Abstract
While hospitalizations among people living with human immunodeficiency virus (PLWH) have been elevated in the past compared to their uninfected counterparts, the introduction of antiretroviral therapy (ART) has resulted in great strides in controlling symptomatic infection. However, research largely overlooks important differences among HIV-infected individuals, primarily PLWH who are symptomatic versus those who are asymptomatic. We conducted a retrospective study assessing the length of hospital stay among 717,237 admissions from three hospitals in the New York City area. Using zero-truncated negative binomial regression we documented trends in length of hospital stay among individuals who are HIV positive (with symptoms versus those without symptoms) compared to HIV-negative patients over nine consecutive years, from 2006 to 2014. Approximately 0.85% of the admissions were infected with asymptomatic HIV (n = 6,131), while 1.43% of admissions were infected with symptomatic HIV (n = 10,271). The length of stay (LOS) among symptomatic HIV-infected admissions was 32.0% (95% CI: 29.7%–34.2%) longer than LOS in the general admissions. The mean LOS dropped about 1.5% (95% CI: 1.5%– 1.6%) per year in the study sample. The LOS in inpatients with asymptomatic HIV had the same LOS as the general inpatient population. Our findings highlight the need for comprehensive strategies to reduce length of hospitalization among HIV-infected individuals.
Keywords: HIV, patient care, hospitalization
Introduction
Although the introduction of antiretroviral therapy (ART) has substantially reduced hospitalization among people living with human immunodeficiency virus ([HIV] PLWH) (Berry, Fleishman, Moore, & Gebo, 2012; Buchacz et al., 2008; Crum-Cianflone et al., 2010; Heslin & Elixhauser, 2016; Paul et al., 2002), hospitalizations among this group have still been reported to be elevated compared to individuals hospitalized with conditions other than HIV (Bachhuber & Southern, 2014; Shih, Chen, Rothman, & Hsieh, 2011). In fact, HIV-infected individuals have been twice as likely to experience hospitalization, and experience higher in-hospital mortality rates than the general inpatient population (Krentz, Dean, & Gill, 2006). Although over the past several decades, this rate has decreased substantially, partly due to the introduction of ART and the reduction of acquired immune deficiency syndrome (AIDS) (Feller, Akiyama, Gordon, & Agins, 2016; Krentz et al., 2006; Puthanakit et al., 2007; Sutton, Magagnoli, & Hardin, 2016), hospitalization rates among PLWH remain high (Berry et al., 2012), which may be extremely costly and burdensome for hospitals and insurance companies. Recent research has also indicated that hospitalization rates among PLWH have been underestimated (Bachhuber & Southern, 2014), which can erroneously mask the magnitude of suffering among this population.
While research suggests that hospitalizations among PLWH are largely manageable (Betz et al., 2005), longer duration of hospital stays are more common among this population compared to their uninfected counterparts (Akgun et al., 2013; Pearce et al., 2012). Prolonged hospital stays are also commonly associated with hospital-acquired infections among those already affected by infectious diseases (Dulworth & Pyenson, 2004; Mohammed, Furuya, & Larson, 2014). Longer stays in the hospital place a substantial burden on hospital and health insurance systems (Shih et al., 2011), typically requiring more resources for treatment (Needham et al., 2003; Papi, Pontecorvi, & Setola, 2016).
Although they are crucial to determining the extent to which PLWH are experiencing improvements in clinical outcomes, these trends in length of hospitalization largely overlook differences among HIV-infected individuals, primarily PLWH who are symptomatic versus those who are asymptomatic. Very few studies have compared trends in length of hospital stay among these populations. PLWH who are asymptomatic tend to be individuals who are HIV-positive with no previous diagnosis of opportunistic infections in accordance with the Centers for Disease Control and Prevention (CDC) Classification System (Centers for Disease Control and Prevention, 2008). Asymptomatic HIV-positive individuals tend to report a higher quality of life (Nieuwkerk et al., 2000), and are less likely to experience adverse medical outcomes (Revicki, Wu, & Murray, 1995). Given the importance of distinguishing between individuals more severely impacted by HIV (De Cock & El-Sadr, 2013), the purpose of this study was to document trends in length of hospital stay among individuals who are HIV positive (with symptoms versus those without) compared to patients who are not infected with HIV among hospitals over nine consecutive years (2006–2014) in an area with a high prevalence of HIV infection and the most heavily populated city in the U.S., New York City, NY.
