Abstract
Background and Objectives
Neurologic intolerance (NI) is defined as the occurrence of neurological symptoms during carotid artery stenting (CAS). Because NI is inevitable problem, it may be helpful to anticipate its occurrence. So, we studied factors associated with NI during proximal protected CAS.
Methods
We retrospectively analyzed all consecutive patients underwent proximal protected CAS from August 2012 to January 2017.
Results
We included total 123 patients (109 males, 72±8 years old). The total procedure time was 43±12 minutes, and mean occlusion time was 4.8±1.2 minutes. We divided CAS patients into 2 groups according to presence of NI; neurologic tolerance (NT; n=74, 60%) and NI (n=49, 40%) groups. After the univariate analysis, symptomatic carotid artery stenosis (p=0.003), absence of anterior communicating artery (p=0.015) and low common carotid artery occlusion pressure (CCAOP, p<0.001) were associated with NI. After the multivariate analysis, NI was significantly associated with symptomatic carotid artery stenosis (odds ratio [OR], 5.549; p=0.014) and systolic CCAOP≤42 mmHg (OR, 6.461; p<0.001). In NI group, 43 patients (88%) recovered right after the balloon deflation and 2 patients were normalized within 2 hours. However, 1 had major stroke and 3 had minor strokes in 4 patients with persistent NI ≥24 hours.
Conclusions
About 40% showed NI during the CAS. Most of them (88%, 43 of 49 patients) recovered after the balloon deflation, but stroke incidence was significantly higher in NI group. Symptomatic carotid artery stenosis and systolic CCAOP ≤42 mmHg were significantly associated with the development of NI during proximal protected CAS.
Keywords: Carotid stenosis, Stent, Neurologic symptoms, Embolic protection devices
INTRODUCTION
Periprocedural events due to microembolization are serious problems that occur while performing carotid artery stenting (CAS) in patients with significant carotid artery stenosis. Embolic protection devices (EPDs) have been developed to prevent these issues, and distal filter devices (DFDs) and proximal protection devices (PPDs) are the most actively used EPDs in these days.1)
Many studies reported that PPDs revealed superior or not inferior embolic protection effects compared with DFDs.2),3),4) However, PPDs temporarily block the cerebral blood flow completely during the procedure, and this may lead to the development of neurologic intolerance (NI), especially in cases with poor collateral flow or contralateral occlusion. This NI may give rise to transient neurologic symptoms (aphasia, contralateral motor weakness, disorientation, mental change, and etc.) when distal cerebral blood flow is inhibited. Usually, NI disappears after the balloon deflation. Although there have been a few evidences whether it was associated with long-term neurologic deficits, it may be helpful to predict the development of NI because it is obvious burden on operators. Thus, we studied to find factors associated with developing NI during proximal protected CAS.
METHODS
Study population
We screened all consecutive patients who had undergone CAS procedures in Chungnam National University Hospital from August 2012 to January 2017, retrospectively. The CAS procedures were done in patients with symptomatic carotid stenosis and asymptomatic carotid stenosis ≥75%. We excluded all patients underwent CAS with DPDs because of following reasons; 1) total occlusion of contralateral carotid arteries, 2) involvement of common carotid artery (CCA), 3) severe proximal tortuosity or difficult aortic arch, 4) immediate and severe intolerance with a PPD which lead to use DFDs, and 5) physician's preference to use DFDs. In addition, patients with insufficient data about the procedure were excluded even in patients who were treated with PPDs. All clinical and procedural characteristics were confirmed by reviewing medical and procedural records. The patients were divided into 2 groups according to the occurrence of NI during CAS procedures; neurologic tolerance (NT) and NI groups.
