Abstract
Objective
Current diagnostic assessment tools remain suboptimal in demonstrating complex morphology of congenital heart disease (CHD). This limitation has posed several challenges in preoperative planning, communication in medical practice, and medical education. This study aims to investigate the dimensional accuracy and the clinical value of 3D printed model of CHD in the above three areas.
Methods
Using cardiac computed tomography angiography (CCTA) data, a patient-specific 3D model of a 20-month-old boy with double outlet right ventricle was printed in Tango Plus material. Pearson correlation coefficient was used to evaluate correlation of the quantitative measurements taken at analogous anatomical locations between the CCTA images pre- and post-3D printing. Qualitative analysis was conducted by distributing surveys to six health professionals (two radiologists, two cardiologists and two cardiac surgeons) and three medical academics to assess the clinical value of the 3D printed model in these three areas.
Results
Excellent correlation (r = 0.99) was noted in the measurements between CCTA and 3D printed model, with a mean difference of 0.23 mm. Four out of six health professionals found the model to be useful in facilitating preoperative planning, while all of them thought that the model would be invaluable in enhancing patient-doctor communication. All three medical academics found the model to be helpful in teaching, and thought that the students will be able to learn the pathology quicker with better understanding.
Conclusion
The complex cardiac anatomy can be accurately replicated in flexible material using 3D printing technology. 3D printed heart models could serve as an excellent tool in facilitating preoperative planning, communication in medical practice, and medical education, although further studies with inclusion of more clinical cases are needed.
Introduction
Congenital heart disease (CHD) is the most common birth defect among the newborns [1]. Despite it being so common, patient management of CHD remains challenging due to its complexity and heterogeneity [2–5]. As the cardiovascular morphology varies greatly between individual patients, different surgical options and patient managements are required for each specific case [2]. For this reason, it is imperative to have thorough understanding of the spatial relationship between the intra-cardiac structures, in order to decide the best surgical options [2, 4, 6, 7].
To date, diagnostic assessment and pre-operative planning of CHD is based on volumetric data such as computed tomography (CT), magnetic resonance imaging (MRI), and echocardiography. In conjunction with the three-dimensional (3D) reconstruction method, 3D virtual model of human’s heart can be generated [3–6, 8]. Even though it allows the observers to visualize the heart from various angles, this method falls short in providing full comprehension of the intra-cardiac structures, as it still relies on interpretation from two-dimensional (2D) flat screen [3, 5, 6, 7–11].
In order to resolve this shortcoming, there have been several studies on fabrication of 3D printed cardiac models of CHD. These models were reported to facilitate the surgical decision-making and planning, enhance the patient-doctor communication, and improve the knowledge acquisition among the patients, students, and junior doctors [2–10, 12–30]. The ultimate reason for 3D printed models to outperform current diagnostic tools is because they can be tangibly manipulated and provide additional spatial information of the heart and surrounding cardiovascular structures [5, 6, 14, 19, 20, 26].
However, the evidence to suggest the dimensional accuracy of the 3D printed cardiac models is lacking. Most of the studies in current literature only investigate the clinical usefulness of the models without reporting their dimensional accuracy. Additionally, most of the current studies are case reports or case series focusing on the utility of 3D printed heart models in preoperative planning [2, 4–6, 12, 19–21, 23, 24, 26, 29–31]. There is limited evidence to suggest whether the health professionals and medical academics find the 3D printed heart model useful in their practice. Hence, a detailed investigation of the multi-directional use of the 3D printed heart model is required. Further, most of the models generated in the existing studies were solid, which could not resemble the softness or tissue property of human heart tissues [2–5, 7–9, 13–15, 18, 20, 22, 23, 26–29].
Thus, this study presents a preliminary experience in creating flexible 3D printed heart model from cardiac CT angiography (CCTA). The aim of this study was twofold: (1) to investigate the dimensional accuracy of the 3D printed heart model, and (2) to evaluate the clinical value and feasibility of flexible 3D printed models of CHD, in particular for preoperative planning, medical education, and communication in clinical practice.
Materials and methods
Selection of sample cases for image post-processing
Ethical approval was obtained from Curtin Human Research Ethics Committee. The ethics committee waived the requirement for informed consent due to the retrospective nature of the study and use of de-identified images. Five cases of de-identified CCTA images of complex CHD in Digital Imaging and Communications in Medicine (DICOM) format were obtained from a radiology archive. During the cases selection process, only cases with patients aged from 0–15 years old were included.
All CCTA was performed at 70 kV on a 256-slice GE Revolution scanner (Revolution CT, GE Healthcare, Waukesha, WI) or a 128-slice Siemens Definition Flash (Somatom Definition Flash, Siemens Healthcare, Forchheim, Germany). The contrast medium was administered according to the following protocol:
Injection rate: weight (kilograms) x 0.1 mL/s
Volume of contrast medium: injection rate x 20 s
To reduce the radiation dose to the paediatric patients, prospective electrocardiogram (ECG) triggering technology and tube current modulation were utilized. The selected cases were also ensured to have slice thickness of less than 0.75 mm to guarantee the resolution of acquired images for 3D printing purpose.
