Abstract
Middle-aged and older adults constitute a high suicide risk group. Among adults aged 50 years old and older, suicide rates increased and suicide deaths almost doubled during the period from 2000 to 2015. Suicide rates are elevated for patients hospitalized for suicidality (i.e. active suicidal ideation or suicide attempt) and the three months post-hospitalization is the time of the highest suicide risk. Psychosocial interventions for middle-aged and older adults hospitalized for suicidality are sparse. In this article, we present the main aspects, stages, techniques and a clinical case study of Cognitive Reappraisal Intervention for Suicide Prevention (CRISP), a psychosocial intervention targeting cognitive reappraisal to reduce suicide risk in middle-aged and older adults who have been recently hospitalized for suicidal ideation or suicide attempt. CRISP is based on the theory that hospitalization for suicidality is preceded by an emotional crisis (“perfect storm”); this emotional crisis is related to personalized (patient- and situation-specific) triggers; and identifying these personalized triggers and the associated negative emotions and providing strategies for an adaptive response to these triggers and negative emotions will reduce suicidal ideation and improve suicide prevention. CRISP therapists identify these triggers of negative emotions and employ cognitive reappraisal techniques to reduce these negative emotions. The cognitive reappraisal techniques have been selected from different psychosocial interventions and the affective neuroscience literature and have been simplified for use with middle-aged and older adults. CRISP may fill a treatment need for the post-discharge high risk period for middle-aged and older adults hospitalized for suicidality.
INTRODUCTION
Suicide rates in the US have steadily increased from 2000–2015, from 10.4/100,000 in 2000 to 13.7/100,000 in 2015[1]. Middle-aged and older adults constitute a high suicide risk group. Among adults aged 50 years old and older, suicide rates increased from 13.9/100,000 in 2000 to 18.4/100,000 in 2015 and suicide deaths almost doubled during the same period. The highest risk group for suicide is among white males aged 85 years or older (suicide rate in 2015: 52.5/100,000). The increase in suicide rates of middle-aged and older adults (50 years old and older) may be a cohort effect, since “baby boomers” have had traditionally higher rates of suicide than earlier or subsequent birth cohorts[2]. As a result, the suicide rates of middle-aged and older adults may increase as this cohort becomes older.
Suicide rates are significantly elevated in patients who have been recently discharged from a psychiatric hospital. Across all age groups, recently hospitalized patients are at high suicide risk during the early post-discharge period[3], especially within the first 3 months after discharge[4,5]. In a recent study of 1,861,194 young adults [18–64 years old] of the Center for Medicare and Medicaid Services, the suicide rates for 3 months after hospital discharge were alarmingly high, e.g. 235.1/100,000 (0.235%) for patients with a diagnosis of a depressive disorder and 216/100,000 (0.216%) for bipolar disorder[6]. Suicide risk is even higher in those who have been hospitalized for suicidality (i.e. suicidal ideation or suicide attempt)[7]. The risk of suicide after hospitalization also increases in middle-aged and older adults. In a meta-analysis of 177 studies of suicide risk after hospitalization in North and South America, the risk of suicide was 1.8% (CI 1.5–2) and the risk of non-fatal repeat self-harm after hospitalization was 15.1% within one year[8]. In a study of 564 adults aged 50 years and older who died by suicide, 86 (15%) died during the first week and 154 (27%) during the first month after hospitalization[9,10]. Considering the increase in suicide rates in hospitalized patients within the 3 months of hospital discharge, it is important to develop interventions to reduce suicide risk during the early post-discharge period. The need is pressing for middle-aged and older adults, who have increased suicide mortality.
Despite the need for psychosocial interventions for suicide prevention for middle-aged and older adults hospitalized for suicidality, randomized controlled trials (RCTs) of psychotherapies or psychosocial interventions aimed specifically at reducing suicide risk after a suicide-related hospitalization for middle-aged adults are sparse[11–15], and to our knowledge there are no RCTs for older adults[16–18]. Most psychosocial interventions that have shown efficacy in reducing suicide risk focus on young adults and have been developed to treat mental disorders associated with suicide (e.g. depression, borderline personality disorder) rather than suicide risk per se. Even though treatment approaches for older adults may include psychotherapeutic techniques found effective in young adults, the presence of increased medical comorbidity and disability, decreased cognitive and physical functioning, and adjustment to significant losses of late-life highlight the need for psychotherapeutic techniques specifically for older adults[19]. Our article attempts to address this treatment gap by describing a post-discharge psychosocial intervention for middle-aged and older adults who have been hospitalized for suicidality.
Following the model of neurobiologically informed psychotherapy development of Alexopoulos and Arean[20], we relied on advances in affective neuroscience to develop a novel psychosocial intervention for suicide prevention for this population. Our intervention, entitled “Cognitive Reappraisal Intervention for Suicide Prevention (CRISP),” is based on the insight that the way people think about the situations they encounter shapes their emotional response.
Cognitive reappraisal is the ability to modify the individual’s appraisal of a situation, emotional state, or event to alter its emotional significance[21]. Biologically, cognitive reappraisal is presumed to be a behavioral expression of the Cognitive Control construct of the RDoC Cognitive System domain and to depend on an interaction between the dorsolateral prefrontal cortex (dlPFC), implicated in the governance of emotional functions, and the subcortical circuits associated with emotion processing[22,23].
