Abstract
Chronic kidney disease (CKD) is an important social health problem characterized by a decrease in the kidney glomerular filtration rate (GFR). In this study, we analyzed genome-wide association studies for kidney disease-related traits using data from a Korean adult health screening cohort comprising 7,064 participants. Kidney disease-related traits analyzed include blood urea nitrogen (BUN), serum creatinine, estimated GFR, and uric acid levels. We detected two genetic loci (SLC14A2 and an intergenic region) and 8 single nucleotide polymorphisms (SNPs) associated with BUN, 3 genetic loci (BCAS3, C17orf82, ALDH2) and 6 SNPs associated with serum creatinine, 3 genetic loci (BCAS3, C17orf82/TBX2, LRP2) and 7 SNPs associated with GFR, and 14 genetic loci (3 in ABCG2/PKD2, 2 in SLC2A9, 3 in intergenic regions on chromosome 4; OTUB1, NRXN2/SLC22A12, CDC42BPG, RPS6KA4, SLC22A9, and MAP4K2 on chromosome 11) and 84 SNPs associated with uric acid levels. By comparing significant genetic loci associated with serum creatinine levels and GFR, rs9895661 in BCAS3 and rs757608 in C17orf82 were simultaneously associated with both traits. The SNPs rs11710227 in intergenic regions on chromosome 3 showing significant association with BUN is newly discovered. Genetic variations of multiple gene loci are associated with kidney disease-related traits, and differences in associations between kidney disease-related traits and genetic variation are dependent on the population. The meanings of the mutations identified in this study will need to be reaffirmed in other population groups in the future.
Introduction
Chronic kidney disease (CKD) is an important health problem that increases the incidence of cardiovascular disease and overall mortality [1]. Kidneys function is usually expressed as the glomerular filtration rate (GFR) and is generally deteriorated when the GFR is decreased. Traditionally, blood urea nitrogen (BUN) and serum creatinine levels have been used as surrogate markers of kidney function deterioration. BUN reflects the amount of nitrogen in the blood and is produced as a waste product of protein metabolism [2,3]. Serum creatinine is a representative biochemical indicator of kidney function and is produced by the breakdown of muscle creatine phosphate. Because the exacerbation of kidney function and the increase in serum creatinine level are not directly proportional, the GFR is estimated using demographic and biochemical factors, such as serum creatinine levels, age and sex. Uric acid is the last product of purine metabolism, and hyperuricemia develops when renal function is reduced and uric acid excretion is decreased [4]. Hyperuricemia is prevalent in patients with kidney disease, and genetic susceptibility plays an important role in the development of hyperuricemia [5]. Risk factors for CKD and end-stage renal disease requiring dialysis are diabetes mellitus, hypertension, glomerulonephritis, and polycystic kidney disease. However, these traditional risk factors alone cannot completely explain the development of CKD [6]. Genetic studies have shown that genetic factors affect approximately 36–75% of kidney function and vulnerability to CKD progression [7,8]. Genome-wide association studies have been used to identify genetic variations associated with kidney function in various populations, and differential genetic variation was found in each population group [9,10]. In this study, we conducted a genome-wide association and replication study of a Korean adult population to identify multiple genetic loci associated with kidney disease-related traits, including, BUN, serum creatinine, GFR, and uric acid levels.
Methods
Study participants
Between January 2014 and December 2014, 7,999 adults who underwent a health screening assessment at the Seoul National University Hospital Health Care System Gangnam Center were asked to consent to research, and their blood samples were collected and stored for further study. Most patients voluntarily conducted a personal health check-up or submitted to a health check-up with financial support from the company. The Institutional Review Board of Seoul National University Hospital approved the storage of blood samples for genetic analysis with informed consent. To investigate associations between genetic variations and kidney disease-related traits, we retrospectively enrolled 7,064 healthy participants after performing quality control analysis on the genetic samples. All participants had undergone blood sampling to measure BUN, serum creatinine, and uric acid levels. Demographic and other clinical information (age, sex, body mass index (BMI), comorbidities, and laboratory findings) regarding the participants were collected through electronic medical record review at the time of the health check-up. The Institutional Review Board of Seoul National University Hospital approved the research plan (IRB 1603-120-750), and the study was conducted in compliance with the Helsinki Declaration. Specifically, personal information was encrypted for confidentiality, and genetic information was analyzed by professional analysts in a third space separate from personal information.
Definition of kidney disease-related traits
The kidney function-related traits assessed in this study included BUN, serum creatinine, estimated GFR, and uric acid levels. GFRs were calculated using the Modification of Diet in Renal Disease (MDRD) estimated GFR equation.
Genotyping
Genomic DNA was extracted from venous blood samples genotyped using Affymetrix Axiom® Customized Biobank Genotyping Arrays (Affymetrix, Santa Clara, CA, USA), and the PLINK program (ver. 1.07) was used for quality control procedures. Specimens with the following characteristics were excluded from the analysis: low genotyping call rate (≤ 97%), sex inconsistency, and related and cryptically related individuals (identical by descent > 0.9). Small nucleotide polymorphisms (SNPs) with low call rates (< 97%), low minor allele frequency (MAF ≤ 0.05%), or significant deviation from the Hardy-Weinberg equilibrium permutation test (HWE P < 1.0 × 10−5) were excluded (S1 Table). After performing the quality control evaluations, 345,072 autosomal SNPs were retained for the association analysis. S2–S5 Tables summarize the HWE, MAF, and missing rates of each SNP. Targeted imputation was performed in the validation set when SNP information could not be confirmed as significant in the discovery set. Imputation was performed as follows: genotypes were pre-phased using SHAPEIT2, imputed with IMPUTE2, and analyzed using 1000 genome phase 3 haplotypes as the reference panel.
Statistical analysis
SNPs associated with kidney disease-related outcomes, including BUN serum creatinine, GFR, and uric acid levels, were identified with multiple linear or logistical regression methods with adjustments for age, sex, diabetes mellitus, hypertension, and BMI effects. Principal component (PC) scores were estimated with the EIGENSTRAT approach to adjust the population substructure, and the first five PC scores were also included as covariates [11]. A total of 345,072 SNPs that passed the quality control assessment were used for the genome-wide association study. Distributions of normality for BUN, serum creatinine, GFR, and uric acid levels were evaluated with a histogram and Kolmogorov-Smirnov test. Because the continuous variables did not show normal distribution, the characteristics of the continuous variables were displayed using median values and interquartile ranges. Categorical variables were expressed as frequencies or percentages. The R software package (version 3.1.1., R development Core Team; R Foundation for Statistical Computing, Vienna, Austria) was used for statistical analysis and to draw the Manhattan–log10 plots. Analysis results were verified using discovery and validation sets. The discovery set comprised 7,064 of the participants included in this study. Significant SNPs (P < 1.45 × 10−7, value derived from the 345,072 QC-qualified SNPs and Bonferroni correction) were tested in the validation cohort samples. BUN, serum creatinine, and GFR validation was performed using results from participants of the genome-wide association study of the Korea Association Resource (KARE), and uric acid validation was performed using results from participants of the Health Examinee shared control (HEXA) study. The KARE is a prospective cohort designed to identify risk factors for major chronic diseases in Koreans, including diabetes and hypertension [12–14]. The KARE cohort consists of 10,038 adults (aged 40–69) who are representative samples of residents in two cities (Ansung and Ansan) in South Korea. Data obtained from physical examinations and laboratory tests have been collected since 2001, and follow-up studies have been conducted every two years. Genetic testing results from 6,509 participants in the third phase of the KARE cohort study were used to validate BUN, serum creatinine, and GFR. HEXA is a large-scale cohort designed for the general population to identify environmental genetic factors for major chronic diseases in Koreans. Since 2004, adults 40–70 years of age representing the general population have been recruited from health screenings and medical institutions. The cohort includes data from health checkups and epidemiological surveys as well as follow-up data collected since 2007. Approximately 20 medical institutions exist in Korea nationwide, and approximately 30,000 new participants are enrolled in the study every year. Currently, data from approximately 173,300 adult participants are collected. For the validation of uric acid, we used genetic test results from 3,703 participants in the HEXA cohort study. Validation P values less than 0.05 were considered significant. We grouped significant SNPs by the linkage disequilibrium (LD) and D’ values, and the graphs were generated using Haploview 4.2. software (S1 File, Figure A in S1 File for BUN in chromosome 3, Figure B in S1 File for uric acid in chromosome 4, Figure C in S1 File for uric acid in chromosome 11, Figure D in S1 File for serum creatinine in chromosome 12, Figure E in S1 File for GFR in chromosome 17, Figure F in S1 File for BUN in chromosome 18).
Results
Participant characteristics
Clinical and demographic characteristics of the discovery cohort participants are shown in Table 1. A total of 7,064 participants were enrolled in this study. Median age was 51 years old (interquartile range, IQR 44–56), and male was 58.1%. Median GFR was 90.2 (IQR 81.2–100.9) ml/min/1.73m2, and, 47 patients (0.67% of whole participants) had advanced kidney disease (GFR below 60 ml/min/1.73m2). Genetic information of the whole participants was all included in the discovery samples.