Image segmentation and post-processing
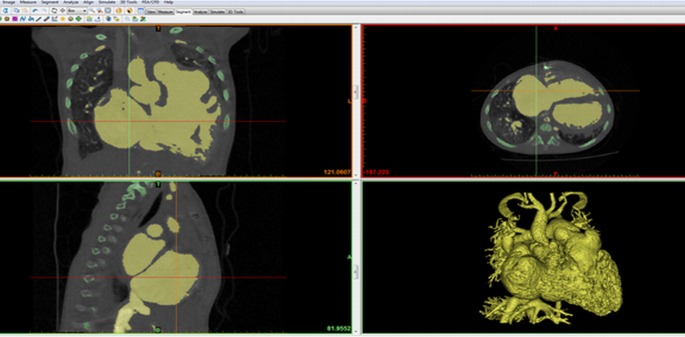
All five cases were segmented using Mimics Innovation Suite software (Materialise HQ, Leuven, Belgium) using thresholding and region growing methods [32]. In the segmentation process, the blood pool in the heart was isolated from other anatomical structures (Fig 1). Following that, a layer of arbitrary thickness of 2 mm was added onto the blood pool surface to represent imaginary heart wall using 3-Matic software (Materialise HQ, Leuven, Belgium). The digital model was hollowed and smoothed before being exported in Standard Tessellation Language (STL) format [32].
Fig 1. Image segmentation using MIMICS Innovation Suite software.
Contrast-enhanced blood and cardiac chambers were highlighted and segmented from the surrounding soft tissue and bony structures.
The STL file exported from 3-Matic was loaded into Geomagic Studio 12 (3D Systems, Inc. Korea) to separate the digital model into two compartments. This was done so that the intra-cardiac structures can be better demonstrated. The model was cut through a plane transecting right atrium and right ventricle to provide a viewing window for the ventricular septal defect (VSD). Mesh doctor function was also used to optimize the file for 3D printing.
The time to generate the STL model was limited to 2 hours to ensure the practicability of producing 3D printed heart models. Only one digital model that requires least manual edition but with excellent demonstration of cardiac anatomical structures and pathologies was chosen for 3D printing.
Three-dimensional printing
The chosen digital model was printed with a commercial printer Stratasys (Objet Eden 260VS) using Polyjet printing technology in Tango Plus material, which is a rubber-like material that has more resemblance to human heart tissue when compared to hard plastic [33, 34]. After obtaining the physical 3D printed heart model, contrast-enhanced CT scan of the 3D model was performed to determine model’s accuracy. This was conducted on a 64-slice CT scanner (Philips Brilliance 64; Philips Medical Systems, Netherlands) using a contrast enhanced chest protocol at 120 kV, with a slice thickness of 0.6 mm. For the contrast scan, the model was submerged in a container filled with approximately 1L of fluid which contained 100 mL of Ultravist 300 (Bayer Australia Ltd, Pymble, NSW, Australia) and 900 mL of water. This allows for generation of CT attenuation of 250 HU which is similar to that used in routine CCTA.
Quantitative measurements of anatomic accuracy
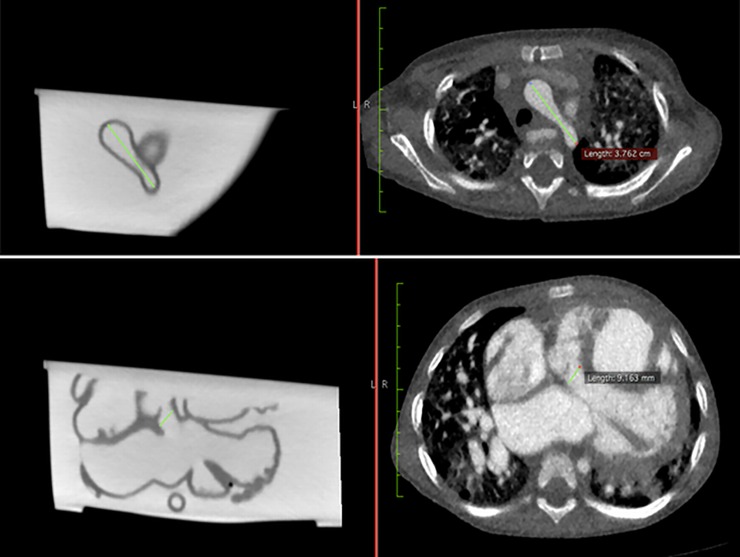
Measurements of different anatomical locations were taken at two stages for comparison: original CCTA and contrast-enhanced CT images of the 3D printed model. Both stages of measurements were done using the ruler function in Horos (Horos Project), which is an open-source DICOM viewer (Fig 2). The internal diameter of ten anatomical locations were measured and compared. These anatomical locations consisted of the base of brachiocephalic trunk, aortic arch, ascending aorta, left pulmonary artery, right pulmonary artery, pulmonary trunk, descending aorta, VSD, right atrium and left ventricle. In order to reduce bias in results, the measurement for each anatomical location was repeated for three times by two independent observers.
Fig 2. An example showing how measurements were taken at the aortic arch (top row) and ventricular septal defect (bottom row) using ruler function in Horos.
The left column images refer to contrast-enhanced CT images of the 3D printed model, while the right column images indicate original CCTA images.
Qualitative assessment of clinical value
To assess the clinical value of the 3D printed model, interviews and surveys were conducted with six health professionals consisting of two radiologists (S1 File), two cardiologists (S2 File), and two cardiac surgeons (S3 File), as well as three medical academic staff (S4 File) who voluntarily participated in the survey (. The health professionals were from major public and private practices, whereas the medical academic staffs were recruited from Curtin University.
Each participant had access to the de-identified CCTA dataset as well as the 3D printed model either online or physically. A brief introduction of the 3D printed model was given to the participants before they were asked to compare the CCTA and 3D model. For the participants to have online access of the 3D printed heart model, an introductory video of it was uploaded to social media. The de-identified CCTA dataset was also uploaded to DICOM Library. DICOM Library is an online platform to share DICOM file for educational and scientific purposes [35].