We chose cognitive reappraisal as the target of the intervention because: a) suicidal ideation and behavior are frequently associated with unsuccessful attempts to regulate intense negative emotions, including depression, anxiety, hopelessness, irritability, anger, and guilt[24–29] b) cognitive reappraisal is an effective emotion regulation strategy with identified neurobiological correlates[21–30,31] ; c) higher levels of cognitive reappraisal are associated with lower suicide risk[32–34]; and d) cognitive reappraisal strategies can be effectively used to reduce suicide risk in middle-aged and older adults[12,35–37]. We place emphasis on suicidal ideation in addition to suicidal behavior, because suicidal ideation after a suicide-related hospitalization is a known significant risk factor for suicide[38]. In the present article, we will present a case study of CRISP and highlight its main aspects, stages, and clinical techniques.
METHODS
Cognitive Reappraisal Intervention for Suicide Prevention (CRISP)
CRISP’s theory of suicide prevention after hospitalization is based on the following assumptions: 1) Hospitalization for suicidality is preceded by an emotional crisis (“perfect storm”). Hospitalized patients have had difficulty dealing with this emotional crisis, leading to increased suicidal ideation and/or a suicide attempt; 2) This emotional crisis is related to personalized (patient- and situation-specific) triggers; and 3) Identifying these personalized triggers and the associated negative emotions and providing strategies for an adaptive response to these triggers and negative emotions will reduce suicidal ideation and improve suicide prevention.
CRISP is a 12-week psychosocial intervention that aims to reduce suicide risk by employing simplified, easy to administer and use, cognitive reappraisal strategies. We utilize these techniques in situations that trigger negative emotions, suicidal ideation, and suicidal behavior. These triggers include interpersonal and financial stressors, pain, disability, health-related concerns and functional impairment. Data on the feasibility, acceptability, attrition, and preliminary efficacy of CRISP compared to control will be presented in another manuscript. Of the 16 participants involved in our ongoing study, 9 (56%) completed 12 weeks of CRISP treatment without any suicidal ideation, 3 (19%) had exacerbation of symptoms or re-hospitalized, and 4 (25%) refused to continue the research assessments or were lost-to follow-up. Ten participants (63%) had an actual, interrupted or aborted suicide attempt before the index hospitalization. Participants were very satisfied with treatment (Mean Client Satisfaction Questionnaire score=3.2, out of 4, higher scores reflect higher treatment satisfaction).
CRISP focuses on middle-aged and older adults who have been hospitalized for suicidality across different depression and anxiety diagnoses. Patients eligible for CRISP include adults 50 years or older, recently admitted to a psychiatric hospital for active suicidal ideation or a suicide attempt (Columbia Suicide Severity Rating Scale ≥ 3, i.e. “Active Suicide Ideation with Some Methods”), with any depression or anxiety diagnosis. Patients who have the capacity to perform cognitive reappraisal techniques are appropriate for CRISP. CRISP is not appropriate for patients with moderate to severe cognitive impairment, with psychosis, or in manic episodes.
The selection of the cognitive reappraisal techniques used in CRISP is based on a robust body of basic affective science findings[39,40] as well as our experience in utilizing such techniques in successful interventions, i.e. Cognitive Behavior Therapy (CBT)[12,41], Dialectical Behavior Therapy (DBT)[42], and Problem Adaptation Therapy (PATH)[35], and on the affective neuroscience literature. We have selected the most salient strategies which could be easily employed by middle-aged and older adults (50 years old and older). The CRISP therapist and the patient identify and simplify cognitive reappraisal techniques, rate their effectiveness at reducing negative emotions in the therapist’s office, and create a plan to repeatedly employ and rate those techniques outside of the office, in between sessions.
CRISP’s targeted repetition and practice of individualized cognitive reappraisal strategies may contribute to long-lasting improvement in cognitive reappraisal[43]. CRISP’s cognitive reappraisal stages include: a) Identification of the “Perfect Storm”; b) Identification of situations/triggers, negative emotions and thoughts; c) Examination of the utility of negative emotions; d) Reappraisal of an emotional trigger; and e) Distancing (shifting away) from the emotional experience; and e) Reappraisal of the emotional response to the trigger (Table 1).
TABLE 1.
Cognitive Reappraisal Intervention for Suicide Prevention (CRISP): Main Stages and Techniques
| Stage | Techniques |
|---|---|
| Identification of the “perfect storm” | Overview: After obtaining information from the patient, the therapist provides a realistic explanation of the path to suicidality (suicidal ideation or suicide attempt) that led to the current hospitalization. The goal is to help the patient understand the factors that may have contributed to increased suicidality (suicidal ideation or behavior). To understand the contributing factors, the CRISP therapist creates a path that describes the association of situations/triggers, emotions, and suicidal ideation or behavior. In addition, the therapist incorporates other risk and protective factors. The patient and the therapist work through each step of the path and identify areas and time points at which they could have intervened. |
| Identification of situations/triggers and negative emotions and thoughts | Overview: The therapist asks the patient to identify situations/triggers and negative emotions that preceded, are related or linked to recent and past incidents of suicidal ideation or suicide attempt. Triggers can be external or internal events, concerns, or problems. Even if the patient cannot identify a specific emotion, the therapist focuses on the emotional experience that is related to the trigger. |
Pertinent Questions and Suggestions
| |
| Examination of the utility of negative emotions | Overview: The purpose of this stage is to understand the patient’s perspective on negative emotions and to explore the patient’s motivation to reduce these negative emotions. The examination starts by identifying the positive and negative aspects of these negative emotions. |
Pertinent Questions and Suggestions
| |
| Reappraisal of an emotional trigger | Overview: The therapist systematically evaluates and helps the patient change perspective on the emotional trigger, for example, all aspects of the trigger, positive and negative perspectives of the trigger. |
Pertinent Questions and Suggestions
| |
| Distancing (shifting away) from the emotional experience | Overview:“Distancing” is a cognitive reappraisal strategy which“involves changing one’s construal of an emotional event by increasing or decreasing one’s psychological distance from it”.30,39,42 To successfully apply this strategy, the therapist helps the patient perceive a situation or the emotional experience from an objective point of view.39,42 |
Pertinent Questions and Suggestions
| |
| Reappraisal of the emotional response to the trigger | Overview: The therapist and the patient explore the patient’s emotional reaction to the situation. The therapist may identify ways to change the patient’s perspective to reduce the patient’s negative emotional response. |
Pertinent Questions and Suggestions
|
Notes: The stages of treatment do not need to be followed sequentially, even though some of the stages appear to precipitate others. For example, it makes sense to evaluate the utility of negative emotions before you devise a plan with techniques to reduce them. Nevertheless, the therapist and the patient will work collaboratively to apply the stages necessary to reduce the negative emotions and their impact.
