Abstract
Background and Objectives
Multifocal atrial tachycardia (MAT), in general, has a favorable outcome. However, there are insufficient data regarding MAT in a pediatric population. This study sought to determine the clinical course of MAT and identify potential prognostic factors.
Methods
The medical records of MAT patients from 1997–2015 were reviewed. The arrhythmia control rate and factors for unfavorable outcomes were assessed and compared to those in the literature.
Results
Of the 33 included patients (19 boys and 14 girls), 27 were infants less than 1 year of age. The median age at diagnosis was 1.7 months (range, 0 day to 14 years). Fourteen (42%) patients had structural heart disease. Eight (24%) patients had lung disease and 6 (18%) had a syndromic diagnosis belonging to RASopathy. Two patients developed polymorphic ventricular tachycardia, in whom genetic analysis confirmed the presence of the RyR2 mutation several years later. MAT was controlled in 26 patients (84%) within 3.9 months (median; range, 16 days–18.4 years) using an average of 2.4 medications. There were 3 cases of cardiopulmonary mortality. The arrhythmia control rate was higher in the infant group (85%) than in the non-infant group (67%), although this trend was not statistically significant. There was a significantly lower rate of unfavorable outcomes in the idiopathic infant group (n=11) than in the other groups (p=0.008). Considering the findings of previous studies, the mortality rate was significantly higher in patients with structural heart disease than in patients without (21% vs. 5%, p=0.01).
Conclusions
MAT usually affects infants and has a favorable prognosis, particularly in the idiopathic infant group. However, in the presence of other comorbidities, MAT may have a variable clinical course.
Keywords: Supraventricular tachycardias, Atrial fibrillation, Atrial flutter
INTRODUCTION
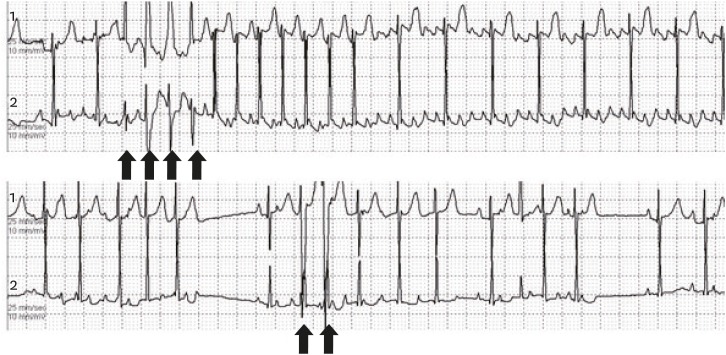
Multifocal atrial tachycardia (MAT) is defined as a tachycardia with at least 3 morphologically distinct P-waves. It is also characterized by irregular P-P, R-R, and P-R intervals, and an isoelectric baseline between the P-waves.1) MAT episodes typically last for several minutes to hours. Although the rhythm typically returns to normal between episodes, it can also coexist with atrial fibrillation (AF), atrial flutter (AFL), or both. During the tachycardia period, aberrant ventricular conductions are frequently observed, which must be differentiated from ventricular tachycardia (VT) (Figure 1).
Figure 1.
Holter monitoring of multifocal atrial tachycardia showed irregular narrow-QRS tachycardia with aberrantly conducted wide QRS complexes (arrows) and multiple morphologically distinct P-waves with variable P-R intervals.
MAT is prevalent in the elderly, particularly those with pulmonary diseases including chronic obstructive pulmonary disease. However, it is relatively rare in the pediatric population. Therefore, the clinical features of MAT in children is not well established.2),3) Several investigators have described MAT as having a mild clinical course with few sequelae and rare mortality,4),5) while others reported adverse outcomes including cardiogenic death or persistent arrhythmia.6),7) The purpose of this report was to ascertain the clinical course and prognosis of pediatric patients with MAT, and identify its potential prognostic factors.
METHODS
Thirty-three patients who were diagnosed with MAT between 1997 and 2015 were identified by searching the medical records of Seoul National University Children's Hospital. The clinical histories, vital signs, and laboratory and imaging findings, including ECG, Holter monitor, and echocardiography were reviewed.
MAT with a P-wave interval <200 milliseconds or with coexisting AF or AFL was considered to have chaotic features. We defined patients as having “incessant-type MAT” if the arrhythmia persists for >30% of the day on Holter monitoring. In contrast, it was defined as “paroxysmal-type MAT” if the arrhythmia persists briefly. Echocardiographic data, including left ventricular (LV) ejection fraction (EF), ventricular dimension, and atrioventricular valve regurgitation were also reviewed. The ECG and echocardiographic data, as well as the patients' age at onset and accompanied diseases, were investigated as potential prognostic factors. Patients were grouped into infant and non-infant groups based on the age of MAT onset. We additionally placed patients in the idiopathic infant group if the patient had no underlying disease and had onset of MAT at <1 year of age.
With regard to the treatment response, MAT was considered to be controlled if the patient became asymptomatic and had evidence of sinus rhythm either on Holter monitoring or on 2 consecutive ECGs (performed at an interval of >3 months). Cardiopulmonary mortality, or persistence of the arrhythmia for >1 year despite treatment was considered an unfavorable outcome.
