Abstract
Objectives
Cooking interventions are used in therapeutic and rehabilitative settings; however, little is known about the influence of these interventions on psychosocial outcomes. This systematic review examines the research evidence regarding the influence of cooking interventions on psychosocial outcomes.
Methods
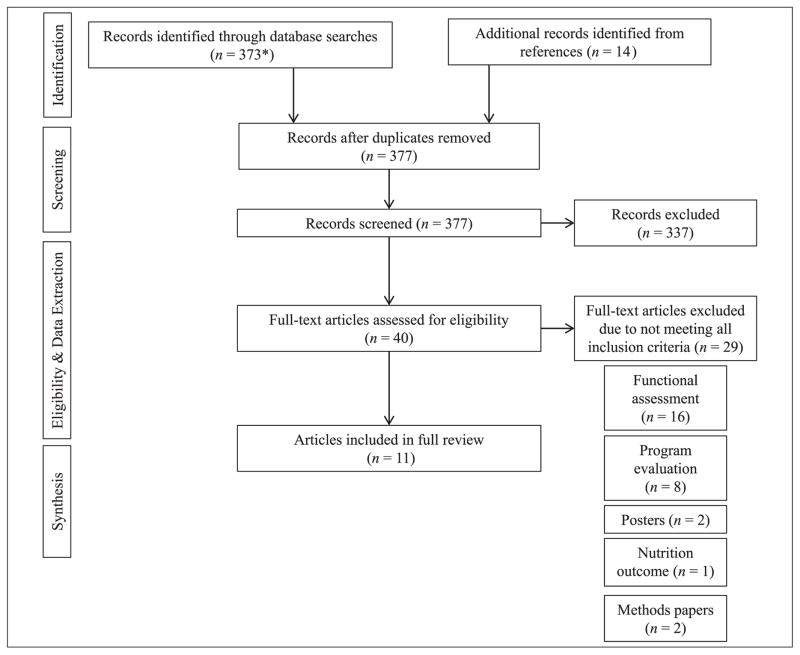
A systematic review of the literature examined peer-reviewed research using Embase, PubMed, CINALH Plus, and PsychInfo with the following search terms: cooking, culinary, baking, food preparation, cookery, occupational therapy, mental health, mood, psychosocial, affect, confidence, self-confidence, self-esteem, socialization, and rehabilitation. Inclusion criteria were the following: adults, English, influence of cooking interventions on psychosocial outcomes. PRISMA guidelines were used.
Results
The search yielded 377 articles; and 11 ultimately met inclusion criteria and were reviewed. Generally, the quality of the research was weak due to nonrandomization, unvalidated research tools, and small sample sizes. However, inpatient and community-based cooking interventions yielded positive influences on socialization, self-esteem, quality of life, and affect.
Conclusions
Finding benefits to cooking that extend beyond nutritional may be helpful in increasing motivation and frequency of cooking. This review suggests that cooking interventions may positively influence psychosocial outcomes, although this evidence is preliminary and limited. Further qualitative and rigorous quantitative research are needed to identify mechanisms by which cooking interventions may improve psychosocial outcomes.
Keywords: cooking, cooking interventions, behavior, mood, psychosocial, rehabilitation, socialization, confidence
According to the cooking hypothesis, learning to cook likely evolved as a survival mechanism; individuals learned that cooking increased the digestibility of foods and reduced harmful bacteria, ultimately enhancing survival and nutritional fitness for a population (Aiello & Wheeler, 1995; Carmody & Wrangham, 2009). Anthropologic evidence suggests that cooking influenced not only biology but also social relationships and a sense of community in early humans in that cooking contributed to and strengthened male–female pair bonds (Wrangham, Jones, Laden, Pilbeam, & Conklin-Brittain, 1999). Today, individuals are cooking at home less frequently (Drewnowski & Rehm, 2013), primarily because they lack the time to engage in cooking (Smith, Ng, & Popkin, 2013), and cooking at home is not required for an individual to access nutritious, easily digestible foods. Yet individuals remain eager to learn about cooking and seek instruction from television, magazines, the Internet, and cooking classes (Worsley, Wang, Ismail, & Ridley, 2014). Cooking TV shows are popular, and today they are one of the primary methods that individuals learn to cook (Wolfson, Bliech, Clegg Smith, & Frattaroli, 2016). The content of these shows is not entirely nutritional, suggesting that there may be characteristics of cooking beyond nutrition spurring individuals to learn to cook.
