Abstract
Background
The purpose of this study was to determine the joint associations of sedentary time and physical activity with mobility disability in older age.
Methods
We analyzed prospective data from 134,269 participants in the National Institutes of Health (NIH)—American Association of Retired Persons (NIH-AARP) Diet and Health Study between 1995–1996 and 2004–2005. Total sitting time (h/d), TV viewing time (h/d) and light- and moderate-to-vigorous-intensity physical activity (h/wk) were self-reported at baseline, and mobility disability at follow-up was defined as being “unable to walk” or having an “easy usual walking pace (<2 mph).” Multivariable logistic regression determined the independent and joint associations of sedentary time and total physical activity with the odds of disability.
Results
Among the most active participants (>7 h/wk), sitting <6 h/d was not related to excess disability at follow-up, and those in the most active group reporting the highest level of sitting time (≥7 h/d) still had a significantly lower odds (odds ratios = 1.11; 95% confidence interval = 1.02, 1.20) compared with those reporting the lowest level of sitting (<3 h/d) in the least active group (≤3 h/wk; odds ratios = 2.07; 95% confidence interval = 1.92, 2.23). Greater TV time was significantly related to increased disability within all levels of physical activity.
Conclusions
Reduction of sedentary time, combined with increased physical activity may be necessary to maintain function in older age.
Keywords: Exercise, Epidemiology, Functional performance
The modern-day lifestyle is characterized by a majority of time spent sitting and reclining throughout the day. Older people may spend up to 60%–70% (10–11 h/d) of their waking hours sitting or reclining (1), and may be more susceptible to the detrimental effects of sedentary time compared with younger or middle-aged people, due to a loss of physiologic reserve. The relationship between physical inactivity and risk of mobility loss, frailty, and early mortality has been well established in the literature (2–4); however, less is known about the independent hazards of sedentary time on health and function in older age. A recent cross-sectional study using the U.S. National Health and Nutrition Examination Survey (NHANES) data from 2003 to 2006 suggests that even meeting moderate-to vigorous–intensity physical activity guidelines (≥150 min/wk) was not sufficient to ameliorate the negative association between extended sedentary time and activities of daily living disability risk among older people living in the United States (5). There is also now evidence that the deleterious associations often reported between sedentary time and chronic disease risk may be attributable to the fact that sedentary time displaces time spent in health-accruing lower-intensity activity (6); however, most previous analyses have adjusted only for moderate-to-vigorous–intensity activity, rather than for total physical activity. In addition, many studies of sedentary behavior, physical activity, and mobility disability in older people are cross-sectional in design, which limits our ability to makes causal inferences.
We are not aware of any prospective investigations that have considered the independent and joint associations of sedentary behavior and total physical activity with mobility disability. Moreover, it is not clear what level of physical activity is necessary to minimize the deleterious effects of large amounts of sitting on mobility disability in older people. Accordingly, we analyzed prospective data from 134,269 participants in the National Institutes of Health (NIH)—American Association of Retired Persons (AARP) Diet and Health Study between 1995–1996 and 2004–2005. We hypothesized that self-reported daily sedentary time at baseline would significantly increase the odds of self-reported mobility disability at follow-up, independent of baseline levels of light-, moderate-, and vigorous-intensity physical activity. We further proposed that this excess disability would be accelerated among those with the highest levels of sedentary time and the lowest levels of physical activity.
Methods
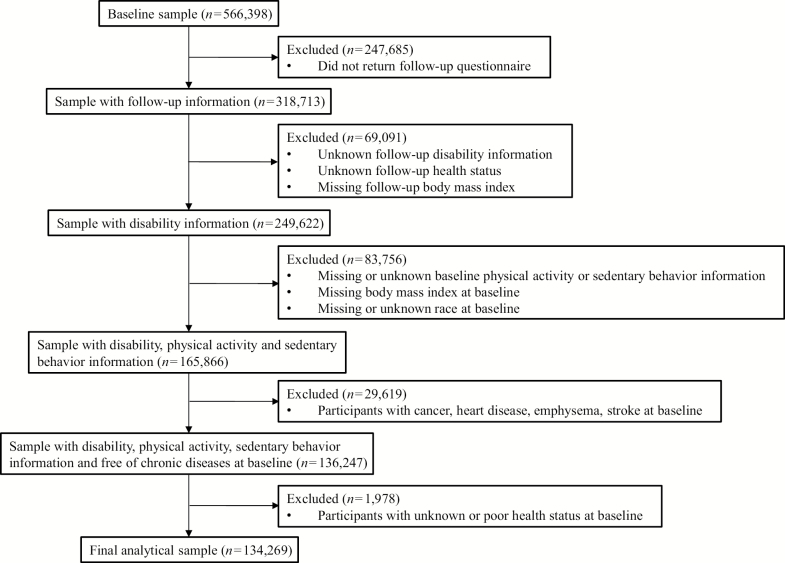
The NIH-AARP Diet and Health Study was established in 1995–1996 and comprised 566,398 AARP members (50–71 years) in six states and two metropolitan areas who responded to a questionnaire about their medical history, diet, physical activity, and sedentary behaviors (7). A follow-up questionnaire was completed in 2004–2006 by 318,714 participants. Those respondents who provided complete data on both questionnaires and who were free of chronic disease (eg, diabetes, heart disease, emphysema, cancer, or stroke) at baseline were eligible to be included in the analysis. To ensure the healthiest cohort possible, we also only included people who reported their health status as fair or better (N = 134,269; Figure 1).
