Abstract
Background
Frequent complaints of pain (FCP) are common in high-income countries, affecting about 25% of children, and may have significant adverse consequences including prolonged school absence and disability. Most FCP are unexplained, and the aetiology is poorly understood. This study aimed to identify risk factors for FCP and explore how risk factors explain variation in pain reporting by childhood socioeconomic conditions (SECs).
Methods
Analysis of the UK Millennium Cohort Study, including 8463 singleton children whose parents provided data throughout the study. At 11 years, mothers were asked whether their child frequently complains of pain. Risk ratios (RR) and 95% CIs for FCP were estimated using Poisson regression, according to maternal education. Other risk factors were explored to assess if they attenuated any association between FCP and SECs.
Results
32.3% of children frequently complained of pain. Children of mothers with no educational qualifications were more likely to have FCP than children of mothers with higher degrees (RR 2.06, 95% CI 1.64 to 2.59) and there was a clear gradient across the socioeconomic spectrum. Female sex, fruit consumption, childhood mental health and maternal health measures were associated with childhood FCP in univariable and multivariable analyses. Inclusion of these factors within the model attenuated the RR by 17% to 1.70 (95% CI 1.36 to 2.13).
Conclusion
In this representative UK cohort, there was a significant excess of FCP reported in less advantaged children that was partially attenuated when accounting for indicators of parental and childhood mental health. Addressing these factors may partially reduce inequalities in childhood FCP.
Keywords: Educational Status, Chronic Pain, Risk Factors, Longitudinal Study, Children
What is already known on this topic?
Frequent complaints of pain are common in children and the causes, but the social patterning is unclear.
Clinical presentations are heterogeneous and are variously categorised, including as unexplained chronic pain.
Frequent complaints of pain in children may have serious lifelong consequences for a child’s health, education and well-being.
What this study hopes to add?
About a third of children in the UK frequently complain of pain, with significantly higher prevalence in children living in less advantaged families.
Poor maternal mental health and early indicators of poor childhood emotional and behavioural development are associated with frequent pain complaints.
These differences in maternal and childhood mental health partially explain the social patterning.
Introduction
Frequent complaints of pain (FCP) in children are reported in 25%–33% of children in industrialised countries.1 2 Terms including functional pain, frequent pain, unexplained chronic pain (UCP) and somatic symptoms are commonly used. Case definitions vary widely. Pain complaints often relate to regular, unexplained headaches, stomachaches or musculoskeletal complaints that are serious enough to prompt a general practitioner consultation for a third of these children.3 Children with UCP are time consuming within general practice, difficult to investigate and hard to treat,3 with a proportion of patients being referred to tertiary paediatric pain clinics. Some children with UCP suffer serious consequences, including disability and prolonged school absence.4 UCP may have important social consequences. Some children with UCP report problems in eating, sleeping, pursuit of hobbies, attending school and meeting their friends.5
The aetiology of FCP is varied. Pain may occur after childhood cancer, traumatic or nerve injury, but most cases remain unexplained.4 International consensus diagnostic criteria allow categorisation for functional gastrointestinal (GI) disorders, but do not imply causation.6 Associations with parental pain experience and diet have been found for many of these disorders. A link between UCP and mental health conditions has been demonstrated, prompting theories invoking psychosomatic causation of these symptoms.7 It is expected that socioeconomic factors have a substantial impact on a child’s risk of FCP. This study therefore aimed to assess the social patterning of, and risk factors for, FCP in UK children. A secondary aim was to assess whether any risk factors identified attenuate inequalities in pain complaints.
Method
Design, setting and data source
This study uses data from the UK Millennium Cohort Study (MCS), a nationally representative stratified multistage random sample of approximately 18 000 children born in the UK between September 2000 and January 2002, coordinated by the Centre for Longitudinal Studies, University of London.8–12 Oversampling ensured adequate power to assess outcomes in children living in deprived areas and across ethnic groups. This analysis makes use of data on singleton children across all waves of the study, from 9 months to 11 years.
Outcome measure: parent-reported FCP
Childhood pain was assessed by a Strengths and Difficulties Questionnaire (SDQ) item in survey 5 of the MCS at age 11 years, representing an age at which persistent pain that causes school absence would be disruptive to both social development and education. Main respondents (99.2% mothers) were asked whether their child ‘often complains of headaches, stomach-aches or sickness.’ Possible answers were: not true, somewhat true, certainly true or don’t know. This was recoded to compare those children for whom the description of frequent pain was certainly or somewhat true at age 11 (yes=1) with those for whom the statement was not true (no=0).
