Abstract
Background
Quick and successful vascular access in injured patients arriving in extremis is crucial to enable early resuscitation and rapid OR transport for definitive repair. We hypothesized that intraosseous (IO) access would be faster and have higher success rates than peripheral IVs (PIVs) or central venous catheters (CVCs).
Methods
High-definition video recordings of resuscitations for all patients undergoing Emergency Department Thoracotomy (EDT) from 4/2016-7/2017 were reviewed as part of a quality improvement initiative. Demographics, mechanism of injury, access type, access location, start and stop time, and success of each vascular access attempt were recorded. Times to completion for access types (PIV, IO, CVC) were compared using Kruskal-Wallis test adjusted for multiple comparisons while categorical outcomes such as success rates by access type were compared using chi-squared test or Fisher’s exact test.
Results
Study patients had a median age of 30 (IQR 25–38), were 92% male, 92% African American, and 93% sustained penetrating trauma. A total of 145 access attempts in 38 patients occurred (median 3.8 (SD 1.4) attempts per patient). There was no difference between duration of PIV and IO attempts (0.63 IQR 0.35–0.96 vs. 0.39 IQR 0.13-0.65 minutes, adjusted p = 0.03), but both PIV and IO were faster than CVC attempts (3.2 IQR 1.72 – 5.23 minutes, adjusted p<0.001 for both comparisons). Intraosseous lines had higher success rates than PIVs or CVCs (95% vs. 42% vs. 46%, p<0.001).
Conclusions
Access attempts using IO are as fast as PIV attempts but are more than twice as likely to be successful. Attempts at CVC access in patients in extremis have high rates of failure and take a median of over 3 minutes. While IO access may not completely supplant PIVs and CVCs, IO access should be considered as a first line therapy for trauma patients in extremis.
Keywords: Intraosseous access, video review, vascualr access, trauma, extremis
Background
Vascular access may be challenging for injured patients presenting in profound hemorrhagic shock. For the majority of the 20th century, peripheral intravenous (PIV) access complemented by venous cut-down served as the standard of care for vascular access after injury (1, 2). These intravascular access techniques were supplanted by the development of percutaneous central venous catheters (CVC) in 1952 (2, 3). Despite its development in the early 1920s(4) and subsequent use in World War II, until recently intraosseous (IO) access was uncommonly utilized for vascular access in civilian populations of adult patients. (5). Of late, IO access has gained newfound popularity in part spurred by the American Heart Association (AHA) guidelines that call for prompt administration of resuscitation agents and minimal interruption of chest compressions for patients in cardiac arrest(6). In the trauma population, the modern military combat experience has led to increased attention to IO access in both clinical practice and scientific investigation (7) (5).
Although PIV, CVC, and IO are all available for use in resuscitation, there is still a paucity of data about the success rates and time to successful completion for vascular access in hypovolemic adult trauma patients. Using audiovisual review of trauma resuscitations as a part of our quality improvement efforts, we identified an opportunity for improvement in the provision of vascular access at our level I trauma center in urban Philadelphia. Philadelphia is unlike many cities in the US in that police have been allowed to transport victims of penetrating injury to trauma centers since 1996 (Philadelphia Police Department Directive 3.14, available online at http://www.phillypolice.com/accountability). Increasing numbers of penetrating trauma patients are being transported by police (8) and in such cases, patients typically arrive with limited pre-notification and no vascular access (3) (9). We noted that in patients arriving in extremis, establishing successful vascular access was challenging and often resulted in multiple failed attempts with potential delays to lifesaving therapies.
With the goal of informing guidelines for vascular access in hypovolemic trauma patients, we sought to study the real-time provision of vascular access in patients presenting to the hospital in extremis, defined for the purpose of this study as the absence of a palpable pulse or measurable blood pressure. To do this, we leveraged the utility of our existing audiovisual review program to provide enhanced prospective data collection from high fidelity audiovisual recordings of trauma resuscitations. Based on our preliminary observations, we hypothesized that intraosseous (IO) access attempts have higher success rates and are faster than peripheral IV (PIV) or central venous catheter (CVC) access attempts in this patient population.