Figure 1.
Participant selection from the National Institutes of Health—American Association of Retired Persons (NIH-AARP) Diet and Health Study cohort. Those respondents who provided complete data on both questionnaires and who were free of chronic disease (eg, diabetes, heart disease, emphysema, cancer, or stroke) at baseline were eligible to be included in the analysis. To ensure the healthiest cohort possible, we also only included people who reported their health status as fair or better at baseline (N= 134,269).
Assessment of Primary Study Variables
Sedentary time typical of a 24-h period during the past 12 months was assessed in the risk factor questionnaire at baseline in two ways: (a) time spent sedentary (sitting, TV watching, computer time, napping; <3, 3–4, 4–7, and ≥7 h/d) and (b) time spent watching TV (0–2, 3–4, and ≥5 h/d). Participants were also asked about the typical amount of time per week spent in light-intensity (eg, housework, walking, shopping) and in moderate-to-vigorous–intensity (eg, brisk walking, yard work, jogging) physical activity over the past 10 years (<1, 1–3, 4–7, and >7 h/wk). Physical activity and sedentary time questions from the risk factor questionnaire were not validated directly, but they have demonstrated expected associations with colon, rectal, and endometrial cancer risk and mortality in this cohort (8–10). Also, to quantify the level of multicollinearity among the physical activity and sedentary time variables, we generated variance infiltration factors using least squares regression modeling. The variance infiltration factor values for total sitting, light, and moderate-to-vigorous intensity were 1.05, 1.27, and 1.28, respectively, whereas the variance infiltration factor values for TV time, light, and moderate-to-vigorous intensity were 1.09, 1.27, and 1.26, respectively. In general, a variance infiltration factor < 2.0 indicates low collinearity among variables. Mobility status at the 2004–2005 follow-up was assessed by a question about normal walking pace (unable to walk; easy [<2 mph]; normal [2–2.9 mph]; brisk [3–3.9 mph]; very brisk [≥4 mph]). Mobility disability was defined as a response of “unable to walk” or “easy (<2 mph).”
Statistical Analysis
Univariate analyses (means ± SD, frequencies [%]) first were generated on all study variables in order to determine their distributions within the study population. We assessed collinearity and associations among the study variables using correlation and chi-square tests. Given our fixed cohort with little variation in follow-up time, we used logistic regression to evaluate the simple associations of each study variable and covariable on the odds of mobility disability. Multivariable logistic regression models were then used to determine associations between sedentary time and mobility disability when adjusting for light-intensity and moderate-to-vigorous–intensity physical activity, as well as for the covariables age at entry, sex, race, level of educational attainment, change in body mass index (kilogram per square meter) between baseline and follow-up, baseline smoking status, and self-reported health at follow-up. These covariables were chosen based on their associations with mobility disability in the simple analysis. Total sedentary time and TV viewing time were entered into separate multivariable models.
In order to determine the joint effects of sedentary behavior and physical activity on disability risk, categorical scores for light activity were added to scores of moderate-to-vigorous–intensity physical activity to create a total physical activity variable with scores ranging from 0 to 6. Total physical activity score was then divided into tertiles based on its distribution (0 = >7, 1 = 4–7, and 2 = ≤3 h/wk). We tested the joint effects of sedentary time (0 = <3, 1 = 3–4, 2 = 5–6, and 3 = ≥7 h/d) within each tertile of total physical activity on mobility disability by creating 12 indicator variables. This allowed us to compare directly groups with varying amounts of sedentary time and physical activity against those who sat the least and also had the most physical activity (referent group). All multivariable models were adjusted for age, sex, race, level of educational attainment, smoking, change in body mass index, as well as for reported health status at follow-up. These analyses then were repeated using categories of TV viewing time as the indicator of sedentary behavior. We also conducted a sensitivity analysis in which we defined mobility disability only by a response of “unable to walk” (n = 3,009) to determine whether any misclassification of mobility status may have affected our findings. Odds ratios (OR) and 95% confidence intervals (CI) are reported from the final logistic regression models to describe the excess odds of mobility disability within each level of sedentary time and physical activity relative to the referent group.