The participants were then asked to complete a set of questionnaires. The questions focused on evaluating their perception of 3D printing of CHD in preoperative planning, medical education, and communication in clinical practice, by using 3-point Likert scale and written response format. Each group of professionals received a different set of questionnaires, as the questionnaires were specifically designed to be relevant to the participants’ scope of practice. The questionnaires were generated and modified based on the findings of previous studies [4, 6, 7, 9, 14–16, 28–30, 33, 34].
Statistical analysis
Due to the limited number of case and participants, the data analysis of this study was strictly limited to descriptive statistics. For quantitative analysis, Pearson’s correlation coefficient was used to assess correlation of the measurements on original CCTA and 3D printed model [27]. All the measurements were recorded in Microsoft Excel with the mean values, mean difference, and correlation coefficient calculated. For qualitative analysis, the questions were grouped into three main categories, namely preoperative planning, communication in clinical practice, and medical education. The responses of each category were entered into SPSS 24.0 (SPSS, IBM Corporation, Armonk, NY, USA) and tabulated in frequency tables.
Results
Image post-processing and three-dimensional printing
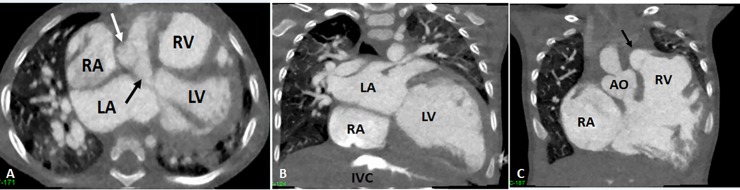
The chosen case for 3D printing is a case of a 20-month-old boy who was diagnosed with double outlet right ventricle with a sub-aortic VSD. The CCTA demonstrated both the aorta and pulmonary trunk originate from the right ventricle. Both the great arteries are transposed with aorta at the right side. The aortic arch and descending aorta are narrowed. The VSD is located below the aortic valve, with the size of approximately 13.2 mm (Fig 3).
Fig 3. Cardiac computed tomography (CT) angiography showing double outlet right ventricle and ventricular septal defect (VSD).
A: 2D axial CT image showing the four-chamber view with sub-aortic VSD (black arrow). B: 2D coronal CT image showing left atrium (LA), right atrium (RA) and left ventricle (LV). C: 2D coronal CT image showing that aorta (AO) and pulmonary artery (black arrows) all arise from right ventricle (RV). IVC-inferior vena cava, white arrow in A refers to ascending aorta.
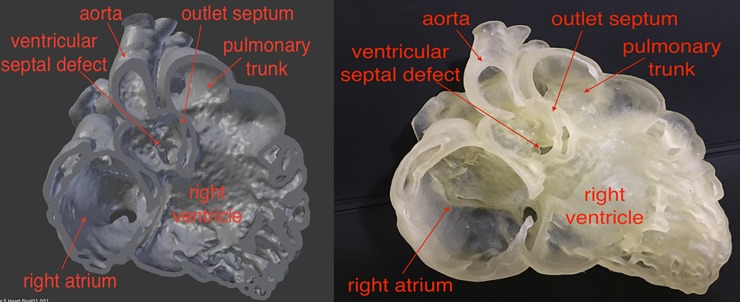
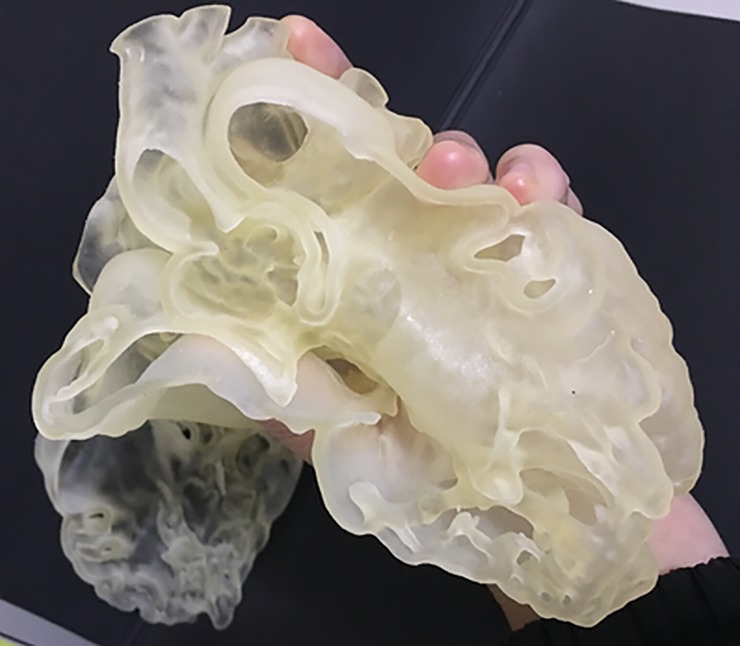
The time taken to complete the image post-processing using Mimics was 15 minutes. The total cost of 3D printing was around AUD $300. The resulting 3D model shows that it is feasible to replicate the heart in rubber-like material, with excellent demonstration of intra-cardiac structures (Figs 4 and 5).
Fig 4.
Labeled screen-display of the virtual model (left) and photograph of the 3D printed heart model (right). Reprinted with permission under the open access from Lau and Sun [31].
Fig 5. Demonstration of the flexibility of the 3D printed heart model in Tango Plus material.
Reprinted with permission under the open access from Lau and Sun [31].
