Abstract
Survivorship care plans (SCPs) have been recommended as tools to improve care coordination and outcomes for cancer survivors. SCPs are increasingly being provided to survivors and their primary care providers. However, most primary care providers remain unaware of SCPs, limiting their potential benefit. Best practices for educating primary care providers regarding SCP existence and content are needed. We developed an education program to inform primary care providers of the existence, content, and potential uses for SCPs. The education program consisted of a 15-min presentation highlighting SCP basics presented at mandatory primary care faculty meetings. An anonymous survey was electronically administered via email (n = 287 addresses) to evaluate experience with and basic knowledge of SCPs pre-and post-education. A total of 101 primary care advanced practice providers (APPs) and physicians (35% response rate) completed the baseline survey with only 23% reporting prior receipt of a SCP. Only 9% could identify the SCP location within the electronic health record (EHR). Following the education program, primary care physicians and APPs demonstrated a significant improvement in SCP knowledge, including improvement in their ability to locate one within the EHR (9 vs 59%, p < 0.0001). A brief educational program containing information about SCP existence, content, and location in the EHR increased primary care physician and APP knowledge in these areas, which are prerequisites for using SCP in clinical practice.
Keywords: Survivorship care plans, Primary care providers, Education program, Cancer survivor, Communication
Introduction
The Institute of Medicine published their landmark report, “From Cancer Patient to Cancer Survivor: Lost in Transition,” highlighting the need for improved communication and care coordination between oncologists and primary care in 2005 [1]. One recommendation from this report was that survivorship care plans (SCPs) be provided to all cancer survivors, along with a copy to each survivor’s primary care provider. SCPs are documents that provides summaries of [1] cancer diagnosis, [2] cancer treatment, and [3] recommendations for follow-up care. SCPs may be tools to improve communication and care coordination between oncology and primary care as patients move from active cancer treatment to a focus on survivorship. However, the decade since the IOM’s report has been marked by controversy regarding the potential benefits of SCPs and how to measure these benefits, along with the efficiency of coordination.
The electronic health record (EHR) has evolved as a central repository of patient information and as a tool for communication with patients and coordination between health care teams. As a result, the American Society of Clinical Oncology (ASCO) has advocated utilizing the EHR in order to generate and provide SCPs to survivors and primary care providers [2]. In previous research, we reported that primary care providers identified receipt via the EHR as the preferred method for delivery of SCPs [3]. However, a significant percentage of primary care providers lacked knowledge of SCPs or were unaware that they received one for a survivor followed by their practice. The Engineering, Primary care, and Oncology Collaborative for Survivorship Health (EPOCH) formed to address ongoing survivorship health needs, such as improvements in SCP design and provision, at the University of Wisconsin. This Collaborative seeks to incorporate unique primary care perspectives into optimizing the care of cancer survivors.
As the first initiative of this Collaborative, we created a primary care-directed education program. This education program was designed to increase primary care physician and advanced practice provider (APP) knowledge regarding SCP existence, content, and potential use as a clinical decision-making tool. Here, we report the impact of this education program on primary care physician and APP reported knowledge as reflected by the change between pre- vs post-education program surveys.
Methods
Setting
UW Health is the integrated health system of the University of Wisconsin-Madison (UW) serving more than 600,000 patients each year in the Upper Midwest and beyond, and employing 1400 physicians plus 16,500 staffs. This includes the Carbone Cancer Center, an NCI-designated comprehensive cancer center with accreditation from the American College of Surgeons-Commission on Cancer (CoC) and participation in the National Comprehensive Cancer Network (NCCN). All UW Health patients are assigned a primary care physician; physicians work in collaborative primary care teams including nurse practitioner and physician assistant APPs. The UW Department of Family Medicine and Community Health (FM) has 20 statewide clinics. The UW Division of General Internal Medicine (GIM) has nine clinics in Dane County and one regional clinic. UW Health utilizes an identical EHR interface between the in-patient and out-patient setting as well as at regional clinics.
