Abstract
Background:
This study aims to assess cognitive change in a 2-year period among U.S. Chinese older adults and examine sociodemographic characteristics associated with the change.
Methods:
Data were from the Population Study of Chinese Elderly (PINE) in which 2,713 participants (aged 60 and older) received in-home interviews at both the baseline and 2-year follow-up. A battery of cognitive tests that assessed episodic memory, working memory, perceptual speed, and overall cognitive status were administered in both times. A composite global cognition was constructed using all tests. Mixed-effect regression was conducted.
Results:
Older age was associated with worse baseline cognition (ie, in all cognitive abilities) and faster decline in global cognition, episodic memory, and perceptual speed—rates of decline increased by .006, .004, and .009 standard score units, respectively, for each year older. More education was associated with better baseline cognition, but each year of additional schooling increased rates of decline in global cognition and episodic memory by .004 and .012 standard score units, respectively. Men performed better than women in most cognitive abilities at baseline but had faster rates of decline in working memory. Higher income was associated with better cognition at baseline and reduced rates of decline in working memory.
Conclusions:
Findings suggest differences in the rates of cognitive change by age, sex, education, and income. Those in advancing age are vulnerable to cognitive decline. The effects of education and sex on baseline performance versus change suggest a role for life experiences in cognition.
Keywords: Cognitive aging, Chinese, Longitudinal study
With the trend of population aging and increased risks of dementia with age, there is increasing interest to understand how cognitive function changes in older adults. Thus far, most attention has been given to detecting cognitive impairment and assessing cognitive decline of those with dementias. To provide basic and relevant information for policy, program, and service development to support the public to maintain cognitive function, experts in the field have called for taking “a more complete view about the nature and extent of cognitive aging in older adults” (1). Population-based data are particularly suited for such purpose. Indeed, longitudinal data from population-based surveys have revealed substantial interindividual and intraindividual variation in the trajectory and patterns of cognitive change among older adults (1). These data also highlight the importance of considering race/ethnicity in understanding cognitive aging (2,3). To our knowledge, no studies have examined cognitive change in U.S. Chinese adults to date. This is because in part, until now, no population-based data are available to study this population.
Chinese is the largest subgroup of Asian Americans who are the fastest growing ethnic minority group in the United States (4). In 2015, there were 4.9 million Chinese in the United States and the number was expected to grow in an exponential rate (5). There is a perception that Chinese are a “model minority” who have achieved socioeconomic success in the United States and are living the American dream (6). This view discounts socioeconomic disparities within the Chinese American population and ignore barriers to aging well for many older Chinese adults. Some aspects of the Chinese culture, a few qualitative studies suggest, may increase the risk of cognitive decline for Chinese people (7,8). These studies show that Chinese tend to perceive cognitive decline with age as inevitable, and they attach strong shame and stigma to dementia. Such attitude may discourage Chinese adults from engaging in behavior to maintain cognitive function and seeking early treatment for cognitive complaints.
The Population Study of Chinese Elderly (PINE) is the first population-based epidemiological study of U.S. Chinese older adults in the United States (9). The purpose of the study was to provide population-based information about older Chinese Americans and to examine key determinants of their health and well-being. Using the PINE baseline data, a study has reported cognitive function in multiple domains among the sample and examined how each domain is related to sociodemographic and health characteristics of respondents (10). The present study extends this prior work. Taking advantage of the newly available Wave 2 data from the PINE study, we aim to assess changes in a multiplicity of cognitive function over a 2-year period and examine variation in the rate of change, as related to sociodemographic characteristics and health status, in U.S. Chinese older adults.
