Abstract
Background:
Quadrupled (4-strand) hamstring tendon autografts are commonly used in anterior cruciate ligament (ACL) reconstruction, but there is significant variability in their diameter. The 5-strand hamstring autograft has been used as a means of increasing the graft diameter in patients with undersized hamstring grafts.
Purpose:
To report the outcomes of primary ACL reconstruction using 5-strand hamstring autografts in patients in whom the 4-strand configuration produced a graft diameter of <8 mm and to compare these outcomes with those of ACL reconstruction using 4-strand semitendinosus-gracilis autografts with a graft diameter of ≥8 mm.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
The primary study group comprised 25 patients who underwent ACL reconstruction using a 5-strand hamstring autograft. The comparison group comprised 20 patients who underwent ACL reconstruction using a 4-strand hamstring autograft with a graft diameter of ≥8 mm. Interference screw fixation was used at the tibial and femoral ends for both groups of patients. Subjective questionnaires, including the Knee injury and Osteoarthritis Outcome Score (KOOS), the Lysholm score, and the Physical Component Summary and Mental Component Summary of the Short Form–36 (SF-36), were administered preoperatively as well as at 1- and 2-year follow-up visits.
Results:
There were no significant differences in the patient demographics and preoperative scores between the 2 groups. The mean graft diameter was 9.06 ± 0.60 mm in the 5-strand group and 8.13 ± 0.32 mm in the 4-strand group (P < .05). There was no statistically significant difference between groups on postoperative Lysholm, KOOS Pain, KOOS Symptoms, KOOS Activities of Daily Living, KOOS Sports, KOOS Quality of Life, and SF-36 Physical Component Summary scores.
Conclusion:
In primary ACL reconstruction, the 5-strand hamstring autograft achieves clinical outcomes that are comparable to those of the 4-strand hamstring autograft with a graft diameter of ≥8 mm. The 5-strand graft technique is therefore a useful means of increasing the graft diameter when faced with an undersized hamstring graft.
Keywords: 5-strand hamstring autograft, ACL reconstruction, interference screw, clinical outcomes
Quadrupled (4-strand) hamstring tendon autografts are commonly used in anterior cruciate ligament (ACL) reconstruction surgery. Several studies have suggested that these grafts produce functional results comparable to those of bone–patellar tendon–bone autografts.3,5,13
An important shortcoming of this graft, however, is the variability of its diameter. While several studies have attempted to identify anthropometric predictors for graft diameter, none has demonstrated a reliable correlation between these predictors and ultimate graft diameter.4,9,10,17
Biomechanical studies have established an increased load-to-failure rate with an increasing graft diameter,1 and clinical studies have demonstrated a reduced revision risk with an increased graft diameter.14,16 In several studies, a larger graft diameter has also been associated with better patient-reported outcomes, while a smaller graft diameter has been associated with a greater rate of failure.11–14
Several techniques have been described to increase the hamstring graft diameter when faced with undersized tendon grafts. One of these is the 5-strand hamstring autograft in which the longer semitendinosus tendon is tripled and the gracilis tendon doubled to produce a 5-strand configuration. This technique has been reported to increase the graft diameter by 1 to 2 mm.7,8
The purpose of this study was to report the outcomes of primary ACL reconstruction using a 5-strand hamstring autograft in patients in whom the 4-strand configuration produced a graft diameter of <8 mm and to compare these outcomes with those of ACL reconstruction using a 4-strand semitendinosus-gracilis autograft with a graft diameter of ≥8 mm. The hypothesis was that the outcomes of ACL reconstruction using a 5-strand hamstring autograft would be comparable with those of ACL reconstruction using a 4-strand hamstring autograft.
Methods
Study Design
This study was granted ethical approval by the institutional domain-specific review board before commencement. The inclusion criteria for the study were as follows: (1) patients who underwent primary ACL reconstruction using a hamstring autograft by the senior author (L.K.) between December 2014 and June 2016; (2) patients in whom the 5-strand autograft was used because their 4-strand configuration produced a graft diameter of <8 mm (study group) or in whom the 4-strand hamstring autograft used had a graft diameter of ≥8 mm (comparison group); (3) the use of interference screw fixation at both the femoral and tibial ends of the ACL graft; (4) consent obtained to participate in our institution’s ACL reconstruction registry and to complete preoperative and postoperative outcome questionnaires; and (5) completion of at least 1 year of follow-up.
