Dear Editor,
I'm Dr. Qing-Huai Liu from Department of Ophthalmology, the First Affiliated Hospital of Nanjing Medical University, Nanjing, China. I write to present four cases diagnosed with the intraocular foreign body (IOFB) at or near the ciliary body and to evaluate the effect of extracting IOFB with scleral indentation in direct visualization.
The IOFB generally yields a poor prognosis because it may cause endophthalmitis, or the IOFB itself may lead to ocular siderosis and chalcosis because of metal properties. The occurrence of IOFB at or near the ciliary body constitute about 5% of all IOFB cases[1]–[2]. Because of its anatomical particularity, foreign bodies at or near the ciliary body seems hard to be diagnosed in clinic[3]. Since the IOFB can be followed with serious ocular complications such as secondary glaucoma and retinal toxicity[4], the early diagnosis and removal of the IOFB is strongly recommended[5].
Here we reported four patients who were diagnosed with the IOFB at or near the ciliary body. Each of the middle-aged men reported here got a visible corneal wound and a relatively quiet anterior chamber and vitreous. Different levels of cataract were observed. Foreign bodies were precisely localized and their sizes were carefully evaluated by physical examination, slit-lamp examination (Figure 1A), computerized tomography (CT, Figure 2A-2C), and ultrasound bio-microscopy (Figure 2D). A- and B-scan ultrasound were also applied to confirm the location of the IOFB and the intactness of chorio-retinal profile. Briefly, pupil was dilated and retrobulbar block was performed preoperatively. After routine phacoemulsification, the remnant posterior capsular was removed via posterior continuous curvilinear capsulorhexis (PCCC). Upon completion of PCCC, a 2.5 mm chalazion curette was used to lift up the sclera around the foreign body, whose location had been established before operation (Figure 3A). By adjusting the eye position and microscope focus to clear exposure of the ciliary body and ora serrata, foreign body was discovered prior to the ora serrata (Figure 3B). Once vitreous proliferation or peripheral retina traction was confirmed absent, the IOFB forceps was applied to reach the foreign body through the primary cornea incision and the anterior and posterior capsular opening (Figure 3C). With the chalazion curette jacking outside the sclera as a depressor, foreign body was then removed directly. A foldable intraocular lens was inserted into the capsular bag one month postoperatively. Postoperative best corrected visual acuity (BCVA), intraocular pressure (IOP) and condition of posterior segment were evaluated.
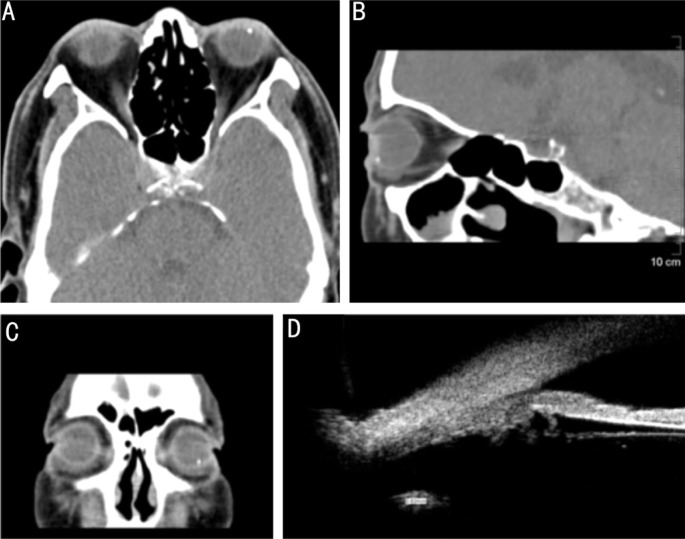
Figure 1. Slit-lamp examination of before and after surgery (patient No.4).
A: Relatively quiet anterior chamber and vitreous before surgery, visible corneal wound at about 12 o'clock with local lens opacity (white arrow); B: Anterior segment status after the IOFB extraction following intraocular lens implantation and drainage valve implantation (white arrow, the drainage tube).
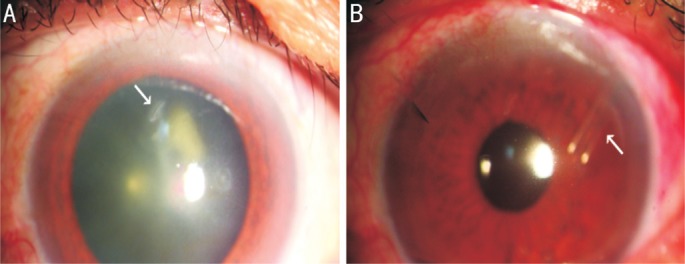
Figure 2. Confirmation of the IOFB location before surgery (patient No.4).