Methods
Sample and Setting
The PINE study was a community–academic collaboration among Rush Institute for Healthy Aging, Northwestern University, and more than 20 community-based social service organizations throughout the greater Chicago area. Given the low percentage of Chinese older adults in the U.S. population, a targeted community-based recruitment strategy was used to recruit the sample. The research team engaged the social service organizations to be recruitment sites. In a way sample recruitment was integrated with routine services provided to Chinese families throughout the city and suburban areas. The study was also widely promoted in local Chinese quarterly newspaper and through flyers in public places that were frequented by Chinese people. Baseline survey was conducted between 2011 and 2013 through in-home interviews with 3,157 Chinese adults aged 60 and older. The interviews were conducted in respondents’ preferred language (Chinese, English) and dialect (Cantonese, Taishanese, Mandarin, and Teochew). Detailed descriptions of the baseline PINE data collection have been published elsewhere (9). Demographic characteristics of the PINE sample were comparable to those available from the 2010 U.S. Census and a random street-block census of the Chinese community in Chicago (11). The second wave of data was collected 2 years after the baseline and completed in 2015. A total of 2,713 respondents (86% of baseline sample) were successfully followed up. Among the 444 who did not complete follow-up, 115 were deceased and 329 were lost. Compared with those who participated in Wave 2, those who did not were older and performed worse on the Chinese Mini-Mental State Exam (C-MMSE) and global cognition. The Institutional Review Boards of the Rush University Medical Center have approved the PINE study.
Measures
Cognitive function
A battery of five cognitive tests was administered during the in-home interviews at both waves. Higher scores represent better performance for all tests. Four of the five tests assessed three cognitive domains—episodic memory, working memory, and perceptual speed. Episodic memory was a composite of the East Boston Memory Test-Immediate Recall (EBMT) and the East Boston Memory Test-Delayed Recall (EBDR) (12). The two tests used immediate (EBMT) and delayed recall (EBDR) of brief stories. The second domain, working memory, was assessed by the Digit Span Backwards which was drawn from the Wechsler Memory Scale-Revised (12). Perceptual speed was measured by the Symbol Digit Modalities Test (SDMT)—a 11-item test that calls for rapid perceptual comparisons of numbers and symbols in 90 seconds (13). The fifth test in the battery, the C-MMSE, was based on the MMSE (Mini-Mental State Examination) which is a widely used measure in epidemiological studies to assess overall cognitive status (14). The C-MMSE has been validated in Chinese older adults in Hong Kong (15). Raw scores of all five tests were converted to z scores, using the baseline population estimates of the mean and standard deviation, to construct cognitive factors (three cognitive domains and C-MMSE). In addition, to minimize floor and ceiling artifacts and other measurement errors, we constructed a composite measure of global cognition by averaging the z scores of all five cognitive tests (16). Principal component analysis shows that the five tests had loadings between .72 and .87 on the first component which accounted for 67% of the variance.
Sociodemographic characteristics and health status
Sociodemographic characteristics included age, sex, education, income, and marital status. Age was measured in chronological years and was centered at 72 in the mixed-effect regression analysis. Men were coded 1. Education was indicated by completed years of regular schooling. Income refers to total annual income of the respondent and was measured in 10 categories. Marital status was coded as currently married = 1 versus not = 0. Health status was indicated by medical conditions, which was a count of chronic conditions, among nine, that the participant had been told by a doctor, nurse, or therapist that (s)he had.
Time
Time was measured as the difference between baseline and Wave 2 interviews. The mean was 1.92 (SD = 0.30) years, with a minimum of 1.75 years and a maximum of 3.72 years.
Data Analysis
Univariate statistics were used to summarize the five cognitive tests and the cognitive factors (ie, the three cognitive domains, C-MMSE, and global cognition) at two time points, and their difference scores between the time points (ie, Wave 2 – baseline). Spearman correlations were used to assess bivariate associations of baseline sociodemographic and health status variables with difference scores of the cognitive factors. Mixed-effect regression models were used to estimate the annual rate of change in the three cognitive domains and global cognition and to examine associations of sociodemographic characteristics and health status with the rates of change in the cognitive factors. The distribution of C-MMSE was highly skewed; so, it was not included in the mixed-effect regression analysis. All statistical analyses were undertaken using SAS, Version 9.2 (SAS Institute, Cary, NC).
Results
Baseline Characteristics of the Sample
Of the 2,713 participants who were interviewed at both baseline and Wave 2, the average age was 72.6 years old and 58.4% were women. On average, they had 8.7 years of education, and 85.8% had income of less than $10,000. At baseline, 69.9% were married. On average, they had 2.1 chronic conditions.