Continuous variables were recorded as mean±standard deviation or as median and range. Continuous variables were compared between the groups using the Mann-Whitney U test. Fisher's exact test was used to determine statistical significance between categorical variables. Multivariate logistic regression analysis was conducted to decide the major determinant of the nominal outcome. A p value < 0.05 was considered statistically significant. Statistical analyses were conducted using SPSS 20.0 (IBM, Armonk, NY, USA). This study was approved by the Institutional Review Board at Seoul National University Hospital (No. 1701-087-824, approved, 2017).
RESULTS
Among 33 patients with identified MAT, 19 were boys and 27 (82%) were younger than 1 year old at the time of diagnosis (infant group). The median age at diagnosis of MAT was 1.7 months (range, 0 days–14.2 years). Ten patients (30%) had fetal arrhythmias/tachycardia on fetal monitoring, while nine were first detected incidentally on physical examination (27%). Otherwise, the initial manifestation of MAT included fast/irregular heart beat on monitoring (n=8, 24%), tachypnea/dyspnea/feeding difficulty (n=4, 12%), and lethargy (n=1, 3%).
Comorbidities and other arrhythmias
Table 1 summarizes the patients' profiles and clinical courses. Fourteen (42%) patients had structural heart disease (8 with atrial septal defects, 2 with ventricular septal defects, and 5 with hypertrophic cardiomyopathy [HCMP]). Eight (24%) patients had lung disease, of whom 5 patients required mechanical ventilator support. Five patients had a syndromic diagnosis, including 3 with Costello syndrome and 2 with Noonan syndrome. One patient (patient number 21) had syndromic features suggestive of RASopathy (facial dysmorphism and HCMP), although the genetic study has not yet been reported (negative for HRAS and PTPN mutations; whole exome sequencing is pending). Including this suggestive case, 6 (18%) patients had syndromes belonging to RASopathy. Among 27 patients with infant onset of MAT, 11 patients (41%) were included in the idiopathic group.
Table 1. Patient characteristics and treatment outcomes.
| Number | Diagnosis | Status at diagnosis | Treatment and follow-up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age/sex | Underlying disease | HoT | EF (%) | LVID z score | Valve regurgitation | Medications | Arrhythmia duration (days) | Treatment duration (years) | Follow-up duration (years) | Treatment result | ||
| Infantile onset | ||||||||||||
| 1 | 0 months/M | None | Normal | Normal | 2.74 | None | BB, DGX, STL | 56 | 1.8 | 5.2 | Off | |
| 2 | 0 months/F | None | Normal | Normal | 0.17 | None | BB, DGX, STL | 86 | 0.5 | 1.1 | Off | |
| 3 | 0 months/M | None | Normal | Normal | −0.20 | None | BB, DGX, STL | 70 | 1.0 | 6.5 | Off | |
| 4 | 1 month/M | None | Normal | Normal | −0.43 | Mild TR | BB, DGX, STL | 189 | 2.0 | 10.2 | Off | |
| 5 | 1 month/M | None | Normal | Normal | NA | Mild MR | DGX, STL | 74 | 0.3 | 8.8 | Off | |
| 6 | 2 months/M | None | Normal | 48 | 1.27 | Mild TR | BB, DGX, STL | 78 | 1.2 | 1.6 | Off | |
| 7 | 2 months/F | None | Yes | 40 | 0.49 | Mild MR and mild TR | AMO, DGX | 50 | 0.4 | 0.4 | Off | |
| 8 | 2 months/M | None | Yes | Normal | 0.1 | None | AMO, BB | 186 | 1.1 | 1.2 | Off | |
| 9 | 2 months/F | None | Normal | 46 | −0.52 | None | BB | 51 | 1.3 | 3.2 | Off | |
| 10 | 2 months/F | None | Normal | 46 | 1.70 | Severe MR | AMO, BB, DGX | 70 | 0.4 | 2.9 | Off | |
| 11 | 3 months/M | None | Normal | 35 | NA | Not available | BB, DGX | 38 | NA | 0.8 | NA | |
| 12 | 0 months/F | Costello syndrome, pleural effusion | Yes | Normal | −2.65 | Mild MR and mild TR | AMO, BB, DGX | 680 | 1.5 | 3.5 | Off | |
| 13 | 0 months/M | Pericardial effusion, PDA, ASD | Normal | Normal | NA | None | BB, DGX | 46 | 0.9 | 9.4 | Off | |
| 14 | 0 months/F | Noonan syndrome, HCMP, valvular PS | Yes | Normal | −0.37 | None | None | 354 | Not treated | 3.7 | Off | |
| 15 | 0 months/M | Suspicious Noonan syndrome, HCMP | Normal | Normal | −1.24 | None | None | 495 | Not treated | 1.4 | Off | |
| 16 | 0 months/M | ASD | Yes | Normal | −0.91 | None | AMO, BB, DGX | 82 | 0.3 | 0.2 | Off | |
