ABSTRACT
Influenza vaccination is the most effective way to reduce influenza infection and related complications. Unfortunately, vaccination coverage remains suboptimal. The addition of pharmacists as immunizers may assist in improving vaccine coverage. The experiences of patients who have received influenza vaccines from pharmacists is an important consideration for jurisdictions considering the addition of pharmacists as immunizers. We describe the reported experiences of recipients of influenza vaccinations by pharmacists in the community pharmacy setting in Nova Scotia, Canada. During the 2013–2014 influenza season, a paper-based quality assurance questionnaire was provided to interested vaccine recipients to assess their previous vaccination experiences and current experience at the pharmacy. More than 6,500 vaccine recipients completed questionnaires. The majority of respondents cited convenience as a main reason for receiving the vaccine in the pharmacy, with 50% indicating the service was better in the pharmacy and another 40% that the service was as good as elsewhere. Respondents also reported a positive environment in the pharmacy (e.g., less stressful, less exposure to sick people) as well as professionalism and knowledge of the pharmacists. Areas for improvement identified included better communication around the paperwork required (e.g., consent forms) and the wait time post-vaccination. This evaluation demonstrated that people who chose to be vaccinated by community pharmacists reported positive experiences and convenience was the primary factor for selecting a pharmacy as the site for vaccination.
KEYWORDS: pharmacist, immunization, influenza vaccination, pharmaceutical services, Canada
Introduction
Influenza is a respiratory illness that can cause severe illness, leading to increased hospitalizations and mortality.1 Although variable on an annual basis, influenza infection results in an average of three to five million severe cases and up to 500,000 deaths worldwide each year.1 Within Canada, influenza is associated with an average of 12,000 hospitalizations and 3,500 deaths annually.2 Receipt of the annual seasonal influenza vaccine remains the most effective means to reduce influenza-related complications, but immunization coverage remains suboptimal in many countries, including Canada.3-5
Many factors contributing to vaccine hesitancy have been identified, often described by the “3Cs” model - Confidence, Complacency, and Convenience.6-9 Incorporating non-traditional vaccine providers into vaccination programs has been suggested as one way to improve immunization coverage related to some of these barriers.10
Pharmacists are trusted and accessible health care providers that have always played an important role in advocating for and providing education to patients on vaccines.11,12 While pharmacists have administered immunizations in the United States since 1996, this practice is relatively new in Canada and other jurisdictions.13-16 Pharmacists in Nova Scotia, Canada began administering influenza vaccines in the 2013–2014 influenza season to those 5 years of age and older.17
Patient experiences in the United States with pharmacists administering immunizations have generally been positive.18,19 One study found that 98% of respondents claimed they would continue to use pharmacy immunization services.20 There is limited Canadian data regarding patient experiences with influenza immunization in the pharmacy setting by pharmacists and currently no information from Nova Scotia patients.21-23 The experiences of persons receiving influenza vaccinations by pharmacists in community pharmacy settings is valuable for jurisdictions and pharmacy practices considering the addition of pharmacist immunization services. Using data from a questionnaire developed for quality assurance purposes, we describe the reported experiences of Nova Scotians who received influenza vaccination by a pharmacist in the community pharmacy setting.
Results
A total of 6,530 questionnaires were returned to Pharmacy Association of Nova Scotia (PANS), which is approximately 8.4% of the 78,102 people who received vaccines from pharmacists in Nova Scotia in 2013–2014.24 More than 64% of respondents reported receiving an annual influenza vaccination in the past five years, nearly 30% received at least one in the past, but not annually, and 6% had not previously received an influenza vaccination. When asked where previous vaccines were most often received, more than 40% indicated another healthcare provider location (such as a physician), 34% indicated they previously received their influenza vaccination at a public health clinic, and the remaining received past vaccinations at “other locations”, such as the work place. When asked where they preferred to receive their vaccine, nearly 72% indicated the pharmacy, 11% indicated the physician's office, 5% preferred public health clinics, and the remaining indicated other locations, such as the work place.