Descriptive Statistics of Baseline, Follow-up, and Difference Scores in Cognition
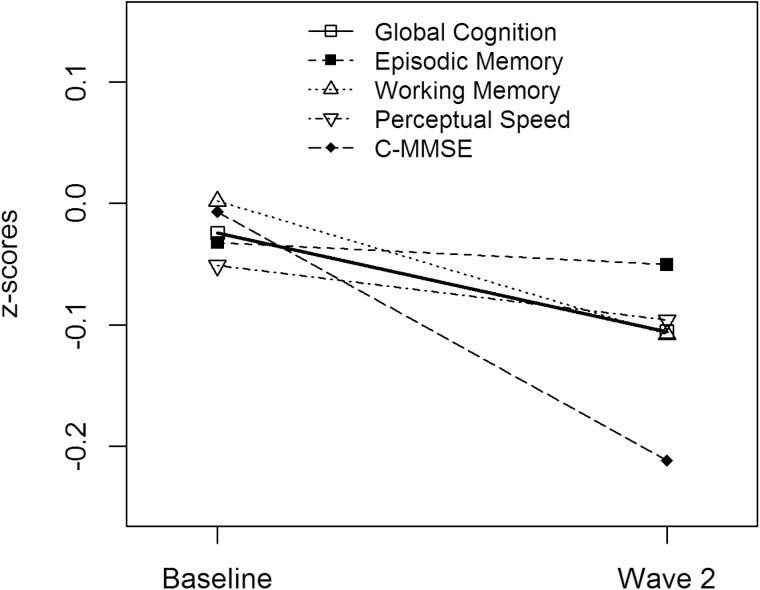
The upper panel of Table 1 presents descriptive statistics of the five cognitive tests. Sample size varied across tests and waves due to missing data. As shown, all cognitive test scores, except that for the EBDR, were lower at Wave 2 compared to that at baseline. The lower panel of Table 1 presents descriptive statistics of the cognitive factors in z-score units. The scores for all were lower at Wave 2 than at baseline. Figure 1 illustrates the difference in the scores of each cognitive factor between the two waves. Relatively, C-MMSE had the sharpest decline while episodic memory was the most stable.
Table 1.
Descriptive Statistics of Baseline, Wave 2, and Change in Cognitive Tests, and Cognitive Factorsa
| Baseline | Wave 2 | Difference (Wave 2—Baseline) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Number | Mean (SD) | Skewness | Total Number | Mean (SD) | Skewness | Total Number | Mean (SD) | Skewness | |
| Cognitive Testsa | |||||||||
| C-MMSE | 2,631 | 25.42 (4.53) | −1.87 | 2,648 | 24.47 (5.22) | −1.76 | 2,579 | −0.86 (3.47) | −0.66 |
| EBMT | 2,674 | 7.47 (2.70) | −0.75 | 2,682 | 7.36 (2.76) | −0.81 | 2,646 | −0.10 (2.71) | −0.10 |
| EBDR | 2,663 | 7.04 (2.99) | −0.75 | 2,685 | 7.04 (2.95) | −0.083 | 2,638 | 0.03 (2.83) | −0.00 |
| DB | 2,677 | 5.04 (2.38) | 0.58 | 2,677 | 4.77 (2.40) | 0.59 | 2,645 | −0.26 (2.00) | 0.03 |
| SDMT | 2,171 | 29.71 (11.96) | 0.19 | 2,632 | 29.11 (13.92) | 0.90 | 2,114 | −0.13 (11.30) | 1.93 |
| Cognitive factorsb | |||||||||
| Global cognition | 2,669 | −0.02 (0.80) | −0.73 | 2,679 | −0.11 (0.85) | −0.83 | 2,640 | −0.07 (0.56) | −0.08 |
| C-MMSE | 2,631 | −0.01 (0.99) | −1.87 | 2,648 | −0.22 (1.15) | −1.76 | 2,579 | −0.19 (0.76) | −0.66 |
| Episodic memory | 2,677 | −0.03 (0.97) | −0.075 | 2,688 | −0.05 (0.97) | −0.83 | 2,654 | −0.01 (0.92) | −0.07 |
| Working memory | 2,677 | 0.00 (0.99) | 0.58 | 2,677 | −0.11 (0.10) | 0.59 | 2,645 | −0.11 (0.83) | 0.03 |
| Perceptual speed | 2,171 | −0.05 (0.91) | 0.19 | 2,632 | −0.10 (1.06) | 0.90 | 2,114 | −0.01 (0.86) | 1.93 |
Note: aC-MMSE = Chinese Mini Mental State Exam; DB = Digit Span Backwards; EBDR = East Boston Memory Test-Delayed Recall; EBMT = East Boston Memory Test-Immediate Recall; SDMT = Symbol Digit Modalities Test. bRaw scores of the cognitive tests were converted to z scores to construct cognitive factors. Global cognition was a composite of all five cognitive tests. Episodic memory was a composite of EBMT and EBDR. Working memory, and perceptual speed were from DB and SDMT, respectively.