CAS procedure
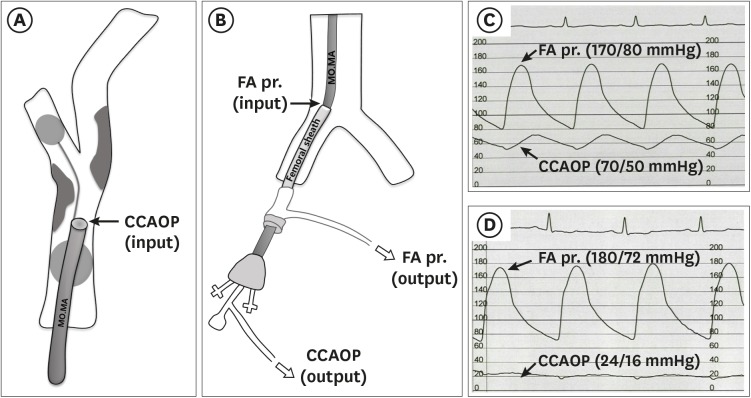
All patients were treated with aspirin (100 mg/day; Boryung Pharmaceutical Company, Seoul, Korea) and clopidogrel (75 mg/day; Bristol-Myers Squibb/Sanofi Pharmaceuticals, Bridgewater, NJ, USA) for at least 3 days before the procedure, and combination therapy with clopidogrel was maintained at least 1 month after the procedure. All procedures were performed percutaneously through the femoral artery. Baseline angiography was performed on the carotid arteries and intracranial vessels of both sides using a 5-Fr Judkins right diagnostic catheter (Cook medical Inc., Bloomington, IN, USA). We checked the presence of anterior communicating artery (ACOM) communication. In cases with invisible ACOM connection, contralateral carotid angiogram while compressing ipsilateral CCA manually was performed to find ACOM connection (compression test). After the angiographic confirmation of the carotid target lesion stenosis, conventional heparin was intravenously injected at 100 IU/kg. We inserted a 0.035-inch soft guidewire into the distal part of the external carotid artery (ECA), and a 5-Fr Judkins catheter was advanced in the ECA. After the stabilizing the diagnostic catheter in the distal ECA, a 0.035-inch Amplatzer Extra stiff guidewire was changed instead of the soft guidewire. A 5-Fr sheath was replaced by a 9-Fr standard sheath and systemic arterial blood pressure was monitored during the procedures using this sheath. The MO.MA device (MO.MA Ultra®; Medtronic, Minneapolis, MN, USA) was positioned via a 9-Fr standard sheath in the CCA with the single marker of the distal balloon located in the ECA, aiming at fully occluding all side branches including superior thyroid artery. All devices, balloons for pre- and post-dilatation and stent, for CAS should be prepared on the table before the ECA occlusion. The distal ECA balloon was inflated, and then the ECA occlusion was confirmed by small contrast injection. The proximal CCA balloon was inflated. We recorded pressures in both femoral artery and common carotid artery occlusion pressure (CCAOP) simultaneously. CCAOP was measured immediately after expansion of the proximal balloon of the MO.MA catheter after the insertion into the CCA (Figure 1A and B). Femoral arterial pressure was measured by the blood pressure measured from the distal aorta through a 25-cm-long sheath inserted into the femoral artery (Figure 1B). These 2 pressures were monitored throughout the procedure (Figure 1C and D). A 0.014-inch guide wire was advanced through the lesion and positioned in the distal internal carotid artery and pre-dilatation, stent deployment, and post-dilatation were performed as soon as possible. After the stent deployment, aspiration of 60 mL of blood was performed through the guiding catheter, and if no debris was found in the last basket, the occlusion balloons were deflated. An additional 20 mL of blood aspiration was performed if debris was found in the last basket. The final angiography included ipsilateral biplanar carotid and intracranial views were obtained to exclude cerebral embolisms.
Figure 1.
Graphic illustration and case examples of the CCAOP measurement. CCAOP was measured immediately after expansion of the proximal balloon of the MO.MA catheter after the insertion into the CCA (A and B). Femoral arterial pressure was measured by the blood pressure measured from the distal aorta through a 25-cm-long sheath inserted into the femoral artery (B). These 2 pressure tracings were monitored throughout the procedure simultaneously. A patient with CCAOP of 70/50 mmHg had no change in consciousness throughout the procedure (C). However, a patient with low CCAOP (24/16 mmHg) and poor pulse pressure had transient NI during the procedure (D).
