Abstract
AIM
To evaluate the long-term results and complications of Ahmed glaucoma valve (AGV) implantation in a cohort of Egyptian patients.
METHODS
A retrospective study of 124 eyes of 99 patients with refractory glaucoma who underwent AGV implantation and had a minimum follow-up of 5y was performed. All patients underwent complete ophthalmic examination and intraocular pressure (IOP) measurement before surgery and at 1d, weekly for the 1st month, 3, 6mo, and 1y after surgery and yearly afterward for 5y. IOP was measured by Goldmann applanation tonometry and/or Tono-Pen. Complications and the number of anti-glaucoma medications needed were recorded. Success was defined as IOP less than 21 mm Hg with or without anti-glaucoma medication and without additional glaucoma surgery.
RESULTS
Mean age was 23.1±19.9y. All eyes had at least one prior glaucoma surgery. IOP was reduced from a mean of 37.2±6.8 to 19.2±5.2 mm Hg after 5y follow-up with a reduced number of medications from 2.64±0.59 to 1.81±0.4. Complete and qualified success rates were 31.5% and 46.0% respectively at the end of follow-up. The most common complications were encapsulated cyst formation in 51 eyes (41.1%), complicated cataract in 9 eyes (7.25%), recessed tube in 8 eyes (6.45%), tube exposure in 6 eyes (4.8%) and corneal touch in 6 eyes (4.8%). Other complications included extruded AGV, endophthalmitis and persistent hypotony. Each of them was recorded in only 2 eyes (1.6%).
CONCLUSION
Although refractory glaucoma is a difficult problem to manage, AGV is effective and relatively safe procedure in treating refractory glaucoma in Egyptian patients with long-term follow-up. Encapsulated cyst formation was the most common complication, which limits successful IOP control after AGV implantation. However, effective complications management can improve the rate of success.
Keywords: intraocular pressure, Ahmed glaucoma valve, refractory glaucoma, long-term follow-up of glaucoma, Ahmed valve complications
INTRODUCTION
Various surgical techniques have been proposed for treatment of refractory glaucoma such as mitomycin C, augmented trabeculectomy and the use of glaucoma drainage devices[1]–[2]. The use of glaucoma drainage devices has increased dramatically in the past 20y. The number of the aqueous shunt implantations performed annually has risen from 2356 in 1994 to 12 012 in 2012 according to a recent analysis of US Medi Care database[2]–[3].
Different kinds of glaucoma drainage devices have been used as an alternative to the standard filtering surgery or cyclodestructive procedures in refractory glaucoma[4]–[6]. Indications include eyes with refractory glaucoma, such as neovascular glaucoma, uveitic glaucoma, glaucoma in aphakia and pseudophakia and eyes that have previously failed filtering operation[5].
The Ahmed glaucoma valve (AGV; New World Medical Inc., Rancho Cucamonga, California, USA) was introduced into market in 1993. It is a restrictive type of glaucoma devices that prevent postoperative hypotony[7]. Several studies on the success rate of AGV had been reported a number of complications involving the tube have been reported following insertion, such as tube blockage, retraction, exposure, malposition as well as more serious complications like hypotony, choroidal effusion, choroidal hemorrhage, cataract, retinal detachment and diplopia[2],[8]–[10]. However, long-term reports on the outcomes of the glaucoma devices from the Middle East, including Egypt, are rare[11]. So, it was interesting for us to evaluate safety and efficacy and long-term results of AGV implantation in resistant cases of glaucoma over a long period of follow-up.
SUBJECTS AND METHODS
This is a retrospective study of all patients who underwent AGV implantation for consecutive cases with refractory glaucoma in Mansoura Ophthalmic Center, Mansoura University, Egypt, during the period from May 2007 to September 2011. The study was approved by the Institutional Research Board of the Mansoura Faculty of Medicine and was performed in accordance with the ethical standards laid down in the Declaration of Helsinki with confidentiality of patients' records. Inclusion criteria included patients with increased intraocular pressure (IOP) >21 mm Hg that was not responsive to maximal medical treatment after failed glaucoma surgery.
All patients included in this study attended for regular follow-up visits in our clinic. All the operations were performed by the same surgeon (Elhefney E). The valve used was either S2 or S3 model according to the age of the patient.