Table 1. Demographic and clinical characteristics of participants.
| Whole participants (N = 7,064) | |
|---|---|
| Age (years) | 51.0 (44.0–56.0) |
| Sex (male) | 4104 (58.1%) |
| Weight (Kg) | 64.4 (55.2–72.7) |
| Body mass index | 23.0 (21.0–25.0) |
| Hypertension | 1659 (23.6%) (N = 7,034) |
| Diabetes mellitus | 557 (7.9%) (N = 7,063) |
| Systolic blood pressure (mmHg) | 114 (106–125) |
| Diastolic blood pressure (mmHg) | 75 (69–83) |
| White blood cells (/mm3) | 5,100 (4,300–6,100) |
| Hemoglobin (g/dl) | 14.4 (13.4–15.4) |
| Calcium (mg/dl) | 9.3 (9.0–9.5) |
| Phosphorus (mg/dl) | 3.5 (3.2–3.8) |
| Glucose (mg/dl) | 95.0 (90.0–103.0) |
| BUN (mg/dl) | 14.0 (12.0–16.0) |
| Creatinine (mg/dl) | 0.82 (0.68–0.94) |
| GFR (ml/min/1.73m2) | 90.2 (81.2–100.9) |
| Uric acid (mg/dl) | 5.4 (4.4–6.4) |
| Cholesterol (mg/dl) | 192.0 (169.0–215.0) |
| Protein (mg/dl) | 7.3 (7.0–7.6) |
| Albumin (mg/dl) | 4.6 (4.4–4.7) |
| Bilirubin (mg/dl) | 0.9 (0.7–1.2) |
| Alkaline phosphatase (mg/dl) | 51.0 (43.0–62.0) |
| LDL cholesterol (mg/dl) | 119.0 (99.0–141.0) |
| AST (IU/ml) | 21.0 (18.0–26.0) |
| ALT (IU/ml) | 16.0 (14.0–27.0) |
| HbA1c (%) | 5.5 (5.4–5.8) |
GFR, glomerular filtration rate; LDL, low-density lipoprotein
Genome-wide association study of BUN, creatinine, GFR, and uric acid
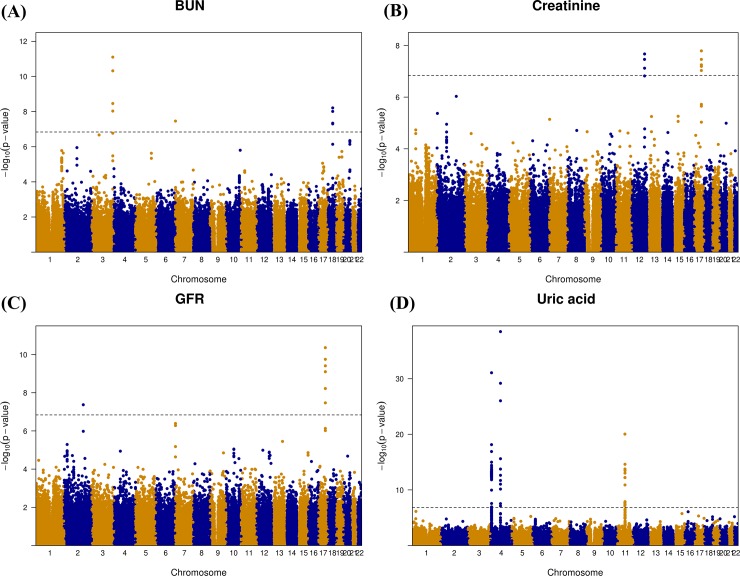
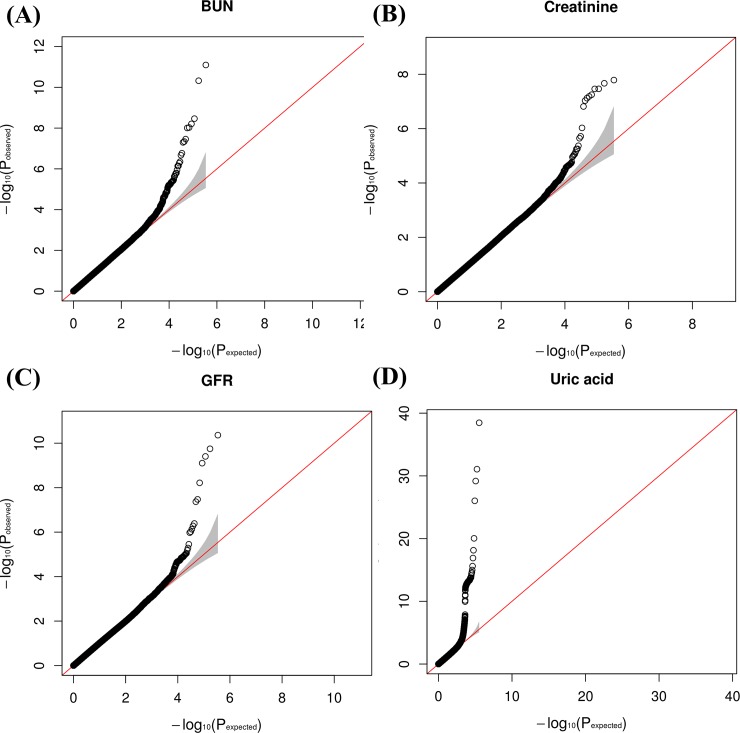
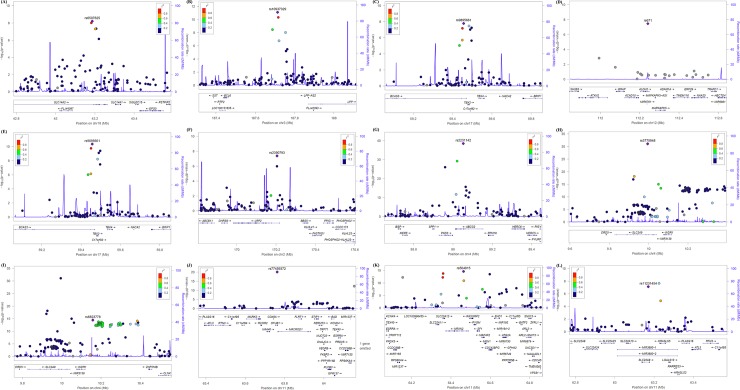
Results of the genome-wide association study on BUN, creatinine, GFR, and, uric acid across the discovery samples are depicted using a Manhattan plot in Fig 1. The Manhattan plot was drawn using data from the discovery set. Genetic loci significantly associated (P < 1.45 × 10−7 in the discovery set) with BUN were found on chromosomes 3, 7, and 18, and those significantly associated with serum creatinine were found on chromosomes 12, and 17. Genetic loci significantly associated with GFR were found on chromosomes 2 and 17. Genetic loci significantly associated with uric acid levels were found on chromosomes 4 and 11. In addition, the distribution statuses of the observed versus expected P values are described using quantile-quantile (QQ) plots in Fig 2. The QQ plots showed good adherence to null expectations. Studies on specific genetic inflation factors did not show substantial inflation of the test statistics on these traits. The calculated values (-log10 P values) are shown according to genomic position using a regional plot chart (Fig 3), and P values were obtained from the discovery set. Among the SNPs, the most significant SNP with the lowest P value is colored purple. On chromosome 18, rs6507625 in SLC14A2 was identified as the most significant SNP for BUN (P = 6.20 × 10−9). On chromosome 3, rs10937329 in an intergenic locus was identified as the most significant SNP for BUN (P = 8.00 × 10−12). On chromosome 17, rs9895661 in BCAS3 was identified as the most significant SNP for creatinine and GFR (P = 1.63 × 10−8 for creatinine, P = 4.34 × 10−11 for GFR). On chromosome 17, rs757608 in C17orf82 was also identified as significant SNP for both creatinine and GFR (P = 5.65 × 10−8 for creatinine, P = 3.93 × 10−10 for GFR). On chromosome 12, rs671 in ALDH2 was identified as the most significant SNP for creatinine (P = 3.45 × 10−8). On chromosome 2, rs2390793 in LRP2 was identified as the most significant SNP for GFR (P = 4.28 × 10−8). On chromosome 4, rs2231142 in ABCG2 (P = 3.38 × 10−39) and rs3775948 in SLC2A9 (P = 8.59 × 10−32) were identified as the most significant SNPs for uric acid. On chromosome 11, rs77459372 in OTUB1 was identified as the most significant SNP for uric acid (P = 9.12 × 10−21).
Fig 1.
Genome-wide association analysis -log10 (P-value) vs. genomic position plots (Manhattan plot) for BUN (A), serum creatinine (B), GFR (C), and uric acid (D) in the discovery cohort. Genetic loci significantly associated (P < 1.45 × 10−7 in the discovery set) with BUN were found on chromosomes 3, 7, and 18. Genetic loci significantly associated with serum creatinine were found on chromosomes 12 and 17. Genetic loci significantly associated with GFR were found on chromosomes 2 and 17. Genetic loci significantly associated with uric acid were found on chromosomes 4 and 11.
Fig 2.
Quantile-quantile plots of the association test results (expected vs. observed -log10 (P-value)) for BUN (A), serum creatinine (B), GFR (C), and uric acid (D) in the discovery cohort. The red line shows the expected distribution under the null hypothesis of no association at any locus, and the gray area shows the 95% confidence limits of the null hypothesis distribution.
Fig 3. Genetic architecture of genome-wide susceptibility loci significantly associated with kidney disease-related traits in the discovery cohorts.
(A) SLC14A2 on chromosome 18 for BUN. (B): Null intergenic region on chromosome 3 for BUN. (C) BCAS3 on chromosome 17 for creatinine. (D) ALDH2 and HECTD4 on chromosome 12 for creatinine. (E) BCAS3 on chromosome 17 for GFR. (F) LRP2 on chromosome 2 for GFR. (G) ABCG2 on chromosome 4 for uric acid. (H): SLC2A9 on chromosome 4 for uric acid. (I) intergenic region on chromosome 4 for uric acid. (J) OTUB1 on chromosome 11 for uric acid. (K) NRXN2/SLC22A12 on chromosome 11 for uric acid. (L) SLC22A9 on chromosome 11 for uric acid. The calculated -log10 P values are shown according to genomic position. P values were obtained from the discovery set. Among the SNPs, the most significant SNP with the lowest P value is colored purple. LD values (based on the HapMap CEU sample) are displayed as different colors is marked in colors: red (r2 to top SNP 0.8–0.0), orange (0.4–0.6), green (0.4–0.6), sky blue (0.2–0.4), and dark blue (<0.2). Gene annotations are based on Build 36. The directions of the arrows indicate the direction of transcription.
The most significant SNPs at each genetic locus associated with kidney disease-related traits are summarized in Table 2. We detected 4 SNPs on chromosome 18 (SLC14A2), 4 SNPs on chromosome 3 (intergenic loci), and 1 SNP on chromosome 7 (UNCX) associated with BUN in the discovery set (Tables 2 and 3). After validation set analysis, 4 SNPs on chromosome 18 (SLC14A2) and 4 SNPs on chromosome 3 (intergenic loci) still showed a significant association with BUN. The top SNPs in SCL14A2 on chromosome 18 and in intergenic loci on chromosome 3 were rs6507625 (P = 6.20 × 10−9 in the discovery set, P = 3.70 × 10−4 in the validation set) and rs10937329 (P = 8.00 × 10−12 in the discovery set, P = 2.11 × 10−9 in the validation set), respectively. rs11710227 in an intergenic region on chromosome 3 is a newly discovered SNP that showed significant association with BUN.