CCA = common carotid artery; CCAOP = common carotid artery occlusion pressure; FA pr. = femoral artery pressure; NI = neurologic intolerance.
A neurologist observed all the procedures and continuously evaluated the neurological state of patients before and after the procedures. Diffusion-weighted magnetic resonance imaging (DW-MRI) of brain was performed in all patients except 5 within 24 hours after the procedure.
Definition
Symptomatic carotid stenosis was defined as carotid stenosis with having ipsilateral neurological ischemic events within 6 months before the intervention. Procedural success was defined as residual stenosis ≤30% after the CAS without immediate procedural complications. NI was defined as transient neurologic symptoms during balloon occlusion. Neurological symptoms occurring within 24 hours after the procedure were regarded as periprocedural events. The definition of procedural events was following:
1) Stroke: any of these neurological deficits persisting >24 hours
2) Major stroke: new neurological deficit that persisted for >30 days and increased the National Institute of Health Stroke Scale (NIHSS) by ≥4
3) Minor stroke: neurologic deficit resolved completely within 30 days or did not lead to an impairment in daily activities, NIHSS ≤3
4) Transient ischemic attack (TIA): new neurologic deficit that persisted more than 30 minutes after the procedure but completely improved within 24 hours.
We defined neurologic events as major or minor stroke during the procedure.
Statistical analysis
The data were analyzed using commercial software (SPSS version 22.0; IBM Co., Chicago, IL, USA). Continuous data were presented as the mean ± standard deviation. Categorical variables were described with numbers and percentages, and unless otherwise specified. A Student's t-test was performed for statistical comparison between the nominal measures, while a χ2 test was performed for the categorical data. Threshold for categorization of systolic CCAOP was specified using best cut-off value from receiver operator characteristic (ROC) curve. Binary logistic regression was used in the prediction of NI, and multivariable analysis was performed on parameters that were significant on the univariate analysis. We performed multivariate analysis with 4 variables to prevent overfitting of the model. Statistical significance was assumed at p<0.05.
RESULTS
Clinical characteristics
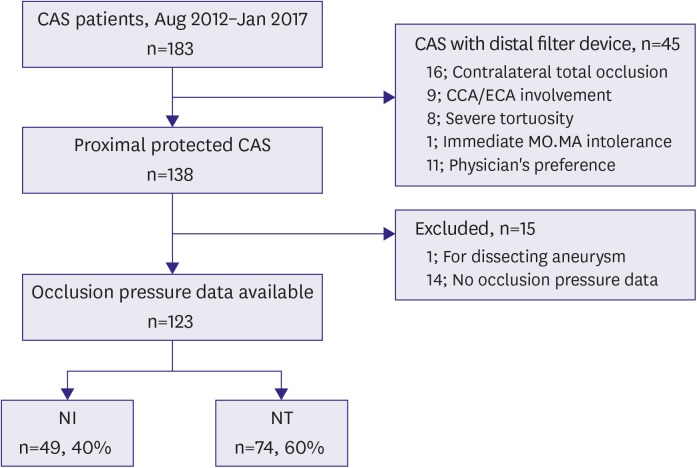
We screened a total of 183 patients underwent CAS from August 2012 to January 2017 (Figure 2). Sixty patients were excluded: 45 patients treated with DFDs, 14 with insufficient pressure data and 1 with dissecting aneurysm. So, we analyzed total 123 patients in this study. Their clinical characteristics were summarized in the Table 1. The mean age was 72±8 years old, 89% were male, and 78% had symptomatic carotid stenosis. Of total 123 patients, 49 patients (40%) had NI during CAS procedures (NI group). Univariate analysis was performed to find the factor that associated with the NI, and the results were expressed together in the Table 1. NI was significantly associated with symptomatic carotid stenosis (odds ratio [OR], 6.915; 95% confidential interval [CI], 1.947–24.560; p=0.003). There were no statistical differences in the presence of underlying diseases such as hypertension, peripheral arterial disease and ischemic heart disease between the 2 groups. The incidence of diabetes mellitus was seemed to be higher in the NI group than in the NT group, but it was statistically insignificant (49% vs. 32%; p=0.067).