Figure 1.
Plotted data on cognitive factors at baseline and Wave 2.
Spearman Correlations
Bivariate correlations of sociodemographic characteristics and health status with difference scores of the cognitive factors are presented in Table 2. Older age was significantly correlated with greater decrease of scores in global cognition, C-MMSE, and perceptual speed. Men had more reduction in scores on working memory than women. More education was correlated with more decrease in scores on global cognition and episodic memory, but more increase in scores on C-MMSE. Income, marital status, and medical conditions had no statistically significant correlations with difference scores of any cognitive factors.
Table 2.
Spearman Correlations Between Sociodemographic Characteristics, Health Status, and Difference Scores of Cognitive Factors
| Age | Sex | Education | Income | Marital Status | Medical Conditions | |
|---|---|---|---|---|---|---|
| Global cognition | −0.12‡ | −0.02 | −0.05† | 0.01 | 0.03 | −0.01 |
| C-MMSE | −0.17‡ | −0.01 | 0.07‡ | −0.03 | 0.04 | −0.04 |
| Episodic memory | −0.04* | −0.02 | −0.11‡ | 0.00 | 0.01 | 0.01 |
| Working memory | 0.00 | −0.05† | 0.01 | 0.02 | 0.01 | 0.02 |
| Perceptual speed | −0.14‡ | −0.00 | 0.00 | 0.03 | 0.02 | −0.03 |
Note: *p<.05. †p < .01. ‡p < .001.
Estimation From Mixed-Effects Models
Mixed-effects regression models were used to estimate rates of change in the three cognitive domains and global cognition. We first estimated an unconditional model (Table 3, Model 1) and the estimation shows that on average, global cognition declined by .039 (p < .001) standard score units and working memory declined by .055 (p < .001) standard score units, per year. Changes in episodic memory (−.007) and perceptual speed (−.008) were not statistically significant. These average rates of change, however, did not take into account heterogeneity in the population sample.
Table 3.
Associations of Sociodemographic Characteristics and Health Status With Baseline and Change of Cognition, Estimated From Mixed-Effects Models
| Cognitive Factors | ||||
|---|---|---|---|---|
| Global Cognition Estimate (SE) | Episodic Memory Estimate (SE) | Working Memory Estimate (SE) | Perceptual Speed Estimate (SE) | |
| Model 1 | ||||
| Intercept | −0.013 (0.015) | −0.020 (0.019) | 0.009 (0.019) | −0.033 (0.019) |
| Time | −0.039 (0.006)‡ | −0.007 (0.009) | −0.055 (0.008)‡ | −0.008 (0.009) |
| Model 2 | ||||
| Time | 0.008 (0.006) | 0.036 (0.010)‡ | −0.030 (0.009)‡ | 0.044 (0.010)‡ |
| Agea | −0.034 (0.002)‡ | −0.036 (0.002)‡ | −0.024 (0.002)‡ | −0.036 (0.002)‡ |
| Age × Time | −0.006 (0.001)‡ | −0.004 (0.001)† | −0.001 (0.001) | −0.009 (0.001)‡ |
| Model 3 | ||||
| Time | −0.001 (0.013) | 0.044 (0.021)* | −0.049 (0.019)† | 0.006 (0.021) |
| Age | −0.029 (0.002)‡ | −0.031 (0.002)‡ | −0.018 (0.002)‡ | −0.032 (0.002)‡ |
| Age × Time | −0.006 (0.002)‡ | −0.004 (0.001)‡ | −0.001 (0.001) | −0.009 (0.001)‡ |
| Male | 0.080 (0.024)† | −0.027 (0.033) | 0.198 (0.034)‡ | 0.068 (0.031)* |
| Male × Time | −0.005 (0.012) | −0.002 (0.019) | −0.043 (0.017)* | 0.013 (0.019) |
| Education | 0.087 (0.002)‡ | 0.083 (0.003)‡ | 0.093 (0.003)‡ | 0.091 (0.003)‡ |
| Education × Time | −0.004 (0.001)‡ | −0.012 (0.002)‡ | 0.001 (0.002) | −0.002 (0.002) |
| Income | 0.039 (0.011)‡ | 0.037 (0.015)† | 0.030 (0.015)* | 0.057 (0.014)‡ |
| Income × Time | 0.003 (0.005) | −0.006 (0.008) | 0.016 (0.008)* | 0.015 (0.009) |
| Marital status | −0.033 (0.029) | −0.025 (0.040) | −0.010 (0.041) | −0.027 (0.039) |