Results
Participants were followed for an average of 8.6 ± 0.42 years, and the average age at entry was 61.2 ± 5.3 years. Approximately 43% of the NIH-AARP cohort were women, 94% were white, and nearly 45% had a college degree. Twenty-nine percent (n = 38,798) of the participants reported mobility disability at follow-up. As indicated in Table 1, women, as well as those who reported lower educational attainment, poorer self-reported health at baseline and follow-up, and smoking at baseline, were significantly more likely to report mobility disability at follow-up (p < .001). Also, baseline body mass index was significantly higher in those reporting mobility disability compared with those who did not (p < .001). Baseline levels of light-intensity and moderate-to-vigorous–intensity physical activity, as well as time per day spent sitting or watching TV were significantly associated with reported mobility disability at follow-up (p < .001; Table 2), and these simple associations appeared stronger for moderate-to-vigorous activity and for TV viewing compared with light-intensity physical activity and total sitting time.
Table 1.
Demographic Characteristics of the NIH-AARP Diet and Health Study Cohort (N = 134,269)
| Variable | All | Mobility Disability (n = 38,798) | No Mobility Disability (n = 95,471) | p Value |
|---|---|---|---|---|
| Age at entry (y) | 61.2 ± 5.3 | 62.4 ± 5.2 | 60.7 ± 5.3 | <.001 |
| Sex (% female) | 43.18 | 58.00 | 37.16 | <.001 |
| Race (%) | <.001 | |||
| White | 94.27 | 92.32 | 95.06 | |
| Black | 2.87 | 4.47 | 2.22 | |
| Hispanic | 1.54 | 1.90 | 1.40 | |
| Other | 1.32 | 1.31 | 1.32 | |
| Education (%) | <.001 | |||
| High school or below | 22.86 | 33.97 | 18.35 | |
| Post-high school training/some college | 32.75 | 35.17 | 31.77 | |
| College or above | 44.38 | 30.86 | 49.88 | |
| Baseline health status (%) | <.001 | |||
| Fair | 5.30 | 11.21 | 2.89 | |
| Good | 30.85 | 42.12 | 26.27 | |
| Very good | 41.19 | 35.08 | 43.68 | |
| Excellent | 22.66 | 11.60 | 27.15 | |
| Smoking status (%) | 9.57 | 14.09 | 7.74 | <.001 |
| BMI (kg/m2) | 26.8 ± 4.8 | 28.5 ± 5.9 | 26.1 ± 4.1 | <.001 |
| Follow-up health status (%) | <.001 | |||
| Poor | 1.22 | 3.53 | 0.28 | |
| Fair | 9.35 | 20.45 | 4.84 | |
| Good | 33.58 | 43.69 | 29.47 | |
| Very good | 40.09 | 26.87 | 45.46 | |
| Excellent | 15.77 | 5.47 | 19.96 |
Note: BMI = body mass index; NIH-AARP = National Institutes of Health—American Association of Retired Persons. Data are all self-reported from the baseline (1994–1995) questionnaire with the exception of follow-up health status, which was reported in 2004–2005.
Table 2.
Categories of Light-Intensity and Moderate-to-Vigorous–Intensity Physical Activity and Sedentary Time According to Mobility Disability Status in the NIH-AARP Diet and Health Study Cohort (N= 134,269)
| Variable | Mobility Disability (n = 38,798) | No Mobility Disability (n = 95,471) | p Value |
|---|---|---|---|
| Light activity in past 10 y (%) | <.001 | ||
| <1 h/wk | 16.90 | 13.76 | |
| 1–3 h/wk | 24.40 | 23.18 | |
| 4–7 h/wk | 26.20 | 27.97 | |
| >7 h/wk | 32.50 | 35.08 | |
| MVPA in past 10 y (%) | <.001 | ||
| <1 h/wk | 33.33 | 18.36 | |
| 1–3 h/wk | 26.23 | 25.29 | |
| 4–7 h/wk | 21.69 | 28.66 | |
| >7 h/wk | 18.75 | 27.70 | |
| Sitting per day in past 12 mo (%) | .043 | ||
| <3 h | 19.92 | 19.37 | |
| 3–4 h | 28.78 | 28.77 | |
| 5–6 h | 27.46 | 28.07 | |
| ≥7 h | 23.85 | 23.79 | |
| TV viewing per day in past 12 mo (%) | <.001 | ||
| 0–2 h | 27.81 | 42.58 | |
| 3–4 h | 45.80 | 43.00 | |
| >5 h | 26.39 | 14.41 |
Note: MVPA = moderate-to-vigorous intensity physical activity; NIH-AARP = National Institutes of Health—American Association of Retired Persons. All physical activity and sedentary time were self-reported at baseline (1994–1995). Mobility disability was defined as a self-reported walking speed of “unable to walk” or “easy (<2 mph)” at the follow-up (2004–2005).
Multivariable parameter estimates for the associations of sedentary time and of TV time with mobility disability are shown in Table 3. After adjustment for light-intensity and moderate-to-vigorous–intensity physical activity, as well as for the covariables of interest, the independent relationship of total sedentary time to mobility disability was almost negligible (Model 1). On the other hand, disability increased in a dose-response manner with increasing category of TV time (Model 2). Participants reporting 3–4 h/d of TV viewing experienced a 25% higher odds of mobility disability compared with those reporting ≤2 h/d (referent group), whereas those people reporting ≥5 h/d had a 65% higher odds. These findings also were not affected by race, education, change in body mass index, smoking, or self-reported health status at follow-up. In both of these models, the odds of mobility disability was progressively lower with increasing frequency and intensity of physical activity (Table 3), independent of sitting or TV time and the remaining covariables. When we removed physical activity from these models, the results were relatively unchanged (Supplementary Table 1). Also, when we repeated these analyses defining mobility disability only by a response of “unable to walk,” we observed even stronger effect sizes.