Patients were excluded if their ACL reconstruction was part of a multiligament reconstruction procedure or if concomitant lateral tenodesis was performed. The primary study group therefore consisted of patients in whom the 5-strand hamstring autograft was used for the above reason, and the comparison group consisted of patients who had a 4-strand semitendinosus-gracilis autograft with a graft diameter of ≥8 mm. The femoral and tibial fixation technique was standardized across both groups to prevent confounding.
Patient Demographics and Functional Assessment
Demographic data were documented at the initial clinical evaluation. The patients were seen in our institution’s sports medicine clinic after their injury and diagnosed with ACL tears clinically. After the clinical evaluation, patients underwent confirmatory preoperative magnetic resonance imaging of the injured knee. Patient-reported outcome scores, namely, the Knee injury and Osteoarthritis Outcome Score (KOOS), the Lysholm score, and the Physical Component Summary (PCS) and Mental Component Summary of the Short Form–36 (SF-36), were obtained preoperatively as well as at the 1- and 2-year follow-up periods.
Surgical Technique
Standard medial and lateral arthroscopic portals were created adjacent to the patellar tendon, and diagnostic arthroscopic surgery was performed to assess the ACL tear and concurrent injuries. A longitudinal skin incision of approximately 3 cm was then made on the anteromedial tibial surface at the level of the pes anserinus. The gracilis and semitendinosus tendons were harvested using a closed tendon stripper. The tendon lengths were measured after clearing the residual muscle tissue, and preliminary sizing of the 4-strand graft was performed by passing it through a sizing block to measure its diameter. Graft diameter was defined as the smallest diameter lumen through which the entire graft could pass through smoothly, and the diameter was measured to the nearest 0.5 mm.
If the graft diameter of the 4-strand graft configuration was <8 mm, a 5-strand graft was prepared if the tendon lengths had a minimum length as follows: 24 cm for the semitendinosus tendon and 16 cm for the gracilis tendon. This was required to prepare a 5-strand hamstring graft with a minimum length of 80 mm, given the need to triple the semitendinosus tendon and double the gracilis tendon. This allowed for at least 25 mm of the graft in the femoral tunnel, 30 mm inside the joint, and at least 25 mm in the tibial tunnel. If the minimum length requirements were not met, a standard 4-strand graft was prepared as described below.
Five-Strand Graft
The final expected length of the 5-strand graft was calculated as one-third of the usable length of the semitendinosus tendon after removal of the residual muscle tissue. This was based on tripling of the semitendinosus tendon during preparation of the 5-strand graft.
The gracilis tendon was first shortened to double that of the final expected graft length. This was based on doubling of the gracilis tendon during preparation of the 5-strand graft. A whipstitch was placed at each end of the gracilis tendon with nonabsorbable sutures (Ultrabraid; Smith & Nephew). In the semitendinosus tendon, a whipstitch was first placed using nonabsorbable sutures (Ethibond Excel No. 2; Ethicon) at the distal free end. The semitendinosus tendon was measured and marked to identify 3 equal segments. The graft was then folded such that the proximal free end reached the junction between the proximal two-thirds and distal third of the tendon. This end was whipstitched to the body of the tendon using a nonabsorbable Ultrabraid suture (Figure 1). The free ends of the nonabsorbable suture were then tied over the looped end of the graft. A second nonabsorbable suture (Ethibond Excel No. 2) was then passed around the free looped segment of the semitendinosus graft.
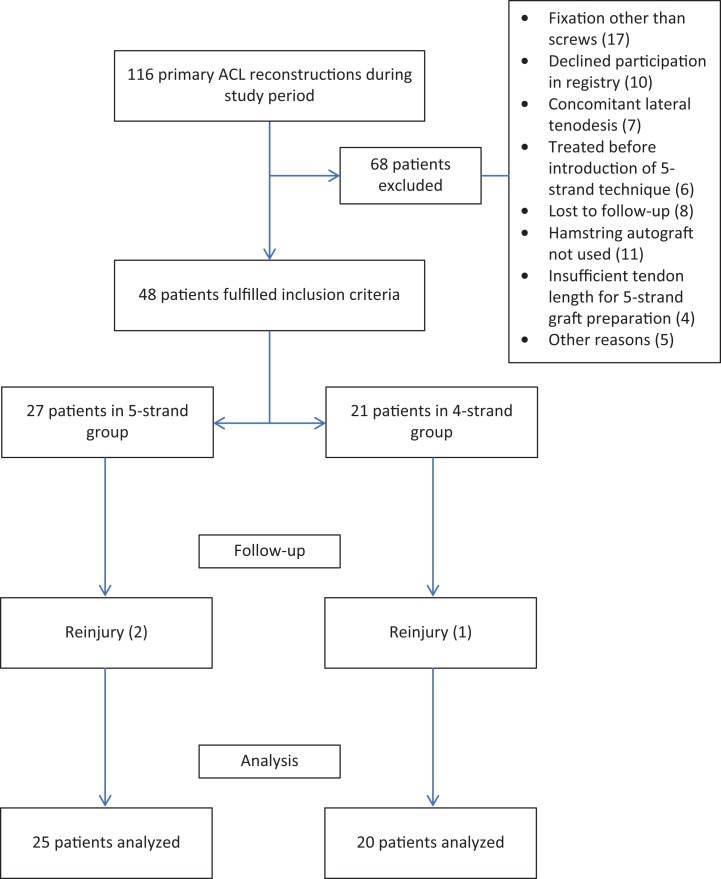
Figure 1.