Methods
As part of a quality improvement project targeted at better understanding the relationship between procedural quality and outcomes after resuscitative thoracotomy (RT), we reviewed high-definition video recordings (Black Diamond Video, Port Richmond, CA) of resuscitations for all patients undergoing RT from 4/2016-7/2017. Annual trauma volume at our academic level one trauma center approaches 2700 contacts per year, 21% of whom suffer penetrating injuries. The use of audiovisual recordings allowed us to collect data in a fashion similar to prospective real-time data collection except with the ability to pause, rewind, and re-review areas of ambiguity or data points missed on the first iteration (Figure 1). All videos were reviewed by one of three independent reviewers (DH, RD, KC), 10% of which were reviewed and abstracted independently to ensure agreement between times by abstractors.
Figure 1.

Representative views from the foot-of-the-bed (A) and overhead (B) HDVR cameras located in each resuscitation bay.
The primary exposure of interest was the type of vascular access attempted, categorized as PIV, IO (including tibial and humoral attempts), CVC (including internal jugular, subclavian, and femoral line attempts) or intracardiac line (ICL) attempts. Access attempt start times (needle insertion) and access attempt stop times, and the success of each attempt were also collected. The primary outcome of interest was success of the access attempt, as defined by visualization of flow of blood product or intravenous fluid through the device placed. Secondary endpoints of interest included median duration of each type of access attempt and the median time for failed access attempts by access type. Patient level variables collected for this work included demographic information (age, sex, race), mechanism of injury, injury severity (as measured by Injury Severity Score (ISS) and New Injury Severity Score (NISS)), and secondary outcomes (return of spontaneous circulation (ROSC) and mortality). We collected provider level variables including discipline (medic, physician, nurse) as well as training level (resident, fellow, or attending) for physician providers.
Demographics and descriptors of care are presented using descriptive statistics. The distribution of continuous data was visually inspected and tested for normality using Shapiro-Wilk test. We compared non-normally distributed continuous data using Kruskal-Wallis test adjusted for multiple comparisons. Categorical outcomes were compared using chi-squared or Fisher’ s exact test. We defined two-tailed statistical significance as α<0.05. Prior to initiation of data collection, this project was vetted and approved through the University of Pennsylvania institutional review board for future publication. We used Stata v14.0 for all statistical analyses (StataCorp, College Station. TX).
Results
A total of 39 patients met inclusion criteria, of whom one arrived with PIV access from the field with no further vascular access attempts; this patient was excluded from analysis. There were 145 access attempts in the remaining 38 patients in the study. Patients were predominantly African American males with penetrating mechanism of injury who were transported to the trauma center by police (Table 1). These patients were severely injured (median ISS 25 IQR 16-25; median NISS 36 IQR 25–75) and all arrived in extremis.
Table 1.
Characteristics of patients in the study.
| Patient characteristic | Included Patients n = 38 |
|---|---|
|
| |
| Age in years | 30 (IQR 25–38) |
| Male sex | 35 (92%) |
| Race | |
| African American | 35 (92%) |
| Caucasian | 1 (3%) |
| Missing | 2 (5%) |
| Injury Mechanism | |
| Gunshot wound | 31 (82%) |
| Stab wound | 4 (10%) |
| Other | 3 (8%) |
| Injury Severity Score | 25 (IQR 16–25) |
| New Injury Severity Score | 36 (IQR 25–57) |
| Prehospital Transport | |
| Police | 24 (63%) |
| Ambulance | 11 (29%) |
| Other | 3 (8%) |
Abbreviations: IQR = Interquartile range.
Each patient underwent a mean of 3.8 (SD 1.4) vascular access attempts. Of the 145 vascular access attempts overall, CVC lines (52/145, 35.8%) and IO lines (53/145, 35.8%) were most frequently undertaken. For a given patient, the first type of vascular access attempted was most often a PIV (20/38, 53.6%) followed by IO (16/38, 42.1%) and CVC (2/38, 5.3%). In examining vascular access types by provider group, physicians made the most attempts (75/145, 51%) followed by nurses (52/145, 35%) and medics (11/145, 8%). The provider type was assigned as unknown if the reviewer could not identify the insertion provider due to personal protective equipment, obstacles or omissions in the EMR. The type of vascular access attempt differed significantly (p<0.001) by provider type (Table 2). Unlike PIV or CVCs, IO line attempts were completed by a mixture of physicians (21/52, 40%), nurses (20/52, 39%), and medics (9/52, 17%).
