Abstract
AIM
To investigate the effects of different concentrations of artificial tears on lipid layer thickness (LLT) and blink rate (BR) in dry eye patients.
METHODS
This study included 106 eyes of 58 patients with dry eye. The lipid deficiency type was defined as the LLT baseline <75 nm. The LLT and BR were measured at baseline and 1, 5 and 15min after the instillation of 0.1% or 0.3% sodium hyaluronate (SH) eye drops by using the LipiView ocular surface interferometer.
RESULTS
In the lipid deficiency group, the LLT increased from baseline at 1min post instillation. The LLT after the instillation of 0.1% SH was significantly higher than that after the instillation of 0.3% SH (P<0.001). The LLT returned to baseline at 15min post instillation of 0.1% SH and at 5min post instillation of 0.3% SH. In the non-lipid deficiency group, the LLT decreased from baseline at 1min and returned to baseline at 5min for both treatments. The BRs were not significantly different at different time points for both treatments.
CONCLUSION
SH eye drops induce a short-term increase in LLT of patients with lipid deficiency. A low concentration of artificial tears have a stronger effect than a high concentration of artificial tears on the increase in LLT. In comparison, SH eye drops induce a transient and slight decrease in LLT of patients without lipid deficiency. A low concentration of artificial tears might be better for patients with lipid deficiency.
Keywords: tear film lipid layer thickness, dry eye, artificial tears, ocular surface interferometer, sodium hyaluronate
INTRODUCTION
Increased tear evaporation is an important etiological cause of dry eye. More than 80% of patients with dry eye have signs of meibomian gland dysfunction, which is the most common cause of evaporative dry eye[1]. The tear film lipid layer is the important barrier for preventing tear evaporation and maintaining tear film stability[2]. A four-fold increase in tear evaporation can be observed when the lipid layer is absent or is not confluent[3]. Thinning of the lipid layer can lead to an increased evaporation rate of the underlying aqueous layer and shorter tear break-up time (TBUT). Blackie et al[4] found that for the patients with severe dry eye symptoms, 74% had a lipid layer thickness (LLT) ≤60 nm, while 72% of patients without dry eye symptoms had an LLT≥75 nm. Therefore, in clinical practice, maintaining the stability of the tear film lipid layer is important for preventing evaporation and improving the patients' symptom and ocular comfort.
Artificial tears usually are the first-line treatment for dry eye, which can replenish tears and improve dry eye symptoms. The instillation of artificial tears transitorily interferes with the normal structure of tear film[5]–[6] and induces changes of the tear dynamics. Trees and Tomlinson[7] found that the tear evaporation rates increased after the instillation of artificial tears and saline in normal subjects. They suggested that the tear film instability produced by the instillation of artificial tears might result from the increased fluid volume within the eye, which affected or even disrupted the tear film lipid layer. A study by Tsubota and Yamada[8] also showed that the tear evaporation rate significantly increased after the instillation of artificial tears. The duration of this disturbance and the reforming speed of the tear film lipid layer may affect the tear evaporation and the feelings of patients after the application of artificial tears. The ocular surface tear volume significantly increases after the instillation of artificial tears. A dynamic balance of ocular surface tear volume can be maintained through blinking, which is important for the distribution and removal of instilled tears[9]. Blinking is also important for the formation and distribution of the lipid layer[10]–[11].
Sodium hyaluronate (SH) is a widely used water solution artificial tears because of its good biocompatibility, viscoelastic properties, and strong water retention, which can increase the tear film thickness, stabilize the tear film, and improve symptoms[12]–[14]. SH can also promote corneal epithelial wound healing[15]. We used SH eye drops to investigate the effects of different concentrations of SH eye drops on the lipid layer and blinks by measurements of LLT and blink rate (BR) in dry eye patients with different degrees of lipid deficiency.
SUBJECTS AND METHODS
Subjects
Subjects were recruited from Zhongshan Ophthalmic Center, Sun Yat-sen University from May 2016 to November 2016. A total of 58 dry eye patients (106 eyes) were included in this study (18 men and 40 women). The mean age was 46.50±15.57y (ranged from 18-83y). All subjects were informed of the purpose and procedure of the study. We conducted this study in accordance with the Declaration of Helsinki and received approval from the Medical Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University. Clinical trial registration number: ChiCTR-IOR-17010483 (http://www.chictr.org.cn).