Surgical Technique
Fornix based conjunctival flap was performed in the superior temporal quadrant. The sclera was exposed. The tube was primed using balanced salt solution. The plate was fixed to the sclera at a distance of 8-10 mm from the limbus using two 7/0 prolene sutures. A scleral flap 4 mm×4 mm was created and the tube was inserted into the anterior chamber after being trimmed with the bevel up through a pathway created at the limbus using 23 or 25-gauge needle in a plane parallel to the iris. In children, if scleral patch graft was available, no scleral flap was performed. A 9/0 prolene mattress suture was sutured to the sclera for more fixation of the tube. The conjunctiva was opposed using 6/0 vicryl sutures. At the end of the surgery, subconjunctival cefazoline and dexamethasone were injected.
The postoperative regimen included topical ciprofloxacin 0.3 mg/mL four times daily for one week and 1% prednisolone acetate eight times daily for one week, with subsequent tapering over one month, dictated by the level of postoperative inflammation. Anti-glaucoma medications were added when required if the IOP increased >21 mm Hg. Patients were examined daily in the 1wk, weekly in the 1, 3, 6mo and 1y postoperatively then yearly till 5y after the surgery. Preoperative data included patients' age, sex, IOP and anti-glaucoma medications. Postoperative data included IOP, number of anti-glaucoma medications, success and failure rates and complications.
In our study IOP success was considered with an upper limit of 21 mm Hg and a lower limit of 6 mm Hg. Complete success was defined as IOP<21 mm Hg without anti-glaucoma medication or need for additional surgery and absence of any vision-threatening complication. Qualified success was defined as IOP<21 mm Hg with the use of anti-glaucoma medications.
According to World Glaucoma Association (WGA), failure was defined as an IOP level measured above the upper limit or below the lower limit on two consecutive study visits.
Complete failure was defined as loss of light perception attributable to glaucoma, or the necessity for further glaucoma surgical intervention. However, certain postoperative surgical adjustments, such as flap suturelysis, suture release, or Nd:YAG gonio puncture to the trabeculo-Descemet's window were excluded from this category and would not be recorded as evidence of failure.
Statistical Analysis
Data were analyzed by statistical package SPSS version 15.0 for Windows (SPSS, Inc., Chicago, IL, USA). The values presented are the mean and standard deviation (SD) for each study variable. The Wilcoxon rank-sum test for paired data was applied to assess the significance of differences between preoperative and postoperative data. The level of significance used was always the same (P<0.05).
RESULTS
The study included 124 eyes of 99 patients with 84 eyes receiving model S3 and 40 eyes receiving model S2 AGV implants. The mean age was 23.1±19.9y (range 11mo-40y) at the time of AGV implantation. All eyes had at least one prior filtering glaucoma surgery with or without antimetabolites with a mean number of previous glaucoma surgery of 1.1±0.6 (range 1-3). Demographic data, types of glaucoma and previous ocular surgeries are demonstrated in Tables 1 and 2.
Table 1. The demographic data of the studied population.
| Parameters | Data |
| No. of patients/eyes | 99/124 |
| Mean age (range) | 23.1±19.9y (11mo-40y) |
| Gender | |
| M | 48 (48.5) |
| F | 51 (51.5) |
| Types of glaucoma | |
| Congenital | 25 (20.2) |
| POAG | 10 (8.1) |
| Apakic | 39 (31.5) |
| Pseduphakic | 50 (40.3) |
n (%)
Table 2. Previous ocular surgeries.
| Surgerya | No. of eyes (%) |
| Filtering glaucoma surgery | 124 (100) |
| Combined trabeculotomy and trabeculectomy without MMC | 57 (46.0) |
| Trabeculectomy without MMC | 51 (41.1) |
| Trabeculectomy with MMC | 16 (12.9) |
| Cataract extraction | 89 (71.8) |
| Cataract extraction only | |
| Congenital cataract | 29 (23.4) |
| Traumatic cataract | 10 (8.0) |
| Cataract extraction and intraocular lens implantation | |
| Congenital cataract | 26 (21.0) |
| Traumatic cataract | 15 (12.1) |
| Senile cataract | 9 (7.3) |
aSome patients had more than one previous operation.