Table 2.
Vascular attempt type by provider type.
| Provider type | IO n = 52 |
CVC n = 52 |
PIV n = 37 |
IC Line n = 4 |
p-value |
|---|---|---|---|---|---|
| Junior Resident | 10 (19.2%) | 11 (21.2%) | 2 (5.4%) | 0 (0.0%) | 0.15 |
| Senior Resident | 5 (9.6%) | 14 (26.9%) | 0 (0.0%) | 1 (25.0%) | 0.001 |
| Fellow | 2 (3.8%) | 13 (25.0%) | 0 (0.0%) | 0 (0.0%) | <0.001 |
| Attending | 4 (7.7%) | 11 (21.2%) | 0 (0.0%) | 3 (75.0%) | <0.001 |
| Nurse | 20 (38.5%) | 0 (0.0%) | 32 (86.5%) | 0 (0.0%) | <0.001 |
| Medic | 9 (17.3%) | 0 (0.0%) | 2 (5.4%) | 0 (0.0%) | 0.01 |
| Unknown | 2 (3.8%) | 3 (5.8%) | 1 (2.7%) | 0 (0.0%) | 0.90 |
Abbreviations: IO = intraosseous; CVC = central venous catheter; PIV = peripheral intravenous; IC = intracardiac. P value for Fisher’s exact test of provider type compared to all other provider types.
Success rates by type of vascular access attempt can be seen in Table 3. Data regarding outcome was missing due to obstructed camera views for 4/145 (2.7%) vascular access attempts (2 in tibial IO access attempts and 2 in subclavian CVC attempts); these cases were excluded from analyses of success rates. Overall, IO attempts were successful in 92% of attempts (38/38 (100%) in the tibia and 10/12 (83%) successful in the humerus (p = 0.01). Intracardiac lines had the next highest success rate (75%), although the overall number of these attempts was low (n=4). Peripheral IV attempts and CVC attempts had similar success rates (43% and 44% respectively). Success of CVCs did not differ by site (p=0.99) or provider type (p = 0.79). In a sensitivity analysis of success rates by access type, including both IOs with missing data as failures and both subclavian CVCs as successes, did not substantially alter our findings (success rate for IO 48/52 (92%) vs. 25/52 (48%) for CVC, p=0.001).
Table 3.
Success rates by vascular access type attempt and position.
| IV access type | n = 141 | n = 51 | n =90 | p |
|---|---|---|---|---|
| Intraosseous access | 52 (35.8%) | 2 (3.6%) | 48 (92.3%)* | <0.001 |
| Tibial | 40 | 0 (0%) | 38 (100%) | |
| Humeral | 12 | 2 (16.7%) | 10 (83.3%) | |
| Central Venous Catheter | 52 (35.8%) | 27 (51.9%) | 23 (44.2%)* | |
| Femoral | 24 | 13 (54.2%) | 11 (45.8%) | |
| Subclavian | 24 | 13 (54.2%) | 11 (45.8%) | |
| Internal Jugular | 2 | 1 (50.0%) | 1 (50.0%) | |
| Peripheral IV | 37 (25.5%) | 21 (56.8%) | 12 (43.2%)* | |
| Intracardiac Line | 4 (2.8%) | 1 (25%) | 3 (75%)* |
= statistically significant (p= 0.001) between IO, CVC, PIV and intracardiac lines, Fisher’s exact test. Success rates were not different between sites by access type (p = 0.54 for tibia vs. humeral IO, p = 0.99 for femoral vs. subclavian vs. internal jugular CVC).
The time to completion of access attempts by type of vascular access attempted can be seen in Figure 2. There was no difference between duration of PIV and IO attempts (0.63 IQR 0.35-0.96 vs. 0.39 IQR 0.13-0.65 minutes, adjusted p = 0.03), but both PIV and IO were faster than CVC attempts (3.2 IQR 1.72 – 5.23 minutes, adjusted p<0.001 for both comparisons). Most patients had either a PIV (21/38, 55%) or IO (15/38, 40%) attempt as their first access attempt.