| Marital status × Time | −0.003 (0.014) | −0.011 (0.023) | −0.028 (0.021) | 0.027 (0.024) |
| Medical conditions | −0.008 (0.008) | −0.012 (0.011) | 0.005 (0.012) | −0.013 (0.011) |
| Medical conditions × Time | 0.006 (0.004) | 0.012 (0.007) | 0.005 (0.006) | 0.001 (0.007) |
Note: aAge was centered at 72.
*p < .05. †p < .01. ‡p < .001.
After accounting for the effects of age, a different picture of cognitive change emerged. Model 2 (Table 3) shows that people who were older had lower abilities in all cognitive factors at baseline. Moreover, older age was associated with faster decline in global cognition, episodic memory, and perceptual speed—a .006 (p < .001), .004 (p < .001), and .009 (p < .001) standard score units increase in their rates of decline, respectively, for each year older. The age variation in the rate of cognitive change means that cognitive decline was less apparent in those who were younger. Model 2 indicates that for those who were 72 years old, on average, global cognition was stable (.008, p > .05) in the 2-year period, and episodic memory and perceptual speed improved at an annual rate of .036 (p < .001) and .044 (p < .001) standard score units, respectively. But regardless of age, working memory declined by .030 (p < .001) standard score units per year.
We then entered sex, education, income, marital status, and medical conditions to Model 2 and allowed each to interact with time (Model 3, Table 3), so as to examine whether and how the rates of cognitive change vary by these characteristics and health status. The results suggest that while men had higher levels of global cognition, working memory, and perceptual speed at baseline, men had faster rates of decline (.043 standard score unites more, p < .05) than women in working memory. More education was associated with better performance in all cognitive factors at baseline. But each additional year of schooling was related to a .004 (p < .001) and .012 (p < .001) standard score units increase in the rates of decline in global memory and episodic memory, respectively. People with higher income performed better in all cognitive factors at baseline, and each level up the income category was associated with .016 (p < .05) standard score units reduction in the rate of decline in working memory. Marital status and medical conditions did not have any significant effects on either baseline levels or rates of change of any cognitive factors.
Discussion
We used two waves of data to examine change of cognitive function in a 2-year period among U.S. Chinese older adults. On average, a trend of decline in multiple cognitive abilities was observed in the sample. But the average trend masks heterogeneities in the rate of cognitive change between individuals. Estimates from mixed-effects models show that age is an important factor and older age is associated with faster rates of decline in global cognition, episodic memory, and perceptual speed. While the oldest age group in this Chinese population is vulnerable to cognitive decline, the odds of decline are lower for those who are younger. But there is evidence of decline in working memory across all ages in the sample. In addition to age, education, sex, and income were found to be related to the rate of change in different cognitive abilities. Specifically, more education is associated with faster rates of decline in global cognition and episodic memory; men have faster rates of decline in working memory than women, and higher income is associated with reduction in the rate of decline in working memory.