Methods
The data from this study were collected retrospectively from three hospitals within the New York Presbyterian Hospital (NYP) system in New York, New York over a period of nine years, from 2006 to 2014. The NYP system is one of the largest in the area and in the U.S., currently servicing an average of more than two million patients annually. Administrative data on all inpatient characteristics and clinical outcomes were extracted from an electronic clinical data warehouse and other digital sources containing patient information, including International Classification of Diseases and Related Health Problems, 9th revisions (ICD-9) codes. More information regarding the process of data extraction has been previously described elsewhere (Apte et al., 2011). The study was approved and monitored by the Columbia University Medical Center and the Weill Cornell institutional review boards.
Measures
Data on patient characteristics included age, race and ethnicity, gender, and type of insurance plan. Data on clinical outcomes included HIV status with three categories (negative, asymptomatic or symptomatic HIV), whether the patient was in the intensive care unit (ICU) during their hospital stay, Charlson Comorbidity Index (CCI) (Charlson, Pompei, Ales, & Mackenzie, 1987), hospital of admission, and length of hospital stay (in days). The primary outcome for this study was length of hospital stay (LOS). An HIV diagnosis with symptoms was assigned using ICD-9 code 42; HIV with no symptoms was assigned using ICD-9 code V08.
Data analysis
All data analyses were performed using R software (R core team, 2013) and SAS 9.3 (SAS institute, 2010). Descriptive statistics, including frequency distributions, means and standard deviations by HIV status were used to characterize the sample. We used zero-truncated negative binomial regression to estimate length of hospital stay among three groups of inpatients (symptomatic HIV-infected, asymptomatic HIV-infected, and HIV-negative) from 2006 through 2014, controlling for their key demographic characteristics and patients’ complexity such as CCI score and ICU stay, as well as finance plan as a proxy measure of patients’ social economic status. Since positive HIV with symptoms accounts for six points in CCI score, an adjusted CCI score was created by removing HIV points to alleviate endogeneity in the final regression model. Because we are interested in the trend of length of stay over the nine years, calendar year was treated as a continuous predictor. The overall significance level was set at 0.05 for this study.
Results
A total of 717,237 adult hospital admissions were recorded (see Table 1 for sample characteristics). The vast majority of admissions were HIV-negative (97.71%). Approximately 10,271 (1.43%) of these admissions were HIV-positive with symptoms, while 6,131 admissions (0.86%) were HIV-positive without symptoms. The mean age of the admissions was 57.6 years old (SD = 19.72) with a range of 18–114 years; slightly over half (55.37%) were female. Among those who reported their racial background, the largest proportion of participants was White (30.14%). The largest proportion of admissions identified Medicare (44.90%) as their insurance type; 22.87% used Medicaid. The mean adjusted CCI among all admissions was 1.63 (SD = 2.11). Among those infected with HIV with symptoms, the mean adjusted CCI score was 1.83 (SD = 1.95), while mean score among HIV-infected asymptomatic admissions was 1.65 (SD = 1.94). The median length of stay was four days (IQR = 2–8 days) for HIV-negative inpatients, five days (IQR = 3–8 days) for asymptomatic HIV-infected participants, and six days (IQR = 4–11 days) for symptomatic HIV-infected participants.
Table 1.