Evidence-based cooking interventions have been used to improve nutritional status, weight-related outcomes, and cooking skills, often in low-income and/or minority populations and in specific patient populations such as type 2 diabetes, cardiovascular disease, and cancer (Aycinena et al., 2017; Rees, Hinds, O’Mara-Eves, & Thomas, 2012; Reicks, Trofholz, Stang, & Laska, 2014). A review of 28 research studies found cooking interventions led to favorable changes in health status and dietary intake of fat, fiber, and sodium, and these interventions yielded positive changes in cooking self-efficacy as well as attitudes and behaviors toward cooking (Reicks et al., 2014). Similarly, cooking groups have been used to improve eating behaviors and cooking self-efficacy within specific patient populations (Clark, Bezyak, & Testerman, 2015). Guided cooking groups have also been used in patients with eating disorders, such as anorexia nervosa, to improve cooking-related motivation and ability to prepare and eat healthy meals (Lock, Williams, Bamford, & Lacey, 2012).
Particularly in the fields of occupational and rehabilitation therapy, research on cooking interventions has focused on cooking as a tool for cognitive and physical evaluation and development. Cooking is used because it is a familiar task of daily living, uses physical engagement, and involves executive function utilization (Godbout, Grenier, Braun, & Gagnon, 2005). Cooking tasks have been used to evaluate motor skills in clinical populations including those with chronic obstructive pulmonary disease (Bendixen, Waehrens, Wilcke, & Sorensen, 2014), strokes (Poole, Sadek, & Haaland, 2011), cardiovascular disease (Putzke, Williams, Daniel, Bourge, & Boll, 2000), and in the frail elderly (Provencher, Demers, Gelinas, & Giroux, 2013). Assessment of the ability to perform cooking tasks also is used to evaluate executive function planning in individuals with traumatic brain injury (Poncet et al., 2015), substance abuse (Raphael-Greenfield, 2012), strokes (Baum et al., 2008), and in the elderly (Provencher et al., 2013; M. Y. Wang, Chang, & Su, 2011).
According to social cognitive theory, individuals learn a behavior through observation and modeling, and behaviors that are positively reinforced are likely to be repeated (Bandura, 2004). Universal features of human food and nutrition systems include both cooking and social exchange of food (Bogin, 1998). Because cooking requires integration of cognitive, physical, and socioemotional processes, and learning to cook involves modeling and the mastery of skills, social cognitive theory might explain why a successful food system that relies on cooking would benefit from activity that promotes positive mood, self-confidence, and self-esteem in order to promote exchange of food and ideas. Indeed, some research exists to support the idea that cooking may improve socialization and other physical and mental health outcomes. Community kitchen programs have shown that cooking groups may help foster socialization and improve social isolation (Iacovou, Pattieson, Truby, & Palermo, 2012). In a population-based survey of 8,500 adolescents in New Zealand, Utter, Denny, Lucassen, and Dyson (2016) found self-reported cooking ability was positively associated with better family connections, greater mental well-being, and lower levels of self-reported depression. A study of elderly women in Taiwan showed that cooking frequency was related to a decrease in mortality, even when taking nutritional status and intake into account (Chen, Lee, Chang, & Wahlqvist, 2012); this study found that women who cooked more frequently participated in more health-promoting behaviors such as socialization, and fewer health risk behaviors, such as smoking. These studies represent evidence that cooking may promote psychological and social benefits that are not related exclusively to nutrition.