Age variation in the rate of cognitive change is expected and consistent with prior research (2,16,17). For example, in a sample of Black and White older adults, Wilson and colleagues (2) reported the interaction effects of age and time on episodic memory and perceptual speed to be −.006 (SE = 0.001; p < .001) and −.006 (SE = 0.001; p < .001), respectively. That is, the rate of decline in both cognitive domains increased by .006 standard score units for each year older. The corresponding estimates in our analysis were −.004 (SE = 0.001; p < .001) and −.009 (SE = 0.001; p < .001). Some researchers have argued that advancing age alone is not responsible for substantial cognitive decline in a period of few years, rather, diseases such as Alzheimer’s disease is the likely culprit (16). The PINE participants were not evaluated for Alzheimer’s disease, but it is known that the risk of dementia-related diseases increases with age (18). Probably, the age differences in baseline and rates of decline in cognition reflect differential onset and progression of diseases such as cerebrovascular disease and Alzheimer’s disease (19). It is also possible that the age effects reflect cohort rather than age differences (1).
The findings that education is associated with faster rates of decline in global cognition and episodic memory seem to contradict its positive relationships with cognition at baseline. This pattern of findings, however, has been reported by prior studies (20–22). Possibly, educational differences in cognitive performance at baseline are related to life experiences that accumulated over the life course, such as early life conditions, literacy, and life course physical activity (20,21). A prior study shows that life experience variables reduced effects of education and race/ethnicity on baseline cognition considerably (19). In other words, those with limited education may have been underestimated of their true cognitive abilities at baseline and may benefit from test retaking (22). Studies have shown that ethnic minorities and those with low education show greater improvement from initial to second cognitive assessment, compared to Whites and those with more education (3,23). Nevertheless, it should be noted that the effects of education on levels of cognitive function were relatively large, attesting to the benefits of education to cognition in later life. For example, global cognition at baseline increased by .087 standard units with each additional year of education, which was much larger than the rate of decline in global cognition (.004 standard units) associated with each additional year of education. In addition, our observation only involved two assessment points spanning 2 years. A prior study that followed older adults up to 14 years found that more education is associated with slightly more cognitive decline in earlier years of follow-up but less decline in later years (22). Moreover, older Chinese Americans are diverse in their origin and history of migration. Those with the same years of completed schooling do not necessarily receive the same level of education due to variation in the quality of education.
Sex differences in baseline levels and longitudinal change of cognition also show contradictions. Men have higher scores than women in most cognitive abilities at baseline, but men have significantly faster rates of decline in working memory and are not different from women in the rate of change in other cognitive factors. A recent study also reports that older women are more resilient than their male counterpart in cognitive decline, but they found women to perform better in some cognitive domains at baseline (24). That study was based on a sample of primarily White adults (50 years and older) with mean education of 16.4 years. Gender inequality in Chinese society may render older women at disadvantages in cognitive tests (25). Income, however, has consistent cross-sectional and longitudinal effects—higher income is associated with better baseline performance and reduction in rates of decline in working memory. Access to services including early diagnosis and treatment of diseases may be a reason for the advantage of those with high incomes.
The findings have practice implications. First, many Chinese adults hold strong beliefs that cognitive decline in old age is inevitable (7,8). Our findings can be used to educate them about variability in cognitive decline and potential for cognitive improvement. Second, given the findings that rates of cognitive decline increase with age, health professionals should encourage Chinese adults in advancing age to monitor their changes in behavior and symptoms associated with decline of cognitive function. Family members of these older adults should be educated about signs of cognitive decline. If dementia is detected, health professionals should be cognizant of the stigma associated with dementia in Chinese culture and exercise cultural humility to help the patient (26). Third, income disparities in baseline cognition and cognitive decline ought to be addressed. Since education was controlled in our analysis, the income effects may reflect differences in health care access or quality of services received. It is worthwhile to explore the potential role of interventions that enable low-income Chinese adults to receive quality health services for addressing disparities in cognitive health.