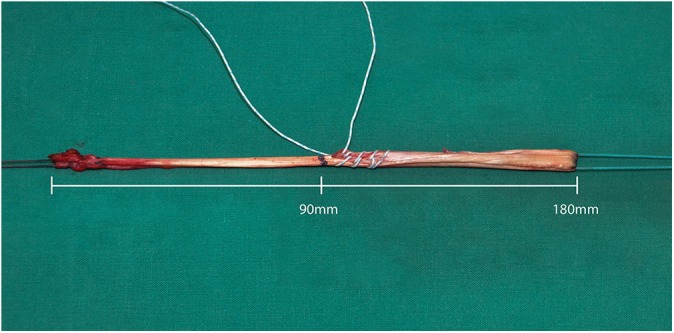
The semitendinosus tendon with one end whipstitched to its body.
A nonabsorbable suture (Ethibond Excel No. 5) was placed around the doubled gracilis tendon graft and around the sutured segment of the semitendinosus graft as shown in Figure 2. A second nonabsorbable suture (Ethibond Excel No. 2) was then passed around the free looped segment of the semitendinosus graft. This formed the 5-strand hamstring graft (Figure 2). The 5-strand graft was then passed through a sizing block to measure its diameter.
Figure 2.
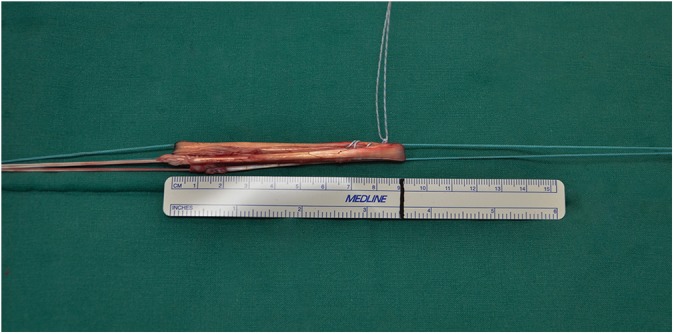
Combination of the doubled gracilis tendon and the tripled semitendinosus tendon to form the 5-strand graft.
The remaining free ends of the nonabsorbable suture in the body of the semitendinosus tendon were then placed in a running whipstitch fashion to tightly unite the strands of the graft at the femoral intratunnel portion of the graft. The tibial intratunnel portion of the graft was similarly prepared with another nonabsorbable Ultrabraid suture. This was done to ensure that the strands were not damaged during passage of the interference screw and to provide an improved fixation interface for the screw6 (Figure 3).
Figure 3.
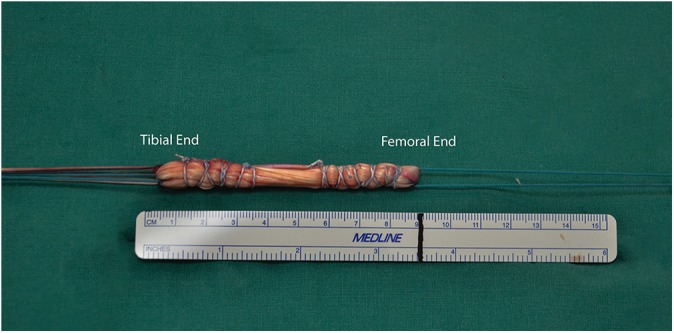
Reinforcement of the femoral and tibial ends of the 5-strand graft.
The graft was then placed on the tension board with the folded end on one side and the free ends on the other, taking care to tension the semitendinosus and gracilis grafts equally.