Exposure measure: socioeconomic circumstances
The primary exposure of interest was maternal education level (higher degree/fist degree/diploma/A, AS, S level/O level GCSE (General Certificate of Secondary Education) A–C/GCSE D–G/none with international and other qualifications excluded), used as a fixed measure of socioeconomic conditions (SECs) at birth. Maternal education level captures the advantages of SECs that accrue to a child,13 and was selected to represent SEC based on similar studies evaluating recurrent abdominal pain14 and other childhood diseases.15
Covariates
Other exposure variables potentially associated with chronic pain were identified through literature review and matched to available data within the MCS. Maternal variables were measured within a year of childbirth and child variables at age 5 or 7 years (details in table 1). Demographic factors included child sex16 and ethnicity16 (coded as white/Asian/black/mixed or other). Potentially mediating covariates included: preterm birth <37 weeks (yes/no), infant behavioural problems17 (regular eating, sleeping yes/no), problematic crying (yes/no), maternal general (excellent/good/fair/poor), maternal complaint of bodily pain18–20 (none/very mild/mild/moderate/severe or very severe), doctor or nurse diagnosed maternal GI disease14 (yes/no), maternal mental health17 measured using the Kessler scale (normal/distressed), child mental health and behaviour19 21 22 using the SDQ (normal/borderline/abnormal), body mass index (BMI) group23 (underweight or normal range/overweight/obese) and daily fruit consumption23 (none or one/two/three or more).
Table 1.
Characteristics of the total study population, by level of maternal qualification at the birth of child
| Maternal education level (Weighted number of observations) | Higher degree (n=341), 3.6% | Degree (n=1515), 15.1% | Diploma (n=990), 9.6% | A levels (n=1020), 10.2% | GCSE-C (n=3744), 38.0% | GCSE-G (n=1099), 11.5% | None (n=1193), 12.0% | Total (n=9902) | χ2 p Value |
| FCP outcome measure (11 years) | |||||||||
| Yes | 21.0% | 24.3% | 29.2% | 28.3% | 33.2% | 38.4% | 43.2% | 32.3% | <0.001 |
| Sex | |||||||||
| Female | 52.0% | 48.8% | 47.7% | 50.7% | 49.6% | 50.3% | 48.5% | 49.4% | 0.876 |
| Ethnicity | |||||||||
| White | 84.8% | 91.8% | 91.6% | 92.5% | 93.3% | 93.6% | 89.8% | 92.1% | 0.004 |
| Mixed or other | 6.3% | 3.7% | 3.5% | 2.9% | 3.0% | 2.3% | 4.7% | 3.4% | |
| Asian | 5.4% | 2.5% | 2.1% | 3.6% | 2.2% | 2.4% | 4.0% | 2.7% | |
| Black | 3.5% | 2.0% | 2.7% | 1.0% | 1.4% | 1.6% | 1.5% | 1.7% | |
| Gestation | |||||||||
| Premature (<37 weeks) | 5.7% | 6.0% | 6.1% | 4.8% | 8.0% | 6.8% | 10.5% | 7.3% | 0.003 |
| Baby eats and sleeps regularly (9 months) | |||||||||
| Disagree | 1.3% | 1.8% | 2.2% | 2.4% | 2.2% | 2.3% | 3.5% | 2.3% | 0.257 |
| Whether baby crying is a problem (9 months) | |||||||||
| Yes | 5.5% | 6.0% | 4.6% | 6.6% | 5.3% | 7.4% | 10.3% | 6.3% | <0.001 |
| Maternal GI conditions (9 months) | |||||||||
| Yes | 11.9% | 9.9% | 11.3% | 10.9% | 9.7% | 7.8% | 8.2% | 9.7% | 0.176 |
| Maternal mental health (Kessler scale at 3 years) | |||||||||
| Distressed | 14.2% | 9.5% | 11.8% | 15.6% | 20.6% | 24.4% | 26.9% | 18.5% | <0.001 |
| Maternal general health (5 years) | |||||||||
| Excellent | 42.6% | 43.6% | 36.9% | 36.0% | 28.8% | 25.3% | 21.1% | 31.8% | <0.001 |
| Good | 45.7% | 48.4% | 50.9% | 51.2% | 53.9% | 54.0% | 55.0% | 52.3% | |
| Fair | 10.0% | 7.3% | 10.4% | 11.4% | 14.7% | 16.9% | 20.8% | 13.6% | |
| Poor | 1.7% | 0.7% | 1.8% | 1.4% | 2.5% | 3.8% | 3.2% | 2.3% | |
| Self-reported maternal bodily pain (5 years) | |||||||||
| None | 47.7% | 50.1% | 49.2% | 48.5% | 47.4% | 50.0% | 45.3% | 48.1% | <0.001 |
| Very mild | 29.1% | 24.9% | 18.3% | 22.0% | 20.1% | 16.8% | 15.6% | 20.3% | |
| Mild | 14.4% | 13.0% | 13.8% | 12.1% | 11.6% | 13.2% | 12.0% | 12.4% | |
| Moderate | 6.4% | 10.0% | 13.8% | 12.6% | 13.8% | 12.1% | 16.3% | 12.9% | |
| Severe or very severe | 2.4% | 2.0% | 4.9% | 4.8% | 7.1% | 7.9% | 10.7% | 6.2% | |
| Child SDQ (5 years) | |||||||||
| Normal | 95.8% | 97.2% | 94.1% | 91.4% | 90.9% | 83.3% | 78.0% | 90.0% | <0.001 |
| Borderline | 3.6% | 1.6% | 3.3% | 5.3% | 5.0% | 8.2% | 10.3% | 5.3% | |
| Abnormal | 0.6% | 1.2% | 2.6% | 3.3% | 4.0% | 8.5% | 11.8% | 4.7% | |
| Child's BMI group (7 years) | |||||||||
| Normal or underweight | 86.3% | 85.8% | 81.1% | 82.2% | 79.2% | 76.8% | 76.7% | 80.4% | <0.001 |
| Overweight | 11.7% | 11.5% | 14.7% | 13.6% | 14.8% | 16.3% | 17.8% | 14.6% | |
| Obese | 2.0% | 2.7% | 4.2% | 4.2% | 6.0% | 6.9% | 5.4% | 5.0% | |
| Child's portions of fruit consumed per day (5 years) | |||||||||
| None or one | 9.3% | 7.9% | 12.8% | 13.1% | 20.2% | 26.8% | 35.2% | 19.0% | <0.001 |
| Two | 22.5% | 21.6% | 21.9% | 23.8% | 27.6% | 32.1% | 26.0% | 25.9% | |
| Three or more | 68.2% | 70.5% | 65.2% | 63.1% | 52.2% | 41.1% | 38.9% | 55.1% | |
All figures are percentages adjusted for sampling design. Missing data reasons are detailed in section 4 of the online supplementary material.