| 17 | 0 months/M | Costello syndrome with HCMP, HPS | Yes | Normal | −3 | None | AMO, BB, DGX | NN | 0.6 | 0.2 | Death | |
| 18 | 1 month/M | Tracheo-esophageal fistula | Normal | Normal | 0.8 | None | BB | 60 | 0.6 | 12.2 | Off | |
| 19 | 1 month/M | Cryptorchidism | Normal | Normal | 2.14 | None | BB | 95 | 0.6 | 2.2 | Off | |
| 20 | 1 month/M | DMD, chylothorax, ASD and PS, syndactyly | Normal | Normal | −0.74 | None | AMO, BB, DGX, STL | NN | 0.3 | 0.3 | Death | |
| 21 | 1 month/F | HCMP, chylothorax, laryngomalacia, suspicious RASopathy | Normal | Normal | −3.42 | None | AMO, DGX, BB | 209 | 1.4 | 0.6 | On | |
| 22 | 1 month/F | Suspicious Costello syndrome, HCMP, ASD, BPD, preterm, pneumothorax, dysmorphic face | Yes | Normal | NA | Severe MR and moderate TR | AMO, BB, DGX, FLC | NN | 0.2 | 0.2 | Death | |
| 23 | 2 months/M | VSD | NA | Normal | 3.04 | Mild MR | AMO, BB | 112 | 0.8 | 4.3 | Off | |
| 24 | 2 months/F | CoA, VSD, ASD, Hypothyroidism | Normal | Normal | 1.42 | None | AMO, BB, DGX | 438 | 1.6 | 2.3 | Off | |
| 25 | 3 months/M | ASD, preterm, PVL, RDS | Normal | Normal | −3.9 | None | BB, DGX | NN | NA | 1.9 | NA | |
| 26 | 4 months/F | ASD | Normal | 30 | 1.69 | Mild MR and mild TR | AMO, DGX | 123 | 1.2 | 2.1 | Off | |
| 27 | 6 months/M | Congenital MR | Yes | 44 | 3.37 | Severe MR and mild TR | AMO, DGX | 501 | 2.0 | 2.0 | Off | |
| Non-infantile onset | ||||||||||||
| 28 | 17 months/F | ASD, AVRT | Normal | Normal | −2.52 | Mild MR and moderate TR | BB, DGX | 335 | 0.8 | 8.3 | Off | |
| 29 | 2 years/M | Catecholaminergic polymorphic VT | Normal | Normal | −0.23 | None | AMO, BB, CCB, DGX, STL, FLC | 6,625 | 20.3 | 19.3 | On | |
| 30 | 6 years/M | Catecholaminergic polymorphic VT | Normal | Normal | 0.60 | None | BB, CCB, FLC | NN | 6.7 | 5.7 | On | |
| 31 | 7 years/F | Rhabdomyosarcoma, tumor lysis syndrome | Normal | 41 | −3.67 | None | BB, DGX | 16 | 0.2 | 1.2 | Death | |
| 32 | 12 years/F | AVRT | Normal | Normal | 0.05 | None | AMO, BB, CCB | 71 | 0.6 | 3.1 | Off | |
| 33 | 14 years/F | None | Normal | Normal | −0.3 | None | BB, FLC | NN | 4.4 | 3.7 | On | |
AMO = amiodarone; ASD = atrial septal defect; AVRT = atrioventricular reentrant tachycardia; BB = β-blockers; BPD = bronchopulmonary dysplasia; CCB = calcium channel blockers; CoA = coarctation of the aorta; DGX = digoxin; DMD = Duchenne muscular dystrophy; EF = ejection fraction; F = female; FLC = flecainide; HCMP = hypertrophic cardiomyopathy; HPS = hypertrophic pyloric stenosis; HoT = hypotension; LVID = left ventricular internal diameter; M = male; MR = mitral regurgitation; NA = not accessible; NN = not normalized; Off = off therapy; On = on medication; PDA = patent ductus arteriosus; PS = pulmonary stenosis; PVL = periventricular leukomalacia; RDS = respiratory distress syndrome; STL = sotalol; TR = tricuspid regurgitation; VSD = ventricular septal defect.
Four patients had the other, following arrhythmias: patient 28 and patient 32 had been managed with atrioventricular reentrant tachycardia (AVRT) prior to MAT diagnosis; patient 30 and patient 29 developed catecholaminergic polymorphic ventricular tachycardia (CPVT) after MAT diagnosis. Patient 30 was transferred to our hospital when he was 6 years old after being treated for recurrent verapamil-sensitive supraventricular tachycardia in another hospital for 10 months. The initial Holter monitoring done at our hospital showed MAT, and treadmill test revealed nonsustained polymorphic VT. He had syncope 5 years after his initial presentation, and the RyR2 mutation was confirmed on genetic analysis. Patient 29 showed paroxysmal atrial tachycardia initially at 2 years of age and was diagnosed as having a MAT on an electrophysiologic study at 9 years of age. This arrhythmia was refractory to combinations of multiple antiarrhythmic drugs, and a radiofrequency catheter ablation for multiple atrial foci was done at 14 years of age in another hospital, after which β-blocker was discontinued. However, the patient had a rescued cardiac arrest with polymorphic VT 1 year later, and genetic analysis confirmed the RyR2 mutation. This patient subsequently underwent an operative sympathetic denervation, after which the recurrent MAT and CPVT was controlled with the addition of flecainide.