Quantitative measurements of anatomical accuracy
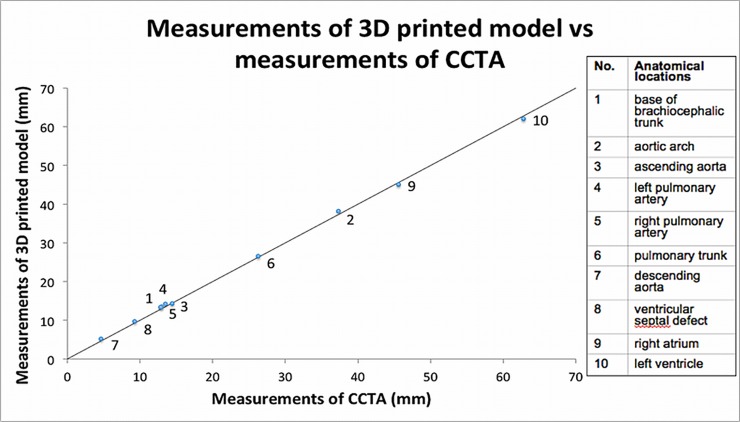
A strong correlation (r = 0.99) was demonstrated between the CCTA and 3D printed model measurements, indicating that the 3D printed model generated in this study is highly accurate in replicating anatomical cardiac structures. Overall, the 3D printed model marginally over-estimated the size of the heart when compared to the CCTA measurements, but only by 0.23 mm in average. Fig 6 demonstrates a scatter plot comparing the measurements of 3D printed model and CCTA. Note that all the data points lie very closely with the perfect correlation line (r = 1.00).
Fig 6. Scatter plot of measurements of 3D printed model against measurements of cardiac computed tomography angiography (CCTA).
Each data point is assigned with a number to represent different anatomical locations. 3D: three-dimensional.
Qualitative assessment of clinical value
Overall, all the participants have at least three years of working experience in the corresponding professional field. Eight out of nine participants had encountered challenges in their profession before due to limitations of current visualization techniques, whereas six out of nine participants reported that they had used 3D printed cardiac models in their practice previously. The average satisfaction score of the model was 8.4 out of 10.
Preoperative planning in congenital heart disease
Four out of six health professionals indicated that the 3D printed models are useful in planning interventions, while three out of six reported that it could be useful in testing devices for pre-surgical simulation (Table 1). There were no participants who responded ‘no’ to the questions in this category, implying that all the participants to some extent agreed that the 3D printed model is useful in pre-surgical planning.
Table 1. Frequency table of usefulness of three-dimensional printed heart models in preoperative planning.
| Do you think patient-specific 3D models are helpful in… | ||
|---|---|---|
| Count % | planning interventions? | testing device for pre-surgical simulation? |
| Yes | 4 (66.7%) | 3 (50.0%) |
| Maybe | 2 (33.3%) | 3 (50.0%) |
| No | 0 (0.0%) | 0 (0.0%) |
| Total* | 6 (100.0%) | 6 (100.0%) |
*with cardiac surgeons, cardiologists, and radiologists as participants
3D: three-dimensional
Both the cardiac surgeons agreed that the 3D printed models would be able to provide additional information of the pathology compared to conventional imaging and computer simulation. They reported that the 3D printed cardiac model is helpful for them to appreciate potential procedural difficulties, and hence will be able to increase the success rate of the surgery.
Communication in clinical practice
The two cardiac surgeons and two cardiologists were asked whether the 3D printed model is useful in enhancing patient-doctor communication, and all of them reported that the model would be invaluable in improving the consultation experience as they would be able to explain the CHD to the patients more efficiently. They also thought that the patients could understand the condition of their heart better with the use of 3D printed model. However, when being asked whether the consultation time could be reduced, only two of them responded ‘yes’ (Table 2).
Table 2. Frequency table of usefulness of three-dimensional printed heart models in communication in medical practice.
| Do you think… | ||||
|---|---|---|---|---|
| Count % | you can clarify/describe the pathology to the patients/health professionals better using this model, rather than using the DICOM dataset itself? | the patients’/parental understanding of the disease and surgical procedures will be enhanced with the use of 3D printed model during consultation time? | the model can improve the consultation experience? |
the model can shorten the consultation time? |
| Yes | 4 (100.0%) | 4 (100.0%) | 4 (100.0%) | 2 (50.0%) |
| Maybe | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (25.0%) |
| No | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (25.0%) |
| Total* | 4 (100.0%) | 4 (100.0%) | 4 (100.0%) | 4 (100.0%) |
* with cardiac surgeons and cardiologists as participants
DICOM: Digital Imaging and Communications in Medicine
3D: three-dimensional
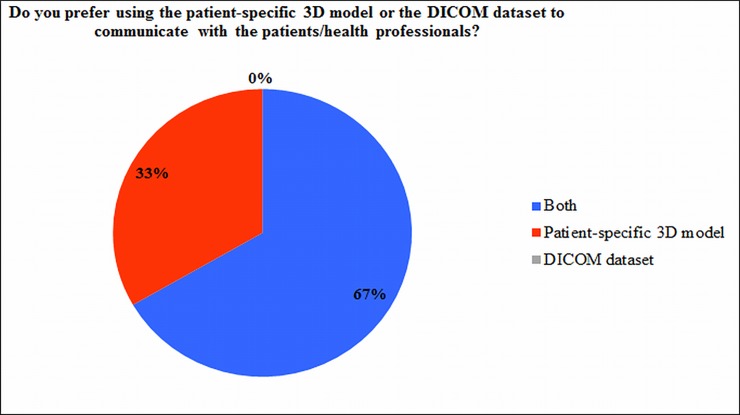
Interestingly, when all the health professionals were asked whether they prefer to use 3D printed model or medical images to communicate with the patients or other health professionals, four out of six indicated they prefer to use both of them as a medium in communication (Fig 7).