BMI, body mass index; FCP, frequent complaints of pain; GI, gastrointestinal; SDQ, Strengths and Difficulties Questionnaire.
Analysis strategy
Following the Baron and Kenny steps to mediation,24 we explored the unadjusted association between maternal qualifications (primary exposure) and FCP at 11 years (outcome measure). The risk of FCP was then estimated based on exposures and mediators of interest, presenting unadjusted risk ratios (RRs) using Poisson regression.
Following a life course approach, covariates that were significant at p<0.1 in univariable analysis were added to a multivariable regression model. We used a sequential approach to construct the adjusted models,25 first adding demographic variables, then perinatal factors and postnatal exposures in the order in which they were experienced by the child. Mediation was taken to be a reduction in, or elimination of, statistically significant RRs in a final complete case sample. Attenuation was calculated as a percentage reduction from baseline to fully adjusted RRs. Data were analysed using Stata V.1326 with survey commands used to weight data for sampling design and attrition.
Sensitivity analysis
Sensitivity analyses were conducted with a stricter specification of the outcome variable, or teacher-reported pain complaints and considering household income and parental occupation instead of education as alternative measures of SECs. Further analyses were undertaken to examine the possibility that the result was influenced by collinearity between a mediator (SDQ) and the outcome (an item from the SDQ) and to explore the impact of missing data.27
Ethics
Ethical approval for the MCS was received from a National Health Service research ethics committee prior to each survey.28 Our secondary data analysis did not require additional ethics approval.
Results
Up to 8463 children had complete data on all covariates of interest, 82.1% of children present at all sweeps up to age 11 years.
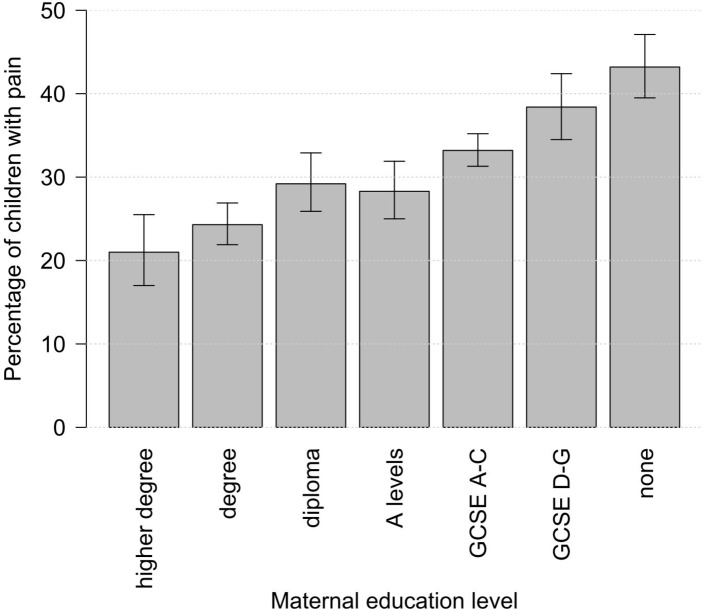
Overall, 32.3% of children frequently complained of pain at age 11, and this differed significantly by childhood SECs (table 1). Up to 43.2% of children in the lowest maternal education group (no qualifications) reported experiencing frequent pain compared with 21.0% in the highest maternal education group (higher degree). A clear socioeconomic gradient is present, with higher reporting of frequent pain in more disadvantaged children (figure 1).
Figure 1.
Bar chart showing the percentage of children who frequently complained of pain at age 11 years by maternal education level. GCSE, General Certificate of Secondary Education.
Lower maternal qualifications are associated with deteriorations in maternal and child health covariates, with the exception of measures of maternal GI disease and infant behaviour. Fruit consumption, a possible protective factor, increases with increased maternal qualifications.
Univariable analysis
In univariable Poisson regression (table 2), lower maternal qualifications were associated with increased risk of FCP. Children in families in which the mother had no qualifications were more likely than children whose mother had a higher degree to complain of FCP (RR 2.06, 95% CI 1.64 to 2.59). Lower maternal education qualifications, female sex, black ethnicity, problematic crying, maternal GI disease, poor maternal mental health, poor maternal general health, maternal bodily pain, childhood emotional difficulties and high BMI were all associated with an increased risk of childhood pain at age 11 years. Eating two or more portions of fruit daily was associated with lower risk of childhood pain. Dose–response relationships were shown for maternal education level, maternal general health, maternal bodily pain, child SDQ, high BMI and fruit consumption.