Four-Strand Graft
A whipstitch was placed at both ends of each tendon with nonabsorbable Ultrabraid sutures. The gracilis and semitendinosus tendons were then looped around a nonabsorbable suture (Ethibond Excel No. 5) to form the 4-strand hamstring graft. As with the 5-strand graft, nonabsorbable Ultrabraid sutures were placed in a running whipstitch fashion to tightly unite the strands at the femoral and tibial intratunnel portions of the graft.
Tunnel Preparation and Graft Fixation
A tibial guide wire was inserted from the anteromedial surface of the tibia to the center of the ACL tibial insertion using an Acufex tibial guide (Smith & Nephew), and the tibia was reamed with a cannulated drill.
For the femoral tunnel, a guide wire was placed using an anteromedial portal approach at the anatomic anteromedial bundle position through the anteromedial portal with the knee in 120° of flexion. A 25 mm– to 30 mm–long femoral socket was created with a cannulated drill. Femoral and tibial tunnel sizes were determined by the diameter of the graft constructs. The femoral drill hole was then extended to the lateral cortex of the femur with a 4.5 mm–diameter cannulated drill.
After creation of the femoral and tibial tunnels, the leading suture of the graft (Ethibond Excel No. 5) was pulled through the tibial tunnel and then into the femoral tunnel. After passage of the graft through the tibial and femoral tunnels, it was fixed at the femoral tunnel with a bioabsorbable interference screw (Biosure; Smith & Nephew) (Figure 4). The graft was then tensioned with the knee in slight flexion before fixation at the tibial tunnel with another bioabsorbable Biosure interference screw. A concomitant meniscal injury was treated with either meniscal repair or partial meniscectomy as indicated intraoperatively.
Figure 4.
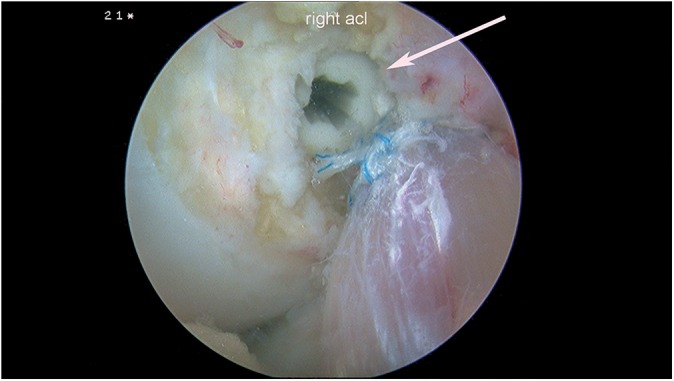
Intraoperative fixation of the anterior cruciate ligament with an interference screw (arrow) in situ.
Postoperative Rehabilitation Protocol
Postoperatively, all patients received appropriate analgesia and underwent a standard rehabilitation program as per our institutional protocol. Patients were prescribed with early weightbearing and range-of-motion exercises. Patients who underwent concomitant meniscal repair were restricted to 0° to 90° of flexion for the first 6 weeks after surgery.
Statistical Analysis
A post hoc sample size analysis was performed assuming 2-tailed testing, with an alpha of 0.05. A minimum sample size of 40 patients was sufficient to detect an effect size of d = 0.92 with 80% statistical power. SPSS version 23 (IBM) was used for data analysis. The Pearson chi-square test was used for categorical variables. For continuous variables, the paired-samples t test was used for the analysis of paired variables, while the Mann-Whitney U test was performed for comparison of outcome scores and population characteristics between both groups. The level of statistical significance was set at P < .05.
Results
Patient Characteristics
Between December 2014 and June 2016, a total of 116 patients underwent primary ACL reconstruction by the senior author. The 5-strand technique was routinely used to increase the graft size during the latter part of the study period, from May 2015 to June 2016. During the study period and after the introduction of the 5-strand technique, 4 patients were found to have a 4-strand tendon graft diameter of <8 mm and to have a semitendinosus tendon length of <24 cm. This precluded the preparation of the 5-strand graft, based on our requirements, and the 4-strand graft was therefore used. There were also 6 patients who had 4-strand graft diameters of <8 mm but who did not receive the 5-strand graft because they were treated before the 5-strand technique was introduced (Figure 5).
Figure 5.
Study flowchart. ACL, anterior cruciate ligament.
Application of the inclusion and exclusion criteria yielded 48 patients, of whom 27 patients had a 5-strand graft because their 4-strand configuration produced a graft diameter of <8 mm (study group), and 21 patients had a 4-strand hamstring autograft with a graft diameter of ≥8 mm (comparison group). Figure 5 illustrates the study flowchart.