There is significant reduction of IOP from 37.2±6.8 mm Hg (range 28-46) preoperatively to19.2±5.2 mm Hg (range 16-24) at the end of follow-up time (P<0.001, Wilcoxon rank-sum test). The mean preoperative and postoperative glaucoma medications were 2.64±0.59 and 1.81±0.4 respectively (P=0.04, Wilcoxon rank-sum test) at the last follow-up (Table 3). Postoperative outcomes in different patients groups at the end of follow-up were recorded in Table 4.
Table 3. Changes of IOP and anti-glaucoma medications during follow-up periods.
| Parameters | Preoperative | Postoperative |
|||||||||
| 1mo | P | 6mo | P | 1y | P | 3y | P | 5y | P | ||
| IOP (mm Hg) | 37.2±6.8 | 12.1±1.3 | <0.001 | 15.2±2.2 | <0.001 | 16.4±4.1 | <0.001 | 19.3+4.1 | <0.001 | 19.2±5.2 | <0.001 |
| Glaucoma medication | 2.64±0.59 | 1.81±0.59 | 0.02 | 1.46±0.44 | 0.03 | 1.9±0.65 | 0.02 | 1.74±0.51 | 0.02 | 1.81±0.4 | 0.04 |
IOP: Intraocular pressure. P: Wilcoxon rank-sum test, significance <0.0.5.
mean±SD
Table 4. Postoperative outcomes in different patients groups.
| Parameters | No. of eyes (%) |
| Previous trabeculectomy or combinedprocedure without MMC | 108 (100) |
| Failure | 25 (23.1) |
| Qualified success | 53 (49.1) |
| Complete success | 30 (27.8) |
| Previous trabeculectomy with MMC | 16 (100) |
| Failure | 3 (18.75) |
| Qualified success | 4 (25.00) |
| Complete success | 9 (56.25) |
| Previous cataract extraction | 89 (100) |
| Failure | 17 (19.1) |
| Qualified success | 41 (46.1) |
| Complete success | 31 (34.8) |
| Overall group | 124 (100) |
| Failure | 28 (22.6) |
| Qualified success | 57 (46.0) |
| Complete success | 39 (31.5) |
Outcomes of overall patients in different follow-up period were demonstrated in Table 5. At the end of follow-up period (5y), the percentage of success including both complete and qualified success was encountered in 77.5%. Of those, 39 eyes (31.5%) had complete success, 57 eyes (46.0%) had qualified success.
Table 5. Postoperative outcome in different follow-up periods.
| Outcome | 6mo | 1y | 3y | 5y |
| Complete success | 80 (64.5) | 72 (58.1) | 54 (43.5) | 39 (31.5) |
| Qualified success | 31 (25.0) | 38 (30.6) | 47 (37.9) | 57 (46.0) |
| Failure | 13 (10.5) | 14 (11.3) | 23 (18.5) | 28 (22.6) |
n (%)
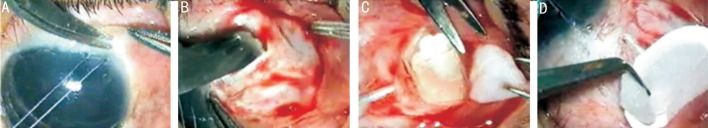
Postoperative complications were recorded in Table 6. Encapsulated AGV was the most common late complication encountered postoperatively (51 eyes, 41.1%). Other complications included cataract in 9 eyes (7.25%), recessed tube in 8 eyes (6.45%) following AGV implantation in eyes with pediatric glaucoma. Four eyes of them were managed by AGV exchange with supra-tenon flexible AGV implantation. Of 18 eyes were successfully managed by needling with MMC application followed by anti-glaucoma medication. Deroofing of the encapsulated plate was successfully performed in 20 eyes (Figure 1). The other 4 eyes were managed by second AGV implantation in the superior or superior nasal quadrant of the globe (Figure 2). Totally 13 eyes with encapsulated plate showed failure after deroofing (IOP>21 mm Hg with maximum anti-glaucoma medications). Postoperative interventions to achieve the success criteria and causes of failure are demonstrated in Tables 7 and 8 respectively.