Figure 2.
Study scheme.
CAS = carotid artery stenting; CCA = common carotid artery; ECA = external carotid artery; NI = neurologic intolerance; NT = neurologic tolerance.
Table 1. The baseline characteristics and univariate analysis data in the prediction of NI.
| Characteristics | Total (n=123) | NT group (n=74) | NI group (n=49) | OR (95% CI) | p value | ||
|---|---|---|---|---|---|---|---|
| Clinical characteristics | |||||||
| Age (years) | 72±8 | 71±8 | 73±8 | 1.037 (0.989–1.086) | 0.130 | ||
| Male gender | 109 (89) | 65 (88) | 44 (90) | 1.218 (0.383–3.880) | 0.738 | ||
| Symptomatic stenosis | 97 (79) | 51 (69) | 46 (94) | 6.915 (1.947–24.560) | 0.003 | ||
| Recent stroke (<6 months) | 93 (76) | 49 (67) | 44 (90) | 4.490 (1.582–12.740) | 0.005 | ||
| Comorbidity | |||||||
| Hypertension | 92 (75) | 52 (72) | 40 (82) | 1.880 (0.781–4.525) | 0.159 | ||
| Diabetes mellitus | 48 (39) | 24 (32) | 24 (49) | 2.000 (0.952–4.200) | 0.067 | ||
| Current smoking | 28 (23) | 17 (23) | 11 (22) | 0.971 (0.410–2.299) | 0.946 | ||
| Hypercholesterolemia | 61 (50) | 39 (53) | 23 (47) | 0.794 (0.385–1.636) | 0.532 | ||
| Peripheral arterial disease | 17 (14) | 8 (13) | 8 (18) | 1.409 (0.503–3.945) | 0.514 | ||
| Ischemic heart disease | 64 (52) | 31 (51) | 26 (59) | 1.407 (0.681–2.911) | 0.357 | ||
| Lesion characteristics | |||||||
| Diameter stenosis (%) | 91±6 | 91±7 | 91±6 | 0.995 (0.937–1.057) | 0.875 | ||
| Severe proximal tortuosity | 3 (2) | 1 (1) | 2 (4) | 3.106 (0.274–35.224) | 0.360 | ||
| Intraluminal thrombus | 14 (11) | 7 (10) | 7 (14) | 1.595 (0.522–4.872) | 0.412 | ||
| Ulcerative lesion | 12 (10) | 7 (10) | 5 (10) | 1.088 (0.325–3.644) | 0.892 | ||
| Moderate to severe calcification | 12 (10) | 5 (7) | 7 (14) | 2.300 (0.686–7.713) | 0.177 | ||
| Contralateral carotid stenosis* | 18 (15) | 10 (14) | 8 (16) | 1.249 (0.455–3.425) | 0.666 | ||
| Procedural characteristics | |||||||
| Procedure time (minutes) | 43±12 | 42±13 | 45±11 | 1.022 (0.992–1.054) | 0.156 | ||
| Duration of protection (minutes) | 4.8±1.2 | 4.8±1.3 | 4.7±1.1 | 0.910 (0.672–1.231) | 0.540 | ||
| Absence of ACOM on TFCA | 20 (16) | 7 (10) | 13 (27) | 3.456 (1.266–9.434) | 0.015 | ||
| Use of vasopressors | 11 (9) | 3 (4) | 8 (16) | 4.618 (1.160–18.383) | 0.030 | ||
| Femoral artery pressure (mmHg) | |||||||
| Systolic | 176±25 | 175±25 | 177±24 | 1.002 (0.988–1.017) | 0.759 | ||
| Diastolic | 80±12 | 80±12 | 80±12 | 0.998 (0.969–1.029) | 0.910 | ||
| CCAOP (mmHg) | |||||||
| Systolic | 50±21 | 57±20 | 39±18 | 0.950 (0.928–0.973) | <0.001 | ||
| Diastolic | 38±15 | 42±14 | 31±14 | 0.947 (0.920–0.976) | <0.001 | ||
Values are presented as mean ± standard deviation or number of patients (%).