Characteristics of admissions, 2006–2014 (N = 717,237).
| HIV–negative (N = 700,835) |
Asymptomatic HIV-infected (N = 6,131) |
Symptomatic HIV-infected (N = 10,271) |
Total (N = 717,237) |
|
|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | |
| Sex | ||||
| Male | 309,160 (44.11) | 4,101 (66.89) | 6,800 (66.21) | 320,061 (44.62) |
| Female | 391,667 (55.89) | 2,030 (33.11) | 3,471 (33.79) | 397,168 (55.37) |
| Age mean (SD) | 57.82 (19.82) | 49.42 (12.31) | 47.34 (10.82) | 57.59 (19.72) |
| Race | ||||
| White non-Hispanic | 214,323 (30.58) | 837 (13.65) | 1,010 (9.83) | 216,170 (30.14) |
| Hispanic | 47,263 (6.74) | 449 (7.32) | 937 (9.12) | 48,649 (6.78) |
| African-American non-Hispanic | 68,129 (9.72) | 1,546 (25.22) | 2,806 (27.32) | 72,481 (10.11) |
| Asian | 12,415 (1.77) | 16 (0.26) | 16 (0.16) | 12,447 (1.74) |
| Other | 121,156 (17.29) | 1,568 (25.57) | 3,038 (29.58) | 125,762 (17.53) |
| Unknown or decline | 237,549 (33.9) | 1,715 (27.97) | 2,464 (23.99) | 241,728 (33.7) |
| Insurance Plan | ||||
| Medicare | 316,743 (45.28) | 1,907 (31.18) | 2,804 (27.32) | 321,454 (44.9) |
| Medicaid | 154,227 (22.05) | 3,051 (49.88) | 6,476 (63.1) | 163,754 (22.87) |
| Blue Cross | 75,608 (10.81) | 314 (5.13) | 297 (2.89) | 76,219 (10.65) |
| Commercial | 136,182 (19.47) | 633 (10.35) | 556 (5.42) | 137,371 (19.19) |
| Other | 1,568 (0.22) | 80 (1.31) | 34 (0.33) | 1,682 (0.23) |
| ICU stay | 88,063 (12.57) | 632 (10.31) | 1,164 (11.33) | 89,859 (12.53) |
| Adjusted charlson index mean (SD) | 1.63 (2.11) | 2 (1.94) | 2 (1.95) | 2 (2.11) |
| Length of stay (days) median (Q1–Q3) | 4 (3.00–8.00) | 5 (3.00–8.00) | 6 (4.00–11.00) | 4 (3.00–8.00) |
| Hospital of Admission | ||||
| A | 9,279 (13.24) | 653 (10.65) | 752 (7.32) | 94,196 (13.13) |
| M | 299,166 (42.69) | 2,549 (41.58) | 5,669 (55.19) | 307,384 (42.86) |
| G | 308,878 (44.07) | 2,929 (47.77) | 3,850 (37.48) | 315,657 (44.01) |
| Admission year | ||||
| 2006 | 75,454 (10.77) | 649 (10.59) | 1,297 (12.63) | 77,400 (10.52) |
| 2007 | 75,524 (10.78) | 674 (10.99) | 1,278 (12.44) | 77,476 (10.53) |
| 2008 | 73,176 (10.44) | 565 (9.22) | 1,225 (11.93) | 74,966 (10.20) |
| 2009 | 79,365 (11.32) | 681 (11.11) | 1,244 (12.11) | 81,290 (11.07) |
| 2010 | 82,198 (11.73) | 733 (11.96) | 1,129 (10.99) | 84,060 (11.46) |
| 2011 | 82,346 (11.75) | 679 (11.07) | 1,029 (10.02) | 84,054 (11.48) |
| 2012 | 80,519 (11.49) | 790 (12.89) | 1,041 (10.14) | 82,350 (11.23) |
| 2013 | 80,296 (11.46) | 734 (11.97) | 1,096 (10.67) | 82,126 (11.20) |
| 2014 | 71,957 (10.27) | 626 (10.21) | 932 (9.07) | 73,515 (10.03) |
Over the nine years of our study, about a third of the inpatients were admitted more than once. There were 399,120 individual inpatients in total in this study: 269,866 (67.62%) were admitted once during the nine-year study period, 68,581 (17.18%) were admitted twice, and 60,673 (15.2%) were admitted more than twice.
