Abstract
The long-term care sector is characterized by high morbidity and employee turnover, along with associated costs. Effective health protection and health promotion are important to improve physical and psychosocial well-being of caregivers. Assessment of organizational readiness for change is an essential precursor to the successful implementation of workplace programs addressing work climate, structure of tasks and relationships, and other issues that may be perceived as challenging by some within the institution. This study qualitatively assessed readiness of five skilled nursing facilities for a participatory occupational health/health promotion intervention. Selection criteria were developed to screen for program feasibility and ability to conduct prospective evaluations, and information was collected from managers and employees (interviews and focus groups). Three centers were selected for the program, and the first year of formative evaluation and intervention experience was then reviewed to evaluate and modify our selection criteria after the fact. Lessons learned include adding assessment of communication and the structure of problem solving to our selection criteria, improving methods to assess management support in a concrete (potentially nonverbal) form, and obtaining a stated financial commitment and resources to enable the team to function. Assessment of organizational readiness for change is challenging, although necessary to implement effective and sustainable health promotion programs in specific organizations.
Keywords: intervention readiness, worker participation, occupational health, health promotion
INTRODUCTION
The long-term care sector is the second most hazardous in the United States in terms of recognized work-related injuries and illnesses (Bureau of Labor Statistics, U.S. Department of Labor, 2004). Numerous exposures in the work environment threaten employees’ health and safety, including infectious diseases, needlesticks, violence, heavy lifting, shift work, and organizational stressors (Sofie, Belza, & Young, 2003; Zhang et al., 2011). Probably not unrelated, turnover is extremely high among long-term care employees. Average 1-year turnover in one study was 86% for certified nursing assistants (CNAs) and licensed practical nurses and 55% for registered nurses (Castle & Engberg, 2005). Programs that improve physical and psychosocial well-being of long-term care employees might help stabilize this important workforce.
Traditionally, health promotion practice focused on individual behavior changes, but as the field has matured, more comprehensive approaches have emerged, with interventions operating at multiple levels of influence (Weiner, Lewis, & Linnan, 2009). Some newer interventions have addressed work environment influences on health behaviors (Ball, Timperio, & Crawford, 2006; Duncan, Spence, & Mummery, 2005). In particular, there is increasing evidence that psychosocial work stressors, especially low decision latitude, contribute to unhealthy personal behaviors (Punnett et al., 2009). The psychosocial work environment can be improved in a variety of ways (LaMontagne, Keegel, & Vallance, 2007; Lohela, Bjorklund, Vingård, Hagberg, & Jensen, 2009; Michie & Williams, 2003): increase employees’ autonomy and decision making, allow for greater creativity and problem solving, promote recognition or rewards for good work, provide consistent and constructive feedback, and arrange healthier schedules. Therefore, an integrated workplace intervention that seeks to improve the work environment, in coordination with health promotion activities, should be more effective to promote worker health and well-being.
However, comprehensive workplace health promotion involving work organization change is challenging to implement (Lavoie-Tremblay, 2004). Several investigators have reported limited success with organizational change programs in health care institutions (Alexander, Weiner, Shortell, Baker, & Becker, 2006; Pearson et al., 2005). Kotter (1996) discussed that one half of failures to implement large-scale organizational change were attributable to the institutions’ insufficient readiness. Therefore, it is important to assess organizational readiness for change before the actual implementation of the intervention. In a research study, effort would be wasted by trying to carry out a complex program in an unreceptive institution. In a programmatic setting, the institution itself would need the preconditions that support the effort and its long-term success and sustainability. To our knowledge, there is limited literature about how to assess organizational readiness for change.
This study was part of a research project that sought to initiate an integrated, participatory worker health intervention in selected skilled nursing facilities (SNFs). Participatory processes engage the workers to take actions to improve their own health (Baum, MacDougall, & Smith, 2006). Enabling workers to act can have a transformative effect at the workplaces; since decision making is a key psychosocial determinant of worker health, providing opportunities to set priorities and design key program features should itself improve worker health, both directly and indirectly (Punnett et al., 2009).