CRISP is different from CBT, DBT and PATH. CRISP does not utilize a comprehensive CBT approach (including cognitive case conceptualization, guided discovery, change of long-standing core maladaptive beliefs, and activity scheduling)[12,41] or DBT approach (including the DBT general skills training group, or its focus on mindfulness)[42]. CRISP is shorter than CBT for suicidal older men (which requires 12–16 weekly sessions plus 3 booster sessions) or DBT adapted for older adults[42] (weekly group DBT skills training plus 24 individual DBT sessions). CRISP is also different from PATH, because PATH targets older adults with cognitive impairment (from mild cognitive deficits to moderate dementia), utilizes a wide range of emotion regulation strategies (including situation selection, situation modification, attentional deployment, and response modulation), employs compensatory strategies for older adults with cognitive impairment, and involves the caregiver in treatment. Last but not least, CRISP is a psychosocial intervention that specifically targets suicide prevention following hospital discharge across different diagnoses (excluding psychosis and dementia) and is not designed to treat residual symptoms or mental conditions, including depression, anxiety disorders, or personality disorders. Therefore, it is administered in conjunction with other pharmacological or psychotherapeutic treatments. Once the suicide risk is significantly reduced at the end of 3 months, patients may continue to utilize other psychosocial interventions (e.g. Problem Solving Therapy, PATH, DBT, Interpersonal Psychotherapy and Supportive Therapy) to treat these conditions.
Following the recommendations of an expert panel on indicated suicide prevention in older adults[44], CRISP offers additional assistance after a suicide-related hospitalization, which include a tablet app, phone or home-delivered sessions, and phone calls for immediate help during periods of increased stress and heightened negative emotions in between sessions[44]. Therefore, even though CRISP is delivered in the therapist’s office, we offer the following two aids to enhance its effectiveness and generalizability across patients and situations:
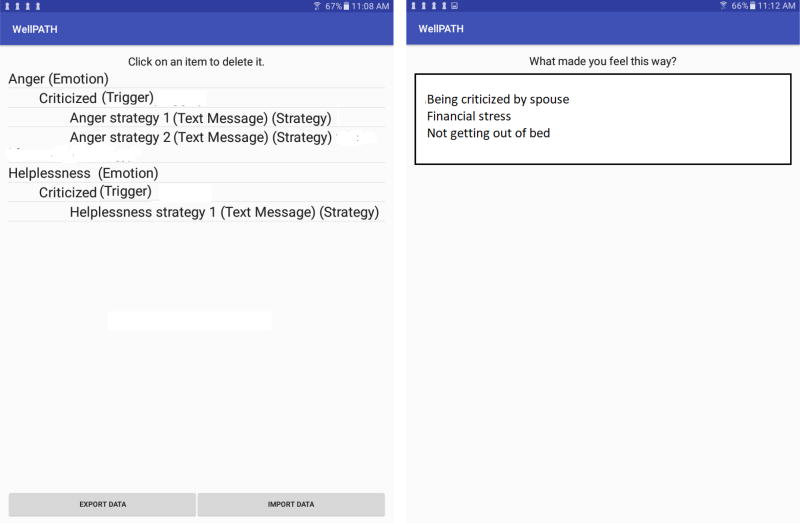
Emotion Regulation During Emotionally Charged Situations
The CRISP therapist incorporates environmental adaptations/aids to help patients improve cognitive reappraisal and regulate their emotions during emotionally charged situations outside of the office. These environmental adaptations/aids are based on patient preference and clinician recommendations. They include the utilization of the WellPATH tablet application, written step-by-step plans and phone calls. WellPATH: WellPATH is a tablet application that focuses on cognitive reappraisal strategies to reduce negative emotions when the patient faces them outside of the therapist’s office. The patient and CRISP therapist identify situations, problems, or concerns that trigger intense negative emotions and suicidal ideation, and develop a plan that includes: a) a list of cognitive reappraisal strategies; b) a video of the therapist highlighting these strategies; and c) telephone numbers to utilize if the patient has active suicidal ideation. The plan is entered into the WellPATH app and the patient takes the tablet with them (the tablets are provided by the study). For example, a patient may identify “Spouse Criticism” as the trigger, and “Worthlessness” as the negative emotion associated with the trigger. Then, the therapist and the patient develop specific text or video strategies to help the patient reduce the feeling of worthlessness and incorporate these strategies into WellPATH (Figure 1). When the patient is faced with negative emotions, and during scheduled reminders, the patient uses the app to access and utilize the pre-planned strategies. WellPATH adds to CRISP’s clinical utility by helping the patient use the CRISP techniques outside of the office when the patient needs or wants to reduce negative emotions. In addition to helping the patient, the app collects data on the frequency of use, utilization and effectiveness of strategies and change of negative emotions.