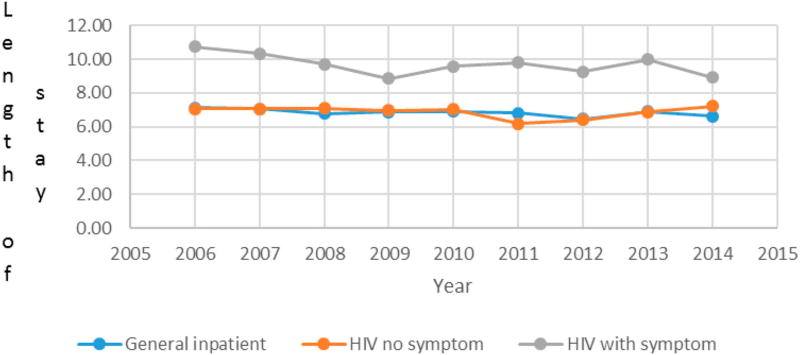
Figure 1 presents the mean LOS in the hospital by year according to HIV status. The mean LOS remained decreased among all admissions over the nine year period, regardless of their HIV status. Although all groups experienced decreases in mean LOS from 2006 to 2014, the mean LOS remained the highest among those with symptomatic HIV. Table 2 presents the zero truncated negative binomial regression results by taking the exponential of the regression coefficients, the Incidence Rate Ratio (IRR), and the corresponding 95% confidence interval. As Table 2 demonstrates, controlling for the patients’ age, sex, CCI (adjusted), insurance plan, ICU stay status and hospital of admission, the LOS among symptomatic HIV-infected patients was 32.0% (95% CI: 29.7%–34.2%) longer than LOS in the HIV-negative population. The mean LOS dropped about 1.5% (95% CI: 1.5%–1.6%) per year in the study population. The LOS in asymptomatic HIV-infected inpatients had the same LOS as the HIV-negative inpatient (see Figure 1 and Table 2).
Figure 1.
Trends in mean length of stay differentiated by HIV category.
Table 2.
Final model assessing the trend of length of stay for general inpatients, inpatients with asymptomatic HIV, and inpatients with symptomatic HIV*
| Incident Rate Ratio (IRR) |
95% CI of IRR | p-value | ||
|---|---|---|---|---|
|
| ||||
| Lower | Upper | |||
| HIV with symptoms** | 1.320 | 1.297 | 1.342 | <0.0001*** |
| HIV no symptoms | 0.979 | 0.957 | 1.001 | 0.0600 |
| Year | 0.985 | 0.984 | 0.985 | <0.0001*** |
Final zero truncated negative binomial model controlling for age, sex, race, adjusted charlson index, insurance plan, ICU stay, and hospital of admission. Calendar year was treated as a continuous variable.
HIV-negative is the reference category.
Significant at 0.05 level.
Discussion
Our findings demonstrated that between 2006 and 2014 the average length of hospitalization decreased among all inpatient populations in our study. However, our results indicated that hospitalization trends vary based on HIV status. Asymptomatic HIV inpatients generally experienced reductions in hospital LOS comparable to those of the HIV-negative inpatient population. Symptomatic HIV-infected patients still have considerably longer average length of hospitalization (Shih et al., 2011), which may be indicative of their non-adherence to their ART regimen (Fielden et al., 2008). Our results are comparable to research reporting reductions in length of hospital stay in patient populations generally (Weiss & Elixhauser, 2014) and among HIV-infected individuals specifically (Berry et al., 2012; Heslin & Elixhauser, 2016). To the best of our knowledge, our results suggesting that asymptomatic HIV patients are generally hospitalized for the same length as the general inpatient population have not been previously documented in the literature.
Our findings are subject to numerous limitations. First, our sample was derived from only a few hospitals in the New York City, New York metropolitan area. These findings may not be generalizable to other patient populations in other settings. Second, there may be additional confounders that we overlooked in our analysis, including ART adherence and reason for hospitalization. Our study is comprised of hospital administrative data which did not include clinical information such as viral loads or CD4 counts (Crum-Cianflone et al., 2010), which would have provided meaningful information on ART adherence. Finally, while we were unable to perform multilevel analyses, we would like to acknowledge that such approaches may be useful in developing a thorough understanding of the association between HIV status and length of hospitalization.