BACKGROUND: ORGANIZATIONAL READINESS FOR CHANGE
Assessment of organizational readiness for change is an essential precursor to the successful implementation of workplace health programs (O’Connor & Fiol, 2006), especially with a participatory process that is inherently more demanding on an organization. Weiner (2009) has defined readiness to change as “organizational members’ shared resolve to implement a change (change commitment) and shared belief in their collective capability to do so (change efficacy)” (p. 1). It is “a multi-level and multi-faceted construct” (p. 1) that operates at “the individual, group, unit, department, and organizational level” (Weiner, 2009, p. 2). Lehman, Greener, and Simpson (2002) described four dimensions at both the individual and organizational levels: motivation for change, staff attributes, adequacy of resources, and organizational climate.
There is potential ambiguity in the difference between an organization’s need for change and its readiness for change. An organization’s need for participatory change is related to but conceptually distinct from its readiness for such a process. Somewhat paradoxically, an organization that is fully ready for a participatory process would be one that might in theory need no further intervention, because it would already have a fully engaged workforce conducting iterative needs assessments and interventions. On the other hand, an organization that is completely closed to worker participation in decision making might have a great need for change, but it would be a completely infeasible site for a participatory intervention. Considering a hypothetical, continuous scale of organizational readiness for change from 0 to 100%, what is the mid-range of “readiness scores” within which intervention research is both needed and feasible? Furthermore, what method for assessing readiness would successfully identify those organizations that have sufficient need to justify the intervention effort but are also open enough to changing their established ways of operating that the effort has some chance of succeeding?
A number of instruments have been developed to measure organizational readiness for change, although with limited evidence of reliability or validity (Weiner, Amick, & Lee, 2008). These instruments cover different dimensions of organizational readiness for change; in fact, there is no consensus on what dimensions are critical to evaluate. It may be that assessment should be customized according to what kinds of programs are implemented and the specific features of the workplace. However, there ought to be some generic elements that are relevant to all efforts to increase degree of worker participation, even if they are operationalized differently in different settings.
We used several sources of qualitative data to assess five candidate workplaces and select three of them for a participatory worker health intervention. This article describes both that selection process and our subsequent iterative evaluation of the selection criteria.
METHOD
Study Design
The participating company operated over 200 SNFs in eastern United States. Each center in the company was provided with a small annual budget ($700) for health promotion activities, and some centers had extensive health promotion programming. The company’s regional director for health and safety recommended five SNFs that did not yet have active health promotion programs and whose administrators she believed would be receptive to the participatory process. Approval to conduct needs assessments and to implement the participatory program in selected facilities was obtained from corporate officers.
To select three of the five centers, we undertook a selection process involving in-depth interviews with center administrators and directors of nursing (DONs; preinterviews), focus groups with CNAs at the same center, and then follow-up interviews with administrators (postinterviews; Figure 1). The initial selection criteria (Table 1) were developed to screen for conditions that would enhance feasibility of both the program itself and the conduct of prospective evaluations. Interview questions and focus group scripts were designed to collect information on these topics at both the organizational and interpersonal/individual levels.
FIGURE 1. Data Collection Process for Evaluation and Modification of the Initial Selection Criteria.
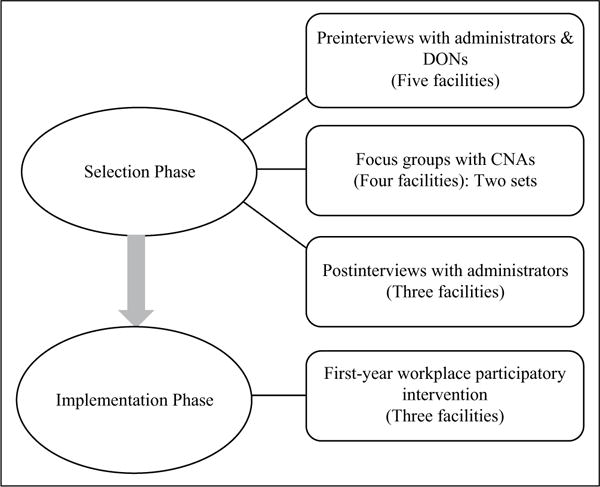
NOTE: DONs = directors of nursing; CNAs = certified nursing assistants.