Table 3.
The Independent Associations of Sedentary Time and Physical Activity With Mobility Disability in the NIH-AARP Diet and Health Study Cohort (N= 134,269)
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Sedentary behaviors | ||||||
| Sitting (h/d) | ||||||
| 0–3 h | 1.00 | |||||
| 3–4 h | 0.94 | 0.902, 0.975 | .001 | |||
| 5–6 h | 0.96 | 0.919, 0.994 | .026 | |||
| ≥7 h | 1.04 | 0.998, 1.084 | .064 | |||
| TV/videos watching (h/d) | ||||||
| 0–2 h | 1.00 | |||||
| 3–4 h | 1.25 | 1.215, 1.293 | <.001 | |||
| ≥5 h | 1.65 | 1.587, 1.713 | <.001 | |||
| Light activity | ||||||
| <1 h/wk | 1.00 | 1.00 | ||||
| 1–3 h/wk | 0.87 | 0.829, 0.907 | <.001 | 0.86 | 0.826, 0.904 | <.001 |
| 4–7 h/wk | 0.80 | 0.766, 0.839 | <.001 | 0.80 | 0.759, 0.831 | <.001 |
| >7 h/wk | 0.83 | 0.790, 0.866 | <.001 | 0.82 | 0.781, 0.857 | <.001 |
| Moderate/vigorous activity | ||||||
| <1 h/wk | 1.00 | 1.00 | ||||
| 1–3 h/wk | 0.65 | 0.626, 0.675 | <.001 | 0.66 | 0.632, 0.682 | <.001 |
| 4–7 h/wk | 0.50 | 0.476, 0.515 | <.001 | 0.50 | 0.484, 0.523 | <.001 |
| >7 h/wk | 0.43 | 0.411, 0.449 | <.001 | 0.44 | 0.418, 0.456 | <.001 |
| Race | ||||||
| White | 1.00 | |||||
| Black | 1.47 | 1.365, 1.581 | <.001 | 1.38 | 1.279, 1.483 | <.001 |
| Hispanic | 1.30 | 1.172, 1.439 | <.001 | 1.32 | 1.187, 1.458 | <.001 |
| Other | 1.09 | 0.969, 1.222 | .155 | 1.09 | 0.969, 1.223 | .152 |
| Education | ||||||
| ≤HS | 1.00 | 1.00 | ||||
| Post-HS or some college | 0.69 | 0.664, 0.711 | <.001 | 0.71 | 0.686, 0.734 | <.001 |
| College and above | 0.49 | 0.478, 0.511 | <.001 | 0.54 | 0.519, 0.556 | <.001 |
| BMI change | 1.02 | 1.011, 1.020 | <.001 | 1.02 | 1.012, 1.021 | <.001 |
| Current smoker | 1.58 | 1.516, 1.650 | <.001 | 1.53 | 1.467, 1.598 | <.001 |
| Self-reported health at follow-up | ||||||
| Poor | 1.00 | 1.00 | ||||
| Fair | 0.31 | 0.272, 0.361 | <.001 | 0.31 | 0.272, 0.362 | <.001 |
| Good | 0.11 | 0.099, 0.131 | <.001 | 0.12 | 0.100, 0.132 | <.001 |
| Very good | 0.05 | 0.044, 0.058 | <.001 | 0.05 | 0.046, 0.060 | <.001 |
| Excellent | 0.03 | 0.024, 0.032 | <.001 | 0.03 | 0.025, 0.033 | <.001 |
Note: BMI = body mass index; CI = confidence intervals; HS = high school; NIH-AARP = National Institutes of Health—American Association of Retired Persons; OR = odds ratios. Data are from multivariable logistic regression modeling. Total sitting time and TV viewing time were entered into separate models. OR and 95% CI are reported to describe the excess risk of disability for each level of sedentary behavior and each level of light-intensity and moderate-to-vigorous–intensity physical activity relative to the referent group (<3 h/d for sitting; <2 h/d for TV viewing; and <1 h/wk for physical activity).