Table 2.
Univariable and multivariable regression showing RRs with 95% CIs
| Univariable RR (95% CI) | Multivariable RR (95% CI) | % (N) with outcome | |||
| Maternal education (at birth, ref Higher degree) | 21% (71) | ||||
| Degree | 1.16 | (0.93 to 1.44) | 1.21 | (0.98 to 1.50) | 24% (368) |
| Diploma | 1.40 ** | (1.10 to 1.78) | 1.38 ** | (1.09 to 1.74) | 29% (290) |
| A levels | 1.35 * | (1.07 to 1.70) | 1.30 * | (1.04 to 1.64) | 28% (289) |
| GCSE A–C | 1.59 *** | (1.29 to 1.95) | 1.46 *** | (1.19 to 1.79) | 33% (1244) |
| GCSE D–G | 1.83 *** | (1.46 to 2.30) | 1.57 *** | (1.25 to 1.98) | 38% (421) |
| None | 2.06 *** | (1.64 to 2.59) | 1.70 *** | (1.36 to 2.13) | 43% (516) |
| Sex (ref Male) | 28% (1403) | ||||
| Female | 1.31 *** | (1.21 to 1.42) | 1.34 *** | (1.24 to 1.44) | 37% (1796) |
| Ethnicity (ref White) | 32% (2915) | ||||
| Mixed or other | 1.06 | (0.86 to 1.31) | 1 | (0.81 to 1.23) | 34% (115) |
| Asian | 1.1 | (0.92 to 1.31) | 0.97 | (0.83 to 1.13) | 35% (96) |
| Black | 1.39 ** | (1.11 to 1.73) | 1.27 * | (1.03 to 1.57) | 44% (75) |
| Gestation (ref Term) | 32% (2960) | ||||
| Premature | 1.03 | (0.88 to 1.21) | 33% (239) | ||
| Eats, sleeps regularly (9 months, ref Agree) | 32% (3113) | ||||
| Disagree or strongly disagree | 1.2 | (0.97 to 1.48) | 39% (87) | ||
| Problematic crying (9 months, ref No) | 32% (2942) | ||||
| Yes | 1.30 *** | (1.14 to 1.47) | 1.11 | (0.98 to 1.25) | 41% (257) |
| Maternal GI disease (9 months, ref No) | 31% (2793) | ||||
| Yes | 1.36 *** | (1.23 to 1.49) | 1.23 *** | (1.12 to 1.36) | 42% (407) |
| Maternal Kessler scale (3 years, ref Normal) | 29% (2346) | ||||
| Distressed | 1.61 *** | (1.50 to 1.73) | 1.33 *** | (1.23 to 1.44) | 47% (853) |
| Maternal health (5 years, ref Excellent) | 26% (819) | ||||
| Good | 1.25 *** | (1.14 to 1.38) | 1.12 * | (1.02 to 1.23) | 33% (1689) |
| Fair | 1.66 *** | (1.49 to 1.85) | 1.22 *** | (1.09 to 1.36) | 43% (582) |
| Poor | 1.90 *** | (1.55 to 2.34) | 1.21 | (0.98 to 1.49) | 49% (110) |
| Maternal amount of bodily pain (5 years, ref None) | 27% (1306) | ||||
| Very mild | 1.17 ** | (1.06 to 1.30) | 1.16 ** | (1.05 to 1.28) | 32% (646) |
| Mild | 1.40 *** | (1.27 to 1.55) | 1.30 *** | (1.17 to 1.44) | 38% (474) |
| Moderate | 1.49 *** | (1.34 to 1.67) | 1.28 *** | (1.14 to 1.43) | 41% (524) |
| Severe or very severe | 1.48 *** | (1.29 to 1.69) | 1.21 ** | (1.06 to 1.39) | 41% (250) |
| Child SDQ (5 years, ref Normal) | 30% (2698) | ||||
| Borderline | 1.59 *** | (1.40 to 1.80) | 1.35 *** | (1.19 to 1.54) | 48% (252) |
| Abnormal | 1.77 *** | (1.54 to 2.04) | 1.41 *** | (1.21 to 1.65) | 54% (249) |
| BMI (7 years, ref Normal or underweight) | 31% (2483) | ||||
| Overweight | 1.14 ** | (1.04 to 1.25) | 1.06 | (0.97 to 1.16) | 36% (514) |
| Obese | 1.31 *** | (1.15 to 1.50) | 1.17 * | (1.02 to 1.33) | 41% (203) |
| Daily fruit portions (5 years, ref None or one) | 39% (742) | ||||
| Two | 0.86 ** | (0.77 to 0.96) | 0.93 | (0.83 to 1.03) | 34% (866) |
| Three or more | 0.74 *** | (0.68 to 0.81) | 0.85 *** | (0.78 to 0.93) | 29% (1592) |
Unweighted n=8463.
***p<0.001; **p<0.01; *p<0.05. BMI, body mass index; GCSE, General Certificate of Secondary Education; GI, gastrointestinal; RR, risk ratio; SDQ, Strengths and Difficulties Questionnaire.