While cooking-related behaviors and psychosocial determinants related to barriers to cooking have been well described (Adams et al., 2015; Crookes et al., 2016; Garcia, Reardon, McDonald, & Vargas-Garcia, 2016; Mills et al., 2017), psychosocial outcomes from cooking interventions have not. We hypothesize that there may be psychosocial benefits to participating in cooking interventions that potentially have clinical and public health implications. If psychosocial benefits of cooking interventions are present, and these benefits are not attributable solely to nutrition, then there may be clinical applications of cooking interventions that extend beyond using cooking as a tool to assess cognitive and physical function or to improve nutritional status. In addition, knowledge about these benefits may help change perceptions surrounding barriers to cooking (Wolfson et al., 2016). This could have public health implications for the general public, as well as for specific, vulnerable populations. The purpose of this review is to assess the state of current research literature regarding the influence of cooking interventions on psychosocial health outcomes and to offer recommendations for future research and practice.
Method
A literature search of Embase, PubMed, CINAHL Plus, and PsychInfo was conducted with a Clinical Informationist in August 2015, December 2016, and June 2017 to identify peer-reviewed research articles examining cooking interventions and psychosocial outcomes using the following key words, phrases, and MESH terms with “and” and/or “or”: cooking, culinary, baking, cookery, food preparation, kitchen, rehabilitation, occupational therapy, mood, psychosocial, affect, confidence, self-confidence, self-esteem, socialization, and mental health. Human studies involving adults and published in English were included if they focused on psychosocial outcomes related to cooking interventions. Case studies were excluded, as were those that focused solely on cooking behavior outcomes such as cooking confidence or cooking self-efficacy. The following cooking intervention studies also were excluded unless they collected psychosocial outcomes: cooking intervention studies that focused exclusively on the assessment of physical or cognitive function, such as those using cooking tasks to assess executive function; and program evaluations, such as those assessing feasibility or participant satisfaction. Results of the search were imported into the citation manager EndNote (Thompson Reuters EndNote X6). Duplicate references were identified and deleted. Three reviewers then independently reviewed the titles and abstracts; those not meeting inclusion criteria were excluded. Each reviewer then read the full text of the remaining articles. Titles and abstracts of articles from reference lists were also screened and evaluated, when appropriate. The researchers then independently extracted key data including study objectives, research question, study type, outcomes measured, instruments, findings, limitations, and threats. In the final stage of review, reviewers independently assessed risk of bias and study rigor using the Cochrane Tool for Assessing Risk of Bias as well as PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Higgins et al., 2011; Moher, Liberati, Tetzlaff, & Altman, 2010; Sterne et al., 2016), and recommended evaluative criteria for qualitative studies (Cohen & Crabtree, 2008). Discrepancies in data analysis were infrequent and were resolved by researcher discussion.
Results
From the database and reference searches, 377 articles were identified (Figure 1). After screening the titles and abstracts, 337 records were excluded because they did not meet inclusion criteria, and 40 articles were read in full to determine eligibility. Of these, 29 articles were excluded for reasons shown in Figure 1. A total of 11 articles underwent full data extraction and are included in this review. An overview of these studies including patient characteristics, study size, cooking intervention details, assessment measures, and study findings is provided in Table 1. A narrative synthesis, grouped by psychosocial outcomes, as well as an evaluation of strengths and limitations is presented below. Assessment of risk of bias for quantitative and mixed methods studies is provided in Table 2.
Figure 1.
Flow diagram of excluded and included studies.
Table 1.
Descriptive Characteristics of Articles Reviewed.
| First author (date) |
Design | Study purpose | Population/setting | Duration (frequency) |
Interventionist | Format | Assessment/measures | Study findings related to psychosocial outcomes |
|---|---|---|---|---|---|---|---|---|
| Cooking intervention details | ||||||||
|
| ||||||||
| Barak-Nahum (2016) | Two-group comparison intervention with waitlist control | Examination of culinary group intervention on health-related quality of life and well-being | Adult cancer patients from Israeli community cancer center (intervention n = 96, 90 female; control n = 88, female 80) | 10 weeks (weekly) | Nutritionist and mental health professional | Sessions involved brainstorming, nutrition topic and shared meal with mental health– related discussion Meals based on American Cancer Society recipes |
Health-Related Quality of Life (HRQOL) Positive and Negative Affect Schedule (PNAS) Short Form 12 (SF12) Intuitive Eating Scale (IES) 24-hour recall (RECALL-24) |
Compared with controls, intervention group had significant improvement in negative affect (p = .004) and HRQOL (p = .005) Impact of the intervention on HRQOL was mediated by healthy food choices (RECALL-24) (p = .05) Impact of the intervention on negative and positive affect was mediated by Intuitive eating (p = .05; p = .01, respectively) and healthy food choices (p = .001; p = .001, respectively) |
| Crawford (1997) | Mixed methods | Evaluation of community kitchens program | Adult low-income participants in British Columbia community kitchen (n = 23 female) | 24 months (monthly) | Community worker and nutritionist | Orientation meeting and supermarket tour then cooking groups with menu planning, shopping, and food preparation for 4 to 5 entrees to take home and share | Pre- and postprogram questionnaire administered by staff addressing perceived benefits and barriers to participation and to obtaining healthy food | Postprogram, 57% of participants reported that socialization was a benefit of participation; up by 12% from preprogram beliefs |
| Engler-Stringer (2007) | Qualitative | Evaluation of social benefits of collective kitchens | Community-based adults from 21 kitchens in three Canadian cities (n = 20, gender not provided) | At least 4 months (not provided) | Community facilitator | Details of individual collective kitchen groups not provided | Individual interviews with participants examining the processes that occurred during collective kitchen planning and cooking sessions and how the experience of participation influenced everyday lives | Participants reported collective kitchens: Helped social relationships flourish Provided opportunities to socialize Reduced social isolation |
| Fitzsimmons (2003) | Randomized control trial with waitlist control group | Evaluation of participation in therapeutic cooking program in older adults with dementia | Elderly females with dementia living in a residential facility (n = 12 females) | 10 days (daily) | Recreational therapist | Two days of meal planning and shopping followed by three days of cooking sessions Cooking recipes and tasks were adapted to participant ability | Cohen–Mansfield Agitation Inventory Passivity in Dementia Scale |
Compared with controls, those in intervention group had significant improvements in agitation (p = .00) and passivity (p = .00) |
| Haley (2004) | Qualitative | Examination of mental health users’ views of engaging in baking | Adult mental health inpatients (n = 12, 2 female) | Not provided (average of 2 sessions) | Occupational therapist | Details not provided | Semistructured interviews assessing participants’ understanding of cooking group’s therapeutic goals, purpose, and structure; participant’s perspectives on the baking group experience | Participants reported baking groups helped: Increased concentration Improved coordination Built confidence Provided a sense of achievement |
| Herbert (2014)a | Two-group comparison design (intervention/waitlist control) using mixed methods | Examination of impact of a cooking program on cooking behaviors as well as social and health benefits | Community- dwelling Australian adults (intervention n = 694, female 525; control n = 237 female 198) | 10 weeks (weekly) | Program facilitators | 90-Minute groups based on learning cooking skills using fresh ingredients on a budget Shared meal at the end of session and meal for two to take home to share |