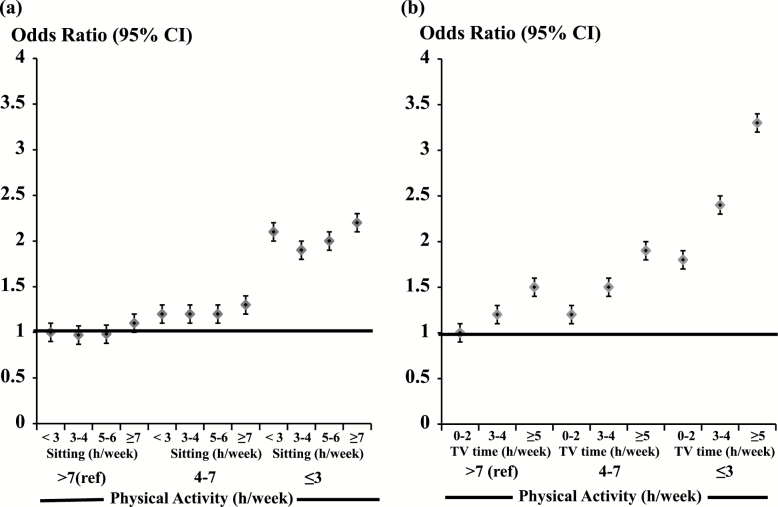
The OR for the joint associations of total sedentary time and total physical activity with mobility disability are shown in Figure 2a. We observed a dose–response association between increasing levels of sitting time in combination with decreasing levels of physical activity and mobility disability at follow-up. Indeed, compared with the referent group (those reporting <3 h/d of sitting and in the most active tertile [>7 h/wk]), those reporting the most sitting time (≥7 h/d) and the lowest levels of physical activity (≤3 h/wk) had over a twofold higher odds of mobility disability (OR = 2.17; 95% CI = 2.03, 2.32). Those people reporting the highest level of sitting time who reported 4–7 h/wk of physical activity had a 34% higher odds (OR = 1.34; 95% CI = 1.25, 1.43) compared with the referent group, whereas those reporting the highest level of sitting but who were the most physically active (>7 h/wk) had excess odds of 11% (OR = 1.11; 95% CI = 1.02, 1.20). Among those in the most active tertile, sitting ≤6 h/d was not related to excess mobility disability and those in the most active group who reported the highest level of sitting time still had a markedly lower excess odds (OR = 1.11; 95% CI = 1.02, 1.20) compared with the referent group than did those reporting the lowest level of sitting in the least active group (OR = 2.07; 95% CI = 1.92, 2.23). We observed no statistically significant interaction between sitting time and total physical activity (Wald χ2 = 2.71; df = 6; p > .05), however.
Figure 2.
The joint association between daily sedentary time (h/d; a) or TV viewing time (h/d; b) and total physical activity (h/wk) on mobility disability in the National Institutes of Health—American Association of Retired Persons (NIH-AARP) Diet and Health Study cohort (N= 134,269). This joint analysis allowed us to compare directly groups with varying amounts of sedentary time and physical activity against those who sat the least and also had the most physical activity (referent group). Odds ratios (OR) and 95% confidence intervals (CI) are reported from the final logistic regression models to describe the excess odds of mobility disability within each level of sedentary time and physical activity relative to the referent group. All models were adjusted for age, sex, race, level of educational attainment, smoking, change in body mass index, as well as for reported health status at follow-up.
When we repeated these analyses using TV time, the results were even stronger (Figure 2b). Within all levels of physical activity, increasing amounts of TV time increased the odds of mobility disability in a dose–response manner, with almost a curvilinear accelerated odds of disability observed with increasing TV time in combination with the lowest levels of physical activity. Those people reporting the greatest amount of TV time (≥5 h/d) within the lowest tertile of physical activity experienced over a threefold increase in odds of mobility disability (OR = 3.31; 95% CI = 3.10, 3.53) relative to the referent group (0–2 h/d of TV time) in the most active tertile, and the odds of disability with ≥5 h/d of TV time among those reporting 4–7 h/wk of physical activity (OR = 1.94; 95% CI = 1.82, 2.08) was nearly similar to that of those watching the least amount of TV, but who were also the least active (OR = 1.83; 95% CI = 1.73, 1.94). In this latter model, we observed a significant statistical interaction between TV viewing time and total physical activity (Wald χ2 = 14.1; df = 4; p < .01) indicating that the association between TV time and mobility disability varied substantially by level of physical activity.
Discussion
Our findings indicate that sedentary time is a potent risk factor for mobility loss in older age that is independent of light-intensity and moderate-to-vigorous–intensity physical activity, as well as sex, educational attainment, smoking, and prevailing health status. Among those people reporting ≥7 h/wk of physical activity, there was no significant association between sitting up to 6 h/d and mobility disability, suggesting that higher levels of physical activity can mitigate some of the deleterious effects of prolonged sitting in older age. In contrast, increased TV time was significantly associated with increased mobility disability at follow-up within all levels of reported physical activity—and this was especially so in the least active participants.
This prominence of sedentary living has been especially evident over the last several decades, as occupational-related energy expenditure has declined (11) and passive leisure-time activity (internet use, video games, television/movie viewing) has increased. Several recent studies now confirm the deleterious association between prolonged (ie, uninterrupted) periods of daily sitting and cardiometabolic risk (12–15), as well as all-cause, cardiovascular, and cancer mortality (16–19)—even after adjustment for leisure-time physical activity (which has not changed substantially over the past decades) (20). Recent evidence from a large population-based study (21) suggest that compared with older people who maintained a sedentary lifestyle (ie, >7 h of sitting/day), those who reduced their daily sitting time by 3 h/d reduced their 8-year odds of mortality by 14% (hazard ratio = 0.86 [0.70–1.05]), whereas those who maintained ≤3 h/d of sitting reduced their odds by 25% (hazard ratio = 0.75 [0.62–0.90]), independent of reported physical activity level.