EHR-Based SCPs
Since July 2015, UW Health has leveraged the EHR in generating SCPs for all curatively treated breast cancer survivors, with additional survivor types being added annually (e.g., colorectal cancer in 2016, prostate and gynecologic cancers in 2017). Each SCP is auto-populated using diagnosis and treatment data previously entered into the EHR for clinical use, typically by treating physicians throughout the course of cancer diagnosis and treatment [4]. When active treatment ends, an individualized SCP document is created within the EHR for each survivor. An EHR-based SCP template pulls diagnosis and treatment data along with pre-populated text about follow-up recommendations, future and chronic side effects, and additional resources, which is further individualized as necessary.
This individualized SCP document is provided to the survivor (as a printed document and/or via the electronic patient health portal) within the context of a care planning visit [5]. As recommended, each survivor’s primary care physician also receives a copy of this individualized SCP. In the case of UW Health primary care physicians, receipt is electronic within the EHR’s internal communication and task-management system. Individualized SCPs are permanently associated with the cancer diagnosis in each survivor’s problem list and visible to members of the healthcare team with EHR access. Because the EHR generates the SCPs, it can rapidly generate lists of survivors who have received SCPs and the date(s) of receipt [6].
Engineering-Primary Care-Oncology Initiative
The UW Collaborative for Survivorship Health formed in 2015 under guidance from the UW’s GIM and oncology leadership. EPOCH’s first quality improvement (QI) initiative targeted improving SCP utilization and facilitating communication and coordination between primary care and oncology teams with input from human factors engineers. Because prior research demonstrated that lack of awareness of SCP existence was a key barrier to primary care SCP utilization, the Collaborative designed an education program targeting UW Health primary care physicians and APPs. The education program’s objective was to increase primary care physician and APP knowledge regarding SCP existence, content, and potential use as a clinical decision-making tool.
Primary-Care Directed SCP Education Program
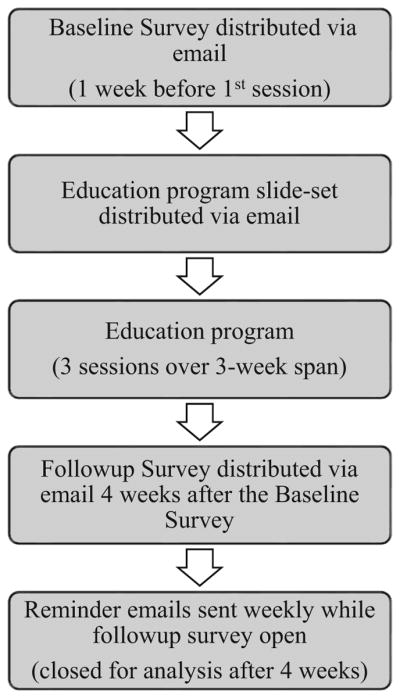
Figure 1 outlines the education program initiative. The surveys and subsequent results were exempted from UW institutional research board (IRB) review based on QI project status.
Fig. 1.
Schema
Participants
The education program targeted the two largest UW primary care specialties, FM and GIM. The 15-min education program was presented to each department as part of a regularly scheduled mandatory departmental meeting. All FM and GIM physicians and APPs are expected to participate in these mandatory meetings. Participating FM included 203 physicians and APPs at clinics in Dane County (including resident physicians at the Madison, WI, residency clinics) and surrounding regional clinics in Fort Atkinson, Beaver Dam, and Portage, WI. Participating GIM consisted of 84 physicians and APPs (internal medicine residents were not included) for a total of 287 FM and GIM providers.
Education Program Materials
A 10-min presentation outlining the reasoning behind, content of, and location within the EHR of SCPs was given by a primary care physician (author JEH) specializing in cancer survivorship (see Supplemental Material 1). A 5-min question-answer session immediately followed. Three education program sessions were held. The presentation slide-set was provided to primary care physicians and APPs via the FM and GIM email listservs prior to the education program sessions.