The mean follow-up period was 17.3 months (17.8 months in the 5-strand group and 16.8 months in the 4-strand group; P = .596). The mean age of patients in the 5-strand group was 25.6 ± 7.3 years, while that of the 4-strand group was 29.2 ± 8.0 years (P = .084). The mean body mass index was 24.1 ± 3.4 kg/m2 and 26.1 ± 3.8 kg/m2 for the 5- and 4-strand groups, respectively (P = .090). In the 5-strand group, there were 19 male patients (76%), and in the 4-strand group, there were also 19 male patients (95%) (P = .081). A total of 13 (52%) and 12 (60%) right legs were performed on in the 5- and 4-strand groups, respectively (P = .592) (Table 1).
TABLE 1.
Patient Demographicsa
| 5-Strand Group (n = 25) | 4-Strand Group (n = 20) | P Value | |
|---|---|---|---|
| Age, y | 25.6 ± 7.3 | 29.2 ± 8.0 | .084 |
| Sex, n (%) | .081 | ||
| Male | 19 (76.0) | 19 (95.0) | |
| Female | 6 (24.0) | 1 (5.0) | |
| Height, cm | 171.3 ± 8.0 | 171.1 ± 5.9 | .953 |
| Weight, kg | 71.2 ± 14.1 | 76.5 ± 12.5 | .144 |
| Body mass index, kg/m2 | 24.1 ± 3.4 | 26.1 ± 3.8 | .090 |
| Graft diameter, mm | 9.06 ± 0.60 | 8.13 ± 0.32 | <.001 |
| Mean follow-up duration, mo | 17.8 | 16.8 | .596 |
| Side of surgery, n (%) | .592 | ||
| Left | 12 (48.0) | 8 (40.0) | |
| Right | 13 (52.0) | 12 (60.0) | |
| Type of injury, n (%) | .141 | ||
| Sports | 21 (84.0) | 13 (65.0) | |
| Nonsports | 4 (16.0) | 7 (35.0) | |
| Concomitant injury, n | |||
| Medial meniscal tear | 11 | 8 | .787 |
| Lateral meniscal tear | 12 | 10 | .894 |
| Chondral injury | 4 | 6 | .262 |
aData are shown as mean ± SD unless otherwise specified.
The mean graft diameter was 9.06 ± 0.60 mm in the 5-strand group and 8.13 ± 0.32 mm in the 4-strand group (P < .001). In the 5-strand group, there were 21 (84%) sports-related injuries, while there were 13 (65%) in the 4-strand group (P = .141). There were no significant differences in preoperative outcome scores between the 2 groups (Table 2).
TABLE 2.
Comparison of Outcome Scoresa
| 5-Strand Group (n = 25) | 4-Strand Group (n = 20) | P Value | |
|---|---|---|---|
| Preoperative scores | |||
| Lysholm | 72.6 ± 16.4 | 70.5 ± 14.5 | .478 |
| KOOS Symptoms | 79.7 ± 17.7 | 76.1 ± 13.3 | .384 |
| KOOS Pain | 86.7 ± 14.0 | 79.2 ± 14.4 | .073 |
| KOOS Activities of Daily Living | 88.1 ± 11.6 | 87.4 ± 9.9 | .544 |
| KOOS Sports | 45.2 ± 28.1 | 33.3 ± 28.7 | .128 |
| KOOS Quality of Life | 47.5 ± 19.8 | 49.7 ± 16.4 | .305 |
| SF-36 PCS | 47.4 ± 7.3 | 44.4 ± 6.3 | .144 |
| SF-36 MCS | 50.3 ± 9.5 | 53.9 ± 5.3 | .235 |
| Postoperative scores at latest follow-up | |||
| Lysholm | 90.4 ± 8.1 | 88.5 ± 10.5 | .579 |
| KOOS Symptoms | 88.1 ± 11.9 | 89.1 ± 10.7 | .826 |
| KOOS Pain | 93.6 ± 9.3 | 93.6 ± 6.5 | .458 |
| KOOS Activities of Daily Living | 96.5 ± 8.7 | 96.0 ± 5.4 | .519 |
| KOOS Sports | 85.4 ± 14.3 | 83.5 ± 17.1 | .693 |
| KOOS Quality of Life | 66.8 ± 21.6 | 69.1 ± 13.2 | .991 |
| SF-36 PCS | 52.7 ± 4.8 | 53.9 ± 3.8 | .591 |
| SF-36 MCS | 52.0 ± 10.6 | 56.2 ± 5.9 | .209 |
aData are shown as mean ± SD. KOOS, Knee injury and Osteoarthritis Outcome Score; MCS, Mental Component Summary; PCS, Physical Component Summary; SF-36, Short Form–36.