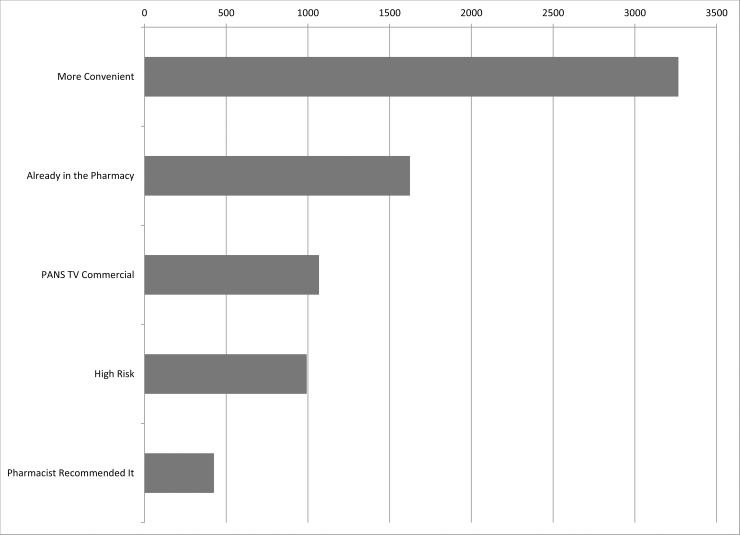
Respondents' reasons for receiving their influenza vaccine in the pharmacy are shown in Fig. 1. Convenience was most frequently cited followed by already being in the pharmacy and deciding to be vaccinated while there. Approximately 9% reported difficulty in finding someone to administer their influenza vaccination in the past.
Figure 1.
Questionnaire respondents' reasons for receiving the influenza vaccine in the pharmacy. *Totals do not equal 6,530, as respondents could provide more than one response.
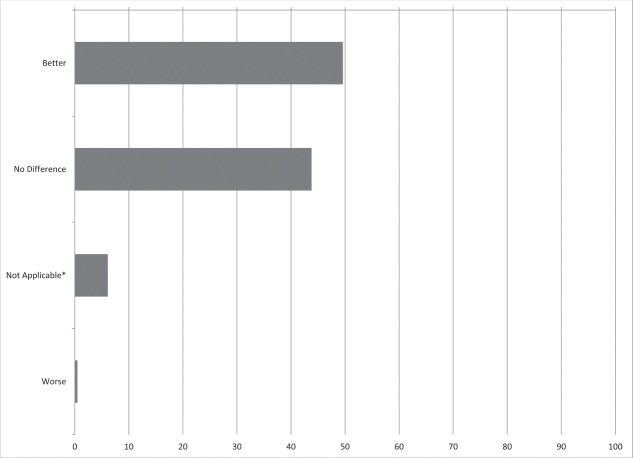
The quality of the immunization service as rated by respondents is found in Fig. 2. More than 90% of respondents reported that the quality of the service by the pharmacist to be as good or better than that received in the past by other immunizers. Less than 1% reported the service to be worse than that previously received.
Figure 2.
Questionnaire respondents' rating of the quality of influenza vaccination service received by the pharmacist compared to previous service providers. *Not Applicable was used by those who had not previously received an influenza vaccination.
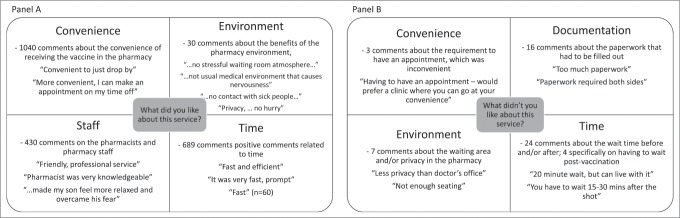
Written responses to the open-ended questions were included on 1800 questionnaires. Key themes identified included: Convenience, Documentation, Environment, Staff, and Time (Fig. 3).
Figure 3.
Most common themes and example quotes from respondents when asked the open-ended questions “What did you like about this service?” (Panel A) and “What didn't you like about this service?” (Panel B).
Key themes identified as areas that respondents liked about the service were: Convenience, Environment, Staff and Time (Fig. 3). The majority of responses were related to Convenience (n = 1040), which included comments about location, hours, ability to book appointments, walk-in options, and the benefit of already being in the pharmacy (e.g., a grocery store with a pharmacy). Of the comments related to positive experiences with Staff (n = 430), 40 were specifically related to the knowledge of the pharmacist. Responses identified within the Environment (n = 30) theme were diverse, and included comments related to the positive atmosphere in general, being less stressful than waiting in a medical office, avoiding contact with sick people (versus other waiting rooms) and the amount of privacy. In addition to the main themes identified, there were more than 200 general positive comments made, such as “excellent,” “great,” and “good.”