Outcomes
We assessed the education program’s impact using electronic pre- and post-session surveys of primary care physicians and APPs (Fig. 1). The baseline survey consisted of 10 multiple-choice questions assessing knowledge about (1) which providers and/or cancer patients could be expected to receive SCPs, (2) the timing of SCP provision, (3) expected SCP content, and (4) location of SCPs in the UW Health EHR. This survey also contained one free text question for primary care physicians and APPs who reported previously receiving SCPs, “When you reviewed that Survivorship Care Plan, what if any change(s) occurred in your knowledge or clinical decision making?” The follow-up survey consisted of the same 10 multiple-choice questions reassessing primary care knowledge, and one free text question for primary care physicians and APPs “Thinking about how patients might use Survivorship Care Plans, do you have any suggestions for how we might improve them?” Supplemental Material 2 contains both surveys.
Baseline surveys were sent to all primary care physicians and APPs on the FM and GIM listservs (n = 287) at least 1 week before the education program sessions, while follow-up surveys were sent 1 week following the last education program session (4 weeks following the baseline survey). Survey responses were closed for analysis roughly 4 weeks after the follow-up survey was distributed. We sought to evaluate the impact on clinically active primary care physicians and APPs receiving the educational program. Therefore, the baseline survey terminated if the respondent was not clinically active and the follow-up survey terminated if the respondent had not attended the education program or reviewed the slide-set. Surveys were administered by the UW Cancer Prevention and Outcomes Data (C-POD) services using Qualtrics. Surveys were anonymous; however, C-POD matched and linked the pre- and post-survey data for respondents who completed both.
Statistical Analysis
The proportions of correctness of responses to questions at baseline and at follow-up for all respondents were compared with Fisher’s exact tests due to small cell counts. The proportions of correctness of responses to questions at baseline and follow-up for matched respondents were compared with McNemar’s tests for pairing effects. A single author (SMD) reviewed all free text answers and performed an inductive thematic analysis to group respondent comments to the free text questions (“Thinking about how patients might use survivorship care plans, do you have any suggestions for how we might improve them?” and for those PCPs who reported receiving a SCP in the past “When you reviewed that Survivorship Care Plan, what, if any, change(s) occurred in your knowledge or clinical decision making?”). The thematic analysis was then reviewed and revised (as necessary) by authors JEH and AJT.
Results
The education program sessions (n = 3) were completed within a 3-week timespan. The first two sessions took place on May 4th, 2016 and were attended by 76 participants from FM and 65 from GIM, respectively. An additional education program session took place on May 25th and was attended by 50 FM participants. Thus, at least 191 physicians and APPs attended the education program in person over the course of 3 weeks. The education program slide-set was also sent to physicians and APPs via the FM and GIM listservs (n = 287).
Respondent Characteristics
The baseline survey was completed by 101 respondents (35% response rate) prior to attending the education program, of whom 80 (79%) were physicians and 21 (21%) were APPs. The median number of days/week in clinic was three (range 0.5–5 days/week). The follow-up survey had 66 respondents, (83% physicians), with a median number of days/week in clinic of 3.5 (range 0.5–5 days/week).
Baseline Knowledge
The baseline survey examined pre-existing knowledge of SCP existence, content, and identified uses and clinical utilization, all from the perspective of primary care physicians and APPs.
SCP Location and Content
With regards to pre-existing knowledge at baseline, 27 respondents (27%) reported not knowing what SCPs were, 50 (50%) knew but reported never receiving one, while only 23 respondents (23%) reported having received one. Only nine respondents (9%) reported knowing where to locate a SCP within the EHR. When asked about information a SCP should contain, 76 respondents (75%) correctly identified them as containing recommendations for follow-up and screening, while 18 respondents (18%) reported not knowing.
SCP-Intended Recipients and Timing of Delivery
Eighty-seven respondents (86%) selected both the cancer survivor and PCP as the intended recipients of a SCP. However, only 26 respondents (26%) correctly selected cancer patients treated with curative intent as the population who would be receiving SCPs. Likewise, only 25 respondents (25%) were able to correctly identify the timing of SCP delivery as being at the end of active cancer treatment.