Our findings corroborate those of other studies reporting sedentary behavior to be a risk factor for loss of physical function that is distinct from level of moderate-to-vigorous–intensity physical activity (5,15,22–25). Reid and colleagues (25) studied 12-year trajectories of TV viewing time in older adults participating in the Australian Diabetes, Obesity, and Life-style (Aus/Diab) Study between 1999/2002; 2004/2005; and 2011/2012. Their findings indicated that those with either a consistently low or a low, but increasing pattern of TV viewing had significantly greater knee extensor strength at follow-up, compared with those having a moderate, but increasing viewing pattern. Moreover, two recent cross-sectional studies using NHANES data from 2003 to 2006 suggest that even meeting moderate-to-vigorous–intensity physical activity guidelines (≥150 min/wk) was not sufficient to ameliorate the negative association between extended sedentary time and self-reported physical function (15) and activities of daily living disability (5), among older people living in the United States. Our findings are also consistent with these studies in that the excess mobility disability observed with prolonged sitting disappeared only with >7 h/wk (ie, 420 min/wk) of total activity. Although light-intensity (as well as moderate-to-vigorous intensity) physical activity was included in our measure, this amount of weekly activity is nearly three times greater than the current U.S. Physical Activity Guidelines.
Recent evidence suggests that the deleterious impact of prolonged sedentary time on chronic disease risk may be attributable to the fact that sedentary time displaces time spent in health-accruing, lower-intensity physical activity (6,26) and that when low-intensity activity is included in the analysis along with moderate-to-vigorous–intensity activity, the disease risk associated with sedentary behavior diminishes (6). We included light-intensity, as well as moderate-to-vigorous–intensity activity, in our modeling and also observed that the association between total sedentary time and mobility disability was negligible; however, TV viewing time continued to demonstrate an independent, graded association. Also, implicit in the displacement hypothesis is that replacing sitting time with some type of physical activity would be associated with lower disease risk. Using an isotemporal modeling approach, Matthews and colleagues (27) recently reported a 30% reduction in mortality risk among older people who were the least active (<2 h/d of total activity) when 1 h/d of sitting was replaced with an equal amount of nonexercise activity, such as walking, gardening, or household chores. These findings underscore the important contributions of light-intensity physical activity to health and function in older age.
To our knowledge, this is the first prospective study to consider the joint associations of sitting time and total physical activity with mobility disability. A recent cross-sectional study of over 4000 community-living older people reported that each additional hour of sitting time was significantly associated with a lower timed walking speed, but this was only evident among those in the lowest quartile of moderate-to-vigorous–intensity physical activity (<19.5 min/d) (28). Ekelund and colleagues (29) report findings similar to ours with regard to the joint associations of physical activity and sitting time with all-cause mortality. Indeed, this harmonized meta-analysis of prospective data from over one million men and women indicated a dose-response relation, with accelerated mortality risk observed among those reporting increasing amounts of sitting time in combination with low levels of physical activity. These authors and others (18,26,30,31) also reported a stronger magnitude of effect with TV viewing time compared with total sitting time, which may be due to the greater accuracy of reporting structured television viewing. Alternatively, people may break up their sitting time more frequently during the day compared with when watching TV in the evening (30), and in our older study population, the effects of this on mobility disability were striking. It is also possible that the combination of high levels of TV time with low levels of physical activity is a marker of underlying chronic disease; however, we controlled for self-reported health status at follow-up and still observed excess mobility disability.
A major strength of this article is the prospective nature of the analysis. Other analyses of sedentary time, physical activity, and mobility disability have been cross-sectional in design, thereby precluding the ability to establish the temporal sequencing between exposure and outcome in order to infer causality. Also, few studies have considered the role of sedentary time on disease status while controlling for total physical activity, and we are the first to also consider the joint associations of sitting time and physical activity with mobility disability.
We also note the limitations to our analysis. All information on sedentary behavior, physical activity, and mobility disability were self-reported. People tend to under-report their sedentary behavior and over-report their physical activity (32); however, we expect the misclassification of sedentary time and physical activity to be nondifferential by mobility disability status, thus attenuating our findings toward the null. Also, the top response categories for questions on sedentary time (≥7 h/d) and for light physical activity (>7 h/wk) more than likely underestimated the full extent of these actual behaviors over the course of a day, and this may have minimized the true associations between the highest possible amounts of sitting and light physical activity to mobility disability. It is also important to note that sitting and activity behaviors are interdependent, as time in one displaces time in another over a finite 24-hour day. Compositional data analysis techniques and isotemporal modeling may be stronger statistical methods to capture how shifts in the relative amounts of sitting, light-intensity, and moderate-to-vigorous–intensity physical activity over the course of the day affect health. Unfortunately, the categorical responses to questions about sedentary time and physical activity on the NIH-AARP risk factor questionnaire cannot adequately capture the data needed for the appropriate application of such analytic techniques. Finally, scores for the frequency of light and moderate-to-vigorous physical activity were added together to create a summary index ranging from 0 to 6. Similar to other composite scores (eg, MET-h/wk) it, therefore, was not possible to discern the distinct contributions of light, moderate, or vigorous intensity to a given summary score.