ACOM = anterior communicating artery; CCAOP = common carotid artery occlusion pressure; CI = confidential interval; NI = neurologic intolerance; NT = neurologic tolerance; OR = odds ratio; TFCA = transfemoral cerebral angiography.
*Defined as diameter stenosis more than 50%. Cases with total contralateral carotid occlusion were excluded from this study.
Lesion and procedural characteristics
Lesion and procedural characteristics were compared in the Table 1. The target lesions were similar in the 2 groups. The mean degree of diameter stenosis was 91±6%, which means relatively severe obstructive lesions. There was no difference in the presence of severe tortuosity, intraluminal thrombus, ulcerative lesion and moderate to severe calcified lesion in the 2 groups. Three patients, who had a type III aortic arch that was difficult to approach, developed NI.
The total procedure time was 43±12 minutes, and the mean occlusion time was 4.8±1.2 minutes (range, 3.0–9.7 minutes). The 2 groups did not show a difference in the mean protection time. NI was observed frequently in patients without the visualization of ACOM on pre-procedural transfemoral cerebral angiography (TFCA) (OR, 3.456; 95% CI, 1.266–9.434; p=0.015).
Hemodynamic data
The mean femoral artery pressure was 176/80 mmHg and the mean CCAOP was 50/38 mmHg. The systolic and diastolic femoral artery pressures did not show significant differences between the 2 groups (p=0.759 and 0.910, respectively). In contrast, the NI group had significantly lower systolic and diastolic CCAOP (39±18 vs. 57±20 mmHg; p<0.001 and 31±14 vs. 42±14 mmHg; p<0.001, respectively) than the NT group. NI were significantly associated with low systolic CCAOP (OR, 0.950; 95% CI, 0.928–0.973; p<0.001). The best cut-off value of systolic CCAOP after receiver operating curve analysis was less than 42 mmHg in the prediction of NI with sensitivity of 74% and specificity of 73% (area under the curve [AUC], 0.753; p<0.001). The OR of systolic CCAOP ≤42 mmHg was 7.477 (95% CI, 3.307–16.904; p<0.001). After multivariate analysis, systolic CCAOP ≤42 mmHg (OR, 6.461; 95% CI, 2.716–15.370; p<0.001) and symptomatic carotid artery stenosis (OR, 5.549; 95% CI, 1.415–21.767; p=0.014) were significant predictors of the developing NI during CAS with PPDs (Table 2).
Table 2. Multivariate analysis with variables in the prediction of NI.
| Variables | Beta | OR (95% CI) | p value |
|---|---|---|---|
| Systolic CCAOP (≤42 mmHg) | 1.866 | 6.461 (2.716–15.370) | <0.001 |
| Symptomatic carotid artery stenosis | 1.714 | 5.549 (1.415–21.767) | 0.014 |
| Absence of ACOM | 0.638 | 1.893 (0.602–5.952) | 0.275 |
| Diabetes mellitus | 0.345 | 1.412 (0.595–3.352) | 0.411 |
ACOM = anterior communicating artery; CCAOP = common carotid artery occlusion pressure; CI = confidential interval; NI = neurologic intolerance; OR = odds ratio.
Periprocedural and clinical outcomes
Periprocedural and clinical outcomes were listed in the Table 3. Comparing the amount of debris captured from blood that was suctioned after the procedure, debris was observed in 45% of the NT patients, while it was observed in 71% of the NI patients (p=0.005). More than 10 debris were captured in 43% of the NI group and 18% of the NT group (p=0.009).