Prior Receipt of SCPs
Of the 23 respondents who reported previously receiving a SCP, 22 provided a response to the free text question “When you reviewed that Survivorship Care Plan, what, if any, change(s) occurred in your knowledge or clinical decision making?” General themes were compiled and included SCPs providing useful guidance as follows:
impact on scheduled follow-up, e.g. “better idea of any follow-up testing … to monitor for recurrence or chemo side effects.”
impact on screening recommendations, e.g. “useful guidance re: follow up screening” and
updating the patient’s problem list to reflect primary care responsibilities, e.g. “better understanding of what the oncologist was planning to follow.”
In general, feedback regarding the provision of SCPs was positive and primary care physician and APPs expressed interest in better communication with oncology sub-specialists as follows: “I think the new breast cancer transition [referring to survivorship care planning visits] after chemo and radiation has been really helpful for patients and should be a model for other types of cancer where chemotherapy and/or radiation therapy has been done.”
Change in Knowledge
Sixty-six respondents (23% response rate) completed the follow-up survey after attending the education program or reviewing the slide-set. Thirty-nine respondents that completed the baseline survey were identified as also completing the follow-up survey. These 39 “matched” respondents were linked by C-POD using the Qualtrics software to protect respondent anonymity. The change between baseline and follow-up for respondents as a whole is shown in Table 1. Statistically significant improvements were noted in all areas except with regards to the percentage correctly selecting the intended recipients of a SCP. Change between baseline and follow-up among “matched” primary care physician and APP respondents is shown in Table 2. Again, statistically significant improvements were noted in all areas except that of intended recipients. One of the most significant improvements following the education program was respondent ability to identify SCP location within the EHR (9 vs 59%, p < 0.0001 for all respondents; 10 vs 67%, p = <0.0001 for 39 “matched” respondents).
Table 1.
Comparisons between baseline and follow-up for primary care physicians and APP respondents as a group*
| n/N (%), correct response to question | Baseline total = 101 | Follow-up total = 66 | p value |
|---|---|---|---|
| Selecting both patient and PCP as intended SCP recipients | 87/101 (86) | 63/66 (95) | 0.0669 |
| Selecting patient treated with curative intent as intended recipients | 26/101 (26) | 39/66 (59) | < 0.0001 |
| Selecting timing of SCP provision as end of treatment | 25/101 (25) | 44/66 (67) | < 0.0001 |
| Reporting they know where to find the SCP in EHR | 9/101 (9) | 39/66 (59) | < 0.0001 |
by Fisher’s exact tests
Table 2.
Comparisons between baseline and follow-up among “matched” primary care physicians and APP respondents*
| n/N (%) correct in response to question | Baseline total = 39 | Follow-up total = 39 | p value |
|---|---|---|---|
| Selecting both patient and primary care as intended SCP recipients | 35/39 (90) | 36/39 (92) | 0.65 |
| Selecting patients treated with curative intent as intended recipients | 14/39 (36) | 27/39 (69) | 0.0008 |
| Selecting timing of SCP provision as end of treatment | 10/39 (26) | 27/39 (69) | < 0.0001 |
| Reporting they know where to find the SCP in EHR | 4/39 (10) | 26/39 (67) | < 0.0001 |
by McNemar’s tests
Recommendations for SCP improvement were solicited as part of the follow-up survey, with 17 of 66 respondents providing a response to the free text question, “Thinking about how patients might use Survivorship Care Plans, do you have any suggestions for how we might improve them?” Suggestions focused on the timeframe of delivery, e.g., “after… chemotherapy and radiation” and length, e.g., “keep them short.” Some endorsed the need for consistent and repeated provision of SCPs, e.g., “give immediately and then send again at variable intervals – i.e. one year, 5 years and 10 years later” or the need to leverage the EHR for assistance, e.g., “incorporate it into automated reminders (like health maintenance).”
Discussion
Primary care providers may lack knowledge of the existence of SCPs or be unaware that they have received one for a survivor they are following. Without such knowledge, primary care providers cannot use SCPs to coordinate management with the oncology care team. Our study demonstrated that a brief education program designed for primary care physicians and APPs improved awareness of SCP existence and also improved fund of knowledge with regards to which patient populations would receive SCPs and the timing of SCP delivery. The main barrier identified to increased SCP use as reported by the respondents was difficulty locating SCPs within the EHR, even though the UW EHR interface and SCP location are identical within the out- and in-patient settings for all users. This also improved significantly following the education program (9 vs 59%, p < 0.0001). The only area that did not demonstrate change following the education program was primary care physician and APP knowledge of the intended recipients of a SCP (e.g., both survivor and survivor’s primary care provider). However, there may be a ceiling effect as baseline knowledge was quite high, with 86% respondents correctly selecting both the survivor and primary care provider as intended recipients.