Figure 2.
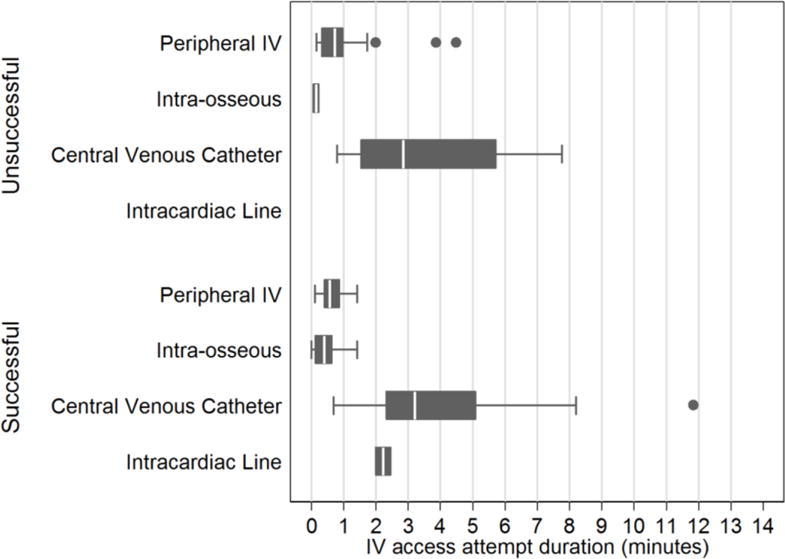
Duration of vascular access attempts in minutes by type of access attempt, stratified by successful and unsuccessful attempts. There were no significant differences in duration of successful vs. unsuccessful vascular access attempts for any vascular access type.
In total, 12/38 (32%) of patients had return of spontaneous circulation and 8 patients survived long enough to be transported to the operating room. There were two patients who survived to discharge, both of whom were neurologically intact for an overall survival rate of 5.3%. After adjusting for mechanism, we found no association between time to first vascular access completion and ROSC (OR 1.21, 95% CI 0.86–1.69).
Discussion
In this prospective observational study of intravascular access in a cohort of patients who arrived in extremis, we found that IO access attempts had a success rate of over 90% and were more than twice as likely to be successful as PIV or CVC attempts. We also found that the time required for IO access attempts and PIV access attempts was similar but both were much faster than CVC attempts.
Given the ramifications of lack of IV access in patients in shock, it is perhaps unsurprising that this topic has been the subject of many previous investigations. Engels et al. found that it took a mean of 20 minutes to successfully obtain venous access in patients presenting in hemorrhagic shock – a major potentially avoidable impediment to salvaging patients in extremis (5). While in a single center prospective observational study of 40 patients undergoing resuscitation for mixed causes in the emergency department, Leidel et al. found significantly higher success rates (85% versus 60%, p=0.024) and shorter insertion times (2.0 versus 8.0 min, p<0.001) using IO access (8). In another study examining the use of IO access in trauma patients, the majority of whom presented in extremis, Johnson et al. reported a median time to IO access of 3 minutes and was obtained first in 72% of the cases (10).
While our results qualitatively agree with these findings, we noted a higher success rate for IO (92%) and found shorter durations for both IO (median 0.39 IQR 0.16-0.65 minutes) and CVC catheters (median 3.1 IQR 1.7-5.2 minutes). While there are many possible explanations for why access attempts were faster in our study, one possibility is that not all patients in the Liedel study were in extremis, perhaps allowing for a less time-pressured approach (8).