Figure 1.
Two screenshots from the WellPATH app. A flow of the triggers, emotions, and strategies (left) and a list of triggers as seen by the patient (right).
Phone or Home-Delivered Sessions
The CRISP therapist may recommend phone or home-delivered sessions in critical situations and only if an in-office session is not feasible or appropriate: 1) Concern about acute suicide risk: If the therapist and the supervising clinician are concerned about suicide risk (e.g. increased suicidal ideation), phone or even home-delivered sessions may be indicated to reduce risk. During the therapists’ visits at home, the CRISP therapist may identify triggers that are missed in office visits and may apply appropriate cognitive reappraisal techniques that take into consideration the triggers in the home-environment. 2) Disability: Disability and functional limitations are risk factors for suicide and may prevent some older patients from following weekly outpatient treatment[2]. By phone or home delivery, we aim to reach these high risk patients. 3) Ambivalence about treatment, low motivation for treatment and repeated missed appointments: Negative emotions such as hopelessness, discouragement about treatment outcome and worthlessness may interfere with the patient’s willingness and motivation to participate in treatment and to follow-through with outpatient treatment. The increase of negative emotions is especially alarming for isolated patients after their discharge, because their isolation may further contribute to increased suicide risk[45]. The option of phone or home delivery may increase patients’ access to therapy when they need it most.
CLINICAL CASE EXAMPLE
Mr. X1, a 64 year old male, was hospitalized for a suicide attempt as he tried to stab himself with a kitchen knife. The wound just missed his heart and after being hospitalized to stabilize, Mr. X was admitted to an inpatient unit with a diagnosis of Major Depressive Disorder, recurrent, severe, without psychotic features without meeting criteria for any Axis II diagnosis. He was hospitalized for 3 weeks, was treated with Lithium 600 mg, Venlafaxine 225 mg, Trazodone 100 mg and inpatient supportive group therapy and was discharged without any suicidal ideation.
Previous psychiatric history
Mr. X’s age of onset of depression was 30 years old. He had three severe episodes of major depression in his life and he had been hospitalized twelve years earlier for exacerbation of depression but not a suicide attempt. Mr. X was treated with antidepressant medications during his previous episodes of depression with modest success; he achieved remission within 2–3 months of pharmacological treatment.
CRISP Treatment
During the first two CRISP sessions after his discharge, Mr. X and the CRISP therapist identified the triggers and negative emotions that led to his suicide attempt. Mr. X had lost his job three months before his attempt, due to reduced company profits, and described a sense of anxiety and hopelessness about his financial situation. He said that he had progressively become more anxious and hopeless during the month before his attempt. (“I was afraid that I won’t be able to find a job”; “Even though I knew I was unlikely to lose my house, I was getting panicky that I may be homeless”; “My 25-year old daughter has financial difficulties and I wanted to support her”). Mr. X also reported an intense feeling of guilt about his suicide attempt.
The therapist and the patient reframed the situation that preceded the suicide attempt as a “perfect storm of negative emotions” that the patient couldn’t handle (“I thought killing myself was the only way out”). During the course of treatment, the patient and the CRISP therapist highlighted the following triggers of intense negative emotions that could lead to suicidal ideation or suicidal behavior: a) financial triggers that contribute to significant anxiety and anger towards himself and his job situation; b) social isolation that may increase his loneliness; and c) tension between Mr. X and his wife that contributed to a strong feeling of worthlessness and helplessness. Then, Mr. X and his therapist identified cognitive reappraisal strategies to improve his perspective about these situations (Table 1). Mr. X asked the following questions to help him develop cognitive reappraisal strategies: “Are the financial triggers realistic? How can I look at the financial situation from a different, third-person perspective? What do I gain by these negative emotions? What can I say to myself to reduce anxiety about the financial situation? How can I reduce my feelings of loneliness and isolation?” Mr. X incorporated the following cognitive reappraisal statements and techniques into his treatment: “Anxiety is not helping me to solve the problem. It interferes with my functioning, contributes to rumination, and prevents me from enjoying life” (utility of negative emotions). “Distancing myself from anxiety by shifting my attention to something else is helpful to me” (distancing from the emotional experience). “The tension between me and my wife is understandable under the significant amount of stress that we’re facing” (reappraisal of the emotional trigger). “She still loves me, cares for me, and is looking out for my well-being” (reappraisal of the emotional response). “Being isolated from my friends and family reinforces the anxiety and other negative emotions” (reappraisal of the emotional response). “These negative emotions were responsible for my previous suicide attempt, which was devastating for me and my family” (reappraisal of the emotional response).”