Table 6. Postoperative complications.
| Complications | No. of eyes (%) |
| Early complicationa | |
| Choroidal effusion | 8 (6.45) |
| Shallow or flat anterior chamber | 6 (4.8) |
| Hyphema | 4 (3.2) |
| Wound leak | 2 (1.6) |
| Aqueous misdirection | 1 (0.8) |
| Late complicationsb | |
| Encapsulated plate | 51 (41.1) |
| Complicated cataract | 9 (7.25) |
| Recessed tube | 8 (6.45) |
| Exposed tube | 6 (4.8) |
| Corneal-tube touch | 6 (4.8) |
| Extruded AGV | 2 (1.6) |
| Endophthalmitis | 2 (1.6) |
| Persistent hypotony | 2 (1.6) |
| Tube infection | 1 (0.8) |
| Total No. of eyesc | 51 (41.1) |
aWithin 1mo; b>1mo; cSome patients had more than one complication.
Figure 1. Deroofing of encapsulated plate.
A: Creation of conjunctival flap; B: An incision for plate deroofing; C: Excision of the fibrotic cyst; D: Application of MMC.
Figure 2. A case of recessed tube (black arrows) managed by second AGV implantation in the superior quadrant of the globe (arrowheads).
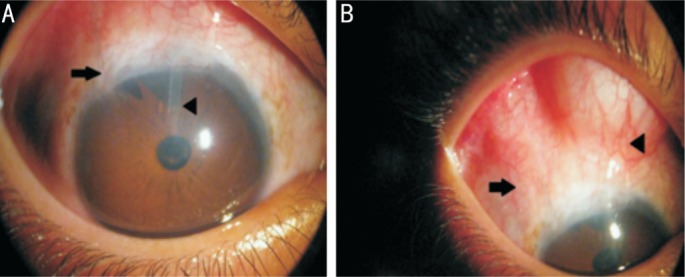
Table 7. Postoperative interventions to achieve the success criteria.
| Postoperative intervention | No. of eyes (%) |
| Needling+MMC | 18 (14.5) |
| Excision of the encapsulated plate cyst (deroofing) | 20 (16.1) |
| Valve replacement (supra-tenon silicon plated AGV) | 7 (5.64) |
| Tube shortening (cornea-tube touch) | 6 (4.8) |
| Intravitreal injection (endophthalmitis) | 2 (1.6) |
| Contact cyclodiode | 2 (1.6) |
| Scleral patch graft | 6 (4.8) |
| Cataract extraction | 7 (5.6) |
Table 8. Causes of failure.
| Causes | No. of eyes (%) |
| Chronic hypotony | 2 (1.6) |
| Endophthalmitis | 2 (1.6) |
| Extruded AGV | 2 (1.6) |
| Recessed tube | 8 (6.45) |
| Tube infection | 1 (0.8) |
| Failure of deroofing of encapsulated plate | 13 (10.5) |
DISCUSSION
AGV, with a restriction flow mechanism, is a shunt device that is used in treatment of refractory glaucoma either as a primary surgical option or after failure of conventional filtration procedures. The overall success rate varies among different types of glaucomas, ranging from 60% to 100% at one year of follow-up in different case series with different follow-up periods[12]. However, prior glaucoma surgery increases the risk of failure of glaucoma implantation by more than three-fold[13]. In addition, the use of antimetabolites increases the long-term side effects particularly in pediatric patients[14].
To best of our knowledge, most of the studies regarding the success of glaucoma drainage devices were carried in the developed countries, with limited numbers of published studies in the developing countries with small sample size and variable follow-up duration[11],[15]–[16]. In the current study, we retrospectively reviewed the results of AGV implantation in cohort of Egyptian patients with refractory glaucoma with long-term follow-up.
In our study, AGV implant was able to decrease the mean preoperative IOP from 37.2±6.8 mm Hg to 16.4±4.1 mm Hg at 12mo and 19.2±5.2 mm Hg at 5y postoperatively. Moreover, reduction of the number or frequency of medications to control IOP is considered as a parameter of success in refractory glaucoma. In our study, glaucoma medications were reduced from 2.64±0.59 preoperatively to 1.81±0.4 at the end of follow-up period. This observation concurs with Souza et al[12] and Wishart et al[10] who reported a significant reduction in the number of medications following AGV implantation.
Zarei et al[11] reported IOP decrease from a mean preoperative value of 30.8±5.6 mm Hg to 20±6.4 mm Hg with a mean follow-up time of 40.50mo after AGV implantation. Similar results were demonstrated in various studies carried in Kuwait[15], Saudi Arabia[16], and Oman[17] in which AGV implantation reduced IOP and the number of medications required to control refractory glaucoma.
In our study, the overall success rate (complete and qualified) varies among different types of glaucoma, with average of 89.5% at 1y, 81.5% at 3y and 77.4% at 5y of follow-up. The failure occurred in 28 eyes (22.6%) at the end of follow-up. Similar results were reported by Smith et al[18], with complete success of rate of 10.5% and guarded success rate of 73.7% in cases that underwent AGV surgeries during a mean follow-up time of 38.8mo. However, failure rate in the current study is a little bit higher than recorded by tube versus trabeculectomy (TVT) study[19] as all included eyes in our study were eyes with failed previous incisional surgeries that could increase the risk of failure of AGV implantation as reported before[12]. On the other hand, our results were somewhat better than recorded in other studies. Lai et al[20] reported IOP control in 73.8% of 65 Chinese eyes during follow-up time ranging from 6-37mo following AGV implantation, the absolute success was 43.1% and qualified success was 30.7%. Souza et al[12] reported that approximately 50% of AGV implantation in refractory glaucoma were successful after 5y of follow-up. Zarei et al[11] reported 70% success rate with adjuvant anti-glaucoma medications within a mean follow-up of 40mo after AGV implantation in 28 eyes with age ranging from 7-75y. The differences on types of races of the study population, type of implants, etiology of glaucoma, and the duration of follow-up, could explain the variations in success rate between studies.
The major cause of failure was excessive fibrosis and encapsulated cyst formation (41.1%) which were consistent with the other studies[23]–[24]. The incidence of bleb encapsulation has been recorded to be between 40% and 80% with the AGV implantation in different studies of refractory glaucoma[5]–[6]. Needling with MMC injection was performed in 18 eyes of our studied patients (14.5%). Deroofing of the encapsulated plate with cyst excision was successfully performed in 20 eyes (16.1%) followed with adjuvant anti-glaucoma treatment. Capsule excision after failed Molteno surgery was examined by Valimaki et al[24], they reported a 52% success rate with revision alone (IOP less than 22 mm Hg), whereas 42% required a second tube shunt for IOP control. Lai et al[20] reported encapsulated bleb in 16 eyes (24.6%). Totally 10 eyes received needling with MMC and 6 eyes received cyst excision. The IOP was successfully controlled in 14 eyes of them[20].
Cataract formation was the second most common complication that reported in 9 eyes (7.25%) in our study. Similarly, Zarei et al[11] reported tube iris touch with cataract in 10.8%. Recessed tube occurred in 8 eyes (6.5%) with recurrent congenital glaucoma most probably due to increased globe size during growth. They were managed with AGV replacement using flexible implant in the supra-tenon space. Tube exposure was recorded in 6 eye (4.8%) with pediatric glaucoma mostly due to recessed conjunctiva and lack of sclera patch graft at the time of AGV implantation, which was managed, by sclera patch graft and conjunctival advancement.
Lai et al[20] reported exposure of the tube due to erosion of the episcleral patch graft in 3.1% and extrusion of the implant in 6.2% of 65 eyes underwent AGV implantation. In our study, extrusion was recorded in only 2 eyes (1.6%). Quaranta et al[25] achieved the outcomes improvement of AGV surgery by usage of, bovine pericardial graft to cover valve without using suture. This enabled to reduce both mean IOP as well as the number of medication in refractory glaucoma patients.
In a study carried by Zarei et al[11] focal corneal decompensation was demonstrated in 10.7% due to corneal tube touch. Chen et al[26] reported corneal decompensation in 2.3% and implant extrusion in 1.4% of 221 eyes following AGV implantation. In the current study, focal corneal tube touch with was recorded in only 6 eyes (4.8%) due to anterior tube migration. However, such problem was managed successfully by tube revision before occurrence of corneal decompensation.
Different studies on AGV implantation outcome for refractory glaucoma reported frequencies of hypotony varying from 9.4% to 12%[27]–[28]. Severe hypotony requiring removal of the AGV occurred in only 2 of the 124 operated eyes in our series (1.6%). Although endophthalmitis is a rare complication after glaucoma drainage implant (GDI) surgery, the exact rate is not known[29]. Several retrospective studies of GDIs have included a single case or a few cases of endophthalmitis resulting in rates ranging from 0.8% to 6.3%[3],[29]–[34]. We reported only 2 eyes with endophthalmitis of 124 studied eyes (1.6%). Conjunctival dehiscence over the GDI tube seems to represent a major risk factor for endophthalmitis[33].
A limitation of this study is that it is a retrospective with inclusion of only subjects with previously failed filtering surgeries and refractory glaucoma. We tried to minimize this by using all of the AGV patients who qualified for the study during last 5y and operated by the same surgeon. Another limitation is lack of homogeneity of the study population, which was eliminated by studying larger sample size with longer follow-up than reported in most of the published literatures.
In conclusion, refractory glaucoma with failed previous incisional glaucoma surgery is very difficult situation to manage. AGV is effective in treating refractory glaucoma with increasing the rate of success by effective management of complications. Encapsulated cyst formation was the most common complication, which can affect successful IOP control without anti-glaucoma medication.
Acknowledgments
Conflicts of Interest: Elhefney E, None; Mokbel T, None; Abou Samra W, None; Kishk H, None; Mohsen T, None; El-Kannishy A, None.
REFERENCES
- 1.Kaya M, Ozbek Z, Yaman A, Durak I. Long-term success of ahmed glaucoma valve in refractory glaucoma. Int J Ophthalmol. 2012;5(1):108–112. doi: 10.3980/j.issn.2222-3959.2012.01.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu Y, Hong T, Li W. Long-term outcomes of Ahmed glaucoma valve implantation for treating refractory glaucoma. Zhonghua Yi Xue Za Zhi. 2015;95(6):440–443. [PubMed] [Google Scholar]
- 3.Budenz DL, Feuer WJ, Barton K, Schiffman J, Costa VP, Godfrey DG, Buys YM, Ahmed Baerveldt Comparison Study Group Postoperative complications in the Ahmed Baerveldt Comparison Study during five years of follow-up. Am J Ophthalmol. 2016;163:75–82.e3. doi: 10.1016/j.ajo.2015.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Susanna R, Jr, Latin American Glaucoma Society Investigators Partial Tenon's capsule resection with adjunctive mitomycin C in Ahmed glaucoma valve implant surgery. Br J Ophthalmol. 2003;87(8):994–998. doi: 10.1136/bjo.87.8.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah AA, WuDunn D, Cantor LB. Shunt revision versus additional tube shunt implantation after failed tube shunt surgery in refractory glaucoma. Am J Ophthalmol. 2000;129(4):455–460. doi: 10.1016/s0002-9394(99)00410-9. [DOI] [PubMed] [Google Scholar]
- 6.Schwartz KS, Lee RK, Gedde SJ. Glaucoma drainage implants: a critical comparison of types. Curr Opin Ophthalmol. 2006;17(2):181–189. doi: 10.1097/01.icu.0000193080.55240.7e. [DOI] [PubMed] [Google Scholar]
- 7.Coleman AL, Hill R, Wilson MR, Choplin N, Kotas-Neumann R, Tam M, Bacharach J, Panek WC. Initial clinical experience with the Ahmed glaucoma valve implant. Am J Ophthalmol. 1995;120(1):23–31. doi: 10.1016/s0002-9394(14)73755-9. [DOI] [PubMed] [Google Scholar]
- 8.Tran DH, Souza C, Ang MJ, Loman J, Law SK, Coleman AL, Caprioli J. Comparison of long-term surgical success of Ahmed valve implant versus trabeculectomy in open-angle glaucoma. Br J Ophthalmol. 2009;93(11):1504–1509. doi: 10.1136/bjo.2008.150870. [DOI] [PubMed] [Google Scholar]
- 9.Jacob J, Stalmans I, Zeyen T. Ahmed and Baerveldt glaucoma drainage implants: long-term results and factors influencing outcome. Bull Soc Belge Ophtalmol. 2009;(313):19–29. [PubMed] [Google Scholar]
- 10.Wishart PK, Choudhary A, Wong D. Ahmed glaucoma valves in refractory glaucoma: a 7-year audit. Br J Ophthalmol. 2010;94(9):1174–1179. doi: 10.1136/bjo.2009.165357. [DOI] [PubMed] [Google Scholar]
- 11.Zarei R, Amini H, Daneshvar R, Nabi FN, Moghimi S, Fakhraee G, Eslami Y, Mohammadi M, Amini N. Long-term outcomes of Ahmed glaucoma valve implantation in refractory glaucoma at Farabi Eye Hospital, Tehran, Iran. Middle East Afr J Ophthalmol. 2016;23(1):104–109. doi: 10.4103/0974-9233.164611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Souza C, Tran DH, Loman J, Law SK, Coleman AL, Caprioli J. Long-term outcomes of Ahmed glaucoma valve implantation in refractory glaucomas. Am J Ophthalmol. 2007;144(6):893–900. doi: 10.1016/j.ajo.2007.07.035. [DOI] [PubMed] [Google Scholar]
- 13.Nilforushan N, Yadgari M, Jazayeri AA, Karimi N. Evaluation of success after second Ahmed glaucoma valve implantation. Indian J Ophthalmol. 2016;64(3):206–210. doi: 10.4103/0301-4738.181740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wells AP, Cordeiro MF, Bunce C, Khaw PT. Cystic bleb formation and related complications in limbus- versus fornix-based conjunctival flaps in pediatric and young adult trabeculectomy with mitomycin C. Ophthalmology. 2003;110(11):2192–2197. doi: 10.1016/S0161-6420(03)00800-5. [DOI] [PubMed] [Google Scholar]
- 15.Aljazzaf AM, Abdelmoaty SM, Behbehani AH, Abdulmuez AA, Aljazzaf HA. The outcome of the Ahmad glaucoma valve implantation for refractory glaucoma in Kuwait. Saudi J Ophthalmol. 2013;27(1):15–18. doi: 10.1016/j.sjopt.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alasbali T, Alghamdi AA, Khandekar R. Outcomes of Ahmed valve surgery for refractory glaucoma in Dhahran, Saudi Arabia. Int J Ophthalmol. 2015;8(3):560–564. doi: 10.3980/j.issn.2222-3959.2015.03.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah MR, Khandekar RB, Zutshi R, Mahrooqi R. Short term outcome of Ahmed glaucoma valve implantation in management of refractory glaucoma in a tertiary hospital in Oman. Oman J Ophthalmol. 2013;6(1):27–32. doi: 10.4103/0974-620X.111905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith M, Geffen N, Alasbali T, Rachmiel R, Buys YM, Trope GE. Outcome of Ahmed valve implantation when preoperative IOP less than 21 mm Hg. J Glaucoma. 2009;18(9):674–678. doi: 10.1097/IJG.0b013e31819c468e. [DOI] [PubMed] [Google Scholar]
- 19.Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL, Tube Versus Trabeculectomy Study Group Three-year follow-up of the tube versus trabeculectomy study. Am J Ophthalmol. 2009;148(5):670–684. doi: 10.1016/j.ajo.2009.06.018. [DOI] [PubMed] [Google Scholar]
- 20.Lai JS, Poon AS, Chua JK, Tham CC, Leung AT, Lam DS. Efficacy and safety of the Ahmed glaucoma valve implant in Chinese eyes with complicated glaucoma. Br J Ophthalmol. 2000;84(7):718–721. doi: 10.1136/bjo.84.7.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ishida K, Ahmed II, Netland PA. Ahmed glaucoma valve surgical outcomes in eyes with and without silicone oil endotamponade. J Glaucoma. 2009;18(4):325–330. doi: 10.1097/IJG.0b013e318182ede3. [DOI] [PubMed] [Google Scholar]
- 22.Kirwan C, O'Keefe M, Lanigan B, Mahmood U. Ahmed valve drainage implant surgery in the management of paediatric aphakic glaucoma. Br J Ophthalmol. 2005;89(7):855–858. doi: 10.1136/bjo.2004.056143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eibschitz-Tsimhoni M, Schertzer RM, Musch DC, Moroi SE. Incidence and management of encapsulated cysts following Ahmed glaucoma valve insertion. J Glaucoma. 2005;14(4):276–279. doi: 10.1097/01.ijg.0000169391.94555.c1. [DOI] [PubMed] [Google Scholar]
- 24.Välimäki J, Tuulonen A, Airaksinen PJ. Capsule excision after failed Molteno surgery. Ophthalmic Surg Lasers. 1997;28(5):382–386. [PubMed] [Google Scholar]
- 25.Quaranta L, Riva I, Floriani IC. Outcomes of using a sutureless bovine pericardial patch graft for Ahmed glaucoma valve implantation. Eur J Ophthalmol. 2013;23(5):738–742. doi: 10.5301/ejo.5000260. [DOI] [PubMed] [Google Scholar]
- 26.Chen H, Zhang SX, Liu L, Lin D, Tang X, Sun L, Wang T, Wang H, Wang NL. Intermediate-term and long-term clinical evaluation of the Ahmed glaucoma valve implantation. Zhonghua Yan Ke Za Zhi. 2005;41(9):796–802. [PubMed] [Google Scholar]
- 27.Topouzis F, Coleman AL, Choplin N, Bethlem MM, Hill R, Yu F, Panek WC, Wilson MR. Follow-up of the original cohort with the Ahmed glaucoma valve implant. Am J Ophthalmol. 1999;128(2):198–204. doi: 10.1016/s0002-9394(99)00080-x. [DOI] [PubMed] [Google Scholar]
- 28.Ayyala RS, Zurakowski D, Smith JA, Monshizadeh R, Netland PA, Richards DW, Layden WE. A clinical study of the Ahmed glaucoma valve implant in advanced glaucoma. Ophthalmology. 1998;105(10):1968–1976. doi: 10.1016/S0161-6420(98)91049-1. [DOI] [PubMed] [Google Scholar]
- 29.Gedde SJ, Scott IU, Tabandeh H, Luu KK, Budenz DL, Greenfield DS, Flynn HW., Jr Late endophthalmitis associated with glaucoma drainage implants. Ophthalmology. 2001;108(7):1323–1327. doi: 10.1016/s0161-6420(01)00598-x. [DOI] [PubMed] [Google Scholar]
- 30.Alvarado JA, Hollander DA, Juster RP, Lee LC. Ahmed valve implantation with adjunctive mitomycin C and 5-fluorouracil: long-term outcomes. Am J Ophthalmol. 2008;146(2):276–284. doi: 10.1016/j.ajo.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 31.Chen A, Yu F, Law SK, Giaconi JA, Coleman AL, Caprioli J. Valved glaucoma drainage devices in pediatric glaucoma: retrospective long-term outcomes. JAMA Ophthalmol. 2015;133(9):1030–1035. doi: 10.1001/jamaophthalmol.2015.1856. [DOI] [PubMed] [Google Scholar]
- 32.AlHadlaq A, AlMalki S, AlShahwan S. Late onset endophthalmitis associated with unexposed glaucoma valved drainage device. Saudi J Ophthalmol. 2016;30(2):125–127. doi: 10.1016/j.sjopt.2015.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Al-Torbak AA, Al-Shahwan S, Al-Jadaan I, Al-Hommadi A, Edward DP. Endophthalmitis associated with the Ahmed glaucoma valve implant. Br J Ophthalmol. 2005;89(4):454–458. doi: 10.1136/bjo.2004.049015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rao A, Wallang B, Padhy TR, Mittal R, Sharma S. Dual infection by streptococcus and atypical mycobacteria following Ahmed glaucoma valve surgery. Semin Ophthalmol. 2013;28(4):233–235. doi: 10.3109/08820538.2012.760621. [DOI] [PubMed] [Google Scholar]