There were 323 responses to the question “What didn't you like about this service?” of which 263 were deemed positive, such as “nothing, everything was good”. Such comments were coded as positive and not further categorized into themes. The remaining 60 responses were grouped into four key themes: Convenience, Documentation, Environment, and Time (Fig. 3). The most common responses were around wait times, predominantly related to the wait time required post-vaccination.
There were 399 additional statements in response to the question “Any other suggestions or comments?”. Nearly 200 responses in this section were general positive comments, like “Very good,” “Well done,” and “Keep up the good work.” The next most common responses were those related to the wish for the service to continue (n = 66), such as “Please continue this service,” “Keep it up every year,” and “I would come here again next year.” In addition, there were 49 positive responses related to the key theme of Convenience. There were six responses related to the key theme of Documentation, with suggestions of informing patients in advance that forms will have to be filled out and suggestions for speeding up the paperwork process.
Discussion
We found that the majority of respondents who received their influenza vaccine from a pharmacist in the community pharmacy setting reported their experience to be positive. Almost half of respondents indicated the immunization service received was better in the pharmacy than that previously experienced elsewhere, with another approximately 40% reporting the experience to be no different. This data is similar to that reported by others, who have described a high degree of patient satisfaction with vaccination services provided by pharmacists in a community pharmacy setting.18,23,25
Consistent with other reports, convenience appeared to be the primary determinant for the positive experience reported based on the number of respondents selecting it as the reason for being immunized in the pharmacy and the number of written comments related to convenience in answering “What did you like about the service?”.23,26,27,28 Pharmacies are generally more geographically accessible than other more traditional immunization providers, such as those delivered in primary care and public health programs. Within Nova Scotia, 78% of residents live within 5 km of a pharmacy and 40% live within walking distance.29 Furthermore, access to primary care in Nova Scotia is a growing problem, with an estimated 11% of the Nova Scotia population reporting they do not have a family doctor.30 We found that 9% of respondents reported difficulty in finding someone to provide their influenza vaccination in the past. Furthermore, adding pharmacists as immunization providers appears to have increased the number of Nova Scotians who received influenza vaccination., with a 6% increase in 2013–2014 compared to the previous influenza season (41.6% and 35.7%, respectively, with 26.6%, 6.3% and 8.7% immunized by family physicians, public health and pharmacists respectively), which is similar to the 6% of respondents reported not having received the influenza vaccine previously.24,31 As convenience is an important contributor to vaccine hesitancy, our data support the premise that provision of influenza vaccine in non-traditional settings, such as community pharmacies, is one means of reducing vaccine hesitancy related to issues of convenience.9 In addition, the provincial Department of Health and Wellness and the Pharmacy Association of Nova Scotia each employed widespread communication plans informing the public about the importance of influenza vaccination and that they could be obtained from various providers, including pharmacists, which may have motivated some individuals to be vaccinated for the first time.
Another contributing factor to respondents' positive reports of their experiences was confidence in the knowledge and competence of pharmacists as immunizers. A number of responses referred to the pharmacist being knowledgeable about vaccines. Other comments referred to the vaccine administration being “quick and easy,” “gentle,” or “didn't feel a thing.” These findings are consistent with those of a recent pan-Canadian survey that found the majority of adult Canadians surveyed reported pharmacists as a trustworthy resource for vaccine-related information and were willing to be vaccinated by a pharmacist, attesting to the confidence the general public has in the ability of pharmacists to provide safe and effective vaccination services.32
A second component contributing to confidence identified was the pharmacy environment. There were many responses that the pharmacy was “less stressful than waiting in a medical office” and not feeling rushed as there was “…no hurry.” Others commented that they appreciated not having to “sit in a waiting room with sick people.” These positive responses that indicated confidence in pharmacist provision of vaccines in the pharmacy setting may assist with overcoming one aspect of vaccine hesitancy, as trust in the systems that deliver vaccines, including in health professionals who vaccinate, was previously identified as a factor - Confidence - influencing vaccine hesitancy.9
The main concerns of respondents were related to the paperwork required (Documentation) and the time to wait (Time) in the pharmacy post-injection. Although provincial legislation requires documentation of oral consent only, many pharmacies obtain written consent primarily for pharmacy records.33 Pharmacies should consider streamlining their current documentation processes and/or better explain them to patients. Likewise, some pharmacists may need to provide a better explanation of the importance of waiting for 10 to 15 minutes post-vaccination to monitor for a potential reaction, which is considered best practice, although the likelihood of a post-vaccination reaction is small.34
Strengths of this evaluation include, the reasonable response rate given the informal nature of the administration of the quality assurance questionnaires; administration of the questionnaire throughout the entire province provided more representative results; and the large number of written comments which provided valuable additional information.