The CRISP therapist practiced the techniques in the office and rated their effectiveness in reducing Mr. X’s negative emotions. The therapist incorporated the most successful strategies into: a) a written list of techniques that the patient kept in his notebook; and b) the WellPATH app and recorded a video, in which the therapist described the detrimental effects of negative emotions in increasing suicidal ideation and emphasizing the importance of utilizing the techniques to reduce negative emotions. The patient was trained in how to use the WellPATH app, took the tablet with him and agreed that when the negative emotions become overwhelming, he would go to the tablet to help him utilize the techniques. Mr. X agreed to use both the list and the WellPATH app, and confirmed that if these did not help, he would make a phone call to the therapist. He successfully used the list but did not use the WellPATH app as he was not comfortable with technology. He used the CRISP strategies for 12 weekly sessions weeks, improved his cognitive reappraisal [(as evidenced by improved score on the Reappraisal Subscale of Emotion Regulation Questionnaire (ERQ)], reduced his negative emotions (by self-report) and prevented an increase in suicidal ideation or suicide risk over 24 weeks. The Emotion Regulation Questionnaire[46] is a self-report assessing two aspects of emotion regulation, cognitive reappraisal and suppression.
DISCUSSION
Psychosocial interventions can reduce deliberate self-harm and suicide risk after hospital discharge[47]. However, the mechanism of action through which psychosocial interventions reduce suicide risk is unknown[48]. Based on the observations that stressors from recent life events[49] (e.g. unemployment, recent loss) and negative emotions (including sadness, anxiety, shame, hopelessness and anger) related to these stressors are associated with suicidal behavior[50,51], CRISP focuses on the triggers and stressors that contribute to negative emotions that lead to the suicide attempt before the hospitalization. We assume that the stressors and negative emotions that contributed to the suicide-related hospitalization remain a significant factor for risk of suicide post-discharge, especially since the period with the highest suicide risk is within 3 months post-discharge.
The case study highlights the main stages of CRISP and the use of its techniques. First, the CRISP therapist identified the triggers of the “emotional storm” that led to the suicide attempt. The therapist carefully revisited the days that led to the suicide attempt and highlighted the triggers and the associated negative emotions leading to the suicide attempt. As soon as the triggers and the negative emotions were identified, the therapist focused mainly on those triggers and devised a plan to reduce the associated negative emotions by using cognitive reappraisal techniques. Additional negative emotions that were not directly associated with suicidal ideation or the suicide attempt could have been addressed but only after the main triggers of negative emotions and suicidal ideation were explored.
Clinically, the patient and the therapist work through the following CRISP stages. First, the patient, with the help of the therapist, identifies negative emotions related to suicidal ideation or previous suicide attempts and their triggers. Clinical data from the use of PATH techniques in older adults demonstrate that identifying emotions is easier for patients than identifying or observing their thoughts. Second, the patient records the intensity (on a scale of 1–10) and duration of these emotions and what can reduce them. Third, the patient and the therapist devise a plan and specify cognitive reappraisal techniques (Table 1) to reduce the negative emotions. Clinical experience reveal that patients are able to monitor and evaluate the degree of change (reduction or increase) of negative emotions, which facilitates the evaluation of the effectiveness of the CRISP techniques.
Executive dysfunction and poor problem solving skills have been found in depressed patients with suicidal ideation and history of suicide attempts[52]. During the “emotional storm,” patients with executive dysfunction and poor problem solving skills – who are at high risk for suicide - may not have the cognitive capacity to generate appropriate cognitive reappraisal techniques. However, the CRISP therapist and the patient can generate these techniques in session and practice them repeatedly so that the patient may use them when exposed to emotional distress in their everyday life. Recent data from the utilization of these techniques reveal that CRISP techniques may reduce the intensity of negative emotions by half even in patients with mild executive dysfunction[53].
Utilization of a tablet is an alternative way to reduce negative emotions in between sessions. By providing alternative solutions for the reduction of negative emotions during emotionally-charged situations, WellPATH allows the use of techniques even in patients who are not technologically sophisticated. This is important as the group with the highest suicide rate is white males over the age of 85; this age group may not use of technology as frequently as younger adults. As the current cohort of middle-aged get older, more patients may be willing to use technology in their treatment, which can be helpful as standalone or in conjunction with treatment[54]. Unique features of WellPATH are the identification of personalized techniques by both the patient and therapist, the practice of techniques in the office before they are incorporated into the tablet[55], and the evaluation of the effectiveness of the techniques as they are applied by the patients using the tablet.
Further development of CRISP can be informed by stakeholder input (e.g. service users, family members, clinicians) and by affective neuroscience findings. Significant figures in a patient’s life may provide information about the meaning of specific events to the patients, taking into consideration the patient’s history and psychosocial context. Such information can inform CRISP’s cognitive reappraisal interventions and increase the likelihood that the patient may incorporate his/her new views in his/her life. Advances in affective neuroscience may improve the targeting of CRISP’s cognitive reappraisal interventions. Recent findings of decision neuroscience research suggest that deficits in cognitive reappraisal may result from an incorrect estimation of a person’s life circumstances leading to impaired decision making[56]. In suicide attempters, impaired decision-making parallels disrupted expected value in reward signals in the ventromedial prefrontal cortex. Behavioral studies have linked increased delay discounting of rewards to low-lethality/poorly planned attempts and multiple attempts. In contrast, high-lethality suicide attempts have been associated with intact delay discounting but impaired social decision-making[57] and a distinct pattern of cognitive inhibition deficits[58]. A meta-analysis of neuropsychological and fMRI studies showed that abnormalities in fronto-limbic circuits are associated with vulnerability to suicide independently of any associated psychopathological conditions including depression[59] ; these circuits are implicated in cognitive reappraisal[60,61].