For confirmed diagnosis of dry eye, subjects should have one of the dry eye symptoms such as dryness, foreign body sensation, burning, eye fatigue and vision fluctuation. At least one eye of the subjects had positive signs that were qualitative (TBUT≤5s) or quantitative (Schirmer I test without anethesia ≤5 mm/5min) disturbances of the tear film, and/or fluorescein staining ≥3 points (excluding other etiologies)[16]. Referring to studies by Scaffidi and Korb[17] and Fogt et al[18], different degrees of lipid deficiency of subjects were defined as follows: lipid deficiency type (LLT baseline <75 nm) and non-lipid deficiency type (LLT baseline ≥75 nm).
If the subject had any of the following conditions, the subject was excluded from the study: age below 18 years old; use of any eye drops and ointments 3h before the study; squeezing eyes or rubbing eyelids 1h before and during the study; wearing contact lenses on the day of the study; abnormality of the cornea, conjunctiva, or eyelid; ocular acute inflammation, including allergic conjunctivitis, and use of topical or systemic drugs for treatment; eye surgery within the past 6mo; autoimmune disease; and allergy to SH formulations.
Both eyes were the experimental eyes. If only one eye met the diagnostic criteria of dry eye, this eye was selected as the experimental eye.
Demographic information and medical history were also taken from the subjects. Before the examinations, slit lamp examination of the anterior segment was performed on both eyes.
Tear Break-up Time and Schirmer I Test
Five microliters of 1% sodium fluorescein solution was instilled into the subject's conjunctiva sac. After blinking 3 to 4 times, the subject was asked to look straight forward without blinking. The time taken for the first dry spot to form since the last blink was recorded and repeated 3 times. The average of the measurements was recorded as TBUT.
The Schirmer test strip (Tianjin Jingming New Technological Development Co., Ltd, Tianjin, China) was placed gently at the junction between the middle and outer third of the lower eyelid without anesthesia. The subject was instructed to close the eyelids gently for 5min. The strip was then removed and the length of the moist portion in millimeters was recorded.
Measurements of Lipid Layer Thickness and Blink Rate
The tear film LLT measurement was performed 1h after the TBUT and Schirmer I test. The tear film LLT was measured using the LipiView ocular surface interferometer (TearScience Inc, Morrisville, NC, USA). The subject was seated in front of the interferometer. The examiner adjusted the height of the interferometer and the chin rest so that the subject's chin and forehead could be positioned properly. The subject was instructed to look forward and blink naturally. The pupil had to be in the center of the screen by adjusting the position of camera. The camera focused on a clear tear film image slightly below the inferior pupillary margin. The interferometer recorded a video for 20s and evaluated LLT automatically in nanometers based on interferometric color unit (ICU). One ICU was approximately equal to 1 nm. The average LLT was recorded for analysis.
According to the 20-second dynamic video, the BR per minute of the right eye or the only eye that was qualified was calculated for analysis.
The temperature and relative humidity in the examination room were kept at 23°C-25°C and 45%-55%. All examinations were performed by the same examiner.
Procedure
Subjects were assessed for LLT and BR at baseline. After receiving 40 µL (one drop) of 0.1% or 0.3% SH eye drops (Hialid, Santen Pharmaceutical Co, Ltd., Japan), subjects were asked to blink naturally and not to squeeze eyes or rub eyelids. The LLT and BR were then measured at 1, 5 and 15min after the instillation.
Statistical Analysis
The assessment of the normality of data was performed using the Shapiro-Wilk test. According to the normality test, an analysis of variance (ANOVA) with repeated measures or a Friedman test was used for analysis. Paired t-tests or Wilcoxon signed-rank tests were used for comparisons between baseline and each time point in the same group. A P value of less than 0.017 was considered statistically significant after correction for multiple comparisons. Two-sample t-tests or Mann-Whitney U tests were used for comparisons between two groups at the same time point. A P value of less than 0.05 was considered statistically significant. Statistical analysis was performed with SPSS (SPSS Inc., Chicago, IL, USA).