Fig 7. Chart representation of the responses obtained from cardiologists, cardiac surgeons and radiologists.
3D: three-dimensional; DICOM: Digital Imaging and Communications in Medicine.
Medical education
The three medical academic staff members were asked about their opinion of using 3D printed cardiac models in teaching anatomy and pathology. All of them found it invaluable, and indicated that the students will be able to learn the pathology quicker with better understanding. However, two medical academics implied that the 3D printed model generated in this study could not help the students to learn normal heart anatomy (Table 3). This is because the printed model is a diseased heart, so it could not represent the normal cardiac structures. Hence, they suggested that a ‘normal’ 3D printed cardiac model should be used for comparison when teaching the students.
Table 3. Frequency table of usefulness of three-dimensional printed heart models in medical education.
| Do you think this model… | |||
|---|---|---|---|
| Count % | can enhance the students’ knowledge of normal heart anatomy? | can enhance the students’ knowledge of cardiac pathology? | will enable the students to learn the disease quicker? |
| Yes | 1 (33.3%) | 3 (100.0%) | 3 (100.0%) |
| Maybe | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| No | 2 (66.7%) | 0 (0.0%) | 0 (0.0%) |
| Total* | 3 (100.0%) | 3 (100.0%) | 3 (100.0%) |
* with medical academics as participants
Discussion
3D printing in medicine was initially introduced in maxillofacial and orthopedic specialties, mainly for preoperative simulation. It was only in recent years that this technique has expanded to cardiovascular diseases. Its clinical value in this area is promising, although more research is needed [4, 6, 26, 29]. A number of studies have shown encouraging results with the use of 3D printed heart models with CHD in preoperative planning, medical education, and communication in clinical practice [2–10, 12–30]. This study further validates these findings by conducting both quantitative and qualitative assessments on a realistic 3D printed heart model with CHD.
Only a few existing studies reported on the dimensional accuracy of the 3D printed heart models. Despite so, all of them are in general agreement that the 3D printed heart models are accurate, with the reported mean difference ranges from 0.05 ± 0.17 mm to 0.4 ± 0.9 mm [7, 8, 26, 27, 30]. There were also a few studies attempted to produce flexible 3D printed model showing that the flexibility of the material allows the surgeons to rehearse the surgical procedures and thus improve the surgical outcomes [6, 12, 24, 30]. Previous studies have also validated the ability of the 3D printed heart models to facilitate decision-making of treatment plan, as it enhances the perception of spatial relationships between the cardiac structures [2, 4–7, 12, 14, 21, 23, 24, 26, 29, 30]. However, studies pointed out that the 3D printed heart models should only be used to complement the current diagnostic tools, instead of stand-alone tool for preoperative planning [4, 18, 20, 26].
The preliminary experience in this study demonstrates that: (1) it is feasible to accurately replicate a heart in flexible material; and (2) the 3D printed heart model of CHD is useful in pre-operative planning, medical education, and communication in medical practice. These positive findings are significant as this is the first report to investigate the accuracy and the multi-directional utility of the 3D printed heart model in a holistic approach. To our knowledge, this is also the first time to confirm model accuracy by performing contrast-enhanced CT scan of the 3D printed heart model for measurement of the intra-cardiac structures (Fig 2), since other studies used caliper for measurements [26, 30]. This has significant clinical value because the luminal size of the flexible heart model changes when a caliper is placed within it. Thus, the approach used in this study to measure the 3D printed model to ensure its size is in its original state, which is demonstrated through performing CT scan on the 3D printed model.
The mean difference of 0.23 mm between the measurements of the 3D printed heart model and the original CCTA could be caused by several reasons. First, it is possible that the measured locations on both CT datasets were not perfectly at the same point. Even though the CT scan of the 3D printed model was reconstructed manually to match the heart orientation of the original CCTA, there is a chance to have slight variations between the analogous locations, impeding a perfect comparison. Second, the image resolution and noise of the source data could also introduce errors in defining the boundaries of the anatomical structures [36]. Although the STL file was smoothed to reduce artifacts caused by the noise prior to printing, the smoothing factor used in this study might not be suitable. Third, the chosen threshold value during the segmentation process might be too low, as the 3D printed model marginally over-estimated the heart size. Fourth, the resolution limits of the 3D printer could also have contributed to the variance between the 3D printed heart model and original CCTA [36]. This mean difference however, is considered acceptable, as it falls within the range of the mean differences reported by other studies [7, 8, 26, 27, 30].
Overall, the cardiac surgeons and cardiologists responded positively with respect to the use of 3D printed heart model in communication within medical practice. However, not all of them agreed that the duration of consultation could be reduced with the use of 3D printed heart model. In a study carried out by Biglino et al, it was found out that the consultation involving the use of 3D printed model lasted 5 minutes longer than usual [13]. This might not necessarily be a negative finding, as the use of 3D printed model could lead to more detailed discussion between the patients and the doctors, thus allowing the patients to achieve better understanding of their condition [13]. Additionally, most of the health professionals prefer to use both medical images and 3D printed heart models in communication. This might indicate that the 3D printed models could not entirely replace the existing approach in communication, but rather to serve as a complementary tool in patient-doctor communication. It could also be due to the fact that the health professionals still rely on 2D medical images for communication, as it is how they have been trained and practicing, although this needs to be further investigated [14]. Some participants also indicated that the current 3D printed model could be improved by color-coding the venous and arterial blood, in order to enhance the patients’ and students’ understanding.
