census-block-group housing value. Baseline sample sizes according to HbA1c stratum: ≥9.0% n = 18,343 persons; 8.0%–8.9%, n = 18,013 persons; 6.5%–7.9%, n = 75,123 persons; <6.5%, n = 48,521 persons. Percentile-based confidence intervals were obtained from 1,000 bootstrapped iterations of the data imputation and model estimation procedure.
However, within each stratum of baseline HbA1c values, change in neighborhood supermarket presence was associated with different magnitudes and directions of annual HbA1c change. Among patients with the lowest HbA1c values, those with no change in supermarket presence experienced an average annual increase in HbA1c of 0.10% (95% confidence interval (CI): 0.10, 0.11), patients who gained neighborhood supermarket presence had values increase by 0.08% (95% CI: 0.07, 0.11), and patients who lost neighborhood supermarket presence had values increase by 0.13% (95% CI: 0.10, 0.15). Among patients with the highest HbA1c values at baseline, those with no change in supermarket presence experienced a decrease in HbA1c of −0.49% (95% CI: −0.47, −0.50), while those who gained or lost neighborhood supermarket presence had a decrease of −0.39% (95% CI: −0.26, −0.47) or −0.33% (95% CI: −0.25, −0.43), respectively.
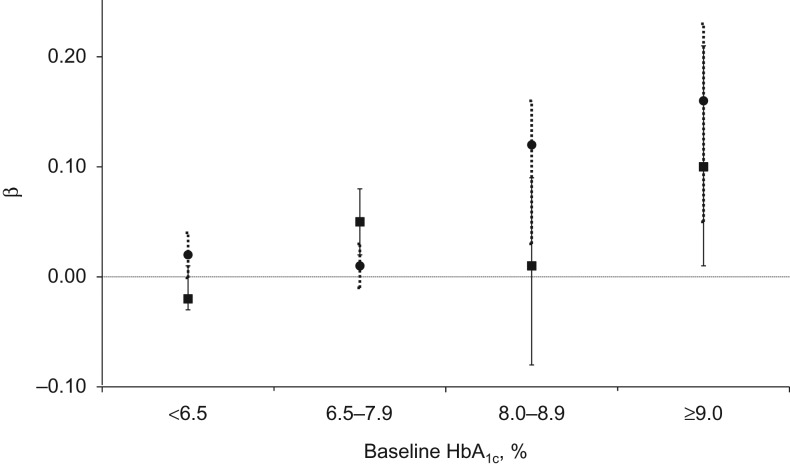
In stratum-specific adjusted associations between changes in neighborhood supermarket presence (i.e., supermarket gain ) or supermarket loss ) and HbA1c change), the reference category is no change in presence (Figure 2). Supermarket gain was not associated with HbA1c trajectories relative to the reference category among patients with near normal (<6.5%) glycemic control at baseline: −0.02% (95% CI: −0.03, 0.01). For patients with good (6.5%–7.9%) or poor (≥9.0%) glycemic control, supermarket gain was associated with slightly worse HbA1c trajectories (greater gains or smaller reductions) compared with the reference category (good control: change = 0.05%, 95% CI: 0.02, 0.08; poor control: change = 0.10%, 95% CI: 0.01, 0.21). Compared with the reference category of no change in presence, neighborhood supermarket loss was associated with worse HbA1c trajectories (greater gains or smaller reductions) for all patient strata. However, the magnitude of the association between supermarket loss and HbA1c change was greatest among patients with moderate (change = 0.12%, 95% CI: 0.03, 0.16) or poor (change = 0.16%, 95% CI: 0.05, 0.23) glycemic control at baseline.
Figure 2.
Adjusted associations between change in neighborhood supermarket presence and change in glycated hemoglobin (HbA1c) values, Kaiser Permanente Northern California Diabetes Registry, 2007–2011. Adjusted associations between change in presence of neighborhood supermarkets (square with solid error bars: neighborhood supermarket presence gain; circle with dotted error bars: neighborhood supermarket presence loss) and annual change in HbA1c, relative to the reference category of no change in neighborhood supermarket presence. Associations were adjusted for Charlson Comorbidity Index, diabetes medication use, physical activity venue density, unhealthful food outlet density, population density, poverty rate, and median census-block-group housing value. Baseline sample sizes HbA1c stratum: ≥9.0%, n = 18,343 persons; 8.0%–8.9%, n = 18,013 persons; 6.5%–7.9%, n = 75,123 persons; <6.5%, n = 48,521 persons. Percentile-based confidence intervals were obtained from 1,000 bootstrapped iterations of the data imputation and model estimation procedure.