TABLE 1.
Initial Site Selection Criteria for the Participatory Employee Health Intervention
| Selection Criterion | Operational Definition |
|---|---|
| Organizational level: Organizational culture and structure | |
|
|
|
|
|
|
|
|
|
|
| Interpersonal/individual level: Manager and employee attributes | |
|
|
|
|
NOTE: WHP = workplace health promotion; OSH = occupational safety and health.
Sample and Data Collection
Selection Phase
One experienced lead researcher and one research assistant conducted all interviews and focus groups. Purpose and procedure were explained and participants were asked to sign a consent form. All interviews and focus groups were tape-recorded and transcribed professionally. The study protocol was approved by the University of Massachusetts Lowell Institutional Review Board (No. 06-1403).
Preinterviews: One hour interviews with administrators and DONs were conducted in the five facilities.
Focus groups: Focus groups with CNAs were conducted in four facilities (see Results section). The first focus group covered information needed for site selection (Table 1). In the second meeting, participants were asked to envision the ideal nursing home, then to suggest and prioritize programs that might bring that goal closer.
Postinterviews: Interviews with administrators were conducted in three facilities (see Results section) after the focus groups were completed. These interviews were designed to assess the reactions of administrators to employee concerns that emerged from the focus groups and their support for recruiting Health and Wellness (H&W) Team members and scheduling team meetings.
The interview guide for preinterviews and focus groups (Zhang et al., 2011) was based on the National Nursing Assistant Survey (http://www.cdc.gov/nchs/data/nnhsd/2004NNASQuestionnaire.pdf), the Heart Check Survey (http://www.health.ny.gov/diseases/cardiovascular/heart_disease/docs/heartcheck.pdf), and other sources (Flum, 2004; Wilson, DeJoy, Vandenberg, Richardson, & McGrath, 2004). The interviews also addressed logistical details for implementation of the focus groups, including recruitment and scheduling; the focus groups asked employees about perceived feasibility of forming an employee H&W Team.
Information from interviews and focus groups was categorized according to the initial selection criteria (Table 1). After site selection, employees were recruited for an H&W Team in each SNF. Researchers’ subsequent observations, meeting minutes, and field notes for the first program year were reviewed to evaluate our selection criteria post hoc.
Implementation Phase
After completion of the assessments and selection, participatory H&W Teams were established. Team members were volunteers responding to posters and management promotion of the program. Each team started with employees from different departments (clinical, dietary, housekeeping, laundry, and business) and met every other week for 1 hour. The same lead researcher who conducted the interviews and focus groups, along with five research assistants, facilitated the H&W Team meetings and served as technical program resources. The first few meetings reexamined the issues that were raised in the focus groups in that facility and were followed by meetings to develop, implement, and evaluate selected programs.
RESULTS
Sample Description
Ten preinterviews with administrators and DONs were completed in the five SNFs in June, 2007. Two administrators and four DONs were female. All administrators and DONs were White and non-Hispanic, with an average length of tenure of 4 years. Three postinterviews with administrators in selected centers were completed in January 2008.
Fourteen focus groups were conducted at four facilities from July to August 2007. A total of 50 CNAs participated, most coming to both focus groups: 90% were female; 58% were White, 36% were Black, 34% were Hispanic, and 1% was Asian or American Indian.
Three H&W Teams were formed with 10 employee participants each. Over time, each team settled into a core group of four-six members who consistently attended meetings and took on specific responsibilities. Of these regular participants, 100% were female; 84% were White, 10% were Black, and 6% were Hispanic.
Selection Phase
Facility A was eliminated from consideration after preinterviews due to high turnover (60%), short tenure, and lack of vision of management and limited awareness of employee concerns (Table 2). Facility B was eliminated due to high perceptible hostility of employees when discussing managers’ response to employee concerns in focus groups, difficulty organizing employee focus groups, lack of employee confidence, interest in the program, and commitment toward improvement of the facility (Table 2).
TABLE 2.