Table 2. Lead SNPs in each genetic loci associated with kidney function-related traits.
| ` | Discovery set | Validation set | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Traits | rsIDα | Chromosome | Position (base pair) | Gene | A1 | β(SE) | P | β(SE) | P |
| BUN | rs6507625* | 18 | 43186842 | SLC14A2 | G/A | -0.4115(0.0714) | 6.20 × 10−9 | -0.3318(0.0983) | 3.70 × 10−4 |
| rs10937329* | 3 | 187713718 | Intergenic | A/T | -0.4044(0.0590) | 8.00 × 10−12 | -0.4695(0.0798) | 2.11 × 10−9 | |
| Creatinine | rs9895661* | 17 | 59456589 | BCAS3 | C/T | 0.0121(0.0021) | 1.63 × 10−8 | 0.0098(0.0045) | 1.38 × 10−2 |
| rs757608* | 17 | 59497277 | C17orf82 | A/G | 0.0130(0.0024) | 5.65 × 10−8 | 0.0109(0.0043) | 5.34 × 10−3 | |
| rs671* | 12 | 112241766 | ALDH2 | A/G | 0.0158(0.0029) | 3.45 × 10−8 | 0.0116(0.0053) | 1.41 × 10−2 | |
| GFR | rs9895661* | 17 | 59456589 | BCAS3 | C/T | -1.705(0.2583) | 4.34 × 10−11 | -0.4283(0.2478) | 4.20 × 10−2 |
| rs757608* | 17 | 59497277 | C17orf82/TBX2 | A/G | -1.800(0.2873) | 3.93 × 10−10 | -0.6187(0.2064) | 1.37 × 10−3 | |
| rs2390793* | 2 | 170205123 | LRP2 | T/C | 1.772(0.3231) | 4.28 × 10−8 | 0.9836(0.2326) | 1.19 × 10−5 | |
| Uric acid | rs2231142* | 4 | 89052323 | ABCG2/PKD2 | T/G | 0.2804(0.0213) | 3.38 × 10−39 | 0.2031(0.0286) | 7.49 × 10−13 |
| rs3114018* | 4 | 89064581 | ABCG2 | A/C | -0.1648(0.0201) | 2.46 × 10−16 | -0.1548(0.0267) | 3.62 × 10−9 | |
| rs12511059* | 4 | 89126193 | ABCG2 | T/C | -0.1081(0.0201) | 7.84 × 10−8 | -0.0912(0.0493) | 3.22 × 10−2 | |
| rs3775948* | 4 | 9995182 | SLC2A9 | G/C | -0.2208(0.0187) | 8.59 × 10−32 | -0.1936(0.0259) | 4.55 × 10−14 | |
| rs13129697* | 4 | 9926967 | SLC2A9 | G/T | -0.1502(0.0187) | 1.03 × 10−15 | -0.1318(0.0254) | 1.14 × 10−7 | |
| rs59420943* | 4 | 10384278 | Intergenic | T/C | 0.1473(0.0189) | 8.02 × 10−15 | 0.1153(0.0262) | 5.60 × 10−6 | |
| rs6839820* | 4 | 10296114 | Intergenic | C/T | -0.1424(0.0189) | 4.73 × 10−14 | -0.0942(0.0252) | 9.55 × 10−5 | |
| rs6823778* | 4 | 10158163 | Intergenic | C/T | -0.1481(0.0188) | 3.79 × 10−15 | -0.1061(0.0254) | 1.52 × 10−5 | |
| rs77459372* | 11 | 63762330 | OTUB1 | A/G | -0.3815(0.0407) | 9.12 × 10−21 | -0.5629(0.209) | 3.56 × 10−3 | |
| rs55975541* | 11 | 64597201 | CDC42BPG | A/G | -0.1858(0.0245) | 3.49 × 10−14 | -0.238(0.0633) | 8.61 × 10−5 | |
| rs504915* | 11 | 64464085 | NRXN2/SLC22A12 | A/T | -0.179(0.0226) | 2.45 × 10−15 | -0.1367(0.0306) | 3.96 × 10−6 | |
| rs79382056* | 11 | 64154676 | RPS6KA4 | C/T | -0.2361(0.0327) | 6.02 × 10−13 | -0.1565(0.0829) | 2.96 × 10−2 | |
| rs11231454* | 11 | 63170735 | SLC22A9 | T/C | -0.2221(0.0413) | 7.48 × 10−8 | -0.1035(0.051) | 2.12 × 10−2 | |
| rs10897526* | 11 | 64559898 | MAP4K2 | T/C | -0.1222(0.0222) | 3.67 × 10−8 | -0.0879(0.036) | 7.36 × 10−3 |
*Lead SNP in each genetic loci
Table 3. Loci associated with kidney function-related traits (blood urea nitrogen).
| ` | Discovery Set | Validation Set | ||||||
|---|---|---|---|---|---|---|---|---|
| rsIDα | Chromosome | Position (base pair) | Gene | A1/A2 | β(SE) | P | β(SE) | P |
| rs6507625* | 18 | 43186842 | SLC14A2 | G/A | -0.4115(0.0714) | 6.20 × 10−9 | -0.3318(0.0983) | 3.70 × 10−4 |
| rs1825475 | 18 | 43182006 | SLC14A2 | A/G | -0.4106(0.0715) | 9.85 × 10−9 | -0.3339(0.0983) | 3.43 × 10−4 |
| rs1484873 | 18 | 43206985 | SLC14A2 | A/G | -0.3982(0.0728) | 4.57 × 10−8 | -0.3232(0.1057) | 1.12 × 10−3 |
| rs7232775 | 18 | 43202404 | SLC14A2 | C/T | -0.3877(0.0711) | 5.02 × 10−8 | -0.3255(0.0980) | 4.52 × 10−4 |
| rs10937329* | 3 | 187713718 | Intergenic | A/T | -0.4044(0.0590) | 8.00 × 10−12 | -0.4695(0.0798) | 2.11 × 10−9 |
| rs4686914 | 3 | 187717540 | Intergenic | T/C | -0.3891(0.0591) | 4.74 × 10−11 | -0.4716(0.0798) | 1.78 × 10−9 |
| rs16862782 | 3 | 187687890 | Intergenic | A/C | -0.4411(0.0746) | 3.44 × 10−9 | -0.5377(0.1033) | 9.90 × 10−8 |
| rs11710227† | 3 | 187753995 | Intergenic | G/A | -0.3512(0.0611) | 9.34 × 10−9 | -0.3683(0.0844) | 6.53 × 10−6 |
*Lead SNP in each genetic loci
†Newly discovered SNP.
Five SNPs on chromosome 17 (BCAS3, C17orf82/TBX2) and 3 SNPs on chromosome 12 (HECTD4, ALDH2) significantly associated with serum creatinine levels were found in the discovery set. During validation, 4 SNPs (2 on BCAS3 and 2 on C17orf82) on chromosome 17 and 2 SNP on chromosome 12 (ALDH2/HECTD4) showed a significant association with serum creatinine levels (Table 4). The lead SNPs in BCAS3 and C17orf82 on chromosome 17 and ALDH2 on chromosome 12 were rs9895661, rs757608, and rs671, respectively.
Table 4. Loci associated with kidney function-related traits (serum creatinine).
| Discovery Set | Validation Set | |||||||
|---|---|---|---|---|---|---|---|---|
| rsIDα | Chromosome | Position (base pair) | Gene | A1/A2 | β(SE) | P | β(SE) | P |
| rs9895661* | 17 | 59456589 | BCAS3 | C/T | 0.0121(0.0021) | 1.63 × 10−8 | 0.0098(0.0045) | 1.38 × 10−2 |
| rs9905274 | 17 | 59450441 | BCAS3 | T/C | 0.0117(0.0022) | 6.52 × 10−8 | 0.0094(0.0047) | 2.21 × 10−2 |
| rs757608* | 17 | 59497277 | C17orf82 | A/G | 0.0130(0.0024) | 5.65 × 10−8 | 0.0109(0.0043) | 5.34 × 10−3 |
| rs9907379 | 17 | 59489893 | C17orf82 | T/C | 0.0128(0.0024) | 9.33 × 10−8 | 0.0101(0.0043) | 9.96 × 10−3 |
| rs671* | 12 | 112241766 | ALDH2 | A/G | 0.0158(0.0029) | 3.45 × 10−8 | 0.0116(0.0053) | 1.41 × 10−2 |
| rs2074356 | 12 | 112645401 | HECTD4 | A/G | 0.0159(0.0030) | 7.58 × 10−8 | 0.0135(0.0053) | 5.17 × 10−3 |
*Lead SNP in each genetic loci
Six SNPs on chromosome 17 (BCAS3, C17orf82/TBX2) and 1 SNP on chromosome 2 (LRP2) significantly associated with GFR were found in the discovery and validation sets (Table 5). The lead SNPs in BCAS3 and C17orf82/TBX2 on chromosome 17 and LRP2 on chromosome 2 were rs9895661, rs757608 and rs2390793, respectively. Comparing significant genetic loci associated with serum creatinine levels and GFR showed that 2 genetic loci (BCAS3 and C17orf82) were simultaneously associated with both traits. A genetic locus in ALDH2 on chromosome 12 was associated with only serum creatinine levels and not with GFR. Genetic loci in LRP2 on chromosome 2 was associated with only GFR and not with serum creatinine levels.
Table 5. Loci associated with kidney function-related traits (glomerular filtration rate).
| Discovery Set | Validation Set | |||||||
|---|---|---|---|---|---|---|---|---|
| rsIDα | Chromosome | Position (base pair) | Gene | A1/A2 | β(SE) | P | β(SE) | P |
| rs9895661* | 17 | 59456589 | BCAS3 | C/T | -1.705(0.2583) | 4.34 × 10−11 | -0.4283(0.2478) | 4.20 × 10−2 |
| rs9905274 | 17 | 59450441 | BCAS3 | T/C | -1.656(0.2592) | 1.78 × 10−10 | -0.4848(0.2517) | 2.71 × 10−2 |
| rs757608* | 17 | 59497277 | C17orf82 | A/G | -1.800(0.2873) | 3.93 × 10−10 | -0.6187(0.2064) | 1.37 × 10−3 |
| rs9907379 | 17 | 59489893 | C17orf82 | T/C | -1.768(0.2872) | 7.90 × 10−10 | -0.5381(0.2090) | 5.04 × 10−3 |
| rs8068318 | 17 | 59483766 | TBX2 | T/C | 1.510(0.2593) | 6.05 × 10−9 | 0.3816(0.1865) | 2.04 × 10−2 |
| rs2079795 | 17 | 59496649 | C17orf82 | T/C | -1.527(0.2763) | 3.35 × 10−8 | -0.5887(0.1947) | 1.25 × 10−3 |
| rs2390793* | 2 | 170205123 | LRP2 | T/C | 1.772(0.3231) | 4.28 × 10−8 | 0.9836(0.2326) | 1.19 × 10−5 |
*Lead SNP in each genetic loci
Fourteen genetic loci (3 in ABCG2/PKD2, 2 in SLC2A9, 3 in intergenic regions on chromosome 4; OTUB1, NRXN2/SLC22A12, CDC42BPG, RPS6KA4, SLC22A9, and MAP4K2 on chromosome 11) and 84 SNPs associated with uric acid levels. According to uric acid, 74 SNPs were identified on chromosome 4 (9 in ABCG2, 2 in PKD2, 7 in SLC2A9, 56 in intergenic region) and 10 SNPs were identified on chromosome 11 (1 in OTUB1, 2 in NRXN2, 1 in CDC42BPG, 2 in SLC22A12, 1 in RPS6KA4, 1 in SLC22A2, 1 in MAP4K2, and 1 in intergenic region) (Table 6). Using linkage disequilibrium (LD) analysis, genetic loci associated with uric acid levels were categorized (Figure B and Figure C in S1 File). On chromosome 4, 8 genetic loci were associated with uric acid levels, and the lead SNPs were rs2231142 in ABCG2/PKD2 (P = 3.38 × 10−39); rs3114018 in ABCG2 (P = 2.46 × 10−16); rs12511059 in ABCG2 (P = 7.84 × 10−8); rs3775948 in SLC2A9 (P = 8.59 × 10−32); rs13129697 in SLC2A9 (P = 1.03 × 10−15); and rs6839820, rs59420943, and rs6823778 in intergenic regions. On chromosome 11, 6 genetic loci were associated with uric acid levels, and the lead SNPs were rs77459372 in OTUB1, rs504915 in NRXN2/SLC22A12, rs55975541 in CDC42BPG, rs79382056 in RPS6KA4, rs11231454 in SLC22A9, and rs10897526 in MAP4K2.