This is the first study to report cognitive change in a population-based sample of Chinese older adults in the United States. Strengths of the study included a relatively large sample whose characteristics were comparable to those available from the Census, and the use of a battery of cognitive tests that allowed assessment of domain-specific cognitive performance. The battery of tests also made it possible to use a composite measure of global cognition with an extended range which helps to minimize bias from floor and ceiling effects (16). Nonetheless, the sample was recruited from an urban area in the mid-west of United States. Hence, the findings do not necessarily generalizable to other geographic areas or settings. The cognitive tests used also do not capture the full range of cognitive abilities, and clinical evaluations of cognitive impairment were lacking. In addition, the observation period in this study is relatively short. A longer follow-up will help to understand the variability in the trajectory of cognitive change in Chinese older adults.
Given the increasing diversity of the older population in the United States, there is a great and urgent need for population-based information about cognitive aging in ethnic minority populations (1). Such information can provide a basis for engaging ethnic minorities to maintain cognitive health, informing helping professionals as they interact with members of ethnic minority groups, and guiding development of programs and services to eliminate health disparities (1). To our knowledge, PINE is the only longitudinal study that has collected cognition data in a population-based sample of U.S. Chinese adults to date. The findings of the present study highlight the vulnerability of older Chinese in advancing age. The extent to which such vulnerability is related to dementia-related diseases needs further investigation. Differences in the rate of cognitive decline in different cognitive abilities by education, sex, and income were detected. Some of the effects are in opposite direction to their effects on baseline test scores, suggesting the influence of life experiences rather than diseases. More research is needed to understand factors accounting for sex, education, and income differences in initial levels and change of cognition among Chinese Americans.
Funding
L.W.L. was supported by a grant from the National Institute of Mental Health (R01 MH100298). X.D. was supported by National Institute on Aging grants (R01 AG042318, R01 MD006173, R01 CA163830, R34MH100443, R34MH100393, P20CA165588, R24MD001650, and RC4 AG039085), Paul B. Beeson Award in Aging, the Starr Foundation, American Federation for Aging Research, John A. Hartford Foundation, and the Atlantic Philanthropies.
Acknowledgment
The authors are grateful to the Community Advisory Board members for their continued effort in this project. The authors also thank Bernie Wong, Vivian Xu, and Yicklun Mo with the Chinese American Service League (CASL); Dr. David Lee with the Illinois College of Optometry; David Wu with the Pui Tak Center; Dr. Hong Liu with the Midwest Asian Health Association; Dr. Margaret Dolan with John H. Stroger Jr. Hospital; Mary Jane Welch with the Rush University Medical Center; Florence Lei with the CASL Pine Tree Council; Julia Wong with CASL Senior Housing; Dr. Jing Zhang with Asian Human Services; Marta Pereya with the Coalition of Limited English Speaking Elderly; and Mona El-Shamaa with the Asian Health Coalition.
References
- 1. Institute of Medicine. Cognitive Aging: Progress in Understanding and Opportunities for Action. Washington, DC: National Academies Press (United States); 2015. [PubMed] [Google Scholar]
- 2. Wilson RS, Capuano AW, Sytsma J, Bennett DA, Barnes LL. Cognitive aging in older Black and White persons. Psychol Aging. 2015;30:279–285. doi:10.1037/pag0000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Early DR, Widaman KF, Harvey D, et al. Demographic predictors of cognitive change in ethnically diverse older persons. Psychol Aging. 2013;28:633–645. doi:10.1037/a0031645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hoeffel EM, Rastogi S, Kim MO, Shahid H. The Asian Population: 2010. U.S. Census Bureau; 2012. http://www.census.gov/library/publications/2012/dec/c2010br-11.html Accessed September 10, 2016. [Google Scholar]
- 5. U.S. Census Bureau. American FactFinder. http://www.factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk Accessed September 10, 2016. [Google Scholar]
- 6. Gee GC, Ro A, Shariff-Marco S, Chae D. Racial discrimination and health among Asian Americans: evidence, assessment, and directions for future research. Epidemiol Rev. 2009;31:130–151. doi:10.1093/epirev/mxp009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Laditka JN, Laditka SB, Liu R, et al. Older adults’ concerns about cognitive health: commonalities and differences among six United States ethnic groups. Ageing and Society. 2011;31:1202–1228. [Google Scholar]
- 8. Liu D, Hinton L, Tran C, Hinton D, Barker JC. Reexamining the relationships among dementia, stigma, and aging in immigrant Chinese and Vietnamese family caregivers. J Cross Cult Gerontol. 2008;23:283–299. doi:10.1007/s10823-008-9075-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dong X, Wong E, Simon MA. Study design and implementation of the PINE study. J Aging Health. 2014;26:1085–1099. doi:10.1177/0898264314526620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chang ES, Dong X. A battery of tests for assessing cognitive function in U.S. Chinese older adults–findings from the PINE Study. J Gerontol A Biol Sci Med Sci. 2014;69(suppl 2):S23–S30. doi:10.1093/gerona/glu195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Simon MA, Chang ES, Rajan KB, Welch MJ, Dong X. Demographic characteristics of U.S. Chinese older adults in the Greater Chicago area: assessing the representativeness of the PINE study. J Aging Health. 2014;26:1100–1115. doi:10.1177/0898264314543472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wechsler D. Wechsler Memory Scale-Revised Manual. San Antonio: Psychological Corporation; 1987. [Google Scholar]
- 13. Smith A. Symbol Digit Modalities Test: Manual. Los Angeles: Western Psychological Services; 1982. [Google Scholar]
- 14. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. [DOI] [PubMed] [Google Scholar]
- 15. Chiu HF, Lee H, Chung W, Kwong P. Reliability and validity of the Cantonese version of mini-mental state examination-a preliminary study. J Hong Kong Coll Psychiatr. 1994;4:25. [Google Scholar]
- 16. Wilson RS, Bennett DA, Beckett LA, et al. Cognitive activity in older persons from a geographically defined population. J Gerontol B Psychol Sci Soc Sci. 1999;54:P155–P160. [DOI] [PubMed] [Google Scholar]
- 17. Korten AE, Henderson AS, Christensen H, et al. A prospective study of cognitive function in the elderly. Psychol Med. 1997;27:919–930. [DOI] [PubMed] [Google Scholar]
- 18. National Institute on Aging, Alzheimer’s Disease Education and Referral Center. Risk Factors for Dementia. https://www.nia.nih.gov/alzheimers/publication/dementias/risk-factors-dementia Accessed December 16, 2016.
- 19. Brewster PW, Melrose RJ, Marquine MJ, et al. Life experience and demographic influences on cognitive function in older adults. Neuropsychology. 2014;28:846–858. doi:10.1037/neu0000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gross AL, Mungas DM, Crane PK, et al. Effects of education and race on cognitive decline: An integrative study of generalizability versus study-specific results. Psychol Aging. 2015;30:863–880. doi:10.1037/pag0000032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jacqmin-Gadda H, Fabrigoule C, Commenges D, Dartigues JF. A 5-year longitudinal study of the Mini-Mental State Examination in normal aging. Am J Epidemiol. 1997;145:498–506. [DOI] [PubMed] [Google Scholar]
- 22. Wilson RS, Hebert LE, Scherr PA, Barnes LL, Mendes de Leon CF, Evans DA. Educational attainment and cognitive decline in old age. Neurology. 2009;72:460–465. doi:10.1212/01.wnl.0000341782.71418.6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Karlamangla AS, Miller-Martinez D, Aneshensel CS, Seeman TE, Wight RG, Chodosh J. Trajectories of cognitive function in late life in the United States: demographic and socioeconomic predictors. Am J Epidemiol. 2009;170:331–342. doi:10.1093/aje/kwp154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McCarrey AC, An Y, Kitner-Triolo MH, Ferrucci L, Resnick SM. Sex differences in cognitive trajectories in clinically normal older adults. Psychol Aging. 2016;31:166–175. doi:10.1037/pag0000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Li X. Gender inequality in China and cultural relativism. In: Nussbaum M, Glover J, eds. Women Culture, and Development: A Study of Human Capabilities. New York: Oxford University Press; 1995:407–425. [Google Scholar]
- 26. Dong X, Chang ES. Lost in translation: to our Chinese patient, Alzheimer’s meant ‘crazy and catatonic’. Health Aff (Millwood). 2014;33:712–715. doi:10.1377/hlthaff.2013.1472. [DOI] [PMC free article] [PubMed] [Google Scholar]