Conclusions
In conclusion, our research demonstrated that longer duration in hospital stays are decreasing among all patients, regardless of HIV serostatus. Our results are intriguing in that they suggest that the LOS among asymptomatic HIV-infected patients is comparable to that among the general inpatient population. Our findings highlight the need for comprehensive strategies to improve ART adherence among HIV-infected individuals in an effort to reduce length of hospitalization. Given the wide ranging clinical benefits of ART, sustained adherence may also result in reductions in hospital costs.
Acknowledgments
Funding
This work was supported by National Institute of Nursing Research: [grant number R01NR010822]; National Institute on Drug Abuse: [grant number K01DA036411].
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Akgun KM, Tate JP, Pisani M, Fried T, Butt AA, Gibert CL, Crothers K. Medical ICU admission diagnoses and outcomes in human immunodeficiency virus-infected and virus-uninfected veterans in the combination antiretroviral era. Critical Care Medicine. 2013;41(6):1458–1467. doi: 10.1097/CCM.0b013e31827caa46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apte M, Neidell M, Furuya EY, Caplan D, Glied S, Larson E. Using electronically available inpatient hospital data for research. Clinical and Translational Science. 2011;4(5):338–345. doi: 10.1111/j.1752-8062.2011.00353.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachhuber MA, Southern WN. Hospitalization rates of people living with HIV in the United States, 2009. Public Health Reports. 2014;129(2):178–186. doi: 10.1177/003335491412900212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry SA, Fleishman JA, Moore RD, Gebo KA, HIV Research Network Trends in reasons for hospitalization in a multisite United States cohort of persons living with HIV, 2001–2008. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2012;59(4):368–375. doi: 10.1097/QAI.0b013e318246b862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betz ME, Gebo KA, Barber E, Sklar P, Fleishman JA, Reilly ED, HIV Research Network Patterns of diagnoses in hospital admissions in a multistate cohort of HIV-positive adults in 2001. Medical Care. 2005;43(9):3–14. doi: 10.1097/01.mlr.0000175632.83060.eb. [DOI] [PubMed] [Google Scholar]
- Buchacz K, Baker RK, Moorman AC, Richardson JT, Wood KC, Holmberg SD, HIV Outpatient Study (HOPS) Investigators Rates of hospitalizations and associated diagnoses in a large multisite cohort of HIV patients in the United States, 1994–2005. Aids. 2008;22(11):1345–1354. doi: 10.1097/QAD.0b013e328304b38b. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years — United States, 2008 (Vol. 57) Atlanta, GA: U.S. Department of Health and Human Services; 2008. [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, Mackenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Crum-Cianflone NF, Grandits G, Echols S, Ganesan A, Landrum M, Weintrob A, Infectious Disease Clinical Research Program Trends and causes of hospitalizations among HIV-infected persons during the late HAART era: What is the impact of CD4 counts and HAART use? JAIDS Journal of Acquired Immune Deficiency Syndromes. 2010;54(3):248–257. doi: 10.1097/QAI.0b013e3181c8ef22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Cock KM, El-Sadr WM. When to start ART in Africa — an urgent research priority. New England Journal of Medicine. 2013;368(10):886–889. doi: 10.1056/Nejmp1300458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulworth S, Pyenson B. Healthcare-associated infections and length of hospital stay in the medicare population. American Journal of Medical Quality. 2004;19(3):121–127. doi: 10.1177/106286060401900305. [DOI] [PubMed] [Google Scholar]