This study has several limitations. First, although comparing the measurements of the original CCTA and 3D printed heart model at ten different anatomical locations was an indicator of the 3D model’s accuracy, it is worthwhile to note that the results may not necessarily reflect the accuracy of the entire model, as the measurements were only taken in axial plane (Fig 2). It is not justified whether 3D printing could distort the size of the heart in other planes, and whether this difference in measurement is uniform in all three dimensions. Future studies are suggested to measure the accuracy of 3D printed models in all three dimensions, including axial, coronal, and sagittal planes to assess the accuracy of the entire model.
Second, there is only one 3D printed heart model generated in this study, therefore, the results lack generalization. Despite this limitation, findings in this study are consistent with those reported in a multi-centre study representing a larger group of patients with 3D printing of CHD [37]. In their recent report involving 10 international centres with inclusion of 40 cases, Valverde et al investigated the impact of 3D printed models on surgical planning and treatment of CHD. Forty 3D printed heart models were generated using cardiac CT and MRI data. Excellent correlation was found in vascular measurements between 3D printed models and original CT or MRI images, with a mean bias of -0.27 ± 0.73 mm, which is very similar to our findings. Further, 3D printed models was ranked satisfactory (>9.0 out of 10) by surgeons and paediatric cardiologists. In nearly half of the cases, 3D models were found to help define the surgical approach [37]. Third, only high quality dataset was used as the source data, therefore the recorded duration for segmentation could not reflect the actual segmentation time for low quality images. In real clinical practice, it is difficult to obtain perfectly CCTA, thus it will require more effort and time in segmentation [6]. Fourth, the 3D printed model generated in this study is static, so it does not allow the observers to understand the haemodynamic function of the heart [2, 11].
As 3D printing in cardiovascular specialty is still in its infancy, future studies should include more cases and participants to confirm the dimensional accuracy and clinical value of the 3D printed heart models. It will also be worthwhile to include surveys with the parents or patients with CHD, as they are the stakeholders who would benefit directly from this novel technology. Additionally, future studies should focus on developing standardized method in generating 3D printed heart models. In the current literature, there is a great variation in terms of how 3D printed models were fabricated, including the source data and segmentation method [18, 38, 39]. These variations can possibly affect the accuracy of the 3D printed models [2, 37]. Furthermore, future investigations should also focus on analyzing the cost-benefit of 3D printing of CHD [3, 9, 13, 18]. The cost of 3D printing was considered as one of the main factors to impede the wide application of 3D printing in medicine [9, 33, 40]. There is a need of a comprehensive cost-benefit analysis to determine the practicability of 3D printing of CHD.
In conclusion, this study has preliminarily assessed the dimensional accuracy as well as the clinical value of flexible patient-specific 3D printed heart models. The flexible 3D printed heart model can be accurately reproduced from cardiac CT images. It is found to facilitate preoperative planning and improve the surgical outcome; enhance patient-doctor and inter-professional communication; and improve approach in medical teaching. These findings warrant further investigations in 3D printing of congenital heart disease.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
The authors would like to acknowledge Dr. Andrew Squelch, Dr. Barry Doyle, Dr. Deanne Yim, Mr Mark Walters, and Mr Werner Ducke in providing the resources and essential knowledge in the process of 3D printing of heart models. Many thanks go to Mr Gil Stevenson for his assistance in statistical analysis.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by National Key R&D Program of China, 2016YFC1300300 (Prof Lei Xu); Natural Science Foundation of China (CN), 81641069 and 81271542 (Prof Lei Xu); and National Heart Foundation of Australia, 101843 (Prof Zhonghua Sun). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Australian Institute of Health and Welfare [Internet]. Australian Government; c2017. How many Australians have cardiovascular disease? [cited 2017 Feb 28]. Available from: http://www.aihw.gov.au/cardiovascular-disease/prevalence/#t5.
- 2.Bhatla P, Tretter JT, Ludomirsky A, Argilla M, Latson LA Jr, S, et al. Utility and scope of rapid prototyping in patients with complex muscular ventricular septal defects or double-outlet right ventricle: Does it alter management decisions? Pediatr Cardiol. 2017;38(1):103–114. doi: 10.1007/s00246-016-1489-1 . [DOI] [PubMed] [Google Scholar]
- 3.Schmauss D, Haeberle S, Hagl C, Sodian R. Three-dimensional printing in cardiac surgery and interventional cardiology: a single-centre experience. Eur J Cardiothorac Surg. 2015;47:1044–1052. doi: 10.1093/ejcts/ezu310 . [DOI] [PubMed] [Google Scholar]