A-C: Coronal and sagittal position of CT-scan, the IOFB located at pars plana of ciliary; D: Ultrasound biomicroscopy (UBM)-scan showed a 0.82 mm foreign body at pars plana of ciliary, with no adhesion to surrounding tissues.
Figure 3. Scleral indentation technique applied in the IOFB removal (patient No.4).
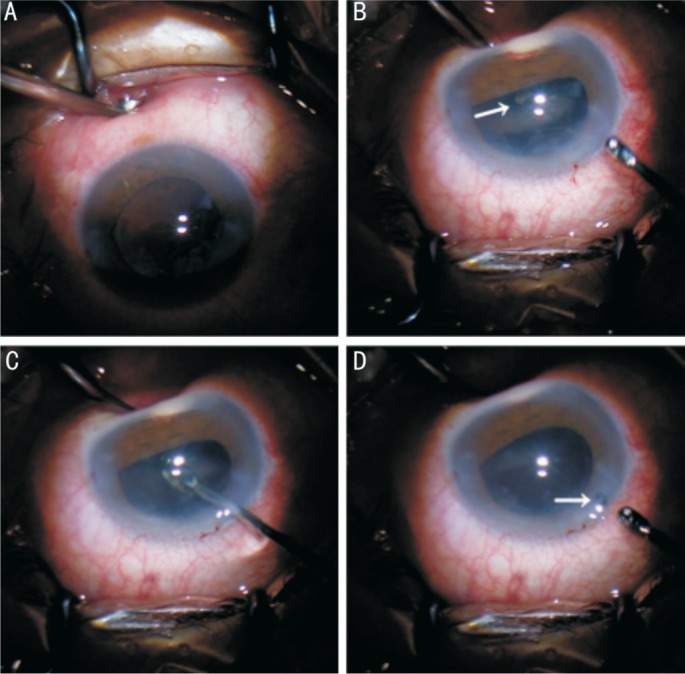
A: Outside force to lift up the sclera around the IOFB with a chalazion curette; B: The IOFB and ciliary body in direct visualization using scleral indentation technique (white arrow, foreign body); C: Reaching the foreign body directly through the primary cornea incision and the anterior and posterior capsular opening with an IOFB forceps; D: The IOFB falling in the cornea incision when removing (white arrow, foreign body).
The general conditions of the four patients were concluded in Table 1. The average surgery time of the four cases were 19.5min. The postoperative follow-up periods ranged from 3 to 48mo. Visual acuity in three patients improved to equal or better than 0.6. Retinal detachment or obvious intravitreous proliferation and inflammation were absent during the long follow-up. High IOP existed in patient No.4 with no release by medication and normal IOP was achieved after implantation of the drainage valve.
Table 1. Clinical features of the four IOFB patients.
| Parameters | No.1 | No.2 | No.3 | No.4 |
| Age (y) | 47 | 33 | 55 | 62 |
| Gender | M | M | M | M |
| Eye type | OS | OS | OS | OS |
| Trauma | Scrap iron | Scrap iron | Iron | NA |
| Injury time | NA | 4d | 2d | NA |
| Cataract | Exist | Exist | Exist | Exist |
| Size of IOFB (mm) | 0.6×0.3 | 2.0×2.4 | 2.0×0. 6 | 1.0×1.2 |
| Property | Magnetic | Magnetic | Magnetic | Non-magnetic |
| Operative time (min) | 25 | 20 | 18 | 15 |
| Retinal detachment | No | No | No | No |
| BCVA before surgery | 0.6 | Hand motion | 0.3 | 0.6 |
| BCVA after surgery | 1.0 | 0.6 | 0.8 | 0.6 |
| IOP before surgery (mm Hg) | 42.9 | 20 | 19 | 46.8 |
| IOP after surgery (mm Hg) | 12.9 | 13.5 | 15.2 | 14.4 |
| Postoperative complications | No | No | No | High IOP; normal IOP after drainage valve implantation |
NA: Not available; IOFB: Intraocular foreign body; BCVA: Best corrected visual acuity; IOP: Intraocular pressure.