Rosenberg Global Self Esteem Scale Researcher-developed 5-point Likert-type scale to assess cooking self-efficacy (based on previously validated tools) Semistructured qualitative interviews explored impact of program on attitudes and behaviors |
Compared with control group, intervention group had significant improvements in global self-esteem from baseline to intervention conclusion (p = .02) Within intervention group, global self-esteem remained steady from conclusion to 6 months post intervention (p = .26) Participants reported more social interactions at home, including working as a household team to prepare meals |
| Hill (2007) | Mixed methods | Evaluation of therapeutic efficacy of a cooking group for burn survivors | Hospitalized adult burn patients (n = 27, 9 female) | Not provided (weekly) | Occupational therapist | Kitchen area of Rehab gym Participants cooked meal and were assigned tasks per ability level Shared meal at the end of each cooking session |
Investigator-designed 5-point Likert-type questionnaire assessed: anxiety, burn preoccupation, peer interaction, and mobility/standing tolerance Open-ended qualitative question assessed general feelings about the cooking group |
78% Strongly agreed or agreed that cooking distracted them from thinking about burns 78% strongly agreed or agreed that cooking helped them meet other people 48% strongly agreed or agreed that they experienced less anxiety in the kitchen |
| Jyväkorpi (2014) | Single-group intervention study | Evaluation of impact of nutrition education and cooking classes on diet quality, nutrient intake, and psychological Well-being | Healthy elderly individuals from Helsinki, Finland (n = 54, 49 female) | Not provided | Nutritionist and professional cooking instructor | Three sessions, conducted at community center, consisted of 1 hour of nutrition education followed by 3 hours of cooking class. Recipes and ingredients were provided | Six validated questions assessing Psychological well-being (PWB) | Participants had significant improvements in PWB from baseline to 4 months postintervention (p = .02) |
| Lee (2010) | Qualitative | Process evaluation of community kitchens | Participants from 11 community kitchens in Australia (n = 52, gender not provided) | Not provided (not provided) | Community facilitator | Details of each community kitchen not provided | Participant focus groups assessed participants’ perceptions about community kitchens | Participants reported that groups: Helped develop social skills Provided an outlet to socialize and enjoy the company of others Provided an enjoyable way to help each other in the kitchen and share information with others helped improve confidence and interpersonal skills |
| Marquis (2001) | Mixed methods | Evaluation of community kitchen programs | Community kitchen participants in British Columbia (n = 24, gender not provided) | 20 weeks (weekly) | Peer counselor | Initial session provided instruction on menu planning, self-esteem, team building On alternating weeks, groups of 4 to 5 met to cook together At conclusion, participants were encouraged to recruit friends and family to cook together at home at least 5 times within 10 weeks |
Periodic survey and focus group with participants | Socialization was a benefit of cooking kitchens Four months after completion, 80% of participants were facilitating their own cooking group After 8 months, 50% of participants were still cooking in groups |
| Tarasuk (1999) | Qualitative | Examination of the potential of community kitchens to enhance food security in population with constrained resources | Low-income participants in 6 Canadian community kitchens (n = 14, 13 female) | 4 months to 5 years (bimonthly) | Community facilitator | First sessions spent planning menu and shopping list Subsequent sessions spent preparing 4–5 main dishes that were taken home |
Qualitative interviews to assess potential of program to affect income-related food insecurity | Socialization cited as a benefit Groups contributed to a sense of “not being alone” |
Two methods articles were published related to this study that provided information regarding recruitment (Flego et al., 2014) and measurement tools (Flego et al., 2013) that are cited in this table.
Table 2.
Risk of Bias.