In the 5-strand group, 11 of 25 patients had medial meniscal tears, of whom 9 underwent meniscal repair and 2 underwent partial meniscectomy. Twelve of 25 patients had lateral meniscal tears; 6 were treated with meniscal repair, 4 underwent partial meniscectomy, and 2 were left alone. Four patients had chondral injuries, of whom 2 underwent microfracture and 2 were left alone.
In the 4-strand group, 8 of 20 patients had medial meniscal tears, of whom 6 underwent meniscal repair and 2 underwent partial meniscectomy. Ten of 20 patients had lateral meniscal tears; 2 were treated with meniscal repair, 6 underwent partial meniscectomy, and 2 were left alone. Six patients had chondral injuries, of whom 2 underwent chondroplasty and 4 were left alone.
Postoperative Outcomes
Postoperatively, there was significant improvement from baseline scores in both the 5-strand and 4-strand groups on the Lysholm (P < .001 for both), KOOS Symptoms (P = .042 and P = .001, respectively), KOOS Pain (P = .035 and P < .001, respectively), KOOS Activities of Daily Living (P = .003 for both), KOOS Sports (P < .001 for both), KOOS Quality of Life (P = .001, respectively), and SF-36 PCS (P = .001 and P < .001, respectively).
Comparing the postoperative outcomes of the 5-strand group versus the 4-strand group, there was no statistically significant difference on the Lysholm, KOOS Symptoms, KOOS Pain, KOOS Activities of Daily Living, KOOS Sports, KOOS Quality of Life, or SF-36 PCS scores (Table 2).
Complications
In the 5-strand group, 1 patient experienced an intraoperative tibial tunnel blowout and underwent primary fixation of the graft by tying over a tibial post and washer. Postoperatively, 1 patient sustained a contralateral ACL tear 13 months after the index procedure, and 2 patients sustained traumatic graft tears during the follow-up period. In the 4-strand group, 1 patient sustained a traumatic graft tear 14 months after surgery.
Discussion
The results of this study indicate that the 5-strand hamstring autograft achieves clinical outcomes that are comparable to those of the 4-strand hamstring autograft with a graft diameter of ≥8 mm in ACL reconstruction. The 5-strand graft technique has been used to increase the graft diameter when faced with an undersized hamstring graft.7,8,18 In this study, the 5-strand graft was used when the 4-strand configuration produced a graft diameter of <8 mm.
The biomechanical advantages of an increased hamstring graft diameter have been well described. Boniello et al1 reported significant increases in strength with every millimeter increase in the graft diameter. An increase in the graft diameter from 6 to 7 mm was associated with a 38% increase in graft strength, and 7 to 8 mm was associated with a 20% increase.
In their case-control study, Spragg et al16 demonstrated a 0.82 times lower likelihood of revision with every 0.5-mm increment in the graft diameter between 7.0 and 9.0 mm. The recent cohort study by Snaebjornsson et al14 based on the Swedish National Knee Ligament Register similarly reported a 0.86 times lower likelihood of revision with every 0.5-mm increment in the graft diameter between 7.0 and 10.0 mm. Similarly, Magnussen et al11 analyzed 256 patients undergoing ACL reconstruction with a hamstring autograft and found that grafts larger than 8.5 mm had a 1.7% revision rate, while grafts between 8 and 8.5 mm and 7.5 and 8 mm had a revision rate of 6.5% and 6.2%, respectively. In the same study, grafts that ranged from 7 to 7.5 mm and ≤7 mm had a revision rate of 11.3% and 33%, respectively.
A larger graft diameter has also been reported to produce better patient-reported outcomes.11–13 A Multicenter Orthopaedic Outcomes Network (MOON) cohort study of 263 patients described an association between larger hamstring graft diameters and better patient-reported outcomes.12 It was reported that a 1-mm increase in the graft diameter was associated with a 5.2-, 3.3-, and 2.0-point increase in KOOS Sports, Pain, and Activities of Daily Living scores, respectively. A 3.4-point increase in the subjective International Knee Documentation Committee (IKDC) score was also reported. It is worth noting that the results by Snaebjornsson et al14 from the Swedish registry did not parallel these findings. In their patient-reported outcomes, measured via the KOOS and EuroQol 5-Dimension questionnaires, there was no demonstrable correlation between increased graft diameter and patient-reported outcomes.