There are several limitations to this evaluation. As a quality assurance project, questionnaire design and administration did not follow standard methodological procedures. However, the questionnaire as administered met the quality assurance needs of PANS. In addition, the response rate was reasonable, with pertinent, usable data for additional analysis. There is also the possibility that results may have been subject to response bias. Respondents may have completed the questionnaire in the pharmacy and responded more positively than they felt. However, there were still a number of negative and constructive comments, suggesting response bias is less likely or less strong. There is also potential for selection bias as the questionnaire was only provided to individuals who were willing to receive their influenza vaccine by a pharmacist in the community pharmacy setting. Those who prefer to receive vaccination services from traditional providers may report less positive experiences. However, more than 75% of adult Canadians surveyed report they would be willing to be immunized by a pharmacist, which suggests that selection bias may be mitigated or diminshed.32
This evaluation further supports data from other jurisdictions that recipients of pharmacist administered vaccines have positive experiences and that pharmacist provision of vaccines may assist in addressing two of the “3 Cs” in vaccine hesitancy - convenience and confidence.9 The results may be helpful to jurisdictions or practices looking to add pharmacist administration of influenza vaccines by providing patient insight around the benefits and potential concerns. Future work should be completed with those who have received vaccines in other settings and those who have not received vaccines to better determine important factors that may further improve the vaccine experience to improve vaccination coverage.
Methods
A questionnaire was administered through pharmacies in Nova Scotia for quality assurance purposes during the first influenza season in which pharmacists were permitted to vaccinate (2013–2014). The questionnaire was developed by pharmacy stakeholders, then reviewed and modified by the Pharmacy Association of Nova Scotia (PANS). The questionnaire consisted of seven multiple choice questions related to previous vaccination experiences and current experience at the pharmacy. Two open-ended questions inquiring about what respondents liked or didn't like about the service and one question to allow for additional comments were included at the end of the questionnaire.
Questionnaires were sent to all pharmacies in Nova Scotia. Pharmacists that were interested in participating provided a paper copy to patients after they administered their influenza vaccine. Patients who chose to complete the survey returned them to the pharmacy. There were no patient identifiers on the questionnaire. Pharmacies returned the questionnaires to PANS via mail or fax, and anonymous data was inputted into a Microsoft Excel database by contracted third parties.
The database was provided to the authors for further analysis and interpretation of the results. Summary statistics were used to describe responses to the multiple-choice questions. Comments from the open-ended questions were transcribed into a single Microsoft Excel file and grouped into categories through inductive and deductive processes to identify codes and themes.35 Preliminary codes were developed using deductive processes, as many codes were expected, such as convenience and time based on previous literature.18,23,25 Inductive processes were considered when unexpected responses were received, leading to new codes. Overlap between codes was minimized by clearly delineating the meaning of each code and using it consistently throughout.
The study was reviewed by the Nova Scotia Health Authority Research Ethics Board and granted ethics exemption for secondary use of quality assurance data.
Abbreviations
- NS
Nova Scotia
- PANS
Pharmacy Association of Nova Scotia
Disclosure of potential conflicts of interest
In accordance with Taylor & Francis policy and the ethical obligation of researchers, ACW reports that she is an employee of the Pharmacy Association of Nova Scotia (PANS) that funded the completion of the quality assurance survey, and subsequently may be affected by the research reported in the enclosed paper. She has disclosed these interests fully to Taylor & Francis. No potential conflicts of interest were reported for JEI or SKB related to this work.
Acknowledgments
The authors would like to thank Deidre Coughran, Sharon Isenor, Jessica Killen, and Beth O'Reilly for their assistance with data entry and manuscript preparation.
Funding
The survey was completed at the expense of the Pharmacy Association of Nova Scotia (PANS). No funds were received for the data analysis, interpretation, or writing of the manuscript.
References
- 1.National Advisory Committee on Immunization (NACI) Canadian immunization guide chapter on influenza and statement on seasonal influenza vaccine for 2017–2018; 2017. June [Accessed September12, 2017]. Available at: https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-statement-seasonal-influenza-vaccine-2017-2018.html.