Table 3. Periprocedural and clinical outcomes.
| Clinical outcomes | Total (n=123) | NT group (n=74) | NI group (n=49) | p value | |
|---|---|---|---|---|---|
| Procedural success | 123 (100) | 74 (100) | 49 (100) | 1.000 | |
| New HSI in DW-MRI | 32 (26) | 16 (22) | 16 (33) | 0.209 | |
| Periprocedural events | 6 (5) | 0 (0) | 6 (12) | 0.003 | |
| Major stroke | 1 (1) | 0 (0) | 1 (2) | 0.398 | |
| Minor stroke | 3 (2) | 0 (0) | 3 (6) | 0.061 | |
| TIA | 2 (2) | 0 (0) | 2 (4) | 0.157 | |
| 24-hour to 30-day events | 0 (0) | 0 (0) | 0 (0) | 1.000 | |
Values are presented as number of patients (%).
DW-MRI = diffusion-weighted magnetic resonance imaging; HSI = high signal intensity; NI = neurologic intolerance; NT = neurologic tolerance; TIA = transient ischemic attack.
The procedures were completed successfully for all patients. Pre- and post-procedural DW-MRI data were available in 121 patients. No differences in the rate of new high signal intensity (HSI) in post-procedural DW-MRI were found between the 2 groups (33% vs. 22%; p=0.215).
NI was persistent more than 30 minutes in 6 patients of the NI group, but it was resolved completely within 2 hours in 2 patients and defined as TIA. However, 4 patients experienced persistent neurologic event; 1 patient (1%) had a major stroke and 3 (3%) had minor strokes. All these 4 neurologic events occurred in the NI group, and the neurologic symptoms, which developed during the procedures, persisted more than 24 hours afterward. Therefore, stroke incidence significantly higher in NI group (8.2% vs. 0%; p=0.023). No patient had myocardial infarction or death during the procedure and during their hospital admission. No new event occurred between 24 hours and 1 month after the procedure.
All 4 patients, who experienced periprocedural neurologic events, had symptomatic carotid artery stenosis, and ACOM was not visualized in 3 patients on the pre-procedural magnetic resonance angiography (MRA) or TFCA. In addition, 3 patients had low systolic CCAOP of less than 42 mmHg. Four patients with strokes exhibited new HSI on DW-MRI. Of them, 2 patients had watershed infarction on the ipsilateral border zone.
DISCUSSION
In this study, we demonstrate that NI was developed in 40% of patients with proximal protected CAS. Low systolic CCAOP (≤42 mmHg) and symptomatic carotid artery stenosis were significantly associated with the development of NI during CAS procedures with PPDs.
Proximal protected CAS has great microembolization protection effect because it does not require crossing of the stenotic lesion without protection, and also has ability to protect even small-sized debris.2),3),4),5) However, NI occurs inevitably during the procedure. The incidence of NI was reported 6–30% in previous studies,6),7),8),9) which is known to be relatively common. In this study, the incidence of NI was 40%, and it seemed more frequently compared with previous studies. Although it was hard to explain the apparent causes, it may come from the relatively old age and high ratio of the patients with symptomatic and severe carotid artery stenosis. Because the attending neurologist continuously monitored the occurring of NI during the whole procedures, neurologist found and reported all neurologic findings.
Predicting of occurring of NI is important because it may big burden to the operator as well as cause adverse effect on the procedure, even transiently. It is recommended to detect the patients who have high risk of NI and pay attention during the CAS. Although it is possible to carry out shunt operation ahead in the patients with high risk of NI in the carotid endarterectomy (CEA), the prevention is not possible in CAS procedures.10) Also, it should be prepared appropriately management when NI happens, and if necessary, be considered of using other EPDs such as DFDs.