Mobility disability status was not assessed by the baseline risk factor questionnaire, and even though we restricted the analysis to those without chronic disease and who reported their health as fair or better, we may have missed some prevalent cases of mobility disability at baseline. Those with existing disability probably reported more sedentary time and less physical activity at baseline, which could have artificially inflated the magnitude of the associations between these behaviors and mobility disability at follow-up—even after adjustment for prevailing health status. Unfortunately, we have no way of determining the extent of any misclassification of baseline mobility status. Also, the question assessing mobility was based on perceived usual walking pace and may have lacked accuracy. The Walking Impairment Questionnaire (WIQ) (33) was developed as a measure of self-perceived walking performance and contains questions about walking speed that are similar to ours. Scores for perceived walking speed from the WIQ correlated significantly with timed walking speed in a sample of older people with and without peripheral artery disease, thereby providing evidence of the validity of this questionnaire (33).
Our findings are based on only 24% of the original NIH-AARP cohort and 94% of this sample was white and of higher educational attainment. Although the sample size was still adequate to ensure the precision of our estimates, it is not clear how generalizable these findings are to the U.S. population of older adults—especially to minority or to less affluent older populations.
In sum, our findings and those of others indicate that reductions in sedentary time, as well as increases in physical activity, are necessary to maintain health and function in older age—particularly among those who are the least active. Current U.S. public health recommendations for physical activity have not addressed sedentary time, but our results suggest doing so may be useful for reducing mobility disability. Given aging demographics and the global economic burden associated with aging- and disuse-related disability, there is a tremendous public health benefit to understanding the extent to which those determinants of mobility disability can be modified in older age.
Supplementary Material
Supplementary data is available at The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences online.
Funding
This work was supported, in part, by the Intramural Research Program of the U.S. National Institutes of Health, National Cancer Institute.
Supplementary Material
Acknowledgments
We are grateful to the participants in the NIH-AARP Diet and Health Study for their outstanding cooperation.
Conflict of Interest
None reported.
References
- 1. Matthews CE, Chen KY, Freedson PS et al. . Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–881. doi:10.1093/aje/kwm390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi:10.1056/NEJM199503023320902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. American College of Sports Medicine. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41:1510–1530. [DOI] [PubMed] [Google Scholar]
- 4. DiPietro L. Physical activity in aging: changes in patterns and their relations to health and function. J Gerontol A Biol Sci Med Sci. 2001;56:1–10. doi:10.1093/gerona/56.suppl_2.13 [DOI] [PubMed] [Google Scholar]
- 5. Dunlop DD, Song J, Arnston EK et al. . Sedentary time in US older adults associated with disability in activities of daily living independent of physical activity. J Phys Act Health. 2015;12:93–101. doi:10.1123/jpah.2013-0311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Maher C, Olds T, Mire E, Katzmarzyk PT. Reconsidering the sedentary behavior paradigm. PLoS ONE. 2014;9:e86403. doi:10.1371/journal.pone.0086403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Schatzkin A, Subar AF, Thompson FE et al. . Design and serendipity in establishing a large cohort with wide dietary intake distributions: the National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol. 2001;154:1119–1125. doi:10.1093/aje/154.12.1119 [DOI] [PubMed] [Google Scholar]
- 8. Gierach GL, Chang SC, Brinton LA et al. . Physical activity, sedentary behavior, and endometrial cancer risk in the NIH-AARP Diet and Health Study. Int J Cancer. 2009;124:2139–2147. doi:10.1002/ijc.24059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Howard RA, Freedman DM, Park Y, Hollenbeck A, Schatzkin A, Leitzmann MF. Physical activity, sedentary behavior, and the risk of colon and rectal cancer in the NIH-AARP Diet and Health Study. Cancer Causes Control. 2008;19:939–953. doi:10.1007/s10552-008-9159-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Arem H, Pfeiffer RM, Engels EA et al. . Pre- and postdiagnosis physical activity, television viewing, and mortality among patients with colorectal cancer in the National Institutes of Health-AARP Diet and Health Study. J Clin Oncol. 2015;33:180–188. doi:10.1200/JCO.2014.58.1355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Church TS, Thomas DM, Tudor-Locke C et al. . Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS One. 2011;6:e19657. doi:10.1371/journal.pone.0019657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Proper KI, Singh AS, van Mechelen W, Chinapaw MJ. Sedentary behaviors and health outcomes among adults: a systematic review of prospective studies. Am J Prev Med. 2011;40:174–182. doi:10.1016/j.amepre.2010.10.015 [DOI] [PubMed] [Google Scholar]