In sensitivity analyses (Web Table 2), we found similar results in unadjusted models, models that adjusted for year effects and subject fixed effects, and in the complete-case analysis. Additionally, the estimated associations between supermarket gain or loss and HbA1c change did not differ by neighborhood poverty rate. However, in the long-difference model, which examined changes over 4 years, no significant associations were found.
DISCUSSION
To our knowledge, this is the first longitudinal study to estimate the influence of neighborhood supermarket availability on disease-management outcomes for residents with a chronic condition. The sheer size of the KPNC analysis sample provided us with the power to detect small effect sizes that would have been statistically ambiguous in smaller studies. Furthermore, several of the measures and analytical methods employed in this study are relatively novel in the literature addressing neighborhoods and health and may serve as a model for future research.
As we expected, relative to no change in supermarket presence, supermarket loss was associated with worse HbA1c trajectories. Also in line with expectations, patients with the poorest glycemic control at baseline appeared to have the largest relative HbA1c increase following supermarket loss. However, in contrast to our hypotheses, supermarket gain was not associated with better HbA1c trajectories. In fact, supermarket gain was associated with relatively worse HbA1c trajectories among patients with poor glycemic control at baseline compared with no change in supermarket presence.
Isolating the impact of local food retail on health is challenging given that many factors influence the selection of residents and retail into neighborhoods, each of which may independently affect health. Residential selection processes may bias study findings if people choose residential neighborhoods based on factors that are correlated with health outcomes (e.g., individuals with healthier lifestyles may be more likely to prioritize convenient access to supermarkets) (22). Retail selection is also problematic, because stores locate in neighborhoods based on factors correlated with individual health outcomes (e.g., local economic growth or population density).
We tested the robustness of our estimates to more conservative model specifications in sensitivity analyses, and we found that although sensitivity analysis estimates were attenuated (Web Table 2), they were consistent with primary analysis results. The associations that we found between neighborhood change in supermarket availability and change in HbA1c values were not explained by secular time trends or patient-level differences in HbA1c trajectories. Nor did the findings appear to be an artifact of the data-imputation process. Moreover, while baseline HbA1c was strongly correlated with neighborhood poverty, the pattern of effect modification by baseline HbA1c does not appear to be attributable to underlying group differences in neighborhood affluence.
Overall, the estimated associations between change in supermarket presence and change in HbA1c were small relative to the influences of standard pharmaceutical and lifestyle recommendations such as metformin (23), exercise (24), and nutrition therapy (25) and would not be considered clinically significant. Additionally, it is important to note that the associations between supermarket gain or loss and change in HbA1c were not observed in long-difference regression models and thus appear to be short-lived.
We propose several possible explanations for our findings. First, both gains and losses of neighborhood supermarket availability constitute major disruptions to the local retail environment and to household routines of food acquisition, preparation, and consumption. A change in the food retail environment may trigger food purchasing changes as residents adapt to different shopping opportunities. Observed differences in associations across baseline HbA1c strata may be due to differences in how patients adapt to this change. Patients with better control of their chronic condition may be better able to leverage the healthful food resources in the supermarket to improve their metabolic outcomes. On the other hand, patients who struggled to maintain glycemic control at baseline may have a harder time adjusting to either gains or losses in neighborhood supermarket availability.
Observed differences in estimates across patient strata may also be due to underlying differences in neighborhood supermarket attributes. Supermarkets vary widely by category (e.g., chain vs. independent, ethnic vs. nonethnic, discount vs. premium) and in-store characteristics (e.g., food availability, variety, product mix, and quality). Our study estimated an average association across all supermarkets and did not account for the influence of store-specific characteristics. This is a limitation of our analysis.
Last, our estimates may be confounded by unmeasured concurrent neighborhood changes. Although we adjusted for changes in the density of fast food outlets and convenience stores, neighborhood supermarket gain may be accompanied by the development of other food retail, such as full-service restaurants and bars. These specific food retail changes were omitted in our study but may nonetheless affect HbA1c values. Alternatively, supermarket closure may be a symptom of general neighborhood disinvestment leading to the deterioration or loss of unmeasured health assets such as a community center or clinic. While we adjusted for changes in several neighborhood-level attributes, inaccurate measurement of these covariates or omission of other time-varying neighborhood factors could bias our results.