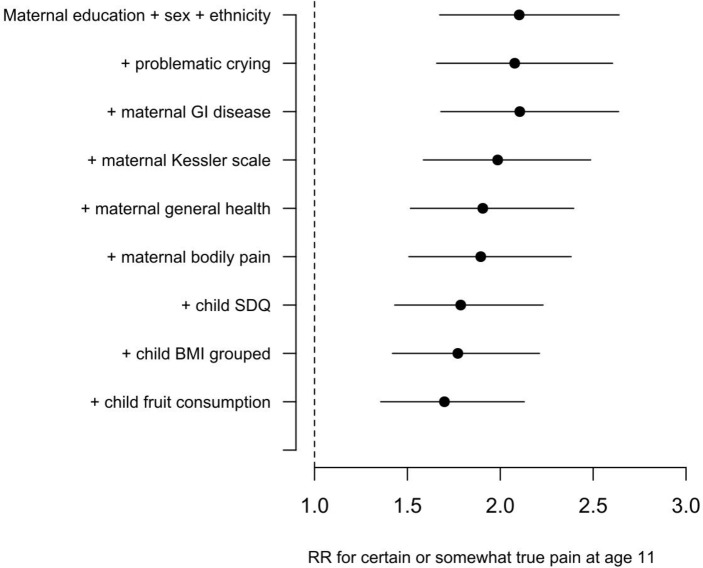
Mediation analysis
The RR for FCP comparing low versus high maternal education is attenuated by 17% after adjustment for covariates comparing the final fully adjusted model relative to a baseline model that included maternal education level, sex and ethnicity. The addition to the model of variables measuring problematic crying, maternal mental health, maternal general health, childhood SDQ and fruit consumption partially attenuated the impact of maternal education on FCP (figure 2).
Figure 2.
Attenuation of the effect size for low versus high maternal education as risk factors are added sequentially to the model as covariates. RR shown is for no qualifications relative to a higher degree. Error bars show 95% CIs around the survey estimates. BMI, body mass index; GI, gastrointestinal; RR, risk ratio; SDQ, Strengths and Difficulties Questionnaire.
The greatest attenuations of the baseline RR occurred on addition of the child’s SDQ score and maternal Kessler scale, with smaller changes for maternal self-reported general health and fruit consumption. Attenuations are small, and lie within the 95% CIs surrounding the baseline RR.
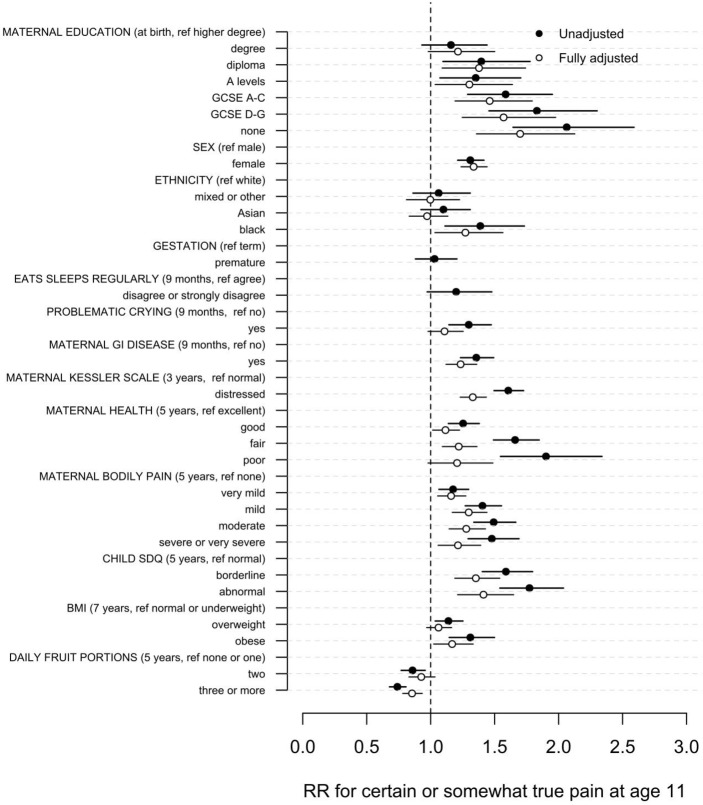
Fully adjusted model
In the fully adjusted regression model, children of families in which the main respondent had no qualifications have more than twice the risk of FCP symptoms experienced by children in families where the main respondent had a higher degree (RR 1.70, 95% CI 1.36 to 2.13, p<0.001).
Female sex and all measures of poor maternal health remained significant predictors of increased FCP (table 2 and figure 3). Black children have increased risk of FCP (RR 1.27, 95% CI 1.03 to 1.57).
Figure 3.
Unadjusted and fully adjusted RRs of frequent complaints of pain prevalence with 95% CIs. BMI, body mass index; GCSE, General Certificate of Secondary Education; GI, gastrointestinal; RR, risk ratio; SDQ, Strengths and Difficulties Questionnaire.
The strongest associations between child health measures and FCP are for child mental health, represented by the SDQ, in which abnormal SDQ scores, compared with normal scores, were associated with increased risk FCP (RR 1.77, 95% CI 1.54 to 2.04).