More recent studies with primary care providers have focused on desire for SCPs, receipt of SCPs, SCP content, or comfort with providing survivorship care [3, 6–15], with limited literature assessing primary care providers use of SCPs. Our previous work [3, 4] suggests that most primary care providers preferred to receive SCPs within the EHR, as does work by Nicolajie et al. [16]. However, to be useful, primary care providers must understand and be able to access what they are receiving, in order to overcome the “information overload” phenomena endemic to EHRs. These results uniquely report the impact of an education program on primary care physician and APP knowledge regarding SCPs rather than focusing on oncology specialists [17, 18]. The Survey of Physicians’ Attitudes Regarding the Care of Cancer Survivors (SPARCCS) found that primary care physicians who reported inadequate knowledge or training to manage the problems of survivors were 43% less likely to discuss and engage in survivorship care planning [19]. Our current fragmented survivorship system poses tremendous challenges [20] given a dwindling oncology workforce [21] and growing number of survivors. It is estimated there will be 20 million survivors by 2026, with 14 million living five or more years past diagnosis, many with other chronic co-morbidities [22]. Survivors may increasingly transition from oncology-led follow-up to shared or primary care-led follow-up [23], but this risks overtasking an already strained primary care workforce [24]. With this literature in mind, assisting primary care providers in providing high-quality survivorship care becomes more important than ever. Our study demonstrated that a brief education program improved primary care physician and APP knowledge regarding SCPs, increasing the potential impact of such SCPs as a tool for improving survivorship care.
With the creation of the Collaborative, we developed an interdisciplinary team that includes the perspective of (1) primary care on integrating SCP content into the primary care medical home; (2) oncology and survivorship experts on creation and dissemination of SCPs to survivors and primary care; and (3) engineers to focus on the usefulness and effectiveness of the tools created. This Collaborative is to our knowledge the first of its kind that has fully integrated the primary care perspective into creating and implementing a primary care education program regarding SCPs. Our approach has several key strengths. We integrated the primary care viewpoint carefully, with the development of a novel education program designed by and specifically intended for primary care physicians and APPs. Our education program carefully minimized the time requirements for busy primary care physicians and APPs while reinforcing the program’s content via surveys (which called attention to the topic and repeated the program’s main points). Finally, we matched pre-and post-survey data at the individual respondent level following receipt of the education program.
Limitations of our data include the survey response rate. The listserv contained 287 primary care physician and APP emails, while the education sessions were attended by at least 191 primary care physicians and APPs. The baseline survey had a response rate of 35% (101/287) while the follow-up survey had a 23% (66/287) response rate, with only 14% (39/287) taking both surveys. Thus, it is possible that we saw improvement between the baseline and follow-up surveys by selecting out more interested and informed respondents for follow-up survey completion. The “matched” respondent results do suggest that change in knowledge occurred at an individual level. Similar to the group as a whole, the matched primary care physician and APPs demonstrated statistically significant improvements in nearly all areas. Another limitation is that this education program occurred within an academic setting and might not be generalizable to non-academic primary care providers. Additionally, we limited participants to primary care physicians and APPs with direct access to our EHR. We did not include primary care providers without access or who had access only through a health information exchange, even though such primary care providers do receive copies of SCPs (via mail or fax). Further efforts should be devoted to including diverse primary care providers in larger scale efforts to evaluate the need and effectiveness of survivorship care education. Continued adaptations to the education program could be made in order to provide online education sessions as a mechanism to improve dissemination and participation by lifting time constraints.