Our study has several other limitations. First, this sample represents an insured population of patients with type 2 diabetes who regularly obtain HbA1c assessments, and results may not be generalizable to other populations. Although we made efforts to minimize selection bias through missing data imputation and regression weighting, subjects who failed to contribute a single HbA1c assessment and subjects with nongeocodable addresses were excluded from analyses. Second, the time lag between neighborhood supermarket change and measurement of HbA1c is also an important consideration for the interpretation of our findings. Our annual measures of neighborhood retail reflect store changes in the preceding calendar year. Thus, the actual time interval between change in neighborhood supermarket presence and patient HbA1c assessment could vary from as short as 1 day to as long as 24 months.
Even with these limitations, we believe that this policy-relevant study makes a valuable contribution to the literature. In several influential cross-sectional studies, decreased proximity and availability of supermarkets have been associated with lower consumption of fruits and vegetables, poorer adherence to dietary guidelines, and greater risk of obesity (26–30). While associations are not indicative of a causal relationship, these findings have shaped the public perception of supermarkets as community health assets (31, 32). Conversely, neighborhoods that lack supermarket presence (i.e., food deserts) are increasingly targets for policy intervention (33).
Supermarket availability is commonly used as a proxy for neighborhood healthful food availability, but this practice is overly simplistic and may mislead policy makers to prioritize supermarket development over other policy solutions. Future longitudinal studies in this research domain should adopt more nuanced measures of healthy food availability that take into account within-store characteristics such as affordability, quality, product mix, and variety.
While access to healthful food is a necessary condition for the successful management of chronic conditions, our findings suggest that supermarket presence is not sufficient. Supermarkets offer a wide array of both healthful and unhealthful foods and the net influences of supermarket development and closure on health likely depend on a complex interaction of individual behavioral, neighborhood, and store characteristics.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Division of Epidemiology, School of Public Health, University of California, Berkeley, Berkeley, California (Y. Tara Zhang, Mahasin S. Mujahid); Division of Public Health Nutrition, School of Public Health, University of California, Berkeley, Berkeley, California (Barbara A. Laraia); Division of Research, Kaiser Permanente, Oakland, California (E. Margaret Warton, Howard H. Moffet, Andrew J. Karter); and Department of Environmental Science, Policy and Management, University of California, Berkeley, Berkeley, California (Samuel D. Blanchard); Center for Health and Community, University of California, San Francisco, San Francisco, California (Janelle Downing).
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (grants R01-DK-080744, R01 DK065664, and P30 DK092924) and the National Heart, Lung, and Blood Institute (grant K01HL115494).
We thank Rucker Johnson of the Goldman School for Public Policy at University of California, Berkeley, for his statistical guidance and assistance in manuscript review.
Conflict of interest: none declared.
REFERENCES
- 1. American Diabetes Association Economic costs of diabetes in the US in 2012. Diabetes Care. 2013;36(4):1033–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Geiss LS, Wang J, Cheng YJ, et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA. 2014;312(12):1218–1226. [DOI] [PubMed] [Google Scholar]
- 3. American Diabetes Association, Bantle JP, Wylie-Rosett J, Albright AL, et al. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2008;31(suppl 1):S61–S78. [DOI] [PubMed] [Google Scholar]
- 4. Horowitz CR, Colson KA, Hebert PL, et al. Barriers to buying healthy foods for people with diabetes: evidence of environmental disparities. Am J Public Health. 2004;94(9):1549–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Office of Sustainability, Department of Planning Baltimore Food Policy Initiative Berkeley, CA; 2010. http://archive.baltimorecity.gov/Government/AgenciesDepartments/Planning/BaltimoreFoodPolicyInitiative/FoodDeserts.aspx. Accessed April 2, 2015. [Google Scholar]
- 6. City of New Orleans Fresh Food Retailer Initiative New Orleans, LA; 2013. http://www.nola.gov/city/fresh-food-retailers-initiative/. Accessed July 23, 2014. [Google Scholar]
- 7. The Food Trust What We Do: With Supermarkets Philadelphia, PA; 2012. http://thefoodtrust.org/what-we-do/supermarkets. Accessed April 29, 2016. [Google Scholar]
- 8. Denver Healthy Food Access Task Force Healthy Food for All: Encouraging Grocery Investment in Colorado Denver, CO: Denver Healthy Food Access Task Force; 2011. [Google Scholar]
- 9. Boone-Heinonen J, Gordon-Larsen P, Kiefe CI, et al. Fast food restaurants and food stores: longitudinal associations with diet in young to middle-aged adults: the CARDIA study. Arch Intern Med. 2011;171(13):1162–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Boone-Heinonen J, Diez-Roux AV, Goff DC, et al. The neighborhood energy balance equation: does neighborhood food retail environment + physical activity environment = obesity? The CARDIA study. PLoS One. 2013;8(12):e85141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff (Millwood). 2014;33(2):283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Elbel B, Moran A, Dixon LB, et al. Assessment of a government-subsidized supermarket in a high-need area on household food availability and children's dietary intakes. Public Health Nutr. 2015;18(15):2881–2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Karter AJ, Schillinger D, Adams AS, et al. Elevated rates of diabetes in Pacific Islanders and Asian subgroups: the Diabetes Study of Northern California (DISTANCE). Diabetes Care. 2013;36(3):574–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. ESRI Methodology Statement: 2015 Esri US Business Locations and Business Summary Data: An Esri White Paper Redlands, CA: Environmental Systems Research Institute; 2015. [Google Scholar]
- 15. ESRI ArcGIS Desktop Redland, CA: Environmental Systems Research Institute; 2012. [Google Scholar]
- 16. US Census Bureau American Community Survey (ACS) Washington, DC: US Census Bureau; 2014. https://www.census.gov/programs-surveys/acs/. Updated June 22, 2015. Accessed July 24, 2014. [Google Scholar]
- 17. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 18. van Walraven C, Escobar GJ, Greene JD, et al. The Kaiser Permanente inpatient risk adjustment methodology was valid in an external patient population. J Clin Epidemiol. 2010;63(7):798–803. [DOI] [PubMed] [Google Scholar]
- 19. Daniel RM, Stavola BLD, Cousens SN. gformula: estimating causal effects in the presence of time-varying confounding or mediation using the g-computation formula. Stata J. 2011;11(4):479–517. [Google Scholar]
- 20. Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. 2nd ed Cambridge, MA: The MIT Press; 2010:1096. [Google Scholar]
- 21. StataCorp Stata Statistical Software: Release 12 College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 22. Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Soc Sci Med. 2004;58(10):1929–1952. [DOI] [PubMed] [Google Scholar]
- 23. Hirst JA, Farmer AJ, Ali R, et al. Quantifying the effect of metformin treatment and dose on glycemic control. Diabetes Care. 2012;35(2):446–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Umpierre D, Ribeiro PA, Kramer CK, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2011;305(17):1790–1799. [DOI] [PubMed] [Google Scholar]
- 25. Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr. 2013;97(3):505–516. [DOI] [PubMed] [Google Scholar]
- 26. Rose D, Richards R. Food store access and household fruit and vegetable use among participants in the US Food Stamp Program. Public Health Nutr. 2004;7(8):1081–1088. [DOI] [PubMed] [Google Scholar]
- 27. Morland K, Wing S, Diez Roux A. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. Am J Public Health. 2002;92(11):1761–1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Laraia BA, Siega-Riz AM, Kaufman JS, et al. Proximity of supermarkets is positively associated with diet quality index for pregnancy. Prev Med. 2004;39(5):869–875. [DOI] [PubMed] [Google Scholar]
- 29. Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am J Prev Med. 2006;30(4):333–339. [DOI] [PubMed] [Google Scholar]
- 30. Moore LV, Diez Roux AV, Nettleton JA, et al. Associations of the local food environment with diet quality—a comparison of assessments based on surveys and geographic information systems. Am J Epidemiol. 2008;167(8):917–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Treuhaft S, Karpyn A. The Grocery Gap: Who Has Access to Healthy Food and Why It Matters Philadelphia, PA: Policy Link and The Food Trust; 2010. [Google Scholar]
- 32. Heinzmann D. Emanuel amplifies the call for more fresh food Chicago, IL: Chicago Tribune; 2011. http://articles.chicagotribune.com/2011-10-25/news/ct-met-emanuel-food-desert-20111025_1_food-deserts-mari-gallagher-stores-in-underserved-areas. Published October 24, 2011. Accessed April 1, 2015. [Google Scholar]
- 33. White House Task Force on Childhood Obesity Report to the President: Solving the Problem of Childhood Obesity Within a Generation Washington, DC: Executive Office of the President of the United States; 2010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.