Table 2 shows the different distributions of the major underlying diseases or other arrhythmias between the infant and non-infant groups. The coexistence or development of other arrhythmias (beside MAT) was significantly higher in the non-infant group (4/6 vs. 0/27, p<0.01). In contrast, the other major comorbidities, including structural heart disease (including HCMP), pulmonary disease, and RASopathy syndrome were more commonly identified in infants with MAT, although the difference was not significant (16/27 vs. 2/6, p=0.38).
Table 2. Underlying disease comparison by age group.
| Infant group (n=27) | Non-infant group (n=6) | p value* | |
|---|---|---|---|
| Sex (M:F) | 17:10 | 2:4 | 0.363 |
| HCMP | 5 | 0 | 0.556 |
| Structural heart disease | 13 | 1 | 0.209 |
| Pulmonary disease | 8 | 0 | 0.396 |
| Syndrome | 6 | 0 | 0.563 |
| Further arrhythmia | 0 | 4 | <0.001 |
HCMP = hypertrophic cardiomyopathy.
*Fisher's exact test.
Arrhythmia characteristics
The medians of the narrowest P-P and R-R intervals were 160 and 240 milliseconds, respectively. Sixteen (49%) patients had coexisting AFL or AF (AFL, 6; AF, 3; both, 7). Among 31 patients with adequate recordings, 24 (77%) patients had incessant-type and 7 (23%) had paroxysmal-type MAT.
Heart failure parameters
Among the 32 patients whose blood pressure measurements were available, 8 (25%) patients were hypotensive on the day of diagnosis and 3 had received intravenous inotropics. In addition, 8 (24%) patients had LV dysfunction and 4 patients showed LV dilatation. Ten (30%) patients had atrioventricular valve regurgitations of more than grade I, and 4 of them had moderate to severe regurgitation. Among those who underwent follow-up echocardiography, all patients except patient 22, had normalized ventricular function (median normalization time, 41 days; range, 3 days–10.24 years), ventricular dilatation (median normalization time, 6 months; range, 24 days–11.8 months), and valve function (median normalization time, 68 days; range, 8 days–10.9 months). None of the patients had significant cardiac enzyme elevation at the time of initial diagnosis.
Treatments and outcomes
Two neonates (patients 14 and 15) had spontaneous resolution of MAT without any medication. Other patients, in contrast, received up to 6 types of medications. The most commonly administered drug was β-blockers, followed by digoxin and amiodarone. Direct current cardioversion and adenosine infusion were attempted in 8 patients, without effect. During the median follow-up period of 27.9 months (range, 2.3 months–19.3 years), 2 patients were lost to follow-up. Among the remaining 31 patients, 26 (84%) patients had therapeutic control of MAT at a median 3.5 months (range, 16 days–18.4 years) after diagnosis. Among 27 patients followed at the time of review, 23 patients were off therapy and 4 were on medications, including 2 with uncontrolled arrhythmias.
There were 4 fatal cases during the follow-up period. Patient 22 was the only patient with definitive cardiac mortality; this patient was clinically suspected to have Costello syndrome given concurrent HCMP and typical facial dysmorphism. However, there were no confirmative tests at the time (2004). The patient died of progressive heart failure, persistent MAT, and respiratory failure.
Patient 20 died of respiratory failure due to refractory chylothorax and poorly controlled MAT. Patient 17 died of aspiration pneumonia despite controlled MAT. In patient 31, the MAT was thought to be caused by tumor lysis syndrome, which occurred after the patient's first cycle of chemotherapy. Her MAT improved briefly, lasting for 16 days, but she ultimately died of respiratory arrest due to leptomeningeal seeding.
Risk analysis for adverse outcomes
The infant group had a higher control rate (88%) than did the non-infant group (67%), although the difference was not statistically significant (p=0.24). Likewise, patients with HCMP, pulmonary disease, or major comorbidities had a lower control rate, also without statistical significance. The idiopathic infant group (n=10) had 100% control rate, but the difference was not significant (p=0.15).
Excluding fatal cases and those lost to follow-up, we compared the arrhythmia duration between the remaining 27 patients. The median duration of MAT was 3.9 months (range, 16 days–18.4 years). The infant group had a shorter duration of arrhythmia than did the non-infant group, (3.5 months, range 50 days–1.9 years vs. 2.3 years, range 16 days–18.4 years, respectively), although the difference was not statistically significant. The idiopathic infant group had a significantly shorter duration of arrhythmia (2.4 months, 50 days–6.3 months), than did the other groups (11.0 months, 16 days–18.4 years) (p=0.001).
We compared the unfavorable outcomes between the age groups and comorbidity groups (Table 3). The idiopathic infant group had a significantly lower rate of unfavorable outcomes than did the others (0% vs. 47%, p=0.008). On multivariate analysis, there was no significantly associated risk factor for unfavorable outcome of MAT.
Table 3. Unfavorable outcome comparison between age and comorbidity groups.
| Group | Unfavorable outcome | p value* |
|---|---|---|
| Infants vs. others | 7/25 vs. 3/6 | 0.358 |
| HCMP vs. others | 3/5 vs. 7/26 | 0.296 |
| Structural heart disease vs. others | 6/13 vs. 4/18 | 0.247 |
| Pulmonary disease vs. others | 4/7 vs. 6/24 | 0.172 |
| Syndrome vs. others | 4/6 vs. 6/25 | 0.067 |
| Further arrhythmia vs. others | 2/4 vs. 8/27 | 0.577 |
| Major comorbidity vs. idiopathic | 9/20 vs. 1/11 | 0.055 |
| Idiopathic infants vs. others | 0/10 vs. 10/21 | 0.008 |
HCMP = hypertrophic cardiomyopathy.
*Fisher's exact test.
In subgroup analysis of 25 infants with available follow-up data, RASopathy syndrome was significantly associated with unfavorable outcomes (p=0.032). In contrast, infants in the idiopathic infant group had a significantly lower rate of unfavorable outcomes (p=0.020) than did those in other groups.
Other potential risk factors for MAT, including fetal presentation, arrhythmia characteristics and heart failure parameters did not have significant differences in control rate, arrhythmia duration or unfavorable outcomes.
DISCUSSION
Most literature regarding pediatric MAT shows a predominance in infants.1),4),5),7),8) Children older than 1 year rarely have documented MAT.9),10),11) Although the patients in this study were mostly infants, the number of non-infant patients was also relatively large. Prior studies have found that MAT is can coexist with structural heart diseases, respiratory diseases, and RASopathy syndromes. Our study confirms these associations. A variety of specific diagnoses in each category was similar to those of previous studies. Consistent with previous studies, the majority of our patients had no definite presenting symptom. Instead, most arrhythmias were detected during routine physical examinations or during other monitoring. However, if tachycardia persists for several days without management, patients can present with heart failure symptoms such as poor feeding, irritability, vomiting, respiratory distress and lethargy due to tachycardia-induced cardiomyopathy. Therefore, if an infant or young child with tachycardia develops poor feeding, irritability, respiratory distress and lethargy, clinicians must consider the possibility of a long-standing tachyarrhythmia. In such cases, immediate management for tachyarrhythmias is necessary.
Atrial premature beats, AF, or AFL are known to accompany MAT in both adults and pediatric patients.1),4),12) The rate of accompanied AFL or AF in our study (49%) was also similar to that of adult reports (55%).13) However, the clinical association between MAT and AVRT was a unique finding in our study. There are 2 reported cases of MAT with Wolff-Parkinson-White syndrome.4),11) Moreover, we also described a phenotypical progression of MAT into CPVT (patients 29 and 30). Although MAT or AF may be found concomitantly with polymorphic VT in CPVT patients, our data emphasize that MAT in young children may be the initial manifestation of a potentially life-threatening arrhythmia of CPVT.
Based on prior studies, the prognosis of MAT varies widely from being clinically benign to refractory. However, the epidemiologic characteristics of MAT had not previously been well defined. Among 29 case reports and/or series identified using ‘MAT in pediatric patients’ as a search term, only 15 studies were available in full text and contained individualized information. These studies are summarized in Table 4. Bisset et al.12) reported 5 patients older than 1 year, 3 of whom were diagnosed with structural heart disease and one with cerebral gigantism. Bradley et al.1) and Dodo et al.7) reported 1 and 2 non-infant patients, respectively, with MAT and structural heart disease. In contrast to previous studies, non-infant patients in our study tended to have other arrhythmias (2 with AVRT and 2 with RyR2 (+) CPVT) with structurally normal hearts (except for a secundum atrial septal defect in patient 28). There are only 17 non-infant patients with MAT described in the prior literature and in our study; regardless, most on these patients (n=15) had MAT with other comorbidities, rather than MAT alone.1),12),14),15) Infant patients, in contrast, had a significantly lower rate of other comorbidities (52% of infant patients had underlying comorbidities, p<0.01). MAT in infant and non-infant patients may have distinct pathophysiologies, and therefore different clinical courses and prognoses. Furthermore, there are varying prognoses between studies, which might have been influenced by age differences and underlying comorbidities.
Table 4. Literature review of MAT in children (15 studies, available in full text).
| Authors | Year | Number | Sex (M:F) | Age | Comorbidity | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median age | Infant | Structural heart disease | Pulmonary disease | RASopathy syndrome | Control rate (%) | Mortality | ||||
| Farooki and Green9) | 1977 | 2 | 2:0 | 0.1 months | 2/2 | 0/2 | 0/2 | 0/2 | 100 | 0/2 |
| Bisset et al.12) | 1981 | 10 | 8:2 | 1 months (1 day–18 years) | 5/10 | 5/10 | 1/10 | 1/10 | 90 | 1/10 |
| Liberthson and Colan5) | 1982 | 9 | 4:5 | 0.4 months (1 day–5 months) | 9/9 | 0/9 | 2/9 | 1/9 | 89 | 0/9 |
| Yeager et al.6) | 1984 | 4 | 3:1 | 1.1 months (1 day–10 months) | 4/4 | 2/4 | 0/4 | 1/4 | 50 | 3/4 |
| Zeevi et al.22) | 1986 | 1 | 1:0 | 3 years | 0/1 | 1/1 | 0/1 | 0/1 | 100 | 0/1 |
| Houyel et al.23) | 1990 | 2 | 1:1 | 1.3 months | 2/2 | 0/2 | 0/2 | 0/2 | 100 | 0/2 |
| Dodo et al.7) | 1995 | 9 | 5:4 | 0.5 months (1 day–30 months) | 7/9 | 7/9 | 2/9 | 3/9 | 44 | 2/9 |
| Salim et al.8) | 1995 | 5 | 3:2 | 1.3 months (1 day–8 months) | 5/5 | 3/5 | 2/5 | n/a | 80 | 1/5 |
| Fish et al.4) | 1996 | 7 | 5:2 | 2 months (1 day–11 months) | 7/7 | 1/7 | 3/7 | 0/7 | 100 | 0/7 |
| Cetta et al.24) | 1997 | 1 | 1:0 | 9 months | 1/1 | 0/1 | 0/1 | 0/1 | 100 | 0/1 |
| Bradley et al.1) | 2001 | 21 | 14:7 | 1.8 months (1 day–7.3 years) | 20/21 | 7/21 | 6/21 | 2/21 | 94 | 1/17 |
| Hsieh et al.15) | 2006 | 2 | 1:1 | 1 day, 5 years | 1/2 | 1/2 | 2/2 | 0/2 | 100 | 0/2 |
| Bouziri et al.25) | 2011 | 1 | 1:0 | 12 days | 1/1 | 1/1 | 0/1 | 0/1 | 100 | 0/1 |
| Pregowska et al.26) | 2014 | 1 | 1:0 | 2 months | 1/1 | 1/1 | 0/1 | 1/1 | 100 | 0/1 |
| Tutar et al.14) | 2016 | 1 | 0:1 | 13 years | 0/1 | 1/1 | 0/1 | 0/1 | 100 | 0/1 |
| This report | 2017 | 33 | 19:14 | 1.7 months (1 day–14.2 years) | 27/33 | 14/33 | 8/33 | 6/33 | 84 | 4/31 |
Considering these findings, we compared the clinical outcome of MAT between patient groups according to their age and presence of major comorbidities. The overall mortality (12%) in our study is similar to that of other studies (0%–22%).1),4),5),7),8),12) All 3 cases of cardiopulmonary mortality were associated with structural heart disease (with or without pulmonary disease). This finding corresponds to those of previous studies; 9 of 12 mortality cases from previous studies also had associated structural heart disease. When considering the prior findings with our results, the mortality rate was significantly higher in patients with structural heart disease than it was in patients without structural heart disease (21% vs. 5%, p=0.01).
Our patients demonstrated a control rate (87%) that is similar to that of patients from previous studies (85%). Individual disease categories failed to show statistically significant differences in the control rate. However, the idiopathic infants had a 100% control rate. When the previous studies were counted together, the idiopathic infants had a significantly higher control rate than did the remaining patients (95% vs. 77%, p=0.01).
Several previous studies have reported an association between the RyR2 mutation and AF and ectopic atrial tachycardia. Di Pino et al.16) reported the case of a novel RyR2 mutation in a 2-year-old patient with AF, AFL, and ectopic atrial tachycardia. Furthermore, Broendberg et al.17) reported 5 cases of MAT in 51 patients with known RyR2 mutations; the group suggested that the young patients with severe MAT may be RYR2 mutation carriers. However, to the best of our knowledge, we have reported the first 2 cases of known MAT confirmed to have RyR2 mutations with life-threatening events. In both patients, the first manifestation of this mutation was with MAT, rather than VT. Therefore, non-infant MAT patients with structurally normal hearts might need thorough evaluations (including exercise testing and genetic evaluation of arrhythmogenesis), and long follow-up.
Lin et al.18) analyzed the cardiovascular abnormalities of RASopathy in their 61 patients with Costello syndrome. In their study population, 15 (25%) of 61 patients with Costello syndrome had MAT or ectopic atrial tachycardia. In addition, 13 (87%) patients had a HRAS mutation in p.Gly12Ser, which was also the most frequent mutation in the entire study population.18) Although less frequent, the mutation foci in our 2 patients with gene-confirmed Costello syndrome (p.Gly12Ala in patient 12 and p.Gly12Cys in patient 17) were also reported to be associated with atrial tachycardia.
According to the review by Lin et al.,18) RASopathies other than Costello syndrome, such as cardiofaciocutaneous syndrome, Noonan syndrome, and neurofibromatosis, were infrequently associated with supraventricular tachycardia. In contrast, Noonan syndrome with the RAF1 mutation is associated with supraventricular tachycardia. There had been 4 cases of Noonan syndrome in the MAT reports—2 from our study and 2 from the reports of Bradley et al.1) and Dodo et al.7) The specific type of gene mutation was only assessed in one patient (patient14), who also had the RAF1 gene mutation. Therefore, the specific type of gene mutation in RASopathy with MAT in our study corresponds well to the report of Lin et al.18) However, since MAT and/or atrial tachycardia have recently been reported in neurofibromatosis or Noonan syndrome with mutations other than RAF1, MAT may not be a differential feature distinguishing Costello syndrome from other RASopathies.19),20)
Two seemingly sporadic cases of rhabdomyosarcoma—patient 31 and a patient from the report of Liberthson and Colan5)—further suggests an association between the RAS gene and MAT.
The prevalence of pulmonary disease in MAT has been well established in adult MAT patients. Right atrial enlargement, hypercapnia, hypoxia, or adrenergic stimulation have been suggested as possible mechanisms by which pulmonary disease causes MAT.3) The majority of MAT reports in pediatric patients have also reported >20% of coexisting pulmonary disease, even though the rate is much higher in adults (up to 60%). However, alveolar growth and decline in pulmonary vascular resistance continues for at least 2 years; therefore, infant patients might be susceptible to MAT even in the absence of overt pulmonary disease. Furthermore, the immaturity of the atrium may also contribute to the infant-predominant age distribution of MAT. Pickoff et al.21) have reported that there is atrial vulnerability in neonatal puppies, showing an atrial refractory period that increases as the dog ages. Therefore, immaturity of both the lungs and the heart might explain the infant-predominant age distribution of MAT and its prevalence in idiopathic infant cases. The benign clinical course in the idiopathic infant group might also be explained by improvement of the immaturity of the lungs and heart as patients’ age.
Despite its valuable findings, this study has several limitations. Since this was an observational study, it has an intrinsic vulnerability to confounding. For example, the treatment strategy changed over different periods: β-blockers and digoxin were the 2 mainstay antiarrhythmic drugs in the 1990s and 2000s, while amiodarone was frequently combined with others in the 2010s. The follow-up interval also varied between patients, which could have influenced the duration of the arrhythmia and/or treatment. The statistical analyses were also limited given the study's small sample size. Given this small sample size, we were unable to identify a significant risk factor for unfavorable outcomes on the multivariate analysis.
Pediatric MAT mostly affects infants, who tend to have a favorable prognosis, especially in the absence of other comorbidities. However, MAT in patients with other underlying comorbidities may have a varying clinical course, ranging from mild and self-limiting to fatal. The prognosis of MAT in these patients may follow the prognosis of their underlying comorbidities. Therefore, it is worthwhile to evaluate for potential underlying causes in order to predict the prognosis of MAT, and potentially correct some of its reversible factors. Non-infant patients with MAT should undergo a thorough survey of underlying conditions, and prolonged follow-up to monitor for the development of other arrhythmias (such as CPVT).
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Song MK, Bae EJ.
- Data curation: Baek SM, Chung H, Song MK, Bae EJ.
- Formal analysis: Song MK, Bae EJ.
- Writing - original draft: Baek SM, Chung H, Kim GB, Noh CI.
- Writing - review & editing: Song MK, Bae EJ, Kim GB, Noh CI.
References
- 1.Bradley DJ, Fischbach PS, Law IH, Serwer GA, Dick M., 2nd The clinical course of multifocal atrial tachycardia in infants and children. J Am Coll Cardiol. 2001;38:401–408. doi: 10.1016/s0735-1097(01)01390-0. [DOI] [PubMed] [Google Scholar]
- 2.Lazaros G, Chrysohoou C, Oikonomou E, et al. The natural history of multifocal atrial rhythms in elderly outpatients: insights from the “Ikaria study”. Ann Noninvasive Electrocardiol. 2014;19:483–489. doi: 10.1111/anec.12165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kastor JA. Multifocal atrial tachycardia. N Engl J Med. 1990;322:1713–1717. doi: 10.1056/NEJM199006143222405. [DOI] [PubMed] [Google Scholar]
- 4.Fish FA, Mehta AV, Johns JA. Characteristics and management of chaotic atrial tachycardia of infancy. Am J Cardiol. 1996;78:1052–1055. doi: 10.1016/s0002-9149(96)00536-x. [DOI] [PubMed] [Google Scholar]
- 5.Liberthson RR, Colan SD. Multifocal or chaotic atrial rhythm: report of nine infants, delineation of clinical course and management, and review of the literature. Pediatr Cardiol. 1982;2:179–184. doi: 10.1007/BF02332108. [DOI] [PubMed] [Google Scholar]
- 6.Yeager SB, Hougen TJ, Levy AM. Sudden death in infants with chaotic atrial rhythm. Am J Dis Child. 1984;138:689–692. doi: 10.1001/archpedi.1984.02140450071022. [DOI] [PubMed] [Google Scholar]
- 7.Dodo H, Gow RM, Hamilton RM, Freedom RM. Chaotic atrial rhythm in children. Am Heart J. 1995;129:990–995. doi: 10.1016/0002-8703(95)90121-3. [DOI] [PubMed] [Google Scholar]
- 8.Salim MA, Case CL, Gillette PC. Chaotic atrial tachycardia in children. Am Heart J. 1995;129:831–833. doi: 10.1016/0002-8703(95)90339-9. [DOI] [PubMed] [Google Scholar]
- 9.Farooki ZQ, Green EW. Multifocal atrial tachycardia in two neonates. Br Heart J. 1977;39:872–874. doi: 10.1136/hrt.39.8.872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beitzke A. Multifocal (chaotic) atrial tachycardia in infancy. Helv Paediatr Acta. 1979;34:319–327. [PubMed] [Google Scholar]
- 11.Chantepie A, Ramponi N, Vaillant MC, Laugier J, Raynaud P, Fauchier JP. Polymorphic atrial tachycardia and Wolff-Parkinson-White syndrome in a newborn infant. Arch Mal Coeur Vaiss. 1986;79:1371–1375. [PubMed] [Google Scholar]
- 12.Bisset GS, 3rd, Seigel SF, Gaum WE, Kaplan S. Chaotic atrial tachycardia in childhood. Am Heart J. 1981;101:268–272. doi: 10.1016/0002-8703(81)90189-7. [DOI] [PubMed] [Google Scholar]
- 13.Lipson MJ, Naimi S. Multifocal atrial tachycardia (chaotic atrial tachycardia). Clinical associations and significance. Circulation. 1970;42:397–407. doi: 10.1161/01.cir.42.3.397. [DOI] [PubMed] [Google Scholar]
- 14.Tutar E, Çiftçi Ö, Fitoz S, et al. Lipomatous hypertrophy of the interatrial septum in a child with atrial tachycardia. Pediatr Int. 2016;58:523–525. doi: 10.1111/ped.12917. [DOI] [PubMed] [Google Scholar]
- 15.Hsieh MY, Lee PC, Hwang B, Meng CC. Multifocal atrial tachycardia in 2 children. J Chin Med Assoc. 2006;69:439–443. doi: 10.1016/S1726-4901(09)70288-6. [DOI] [PubMed] [Google Scholar]
- 16.Di Pino A, Caruso E, Costanzo L, Guccione P. A novel RyR2 mutation in a 2-year-old baby presenting with atrial fibrillation, atrial flutter, and atrial ectopic tachycardia. Heart Rhythm. 2014;11:1480–1483. doi: 10.1016/j.hrthm.2014.04.037. [DOI] [PubMed] [Google Scholar]
- 17.Broendberg AK, Nielsen JC, Bjerre J, et al. Nationwide experience of catecholaminergic polymorphic ventricular tachycardia caused by RyR2 mutations. Heart. 2017;103:901–909. doi: 10.1136/heartjnl-2016-310509. [DOI] [PubMed] [Google Scholar]
- 18.Lin AE, Alexander ME, Colan SD, et al. Clinical, pathological, and molecular analyses of cardiovascular abnormalities in Costello syndrome: a Ras/MAPK pathway syndrome. Am J Med Genet A. 2011;155A:486–507. doi: 10.1002/ajmg.a.33857. [DOI] [PubMed] [Google Scholar]
- 19.Prada CE, Zarate YA, Hagenbuch S, Lovell A, Schorry EK, Hopkin RJ. Lethal presentation of neurofibromatosis and Noonan syndrome. Am J Med Genet A. 2011;155A:1360–1366. doi: 10.1002/ajmg.a.33996. [DOI] [PubMed] [Google Scholar]
- 20.Finsterer J, Stollberger C, Stubenberger E, Tschakoschian S. Lymphangiopathy in neurofibromatosis 1 manifesting with chylothorax, pericardial effusion, and leg edema. Int J Gen Med. 2013;6:743–746. doi: 10.2147/IJGM.S45825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pickoff AS, Singh S, Flinn CJ, McCormack J, Stolfi A, Gelband H. Atrial vulnerability in the immature canine heart. Am J Cardiol. 1985;55:1402–1406. doi: 10.1016/0002-9149(85)90513-2. [DOI] [PubMed] [Google Scholar]
- 22.Zeevi B, Berant M, Sclarovsky S, Blieden LC. Treatment of multifocal atrial tachycardia with amiodarone in a child with congenital heart disease. Am J Cardiol. 1986;57:344–345. doi: 10.1016/0002-9149(86)90920-3. [DOI] [PubMed] [Google Scholar]
- 23.Houyel L, Fournier A, Davignon A. Successful treatment of chaotic atrial tachycardia with oral flecainide. Int J Cardiol. 1990;27:27–29. doi: 10.1016/0167-5273(90)90187-a. [DOI] [PubMed] [Google Scholar]
- 24.Cetta F, Bell TJ, Ros SP. Emergency department evaluation of an infant with chaotic atrial tachycardia. Pediatr Emerg Care. 1997;13:120–122. doi: 10.1097/00006565-199704000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Bouziri A, Khaldi A, Hamdi A, et al. Multifocal atrial tachycardia: an unusual cause of cardiogenic shock in a newborn. Tunis Med. 2011;89:59–61. [PubMed] [Google Scholar]
- 26.Pregowska K, Jurkiewicz E, Miszczak-Knecht M, Turska-Kmiec A, Bieganowska K. Persistent multifocal atrial tachycardia in infant with encephalocraniocutaneous lipomatosis: a case report. Eur J Pediatr. 2014;173:1577–1580. doi: 10.1007/s00431-013-2103-7. [DOI] [PubMed] [Google Scholar]