There are several proposed simple ways to check the tolerability of patients before the procedure. One of them is the assessment of ACOM connection on the pre-procedural MRA. MRA is a non-invasive method, but it is difficult to evaluate precisely in many cases. Another method is to use cerebral angiograms during TFCA. It could be shown the connection of ACOM that was may have been invisible before, if accompanied by the carotid compression test. In this study, we found that the absence of ACOM on TFCA was related to the increased risk of NI. It is similar to other study that interruptions of the circle of Willis are associated with high risk of intolerance to cross-clamping during CEA.11),12)
The measurement of systolic CCAOP is easy, simple, and safe. Both femoral artery and systolic CCAOP can easily be measured using a femoral sheath that is the same in diameter as a MO.MA device. It can also be monitored along with systemic pressure throughout the procedure and is useful for detection of periprocedural hemodynamic change or instability. Moreover, use of a sheath has the advantage of less femoral artery damage, less MO.MA tip and shaft damage and overcoming iliac tortuosity. We demonstrated that low systolic CCAOP (less than 42 mmHg) predicts occurrence of NI during proximal protected CAS. These results are concordant with the previous study by Giugliano et al.,6) and strengthened the importance of the occlusion pressure.7),13) In addition to the occlusion pressure, we found symptomatic carotid artery stenosis and non-visualization of ACOM on MRA or TFCA after the univariate analysis. Finally, symptomatic carotid artery stenosis and low systolic CCAOP were 2 major determinants of the development of NI during CAS procedures.
Another important finding was that there were more frequent periprocedural events in the NI group with statistical significance. There was no reported association between NI and long-term neurologic deficit, previously. Giugliano et al.6) reported no association between NI and the risk of post-procedural adverse clinical events. In our study, however, all patients did not recover from NI, especially, 2 of them showed watershed infarction in border zone area on the post-procedural DW-MRI of the brain. It suggests that these patients were greatly affected by cerebral hypoperfusion due to flow blockage, though there are many potential causes for neurologic sequelae during or after the CAS procedure such as embolization, hypoperfusion or hemodynamic instability.14),15) CCAOP can be affected the amount of collateral blood flow and degree of stenosis of the ipsilateral internal carotid artery. Because the degree of carotid artery stenosis was similar in the 2 groups, the collateral flow from Willis circle is major determinant to CCAOP. So, patients with decreased systolic CCAOP, especially less than 42 mmHg, can have poor collateral circulation and may be influenced greatly by the proximal occlusion. However, additional research on the association between NI and post-procedural neurologic deficits is necessary.
NI was more frequently developed in patients with symptomatic stenosis. It suggests that the cerebral reservoir in these patients is reduced and much vulnerable to flow decrease. Additionally, larger amount of debris captured in patients with NI group as well as symptomatic stenosis.
This study has several limitations. This is a retrospective observational study and was performed in a single center with a relatively small number of patients. And, since patients with contralateral total occlusion were excluded initially, the results should be interpreted with caution. However, all procedures were performed by 1 experienced operator, minimalized the bias that have been occurred by different operators. Additional multi-center research with large population will be needed that can support our findings.
In this study, about 40% showed NI during CAS procedures. Most of them (88%, 43 of 49 patients) recovered just after the balloon deflation but stroke incidence was significantly higher in NI group. Low systolic CCAOP (≤42 mmHg) and symptomatic carotid artery stenosis were significantly associated with the development of NI during CAS procedure using PPDs. Patients with these features should be cautiously monitored for the development of NI in the CAS procedure with PPDs.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Lee JH.
- Data curation: Kwon HJ, Park JH, Kim MJ.
- Formal analysis: Kwon HJ, Park JH, Kwon IS.
- Investigation: Lee JH, Jeong HS, Song HJ, Kim J.
- Supervision: Seong IW.
- Writing - original draft: Kwon HJ, Park JH.
- Writing - review & editing: Park JH, Lee JH.