- 2.Schanzer D, McGeer A, Morris K. Statistical estimates of respiratory admissions attributable to seasonal and pandemic influenza for Canada. Influenza Other Respir Viruses. 2013. September;7(5):799–808. doi: 10.1111/irv.12011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McIntyre A, Gonzalez-Feliciano A, Bryan L, Santibanez T, Williams W, Singleton J, Centers for Disease Control and Prevention (CDC) . Seasonal influenza vaccination coverage - United States, 2009–2010 and 2010–2011. MMWR Suppl. 2013. November;62(3):65–68. [PubMed] [Google Scholar]
- 4.Blank P, Schwenkglenks M, Szucs T. Vaccination coverage rates in eleven European countries during two consecutive influenza seasons. J Infect. 2009. June;58(6):446–58. doi: 10.1016/j.jinf.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Buchan S, Kwong J. Trends in influenza vaccine coverage and vaccine hesitancy in Canada, 2006/07 to 2013/14: Results from a cross-sectional survey data. CMAJ Open. 2016. Aug.;4(3):E455–E462. doi: 10.9778/cmajo.20160050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Public Health Agency of Canada Immunization coverage in Canada (2002 to 2012); 2014. [Accessed Jun. 6, 2014]. Available at http://www.phac-aspc.gc.ca/im/nics-enva/icc-cvc-eng.php.
- 7.Kimmel S, Burns I, Wolfe R, Zimmerman R. Addressing immunization barriers, benefits, and risks. J Fam Pract. 2007;56(2.Suppl.Vaccines):S61–9. [PubMed] [Google Scholar]
- 8.Johnson D, Nichol K, Lipczynski K. Barriers to adult immunization. Am J Med. 2008;12(7.Suppl.2):S28–35. doi: 10.1016/j.amjmed.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 9.MacDonald N, SAGE Working Group on Vaccine Hesitancy . Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 10.Shen A, Bridges C, Tan L. The first national adult immunization summit 2012: Implementing change through action. Vaccine. 2013;31:279–84. doi: 10.1016/j.vaccine.2012.11.033. [DOI] [PubMed] [Google Scholar]
- 11.Lynas K. Pharmacists still most trusted professionals, says Ipsos Reid. Can Pharm J/Revue des Pharmaciens du Canada. 2011;144(2):55. doi: 10.3821/1913-701X-144.2.55b. [DOI] [Google Scholar]
- 12.Hogue M, Grabenstein J, Foster S, Rothholz M. Pharmacist involvement with immunizations: A decade of professional advancement. J Am Pharm Assoc. 2006;46(2):168–79. doi: 10.1331/154434506776180621. [DOI] [PubMed] [Google Scholar]
- 13.Atkins K, van Hoek A, Watson C, Baguelin M, Choga L, Patel A, Raj T, Jit M, Griffiths U. Seasonal influenza vaccination delivery through community pharmacists in England: Evaluation of the London pilot. BMJ Open. 2016. February;6(2):e009739. doi: 10.1136/bmjopen-2015-009739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goad J, Taitel M, Fensterheim L, Cannon A. Vaccination administered during off-clinic hours at a national community pharmacy: Implications for increasing patient access and convenience. Ann Fam Med. 2013;11(5):429–36. doi: 10.1370/afm.1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grabenstein J, Guess H, Hartzema A, Koch G, Konrad T. Effect of vaccination by community pharmacists among adult prescription recipients. Med Care. 2001;39(4):340–48. doi: 10.1097/00005650-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Pharmacy Guild of Australia Vaccination services; 2017. Aug. [Accessed Sept. 20, 2017]. Available at https://www.guild.org.au/programs/vaccination-services.
- 17.Pharmacy Association of Nova Scotia Immunizing and injecting; [Accessed Sept. 25, 2017]. Available at: https://pans.ns.ca/public/pharmacy-services/immunizing-injecting.