In conclusion, our psychosocial intervention targets cognitive reappraisal to reduce suicide risk in middle-aged and older adults who have been recently hospitalized for suicidal ideation or suicide attempt. We focus on middle-aged and older adults because suicide rates in these groups are alarmingly high. CRISP focuses on the first 3 months post-discharge because this is the period with elevated suicide rates after hospitalization. It identifies triggers of negative emotions related to suicidal ideation or previous suicide attempts, and employs cognitive reappraisal techniques to reduce these negative emotions. Our cognitive reappraisal techniques, originated from affective neuroscience literature, have been selected from different psychosocial interventions (e.g., CBT, DBT, PATH) and have been simplified for use in middle-aged and older adults. Since psychosocial interventions focusing on middle-aged and older adults who have been recently hospitalized for suicidality are sparse, we hope that CRISP may reduce suicide risk at the post-discharge period where the patients are particularly vulnerable to suicide.
Acknowledgments
This work was supported by the following grants: NIMH R61 MH110542 (PI: D.N.Kiosses) & R01 MH091045 (PI: D.N. Kiosses), American Foundation for Suicide Prevention (PI: D. N. Kiosses), NARSAD (PI: D. N. Kiosses), and NIMH P30 MH085943 (PI: G.S. Alexopoulos).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Clinical Trials Registration
Official Title: A Novel Cognitive Reappraisal Intervention for Suicide Prevention (CRISP)
Identifier: NCT03026127
Disclosures: Dr. Alexopoulos has served on the speakers’ bureaus of Astra Zeneca, Novartis, Sunovion, and Takeda-Lundbeck. The rest of the authors do not have any financial relationships with commercial interests.
Contributor Information
Dimitris N. Kiosses, Psychology in Clinical Psychiatry, Weill-Cornell Institute of Geriatric Psychiatry, Weill Cornell Medical College.
George S. Alexopoulos, Psychiatry, Weill-Cornell Institute of Geriatric Psychiatry, Weill Cornell Medicine.
Greg Hajcak, Biomedical Sciences and Psychology, Florida State University.
William Apfeldorf, Clinical Psychiatry, Weill-Cornell Institute of Geriatric Psychiatry, Weill Cornell Medicine.
Paul R. Duberstein, Psychiatry and Family Medicine, University of Rochester Medical Center.
David Putrino, Rehabilitation Medicine, Mount Sinai Health System.
James J. Gross, Psychology, Stanford University.
References
- 1.Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. [Accessed April, 26, 2016];Web-based Injury Statistics Query and Reporting System (WISQARS) [online] Available from: http://www.cdc.gov/injury/wisqars/fatal_injury_reports.html.
- 2.Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatr Clin N Am. 2011;34:451–68. doi: 10.1016/j.psc.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bostwick JM, Pankratz VS. Affective disorders and suicide risk: A re-examination. Am J Geriatr Psychiatry. 2000;157:1925–1932. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- 4.Karvonen K, Rasanen P, Hakko H, et al. Suicide after hospitalization in the elderly: A population based study of suicides in Northern Finland between 1988–2003. Int J Geriatr Psychiatry. 2008;23:135–141. doi: 10.1002/gps.1853. [DOI] [PubMed] [Google Scholar]
- 5.Erlangsen A, Mortensed PB, Vach W, et al. Psychiatric hospitalization and suicide in the very old in Denmark: population-based register study. Br J Psychiatry. 2005;187:43–48. doi: 10.1192/bjp.187.1.43. [DOI] [PubMed] [Google Scholar]
- 6.Olfson M, Wall M, Wang S, et al. Short-term suicide risk after psychiatric hospital discharge. JAMA Psychiatry. 2016;73(11):1119–1126. doi: 10.1001/jamapsychiatry.2016.2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chung DT, Ryan CJ, Hadji-Pavlovic D, et al. Suicide rates after discharge from psychiatric facilities. A systematic review and meta-analysis. JAMA Psychiatry. 2017 doi: 10.1001/jamapsychiatry.2017.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carroll R, Metcalfe C, Gunnell D. Hospital presenting self-harm and risk of fatal and non-fatal repetition: A systematic review and meta-analysis. PLoS One. 2014;9(2) doi: 10.1371/journal.pone.0089944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karvonen K, Hakko H, Koponen H, et al. Suicides among older persons in Finland and time since hospitalization discharge. Psychiatr Serv. 2009;60:390–3. doi: 10.1176/ps.2009.60.3.390. [DOI] [PubMed] [Google Scholar]
- 10.Karvonen K, Rasanen P, Hakko H, et al. Suicide after hospitalization in the elderly: A population based study of suicides in Northern Finland between 1988–2003. Int J Geriatr Psychiatry. 2008;23:135–141. doi: 10.1002/gps.1853. [DOI] [PubMed] [Google Scholar]
- 11.Brown GK, Jager-Hyman S. Evidence-based psychotherapies for suicide prevention: Future directions. Am J Prev Med. 2014;47:S186–94. doi: 10.1016/j.amepre.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Brown GK, Ten Have T, Henriques GR, et al. Cognitive therapy for the prevention of suicide attempts: A randomized controlled trial. JAMA. 2005;294:563–70. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- 13.Linehan MM, Korslund KE, Harned MS, et al. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: A randomized clinical trial and component analysis. JAMA Psychiatry. 2015;72:475–82. doi: 10.1001/jamapsychiatry.2014.3039. [DOI] [PubMed] [Google Scholar]