As discussed above, the literature indicates that a larger hamstring graft diameter is associated with biomechanical and clinical advantages. However, this is based primarily on the 4-strand hamstring graft configuration, and it remains unclear if the use of alternative graft configurations (such as the 5-strand graft) to increase the graft diameter results in a similar improvement in outcomes. Previous studies have reported increases in the graft diameter of between 1 and 2 mm with the use of the 5-strand technique.7,8,18 While previously described techniques have utilized suspensory fixation for these grafts, biomechanical studies suggest that this may result in little biomechanical advantage over the 4-strand arrangement. Snow et al15 demonstrated in their biomechanical study that using suspensory fixation in a tripled tendon can produce cyclic elongation of the third strand, resulting in reduced tensile stress. In this manner, the 5-strand graft may behave like a 4-strand graft, losing its effectiveness and purpose.15 Vaillant et al18 demonstrated poor load distribution between strands in their biomechanical study. By directly attaching the fifth strand to the cortical button loop with sutures, it was found that the fifth strand was not biomechanically incorporated.18
Interference screws work as compression fixation devices, unlike suspensory fixation, in which the graft is held in place by the free ends of the whipstitch. Weiler et al19 have demonstrated the promotion of intratunnel healing, and hence tendon-to-bone incorporation, with the use of interference screw fixation. Given that all strands of the graft are held in place within the tunnel by the interference screw, this could mitigate the problem of third-strand elongation and the loss of tensile stress as demonstrated by Snow et al.15 For this reason, we used the interference screw for fixation of the 5-strand graft at the femoral tunnel instead of suspensory fixation.
There have also been limited reports in the literature on the clinical outcomes of the 5-strand hamstring autograft. Calvo et al2 conducted a similar study to ours in which they compared the outcomes of 2 groups of patients undergoing ACL reconstruction: the first with a 4-strand hamstring autograft with a diameter of >8-mm and the second with a 5-strand hamstring autograft with a diameter of >8-mm. In their study, 33 patients received a 4-strand graft, and 37 received a 5-strand graft. The mean follow-up duration was 32.20 months in their 4-strand group and 30.35 months in the 5-strand group, while the mean graft diameter was 8.5 mm in the 4-strand group and 9.2 mm in the 5-strand group. The authors found that the 5-strand hamstring graft was clinically comparable with the 4-strand graft that was >8 mm. The differences in rerupture rates and clinical outcomes were not statistically significant between the 2 groups, suggesting that it was a valid option when faced with a graft of insufficient diameter. Our results corroborate the findings of Calvo et al.2
There are several limitations in our study. First, the sample size was small. This was because the 5-strand graft configuration was only used when faced with a 4-strand graft diameter of <8 mm. The 5-strand group also represented our initial clinical experience with the use of the 5-strand graft. Second, the sizes of the initial 4-strand grafts were not recorded for the 5-strand group, and this meant that we were not able to report the specific increase in graft diameter that resulted from the use of the 5-strand technique in this cohort. However, for a subsequent cohort of 64 patients in whom we conducted a prospective randomized controlled study, comparing the 5-strand graft with the standard 4-strand graft, the mean increase in graft size achieved with the 5-strand technique was 1.4 ± 0.3 mm (unpublished data). Third, the mean follow-up period in our study was less than 2 years. However, all patients completed at least 1 year of follow-up, and the mean follow-up period of both groups was similar. Last, given that interference screw fixation was used exclusively in this study for both femoral and tibial fixation, our findings may not readily translate to reconstruction utilizing suspensory fixation.
In conclusion, the 5-strand hamstring autograft achieves short-term clinical outcomes that are comparable to those of the 4-strand hamstring autograft with a graft diameter of ≥8 mm in primary ACL reconstruction. The 5-strand graft technique is therefore a useful means of increasing the graft diameter when faced with an undersized hamstring graft. This may translate to improved patient-reported outcomes and reduced revision rates. More research is needed to determine if the routine use of the 5-strand hamstring autograft will lead to better outcomes after ACL reconstruction compared to the traditional 4-strand hamstring autograft.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from the National Healthcare Group (DSRB reference 2016/01149).