RESULTS
The baseline characteristics of the subjects are shown in Table 1. There were 56 eyes with lipid deficiency. Twenty-eight eyes were treated with 0.1% SH eye drops and the others were treated with 0.3% SH eye drops. There were 50 eyes without lipid deficiency. Twenty-five eyes were treated with 0.1% SH eye drops and the others were treated with 0.3% SH eye drops. The mean age, gender, TBUT, Schirmer I test and baseline LLT of these two groups were not significantly different (P>0.05). According to the baseline LLT, we separately analyzed the lipid deficiency type (baseline LLT <75 nm) and the non-lipid deficiency type (baseline LLT ≥75 nm). A significant difference was not found across age, gender, TBUT and Schirmer I test between the groups.
Table 1. Comparisons of baseline characteristics of the subjects between the groups.
| Parameters | Baseline LLT <75 nm |
Baseline LLT ≥75 nm |
||||
| 0.1% SH (n=28 eyes) | 0.3% SH (n=28 eyes) | aP | 0.1% SH (n=25 eyes) | 0.3% SH (n=25 eyes) | aP | |
| Age (y) | 48.18±14.75 | 46.69±18.42 | 0.799 | 48.13±15.00 | 52.80±15.76 | 0.413 |
| Gender (M/F) | 7/10 | 5/11 | 0.721 | 1/14 | 5/10 | 0.169 |
| TBUT (s) | 4.00±1.61 | 3.14±1.41 | 0.050 | 4.08±1.71 | 5.04±2.98 | 0.502 |
| Schirmer I test (mm) | 5.82±2.86 | 6.29±2.90 | 0.488 | 4.96±3.14 | 5.60±2.60 | 0.276 |
SH: Sodium hyaluronate; LLT: Lipid layer thickness; TBUT: Tear break-up time. aComparisons between 0.1% SH and 0.3% SH at baseline.
mean±SD
Time Course of Changes in the Lipid Layer Thickness
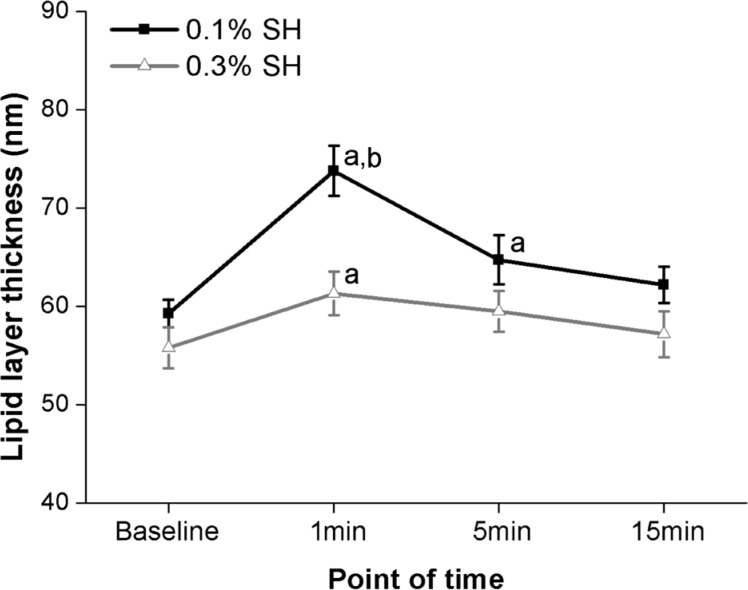
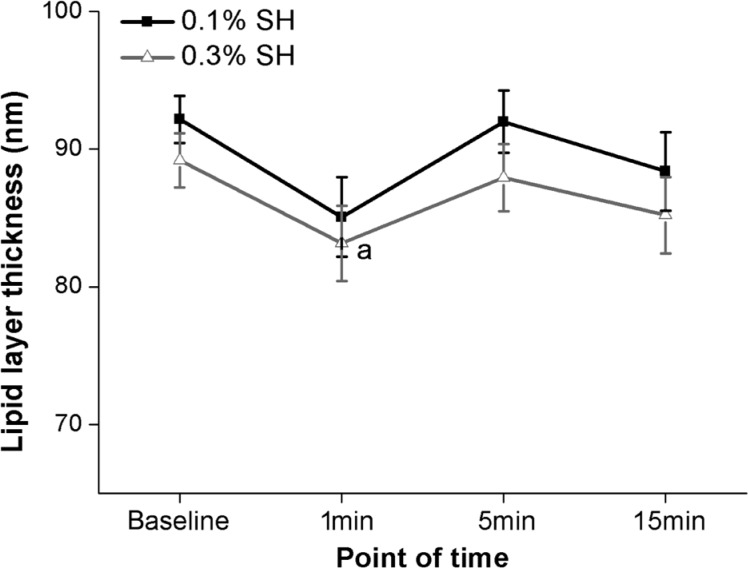
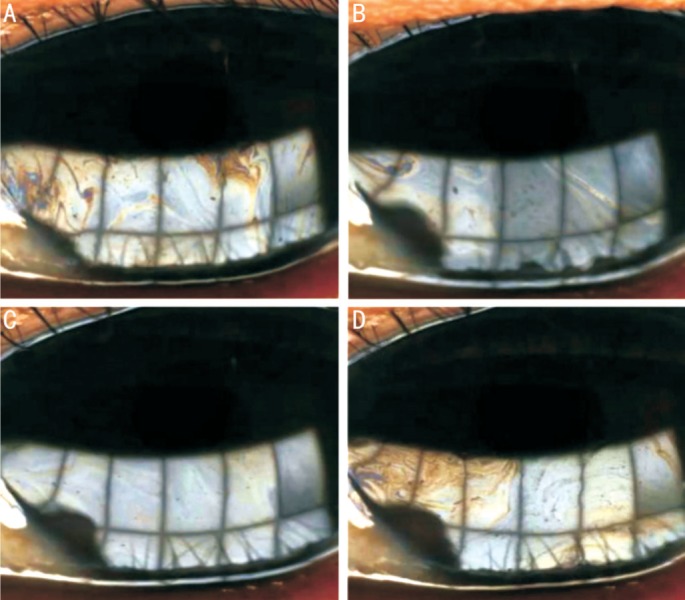