- Feller DJ, Akiyama MJ, Gordon P, Agins BD. Readmissions in HIV-infected inpatients: A large cohort analysis. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2016;71(4):407–412. doi: 10.1097/Qai.0000000000000876. [DOI] [PubMed] [Google Scholar]
- Fielden SJ, Rusch ML, Yip B, Wood E, Shannon K, Levy AR, Hogg RS. Nonadherence increases the risk of hospitalization among HIV-infected antiretroviral naive patients started on HAART. Journal of the International Association of Physicians in AIDS Care. 2008;7(5):238–244. doi: 10.1177/1545109708323132. [DOI] [PubMed] [Google Scholar]
- Heslin KC, Elixhauser A. HIV hospital stays in the United States, 2006–2013 HCUP statistical brief #206. Rockville, MD: Agency for Healthcare Research and Quality; 2016. [PubMed] [Google Scholar]
- Krentz HB, Dean S, Gill MJ. Longitudinal assessment (1995–2003) of hospitalizations of HIV-infected patients within a geographical population in Canada. Hiv Medicine. 2006;7(7):457–466. doi: 10.1111/j.1468-1293.2006.00408.x. [DOI] [PubMed] [Google Scholar]
- Mohammed M, Furuya YE, Larson E. Risk of healthcare associated infections in HIV positive patients. Journal of Infection Prevention. 2014;15(6):9. doi: 10.1177/1757177414548694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Needham DM, Anderson G, Pink GH, McKillop I, Tomlinson GA, Detsky AS. A province-wide study of the association between hospital resource allocation and length of stay. Health Services Management Research. 2003;16(3):155–166. doi: 10.1258/095148403322167915. [DOI] [PubMed] [Google Scholar]
- Nieuwkerk PT, Gisolf EH, Colebunders R, Wu AW, Danner SA, Sprangers MA, Prometheus Study Group Quality of life in asymptomatic- and symptomatic HIV infected patients in a trial of ritonavir/saquinavir therapy. Aids. 2000;14(2):181–187. doi: 10.1097/00002030-200001280-00014. [DOI] [PubMed] [Google Scholar]
- Papi M, Pontecorvi L, Setola R. A new model for the length of stay of hospital patients. Health Care Management Science. 2016;19(1):58–65. doi: 10.1007/s10729-014-9288-9. [DOI] [PubMed] [Google Scholar]
- Paul S, Gilbert HM, Lande L, Vaamonde CM, Jacobs J, Malak S, Sepkowitz KA. Impact of antiretroviral therapy on decreasing hospitalization rates of HIV-infected patients in 2001. Aids Research and Human Retroviruses. 2002;18(7):501–506. doi: 10.1089/088922202317406646. [DOI] [PubMed] [Google Scholar]
- Pearce D, Ani C, Espinosa-Silva Y, Clark R, Fatima K, Rahman M, Ovbiagele B. Comparison of in-hospital mortality from acute myocardial infarction in HIV sero-positive versus sero-negative individuals. The American Journal of Cardiology. 2012;110(8):1078–1084. doi: 10.1016/j.amjcard.2012.05.045. [DOI] [PubMed] [Google Scholar]
- Puthanakit T, Aurpibul L, Oberdorfer P, Akarathum N, Kanjananit S, Wannarit P, Sirisanthana V. Hospitalization and mortality among HIV-infected children after receiving highly active antiretroviral therapy. Clinical Infectious Diseases. 2007;44(4):599–604. doi: 10.1086/510489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Revicki DA, Wu AW, Murray MI. Change in clinical status, health-status, and health utility outcomes in HIV-infected patients. Medical Care. 1995;33(4):As173–As182. [PubMed] [Google Scholar]
- Shih TY, Chen KF, Rothman RE, Hsieh YH. US national estimation of emergency department utilization by patients given “HIV/AIDS-related illness” as their primary diagnosis. Hiv Medicine. 2011;12(6):343–351. doi: 10.1111/j.1468-1293.2010.00888.x. [DOI] [PubMed] [Google Scholar]
- Sutton SS, Magagnoli J, Hardin JW. Impact of pill burden on adherence, risk of hospitalization, and viral suppression in patients with HIV infection and AIDS receiving antiretroviral therapy. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 2016;36(4):385–401. doi: 10.1002/phar.1728. [DOI] [PubMed] [Google Scholar]
- Weiss AJ, Elixhauser A. Overview of hospital stays in the United States, 2012. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [PubMed] [Google Scholar]