Table 6. Loci associated with kidney function-related traits (uric acid).
| Discovery Set | Validation Set | |||||||
|---|---|---|---|---|---|---|---|---|
| rsIDα | Chromosome | Position (base pair) |
Gene | A1/A2 | β(SE) | P | β(SE) | P |
| rs2231142* | 4 | 89052323 | ABCG2 | T/G | 0.2804(0.0213) | 3.38 × 10−39 | 0.2031(0.0286) | 7.49 × 10−13 |
| rs4148157 | 4 | 89020934 | ABCG2 | A/G | 0.2527(0.0221) | 6.64 × 10−30 | 0.1981(0.0296) | 1.26 × 10−11 |
| rs2231164 | 4 | 89015857 | ABCG2 | C/T | 0.1344(0.0191) | 1.98 × 10−12 | 0.0832(0.0257) | 6.17 × 10−4 |
| rs2725220 | 4 | 88959922 | PKD2 | C/G | 0.2383(0.0222) | 9.40 × 10−27 | 0.1831(0.0296) | 3.47 × 10−10 |
| rs2725201 | 4 | 88999306 | PKD2 | T/G | 0.1050(0.0189) | 2.95 × 10−8 | 0.1558(0.0394) | 3.96 × 10−5 |
| rs3114018* | 4 | 89064581 | ABCG2 | A/C | -0.1648(0.0201) | 2.46 × 10−16 | -0.1548(0.0267) | 3.62 × 10−9 |
| rs17731799 | 4 | 89068455 | ABCG2 | G/T | -0.1598(0.0208) | 1.77 × 10−14 | -0.1304(0.0277) | 1.35 × 10−6 |
| rs3114020 | 4 | 89083666 | ABCG2 | T/C | -0.1534(0.0209) | 2.33 × 10−13 | -0.1380(0.0278) | 3.72 × 10−7 |
| rs3109823 | 4 | 89064602 | ABCG2 | C/T | -0.1781(0.0261) | 9.30 × 10−12 | -0.1012(0.0337) | 1.34 × 10−3 |
| rs2622604 | 4 | 89078924 | ABCG2 | T/C | -0.1729(0.0265) | 7.07 × 10−11 | -0.0955(0.034) | 2.48 × 10−3 |
| rs12511059* | 4 | 89126193 | ABCG2 | T/C | -0.1081(0.0201) | 7.84 × 10−8 | -0.0912(0.0493) | 3.22 × 10−2 |
| rs3775948* | 4 | 9995182 | SLC2A9 | G/C | -0.2208(0.0187) | 8.59 × 10−32 | -0.1936(0.0259) | 4.55 × 10−14 |
| rs733175 | 4 | 10050141 | SLC2A9 | C/T | -0.1502(0.0187) | 1.03 × 10−15 | -0.1318(0.0254) | 1.14 × 10−7 |
| rs6834555 | 4 | 10062326 | SLC2A9 | G/A | -0.1415(0.0187) | 4.30 × 10−14 | -0.129(0.0252) | 1.70 × 10−7 |
| rs62295971 | 4 | 9978142 | SLC2A9 | A/G | 0.1216(0.0188) | 1.11 × 10−10 | 0.1188(0.0261) | 2.65 × 10−6 |
| rs13129697* | 4 | 9926967 | SLC2A9 | G/T | -0.1667(0.0187) | 7.18 × 10−19 | -0.1406(0.0259) | 3.15 × 10−8 |
| rs3733591 | 4 | 9922130 | SLC2A9 | C/T | 0.1756(0.0205) | 1.27 × 10−17 | 0.1545(0.0276) | 1.20 × 10−8 |
| rs4292327 | 4 | 9943700 | SLC2A9 | A/G | 0.1991(0.0376) | 1.25 × 10−7 | 0.1103(0.0494) | 1.28 × 10−2 |
| rs59420943* | 4 | 10384278 | Intergenic | T/C | 0.1473(0.0189) | 8.02 × 10−15 | 0.1153(0.0262) | 5.60 × 10−6 |
| rs9990427 | 4 | 10388313 | Intergenic | A/G | -0.148(0.0195) | 3.63 × 10−14 | -0.1355(0.0264) | 1.44 × 10−7 |
| rs11732092 | 4 | 10377405 | Intergenic | T/G | -0.1402(0.0189) | 1.31 × 10−13 | -0.1037(0.0253) | 2.17 × 10−5 |
| rs1544599 | 4 | 10349168 | Intergenic | G/A | -0.1393(0.0188) | 1.38 × 10−13 | -0.0972(0.0253) | 6.02 × 10−5 |
| rs9990701 | 4 | 10388610 | Intergenic | A/G | -0.1371(0.0188) | 3.55 × 10−13 | -0.1239(0.0273) | 2.93 × 10−6 |
| rs6839820* | 4 | 10296114 | Intergenic | C/T | -0.1424(0.0189) | 4.73 × 10−14 | -0.0942(0.0252) | 9.55 × 10−5 |
| rs7670709 | 4 | 10288932 | Intergenic | C/T | -0.1405(0.0188) | 8.53 × 10−14 | -0.0935(0.0252) | 1.06 × 10−4 |
| rs6449450 | 4 | 10311887 | Intergenic | A/G | -0.1462(0.0196) | 9.33 × 10−14 | -0.1365(0.0264) | 1.17 × 10−7 |
| rs11945358 | 4 | 10287559 | Intergenic | G/T | -0.1396(0.0188) | 1.14 × 10−13 | -0.0934(0.0252) | 1.07 × 10−4 |
| rs4697744 | 4 | 10298147 | Intergenic | A/G | -0.1402(0.0189) | 1.20 × 10−13 | -0.0939(0.0252) | 9.82 × 10−5 |
| rs6856707 | 4 | 10297330 | Intergenic | A/G | -0.1386(0.0189) | 2.21 × 10−13 | -0.0942(0.0252) | 9.55 × 10−5 |
| rs757628 | 4 | 10290297 | Intergenic | T/C | -0.1387(0.0189) | 2.22 × 10−13 | -0.0944(0.0252) | 9.19 × 10−5 |
| rs10014800 | 4 | 10302493 | Intergenic | G/A | -0.1378(0.0189) | 3.18 × 10−13 | -0.0948(0.0253) | 9.13 × 10−5 |
| rs4698017 | 4 | 10298094 | Intergenic | G/A | -0.1372(0.0189) | 3.71 × 10−13 | -0.0939(0.0252) | 9.88 × 10−5 |
| rs10939818 | 4 | 10286962 | Intergenic | G/T | -0.1362(0.0188) | 4.92 × 10−13 | -0.0889(0.0259) | 3.08 × 10−4 |
| rs9291683 | 4 | 10324160 | Intergenic | A/G | 0.1119(0.0201) | 2.74 × 10−8 | 0.0962(0.027) | 1.84 × 10−4 |
| rs6823778* | 4 | 10158163 | Intergenic | C/T | -0.1481(0.0188) | 3.79 × 10−15 | -0.1061(0.0254) | 1.52 × 10−5 |
| rs11724092 | 4 | 10186604 | Intergenic | T/C | -0.1445(0.0188) | 1.68 × 10−14 | -0.0906(0.0253) | 1.72 × 10−4 |
| rs11723976 | 4 | 10186251 | Intergenic | T/C | -0.1442(0.0188) | 1.88 × 10−14 | -0.0906(0.0253) | 1.72 × 10−4 |
| rs4697972 | 4 | 10201503 | Intergenic | C/A | -0.1435(0.0188) | 2.37 × 10−14 | -0.0904(0.0252) | 1.69 × 10−4 |
| rs4697973 | 4 | 10203152 | Intergenic | G/A | -0.1418(0.0188) | 4.78 × 10−14 | -0.0904(0.0252) | 1.69 × 10−4 |
| rs2159865 | 4 | 10193287 | Intergenic | T/G | -0.1422(0.0188) | 4.84 × 10−14 | -0.0718(0.0261) | 2.97 × 10−3 |
| rs55878266 | 4 | 10199948 | Intergenic | C/T | -0.1418(0.0188) | 5.07 × 10−14 | -0.0902(0.0252) | 1.73 × 10−4 |
| rs11734623 | 4 | 10208303 | Intergenic | C/T | -0.1418(0.0188) | 5.09 × 10−14 | -0.0904(0.0252) | 1.69 × 10−4 |
| rs4697962 | 4 | 10188832 | Intergenic | G/A | -0.1419(0.0188) | 5.57 × 10−14 | -0.0919(0.0252) | 1.33 × 10−4 |
| rs2868420 | 4 | 10202997 | Intergenic | G/A | -0.1415(0.0188) | 5.67 × 10−14 | -0.0904(0.0252) | 1.69 × 10−4 |
| rs28496435 | 4 | 10190318 | Intergenic | T/C | -0.1418(0.0188) | 5.97 × 10−14 | -0.0876(0.0253) | 2.71 × 10−4 |
| rs4697974 | 4 | 10205718 | Intergenic | A/G | -0.1411(0.0188) | 6.35 × 10−14 | -0.0904(0.0252) | 1.71 × 10−4 |
| rs2215691 | 4 | 10192108 | Intergenic | C/T | -0.1414(0.0188) | 6.58 × 10−14 | -0.0875(0.0253) | 2.71 × 10−4 |
| rs10000104 | 4 | 10191766 | Intergenic | G/A | -0.1413(0.0188) | 6.59 × 10−14 | -0.0884(0.0253) | 2.37 × 10−4 |
| rs6836606 | 4 | 10198086 | Intergenic | G/A | -0.1408(0.0188) | 7.10 × 10−14 | -0.0903(0.0252) | 1.70 × 10−4 |
| rs6449351 | 4 | 10192744 | Intergenic | T/C | -0.1408(0.0188) | 8.00 × 10−14 | -0.0851(0.0254) | 4.07 × 10−4 |
| rs4697963 | 4 | 10189483 | Intergenic | T/C | -0.1411(0.0189) | 8.29 × 10−14 | -0.0894(0.0253) | 2.09 × 10−4 |
| rs11726987 | 4 | 10190792 | Intergenic | C/T | -0.1408(0.0188) | 8.64 × 10−14 | -0.0876(0.0253) | 2.71 × 10−4 |
| rs6826185 | 4 | 10208656 | Intergenic | G/A | -0.1396(0.0188) | 1.13 × 10−13 | -0.0905(0.0253) | 1.81 × 10−4 |
| rs55775442 | 4 | 10200204 | Intergenic | T/G | -0.1422(0.0191) | 1.22 × 10−13 | -0.0902(0.0252) | 1.73 × 10−4 |
| rs6832085 | 4 | 10194270 | Intergenic | T/C | -0.1396(0.0188) | 1.26 × 10−13 | -0.0778(0.0263) | 1.55 × 10−3 |
| rs11726996 | 4 | 10199139 | Intergenic | G/T | -0.1411(0.019) | 1.32 × 10−13 | -0.0902(0.0252) | 1.73 × 10−4 |
| rs7690319 | 4 | 10207061 | Intergenic | T/C | -0.1394(0.0188) | 1.37 × 10−13 | -0.0903(0.0252) | 1.75 × 10−4 |
| rs10025980 | 4 | 10185799 | Intergenic | G/A | -0.1391(0.0188) | 1.54 × 10−13 | -0.0906(0.0253) | 1.72 × 10−4 |
| rs62285986 | 4 | 10189213 | Intergenic | A/G | -0.1393(0.0188) | 1.57 × 10−13 | -0.0942(0.0252) | 9.37 × 10−5 |
| rs4697726 | 4 | 10187395 | Intergenic | T/C | -0.1399(0.0189) | 1.61 × 10−13 | -0.0836(0.0259) | 6.35 × 10−4 |
| rs66769576 | 4 | 10197663 | Intergenic | G/T | -0.139(0.0188) | 1.76 × 10−13 | -0.0902(0.0252) | 1.73 × 10−4 |
| rs11724760 | 4 | 10254162 | Intergenic | C/T | -0.1393(0.0189) | 1.83 × 10−13 | -0.0929(0.0253) | 1.20 × 10−4 |
| rs56391253 | 4 | 10187580 | Intergenic | G/A | -0.1385(0.0188) | 2.04 × 10−13 | -0.0847(0.0258) | 5.15 × 10−4 |
| rs4697731 | 4 | 10200718 | Intergenic | G/A | -0.1388(0.0189) | 2.11 × 10−13 | -0.0904(0.0252) | 1.68 × 10−4 |
| rs1860895 | 4 | 10250779 | Intergenic | C/T | -0.1378(0.0188) | 2.76 × 10−13 | -0.0932(0.0253) | 1.16 × 10−4 |
| rs11735623 | 4 | 10251925 | Intergenic | G/T | -0.1375(0.0188) | 3.01 × 10−13 | -0.0931(0.0253) | 1.18 × 10−4 |
| rs10017447 | 4 | 10175536 | Intergenic | C/A | -0.1378(0.0189) | 3.08 × 10−13 | -0.0976(0.0252) | 5.59 × 10−5 |
| rs887734 | 4 | 10182913 | Intergenic | T/C | -0.1371(0.0189) | 4.00 × 10−13 | -0.089(0.0254) | 2.27 × 10−4 |
| rs4697961 | 4 | 10187373 | Intergenic | G/A | -0.1375(0.019) | 4.39 × 10−13 | -0.0841(0.0259) | 5.89 × 10−4 |
| rs1990469 | 4 | 10201652 | Intergenic | G/T | -0.1383(0.0191) | 4.78 × 10−13 | -0.0904(0.0252) | 1.69 × 10−4 |
| rs4697950 | 4 | 10171644 | Intergenic | G/T | -0.1361(0.0188) | 5.00 × 10−13 | -0.099(0.0252) | 4.42 × 10−5 |
| rs4697724 | 4 | 10177818 | Intergenic | C/T | -0.1358(0.0189) | 6.66 × 10−13 | -0.0935(0.0252) | 1.03 × 10−4 |
| rs10026434 | 4 | 10208128 | Intergenic | C/T | -0.1345(0.0188) | 8.27 × 10−13 | -0.0904(0.0252) | 1.69 × 10−4 |
| rs9990501 | 4 | 10204593 | Intergenic | A/G | -0.1318(0.0186) | 1.46 × 10−12 | -0.0896(0.0248) | 1.50 × 10−4 |
| rs77459372* | 11 | 63762330 | OTUB1 | A/G | -0.3815(0.0407) | 9.12 × 10−21 | -0.5629(0.209) | 3.56 × 10−3 |
| rs55975541* | 11 | 64597201 | CDC42BPG | A/G | -0.1858(0.0245) | 3.49 × 10−14 | -0.238(0.0633) | 8.61 × 10−5 |
| rs504915* | 11 | 64464085 | NRXN2 | A/T | -0.179(0.0226) | 2.45 × 10−15 | -0.1367(0.0306) | 3.96 × 10−6 |
| rs471618 | 11 | 64465403 | NRXN2 | C/T | 0.1307(0.0193) | 1.29 × 10−11 | 0.1032(0.0257) | 2.93 × 10−5 |
| rs11231825 | 11 | 64360274 | SLC22A12 | C/T | -0.1745(0.0227) | 1.75 × 10−14 | -0.1361(0.0306) | 4.43 × 10−6 |
| rs9734313 | 11 | 64358311 | SLC22A12 | T/C | -0.1654(0.0229) | 5.96 × 10−13 | -0.1365(0.0306) | 4.22 × 10−6 |
| rs505802 | 11 | 64357072 | Intergenic | T/C | -0.1689(0.0226) | 9.49 × 10−14 | -0.1364(0.0306) | 4.30 × 10−6 |
| rs79382056* | 11 | 64154676 | RPS6KA4 | C/T | -0.2361(0.0327) | 6.02 × 10−13 | -0.1565(0.0829) | 2.96 × 10−2 |
| rs11231454* | 11 | 63170735 | SLC22A9 | T/C | -0.2221(0.0413) | 7.48 × 10−8 | -0.1035(0.051) | 2.12 × 10−2 |
| rs10897526* | 11 | 64559898 | MAP4K2 | T/C | -0.1222(0.0222) | 3.67 × 10−8 | -0.0879(0.036) | 7.36 × 10−3 |
*Lead SNP in each genetic loci
Discussion
In this study, we used genome-wide association analyses of discovery and validation populations to identify 6 genetic loci (SLC14A2 on chromosome 18 and intergenic regions on chromosome 3 for BUN; BCAS3 and C17orf82 on chromosome 17, and ALDH2 on chromosome 12 for serum creatinine; BCAS3 and C17orf82/TBX2 on chromosome 17, and LRP2 on chromosome 2 for GFR) that were associated with BUN, serum creatinine, and GFR. rs9895661 in BCAS3 and rs757608 in C17orf82 were simultaneously associated with both serum creatinine and GFR. rs11710227 was identified as a newly discovered SNP in an intergenic region on chromosome 3 that showed significant association with BUN. For uric acid, 8 genetic loci on chromosome 4 (2 in ABCG2, 1 in ABCG2/PKD2, 2 in SLC2A9, and 3 in intergenic regions) and 6 genetic loci on chromosome 11 (OTUB1, RPS6KA4, NRXN2/SLC22A12, CDC42BPG, SLC22A9, MAP4K2) were significantly associated with uric acid levels. Among the 345,072 SNPs that met the clustering quality control criteria, 101 SNPs in 20 genetic loci were related to kidney disease-related traits.
rs6507625 in SLC14A2 on chromosome 18 was the lead SNP associated with BUN. rs6507625 in SLC14A2 was previously reported to be associated with anthropometric parameters, including BMI and waist circumference, and kidney function-related traits, including serum creatinine and GFR [15]. Other 3 SNPs (rs1825475, rs1484873, and rs7232775) in SLC14A2 on chromosome 18 were known to be associated with serum creatinine and GFR [15]. rs1484873 and rs7232775 in SLC14A2 on chromosome 18 were also associated with BUN and hypertension [16,17]. rs10937329 in an intergenic region was the lead SNP on chromosome 3 associated with BUN. rs10937329 was previously proven to be associated with BUN in an analysis of 71,149 Asian populations [18]. In their study, rs10937329 was not related to serum creatinine, GFR, or uric acid levels, and these findings were similar to ours. The SNPs rs11710227, rs16862782, and rs4686914 were identified as novel SNPs on chromosome 3 (intergenic region) that were significantly associated with BUN. Although rs16862782 was reported to be associated with myopia [19], and rs4686914 with metabolic traits [20], the association of these SNP with BUN or other kidney disease-related traits have not been reported. SNPs rs11710227 on chromosome 3 (intergenic region) is a novel SNP that has not been shown to be related to a particular phenotype, and the relationship with BUN was newly revealed in this study.
The SNP rs9895661 in BCAS3 and SNPs rs757608 in C17orf82 on chromosome 17 on chromosome 17 were the top SNPs associated with both serum creatinine and GFR. A genetic locus in BCAS3 on chromosome 17 was previously reported to be associated with serum creatinine and GFR [18,21,22]. Franceschini et al. reported that BCAS3 was associated with albuminuria [23], and rs9895661 in BCAS3 was reported to be associated with height [24,25]. The SNP rs9895661 in BCAS3 was also reported to be associated with CKD [26]. By contrast, Chambers et al. reported that BCAS3 was not associated with CKD but was associated with serum creatinine levels and GFR [21]. The SNP rs671 in ALDH2 on chromosome 12 was also associated with serum creatinine levels but not with GFR. A genetic locus in ALDH2 on chromosome 12 was previously reported to be associated with BUN and serum creatinine but not with GFR [18]. The SNP rs671 in ALDH2 was reported to be associated with metabolic traits, including diabetes mellitus, and blood pressure [27–29]. The SNP rs671 in ALDH2 also affects acute rejection after kidney transplantation and drug metabolism in end-stage renal disease patients [30,31]. C17orf82 was previously reported to be associated with serum creatinine and GFR [21]. The lead SNP rs757608 in C17orf82 on chromosome 17 was reported to be associated with height [24]. The other SNPs in C17orf82/TBX2 (rs9907379, rs8068318, and rs2079795) was also reported to be associated with height [24,25,32–34]. In this study, the relationship between the C17orf82/TBX2 genetic loci on chromosome 17 and GFR has been newly discovered, but this may be due to the relationship between height and GFR. Therefore, in subsequent studies, it is necessary to reconfirm the relevance of GFR by correcting the height factor among other population groups. The SNP rs2390793 in LRP2 on chromosome 2 was associated with GFR but not with serum creatinine levels. A genetic locus in LRP2 was previously reported to be associated with BUN, GFR, and proteinuria [21,35,36]. The SNP rs2390793 in LRP2 was previously reported to be associated with uric acid levels [37].
Uric acid was significantly associated with 84 SNPs in 14 genetic loci on chromosomes 4 (74 SNPs in 8 genetic loci) and 11 (10 SNPs in 6 genetic loci). Five genetic loci (2 in ABCG2, 1 in ABCG2/PKD2, 2 in SLC2A9) and 3 intergenic regions were associated with uric acid on chromosome 4. In ABCG2 on chromosome 4, 9 SNPs were significant. ABCG2 (ATP-binding cassette subfamily G member 2) is a protein-coding gene on chromosome 4. Mutations in ABCG2 are known to be associated with hyperuricemia and the risk of gout [38–40]. The two lead SNPs rs2231142 and rs3114018 in ABCG2 on chromosome 4 was associated with hyperuricemia or gout [41–50]. In the PKD2 gene region, SNP rs2725220 and rs2725201 were associated with uric acid levels. PKD2 is a protein-coding gene at 4q22.1 that encodes a member of the polycystin protein family. Association of the PKD2 gene with uric acid levels was proven in other previous studies [51]. SLC2A9 (solute carrier family 2 member 9) is located at 4p16.1 and encodes a member of the SLC2A facilitative glucose transporter family. The SCL2A9 gene was previously reported to be associated with uric acid levels and CKD progression [52–62]. The two lead SNPs rs3775948 and rs13129697 in SLC2A9 on chromosome 4 was associated with hyperuricemia or gout [4,41,46,48–50,63–71]. The major 3 SNPs (rs6839820, rs59420943, and rs6823778) on the intergenic region of chromosome 4 were also found to be significantly related to uric acid levels in this study; these findings are novel, as they have not been previously reported.
Six genetic loci (OTUB1, NRXN2/SLC22A12, CDC42BPG, RPS6KA4, SLC22A9, and MAP4K2) were associated with uric acid on chromosome 11. The SNPs rs55975541 in CDC42BPG [72], and rs11231825/rs9734313 in SLC22A12/NRXN2 [46,49,50,72–77], and rs10897526 in MAP4K2 [72] on chromosome 4 were previously reported to be associated with hyperuricemia or gout. In general, OTUB1 is known to be associated with the development and metastasis of colorectal cancer, ovarian cancer, and lung cancer, and increased OTUB1 expression is associated with worsening prognosis [78–81]. Using a genome-wide association study, Mells et al. reported that a genetic locus in RPS6KA4 at 11q13 is associated with the development of primary biliary cirrhosis through NF-κB activation [82]. In this study, lead SNPs rs77459372 in OTUB1, rs79382056 in RPS6KA4, and rs11231454 in SLC22A9 on chromosome 11 were associated with uric acid levels, which is also a new investigational finding.
Despite the clinical significance of this study, some limitations do exist. Relatively few patients in advanced kidney disease (N = 47, who showed GFR below 60 ml/min/1.73m2) were enrolled due to the health screening patients being relatively healthy. In this study, researchers could adjust for only age, sex, diabetes mellitus, hypertension, and BMI as covariates for the analysis of genetic mutations associated with kidney disease-related traits, but many other variables could affect kidney disease-related traits.
In conclusion, we found 20 genetic loci and 101 SNPs that were associated with the kidney disease-related traits serum creatinine, BUN, GFR, and uric acid in the Korean population. SNPs rs11710227 on chromosome 3 (intergenic region) associated with BUN is a novel SNP that has not been reported to be related with specific phenotype. In this study, we also found the six novel genetic loci (3 intergenic region in chromosome 4, and OTUB1, RPS6KA4, and SLC22A9 on chromosome 11) associated with uric acid. Studies on genetic mutations have identified genetic risk factors for kidney disease. In addition to clinical findings, such as the degree of proteinuria and kidney biopsy results, results of genetic analysis may be used as risk factors for CKD progression. Because genetic impacts may vary from population to population, additional validation is needed to confirm whether these findings are similar in other populations.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Figure A describes the pairwise linkage disequilibrium for BUN on chromosome 3. Figure B describes the pairwise linkage disequilibrium for uric acid on chromosome 4. Figure C describes the pairwise linkage disequilibrium for uric acid on chromosome 11. Figure D describes the pairwise linkage disequilibrium for serum creatinine on chromosome 12. Figure E describes the pairwise linkage disequilibrium for glomerular filtration rate on chromosome 17. Figure F describes the pairwise linkage disequilibrium for BUN on chromosome 18. The graphs were generated using Haploview 4.2. software. The colors represent D’ values: dark red, high inter-single nucleotide polymorphism (inter-SNP) D’ value; bright red, low inter-SNP D’ value. Linkage disequilibrium blocks are shown.
(ZIP)
Acknowledgments
This study was provided with bioresources from National Biobank of Korea, the centers for Disease Control and Prevention, Republic of Korea. We thank all the participants of this study.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This research was supported by Hallym University Research Fund 2014 (HURF-2014-58) that was presented to JL (1st author), URL of Hallym University: http://www.hallym.ac.kr/indexpc.php. The funder had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Levey AS, Atkins R, Coresh J, Cohen EP, Collins AJ, Eckardt KU, et al. (2007) Chronic kidney disease as a global public health problem: approaches and initiatives—a position statement from Kidney Disease Improving Global Outcomes. Kidney Int 72: 247–259. doi: 10.1038/sj.ki.5002343 [DOI] [PubMed] [Google Scholar]
- 2.Manoeuvrier G, Bach-Ngohou K, Batard E, Masson D, Trewick D (2017) Diagnostic performance of serum blood urea nitrogen to creatinine ratio for distinguishing prerenal from intrinsic acute kidney injury in the emergency department. BMC Nephrol 18: 173 doi: 10.1186/s12882-017-0591-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lyman JL (1986) Blood urea nitrogen and creatinine. Emerg Med Clin North Am 4: 223–233. [PubMed] [Google Scholar]
- 4.Yang Q, Kottgen A, Dehghan A, Smith AV, Glazer NL, Chen MH, et al. (2010) Multiple genetic loci influence serum urate levels and their relationship with gout and cardiovascular disease risk factors. Circ Cardiovasc Genet 3: 523–530. doi: 10.1161/CIRCGENETICS.109.934455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang Q, Guo CY, Cupples LA, Levy D, Wilson PW, Fox CS (2005) Genome-wide search for genes affecting serum uric acid levels: the Framingham Heart Study. Metabolism 54: 1435–1441. doi: 10.1016/j.metabol.2005.05.007 [DOI] [PubMed] [Google Scholar]
- 6.Kastarinen M, Juutilainen A, Kastarinen H, Salomaa V, Karhapaa P, Tuomilehto J, et al. (2010) Risk factors for end-stage renal disease in a community-based population: 26-year follow-up of 25,821 men and women in eastern Finland. J Intern Med 267: 612–620. doi: 10.1111/j.1365-2796.2009.02197.x [DOI] [PubMed] [Google Scholar]
- 7.Satko SG, Sedor JR, Iyengar SK, Freedman BI (2007) Familial clustering of chronic kidney disease. Semin Dial 20: 229–236. doi: 10.1111/j.1525-139X.2007.00282.x [DOI] [PubMed] [Google Scholar]
- 8.Placha G, Canani LH, Warram JH, Krolewski AS (2005) Evidence for different susceptibility genes for proteinuria and ESRD in type 2 diabetes. Adv Chronic Kidney Dis 12: 155–169. [DOI] [PubMed] [Google Scholar]
- 9.Kopp JB, Smith MW, Nelson GW, Johnson RC, Freedman BI, Bowden DW, et al. (2008) MYH9 is a major-effect risk gene for focal segmental glomerulosclerosis. Nat Genet 40: 1175–1184. doi: 10.1038/ng.226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kottgen A, Glazer NL, Dehghan A, Hwang SJ, Katz R, Li M, et al. (2009) Multiple loci associated with indices of renal function and chronic kidney disease. Nat Genet 41: 712–717. doi: 10.1038/ng.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Price AL, Patterson NJ, Plenge RM, Weinblatt ME, Shadick NA, Reich D (2006) Principal components analysis corrects for stratification in genome-wide association studies. Nat Genet 38: 904–909. doi: 10.1038/ng1847 [DOI] [PubMed] [Google Scholar]
- 12.Cho YS, Go MJ, Kim YJ, Heo JY, Oh JH, Ban HJ, et al. (2009) A large-scale genome-wide association study of Asian populations uncovers genetic factors influencing eight quantitative traits. Nat Genet 41: 527–534. doi: 10.1038/ng.357 [DOI] [PubMed] [Google Scholar]
- 13.Choi S, Bae S, Park T (2016) Risk Prediction Using Genome-Wide Association Studies on Type 2 Diabetes. Genomics Inform 14: 138–148. doi: 10.5808/GI.2016.14.4.138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeong SW, Chung M, Park SJ, Cho SB, Hong KW (2014) Genome-wide association study of metabolic syndrome in koreans. Genomics Inform 12: 187–194. doi: 10.5808/GI.2014.12.4.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hwang SJ, Yang Q, Meigs JB, Pearce EN, Fox CS (2007) A genome-wide association for kidney function and endocrine-related traits in the NHLBI's Framingham Heart Study. BMC Med Genet 8 Suppl 1: S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hong X, Xing H, Yu Y, Wen Y, Zhang Y, Zhang S, et al. (2007) Genetic polymorphisms of the urea transporter gene are associated with antihypertensive response to nifedipine GITS. Methods Find Exp Clin Pharmacol 29: 3–10. doi: 10.1358/mf.2007.29.1.1063490 [DOI] [PubMed] [Google Scholar]
- 17.Ranade K, Wu KD, Hwu CM, Ting CT, Pei D, Pesich R, et al. (2001) Genetic variation in the human urea transporter-2 is associated with variation in blood pressure. Hum Mol Genet 10: 2157–2164. [DOI] [PubMed] [Google Scholar]
- 18.Okada Y, Sim X, Go MJ, Wu JY, Gu D, Takeuchi F, et al. (2012) Meta-analysis identifies multiple loci associated with kidney function-related traits in east Asian populations. Nat Genet 44: 904–909. doi: 10.1038/ng.2352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meng W, Butterworth J, Bradley DT, Hughes AE, Soler V, Calvas P, et al. (2012) A genome-wide association study provides evidence for association of chromosome 8p23 (MYP10) and 10q21.1 (MYP15) with high myopia in the French Population. Invest Ophthalmol Vis Sci 53: 7983–7988. doi: 10.1167/iovs.12-10409 [DOI] [PubMed] [Google Scholar]
- 20.Kim YJ, Go MJ, Hu C, Hong CB, Kim YK, Lee JY, et al. (2011) Large-scale genome-wide association studies in East Asians identify new genetic loci influencing metabolic traits. Nat Genet 43: 990–995. doi: 10.1038/ng.939 [DOI] [PubMed] [Google Scholar]
- 21.Chambers JC, Zhang W, Lord GM, van der Harst P, Lawlor DA, Sehmi JS, et al. (2010) Genetic loci influencing kidney function and chronic kidney disease. Nat Genet 42: 373–375. doi: 10.1038/ng.566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shriner D, Herbert A, Doumatey AP, Zhou J, Huang H, Erdos MR, et al. (2012) Multiple loci associated with renal function in African Americans. PLoS One 7: e45112 doi: 10.1371/journal.pone.0045112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Franceschini N, Haack K, Almasy L, Laston S, Lee ET, Best LG, et al. (2014) Generalization of associations of kidney-related genetic loci to American Indians. Clin J Am Soc Nephrol 9: 150–158. doi: 10.2215/CJN.02300213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gudbjartsson DF, Walters GB, Thorleifsson G, Stefansson H, Halldorsson BV, Zusmanovich P, et al. (2008) Many sequence variants affecting diversity of adult human height. Nat Genet 40: 609–615. doi: 10.1038/ng.122 [DOI] [PubMed] [Google Scholar]
- 25.Zhao J, Li M, Bradfield JP, Zhang H, Mentch FD, Wang K, et al. (2010) The role of height-associated loci identified in genome wide association studies in the determination of pediatric stature. BMC Med Genet 11: 96 doi: 10.1186/1471-2350-11-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kottgen A, Pattaro C, Boger CA, Fuchsberger C, Olden M, Glazer NL, et al. (2010) New loci associated with kidney function and chronic kidney disease. Nat Genet 42: 376–384. doi: 10.1038/ng.568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Suzuki Y, Taniyama M, Muramatsu T, Higuchi S, Ohta S, Atsumi Y, et al. (2004) ALDH2/ADH2 polymorphism associated with vasculopathy and neuropathy in type 2 diabetes. Alcohol Clin Exp Res 28: 111S–116S. [DOI] [PubMed] [Google Scholar]
- 28.Dakeishi M, Murata K, Sasaki M, Tamura A, Iwata T (2008) Association of alcohol dehydrogenase 2 and aldehyde dehydrogenase 2 genotypes with fasting plasma glucose levels in Japanese male and female workers. Alcohol Alcohol 43: 143–147. doi: 10.1093/alcalc/agm173 [DOI] [PubMed] [Google Scholar]
- 29.Yamada Y, Imai T, Ishizaki M, Honda R (2006) ALDH2 and CYP2E1 genotypes, urinary acetaldehyde excretion and the health consequences in moderate alcohol consumers. J Hum Genet 51: 104–111. doi: 10.1007/s10038-005-0330-0 [DOI] [PubMed] [Google Scholar]
- 30.Israni A, Leduc R, Holmes J, Jacobson PA, Lamba V, Guan W, et al. (2010) Single-nucleotide polymorphisms, acute rejection, and severity of tubulitis in kidney transplantation, accounting for center-to-center variation. Transplantation 90: 1401–1408. doi: 10.1097/TP.0b013e3182000085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hara K, Suyama K, Itoh H, Nagashima S (2008) Influence of ALDH2 genetic polymorphisms on aciclovir pharmacokinetics following oral administration of valaciclovir in Japanese end-stage renal disease patients. Drug Metab Pharmacokinet 23: 306–312. [DOI] [PubMed] [Google Scholar]
- 32.Kim JJ, Lee HI, Park T, Kim K, Lee JE, Cho NH, et al. (2010) Identification of 15 loci influencing height in a Korean population. J Hum Genet 55: 27–31. doi: 10.1038/jhg.2009.116 [DOI] [PubMed] [Google Scholar]
- 33.Sovio U, Bennett AJ, Millwood IY, Molitor J, O'Reilly PF, Timpson NJ, et al. (2009) Genetic determinants of height growth assessed longitudinally from infancy to adulthood in the northern Finland birth cohort 1966. PLoS Genet 5: e1000409 doi: 10.1371/journal.pgen.1000409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berndt SI, Gustafsson S, Magi R, Ganna A, Wheeler E, Feitosa MF, et al. (2013) Genome-wide meta-analysis identifies 11 new loci for anthropometric traits and provides insights into genetic architecture. Nat Genet 45: 501–512. doi: 10.1038/ng.2606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pattaro C, Teumer A, Gorski M, Chu AY, Li M, Mijatovic V, et al. (2016) Genetic associations at 53 loci highlight cell types and biological pathways relevant for kidney function. Nat Commun 7: 10023 doi: 10.1038/ncomms10023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parsa A, Fuchsberger C, Kottgen A, O'Seaghdha CM, Pattaro C, de Andrade M, et al. (2013) Common variants in Mendelian kidney disease genes and their association with renal function. J Am Soc Nephrol 24: 2105–2117. doi: 10.1681/ASN.2012100983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kamatani Y, Matsuda K, Okada Y, Kubo M, Hosono N, Daigo Y, et al. (2010) Genome-wide association study of hematological and biochemical traits in a Japanese population. Nat Genet 42: 210–215. doi: 10.1038/ng.531 [DOI] [PubMed] [Google Scholar]
- 38.Kannangara DR, Phipps-Green AJ, Dalbeth N, Stamp LK, Williams KM, Graham GG, et al. (2016) Hyperuricaemia: contributions of urate transporter ABCG2 and the fractional renal clearance of urate. Ann Rheum Dis 75: 1363–1366. doi: 10.1136/annrheumdis-2015-208111 [DOI] [PubMed] [Google Scholar]
- 39.Li R, Miao L, Qin L, Xiang Y, Zhang X, Peng H, et al. (2015) A meta-analysis of the associations between the Q141K and Q126X ABCG2 gene variants and gout risk. Int J Clin Exp Pathol 8: 9812–9823. [PMC free article] [PubMed] [Google Scholar]
- 40.Jiri M, Zhang L, Lan B, He N, Feng T, Liu K, et al. (2016) Genetic variation in the ABCG2 gene is associated with gout risk in the Chinese Han population. Clin Rheumatol 35: 159–163. doi: 10.1007/s10067-015-3105-9 [DOI] [PubMed] [Google Scholar]
- 41.Karns R, Zhang G, Sun G, Rao Indugula S, Cheng H, Havas-Augustin D, et al. (2012) Genome-wide association of serum uric acid concentration: replication of sequence variants in an island population of the Adriatic coast of Croatia. Ann Hum Genet 76: 121–127. doi: 10.1111/j.1469-1809.2011.00698.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yamagishi K, Tanigawa T, Kitamura A, Kottgen A, Folsom AR, Iso H, et al. (2010) The rs2231142 variant of the ABCG2 gene is associated with uric acid levels and gout among Japanese people. Rheumatology (Oxford) 49: 1461–1465. [DOI] [PubMed] [Google Scholar]
- 43.Wang B, Miao Z, Liu S, Wang J, Zhou S, Han L, et al. (2010) Genetic analysis of ABCG2 gene C421A polymorphism with gout disease in Chinese Han male population. Hum Genet 127: 245–246. doi: 10.1007/s00439-009-0760-4 [DOI] [PubMed] [Google Scholar]
- 44.Phipps-Green AJ, Hollis-Moffatt JE, Dalbeth N, Merriman ME, Topless R, Gow PJ, et al. (2010) A strong role for the ABCG2 gene in susceptibility to gout in New Zealand Pacific Island and Caucasian, but not Maori, case and control sample sets. Hum Mol Genet 19: 4813–4819. doi: 10.1093/hmg/ddq412 [DOI] [PubMed] [Google Scholar]
- 45.Woodward OM, Kottgen A, Coresh J, Boerwinkle E, Guggino WB, Kottgen M (2009) Identification of a urate transporter, ABCG2, with a common functional polymorphism causing gout. Proc Natl Acad Sci U S A 106: 10338–10342. doi: 10.1073/pnas.0901249106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stark K, Reinhard W, Grassl M, Erdmann J, Schunkert H, Illig T, et al. (2009) Common polymorphisms influencing serum uric acid levels contribute to susceptibility to gout, but not to coronary artery disease. PLoS One 4: e7729 doi: 10.1371/journal.pone.0007729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Matsuo H, Takada T, Ichida K, Nakamura T, Nakayama A, Ikebuchi Y, et al. (2009) Common defects of ABCG2, a high-capacity urate exporter, cause gout: a function-based genetic analysis in a Japanese population. Sci Transl Med 1: 5ra11 doi: 10.1126/scitranslmed.3000237 [DOI] [PubMed] [Google Scholar]
- 48.Dehghan A, Kottgen A, Yang Q, Hwang SJ, Kao WL, Rivadeneira F, et al. (2008) Association of three genetic loci with uric acid concentration and risk of gout: a genome-wide association study. Lancet 372: 1953–1961. doi: 10.1016/S0140-6736(08)61343-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tabara Y, Kohara K, Kawamoto R, Hiura Y, Nishimura K, Morisaki T, et al. (2010) Association of four genetic loci with uric acid levels and reduced renal function: the J-SHIPP Suita study. Am J Nephrol 32: 279–286. doi: 10.1159/000318943 [DOI] [PubMed] [Google Scholar]
- 50.Kolz M, Johnson T, Sanna S, Teumer A, Vitart V, Perola M, et al. (2009) Meta-analysis of 28,141 individuals identifies common variants within five new loci that influence uric acid concentrations. PLoS Genet 5: e1000504 doi: 10.1371/journal.pgen.1000504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lee YH, Song GG (2012) Pathway analysis of genome-wide association studies on uric acid concentrations. Hum Immunol 73: 805–810. doi: 10.1016/j.humimm.2012.05.004 [DOI] [PubMed] [Google Scholar]
- 52.Xing SC, Wang XF, Miao ZM, Zhang XZ, Zheng J, Yuan Y (2015) Association of an Exon SNP of SLC2A9 Gene with Hyperuricemia Complicated with Type 2 Diabetes Mellitus in the Chinese Male Han Population. Cell Biochem Biophys 71: 1335–1339. doi: 10.1007/s12013-014-0353-2 [DOI] [PubMed] [Google Scholar]
- 53.Ware EB, Riehle E, Smith JA, Zhao W, Turner ST, Kardia SL, et al. (2015) SLC2A9 Genotype Is Associated with SLC2A9 Gene Expression and Urinary Uric Acid Concentration. PLoS One 10: e0128593 doi: 10.1371/journal.pone.0128593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Voruganti VS, Laston S, Haack K, Mehta NR, Cole SA, Butte NF, et al. (2015) Serum uric acid concentrations and SLC2A9 genetic variation in Hispanic children: the Viva La Familia Study. Am J Clin Nutr 101: 725–732. doi: 10.3945/ajcn.114.095364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Testa A, Prudente S, Leonardis D, Spoto B, Sanguedolce MC, Parlongo RM, et al. (2015) A genetic marker of hyperuricemia predicts cardiovascular events in a meta-analysis of three cohort studies in high risk patients. Nutr Metab Cardiovasc Dis 25: 1087–1094. doi: 10.1016/j.numecd.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 56.Testa A, Mallamaci F, Leonardis D, Spoto B, Pisano A, Sanguedolce MC, et al. (2015) Synergism between asymmetric dimethylarginine (ADMA) and a genetic marker of uric acid in CKD progression. Nutr Metab Cardiovasc Dis 25: 167–172. doi: 10.1016/j.numecd.2014.10.016 [DOI] [PubMed] [Google Scholar]
- 57.Long W, Panwar P, Witkowska K, Wong K, O'Neill D, Chen XZ, et al. (2015) Critical Roles of Two Hydrophobic Residues within Human Glucose Transporter 9 (hSLC2A9) in Substrate Selectivity and Urate Transport. J Biol Chem 290: 15292–15303. doi: 10.1074/jbc.M114.611178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cho SK, Kim S, Chung JY, Jee SH (2015) Discovery of URAT1 SNPs and association between serum uric acid levels and URAT1. BMJ Open 5: e009360 doi: 10.1136/bmjopen-2015-009360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wei WH, Guo Y, Kindt AS, Merriman TR, Semple CA, Wang K, et al. (2014) Abundant local interactions in the 4p16.1 region suggest functional mechanisms underlying SLC2A9 associations with human serum uric acid. Hum Mol Genet 23: 5061–5068. doi: 10.1093/hmg/ddu227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Testa A, Mallamaci F, Spoto B, Pisano A, Sanguedolce MC, Tripepi G, et al. (2014) Association of a polymorphism in a gene encoding a urate transporter with CKD progression. Clin J Am Soc Nephrol 9: 1059–1065. doi: 10.2215/CJN.11041013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Simon KC, Eberly S, Gao X, Oakes D, Tanner CM, Shoulson I, et al. (2014) Mendelian randomization of serum urate and parkinson disease progression. Ann Neurol 76: 862–868. doi: 10.1002/ana.24281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shen H, Feng C, Jin X, Mao J, Fu H, Gu W, et al. (2014) Recurrent exercise-induced acute kidney injury by idiopathic renal hypouricemia with a novel mutation in the SLC2A9 gene and literature review. BMC Pediatr 14: 73 doi: 10.1186/1471-2431-14-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Charles BA, Shriner D, Doumatey A, Chen G, Zhou J, Huang H, et al. (2011) A genome-wide association study of serum uric acid in African Americans. BMC Med Genomics 4: 17 doi: 10.1186/1755-8794-4-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Li C, Han L, Levin AM, Song H, Yan S, Wang Y, et al. (2010) Multiple single nucleotide polymorphisms in the human urate transporter 1 (hURAT1) gene are associated with hyperuricaemia in Han Chinese. J Med Genet 47: 204–210. doi: 10.1136/jmg.2009.068619 [DOI] [PubMed] [Google Scholar]
- 65.Zemunik T, Boban M, Lauc G, Jankovic S, Rotim K, Vatavuk Z, et al. (2009) Genome-wide association study of biochemical traits in Korcula Island, Croatia. Croat Med J 50: 23–33. doi: 10.3325/cmj.2009.50.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hollis-Moffatt JE, Xu X, Dalbeth N, Merriman ME, Topless R, Waddell C, et al. (2009) Role of the urate transporter SLC2A9 gene in susceptibility to gout in New Zealand Maori, Pacific Island, and Caucasian case-control sample sets. Arthritis Rheum 60: 3485–3492. doi: 10.1002/art.24938 [DOI] [PubMed] [Google Scholar]
- 67.Wallace C, Newhouse SJ, Braund P, Zhang F, Tobin M, Falchi M, et al. (2008) Genome-wide association study identifies genes for biomarkers of cardiovascular disease: serum urate and dyslipidemia. Am J Hum Genet 82: 139–149. doi: 10.1016/j.ajhg.2007.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vitart V, Rudan I, Hayward C, Gray NK, Floyd J, Palmer CN, et al. (2008) SLC2A9 is a newly identified urate transporter influencing serum urate concentration, urate excretion and gout. Nat Genet 40: 437–442. doi: 10.1038/ng.106 [DOI] [PubMed] [Google Scholar]
- 69.McArdle PF, Parsa A, Chang YP, Weir MR, O'Connell JR, Mitchell BD, et al. (2008) Association of a common nonsynonymous variant in GLUT9 with serum uric acid levels in old order amish. Arthritis Rheum 58: 2874–2881. doi: 10.1002/art.23752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Doring A, Gieger C, Mehta D, Gohlke H, Prokisch H, Coassin S, et al. (2008) SLC2A9 influences uric acid concentrations with pronounced sex-specific effects. Nat Genet 40: 430–436. doi: 10.1038/ng.107 [DOI] [PubMed] [Google Scholar]
- 71.Li S, Sanna S, Maschio A, Busonero F, Usala G, Mulas A, et al. (2007) The GLUT9 gene is associated with serum uric acid levels in Sardinia and Chianti cohorts. PLoS Genet 3: e194 doi: 10.1371/journal.pgen.0030194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tin A, Woodward OM, Kao WH, Liu CT, Lu X, Nalls MA, et al. (2011) Genome-wide association study for serum urate concentrations and gout among African Americans identifies genomic risk loci and a novel URAT1 loss-of-function allele. Hum Mol Genet 20: 4056–4068. doi: 10.1093/hmg/ddr307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lee JH, Choi HJ, Lee BH, Kang HK, Chin HJ, Yoon HJ, et al. (2008) Prevalence of hypouricaemia and SLC22A12 mutations in healthy Korean subjects. Nephrology (Carlton) 13: 661–666. [DOI] [PubMed] [Google Scholar]
- 74.Jang WC, Nam YH, Park SM, Ahn YC, Park SH, Choe JY, et al. (2008) T6092C polymorphism of SLC22A12 gene is associated with serum uric acid concentrations in Korean male subjects. Clin Chim Acta 398: 140–144. doi: 10.1016/j.cca.2008.09.008 [DOI] [PubMed] [Google Scholar]
- 75.Vazquez-Mellado J, Jimenez-Vaca AL, Cuevas-Covarrubias S, Alvarado-Romano V, Pozo-Molina G, Burgos-Vargas R (2007) Molecular analysis of the SLC22A12 (URAT1) gene in patients with primary gout. Rheumatology (Oxford) 46: 215–219. [DOI] [PubMed] [Google Scholar]
- 76.Shima Y, Teruya K, Ohta H (2006) Association between intronic SNP in urate-anion exchanger gene, SLC22A12, and serum uric acid levels in Japanese. Life Sci 79: 2234–2237. doi: 10.1016/j.lfs.2006.07.030 [DOI] [PubMed] [Google Scholar]
- 77.Graessler J, Graessler A, Unger S, Kopprasch S, Tausche AK, Kuhlisch E, et al. (2006) Association of the human urate transporter 1 with reduced renal uric acid excretion and hyperuricemia in a German Caucasian population. Arthritis Rheum 54: 292–300. doi: 10.1002/art.21499 [DOI] [PubMed] [Google Scholar]
- 78.Wang Y, Zhou X, Xu M, Weng W, Zhang Q, Yang Y, et al. (2016) OTUB1-catalyzed deubiquitination of FOXM1 facilitates tumor progression and predicts a poor prognosis in ovarian cancer. Oncotarget 7: 36681–36697. doi: 10.18632/oncotarget.9160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Baietti MF, Simicek M, Abbasi Asbagh L, Radaelli E, Lievens S, Crowther J, et al. (2016) OTUB1 triggers lung cancer development by inhibiting RAS monoubiquitination. EMBO Mol Med 8: 288–303. doi: 10.15252/emmm.201505972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhou Y, Wu J, Fu X, Du W, Zhou L, Meng X, et al. (2014) OTUB1 promotes metastasis and serves as a marker of poor prognosis in colorectal cancer. Mol Cancer 13: 258 doi: 10.1186/1476-4598-13-258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liu X, Jiang WN, Wang JG, Chen H (2014) Colon cancer bears overexpression of OTUB1. Pathol Res Pract 210: 770–773. doi: 10.1016/j.prp.2014.05.008 [DOI] [PubMed] [Google Scholar]
- 82.Mells GF, Floyd JA, Morley KI, Cordell HJ, Franklin CS, Shin SY, et al. (2011) Genome-wide association study identifies 12 new susceptibility loci for primary biliary cirrhosis. Nat Genet 43: 329–332. doi: 10.1038/ng.789 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Figure A describes the pairwise linkage disequilibrium for BUN on chromosome 3. Figure B describes the pairwise linkage disequilibrium for uric acid on chromosome 4. Figure C describes the pairwise linkage disequilibrium for uric acid on chromosome 11. Figure D describes the pairwise linkage disequilibrium for serum creatinine on chromosome 12. Figure E describes the pairwise linkage disequilibrium for glomerular filtration rate on chromosome 17. Figure F describes the pairwise linkage disequilibrium for BUN on chromosome 18. The graphs were generated using Haploview 4.2. software. The colors represent D’ values: dark red, high inter-single nucleotide polymorphism (inter-SNP) D’ value; bright red, low inter-SNP D’ value. Linkage disequilibrium blocks are shown.
(ZIP)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.