- 18.Bounthavong M, Christopher M, Mendes M, Foster E, Johns S, Lim L, Rubin LM, Patel JJ, Stewart AG. Measuring patient satisfaction in the pharmacy specialty immunization clinic: A pharmacist-run immunization clinic at the Veterans Affairs San Diego Healthcare System. Int J Pharm Pract. 2010;18(2):100–7. [PubMed] [Google Scholar]
- 19.Hagermann T, Johnson E, Conway S. Influenza vaccination by pharmacists in a health sciences center: A 3-year experience. J Am Pharm Assoc. 2014;54(3):295–301. [DOI] [PubMed] [Google Scholar]
- 20.Hind C, Bond C, Lee A, van Teiglingen E. Travel medicine services from community pharmacy: Evaluation of a pilot service. Pharm J. 2008;281:625–28. [Google Scholar]
- 21.Cheung W, Tam K, Cheung P, Banh H. Satisfaction with student pharmacists administering vaccinations in the University of Alberta annual influenza campaign. Can Pharm J. 2013;146(4):227–232. doi: 10.1177/1715163513492628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alsabbagh W, Wenger L, Papstergiou J, Pojskic N, Raman-Wilms L, Schneider E, Waite N. Facilitators and barriers of Ontario pharmacists as providers of influenza vaccination: Surveys of pharmacists and patrons of community pharmacies. Can Pharm J. 2015;148(4):21. [Google Scholar]
- 23.Papstergiou J, Folkins C, Li W, Zervas J. Community pharmacist-administered influenza immunization improves patient access to vaccination. Can Pharm J. 2014;147(6):359–65. doi: 10.1177/1715163514552557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Isenor J, Alia T, Killen J, Billard B, Halperin B, Slayter K, McNeil SA, MacDougall D, Bowles SK. Impact of pharmacists as immunizers on influenza vaccination coverage in Nova Scotia, Canada. Hum Vaccin Immunother. 2016;12(5):1225–8. doi: 10.1080/21645515.2015.1127490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hess J, Dai C, Gamer B, Law A. Measuring outcomes of a pharmacist-run travel health clinic located in an independent community pharmacy. J Am Pharm Assoc. 2010;50(2):174–80. doi: 10.1331/JAPhA.2010.09204. [DOI] [PubMed] [Google Scholar]
- 26.Hattingh H, Sim T, Parsons R, Czarniak P, Vickery A, Ayadurai S. Evaluation of the first pharmacist-administered vaccinations in Western Australia: A mixed-methods study. BMJ Open. 2016;6(9):e011948. doi: 10.1136/bmjopen-2016-011948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anderson C, Thornley T. Who uses pharmacy for flu vaccinations? Population profiling through a UK pharmacy chain. Int J Clin Pharm. 2016;38(2):218–22. doi: 10.1007/s11096-016-0255-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grabenstein JD, Guess HA, Hartema AG, Koch GG, Konrad TR. Attitudinal factors among adult prescription recipients associated with choice of where to be vaccinated. J Clin Epidemiol 2002;55(3):279–84. doi: 10.1016/S0895-4356(01)00452-8. [DOI] [PubMed] [Google Scholar]
- 29.Law M, Heard D, Fisher J, Douillard J, Muzika G, Sketris I. The geographic accessibility of pharmacies in Nova Scotia. Can Pharm J. 2013;146(1):39–46. doi: 10.1177/1715163512473062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Statistics Canada Access to a regular medical doctor, 2014; 2015. [Accessed Sept. 29, 2017]. Available at: http://www.statcan.gc.ca/pub/82-625-x/2015001/article/14177-eng.htm.
- 31.Isenor JE, Killen JL, Billard BA, McNeil SA, MacDougall D, Halperin BA, Slayter KL, Bowles SK. Impact of pharmacists as immunizers on influenza vaccination coverage in the community-setting in Nova Scotia, Canada: 2013–2015. J Pharm Policy Pract. 2016;9:32. doi: 10.1186/s40545-016-0084-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MacDougall D, Halperin B, Isenor J, MacKinnon-Cameron D, Li L, McNeil S, Langley JM, Halperin SA. Routine immunization of adults by pharmacists: Attitudes and beliefs of the Canadian public and health care providers. Hum Vaccin Immunother. 2016;12(3):623–31. doi: 10.1080/21645515.2015.1093714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nova Scotia College of Pharmacists Standards of practice: Drug administration; 2015. [Accessed Sept. 22, 2017]. Available at: http://www.nspharmacists.ca/wp-content/uploads/2015/12/DrugAdministrationStandardsOfPractice.pdf.
- 34.D'Heilly S, Blade M, Nichol K. Safety of influenza vaccinations administered in nontraditional settings. Vaccine. 2006;24(18):4024–7. doi: 10.1016/j.vaccine.2005.09.061. [DOI] [PubMed] [Google Scholar]
- 35.Green J, Thorogood N. Qualitative methods for health research. 3rd ed. Thousand Oaks, California: Sage Publications; 2013. [Google Scholar]