Sensitivity analyses
Repeating the analysis using occupational class or household income rather than maternal education as the measure of SECs produced similar results (online supplementary material 1).
bmjpo-2017-000093supp001.pdf (360.1KB, pdf)
Repeating the analysis with a stricter definition of FCP resulted in similar results but wider CIs. The analysis using teacher (instead of parent) reported complaints of FCP also produced similar results, but with considerably larger RRs. Repeating the analysis without variables that contributed large amounts of missing data also produced similar results. Repeating the analysis using a recalculated SDQ measure without the frequent pain item produced near identical results to using the full SDQ score. Results of all sensitivity analyses are presented in online supplementary material.
Discussion
Children from households in which the mother has no qualifications are twice as likely to frequently complain of pain at age 11 years than children from households in which the main respondent has a higher degree, and there is a clear socioeconomic gradient. This finding may be partially explained by the social patterning of risk factors for FCP, including poor parent and child mental health and indicators of poor diet. However, after adjusting for known risk factors, those exposed to the lowest SECs experience twice as many cases of FCP as those with the most advantageous SECs, suggesting a large effect of SECs on risk of FCP that is mediated by unknown risk factors.
Both maternal and child mental health significantly predicted FCP. The effect of SECs on FCP may be partially mediated through the influence of SECs on maternal mental health and subsequently child mental health. Adults with fewer qualifications and lower incomes suffer a greater burden of depression.29 Existing cross-sectional studies also associate parental17 18 30 and childhood19 21 22 31 mental health problems with the development of FCP.
The effect of SECs on FCP may also be mediated through the influence of SECs on maternal GI disease and indicators of childhood diet. This partly replicates Malaty et al’s23 findings in their school-based US sample using a much larger and more representative UK study.
This study provides further evidence that girls complain more frequently of pain than boys, replicating the findings of previous studies that considered recurrent pain or functional somatic symptoms in general,17 32 but not studies focused on abdominal23 or back pain.33
Strengths and limitations
This study was carried out using secondary data from a representative and contemporary UK cohort. To our knowledge, this is the largest study to date of FCP in children. The study had ample statistical power to consider inequalities in pain as a health outcome, which was strengthened through the MCS’s sampling strategy and use of weights to compensate for attrition.
Through its longitudinal analysis, this study provides strong evidence that socioeconomic risk factors measured 10 years before the measurement of an outcome are associated with that outcome. It has demonstrated a large effect of SECs on FCP that was robust in an extensive sensitivity analysis. The MCS’s rich data set has enabled control for possible confounders, and comprehensive data on social conditions have allowed the effect of social inequalities on pain to be confirmed across all the key individual measures of SECs.
The most important limitation of this study is the uncertain clinical validity of the outcome measure, which was unvalidated and did not assess whether the pain about which children complained was categorically chronic, or exclude children who may have an organic cause of pain. While chronic pain is common in children1 and most chronic pain remains unexplained,34–37 cases of severe UCP are much less common.2 Our reported FCP prevalence based on parental report (32.2%) was towards the upper end of that reported in UCP literature, and an existing study38 has suggested that parental report is inaccurate, based on disagreement between parent-reported and self-reported pain in children. These concerns are addressed through a sensitivity analysis in which teacher-reported pain was used as the outcome measure, which supported the main analysis despite finding less than half the prevalence (15.2%) of parent-reported pain.
Given the breadth of the MCS question on FCP, children who frequently complain of pain are reporting a heterogeneous phenomenon. While the term sickness, within the MCS question, may be interpreted as a general state of malaise, particularly in conjunction with complaints, some parents may instead interpret this as nausea. For some children, this pain seems likely to be psychogenic or psychosomatic in origin,30 39 yet for others it might be caused by an underlying predisposition to GI disease, predisease states14 or poor diet. The finding that both psychological and dietary factors independently predict FCP and may mediate the effects of SECs on FCP supports this conclusion. The mediating variables tested within this study were constrained by the questions asked within the MCS. It is possible that a future study using more sensitive measures of childhood and maternal diet and emotional functioning would show that these factors mediate a greater proportion of the association between SECs and FCP. It is possible that our results may be biased by including a mediator (SDQ) in a model for an outcome measure that is an SDQ item, but our sensitivity analysis using a recalculated SDQ score (without the pain item) produced near identical results.
A further limitation of this study is attrition within the MCS, common to any cohort study, but partially mitigated by weighting. A sensitivity analysis that removed the three variables that had the greatest amount of missing data showed similar results to the main analysis, suggesting that the exclusion of children due to missing data did not bias this study.
Policy and practice
This study suggests that a range of existing interventions might be able to reduce the overall prevalence of FCP, but might also be able to reduce the inequalities in FCP across the social gradient. Interventions that reduce differential exposure to risk factors that promote the development of paediatric FCP symptoms could include improved parental healthcare to address GI illness, improved parental mental healthcare and particularly perinatal mental health services. Population level interventions (typically regulatory changes) that address dietary change could also have an effect, particularly where these seek to improve choice of diet for the least advantaged or the development of services to promote early years’ psychological well-being and emotional resilience.