Although IO in our experience was faster and more likely to be successful than other types of access, there are other considerations in the resuscitation of hypovolemic trauma patients which must be evaluated. Specifically, the flow rates through intraosseous catheters are known to be lower than through large bore peripheral IVs or CVC lines. The reported rates of flow through 18 gauge PIVs range from 110ml/min – 212ml/min, while flow through a CVC can be up to-600 ml/min with 8 French introducer sheaths (7) (11). In contrast, commercially available IO devices provide flow rates between 100-200 ml/min depending on insertion site (2). Proximal humerus flow rates may reach 5L/hour (83.3 ml/minute) as opposed to that of the proximal tibia which are limited to IL/hour (16.7 ml/minute) (2). There is therefore a tradeoff function between flow rates in vascular access types and the speed and likelihood of success that must be considered. Both the AHA and the American College of Surgeons (ACS) support IO access as second line therapy in the wake of failed PIV attempts (12) (13). While flow rates may be suboptimal for volume resuscitation, they are still superior to flow rates in vascular access that does not exist and provide a ready means to deliver medication and fluids until other access can be obtained. Therefore, it is reasonable to advance a position in which one or preferably more IO cannulae are placed as first line vascular access in injured adult patients with hemorrhagic shock presenting without vascular access as a bridge to more definitive access. It is plausible that resuscitation through initial IO access may improve the success of subsequent PIV and CVC access attempts by helping restore intravascular volume, but this study was not designed to address this question.
In this study, practitioners inserting IOs had a varied level of experience with insertion. Best practices regarding IO training remain unclear but combining didactic and practical training appears to be one successful option (14) (7) (15). As with many potentially perishable skills, the ideal interval between initial training and reeducation has yet to be determined. While in non-obtunded patients flushing IO access with 2% preservative free lidocaine prior to use to reduce pain is indicated, in our cohort most patients were obtunded on arrival and so this step was often eliminated in the interest of rapid initiation of resuscitation. Other studies have reported lower success rates for proximal humerus insertion relative to tibial insertion(5, 16) (2, 7, 16), but we did not find significant differences in success rates here (Table 3). Although most providers are familiar with the complications that may be incurred by PIV and CVC placement, fewer may be versed in the complications associated with IO access attempts. These issues include increased (albeit small) risk of compartment syndrome, osteomyelitis, and the potential dislodgement(2) (16) (17). Due to the short follow-up time in this study, we are not able to report the incidence of these complications here.
One of the strengths of this study is the rigor with which the data were collected. Real-time data collection on processes and sequence of care is challenging in the rapidly paced trauma bay when there are multiple coincident therapies and interventions. In such circumstances, providers charged with data collection may be unable to accurately ascertain precise nature, timing and details of events occurring during resuscitation. High-fidelity audiovisual recording of injury resuscitation captures all events in a time-stamped fashion allowing for extremely granular evaluation of care processes and performance (9) (18) (19). Audio recording provides supporting data addressing intra-team communication and critical loop closure, essential elements in assessing team leader performance and the timing of recognition of key changes in condition. While we believe that abstraction of audiovisual recordings represents a new gold standard in data collection for studies of trauma resuscitation, evidence for this contention awaits future method-comparison studies.
This study has several important limitations which must be discussed. First, as our study population was limited to patients undergoing resuscitative thoracotomy predominantly for penetrating trauma, our findings may not be generalizable to other subsets of trauma patients. Specifically, it may be inadvisable to place IO lines in the tibial location in blunt trauma patients with major lower extremity or pelvic trauma. Perhaps more importantly, it is possible that in patients with less profound hypovolemia the outcomes of PIV and CVC attempts might compare more favorably to IO attempts. However, we believe our study illustrates the “worst case” scenario, in which a patient arrives in extremis without IV access; arguably, this represents the population in which the answers to the questions we studied matter most(20, 21). We also did not track infused fluid volumes because the focus of our study was on time to vascular access and because the flow rates through the access types we describe are already well-described in the literature. We are unable to comment on how proximal saphenous vein cut-down or Seldinger technique(22) might compare to the techniques we observed here as this technique is rarely if ever practiced at our center. As expected in a cohort of patients undergoing resuscitative thoracotomy, there was an extremely high mortality rate which limits our ability to describe longer term outcomes associated with different types of IV access (23).
Conclusion
Injured patients presenting in extremis without intravascular access, IO attempts are as fast as PIV attempts but over twice as likely to be successful. CVC attempts take longer than PIV and IO attempts and are much less likely to be successful than IO attempts. Based on these findings we provisionally recommend placement of IO cannulae as a best practice to rapidly establish first line vascular access for resuscitation and as a bridge to additional access with faster flow rates as needed. Further study in other subsets of trauma patients may support an expanded role for IO access and elevation in future iterations of trauma resuscitation algorithms.