References
- 1. Boniello MR, Schwingler PM, Bonner JM, Robinson SP, Cotter A, Bonner KF. Impact of hamstring graft diameter on tendon strength: a biomechanical study. Arthroscopy. 2015;31(6):1084–1090. [DOI] [PubMed] [Google Scholar]
- 2. Calvo R, Figueroa D, Figueroa F, et al. Five-strand hamstring autograft versus quadruple hamstring autograft with graft diameters 8.0 millimeters or more in anterior cruciate ligament reconstruction: clinical outcomes with a minimum 2-year follow-up. Arthroscopy. 2017;33(5):1007–1013. [DOI] [PubMed] [Google Scholar]
- 3. Chee MY, Chen Y, Pearce CJ, et al. Outcome of patellar tendon versus 4-strand hamstring tendon autografts for anterior cruciate ligament reconstruction: a systematic review and meta-analysis of prospective randomized trials. Arthroscopy. 2017;33(2):450–463. [DOI] [PubMed] [Google Scholar]
- 4. Goyal S, Matias N, Pandey V, Acharya K. Are pre-operative anthropometric parameters helpful in predicting length and thickness of quadrupled hamstring graft for ACL reconstruction in adults? A prospective study and literature review. Int Orthop. 2016;40(1):173–181. [DOI] [PubMed] [Google Scholar]
- 5. Hamner DL, Brown CH, Jr, Steiner ME, Hecker AT, Hayes WC. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am. 1999;81(4):549–557. [DOI] [PubMed] [Google Scholar]
- 6. Hoher J, Offerhaus C, Steenlage E, Weiler A, Scheffler S. Impact of tendon suturing on the interference fixation strength of quadrupled hamstring tendon grafts. Arch Orthop Trauma Surg. 2013;133(9):1309–1314. [DOI] [PubMed] [Google Scholar]
- 7. Lavery KP, Rasmussen JF, Dhawan A. Five-strand hamstring autograft for anterior cruciate ligament reconstruction. Arthrosc Tech. 2014;3(4):e423–e426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee RJ, Ganley TJ. The 5-strand hamstring graft in anterior cruciate ligament reconstruction. Arthrosc Tech. 2014;3(5):e627–e631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Loo W, Liu B, Lee Y, Soon Y. Can we predict ACL hamstring graft sizes in the Asian male? A clinical relationship study of anthropometric features and 4-strand hamstring graft sizes. Malaysian Orthopaedic Journal. 2010;4:9–12. [Google Scholar]
- 10. Ma CB, Keifa E, Dunn W, Fu FH, Harner CD. Can pre-operative measures predict quadruple hamstring graft diameter? Knee. 2010;17(1):81–83. [DOI] [PubMed] [Google Scholar]
- 11. Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. [DOI] [PubMed] [Google Scholar]
- 12. Mariscalco MW, Flanigan DC, Mitchell J, et al. The influence of hamstring autograft size on patient reported outcomes and risk of revision following anterior cruciate ligament reconstruction: a MOON cohort study. Arthroscopy. 2013;29(12):1948–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sajovic M, Strahovnik A, Dernovsek MZ, Skaza K. Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: an 11-year follow-up of a randomized controlled trial. Am J Sports Med. 2011;39(10):2161–2169. [DOI] [PubMed] [Google Scholar]
- 14. Snaebjornsson T, Hamrin Senorski E, Ayeni OR, et al. Graft diameter as a predictor for revision anterior cruciate ligament reconstruction and KOOS and EQ-5D values: a cohort study from the Swedish National Knee Ligament Register based on 2240 patients. Am J Sports Med. 2017;45(9):2092–2097. [DOI] [PubMed] [Google Scholar]
- 15. Snow M, Cheung W, Mahmud J, et al. Mechanical assessment of two different methods of tripling hamstring tendons when using suspensory fixation. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):262–267. [DOI] [PubMed] [Google Scholar]
- 16. Spragg L, Chen J, Mirzayan R, Love R, Maletis G. The effect of autologous hamstring graft diameter on the likelihood for revision of anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44(6):1475–1481. [DOI] [PubMed] [Google Scholar]
- 17. Tuman JM, Diduch DR, Rubino LJ, Baumfeld JA, Nguyen HS, Hart JM. Predictors for hamstring graft diameter in anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35(11):1945–1949. [DOI] [PubMed] [Google Scholar]
- 18. Vaillant ER, Parks BG, Camire LM, Hinton RY. Five-strand versus four-strand hamstring tendon graft technique for anterior cruciate ligament reconstruction: a biomechanical comparison. J Knee Surg. 2017;30(9):916–919. [DOI] [PubMed] [Google Scholar]
- 19. Weiler A, Hoffmann RF, Bail HJ, Rehm O, Sudkamp NP. Tendon healing in a bone tunnel, part II: histologic analysis after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy. 2002;18(2):124–135. [DOI] [PubMed] [Google Scholar]