While targeting some of the mediating factors linking SECs to FCP is likely to reduce inequalities in FCP, given the large direct effect of SECs in this study, action is needed to address the underlying inequalities in the social determinants of child health.
Footnotes
Contributors: BF designed the study, analysed the data and drafted the manuscript. GC, SLW and DCTR provided input on the study design. SLW and DCTR contributed to the analytical strategy. GC, SLW, BRB and DCTR commented on drafts of the manuscript. All authors read and approved the final manuscript.
Funding: SLW is supported by a Wellcome Trust research fellowship. This piece of work was also supported by The Farr Institute for Health Informatics Research (MRC grant: MR/M0501633/1). The Millennium Cohort Study is funded by grants to former and current directors of the study from the Economic and Social Research Council (Professor HeatherJoshi, Professor Lucinda Platt and Professor Emla Fitzsimons) and a consortium of government funders. All researchers were independent of the funders, and the funders played no part in the study design, analysis or interpretation of the data, writing of the report or the decision to submit for publication.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The data used in this study are available from the UK data service.
References
- 1.Perquin CW, Hazebroek-Kampschreur AA, Hunfeld JA, et al. . Pain in children and adolescents: a common experience. Pain 2000;87:51–8. doi:10.1016/S0304-3959(00)00269-4 [DOI] [PubMed] [Google Scholar]
- 2.Huguet A, Miró J. The severity of chronic pediatric pain: an epidemiological study. The Journal of Pain 2008;9:226–36. doi:10.1016/j.jpain.2007.10.015 [DOI] [PubMed] [Google Scholar]
- 3.Perquin CW, Hunfeld JAM, Hazebroek-Kampschreur AAJM, et al. . Insights in the use of health care services in chronic benign pain in childhood and adolescence. Pain 2001;94:9p:205–13. doi:10.1016/S0304-3959(01)00355-4 [DOI] [PubMed] [Google Scholar]
- 4.Konijnenberg AY, Uiterwaal CS, Kimpen JL, et al. . Children with unexplained chronic pain: substantial impairment in everyday life. Arch Dis Child 2005;90:680–6. doi:10.1136/adc.2004.056820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roth-Isigkeit A, Thyen U, Stöven H, et al. . Pain among children and adolescents: restrictions in Daily living and triggering factors. Pediatrics 2005;115:e152–e162. doi:10.1542/peds.2004-0682 [DOI] [PubMed] [Google Scholar]
- 6.Rome III Diagnostic Criteria for functional gastrointestinal disorders. 2016. Available at www.romecriteria.org/assets/pdf/19_RomeIII_apA_885-898.pdf (accessed 28 jun 2016).
- 7.Eriksen HR, Ursin H. Subjective health complaints, sensitization, and sustained cognitive activation (stress). J Psychosom Res 2004;56:445–8. doi:10.1016/S0022-3999(03)00629-9 [DOI] [PubMed] [Google Scholar]
- 8.University of London. Institute of Education. Centre for Longitudinal Studies. Millennium Cohort Study: First Survey, 2001-2003. [data collection]: UK Data Service, 2012. [Google Scholar]
- 9.University of London. Institute of Education. Centre for Longitudinal Studies. Millennium Cohort Study: Second Survey, 2003-2005. [data collection]: UK Data Service, 2012. [Google Scholar]
- 10.University of London. Institute of Education. Centre for Longitudinal Studies. Millennium Cohort Study: Third Survey, 2006. [data collection]: UK Data Service, 2012. [Google Scholar]
- 11.University of London. Institute of Education. Centre for Longitudinal Studies. Millennium Cohort Study: Fifth Survey, 2012 [data collection]: UK Data Service, 2015. [Google Scholar]
- 12.University of London. Institute of Education. Centre for Longitudinal Studies. Millennium Cohort Study: Fourth Survey, 2008. [data collection]: UK Data Service, 2015. [Google Scholar]
- 13.Galobardes B, Shaw M, Lawlor DA, et al. . Indicators of socioeconomic position (part 1). J Epidemiol Community Health 2006;60:7–12. doi:10.1136/jech.2004.023531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bode G, Brenner H, Adler G, et al. . Recurrent abdominal pain in children: evidence from a population-based study that social and familial factors play a major role but not Helicobacter pylori infection. J Psychosom Res 2003;54:417–21. [DOI] [PubMed] [Google Scholar]
- 15.Massion S, Wickham S, Pearce A, et al. . Exploring the impact of early life factors on inequalities in risk of overweight in UK children: findings from the UK Millennium Cohort Study. Arch Dis Child 2016;101:724–30. doi:10.1136/archdischild-2015-309465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Evans S, Taub R, Tsao JCI, et al. . Sociodemographic factors in a pediatric chronic pain clinic: the roles of age, sex and minority status in pain and health characteristics. J Pain Manage 2010;3:273. [PMC free article] [PubMed] [Google Scholar]