In conclusion, this study suggests that education of primary care physicians and APPs with regards to SCPs is warranted. Such education may serve to increase primary care awareness, which in turn could increase the potential impact of SCPs. Increasing SCP provision in the wake of the Commission on Cancer guidelines [25] may partially address this by further familiarizing primary care providers with them. However, our results suggest the need for continued work customizing the EHR to support primary care participation in managing or co-managing survivors: despite routine provision, in the initial survey only a few primary care physicians and APPs (9%) could find the SCP document, even though 50% were aware that such documents existed. Further research is warranted to identify best methods to address these barriers in communication and coordination of care between oncology and primary care, and to evaluate “real-world” SCP utilization as a tool for clinical decision-making at the point-of-care during primary care visits.
Supplementary Material
Acknowledgments
Funding This work was supported by the NCI Cancer Center Support Grant P30 CA014520 and Aging and Cancer Program P20 CA103697, a UW Division of General Internal Medicine grant and School of Medicine and Public Health Research Honors Program. AJT received support from the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grants UL1TR000427and KL2TR000428.
Footnotes
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s13187-017-1281-9) contains supplementary material, which is available to authorized users.
Compliance with Ethical Standards
Conflict of Interest
SMD: none
JEH: none
ZL: none
ERT: none
SAK: none
DAF: none
JMS: none
LGW: ElucentMedical
MES: none
AJT: Epic Systems, Corp (family member)
References
- 1.Hewitt ME, Greenfield S, Stovall E. From cancer patient to cancer survivor: lost in transition. National Academy Press; Washington, D.C: 2006. [Google Scholar]
- 2.McCabe MS, Bhatia S, Oeffinger KC, et al. American Society of Clinical Oncology statement: achieving high-quality cancer survivorship care. J Clin Oncol. 2013;31:631–640. doi: 10.1200/JCO.2012.46.6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donohue SM, Sesto ME, Hahn DL, et al. Evaluating primary care providers’ views on survivorship care plans generated by an electronic health record system. J Oncol Pract. 2015;11:e329–e335. doi: 10.1200/JOP.2014.003335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tevaarwerk AJ, Wisinski KB, Buhr KA, et al. Leveraging electronic health record systems to create and provide electronic cancer survivorship care plans: a pilot study. J Oncol Pract. 2014;10:e150–e159. doi: 10.1200/JOP.2013.001115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seaborne LA, Hueneberg K, Bohler A, et al. Developing electronic health record (EHR)-based program to deliver survivorship care plans (SCPs) and visits at the UW Breast Center. Presented at 2016 Cancer Survivorship Symposium; San Diego CA. [Google Scholar]
- 6.Watson EK, Sugden EM, Rose PW. Views of primary care physicians and oncologists on cancer follow-up initiatives in primary care: an online survey. J Cancer Surviv: Res Pract. 2010;4:159–166. doi: 10.1007/s11764-010-0117-y. [DOI] [PubMed] [Google Scholar]
- 7.Smith SL, Wai ES, Alexander C. Caring for survivors of breast cancer: perspective of the primary care physician. Curr Oncol. 2011;18:218–226. doi: 10.3747/co.v18i5.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mayer DK, Gerstel A, Leak AN, et al. Patient and provider preferences for survivorship care plans. J Oncol Pract/Am Soc Clin Oncol. 2012;8:e80–e86. doi: 10.1200/JOP.2011.000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salz T, Oeffinger KC, Lewis PR, et al. Primary care providers’ needs and preferences for information about colorectal cancer survivorship care. J Am Board Fam Med. 2012;25:635–651. doi: 10.3122/jabfm.2012.05.120083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Merport A, Lemon SC, Nyambose J, et al. The use of cancer treatment summaries and care plans among Massachusetts physicians. Support Care Cancer. 2012;20:1579–1583. doi: 10.1007/s00520-012-1458-z. [DOI] [PubMed] [Google Scholar]