Selection Criteria for Organizational Readiness of the Participatory Intervention (Selection Phase)
| Selection Criteria | Findings From Interviews and Focus Groups |
|---|---|
| Organizational level: Organizational culture and structure | |
|
|
|
|
|
|
|
|
|
|
| Interpersonal/individual level: Manager and employee attributes | |
|
|
|
|
NOTE: H&W = Health and Wellness; WHP = workplace health promotion; OSH = occupational safety and health.
Implementation Phase
In the first year, there were 64 team meetings altogether at the three facilities. A number of similar interests were expressed, including desired availability of low-cost or free healthy meals onsite, clean and uncluttered break areas, a quiet relaxation room to escape from the continual sensory input of their jobs, walking clubs or paths, on-site counseling or workshops on stress control, and nutrition and weight loss programs. Researchers’ observations, meeting minutes, and field notes were used in the quotes below.
Management in all three facilities was involved to some extent, in the form of asking for updates of team activities, occasionally participating in team meetings, and voicing support to team members. For example, one administrator asked to “receive meeting minutes to be kept up to speed.”
Consistent with focus group results, employee empowerment and participation in making changes were considered important by members of all three teams. Even though the teams “lack[ed] the influence to change large organizational issues (e.g., staff–resident ratio),” they were able to “voice their opinions about the facility,” and initiated and implemented projects that “they felt confident they could accomplish that would improve their health and well-being.” For example, when discussing a garden project in one facility, the team was enthusiastic and “felt a sense of empowerment from their decision to tackle this project.” The garden project was viewed as a way of reducing stress, building teamwork, and promoting healthy eating and exercise among workers. In this project, the H&W Team obtained broad employee-based participation from different departments.
In another facility, team proposals led to improving the staff break room to make it a place where workers could relax and escape the stressful conditions of their job. The team selected paint, borders, smaller tables, and curtains for the break room. From this project, the team members felt a sense of “control over decision” and “there is a lot of pride in the group.”
Flexibility with work schedule was a goal but difficult to achieve in all three facilities, given the nature and responsibility of caregiving work itself. Furthermore, tight staffing and lack of time were the biggest challenges to employees’ participation in team meetings and involvement in program development.
Communication issues were also of concern in all three facilities and discussed frequently as a barrier to the intervention process. All three H&W Teams planned to tackle communication “from management,” “between nurses and nursing assistants,” and “between shifts and departments” by the end of the first year.
Two facilities had difficulties with program initiation and implementation that were closely associated with the problem-solving process and management support. Both administrators, although well-meaning, repeatedly failed to follow through on tasks they promised to complete, which delayed program implementation, leaving team members frustrated. For example, several projects at one facility were delayed: “The process of waiting for and requesting follow-up from management is a constant struggle for the team and is one of the primary sources of discouragement and disempowerment.” On the other hand, “The management does not have an approval protocol for such projects and therefore, they tend to be pushed to the bottom of their priority lists.”
Management support and commitment of resources was a determinant of employee ability to make changes. Successful projects involving break room redesign depended on management willingness to cover materials costs as well as a commitment of staff resources for renovation. At one facility,
the initialization of many projects depends on the willingness of the administrator to support the team’s endeavors, to allocate resources, to facilitate tasks with middle management, and it also depends on the willingness of middle management and different departments to follow through.
However, at both facilities, administrators had expressed support during the interviews in the selection phase.
Evaluation of Initial Selection Criteria
Our first-year intervention experience verified the importance of our initial selection criteria and suggested that others should be added: assessment of communication, the structure of problem solving, and management financial support/commitment of resources to our selection criteria (see Table 3). Key to these would be improved methods to assess management support in a concrete form.
TABLE 3.
Added Selection Criteria for Organizational Readiness of the Participatory Intervention (Implementation Phase)
| Added Selection Criteria | Findings From First-Year Intervention |
|---|---|
| Organizational level: Organizational culture and structure | |
|
|
|
|
|
|
|
|
NOTE: H&W = Health and Wellness.
DISCUSSION
In this study, we developed a set of criteria to assess the organizational readiness of SNFs for a participatory program, used these criteria to select three out of five worksites for an employee health intervention, and evaluated our selection criteria through field experience in the first year of the intervention. Criteria were applied at both the organizational and interpersonal/individual levels, using qualitative data from both managers and employees.