- 17.Rask CU, Ørnbøl E, Olsen EM, et al. . Infant behaviors are predictive of functional somatic symptoms at ages 5-7 years: results from the Copenhagen Child Cohort CCC2000. J Pediatr 2013;162:335–42. doi:10.1016/j.jpeds.2012.08.001 [DOI] [PubMed] [Google Scholar]
- 18.Hotopf M, Carr S, Mayou R, et al. . Why do children have chronic abdominal pain, and what happens to them when they grow up? Population based cohort study. BMJ 1998;316:1196–200. doi:10.1136/bmj.316.7139.1196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janssens KA, Klis S, Kingma EM, et al. . Predictors for persistence of functional somatic symptoms in adolescents. J Pediatr 2014;164:900–5. doi:10.1016/j.jpeds.2013.12.003 [DOI] [PubMed] [Google Scholar]
- 20.Sherman AL, Bruehl S, Smith CA, et al. . Individual and additive effects of mothers' and fathers' chronic pain on health outcomes in young adults with a childhood history of functional abdominal pain. J Pediatr Psychol 2013;38:365–75. doi:10.1093/jpepsy/jss131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rousseau-Salvador C, Amouroux R, Annequin D, et al. . Anxiety, depression and school absenteeism in youth with chronic or episodic headache. Pain Res Manag 2014;19:235–40. doi:10.1155/2014/541618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Galli F, D'Antuono G, Tarantino S, et al. . Headache and recurrent abdominal pain: a controlled study by the means of the Child Behaviour Checklist (CBCL). Cephalalgia 2007;27:211–9. doi:10.1111/j.1468-2982.2006.01271.x [DOI] [PubMed] [Google Scholar]
- 23.Malaty HM, Abudayyeh S, Fraley K, et al. . Recurrent abdominal pain in school children: effect of obesity and diet. Acta Paediatr 2007;96:572–6. doi:10.1111/j.1651-2227.2007.00230.x [DOI] [PubMed] [Google Scholar]
- 24.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–82. doi:10.1037/0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- 25.Taylor-Robinson DC, Pearce A, Whitehead M, et al. . Social inequalities in wheezing in children: findings from the UK Millennium Cohort Study. Eur Respir J 2016;47:818–28. doi:10.1183/13993003.01117-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Corp S. Stata statistical software. release 13. 2013.
- 27.Cole SR, Platt RW, Schisterman EF, et al. . Illustrating bias due to conditioning on a collider. Int J Epidemiol 2010;39:417–20. doi:10.1093/ije/dyp334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Millennium Cohort Study – Ethical review and Consent. 2016. Available at http://www.cls.ioe.ac.uk/shared/get-file.ashx?id=1601&itemtype=document (accessed 28 Jun 2016).
- 29.Lorant V, Deliège D, Eaton W, et al. . Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol 2003;157:98–112. doi:10.1093/aje/kwf182 [DOI] [PubMed] [Google Scholar]
- 30.Rousseau S, Grietens H, Vanderfaeillie J, et al. . Parenting stress and dimensions of parenting behavior: cross-sectional and longitudinal links with adolescents' somatization. Int J Psychiatry Med 2013;46:243–70. doi:10.2190/PM.46.3.b [DOI] [PubMed] [Google Scholar]
- 31.Varni JW, Rapoff MA, Waldron SA, et al. . Effects of perceived stress on pediatric chronic pain. J Behav Med 1996;19:515–28. doi:10.1007/BF01904901 [DOI] [PubMed] [Google Scholar]
- 32.Grøholt EK, Stigum H, Nordhagen R, et al. . Recurrent pain in children, socio-economic factors and accumulation in families. Eur J Epidemiol 2003;18:965–75. doi:10.1023/A:1025889912964 [DOI] [PubMed] [Google Scholar]
- 33.Leboeuf-Yde C, Wedderkopp N, Andersen LB, et al. . Back pain reporting in children and adolescents: the impact of parents' educational level. J Manipulative Physiol Ther 2002;25:216–20. doi:10.1067/mmt.2002.123172 [DOI] [PubMed] [Google Scholar]
- 34.Apley J, Naish N. Recurrent abdominal pains: a field survey of 1,000 school children. Arch Dis Child 1958;33:165–70. doi:10.1136/adc.33.168.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.El-Matary W, Spray C, Sandhu B. Irritable bowel syndrome: the commonest cause of recurrent abdominal pain in children. Eur J Pediatr 2004;163:584–8. doi:10.1007/s00431-004-1503-0 [DOI] [PubMed] [Google Scholar]
- 36.Clinch J, Eccleston C. Chronic musculoskeletal pain in children: assessment and management. Rheumatology 2009;48:466–74. doi:10.1093/rheumatology/kep001 [DOI] [PubMed] [Google Scholar]
- 37.King S, Chambers CT, Huguet A, et al. . The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain 2011;152:2729–38. doi:10.1016/j.pain.2011.07.016 [DOI] [PubMed] [Google Scholar]
- 38.Graungaard AH, Siersma V, Lykke K, et al. . Maternal pain influences her evaluation of recurrent pain in 6- to 11-year-old healthy children. Acta Paediatr 2016;105:183–90. doi:10.1111/apa.13216 [DOI] [PubMed] [Google Scholar]
- 39.Walker LS, Garber J, Greene JW. Psychosocial correlates of recurrent childhood pain: a comparison of pediatric patients with recurrent abdominal pain, organic illness, and psychiatric disorders. J Abnorm Psychol 1993;102:248–58. doi:10.1037/0021-843X.102.2.248 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjpo-2017-000093supp001.pdf (360.1KB, pdf)