References
- 1.Brott TG, Halperin JL, Abbara S, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/ SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. Vasc Med. 2011;16:35–77. doi: 10.1177/1358863X11399328. [DOI] [PubMed] [Google Scholar]
- 2.Bersin RM, Stabile E, Ansel GM, et al. A meta-analysis of proximal occlusion device outcomes in carotid artery stenting. Catheter Cardiovasc Interv. 2012;80:1072–1078. doi: 10.1002/ccd.24433. [DOI] [PubMed] [Google Scholar]
- 3.Bijuklic K, Wandler A, Hazizi F, Schofer J. The PROFI study (Prevention of Cerebral Embolization by Proximal Balloon Occlusion Compared to Filter Protection During Carotid Artery Stenting): a prospective randomized trial. J Am Coll Cardiol. 2012;59:1383–1389. doi: 10.1016/j.jacc.2011.11.035. [DOI] [PubMed] [Google Scholar]
- 4.Montorsi P, Caputi L, Galli S, et al. Microembolization during carotid artery stenting in patients with high-risk, lipid-rich plaque. A randomized trial of proximal versus distal cerebral protection. J Am Coll Cardiol. 2011;58:1656–1663. doi: 10.1016/j.jacc.2011.07.015. [DOI] [PubMed] [Google Scholar]
- 5.Cassese S, Ndrepepa G, King LA, et al. Proximal occlusion versus distal filter for cerebral protection during carotid stenting: updated meta-analysis of randomised and observational MRI studies. EuroIntervention. 2015;11:238–246. doi: 10.4244/EIJY15M03_01. [DOI] [PubMed] [Google Scholar]
- 6.Giugliano G, Stabile E, Biamino G, et al. Predictors of carotid occlusion intolerance during proximal protected carotid artery stenting. JACC Cardiovasc Interv. 2014;7:1237–1244. doi: 10.1016/j.jcin.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 7.Reimers B, Sievert H, Schuler GC, et al. Proximal endovascular flow blockage for cerebral protection during carotid artery stenting: results from a prospective multicenter registry. J Endovasc Ther. 2005;12:156–165. doi: 10.1583/04-1400MR.1. [DOI] [PubMed] [Google Scholar]
- 8.Cremonesi A, Manetti R, Liso A, Ricci E, Bianchi P, Castriota F. Endovascular treatment of soft carotid plaques: a single-center carotid stent experience. J Endovasc Ther. 2006;13:190–195. doi: 10.1583/05-1702MR.1. [DOI] [PubMed] [Google Scholar]
- 9.Stabile E, Salemme L, Sorropago G, et al. Proximal endovascular occlusion for carotid artery stenting: results from a prospective registry of 1,300 patients. J Am Coll Cardiol. 2010;55:1661–1667. doi: 10.1016/j.jacc.2009.11.079. [DOI] [PubMed] [Google Scholar]
- 10.Shahidi S, Owen-Falkenberg A, Gottschalksen B. Clinical validation of 40-mmHg carotid stump pressure for patients undergoing carotid endarterectomy under general anesthesia. J Cardiovasc Surg (Torino) 2017;58:431–438. doi: 10.23736/S0021-9509.16.08173-8. [DOI] [PubMed] [Google Scholar]
- 11.Montisci R, Sanfilippo R, Bura R, Branca C, Piga M, Saba L. Status of the circle of Willis and intolerance to carotid cross-clamping during carotid endarterectomy. Eur J Vasc Endovasc Surg. 2013;45:107–112. doi: 10.1016/j.ejvs.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 12.Bagan P, Vidal R, Martinod E, et al. Cerebral ischemia during carotid artery cross-clamping: predictive value of phase-contrast magnetic resonance imaging. Ann Vasc Surg. 2006;20:747–752. doi: 10.1007/s10016-006-9126-8. [DOI] [PubMed] [Google Scholar]
- 13.Diederich KW, Scheinert D, Schmidt A, et al. First clinical experiences with an endovascular clamping system for neuroprotection during carotid stenting. Eur J Vasc Endovasc Surg. 2004;28:629–633. doi: 10.1016/j.ejvs.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 14.White CJ. Carotid artery stenting. J Am Coll Cardiol. 2014;64:722–731. doi: 10.1016/j.jacc.2014.04.069. [DOI] [PubMed] [Google Scholar]
- 15.Howell M, Krajcer Z, Dougherty K, et al. Correlation of periprocedural systolic blood pressure changes with neurological events in high-risk carotid stent patients. J Endovasc Ther. 2002;9:810–816. doi: 10.1177/152660280200900614. [DOI] [PubMed] [Google Scholar]