As Weiner (2009) has suggested, if the work organization promotes innovation and creativity, has good work relationships, possesses flexible policies, promotes worker empowerment, and provides available resources, it is more likely to be ready for change. Although there is no consensus about the organizational features to assess, a few such as management support, communication, worker empowerment, and opportunities for participation are frequently discussed (Mealiea & Baltazar, 2005; Parboteeah et al., 2010; Wilson et al., 2004; Yukl & Becker, 2006). Some literature provides a theoretical perspective to guide the assessment process, using constructs such as organizational culture, structure, and staff attributes assessed at organizational and individual levels (e.g., Weiner, 2009). However, our process was largely empirical, informed by prior field experience of the investigators (Flum, 2004) and constrained by the available sites within the partnering company as well as study logistics (e.g., travel costs and project schedule). We focused primarily on organizational characteristics, as the future intervention was intended to create organizational change.
Management support was one of the most important selection criteria for intervention (Golaszewski, Barr, & Pronk, 2003; Lowe, Schellenberg, & Shannon, 2003). Logistical feasibility of team meetings was considered as an essential precursor for the implementation of workplace intervention, especially because time strain had been identified previously as a challenge (Zhang et al., 2011).
Organizational readiness for change was assessed in terms of change efficacy and commitment to change. Both managers’ and employees’ ability to envision future improvement and their shared interest in workplace health promotion and occupational safety and health were considered important to undertake a new program that required important inputs from both groups. Assessment of shared interest and commitment between managers and employees are important for successful implementation of a workplace intervention (Weiner, 2009). However, employees’ perceptions of occupational safety and health risks, the participatory culture, and the decision-making power may be different from those of managers (Zhang et al., 2011). Weiner (2009) suggested that a discrepancy between current and desired conditions, and an appealing vision of the future, could indicate the organization’s readiness for change in terms of the degree to which employees perceive the change as needed, important, or worthwhile.
Thus, the process for selecting worksites that both need change and are ready for change is challenging, due to the difficulty associated with acquiring the needed information accurately. The difficulty with initiating and implementing the intervention at two of the three facilities revealed the importance of assessing the structure of problem solving and concrete (rather than merely verbal) management support. Even though managers expressed great support in the selection phase, they did not necessarily provide financial and psychological support in the implementation phase. In this case, the corporation provided (limited) annual funding but did not require detailed accounting of how it was spent nor was there any accountability to employees on this question.
Assessing the possibility and capability of managers to coordinate communications and collaborations between units/departments is also important. “An organization might have all the necessary human, financial, and material resources to implement a change, yet lack the capability to mobilize, coordinate, and apply those resources in an efficacious manner to produce change” (Weiner et al., 2008, p. 425). The structure and dynamics of problem solving in these SNFs had implications for whether the completion of the intervention would happen in a timely manner. These dimensions are also difficult to assess by means of simple questions, as again the answers obtained may be those deemed socially desirable, or administrators may themselves not be highly self-conscious of their processes. This study indicates the potential value of modified assessment methods, possibly by posing brief hypothetical case studies.
Study Strengths and Limitations
The strengths include the large numbers of focus groups and CNAs from multiple sites, units, and shifts; the coordinated scripts for paired interviews and focus groups; and the follow-up evaluation of focus group data with management interviews. The ability to evaluate our criteria based on field experiences during the first year was also a strength.
The generalizability of the results may be limited to the extent that these five facilities were operated by a single corporation and were all located in the New England area. The demographic homogeneity of the administrators and DONs might be considered another limitation to generalizability, although we believe that it is not unusual for the long-term care sector to have administrators who are predominantly White and more often male than the direct care workforce. Another issue that might have more impact on generalizability is that none of these centers were unionized; we could not assess how that might have affected worker willingness to participate in the various stages of the process.
The initial selection of the five potential intervention sites was suggested by the company’s northeast regional director for health and safety, based on her subjective perceptions. The practical selection process relied primarily on assessments from interviews and focus groups, although decisions to eliminate two facilities were also informed by the researchers’ experience. One related possible weakness was the lack of explicit decision rules for grading the worksites according to the selection criteria. Nonetheless, informed judgments are likely to play some role in this process. In this case, multiple individuals weighed the available information and attempted informally to triangulate the decision making.
CONCLUSIONS
A participatory workplace intervention is challenging for an institution to carry out. We describe here a process intended to determine which facilities were suitable to undertake such a program. Our selection criteria addressed both organizational- and interpersonal/individual-level readiness and sought to assess readiness from the perspectives of multiple parties. We learned from the qualitative assessment and the first-year intervention experience regarding the revision and identified some future needs for better assessment methods for the initial criteria. While none of our initial criteria were discarded, some of them were difficult to apply because accurate information was available only to those already inside the institution. It is challenging to collect the necessary information to make appropriate judgments about the organizational readiness before starting the intervention. Nonetheless, both organizations and researchers or evaluators need to invest time in learning about an institution’s organizational and psychosocial features conductive to the effectiveness and sustainability of the intervention.
Acknowledgments
Authors’ Note: The Center for the Promotion of Health in the New England Workplace is supported by Grant No. 1 U19 OH008857the U.S. National Institute for Occupational Safety and Health (NIOSH/CDC). This work is solely the responsibility of the authors and does not necessarily represent the official views of NIOSH. The authors thank Donna LaBombard for her work as company liaison to this study and for her specific assistance in screening the centers for potential participation. Members of the ProCare research team assisted: Lara Blais and Shpend Qamili with initial analysis of focus group transcripts, and Lara Blais, Shpend Qamili, Jennifer Russell, and Michelle Holmberg with recording the Health and Wellness Team meeting minutes and field notes.
References
- Alexander JA, Weiner BJ, Shortell SM, Baker LC, Becker MP. The role of organizational infrastructure in implementation of hospitals’ quality improvement. Hospital Topics. 2006;84:11–20. doi: 10.3200/HTPS.84.1.11-21. [DOI] [PubMed] [Google Scholar]
- Ball K, Timperio AF, Crawford DA. Understanding environmental influences on nutrition and physical activity behaviors: Where should we look and what should we count? International Journal of Behavioral Nutrition and Physical Activity. 2006;3:33. doi: 10.1186/1479-5868-3-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum F, MacDougall C, Smith D. Participatory action research. Journal of Epidemiology & Community Health. 2006;60:854–857. doi: 10.1136/jech.2004.028662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics, U.S. Department of Labor. Lost-worktime injuries and illnesses: Characteristics and resulting time away from work, 2002. 2004 Retrieved from http://www.bls.gov/news.release/archives/osh2_03252004.pdf.
- Castle NG, Engberg J. Staff turnover and quality of care in nursing homes. Medical Care. 2005;43:616–626. doi: 10.1097/01.mlr.0000163661.67170.b9. [DOI] [PubMed] [Google Scholar]
- Duncan MJ, Spence JC, Mummery WK. Perceived environment and physical activity: A meta-analysis of selected environmental characteristics. International Journal of Behavioral Nutrition and Physical Activity. 2005;2:11. doi: 10.1186/1479-5868-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flum M. Involving workers in environmental decisions: A link in improving occupational health. University of Massachusetts; Lowell: 2004. (Unpublished doctoral dissertation) [Google Scholar]
- Golaszewski T, Barr D, Pronk N. Development of assessment tools to measure organizational support for employee health. American Journal of Health Behavior. 2003;27:43–54. doi: 10.5993/ajhb.27.1.5. [DOI] [PubMed] [Google Scholar]
- Kotter JP. Leading change. Boston, MA: Harvard Business Press; 1996. [Google Scholar]
- LaMontagne AD, Keegel T, Vallance D. Protecting and promoting mental health in the workplace: Developing a systems approach to job stress. Health Promotion Journal of Australia. 2007;18:221–228. doi: 10.1071/he07221. [DOI] [PubMed] [Google Scholar]
- Lavoie-Tremblay M. Creating a healthy workplace: A participatory organizational intervention. Journal of Nursing Administration. 2004;34:469–474. doi: 10.1097/00005110-200410000-00008. [DOI] [PubMed] [Google Scholar]
- Lehman WEK, Greener JM, Simpson DD. Assessing organizational readiness for change. Journal of Substance Abuse Treatment. 2002;22:197–209. doi: 10.1016/s0740-5472(02)00233-7. [DOI] [PubMed] [Google Scholar]
- Lohela M, Bjorklund C, Vingård E, Hagberg J, Jensen I. Does a change in psychosocial work factors lead to a change in employee health? Journal of Occupational and Environmental Medicine. 2009;51:195–209. doi: 10.1097/JOM.0b013e318192bd2c. [DOI] [PubMed] [Google Scholar]
- Lowe GS, Schellenberg G, Shannon HS. Correlates of employees’ perceptions of a healthy work environment. Americal Journal of Health Promotion. 2003;17:390–399. doi: 10.4278/0890-1171-17.6.390. [DOI] [PubMed] [Google Scholar]
- Mealiea L, Baltazar R. A strategic guide for building effective teams. Public Personnel Management. 2005;34:141–160. doi: 10.1177/009102600503400202. [DOI] [Google Scholar]
- Michie S, Williams S. Reducing work related psychological ill health and sickness absence: A systematic literature review. Occupational and Environmental Medicine. 2003;60(1):3–9. doi: 10.1136/oem.60.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor EJ, Fiol CM. Creating readiness and involvement. Physician Executive. 2006;32:72–74. [PubMed] [Google Scholar]
- Parboteeah K, Chen HC, Lin YT, Chen IH, Lee A, Chung A. Establishing organizational ethical climates: How do managerial practices work? Journal of Business Ethics. 2010;97:599–611. [Google Scholar]
- Pearson ML, Wu S, Schaefer J, Bonomi AE, Shortell SM, Mendel PJ, Keeler EB. Assessing the implementation of the chronic care model in quality improvement collaboratives. Health Services Research. 2005;40:978–996. doi: 10.1111/j.1475-6773.2005.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Punnett L, Cherniack M, Henning R, Morce T, Faghri P, The CPH-NEW Research Team A conceptual framework for integrating workplace health promotion and occupational ergonomics programs. Public Health Report. 2009;124(Suppl. 1):16–25. doi: 10.1177/00333549091244S103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofie J, Belza B, Young H. Health and safety risk at a skilled nursing facility: Nursing assistants’ perceptions. Journal of Gerontological Nursing. 2003;29(2):13–21. doi: 10.1016/j.jamda.2008.06.004. [DOI] [PubMed] [Google Scholar]
- Weiner BJ. A theory of organizational readiness for change. Implementation Science. 2009;4:67. doi: 10.1186/1748-5908-4-67. Retrieved from http://link.springer.com/article/10.1186%2F1748-5908-4-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner BJ, Amick H, Lee SY. Conceptualization and measurement of organizational readiness for change: A review of the literature in health services research and other fields. Medical Care Research and Review. 2008;65:379–436. doi: 10.1177/1077558708317802. [DOI] [PubMed] [Google Scholar]
- Weiner BJ, Lewis MA, Linnan LA. Using organization theory to understand the determinants of effective implementation of worksite health promotion programs. Health Education Research. 2009;24:292–305. doi: 10.1093/her/cyn019. [DOI] [PubMed] [Google Scholar]
- Wilson MG, DeJoy DM, Vandenberg RJ, Richardson HA, McGrath AL. Work characteristics and employee health and well-being: Test of a model of healthy work organization. Journal of Occupational and Organizational Psychology. 2004;77:565–588. doi: 10.1348/0963179042596522. [DOI] [Google Scholar]
- Yukl GA, Becker WS. Effective empowerment in organizations. Organization Management Journal. 2006;3:210–231. [Google Scholar]
- Zhang Y, Flum M, Nobrega S, Blais L, Qamili S, Punnett L. Work organization and health issues in long-term care centers: Comparison of perceptions between caregivers and management. Journal of Gerontological Nursing. 2011;37(5):32–40. doi: 10.3928/00989134-20110106-01. [DOI] [PMC free article] [PubMed] [Google Scholar]