- 14.Hawton K, Townsend E, Arensman E, et al. Psychosocial versus pharmacological treatments for deliberate self harm. Cochrane Database Syst Rev. 2000;(2):CD001764. doi: 10.1002/14651858.CD001764. [DOI] [PubMed] [Google Scholar]
- 15.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: A systematic review. JAMA. 2005;294:2064–74. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 16.Lapierre S, Erlangsen A, Waern M, et al. International Research Group for Suicide among the Elderly: A systematic review of elderly suicide prevention programs. Crisis. 2011;32:88–98. doi: 10.1027/0227-5910/a000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Celano CM, Beale EE, Mastromauro CA, et al. Psychological interventions to reduce suicidality in high-risk patients with major depression: A randomized controlled trial. Psychol Med. 2017;47:810–821. doi: 10.1017/S0033291716002798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Riblet NBV, Shiner B, Young-Xu Y, et al. Strategies to prevent death by suicide: Meta-analysis of randomised controlled trials. Br J Psychiatry. 2017 doi: 10.1192/bjp.bp.116.187799. [DOI] [PubMed] [Google Scholar]
- 19.Heisel MJ, Talbot NL, King DA, et al. Adapting interpersonal psychotherapy for older adults at risk for suicide. Am J Geriatr Psychiatry. 2015;23:87–98. doi: 10.1016/j.jagp.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alexopoulos GS, Arean P. A model for streamlining psychotherapy in the RDoC era: The example of 'Engage'. Mol Psychiatry. 2014;19(1):14–9. doi: 10.1038/mp.2013.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gross JJ. In: Emotion regulation: Conceptual and empirical foundations, in Handbook of Emotion Regulation. 2. Gross JJ, editor. New York, NY: Guilford; 2014. pp. 3–20. [Google Scholar]
- 22.Morris JS, Frith CD, Perrett DI, et al. A differential neural response in the human amygdala to fearful and happy facial expressions. Nature. 1996;383:812–815. doi: 10.1038/383812a0. [DOI] [PubMed] [Google Scholar]
- 23.Phan KL, Wager T, Taylor SF, et al. Functional neuroanatomy of emotion: A meta-analysis of emotion activation studies in PET and fMRI. NeuroImage. 2002;16:331–348. doi: 10.1006/nimg.2002.1087. [DOI] [PubMed] [Google Scholar]
- 24.Cukrowicz KC, Duberstein PR, Vannoy SD, et al. Course of suicide ideation and predictors of change in depressed older adults. J Affect Disord. 2009;113:30–6. doi: 10.1016/j.jad.2008.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heisel MJ, Flett GL, Besser A. Cognitive functioning and geriatric suicide ideation: Testing a mediational model. Am J Geriatr Psychiatry. 2002;10:428–36. [PubMed] [Google Scholar]
- 26.Lynch TR, Cheavens JS, Morse JQ, et al. A model predicting suicidal ideation and hopelessness in depressed older adults: The impact of emotion inhibition and affect intensity. Aging Ment Health. 2004;8:486–97. doi: 10.1080/13607860412331303775. [DOI] [PubMed] [Google Scholar]
- 27.Hill RD, Gallagher D, Thompson LW, et al. Hopelessness as a measure of suicide intent in the depressed elderly. Psychol Aging. 1988;3:230–2. doi: 10.1037/0882-7974.3.3.230. [DOI] [PubMed] [Google Scholar]
- 28.Szanto K, Reynolds CF, III, Conwell Y, et al. High levels of hopelessness persist in geriatric patients with remitted depression and a history of attempted suicide. J Am Geriatr Soc. 1998;46:1401–6. doi: 10.1111/j.1532-5415.1998.tb06007.x. [DOI] [PubMed] [Google Scholar]
- 29.Lynch TR, Johnson CS, Mendelson T, et al. Correlates of suicidal ideation among an elderly depressed sample. J Affect Disord. 1999;56:9–15. doi: 10.1016/s0165-0327(99)00022-1. [DOI] [PubMed] [Google Scholar]
- 30.Webb TL, Miles E, Sheeran P. Dealing with feeling: A meta-analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychol Bull. 2012;138:775–808. doi: 10.1037/a0027600. [DOI] [PubMed] [Google Scholar]
- 31.Ochsner KN, Gross JJ. Cognitive emotion regulation: Insights from social cognitive and affective neuroscience. Curr Dir Psychol Sci. 2008;17:153–158. doi: 10.1111/j.1467-8721.2008.00566.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Forkmann T, Scherer A, Böcker M, et al. The relation of cognitive reappraisal and expressive suppression to suicidal ideation and suicidal desire. Suicide Life Threat Behav. 2014;44:524–36. doi: 10.1111/sltb.12076. [DOI] [PubMed] [Google Scholar]
- 33.Kudinova AY, Owens M, Burkhouse KL, et al. Differences in emotion modulation using cognitive reappraisal in individuals with and without suicidal ideation: An ERP study. Cogn Emot. 2015;15:1–9. doi: 10.1080/02699931.2015.1036841. [DOI] [PubMed] [Google Scholar]
- 34.Kalichman SC, Heckman T, Kochman A, et al. Depression and thoughts of suicide among middle-aged and older persons living with HIV-AIDS. Psychiatr Serv. 2000;51:903–7. doi: 10.1176/appi.ps.51.7.903. [DOI] [PubMed] [Google Scholar]
- 35.Kiosses DN, Ravdin LD, Gross JJ, et al. Problem Adaptation Therapy (PATH) for older adults with major depression and cognitive impairment: A randomized clinical trial. JAMA Psychiatry. 2015;72:22–30. doi: 10.1001/jamapsychiatry.2014.1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhar S, Brown GK. Treatment of depression and suicide in older adults. Cogn Behav Pract. 2012;19:116–125. [Google Scholar]