- 11.Sa B, Deal AM, Mayer DK, et al. Following through: the consistency of survivorship care plan use in United States cancer programs. J Cancer Educ: Off J Am Assoc Cancer Educ. 2014;29:689–697. doi: 10.1007/s13187-014-0628-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ezendam NPM, Nicolaije KaH, Kruitwagen RFPM, et al. Survivorship care plans to inform the primary care physician: results from the ROGY care pragmatic cluster randomized controlled trial. J Cancer Surviv: Res Pract. 2014;8:595–602. doi: 10.1007/s11764-014-0368-0. [DOI] [PubMed] [Google Scholar]
- 13.Skolarus TA, Holmes-Rovner M, Northouse LL, et al. Primary care perspectives on prostate cancer survivorship: implications for improving quality of care. Urol Oncol. 2013;31:727–732. doi: 10.1016/j.urolonc.2011.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klabunde CN, Han PKJ, Earle CC, et al. Physician Roles in the Cancer-Related Follow-Up Care of Cancer Survivors. Fam Med. 2013;45(7):463–474. [PMC free article] [PubMed] [Google Scholar]
- 15.Baravelli C, Krishnasamy M, Pezaro C, et al. The views of bowel cancer survivors and health care professionals regarding survivorship care plans and post treatment follow up. J Cancer Surviv. 2009;3:99–108. doi: 10.1007/s11764-009-0086-1. [DOI] [PubMed] [Google Scholar]
- 16.Nicolaije KAH, Ezendam NPM, Vos MC, Pijnenborg JMA, Boll D, Boss EA, Hermans RHM, Engelhart KCM, Haartsen JE, Pijlman BM, et al. Impact of an Automatically Generated Cancer Survivorship Care Plan on Patient-Reported Outcomes in Routine Clinical Practice: Longitudinal Outcomes of a Pragmatic, Cluster Randomized Trial. J Clin Oncol. 2015;33(31):3550–3559. doi: 10.1200/JCO.2014.60.3399. [DOI] [PubMed] [Google Scholar]
- 17.Banerjee SC, Matasar MJ, Bylund CL, et al. Survivorship care planning after participation in communication skills training intervention for a consultation about lymphoma survivorship. Transl Behav Med. 2015;5:393–400. doi: 10.1007/s13142-015-0326-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaw T, Yates P, Moore B, et al. Development and evaluation of an online educational resource about cancer survivorship for cancer nurses: A mixed-methods sequential study. Eur J Cancer Care. 2017;26:e12576. doi: 10.1111/ecc.12576. [DOI] [PubMed] [Google Scholar]
- 19.Blanch-Hartigan D, Forsythe LP, Alfano CM, et al. Provision and discussion of survivorship care plans among cancer survivors: results of a nationally representative survey of oncologists and primary care physicians. J Clin Oncol. 2014;32:1578–1585. doi: 10.1200/JCO.2013.51.7540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rowland JH, Hewitt M, Ganz PA. Cancer survivorship: a new challenge in delivering quality cancer care. J Clin Oncol. 2006;24:5101–5104. doi: 10.1200/JCO.2006.09.2700. [DOI] [PubMed] [Google Scholar]
- 21.Yang W, Williams JH, Hogan PF, et al. Projected supply of and demand for oncologists and radiation oncologists through 2025: an aging, better-insured population will result in shortage. J Oncol Pract. 2014;10:39–45. doi: 10.1200/JOP.2013.001319. [DOI] [PubMed] [Google Scholar]
- 22.Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the “silver tsunami”: prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomark Prev. 2016;25:1029–1036. doi: 10.1158/1055-9965.EPI-16-0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Halpern MT, Viswanathan M, Evans TS, et al. Models of cancer survivorship care: overview and summary of current evidence. J Oncol Pract. 2015;11:e19–e27. doi: 10.1200/JOP.2014.001403. [DOI] [PubMed] [Google Scholar]
- 24.Colwill JM, Cultice JM, Kruse RL. Will generalist physician supply meet demands of an increasing and aging population? Health Aff (Millwood) 2008;27:w232–w241. doi: 10.1377/hlthaff.27.3.w232. [DOI] [PubMed] [Google Scholar]
- 25.American College of Surgeon’s Commission on Cancer. [Accessed May 2017];Cancer Program Standards: Ensuring Patient-Centered Care Manual, 2016 edn. https://www.facs.org/~/media/files/quality%20programs/cancer/coc/2016%20coc%20standards%20manual_interactive%20pdf.ashx.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