- 4.Valverde I, Gomez G, Gonzales A, Suarez-Mejias C, Adsuar A, Coserria JF, et al. Three-dimensional patient-specific cardiac model for surgical planning in Nikaidoh procedure. Cardiol Young. 2015;25(4):698–704. doi: 10.1017/S1047951114000742 . [DOI] [PubMed] [Google Scholar]
- 5.Riesenkampff E, Rietdorf U, Wolf I, Schnackenburg B, Ewert P, Huebler M, et al. The practical clinical value of three-dimensional models of complex congenitally malformed hearts. J Thorac Cardiovascular Surgery. 2009;138(3):571–580. doi: 10.1016/j.jtcvs.2009.03.011 . [DOI] [PubMed] [Google Scholar]
- 6.Shiraishi I, Yamagishi M, Hamaoka K, Fukuzawa M, Yagihara T. Simulative operation on congenital heart disease using rubber-like urethane stereolithographic biomodels based on 3D datasets of multislice computed tomography. Eur J Cardiothorac Surg. 2010;37:302–306. doi: 10.1016/j.ejcts.2009.07.046 . [DOI] [PubMed] [Google Scholar]
- 7.Ma XJ, Tao L, Chen X, Li W, Peng ZY, Chen Y, et al. Clinical application of three-dimensional reconstruction and rapid prototyping technology of multislice spiral computed tomography angiography for the repair of ventricular septal defect of tetralogy of Fallot. Genet Mol Res. 2015;14(1):1301–1309. doi: 10.4238/2015.February.13.9 . [DOI] [PubMed] [Google Scholar]
- 8.Greil GF, Wolf I, Kuettner A, Fenchel M, Miller S, Martirosian P, et al. Stereolithographic reproduction of complex cardiac morphology based on high spatial resolution imaging. Clin Res Cardiol. 2007;96(3):176–185. doi: 10.1007/s00392-007-0482-3 . [DOI] [PubMed] [Google Scholar]
- 9.Biglino G, Koniordou D, Gasparini M, Capelli C, Leaver LK, S, et al. Piloting the use of patient-specific cardiac models as a novel tool to facilitate communication during clinical consultations. Pediatr Cardiol. 2017;38:813–818. doi: 10.1007/s00246-017-1586-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mottl-Link S, Hübler M, Kühne T, Rietdorf U, Krueger JJ, Schnackenburg B, et al. Physical Models Aiding in Complex Congenital Heart Surgery. Ann Thorac Surg. 2008;86(1):273–277. doi: 10.1016/j.athoracsur.2007.06.001 . [DOI] [PubMed] [Google Scholar]
- 11.Cantinotti M, Valverde I, Kutty S. Three-dimensional printed models in congenital heart disease. Int J Cardiovasc Imaging. 2017;33(1):137–144. doi: 10.1007/s10554-016-0981-2 . [DOI] [PubMed] [Google Scholar]
- 12.Bhalta P, Tretter JT, Chikkabyrappa S, Chakravarti S, Mosca RS. Surgical planning for a complex double-outlet right ventricle using 3D printing. Echocardiography. 2017;34:802–804. doi: 10.1111/echo.13512 Epub 2017 Mar 19. . [DOI] [PubMed] [Google Scholar]
- 13.Biglino G, Capelli C, Wray J, Schievano S, Leaver LK, S, et al. 3D-manufactured patient-specific models of congenital heart defects for communication in clinical practice: feasibility and acceptability. BMJ Open. 2015;5(4):e007165 doi: 10.1136/bmjopen-2014-007165 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Biglino G, Capelli C, Leaver LK, Shievano S, Taylor AM, Wray J. Involving patients, families and medical staff in the evaluation of 3D printing models of congenital heart disease. Communication Med. 2015;12(2/3):157–169. . [DOI] [PubMed] [Google Scholar]
- 15.Biglino G, Capelli C, Koniordou D, Robertshaw D, Leaver LK, Schievano S, et al. Use of 3D models of congenital heart disease as an education tool for cardiac nurses. Congenit Heart Dis. 2017;12(1):113–118. doi: 10.1111/chd.12414 . [DOI] [PubMed] [Google Scholar]
- 16.Costello J, Olivieri L, Krieger A, Thabit O, Marshall MB, Yoo SJ, et al. Utilizing Three-Dimensional Printing Technology to Assess the Feasibility of High-Fidelity Synthetic Ventricular Septal Defect Models for Simulation in Medical Education. World J Pediatr Congenit Heart Surg. 2014;5(3):421–426. doi: 10.1177/2150135114528721 . [DOI] [PubMed] [Google Scholar]
- 17.Costello JP, Olivieri LJ, Su L, Krieger A, Alfares F, Thabit O, et al. Incorporating three-dimensional printing into a simulation-based congenital heart disease and critical care training curriculum for resident physicians. Congenit Heart Dis. 2015;10(2):185–190. doi: 10.1111/chd.12238 . [DOI] [PubMed] [Google Scholar]
- 18.Farooqi KM, Lengua CG, Weinberg AD, Nielsen JC, Sanz J. Blood Pool Segmentation Results in Superior Virtual Cardiac Models than Myocardial Segmentation for 3D Printing. Pediatr Cardiol. 2016;37(6):1028–1036. doi: 10.1007/s00246-016-1385-8 . [DOI] [PubMed] [Google Scholar]
- 19.Farooqi KM, Gonzalez-Lengua C, Shenoy R, Sanz J, Nguyen K. Use of a three dimensional printed cardiac model to assess suitability for biventricular repair. World J Pediatr Congenit Heart Surg. 2016;7(3):414–416. doi: 10.1177/2150135115610285 . [DOI] [PubMed] [Google Scholar]
- 20.Garekar S, Bharati A, Chokhandre M, et al. Clinical application and multidisciplinary assessment of three dimensional printing in double outlet right ventricle with remote ventricular septal defect. World J Pediatr Congenit Heart Surg. 2016;7(3):344–350. doi: 10.1177/2150135116645604 . [DOI] [PubMed] [Google Scholar]
- 21.Hadeed K, Dulac Y, Acar P. Three-dimensional printing of a complex CHD to plan surgical repair. Cardiol Young. 2016;26(7):1432–1434. doi: 10.1017/S1047951116000755 . [DOI] [PubMed] [Google Scholar]