Acknowledgments
Source of Funding: DNH is currently supported by a training grant through the National Heart, Lung, and Blood Institute. (K08HL131995)
Footnotes
Conflicts of Interest: No authors have conflicts to declare.
Meetings at which this paper was presented: 76th Annual Meeting of American Association for the Surgery of Trauma, September 13-16th, 2017 in Baltimore MD
Author Contribution:
Kristen M. Chreiman MSN, Ryan P. Dumas MD, Daniel N. Holena MD MSCE, Mark J. Seamon MD, Patrick K. Kim and Patrick M Reilly MD participated in the study design. Kristen M Chreiman MSN, Ryan P Dumas MD, Daniel N Holena MD MSCE and Mark J Seamon MD participated in data collection and interpretation. Daniel N Holena MD, Ryan P Dumas MD and Jason D. Christie MD MSCE were primarily responsible for data analysis and interpretation. Kristen M Chreiman MSN, Ryan P Dumas MD, Lewis J Kaplan MD and Daniel N Holena MD MSCE were involved in the manuscript draft. All authors participated in the critical revisions and approval of the final manuscript.
References
- 1.Kalso E. A short history of central venous catheterization. Acta Anaesthesiol Scand Suppl. 1985;81:7–10. doi: 10.1111/j.1399-6576.1985.tb02313.x. [DOI] [PubMed] [Google Scholar]
- 2.Day MW. Intraosseous devices for intravascular access in adult trauma patients. Crit Care Nurse. 2011;31(2):76–89. doi: 10.4037/ccn2011615. quiz 90. [DOI] [PubMed] [Google Scholar]
- 3.Kaufman EJ, Jacoby SF, Sharoky CE, Carr BG, Delgado MK, Reilly PM, et al. Patient Characteristics and Temporal Trends in Police Transport of Blunt Trauma Patients: A Multicenter Retrospective Cohort Study. Prehosp Emerg Care. 2017:1–7. doi: 10.1080/10903127.2017.1332127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Drinker CK, Drinker KR, Lund CC. The circulation in the mammalian bone marrow. Am J Physiol. 1922;62(1):1–92. [Google Scholar]
- 5.Engels PT, Erdogan M, Widder SL, Butler MB, Kureshi N, Martin K, et al. Use of intraosseous devices in trauma: a survey of trauma practitioners in Canada, Australia and New Zealand. Can J Surg. 2016;59(6):11215. doi: 10.1503/cjs.011215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Engels PT, Passos E, Beckett AN, Doyle JD, Tien HC. IV access in bleeding trauma patients: a performance review. Injury. 2014;45(1):77–82. doi: 10.1016/j.injury.2012.12.026. [DOI] [PubMed] [Google Scholar]
- 7.Anson JA. Vascular access in resuscitation: is there a role for the intraosseous route? Anesthesiology. 2014;120(4):1015–31. doi: 10.1097/ALN.0000000000000140. [DOI] [PubMed] [Google Scholar]
- 8.Leidel BA, Kirchhoff C, Bogner V, Braunstein V, Biberthaler P, Kanz KG. Comparison of intraosseous versus central venous vascular access in adults under resuscitation in the emergency department with inaccessible peripheral veins. Resuscitation. 2012;83(1):40–5. doi: 10.1016/j.resuscitation.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 9.Oakley E, Stocker S, Staubli G, Young S. Using video recording to identify management errors in pediatric trauma resuscitation. Pediatrics. 2006;117(3):658–64. doi: 10.1542/peds.2004-1803. [DOI] [PubMed] [Google Scholar]