- 13. Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol. 2003;551:673–682. doi:10.1113/jphysiol.2003.045591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Healy GN, Dunstan DW, Salmon J, Shaw JE, Zimmet PZ, Owen N. Television time and continuous metabolic risk in physically active adults. Med Sci Sports Exerc. 2008;40:639–645. doi:10.1249/MSS.0b013e3181607421 [DOI] [PubMed] [Google Scholar]
- 15. Gennuso KP, Gangnon RE, Matthews CE, Thraen-Borowski KM, Colbert LH. Sedentary behavior, physical activity, and markers of health in older adults. Med Sci Sports Exerc. 2013;45:1493–1500. doi:10.1249/MSS.0b013e318288a1e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41:998–1005. doi:10.1249/MSS.0b013e3181930355 [DOI] [PubMed] [Google Scholar]
- 17. Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996–2011. Am J Prev Med. 2011;41:207–215. doi:10.1016/j.amepre.2011.05.004 [DOI] [PubMed] [Google Scholar]
- 18. van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med. 2012;172:494–500. doi:10.1001/archinternmed.2011.2174 [DOI] [PubMed] [Google Scholar]
- 19. Patel AV, Bernstein L, Deka A et al. . Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol. 2010;172:419–429. doi:10.1093/aje/kwq155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Centers for Disease Control. Trends in Leisure-time Physical Activity in the United States: BRFSS, 2001–2007. http://www.cdc.gov/physicalactivity/data/surveillance.html 2013. Accessed January 23, 2017. [Google Scholar]
- 21. León-Muñoz LM, Martínez-Gómez D, Balboa-Castillo T, López-García E, Guallar-Castillón P, Rodríguez-Artalejo F. Continued sedentariness, change in sitting time, and mortality in older adults. Med Sci Sports Exerc. 2013;45:1501–1507. doi:10.1249/MSS.0b013e3182897e87 [DOI] [PubMed] [Google Scholar]
- 22. Santos DA, Silva AM, Baptista F et al. . Sedentary behavior and physical activity are independently related to functional fitness in older adults. Exp Gerontol. 2012;47:908–912. doi:10.1016/j.exger.2012.07.011 [DOI] [PubMed] [Google Scholar]
- 23. Sequin R, Lamonte T, Tinker L et al. . Sedentary behavior and physical function decline in older women: findings from the Women’s Health Initiative. J Aging Res. 2012;2012:271589 doi:10.1155/2012/ 271589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rosenberg DE, Bellettiere J, Gardiner PA, Villarreal VN, Crist K, Kerr J. Independent associations between sedentary behaviors and mental, cognitive, physical, and functional health among older adults in retirement communities. J Gerontol A Biol Sci Med Sci. 2016;71:78–83. doi:10.1093/gerona/glv103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Reid N, Healy GN, Daly RM et al. . Twelve-year television viewing time trajectories and physical function in older adults. Med Sci Sports Exerc. 2017;49:1359–1365. doi:10.1249/MSS.0000000000001243 [DOI] [PubMed] [Google Scholar]
- 26. Matthews CE, George SM, Moore SC et al. . Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95:437–445. doi:10.3945/ajcn.111.019620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Matthews CE, Moore SC, Sampson J et al. . Mortality benefits for replacing sitting time with different physical activities. Med Sci Sports Exerc. 2015;47:1833–1840. doi:10.1249/MSS.0000000000000621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Keevil VL, Cooper AJ, Wijndaele K et al. . Objective sedentary time, moderate-to-vigorous physical activity, and physical capability in a British cohort. Med Sci Sports Exerc. 2016;48:421–429. doi10.1249/MSS.0000000000000785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ekelund U, Steene-Johannessen J, Brown WJ et al. . Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonized meta-analysis of data from more than 1 million men and women. Lancet. 2016;388:1302–10. doi:10.1016/S0140-6736(16)30370-1 [DOI] [PubMed] [Google Scholar]
- 30. Kim Y, Wilkens LR, Park SY, Goodman MT, Monroe KR, Kolonel LN. Association between various sedentary behaviours and all-cause, cardiovascular disease and cancer mortality: the Multiethnic Cohort Study. Int J Epidemiol. 2013;42:1040–1056. doi:10.1093/ije/dyt108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wijndaele K, Brage S, Besson H et al. . Television viewing time independently predicts all-cause and cardiovascular mortality: the EPIC Norfolk study. Int J Epidemiol. 2011;40:150–159. doi:10.1093/ije/dyq105 [DOI] [PubMed] [Google Scholar]
- 32. Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71(suppl 2):S1–S14. doi:10.1080/02701367.2000.11082780 [PubMed] [Google Scholar]
- 33. McDermott MM, Liu K, Guralnik JM, Martin GJ, Criqui MH, Greenland P. Measurement of walking endurance and walking velocity with questionnaire: validation of the walking impairment questionnaire in men and women with peripheral arterial disease. J Vasc Surg. 1998;28:1072–1081. doi:10.1016/S0741-5214(98)70034-5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.