Scleral indentation is typically used for thorough removal of peripheral vitreous. This procedure enables the pars plana and process of ciliary body visible, which then enlightens us to use scleral indentation to facilitate the extraction of IOFB at or near the ciliary body. Although scleral indentation is not a novel surgical method, it has not been reported being used in the removal of the IOFB. As for the choice of surgical management of IOFB at or near the ciliary body, there is still no standard procedure. Vitrectomy via pars plana vitrectomy (PPV) is known as the standard method for the management of the IOFB, especially for those remains in vitreous cavity and retinal region[6]–[7]. For those at or near the ciliary body, PPV complications cannot be completely avoided[8], and it had been criticized lately for causing more complications compared to vitrectomy. For more restrictive terms, the IOFB must be magnetic, accurately localized with a size neither too small nor too big. With complex equipment, poor stereoscopic view and long learning curve, ophthalmic endoscope is also not a good choice for the removal of the IOFB. At present, scleral indentation has been applied in PPV, aiming to excision of peripheral vitreous. When executing scleral indentation, the ciliary body and even the ora serrata can be observed through dilated pupil[9]. Basing on this technology, we applied it in our extraction of the IOFB at or near the ciliary body. With the help of deep scleral indentation, the IOFB could be easily exposed and surgical management of the IOFB seemed much easier, which allowed direct visualization and extraction. Furthermore, shorter operative time, free of auxiliary equipments, shorter learning curve for operators and quicker recovery, less cost for patients make it more feasible in clinic.
Before the removal, sagittal CT can be applied to distinguish the foreign bodies from crystalline lens and ciliary body approximately and ultrasound biomicroscopy (UBM)-scan can present accurate localization. However, though surgeons can complete the procedures with no other special equipments, equipments for vitreous surgery are still needed in case. The IOFB with a distance less than 2 mm prior to ora serrate is not fully suitable for this surgery, for surgeries in this area may affect retina potentially and as a consequence, causing retinal traction or retinal tear. If the IOFB turns out to be behind ora serrate and vitreous retraction appeared during operation, PPV then is required.
In summary, the main purpose of this study is to provide the application of scleral indentation in the removal of IOFB at or near the ciliary body. With appropriate entrants, this procedure will yield efficient surgical outcome with less surgical time and quicker recovery.
Acknowledgments
Conflicts of Interest: Ji JD, None; Ding YZ, None; Hu ZZ, None; Xie P, None; Yuan ST, None; Liu QH, None.
REFERENCES
- 1.Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies: a review. Surv Ophthalmol. 2016;61(5):582–596. doi: 10.1016/j.survophthal.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Zhang Y, Zhang M, Jiang C, Qiu HY. Intraocular foreign bodies in china: clinical characteristics, prognostic factors, and visual outcomes in 1,421 eyes. Am J Ophthalmol. 2011;152(1):66–73.e1. doi: 10.1016/j.ajo.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 3.Luo Z, Gardiner M. The incidence of intraocular foreign bodies and other intraocular findings in patients with corneal metal foreign bodies. Ophthalmology. 2010;117(11):2218–2221. doi: 10.1016/j.ophtha.2010.02.034. [DOI] [PubMed] [Google Scholar]
- 4.Ding J, Yoganathan P, Fernando-Sieminski S. Resolution of siderosis glaucoma from chronic intraocular foreign body without glaucoma surgery. Can J Ophthalmol. 2015;50(5):e82–e85. doi: 10.1016/j.jcjo.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 5.Imrie FR, Cox A, Foot B, Macewen CJ. Surveillance of intraocular foreign bodies in the UK. Eye (Lond) 2008;22(9):1141–1147. doi: 10.1038/sj.eye.6702868. [DOI] [PubMed] [Google Scholar]
- 6.Nicoara SD, Irimescu I, Calinici T, Cristian C. Intraocular foreign bodies extracted by pars plana vitrectomy: clinical characteristics, management, outcomes and prognostic factors. BMC Ophthalmol. 2015;15:151. doi: 10.1186/s12886-015-0128-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yuksel K, Celik U, Alagoz C, Dundar H, Celik B, Yazici AT. 23 gauge pars plana vitrectomy for the removal of retained intraocular foreign bodies. BMC Ophthalmol. 2015;15:75. doi: 10.1186/s12886-015-0067-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang X, Li QY, Du S, Ren H, Jia CY, Tang XH. Extraction of intraocular foreign body at or near the ciliary body under endoscopic vitrectomy. Zhonghua Yan Ke Za Zhi. 2013;49(8):691–695. [PubMed] [Google Scholar]
- 9.Sharma YR, Singh DV, Azad RV, Chandra P, Pal N. Iris intraocular foreign bodies: safe and successful removal through limbus. Indian J Ophthalmol. 2006;54(2):125–126. doi: 10.4103/0301-4738.25837. [DOI] [PubMed] [Google Scholar]