- 10.Fulkerson J, Lowe R, Anderson T, Moore H, Craig W, Johnson D. Effects of Intraosseous Tibial vs. Intravenous Vasopressin in a Hypovolemic Cardiac Arrest Model. West J Emerg Med. 2016;17(2):222–8. doi: 10.5811/westjem.2015.12.28825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown JB, Rosengart MR, Forsythe RM, Reynolds BR, Gestring ML, Hallinan WM, Peitzman AB, Billiar TR, Sperry JL. Not all prehospital time is equal: Influence of scene time on mortality. J Trauma Acute Care Surg. 2016;81(1):93–100. doi: 10.1097/TA.0000000000000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neumar RW, Otto CW, Link MS, Kronick SL, Shuster M, Callaway CW, Kudenchuk PJ, Oranto JP, McNally B, Silvers SM, et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S729–67. doi: 10.1161/CIRCULATIONAHA.110.970988. [DOI] [PubMed] [Google Scholar]
- 13.Subcommittee A, American College of Surgeons’ Committee on T, International Awg Advanced trauma life support (ATLS(R)): the ninth edition. J Trauma Acute Care Surg. 2013;74(5):1363–6. doi: 10.1097/TA.0b013e31828b82f5. [DOI] [PubMed] [Google Scholar]
- 14.Calkins MD, Fitzgerald G, Bentley TB, Burris D. Intraosseous infusion devices: A comparison for potential use in special operations. J Trauma. 2000;48(6):1068–74. doi: 10.1097/00005373-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 15.James Cheung W, Rosenberg H, Vaillancourt C. Barriers and facilitators to intraosseous access in adult resuscitations when peripheral intravenous access is not achievable. Acad Emerg Med. 2014;21(3):250–6. doi: 10.1111/acem.12329. [DOI] [PubMed] [Google Scholar]
- 16.Paxton JH, Knuth TE, Klausner HA. Proximal humerus intraosseous infusion: a preferred emergency venous access. J Trauma. 2009;67(3):606–11. doi: 10.1097/TA.0b013e3181b16f42. [DOI] [PubMed] [Google Scholar]
- 17.Lewis P, Wright C. Saving the critically injured trauma patient: a retrospective analysis of 1000 uses of intraosseous access. Emerg Med J. 2015;32(6):463–7. doi: 10.1136/emermed-2014-203588. [DOI] [PubMed] [Google Scholar]
- 18.Hamilton NA, Kieninger AN, Woodhouse J, Freeman BD, Murray D, Klingensmith ME. Video review using a reliable evaluation metric improves team function in high-fidelity simulated trauma resuscitation. J Surg Educ. 2012;69(3):428–31. doi: 10.1016/j.jsurg.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Wurster LA, Thakkar RK, Haley KJ, Wheeler KK, Larson J, Stoner M, Gewirtz Y, Holman T, Buckingham D, Groner JI. Standardizing the initial resuscitation of the trauma patient with the Primary Assessment Completion Tool using video review. J Trauma Acute Care Surg. 2017;82(6):1002–6. doi: 10.1097/TA.0000000000001417. [DOI] [PubMed] [Google Scholar]
- 20.Kauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma. 2006;60(6 Suppl):S3–11. doi: 10.1097/01.ta.0000199961.02677.19. [DOI] [PubMed] [Google Scholar]
- 21.Reades R, Studnek JR, Garrett JS, Vandeventer S, Blackwell T. Comparison of first-attempt success between tibial and humeral intraosseous insertions during out-of-hospital cardiac arrest. Prehosp Emerg Care. 2011;15(2):278–81. doi: 10.3109/10903127.2010.545479. [DOI] [PubMed] [Google Scholar]
- 22.Cotton BA, Jerome R, Collier BR, Khetarpal S, Holevar M, Tucker B, Kurek S, Mowery NT, Shah K, Bromberg W, et al. Guidelines for prehospital fluid resuscitation in the injured patient. J Trauma. 2009;67(2):389–402. doi: 10.1097/TA.0b013e3181a8b26f. [DOI] [PubMed] [Google Scholar]
- 23.Morse BC, Mina MJ, Carr JS, Jhunjhunwala R, Dente CJ, Zink JU, Nicholas JM, Wyrzykowki AD, Salomone JP, Vercruysse GA, et al. Penetrating cardiac injuries: A 36-year perspective at an urban, Level i trauma center. J Trauma Acute Care Surg. 2016;81(4):623–31. doi: 10.1097/TA.0000000000001165. [DOI] [PubMed] [Google Scholar]