Fifty-six eyes with lipid deficiency (baseline LLT <75 nm) were included. The mean LLT was 59.29±1.40 nm for eyes treated with 0.1% SH and 55.82±2.08 nm for eyes treated with 0.3% SH. These baseline LLT were not significantly different (P>0.05). Results of repeated measures ANOVA showed significant differences in LLT among different time points (0.1% SH: F=16.758, P<0.001; 0.3% SH: F=3.416, P=0.021). The LLT significantly increased at 1min post instillation (Figure 1). The LLT increased to 73.79±2.54 nm for eyes treated with 0.1% SH (P<0.001) and to 61.32±2.20 nm for eyes treated with 0.3% SH (P=0.006). The LLT after the instillation of 0.1% SH was significantly higher than that after the instillation of 0.3% SH (P<0.001). The LLT returned to baseline at 15min post instillation of 0.1% SH (P=0.058) and at 5min post instillation of 0.3% SH (P=0.026). After the instillation of 0.1% SH eye drops, the color of the lipid layer interference images became deeper and flowing wave-like patterns could be seen (Figure 2B). At 15min, the lipid layer images became similar to baseline patterns (Figure 2C, 2D).
Figure 1. Time course of the average lipid layer thickness of eyes with lipid deficiency treated with 0.1% and 0.3% SH eye drops.
aSignificant differences compared with baseline (P<0.01); bSignificant difference compared with 0.3% SH (P<0.001).
Figure 2. Changes in the lipid layer patterns of eyes with lipid deficiency before and 1, 5 and 15min after the instillation of 0.1% SH eye drops.
A: Before the instillation, the pattern of the images are gray and uniformly distributed; B: After the instillation, the dominant color of the images become deeper and flowing wave-like pattern can be seen, and the tear meniscus height increases; C, D: The color of the images fades with time and the patterns become basically the same with those before the instillation.
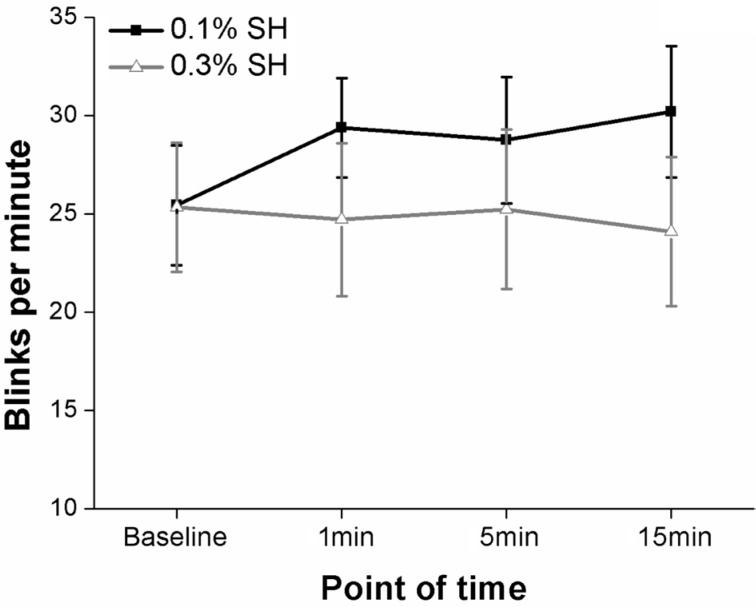
Fifty eyes without lipid deficiency (baseline LLT ≥75 nm) were included. The mean LLT was 92.16±1.73 nm for eyes treated with 0.1% SH and 89.20±1.96 nm for eyes treated with 0.3% SH. These baseline LLT were not significantly different (P>0.05). Results of the Friedman tests showed significant differences in LLT among different time points (0.1% SH: χ2=8.906, P=0.031; 0.3% SH: χ2=15.643, P=0.001). There was a decrease in LLT at 1min post instillation (Figure 3). The LLT decreased to 85.08±2.88 nm for eyes treated with 0.1% SH, but it was not statistically different from baseline (P=0.023>0.017). The LLT decreased to 83.16±2.74 nm for eyes treated with 0.3% SH, which was marginally statistically different from baseline (P=0.015<0.017). The LLT 5min after the instillation of 0.1% and 0.3% SH both returned to baseline (both P>0.05). There was no significant difference in LLT between two treatments at any time point. Before the instillation, the lipid layer interference images mainly showed colored interference fringes and wave-like patterns (Figure 4A). After the instillation, the color of the images became lighter and the waves reduced (Figure 4B, 4C). At 15min, the lipid layer images became similar to baseline patterns (Figure 4D).
Figure 3. Time course of the average lipid layer thickness of eyes without lipid deficiency treated with 0.1% and 0.3% SH eye drops.
aSignificant difference compared with baseline (P=0.015).
Figure 4. Changes in the lipid layer patterns of eyes without lipid deficiency before and 1, 5 and 15min after the instillation of 0.3% SH eye drops.
A: Before the instillation, colored interference fringes and wave-like patterns can be seen; B, C: One minute and 5min after the instillation, the color of the images become lighter, the waves reduce and the tear meniscus height increases; D: Fifteen minutes after the instillation, the patterns become basically the same with those before the instillation.
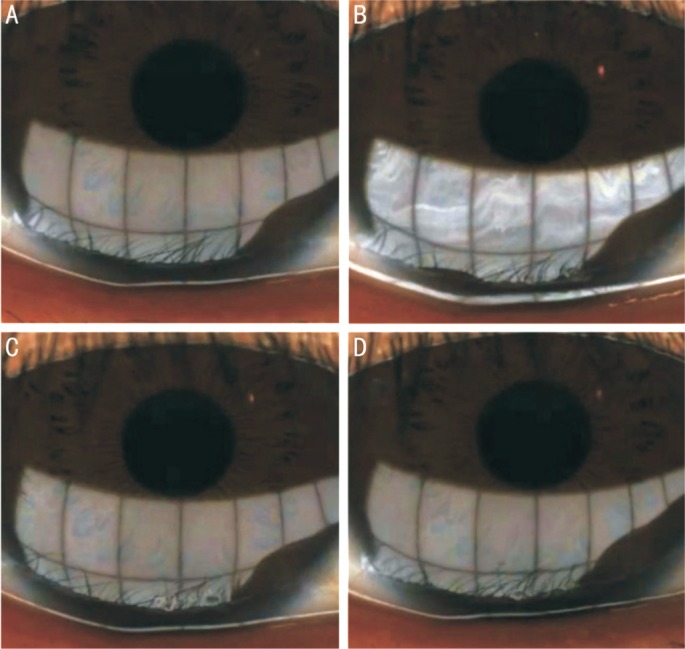
Time Course of Changes in the Blink Rate
The BR were not significantly different at different time points for eyes treated with 0.1% or 0.3% SH (0.1% SH: χ2=6.149, P=0.105; 0.3% SH: χ2=0.299, P=0.960), and there was no significant difference in BR between two treatments at each time point (Figure 5).
Figure 5. Time course of the mean BR of eyes treated with 0.1% and 0.3% SH eye drops.
Data are presented as mean±standard error. BR did not significantly change after the instillation.
DISCUSSION
The integrity of the tear film is the basis of maintaining the integrity and function of the ocular surface and is important for ocular comfort. The tear film lipid layer is important for retarding tear evaporation and maintaining tear film stability[2]. LLT was also correlated with the severity of dry eye symptoms[4]. To offer more ocular comfort to patients, the tear film stability must be maintained by preventing disruption of the normal structure of the lipid layer.
The instillation of artificial tears transitorily interferes with the normal structure of the tear film[5]–[6] and induces changes of the tear dynamics. Trees and Tomlinson[7] reported that tear evaporation rate would increase after the instillation of artificial tears, although this change was relatively short-term (5.5-9.5min) and limited. They speculated that the instillation of artificial tears might disturb or even disrupt the lipid layer, which resulted in tear film instability. In our study, we found that LLT decreased after the instillation of SH in patients without lipid deficiency. The slightly decreased LLT returned to baseline within 5min. The significantly increased tear fluid volume after the instillation of SH eye drops improved the spreading of the lipid layer[19], which induced the thinning of LLT on the inferior cornea. The slight decrease in the thickness of a relatively thick lipid layer produced by the instillation of artificial tears was short-term and limited, which might have little influence on symptoms and feelings of patients after the application of artificial tears. We propose that the frequency of patients using artificial tears would be better set as the minimum times under the premise that the dose was enough for replenishing tears, in order to attempt to avoid interference with the tear film structure from frequent use of artificial tears.
We also found that LLT increased after the instillation of 0.1% and 0.3% SH in patients with lipid deficiency and became similar to baseline within 15min and 5min, respectively. In addition, the LLT was higher for eyes treated with 0.1% SH than that treated with 0.3% SH. However, these increased LLT were still lower than those in patients without lipid deficiency. We speculated that the following reasons might explain why the thickness of a relatively thin lipid layer increased after the instillation of SH eye drops. There is much more lipid in the lid marginal reservoir than the tear film. The preocular tear film contains about 9 µg of lipid, while there is about 300 µg of lipid in the marginal reservoir[20]–[21]. With the up-phase of blinking, the upper eyelid draws lipid from the marginal reservoir to the surface of the tear film and the lipid spreads rapidly to form the tear film lipid layer[10]. The instillation of SH eye drops significantly increased the tear meniscus height and tear meniscus area for 3-10min[13]. The increased tear meniscus measurements suggested that the contact area of the tear meniscus with the lid margin and meibomian orifices increased. More lipid could be drawn from the marginal reservoir and mix with the original lipid on the tear film during blinking, and the tear film LLT could increase. The difference of the increase in LLT between different concentrations of SH eye drops might be associated with the viscosity of eye drops. The viscosity of a low concentration of eye drops was lower than that of a high concentration of eye drops. The fluidity of the aqueous layer and lipid layer would be better after the instillation of a low concentration of eye drops, and the lipid on marginal reservoir would be easier to spread over the tear film. After the instillation of a high concentration of eye drops, the viscous material would initially accumulate on the lower tear meniscus and totally mix with tear film only after repeated blinking. This might affect the spreading of lipid from lid margin to the tear film. The lipid layer of patients with lipid deficiency would be more susceptible to artificial tears and a low concentration of artificial tears had a stronger effect than a high concentration of artificial tears on the increase in LLT. It indicated that a low concentration of artificial tears might be better for patients with lipid deficiency.
The instillation of artificial tears could induce the changes in tear film LLT, which might affect the tear evaporation and tear film stability. If the duration of this disruption was long and the recovery speed was slow, the dry eye symptoms would not improve or would even worsen and the feelings of patients after the instillation would be affected. Besides the degree of aqueous deficiency, the tear film LLT of dry eye patients also needs to be taken into account when considering the frequency of using artificial tears to maintain the stability of the tear film and improve the symptoms. The precise diagnosis could be critical before prescription of SH, as it might affect tear film stability among patients without lipid deficiency.
Blinking is an important mechanism for reforming the tear film, protecting the ocular surface epithelium, and maintaining visual performance[22]. Blinking plays a major role in the distribution and drainage of tears[9]. Blinking causes the redistribution of tear fluid and induces the drainage system to remove excessive fluid to maintain the dynamic balance of tear volume over the ocular surface. Blinking is also important for the formation and distribution of the lipid layer[10]–[11]. Results of our study showed that the changes in LLT caused by the instillation of SH eye drops could return to baseline within a short time. Blinking might play an important role in the quick recovery of LLT. In our study, there was no changes of BR after the instillation. The instillation of SH eye drops might not have influence on BR in a short time.
In conclusion, SH eye drops induced a short-term increase in LLT of patients with lipid deficiency. A low concentration of artificial tears had a stronger effect than a high concentration of artificial tears on the increase in LLT. In comparison, SH eye drops induced a transient and slight decrease in LLT of patients without lipid deficiency. Results of this study indicate that a low concentration of artificial tears may be better for patients with lipid deficiency.
Acknowledgments
Foundations: Supported by Provincial Frontier and Key Technology Innovation Special Fund of Guangdong Province (No.2015B020227001); Guangzhou Science and Technology Plan Scientific Research Projects (No.201504010023); Fundamental Research Funds of State Key Laboratory of Ophthalmology of China, and Five Five Cultivation Project of Ophthalmic Center, Sun Yat-sen University.
Conflicts of Interest: Li Y, None; Sang X, None; Yang L, None; Wang XR, None; Liu JH, None; He XJ, None; Liu Y, None; Lu XH, None; Wang ZC, None.
REFERENCES
- 1.Lemp MA, Crews LA, Bron AJ, Foulks GN, Sullivan BD. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472–478. doi: 10.1097/ICO.0b013e318225415a. [DOI] [PubMed] [Google Scholar]
- 2.Millar TJ, Schuett BS. The real reason for having a meibomian lipid layer covering the outer surface of the tear film-a review. Exp Eye Res. 2015;137:125–138. doi: 10.1016/j.exer.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 3.Craig JP, Tomlinson A. Importance of the lipid layer in human tear film stability and evaporation. Optom Vis Sci. 1997;74(1):8–13. doi: 10.1097/00006324-199701000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Blackie CA, Solomon JD, Scaffidi RC, Greiner JV, Lemp MA, Korb DR. The relationship between dry eye symptoms and lipid layer thickness. Cornea. 2009;28(7):789–794. doi: 10.1097/ICO.0b013e318191b870. [DOI] [PubMed] [Google Scholar]
- 5.Ridder WR, Lamotte JO, Ngo L, Fermin J. Short-term effects of artificial tears on visual performance in normal subjects. Optom Vis Sci. 2005;82(5):370–377. doi: 10.1097/01.opx.0000162646.30666.e3. [DOI] [PubMed] [Google Scholar]
- 6.Ridder WR, LaMotte J, Hall JJ, Sinn R, Nguyen AL, Abufarie L. Contrast sensitivity and tear layer aberrometry in dry eye patients. Optom Vis Sci. 2009;86(9):E1059–E1068. doi: 10.1097/OPX.0b013e3181b599bf. [DOI] [PubMed] [Google Scholar]
- 7.Trees GR, Tomlinson A. Effect of artificial tear solutions and saline on tear film evaporation. Optom Vis Sci. 1990;67(12):886–890. doi: 10.1097/00006324-199012000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Tsubota K, Yamada M. Tear evaporation from the ocular surface. Invest Ophthalmol Vis Sci. 1992;33(10):2942–2950. [PubMed] [Google Scholar]
- 9.Bandlitz S, Purslow C, Murphy PJ, Pult H. Time course of changes in tear meniscus radius and blink rate after instillation of artificial tears. Invest Ophthalmol Vis Sci. 2014;55(9):5842–5847. doi: 10.1167/iovs.14-14844. [DOI] [PubMed] [Google Scholar]
- 10.Bron AJ, Tiffany JM, Gouveia SM, Yokoi N, Voon LW. Functional aspects of the tear film lipid layer. Exp Eye Res. 2004;78(3):347–360. doi: 10.1016/j.exer.2003.09.019. [DOI] [PubMed] [Google Scholar]
- 11.Huang J, Hindman HB, Rolland JP. In vivo thickness dynamics measurement of tear film lipid and aqueous layers with optical coherence tomography and maximum-likelihood estimation. Opt Lett. 2016;41(9):1981–1984. doi: 10.1364/OL.41.001981. [DOI] [PubMed] [Google Scholar]
- 12.Kaya S, Schmidl D, Schmetterer L, Witkowska KJ, Unterhuber A, Aranha DSV, Baar C, Garhofer G, Werkmeister RM. Effect of hyaluronic acid on tear film thickness as assessed with ultra-high resolution optical coherence tomography. Acta Ophthalmol. 2015;93(5):439–443. doi: 10.1111/aos.12647. [DOI] [PubMed] [Google Scholar]
- 13.Akiyama-Fukuda R, Usui T, Yoshida T, Yamagami S. Evaluation of tear meniscus dynamics using anterior segment Swept-Source optical coherence tomography after topical solution instillation for dry eye. Cornea. 2016;35(5):654–658. doi: 10.1097/ICO.0000000000000807. [DOI] [PubMed] [Google Scholar]
- 14.McCann LC, Tomlinson A, Pearce EI, Papa V. Effectiveness of artificial tears in the management of evaporative dry eye. Cornea. 2012;31(1):1–5. doi: 10.1097/ICO.0b013e31821b71e6. [DOI] [PubMed] [Google Scholar]
- 15.Shahraki K, Hosseini SR, Amini FA, Shademan H, Shahraki K, Salari AM, Amini FM. Effects of topical 1% sodium hyaluronate and hydroxypropyl methylcellulose in treatment of corneal epithelial defects. Med Hypothesis Discov Innov Ophthalmol. 2016;5(4):136–144. [PMC free article] [PubMed] [Google Scholar]
- 16.Methodologies to diagnose and monitor dry eye disease: report of the Diagnostic Methodology Subcommittee of the International Dry Eye WorkShop (2007) Ocul Surf. 2007;5(2):108–152. doi: 10.1016/s1542-0124(12)70083-6. [DOI] [PubMed] [Google Scholar]
- 17.Scaffidi RC, Korb DR. Comparison of the efficacy of two lipid emulsion eyedrops in increasing tear film lipid layer thickness. Eye Contact Lens. 2007;33(1):38–44. doi: 10.1097/01.icl.0000247638.50568.c0. [DOI] [PubMed] [Google Scholar]
- 18.Fogt JS, Kowalski MJ, King-Smith PE, Epitropolous AT, Hendershot AJ, Lembach C, Maszczak JP, Jones-Jordan LA, Barr JT. Tear lipid layer thickness with eye drops in meibomian gland dysfunction. Clin Ophthalmol. 2016;10:2237–2243. doi: 10.2147/OPTH.S120158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goto E, Tseng SC. Kinetic analysis of tear interference images in aqueous tear deficiency dry eye before and after punctal occlusion. Invest Ophthalmol Vis Sci. 2003;44(5):1897–1905. doi: 10.1167/iovs.02-0818. [DOI] [PubMed] [Google Scholar]
- 20.Chew CK, Hykin PG, Jansweijer C, Dikstein S, Tiffany JM, Bron AJ. The casual level of meibomian lipids in humans. Curr Eye Res. 1993;12(3):255–259. doi: 10.3109/02713689308999471. [DOI] [PubMed] [Google Scholar]
- 21.Chew CK, Jansweijer C, Tiffany JM, Dikstein S, Bron AJ. An instrument for quantifying meibomian lipid on the lid margin: the Meibometer. Curr Eye Res. 1993;12(3):247–254. doi: 10.3109/02713689308999470. [DOI] [PubMed] [Google Scholar]
- 22.Pult H, Riede-Pult BH, Murphy PJ. The relation between blinking and conjunctival folds and dry eye symptoms. Optom Vis Sci. 2013;90(10):1034–1039. doi: 10.1097/OPX.0000000000000029. [DOI] [PubMed] [Google Scholar]