- 22.Jones TW, Seckeler MD. Use of 3D models of vascular rings and slings to improve resident education. Congenit Heart Dis. 2017;12(5):578–582. doi: 10.1111/chd.12486 . [DOI] [PubMed] [Google Scholar]
- 23.Kappanayil M, Koneti NR, Kannan RR, Kottayil BP, Kumar K. Three-dimensional-printed cardiac prototypes aid surgical decision-making and preoperative planning in selected cases of complex congenital heart diseases: early experience and proof of concept in a resource-limited environment. Ann Paediatr Cardiol. 2017;10(2):117–125. doi: 10.4103/apc.APC_149_16 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kiraly L, Tofeig M, Jha NK, Talo H. Three-dimensional printed prototypes refine the anatomy of post-modified Norwood-1 complex aortic arch obstruction and allow presurgical simulation of the repair. Interact Cardiovasc Thorac Surg. 2016;22(2):238–240. doi: 10.1093/icvts/ivv320 . [DOI] [PubMed] [Google Scholar]
- 25.Loke Y, Harahsheh AS, Krieger A, Olivieri LJ. Usage of 3D models of tetralogy of Fallot for medical education: impact on learning congenital heart disease. BMC Med Educ. 2017;17:54–61. doi: 10.1186/s12909-017-0889-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Olejnik P, Nosal M, Havran T, Cizmar M, Slabej M, Thurzo A, et al. Utilisation of three-dimensional printed heart models for operative planning of complex congenital heart defects. Kardiologia Polska. 2017;75(5): 495–501. doi: 10.5603/KP.a2017.0033 . [DOI] [PubMed] [Google Scholar]
- 27.Olivieri LJ, Krieger A, Loke YH, et al. Three-dimensional printing of intracardiac defects from three-dimensional echocardiographic images: feasibility and relative accuracy. J Am Sco Echocardiogr. 2015;28: 392–97. doi: 10.1016/j.echo.2014.12.016 . [DOI] [PubMed] [Google Scholar]
- 28.Olivieri LJ, Su L, Hynes CF, Krieger A, Alfares FA, Ramakrishnan K, et al. ‘‘Just-In-Time” simulation training using 3-D printed cardiac models after congenital cardiac surgery. World J Pediatr Congenit Heart Surg. 2016;7(2):164–168. doi: 10.1177/2150135115623961 . [DOI] [PubMed] [Google Scholar]
- 29.Sodian R, Weber S, Markert M, Rassoulian D, Kaczmarek I, Lueth TC, et al. Stereolithographic models for surgical planning in congenital heart surgery. Ann Thorac Surg. 2007;83:1854–1857. doi: 10.1016/j.athoracsur.2006.12.004 . [DOI] [PubMed] [Google Scholar]
- 30.Valverde I, Gomez G, Coserria JF, Suarez-Mejias C, Uribe S, Sotelo J, et al. 3D printed models for planning endovascular stenting in transverse aortic arch hypoplasia. Catheter Cardiovasc Interv. 2015;85:1006–1012. doi: 10.1002/ccd.25810 . [DOI] [PubMed] [Google Scholar]
- 31.Lau I, Sun Z. Three-dimensional printing in congenital heart disease: A systematic review. J Med Radiat Sci 2018. February 17 doi: 10.1002/jmrs.268 [Epub ahead of print]. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Giannopoulos AA, Chepelev L, Sheikh A, Wang A, Dang W, Akyuz E, et al. 3D printed ventricular septal defect patch: a primer for the 2015 Radiological Society of North America (RSNA) hands-on course in 3D printing. 3D Printing Med. 2015;1(1):1–20. doi: 10.1186/s41205-015-0002-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim MS, Hansgen AR, Carroll JD. Use of Rapid Prototyping in the Care of Patients with Structural Heart Disease. Trends Cardiovasc Med. 2008;18(6):210–216. doi: 10.1016/j.tcm.2008.11.001 . [DOI] [PubMed] [Google Scholar]
- 34.Yoo S, Thabit O, Kim EK, Ide H, Yim D, Dragulescu A, et al. 3D printing in medicine of congenital heart diseases. 3D Printing Med. 2015;2(1):1–12. doi: 10.1186/s41205-016-0004-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.DICOM Library [Internet]. DICOM Library; c2017. Anonymize, Share, View DICOM files online [cited 2017 Nov 08]. Available from: https://www.dicomlibrary.com.
- 36.Ogden KM, Aslan C, Ordway N, Diallo D, Tillapaugh-Fay G, Soman P. Factors affecting dimensional accuracy of 3-D printed anatomical structures derived from CT data. J Digit Imaging. 2015;28(6):654–663. doi: 10.1007/s10278-015-9803-7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Valverde I, Gomez-Ciriza G, Hussain T, Suarez-Mejias C, Velasco-Forte MN, Byrne N, et al. Three-dimensional printed models for surgical planning of complex congenital heart defects: an international multicenter study. Eur J Cardiothorac Surg. 2017;52(6):1139–1148. doi: 10.1093/ejcts/ezx208 . [DOI] [PubMed] [Google Scholar]
- 38.George E, Liacouras P, Rybicki FJ, Mitsouras D. Measuring and establishing the accuracy and reproducibility of 3D printed medical models. Radiographics 2017; 37: 1424–1450. doi: 10.1148/rg.2017160165 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Farooqi KM, Uppu SC, Nguyen K, Srivastava S, Ko HH, Choueiter N, et al. Application of virtual three-dimensional models for simultaneous visualization of intracardiac anatomic relationships in double outlet right ventricle. Pediatr Cardiol. 2016; 37(1):90–98. doi: 10.1007/s00246-015-1244-z . [DOI] [PubMed] [Google Scholar]
- 40.Itagaki MW. Using 3D printed models for planning and guidance during endovascular intervention: a technical advance. Diagn Interv Radiol. 2015; 21(4):338–341. doi: 10.5152/dir.2015.14469 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper.