Abstract
AIM
To assess visual quality after presbyopia correction using an aspheric ablation profile and a micro-monovision protocol.
METHODS
This is a retrospective interventional study. Fifty-four eyes of 27 patients (mean age, 50.2±7.5y) who underwent presbyopia correction with an aspheric micro-monovision protocol were enrolled. The values of modulation transfer function (MTF) cutoff frequency, Strehl ratio, objective scattering index (OSI) and accommodation range were quantitatively assessed using the HD analyzer. Preoperative and postoperative contrast sensitivity (CS) at far (2.5 m) and near (40 cm) distance and higher-order aberrations (HOAs) were analyzed. Subjective visual satisfaction was evaluated by self-reported questionnaire regarding optical visual symptoms.
RESULTS
One year after presbyopia correction, no significant differences were found in the MTF cutoff frequency, Strehl ratio and OSI, however, the HD analyzer accommodation range significantly differed postoperatively (P=0.004). Postoperative CS at 12 and 18 cpd at near showed statistically significant improvement (P=0.020 and 0.008, respectively). Visual performance by self-reported questionnaire revealed satisfactory results in terms of subjective visual quality improvement.
CONCLUSION
Objective optical quality parameters show good visual outcomes. Subjective visual quality assessed by self-reported questionnaire in the presbyopia correction group show satisfactory results.
Keywords: presbyopia correction, laser blended vision, visual quality, LASIK
INTRODUCTION
Presbyopia is an inability of the eye to focus sharply on nearby objects, resulting from the age-related loss of accommodation[1]. As the prevalence of the presbyopia-affected population continues to grow in an aging society, many kinds of presbyopia correction strategies have been attempted to optically restore near vision. These approaches include genuine restoration of accommodation such as an accommodative intraocular lens (IOL), pseudoaccommodation or increase of depth of focus (DoF) by multifocal IOL, corneal refractive surgery, or small aperture corneal inlay[2]–[10].
Despite a number of different approaches, effective treatment of presbyopia that successfully preserves both distant and near vision is still challenging. Reinstein et al[11]–[13] reported the use of the Laser Blended Vision (LBV; Carl Zeiss Meditec, Jena, Germany) technique, which combines control of spherical aberration (SA) to increase depth of field with micro-monovision [anisometropia of 1.50 diopters (D) in the nondominant eye] irrespective of age, in myopic, hyperopic and emmetropic presbyopia populations. They suggested that this aspheric micro-monovision protocol was well-tolerated, stable, and effective, exceeding the US Food and Drug Administration criteria for treating presbyopic patients[11]–[13].
Since presbyopic patients often have high expectations, particularly those who are not accustomed to wearing glasses, some patients complain of compromised visual function, such as reduced low contrast visual acuity and reduced contrast sensitivity (CS). Therefore, evaluation of visual quality or patient satisfaction after presbyopic correction has become a major concern, although studies have previously demonstrated the objective outcomes of the surgery[5],[14]–[23].
This is the first report to objectively investigate comprehensive visual quality by the HD analyzer (formerly called Optical Quality Analysis System; OQAS, Visiometrics, Terrassa, Spain) as well as visual acuity both at far and near, CS, and higher-order aberrations (HoAs) after presbyopic correction using LBV during a relatively long follow-up period. The purpose of the current study was to objectively evaluate postoperative visual performance after LBV using the HD analyzer and subjectively by self-reported questionnaire.
SUBJECTS AND METHODS
This study enrolled patients consecutively who underwent presbyopia correction with laser in-situ keratomileusis (LASIK)-induced micro-monovision between March 2011 and October 2011 at Samsung Medical Center, Seoul, Korea. Inclusion criteria were as follows: corrected distance visual acuity (CDVA) of 20/25 or better and distance corrected near visual acuity (DCNVA) of J3 or worse in both eyes. All patients were Korean and had no previous ocular surgeries or other laser treatments. Subjects with visually significant cataract or any history of ocular diseases other than presbyopia were excluded. Additional inclusion criteria were a postoperative follow-up period of at least one year and availability of preoperative and postoperative data for distant and near visual acuity, CS, and HoAs. A total of 54 eyes of 27 patients were enrolled in the study group. The HD analyzer has only been available since March 2012 in our clinical setting, so the HD analyzer measurements including modulation transfer function (MTF) cutoff frequency, Strehl ratio, objective scattering index (OSI), and accommodation range were only evaluated postoperatively. The self-reported questionnaire for the assessment of subjective patient satisfaction about visual quality after presbyopia correction was administered 12mo postoperatively, when enrolled patients in the study group performed the HD analyzer.
An age-matched control group with no history of ocular surgery was recruited consecutively from the outpatients who visited our clinics for routine ophthalmologic evaluations. Inclusion criteria were as follows: uncorrected distance visual acuity (UDVA) of 20/25 or better, distance spherical equivalent refraction between -0.5 D to 0.5 D, and a normal eye without cataract, as determined by slit-lamp biomicroscopy and funduscopy. Fifty-four age-matched normal eyes of 27 volunteers without presbyopia were enrolled in the control group, and performed the HD analyzer. The mean patient age was 50.5±5.4y (range, 42-60y). This study was approved by the Institutional Review Board of the Samsung Medical Center and the work was carried out in accordance with the Declaration of Helsinki.
Ophthalmologic Examination at Baseline and Postoperative Follow-up Visits
The medical charts of enrolled patients were reviewed to obtain patient demographics, clinical examination details, procedures, and complications. The preoperative and postoperative information included UDVA and CDVA, and uncorrected near visual acuity (UNVA) and intermediate visual acuity (UIVA) measured by Jaeger chart at the distance of 40 and 80 cm from the eye. The measurements were performed in each eye and binocularly, and converted to a logarithm of the minimal angle of resolution (logMAR). The results of ocular dominancy test, refractive errors including spherical and cylindrical values, and manifest refraction spherical equivalent (MRSE) were reviewed. Regarding measurements of visual quality, preoperative and postoperative CS at 1.5, 3, 6, 12, and 18 cycles per degree (cpd) with a CSV-1000E and CSV-1000-1.5 cpd (VectorVision, Greenville, OH, USA) under photopic conditions with an illumination of 230 lx at far (2.5 m) and near distance (40 cm from the eye), and wavefront assessment for a 6-mm pupil by WASCA (Carl Zeiss Meditec AG, Jena, Germany) aberrometer were analyzed. As the recommended distance of 2.5 m for CSV-1000, the CS measured at near distance was evaluated on a relative scale between groups.
Surgical Procedure of Laser Blended Vision Technique for Presbyopia Correction
All patients in the study group underwent bilateral simultaneous LASIK using the MEL 80 (Carl Zeiss Meditec, Germany) excimer laser and VisuMax (Carl Zeiss Meditec, Germany) femtosecond laser by a skilled surgeon (Chung ES). Presbyopia correction was performed using an aspheric ablation profile and a micro-monovision protocol with an intended postoperative refraction of plano for the dominant eye and in the range of -1.00 to -1.50 D for the non-dominant eye, irrespective of the patient's age. The mean value of target spherical equivalent for the non-dominant eye was -1.44±0.21 D. Proprietary non-linear aspheric ablation profiles were used for all eyes, which incorporated a small amount of SA determined according to the patient's age, preoperative SA, and the amount of refractive correction; the profiles were intended to control the induction of SA to a level that would provide an increased depth of field, but without affecting CS and quality of vision[11]–[13]. The CRS-Master software platform (Carl Zeiss Meditec, Germany) was used to generate the ablation profiles for the MEL 80 excimer laser and flaps were created using the VisuMax femtosecond laser[11]–[13].
Objective and Subjective Optical Quality Measurement
Objective optical quality measured by the HD analyzer included MTF cutoff frequency, Strehl ratio, OSI, and accommodation range one year after LBV presbyopia correction surgery in the study group and age-matched normal control group. The refractive errors of the subjects were corrected during the measurements and the pupil diameter was provided by the device, which was more than 4.0 mm in all eyes.
Accommodation range was assessed through the retinal image quality which was analyzed by the value of point spread function (PSF) when near vision was simulated. The stimulus is presented automatically by the HD analyzer at different distances (from infinity to 10 cm or less if it is need). To put the stimulus at these different distances, the badal system included in the instrument is used. Simulated object distances ranged from -1.00 D (beyond infinity) to +3.00 D (near vision) in 0.5 D increments. Starting with the retinal image quality corresponding to the best focus position, the object distance is considered as successfully resolved if the retinal image quality has not been reduced by more than 50%.
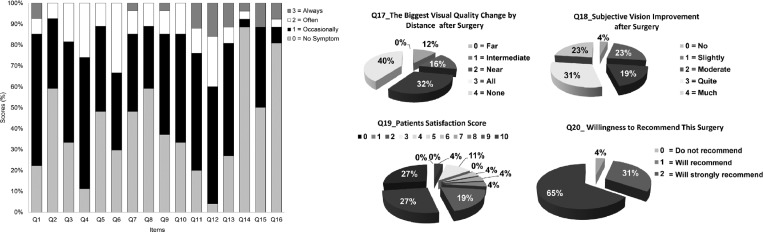
The subjective visual performance was evaluated by self-reported questionnaire. The questionnaire consisted of 20 items. The questionnaire items were described in Table 1.
Table 1. Results of the self-reported questionnaire on subjective visual quality administered 12mo after presbyopia correction using an aspheric ablation profile and a micro-monovision protocol by LBV technique.
| Item | Contents | Scores (%) |
mean±SD (Mode) | Min, max (Median) | |||
| 0 | 1 | 2 | 3 | ||||
| Q1 | Presence of halo | 22.2 | 63 | 7.4 | 7.4 | 1.00±0.78 (1) | 0, 3 (1) |
| Q2 | Presence of headache | 59.3 | 33.3 | 7.4 | 0 | 0.48±0.64 (0) | 0, 2 (0) |
| Q3 | Presence of photo sensitivity | 33.3 | 48.2 | 18.5 | 0 | 0.85±0.72 (1) | 0, 2 (1) |
| Q4 | Presence of dryness | 11.1 | 63 | 25.9 | 0 | 1.15±0.60 (1) | 0, 2 (1) |
| Q5 | Presence of epiphora | 48.1 | 40.8 | 11.1 | 0 | 0.63±0.69 (0) | 0, 2 (1) |
| Q6 | Presence of glare | 29.6 | 37.1 | 33.3 | 0 | 1.04±0.81 (1) | 0, 2 (1) |
| Q7 | Presence of haziness | 48.1 | 37.1 | 11.1 | 3.7 | 0.70±0.82 (0) | 0, 3 (1) |
| Q8 | Presence of diplopia | 59.3 | 29.6 | 11.1 | 0 | 0.52±0.70 (0) | 0, 2 (0) |
| Q9 | Visual fluctuation under photopic conditions | 37 | 48.2 | 11.1 | 3.7 | 0.81±0.79 (1) | 0, 3 (1) |
| Q10 | Visual fluctuation under common environment | 33.3 | 51.9 | 14.8 | 0 | 0.81±0.68 (1) | 0, 2 (1) |
| Q11 | Visual fluctuation under dim conditions | 20 | 56 | 12 | 12 | 1.16±0.90 (1) | 0, 3 (1) |
| Q12 | Night driving difficulty | 4 | 56 | 24 | 16 | 1.52±0.82 (1) | 0, 3 (1) |
| Q13 | Presence of near work disturbance | 26.9 | 53.9 | 7.7 | 11.5 | 1.04±0.92 (1) | 0, 3 (1) |
| Q14 | Need for near-vision glasses | 88.5 | 3.8 | 3.9 | 3.8 | 0.23±0.71 (0) | 0, 3 (0) |
| Q15 | Presence of far work disturbance | 50 | 38.5 | 0 | 11.5 | 0.73±0.96 (0) | 0, 3 (0.5) |
| Q16 | Need for far-vision glasses | 80.8 | 7.7 | 3.8 | 7.7 | 0.38±0.90 (0) | 0, 3 (0) |
| Q17a | The biggest visual quality change by distance after surgery | Presented on the pie chart in Figure 4 | NA (3) | NA | |||
| Q18b | Subjective vision improvement after surgery | 2.46±1.21 (3) | 0, 4 (3) | ||||
| Q19c | Patient satisfaction scale (10) | 7.77±2.52 (10) | 2, 10 (9) | ||||
| Q20d | Willingness to recommend this surgery | NA (2) | 0, 2 (2) | ||||
SD: Standard deviation; NA: The calculation of mean value SD is not applicable. Q: Question; 0: No symptoms, 1: Occasionally, 2: Often, 3: Always. a0: Far, 1: Intermediate, 2: Near, 3: All, 4: None. b0: No, 1: Slightly, 2: Moderate, 3: Quite, 4: Much. cScores from 0 (low satisfaction) to 10 (high satisfaction) by 1-point increment. d0: Do not recommend, 1: Will recommend, 2: Will strongly recommend.
Statistical Analysis
All data were entered into the database using Microsoft Office Excel 2010 (Microsoft Corporation, Redmond, WA, USA), and all statistical analyses were performed using SPSS software version 21 for Windows (SPSS Inc., Chicago, IL, USA). A statistical power estimation and adequate sample size calculation based on the previous data to confirm the difference between presbyopia correction and control group could not be performed because of the exploratory nature of this study. The independent t-test was used to compare the data between the study and control group. The paired t-test was used to compare the data of the study group before and after surgery. The results were expressed as mean±standard deviation (SD), and a value of P<0.05 was considered statistically significant.
RESULTS
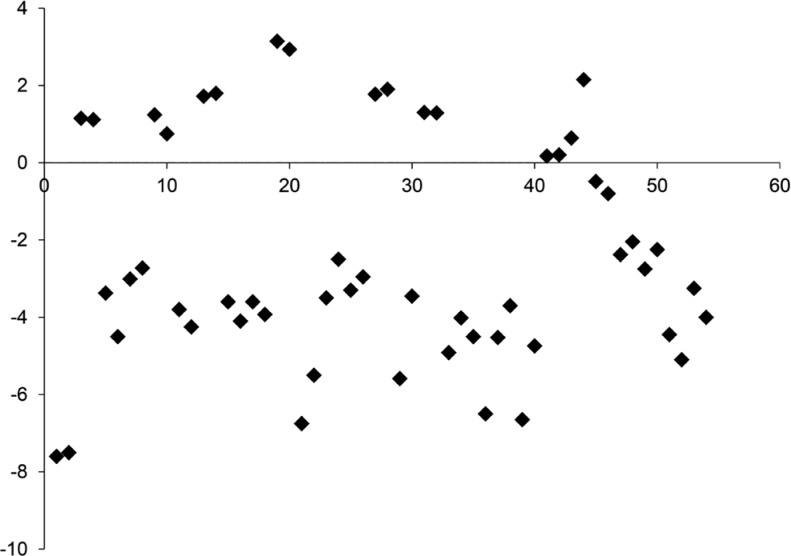
The mean patient age was 50.2±7.5y (range, 40-65y) and the mean follow-up period was 22.26±11.79mo (range, 12 to 30). Preoperatively, all eyes had a CDVA of 20/25 or better, with 85% achieving 20/20 or better. Patient baseline characteristics were listed in Table 2 and the distribution of preoperative spherical equivalent was shown in Figure 1. There were no significant intraoperative or postoperative complications such as flap-associated complications.
Table 2. Baseline characteristics of 54 eyes of 27 patients who underwent presbyopia correction using an aspheric ablation profile and a micro-monovision protocol with the LBV technique.
| Parameters | Mean±SD | Range (min, max) |
| Age (y) | 50.2±7.5 | 40, 65 |
| Follow-up period (mo) | 22.26±11.79 | 12, 30 |
| Sex, M/F (%) | 15 (56)/12 (44) | |
| Dominancy, R/L (%) | 19 (70)/8 (30) | |
| Target SE in the near eye (D) | -1.44±0.21 | -1.50, -1.00 |
| CDVA (logMAR) | 0.01±0.03 | 0.00, 0.10 |
| UDVA (logMAR) | 0.65 ±0.50 | 0.00, 1.70 |
| UNVA (logMAR) | 0.58±0.45 | 0.00, 1.60 |
| UIVA (logMAR) | 0.65±0.48 | 0.00, 2.00 |
| MRSE (D) | -2.39±2.89 | -7.60, 3.15 |
| Spherical refractive error (D) | -2.14±2.91 | -7.50, 3.25 |
| Cylindrical refractive error (D) | -0.52±0.44 | -2.00, 0.00 |
SD: Standard deviation; M: Male; F: Female; R: Right; L: Left; SE: Spherical equivalent; CDVA: Corrected distant visual acuity; logMAR: Logarithm of the minimum angle of resolution; UDVA: Uncorrected distant visual acuity; UNVA: Uncorrected near visual acuity; UIVA: Uncorrected intermediate visual acuity; MRSE: Manifest refraction spherical equivalent; D: Diopters.
Figure 1. Scatter plot for the distribution of preoperative spherical equivalent.
X axis: Number of eyes; Y axis: Preoperative spherical equivalent, diopter (D). The mean preoperative MRSE was -2.39± 2.89 D (range, -7.60 to 3.15), which consisted of 37 myopic (≤-0.5 D), 14 hyperopic (≥0.5 D), and 3 emmetropic (<0.5 and >-0.5 D) eyes. Preoperative sphere ranged from -7.50 to 3.25 D and cylinder ranged from 0 to -2.00 D.
Visual Acuity and Refractive Errors
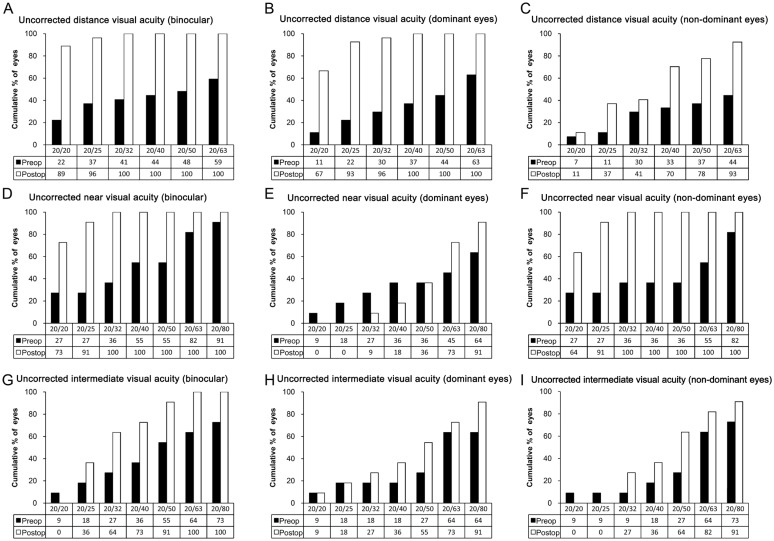
After presbyopia correction, 67% of dominant eyes for far sight achieved a UDVA of 20/20 or better and 93% achieved 20/25 or better. Of non-dominant eyes for near, 11% achieved a UDVA of 20/20 or better, 37% achieved 20/25 or better, and 70% achieved 20/40 or better. Binocularly, 89% of patients achieved a UDVA of 20/20 or better and 96% achieved 20/25 or better. Cumulative histograms of UDVA, UNVA, and UIVA were presented in Figure 2.
Figure 2. Cumulative histograms of uncorrected distance visual acuity (A, B, C), uncorrected near visual acuity (D, E, F), and uncorrected intermediate visual acuity (G, H, I) for binocular vision (A, D, G), dominant eyes (B, E, H), and non-dominant eyes (C, F, I) preoperatively (black bars) and postoperatively (gray bars).
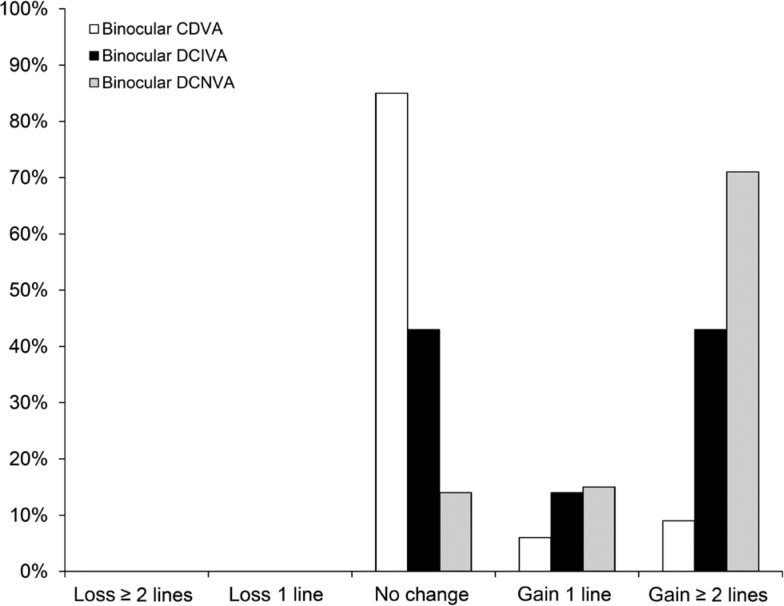
The overall efficacy index (given by mean postoperative UDVA/mean preoperative CDVA) including dominant eyes and non-dominant eyes was 0.76 and the safety index (ratio of postoperative to preoperative CDVA) was 1.02. No eyes lost 1 or more lines of CDVA, 46 eyes retained the same CDVA, 3 eyes gained 1 line of CDVA, and 5 eyes gained 2 lines of CDVA after surgery. Binocular results for lines lost or gained for distance, intermediate and near logMAR visual acuity using distance corrected preoperative values were presented in Figure 3.
Figure 3. Binocular results for lines lost or gained for distance, intermediate and near logMAR visual acuity using distance corrected preoperative values.
CDVA: Corrected distant visual acuity; DCIVA: Distant corrected intermediate visual acuity; DCNVA: Distant corrected near visual acuity.
For refractive errors, there was no statistical difference between dominant and non-dominant eyes in preoperative MRSE, sphere, and cylinder (paired t-test, P>0.05). The difference between preoperative and postoperative MRSE, sphere and cylinder in dominant eyes, and cylinder in non-dominant eyes were statistically significant (paired t-test, P<0.05). However, preoperative and postoperative MRSE and sphere in non-dominant eyes were not significantly different (paired t-test, P=0.068 and 0.106, respectively). The distance, near and intermediate UCVA and refractive errors before and after presbyopic correction treatments were presented for dominant eyes, non-dominant eyes, and binocularly in Table 3.
Table 3. Preoperative and postoperative visual acuity and refractive errors.
| Parameters | Eye | Preoperative | Postoperative | P |
| UDVA (logMAR) | Dominant eye | 0.61±0.50 | 0.05±0.14 | 0.000 |
| Non-dominant eye | 0.70±0.50 | 0.32±0.26 | 0.001 | |
| Binocular | 0.47±0.42 | 0.01±0.05 | 0.000 | |
| UNVA (logMAR) | Dominant eye | 0.65±0.48 | 0.52±0.22 | 0.418 |
| Non-dominant eye | 0.51±0.43 | 0.05±0.07 | 0.003 | |
| Binocular | 0.42±0.42 | 0.04 ±0.07 | 0.008 | |
| UIVA (logMAR) | Dominant eye | 0.68±0.55 | 0.39±0.22 | 0.090 |
| Non-dominant eye | 0.63±0.43 | 0.40±0.17 | 0.070 | |
| Binocular | 0.53±0.45 | 0.25±0.16 | 0.049 | |
| MRSE (D) | Dominant eye | -2.37±2.96 | -0.22±0.73 | 0.001 |
| Non-dominant eye | -2.42±2.89 | -1.36±0.83 | 0.068 | |
| Spherical (D) | Dominant eye | -2.12±3.01 | -0.14±0.69 | 0.002 |
| Non-dominant eye | -2.16±2.87 | -1.22±0.84 | 0.106 | |
| Cylindrical (D) | Dominant eye | -0.51±0.50 | -0.14±0.19 | 0.001 |
| Non-dominant eye | -0.53±0.38 | -0.27±0.28 | 0.006 |
UDVA: Uncorrected distant visual acuity; UNVA: Uncorrected near visual acuity; UIVA: Uncorrected intermediate visual acuity; logMAR: Logarithm of the minimum angle of resolution; MRSE: Manifest refraction spherical equivalent; Spherical: Spherical refractive error; Cylindrical: Cylindrical refractive error; D: Diopters. Paired t-test was used for statistical analysis. P values <0.05 were considered statistically significant.
mean±SD
Higher-order Aberrations
After presbyopia correction using an aspheric ablation profile and a micro-monovision protocol, HoAs in the root mean square (RMS) showed statistically significant increase (paired t-test, P=0.002). More specifically, coma (Z3−1 and Z31) in RMS and SA (Z40) in RMS were significantly different, except for trefoil (Z3−3 and Z33) in RMS (paired t-test, P=0.014, P=0.020 and P=0.223, respectively). Table 4 shows the mean preoperative and postoperative HoAs in detail [presented in standard Optical Society of America (OSA) convention].
Table 4. Changes in higher-order aberrations after presbyopia correction.
| HoAs (µm) | Preoperative | Postoperative | P |
| Oblique trefoil (Z3−3) | 0.037±0.172 | 0.008±0.241 | 0.548 |
| Vertical coma (Z3−1) | 0.006±0.238 | -0.026±0.279 | 0.478 |
| Horizontal coma (Z31) | -0.054±0.267 | -0.108±0.471 | 0.851 |
| Horizontal trefoil (Z33) | 0.218±0.316 | 0.211±0.307 | 0.694 |
| SA (Z40) | 0.149±0.110 | 0.183±0.224 | 0.669 |
| RMS coma | 0.315±0.170 | 0.461±0.309 | 0.014 |
| RMS trefoil | 0.366±0.202 | 0.388±0.209 | 0.223 |
| RMS SA | 0.162±0.089 | 0.240±0.161 | 0.020 |
| RMS HoAs | 0.208±0.070 | 0.269±0.103 | 0.002 |
The values were presented in standard Optical Society of America (OSA) convention. HoAs: Higher-order aberrations; Z: Zernike polynomials; SA: Spherical aberration; RMS: Root mean square. Paired t-test was used for statistical analysis. P values <0.05 were considered statistically significant.
mean±SD
Contrast Sensitivities
The preoperative and postoperative mean CS measured in log units were shown in Table 5. There were no significant differences in the CS through all frequencies at far under photopic conditions before and after surgery. On the other hand, there was a significant improvement at 12 and 18 cpd at near postoperatively compared to preoperative CS (paired t-test, P=0.020 and 0.008, respectively).
Table 5. Changes in binocular contrast sensitivity after presbyopia correction (measured in log units).
| CS (cpd) | Preoperative | Postoperative | P | |
| Fara | 1.5 | 1.601±0.099 | 1.566±0.095 | 0.337 |
| 3 | 1.826±0.113 | 1.781±0.148 | 0.339 | |
| 6 | 1.866±0.156 | 1.863±0.202 | 0.967 | |
| 12 | 1.390±0.294 | 1.426±0.300 | 0.764 | |
| 18 | 0.800±0.312 | 0.855±0.325 | 0.642 | |
| Nearb | 1.5 | 1.470±0.075 | 1.437±0.109 | 0.347 |
| 3 | 1.601±0.120 | 1.649±0.154 | 0.401 | |
| 6 | 1.567±0.050 | 1.697±0.163 | 0.069 | |
| 12 | 1.116±0.136 | 1.313±0.134 | 0.020 | |
| 18 | 0.337±0.158 | 0.729±0.298 | 0.008 | |
aMeasured at 2.5 m; bMeasured at 40 cm; CS: Contrast sensitivity; cpd: Cycle per degree. Paired t-test was used for statistical analysis. P values <0.05 were considered statistically significant.
mean±SD
The HD analyzer (Optical Quality Analysis System) Measurements
The objective optical quality parameters measured by the HD analyzer were compared between the presbyopia correction group and the age-matched normal control group. There were no significant differences in terms of patient age (P=0.981), sex (P=0.343), MRSE (P=0.551), sphere (P=0.304), cylinder (P=0.968), or logMAR CDVA (P=0. 937) between the two groups.
Table 6 showed the HD analyzer measurements in the presbyopia correction group and the normal control group. The mean MTF cutoff frequency, Strehl ratio, OSI did not show significant differences between two groups. However, the HD analyzer accommodation range was statistically significantly increased after the presbyopia correction compared to the control groups (P=0.004, independent t-test).
Table 6. Comparison of quantitative visual quality using the HD analyzer (OQAS) between the presbyopia correction group and the normal control group.
| OQAS measurements | Presbyopia correction group | Normal control group | P |
| MTF cutoff frequency (cpd) | 37.152±8.018 (17.101-54.91) | 36.467±9.977 (19.005-54.731) | 0.551 |
| Strehl ratio | 0.186±0.040 (0.1-0.271) | 0.198±0.063 (0.095-0.399) | 0.466 |
| OSI | 1.026±0.473 (0.3-2.2) | 1.007±0.789 (0.2-3.3) | 0.202 |
| Accommodation, range (D) | 1.182±0.305 (0.344-1.854) | 0.984±0.254 (0.357-1.542) | 0.004 |
OQAS: Optical quality analysis system; MTF: Modulation transfer function; cpd: Cycle per degree; OSI: Objective scattering index; D: Diopters. Independent t-test was used for statistical analysis. P values <0.05 were considered statistically significant.
mean±SD (range)
Self-reported Questionnaire about Subjective Visual Performance
Among questions 1 to 16, the most frequent value was 1 in 9 questions and 0 in 7 questions. Most of the patients experienced occasional visual discomfort such as halo, headache, photo sensitivity, dryness, etc.; however, the severity and frequency were not high. Patients responded that they experienced visual quality change at all distances including far, intermediate, and near after presbyopia correction surgery (Q17), and quite subjective vision improvement after presbyopia surgery (Q18). In Q19, the mean value of patients' satisfaction scale was 7.77±2.52 (range 2 to 10), and the most frequent value was the highest score of 10. Ninety six percent of the patients replied that they will recommend the presbyopic surgery to others (Q20). The distribution of scores, and mean, mode, and median values of each question in the self-reported questionnaire on a subjective visual quality were shown in Table 1 and Figure 4.
Figure 4. Results of the self-reported questionnaire on subjective visual quality administered 12mo after presbyopia correction using an aspheric ablation profile and a micro-monovision protocol with the LBV technique.
DISCUSSION
In our study, optical quality was measured objectively using the HD analyzer. We found that no significant differences in the optical quality parameters, including the MTF cutoff frequency, Strehl ratio, or OSI, between the presbyopia treatment group and the normal control group. These results indicated that the optical quality was basically equivalent to that of normal eyes, which were adjusted for age. Equivalence of the optical quality to age-matched eyes suggests that the procedure has not detrimentally affected optical quality of the treated eyes[24]–[31].
With regard to accommodative range, the treatment group showed significantly better result compared to the normal control group. However, comparison of the change in accommodation found with the HD analyzer to the improvement in intermediate and near visual acuity for the treated eyes did not show causative relationship. The patients had a 4 line increase in near acuity and a 3-line increase in intermediate acuity. It can be postulated that since the device is generating simulated visual acuity from the retinal image only and does not consider the monocular benefits of vision that the visual cortex provides or the impact of binocular summation.
We also investigated subjective visual quality after presbyopia correction by conducting a patient satisfaction survey. Improvement of accommodative range was supported by a questionnaire elucidating subjective postoperative visual performance. According to the questionnaire on subjective visual quality, patients experienced definite visual improvement at near distance after surgery. About 25% of the patients responded that they did not experience any disturbance of near vision, and over 50% of the patients experienced discomfort only occasionally (Q13; Table 1). Approximately 90% of patients did not require glasses for near vision at all (Q14; Table 1).
Over the last decade, patient-reported outcome instruments or questionnaires have rapidly gained importance as outcome measures in clinical research[32]. In a previous study, Luo et al[23] reported that presbyopia corrected with glasses is associated with a nominal decrease in quality of life similar to that of treated hypertension, and approximately 10% of such patients may be candidates for presbyopia correction. In other words, presbyopia patients have high expectations for visual quality, since they have had little experience in visual disturbance during their earlier lives. Therefore, a number of presbyopia correction strategies have been introduced. Surgical strategies for dealing with presbyopia may be extraocular (corneal or scleral) or intraocular (removal and replacement of the crystalline lens or some type of treatment on the crystalline lens itself)[33]. Studies have reported success rates ranging from 80%-98% for monovision post laser vision correction (LVC), 91% for monovision after cataract surgery and 95% following clear lens extraction with good satisfaction[33]. In the present study, the overall satisfaction level was quite high. A very impressive aspect was that in Q19 the most frequent score among patients was 10, which is the highest possible score. Fifteen percent of subjects showed a satisfaction score of 3 or less following surgery (Q19), but only 4% did not recommend the surgery (Q20). This would reflect the character of presbyopic patients who usually have higher expectations for treatments. In our study, the proportion of patients who always need near glasses and do not recommend surgery were the same as 4%. This is comparable results compared to previous studies.
There were several limitations in the present study, including its design and small sample size. Owing to the retrospective nature of the study, the follow-up period and the intervals between each visit or examination varied among cases, and the different follow-up period may affect the postoperative refractive outcomes. Unfortunately, we did not have the controls answered the relevant survey questions. Controls for the survey would have shown some perspective to the results gathered. Furthermore, it would be an interesting study to investigate the correlation of survey questions scores to relevant clinical measures for other presbyopia correction procedures. Lastly, the questionnaire used to evaluate patient vision performance subjectively was not certified according to global standards for quality, such as the Ocular Surface Disease Index (OSDI). We received consultation about content development, the response scale, and measurement precision; however, we did not perform validity or reliability testing. Therefore, we were only able to determine the overall trend of subjective patient satisfaction. If the quality of the questionnaire were to be verified, the evaluation would be more meaningful.
In conclusion, the present study showed good visual outcomes with satisfactory optical quality objectively evaluated by the HD analyzer and subjectively assessed by self-reported questionnaire after LBV treatment using an aspheric ablation profile and a micro-monovision protocol.
Acknowledgments
Conflicts of Interest: Lim DH, None; Chung ES, None; Kim MJ, None; Chung TY, None.
References
- 1.Koretz JF, Cook CA, Kaufman PL. Accommodation and presbyopia in the human eye. Changes in the anterior segment and crystalline lens with focus. Invest Ophthalmol Vis Sci. 1997;38(3):569–578. [PubMed] [Google Scholar]
- 2.Davison JA, Simpson MJ. History and development of the apodized diffractive intraocular lens. J Cataract Refract Surg. 2006;32(5):849–858. doi: 10.1016/j.jcrs.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 3.Kim MJ, Zheleznyak L, Macrae S, Tchah H, Yoon G. Objective evaluation of through-focus optical performance of presbyopia-correcting intraocular lenses using an optical bench system. J Cataract Refract Surg. 2011;37(7):1305–1312. doi: 10.1016/j.jcrs.2011.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bellucci R. Multifocal intraocular lenses. Curr Opin Ophthalmol. 2005;16(1):33–37. doi: 10.1097/00055735-200502000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Alio JL, Chaubard JJ, Caliz A, Sala E, Patel S. Correction of presbyopia by technovision central multifocal LASIK (presbyLASIK) J Refract Surg. 2006;22(5):453–460. doi: 10.3928/1081-597X-20060501-06. [DOI] [PubMed] [Google Scholar]
- 6.Epstein RL, Gurgos MA. Presbyopia treatment by monocular peripheral presbyLASIK. J Refract Surg. 2009;25(6):516–523. doi: 10.3928/1081597X-20090512-05. [DOI] [PubMed] [Google Scholar]
- 7.Waring GO. Correction of presbyopia with a small aperture corneal inlay. J Refract Surg. 2011;27(11):842–845. doi: 10.3928/1081597X-20111005-04. [DOI] [PubMed] [Google Scholar]
- 8.Tabernero J, Schwarz C, Fernandez EJ, Artal P. Binocular visual simulation of a corneal inlay to increase depth of focus. Invest Ophthalmol Vis Sci. 2011;52(8):5273–5277. doi: 10.1167/iovs.10-6436. [DOI] [PubMed] [Google Scholar]
- 9.Seyeddain O, Hohensinn M, Riha W, Nix G, Rückl T, Grabner G, Dexl AK. Small-aperture corneal inlay for the correction of presbyopia: 3-year follow-up. J Cataract Refract Surg. 2012;38(1):35–45. doi: 10.1016/j.jcrs.2011.07.027. [DOI] [PubMed] [Google Scholar]
- 10.Lim DH, Han JC, Kim MH, Chung ES, Chung TY. Factors affecting near vision after monofocal intraocular lens implantation. J Refract Surg. 2013;29(3):200–204. doi: 10.3928/1081597X-20130129-06. [DOI] [PubMed] [Google Scholar]
- 11.Reinstein DZ, Archer TJ, Gobbe M. LASIK for myopic astigmatism and presbyopia using non-linear aspheric micro-monovision with the Carl Zeiss Meditec MEL 80 platform. J Refract Surg. 2011;27(1):23–37. doi: 10.3928/1081597X-20100212-04. [DOI] [PubMed] [Google Scholar]
- 12.Reinstein DZ, Carp GI, Archer TJ, Gobbe M. LASIK for presbyopia correction in emmetropic patients using aspheric ablation profiles and a micro-monovision protocol with the Carl Zeiss Meditec MEL 80 and VisuMax. J Refract Surg. 2012;28(8):531–541. doi: 10.3928/1081597X-20120723-01. [DOI] [PubMed] [Google Scholar]
- 13.Reinstein DZ, Couch DG, Archer TJ. LASIK for Hyperopic astigmatism and presbyopia using micro-monovision with the Carl Zeiss Meditec MEL80 Platform. J Refract Surg. 2009;25(1):37–58. doi: 10.3928/1081597X-20090101-07. [DOI] [PubMed] [Google Scholar]
- 14.Vandermeer G, Rio D, Gicquel JJ, Pisella PJ, Legras R. Subjective through-focus quality of vision with various versions of modified monovision. Br J Ophthalmol. 2015;99(7):997–1003. doi: 10.1136/bjophthalmol-2014-305437. [DOI] [PubMed] [Google Scholar]
- 15.Jackson WB, Tuan KM, Mintsioulis G. Aspheric wavefront-guided LASIK to treat hyperopic presbyopia: 12-month results with the VISX platform. J Refract Surg. 2011;27(7):519–529. doi: 10.3928/1081597X-20101110-02. [DOI] [PubMed] [Google Scholar]
- 16.Alarcón A, Anera RG, Villa C, Jiménez del Barco L, Gutierrez R. Visual quality after monovision correction by laser in situ keratomileusis in presbyopic patients. J Cataract Refract Surg. 2011;37(9):1629–1635. doi: 10.1016/j.jcrs.2011.03.042. [DOI] [PubMed] [Google Scholar]
- 17.Gifford P, Kang P, Swarbrick H, Versace P. Changes to corneal aberrations and vision after PresbyLASIK refractive surgery using the MEL 80 platform. J Refract Surg. 2014;30(9):598–603. doi: 10.3928/1081597X-20140709-01. [DOI] [PubMed] [Google Scholar]
- 18.Zheleznyak L, Sabesan R, Oh JS, MacRae S, Yoon G. Modified monovision with spherical aberration to improve presbyopic through-focus visual performance. Invest Ophthalmol Vis Sci. 2013;54(5):3157–3165. doi: 10.1167/iovs.12-11050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pallikaris IG, Panagopoulou SI. PresbyLASIK approach for the correction of presbyopia. Curr Opin Ophthalmol. 2015;26(4):265–272. doi: 10.1097/ICU.0000000000000162. [DOI] [PubMed] [Google Scholar]
- 20.Pinelli R, Ortiz D, Simonetto A, Bacchi C, Sala E, Alió JL. Correction of presbyopia in hyperopia with a center-distance, paracentral-near technique using the Technolas 217z platform. J Refract Surg. 2008;24(5):494–500. doi: 10.3928/1081597X-20080501-07. [DOI] [PubMed] [Google Scholar]
- 21.Levinger E, Trivizki O, Pokroy R, Levartovsky S, Sholohov G, Levinger S. Monovision surgery in myopic presbyopes: visual function and satisfaction. Optom Vis Sci. 2013;90(10):1902–1907. doi: 10.1097/OPX.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 22.Dexl AK, Seyeddain O, Riha W, Rückl T, Bachernegg A, Emesz M, Ruckhofer J, Grabner G. Reading performance and patient satisfaction after corneal inlay implantation for presbyopia correction: two-year follow-up. J Cataract Refract Surg. 2012;38(10):1808–1816. doi: 10.1016/j.jcrs.2012.06.047. [DOI] [PubMed] [Google Scholar]
- 23.Luo BP, Brown GC, Luo SC, Brown MM. The quality of life associated with presbyopia. Am J Ophthalmol. 2008;145(4):618–622. doi: 10.1016/j.ajo.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 24.Guell JL, Pujol J, Arjona M, Diaz-Douton F, Artal P. Optical Quality Analysis System; Instrument for objective clinical evaluation of ocular optical quality. J Cataract Refract Surg. 2004;30(7):1598–1599. doi: 10.1016/j.jcrs.2004.04.031. [DOI] [PubMed] [Google Scholar]
- 25.Vilaseca M, Padilla A, Pujol J, Ondategui JC, Artal P, Güell JL. Optical quality one month after Verisyse and Veriflex phakic IOL implantation and Zeiss MEL 80 LASIK for myopia from 5.00 to 16.50 diopters. J Refract Surg. 2009;25(8):689–698. doi: 10.3928/1081597X-20090707-03. [DOI] [PubMed] [Google Scholar]
- 26.Martinez-Roda JA, Vilaseca M, Ondategui JC, Giner A, Burgos FJ, Cardona G, Pujol J. Optical quality and intraocular scattering in a healthy young population. Clin Exp Optom. 2011;94(2):223–229. doi: 10.1111/j.1444-0938.2010.00535.x. [DOI] [PubMed] [Google Scholar]
- 27.Logean E, Dalimier E, Dainty C. Measured double-pass intensity point-spread function after adaptive optics correction of ocular aberrations. Opt Express. 2008;16(22):17348–17357. doi: 10.1364/oe.16.017348. [DOI] [PubMed] [Google Scholar]
- 28.Saad A, Saab M, Gatinel D. Repeatability of measurements with a double-pass system. J Cataract Refract Surg. 2010;36(1):28–33. doi: 10.1016/j.jcrs.2009.07.033. [DOI] [PubMed] [Google Scholar]
- 29.Ondategui JC, Vilaseca M, Arjona M, Montasell A, Cardona G, Güell JL, Pujol J. Optical quality after myopic photorefractive keratectomy and laser in situ keratomileusis: comparison using a double-pass system. J Cataract Refract Surg. 2012;38(1):16–27. doi: 10.1016/j.jcrs.2011.07.037. [DOI] [PubMed] [Google Scholar]
- 30.Alio JL, Schimchak P, Montes-Mico R, Galal A. Retinal image quality after microincision intraocular lens implantation. J Cataract Refract Surg. 2005;31(8):1557–1560. doi: 10.1016/j.jcrs.2005.01.026. [DOI] [PubMed] [Google Scholar]
- 31.Fernandez-Vega L, Madrid-Costa D, Alfonso JF, Montes-Mico R, Poo-Lopez A. Optical and visual performance of diffractive intraocular lens implantation after myopic laser in situ keratomileusis. J Cataract Refract Surg. 2009;35(5):825–832. doi: 10.1016/j.jcrs.2008.12.040. [DOI] [PubMed] [Google Scholar]
- 32.Khadka J, McAlinden C, Pesudovs K. Quality assessment of ophthalmic questionnaires: review and recommendations. Optom Vis Sci. 2013;90(8):720–744. doi: 10.1097/OPX.0000000000000001. [DOI] [PubMed] [Google Scholar]
- 33.Gil-Cazorla R, Shah S, Naroo SA. A review of the surgical options for the correction of presbyopia. Br J Ophthalmol. 2016;100(1):62–70. doi: 10.1136/bjophthalmol-2015-306663. [DOI] [PubMed] [Google Scholar]