- 37.Kiosses DN, Rosenberg PB, McGovern A, et al. Depression and Suicidal ideation during two psychosocial treatments in older adults with major depression and dementia. J Alzheimers Dis. 2015;48:453–462. doi: 10.3233/JAD-150200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beghi M, Rosenbaum JF, Cerri C, et al. Risk factors for fatal and nonfatal repetition of suicide attempts: A literature review. Neuropsychiatr Dis Treat. 2013;9:1725–36. doi: 10.2147/NDT.S40213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- 40.Denny BT, Inhoff MC, Zerubavel N, et al. Getting over it: Long-lasting effects of emotion regulation on amygdala response. Psychol Sci. 2015;26:1377–88. doi: 10.1177/0956797615578863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bhar S, Brown GK. Treatment of depression and suicide in older adults. Cog Behav Pract. 2012;19:116–125. [Google Scholar]
- 42.Lynch TR, Morse JQ, Mendelson T, et al. Dialectical behavior therapy for depressed older adults: A randomized pilot study. Am J Geriatr Psychiatry. 2003;11:33–45. [PubMed] [Google Scholar]
- 43.Denny BT, Ochsner KN. Behavioral effects of longitudinal training in cognitive reappraisal. Emotion. 2014;14:425–33. doi: 10.1037/a0035276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Erlangsen A, Nordentoft M, Conwell Y, et al. International Research Group on Suicide Among the Elderly. Key considerations for preventing suicide in older adults: Consensus opinions of an expert panel. Crisis. 2011;32:106–9. doi: 10.1027/0227-5910/a000053. [DOI] [PubMed] [Google Scholar]
- 45.Draper BM. Suicidal behaviour and suicide prevention in later life. Maturitas. 2014;79:179–183. doi: 10.1016/j.maturitas.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85:348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- 47.Calati R, Courtet P. Is psychotherapy effective for reducing suicide attempt and non-suicidal self-injury rates? Meta-analysis and meta-regression of literature data. J Psychiatr Res. 2016;79:8–20. doi: 10.1016/j.jpsychires.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 48.Oquendo MA, Courtet P. Suicidal behaviour: Identifying the best preventive interventions. Lancet Psychiatry. 2015;2:5–6. doi: 10.1016/S2215-0366(14)00059-5. [DOI] [PubMed] [Google Scholar]
- 49.Hunt IM, Kapur N, Webb R, et al. Suicide in recently discharged psychiatric patients: a case-control study. Psychol Med. 2009;39:443–9. doi: 10.1017/S0033291708003644. [DOI] [PubMed] [Google Scholar]
- 50.Conner KR, Conwell Y, Duberstein PR, et al. Aggression in suicide among adults ages 50 and over. Am J Geriatr Psychiatry. 2004;12:37–42. [PubMed] [Google Scholar]
- 51.Duberstein PR, Conwell Y, Conner KR, et al. Suicide at 50 years of age and older: Perceived physical illness, family discord, and financial strain. Psychol Med. 2004;44:137–146. doi: 10.1017/s0033291703008584. [DOI] [PubMed] [Google Scholar]
- 52.Gujral S, Dombrovski AY, Butters M, et al. Impaired executive function in contemplated and attempted suicide in late life. Am J Geriatr Psychiatry. 2014;22:811–819. doi: 10.1016/j.jagp.2013.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kiosses DN, Hajcak G, Gross JJ, et al. Suicide prevention in hospitalized middle-aged and older adults. International College of Geriatric Psychopharmacology (ICGP), held in Chicago IL. 2017 Oct 4–7; [Google Scholar]
- 54.Cuijpers P, Kleiboer A, Karyotaki E, et al. Internet and mobile interventions for depression: Opportunities and challenges. Depress Anxiety. 2017 doi: 10.1002/da.22641. [DOI] [PubMed] [Google Scholar]
- 55.Lui JHL, Marcus DK, Barry CT. Evidence-based apps? A review of mental health mobile applications in a psychotherapy context. Prof Psychol Res Pr. 2017;48:199–210. [Google Scholar]
- 56.Dombrovski AY, Hallquist MN. The decision neuroscience perspective on suicidal behavior: Evidence and hypotheses. Curr Opin Psychiatry. 2017;30:7–14. doi: 10.1097/YCO.0000000000000297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dombrovski AY, Hallquist MN. The decision neuroscience perspective on suicidal behavior: Evidence and hypotheses. Curr Opin Psychiatry. 2017;30:7–14. doi: 10.1097/YCO.0000000000000297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Richard-Devantoy S, Szanto K, Butters MA, et al. Cognitive inhibition in older high-lethality suicide attempters. Int J Geriatr Psychiatry. 2015;30(3):274–83. doi: 10.1002/gps.4138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Richard-Devantoy S, Jollant F, Deguigne F, et al. Neurocognitive markers of suicide vulnerability in the elderly: A review. Geriatr Psychol Neuropsychiatr Vieil. 2013;11(4):367–78. doi: 10.1684/pnv.2013.0442. [DOI] [PubMed] [Google Scholar]
- 60.Morris JS, Frith CD, Perrett DI, et al. A differential neural response in the human amygdala to fearful and happy facial expressions. Nature. 1996;383:812–815. doi: 10.1038/383812a0. [DOI] [PubMed] [Google Scholar]
- 61.Phan KL, Wager T, Taylor SF, et al. Functional neuroanatomy of emotion: A meta-analysis of emotion activation studies in PET and fMRI. NeuroImage. 2002;16:331–348. doi: 10.1006/nimg.2002.1087. [DOI] [PubMed] [Google Scholar]