| First author (year) | Bias domain | Source of bias | Author’s judgment | Support for judgment |
|---|---|---|---|---|
| Randomized studies | ||||
|
| ||||
| Barak-Nahum (2016) | Selection bias | Random sequence generation | Low | Low risk due to randomization done in block groups |
| Allocation concealment | Unclear | Not discussed | ||
| Performance bias | Blinding of participants and personnel | Unclear | Blinding not addressed | |
| Detection bias | Blinding of outcome assessment | NA | Only one intervention | |
| Attrition bias | Incomplete outcome data | High risk | Potential data lost due to lack of follow-up with participants | |
| Reporting bias | Selective reporting | Low risk | All prespecified outcomes were reported | |
| Fitzsimmons (2003) | Selection bias | Random sequence generation | Unclear | Process for randomization not provided |
| Allocation concealment | Unclear | Not discussed | ||
| Performance bias | Blinding of participants and personnel | Unclear | Only one intervention, however, participants in delayed intervention group did observe intervention participant sessions. Despite this observation, the role of type of bias would have pointed the pre- and posteffect in the delayed group away from null | |
| Detection bias | Blinding of outcome assessment | NA | Only one intervention | |
| Attrition bias | Incomplete outcome data | Low | Loss of participant follow-up low due to participant location (in residential facility) and short duration of intervention | |
| Reporting bias | Selective reporting | Low | All prespecified outcomes were reported | |
|
| ||||
| First author (year) | Type of bias | Bias present | Bias level | Description of bias |
|
| ||||
| Nonrandomized studies | ||||
|
| ||||
| Crawford (1997)a | Bias due to confounding | Yes | Severe | No confounders addressed |
| Bias in selection of participants into the study | Yes | Severe | No exclusion criteria stated | |
| Bias in classification of interventions | No | NA | Single-group intervention | |
| Bias due to deviations from intended interventions | Unclear | NI | NI | |
| Bias due to missing data | Yes | Moderate | 50% of intervention group completed postintervention questionnaire and no information about missing participants was given | |
| Bias in measurement outcomes | Yes | Severe | Self-report using unvalidated outcome measures | |
| Bias in selection of reported result | Unclear | NI | NI | |
| Overall bias | Severe | |||
| Herbert (2014)a | Bias due to confounding | Yes | Low | Potential confounders controlled for in analyses |
| Bias in selection of participants into the study | Yes | Moderate | Control group comprised of individuals who registered for program 10 weeks in advance | |
| Bias in classification of interventions | No | NA | NA | |
| Bias due to deviations from intended interventions | No | NA | NA | |
| Bias due to missing data | Yes | Moderate | 55% of intervention group completed postintervention questionnaire compared with 63% of control group. Loss to follow-up in both groups over time statistically differed by age | |
| Bias in measurement outcomes | Yes | Low | Self-report using validated outcome measures | |
| Bias in selection of reported result | Unclear | NI | NI | |
| Overall bias | Low | |||
| Hill (2007) | Bias due to confounding | Yes | Severe | No confounders addressed |
| Bias in selection of participants into the study | No | NA | Exclusion criteria determined in advance | |
| Bias in classification of interventions | No | NA | Single-group intervention | |
| Bias due to deviations from intended interventions | Unclear | NI | NI | |
| Bias due to missing data | Unclear | NI | Total recruited to cooking group unknown | |
| Bias in measurement outcomes | Yes | Severe | Self-report using unvalidated outcome measures | |
| Bias in selection of reported result | Unclear | NI | NI | |
| Overall bias | Severe | |||
| Jyväkorpi (2014) | Bias due to confounding | Yes | Severe | No confounders addressed. Vitamin D supplementation, which can affect mood, was recommended to participants at start of study |
| Bias in selection of participants into the study | Unclear | NI | NI | |
| Bias in classification of interventions | No | NA | Single-group intervention | |
| Bias due to deviations | Unclear | NI | NI | |
| from intended | ||||
| interventions | ||||
| Bias due to missing data | No | NA | 90% of participants completed assessment measures | |
| Bias in measurement outcomes | Yes | Low | Self-report using six questions regarding well-being from a previously validated research study | |
| Bias in selection of reported result | Unclear | NI | NI | |
| Overall bias | Moderate | |||
| Marquis (2001)a | Bias due to confounding | Yes | Severe | No confounders addressed |
| Bias in selection of participants into the study | Unclear | NI | NI | |
| Bias in classification of interventions | Unclear | NI | NI | |
| Bias due to deviations from intended interventions | Unclear | NI | NI | |
| Bias due to missing data | PN | Low | 90% of participants completed assessment measures | |
| Bias in measurement outcomes | Yes | Severe | Self-report using unvalidated outcome measure | |
| Bias in selection of reported result | Unclear | NI | NI | |
| Overall bias | Severe | |||
Note. For nonrandomized studies, if bias is present, indicated by Yes or Probably Yes (PS), then bias level could be Low, Moderate, Severe, or Critical. If bias is not present, indicated by No, bias level is Not Applicable (NA). If presence of bias is unclear, bias level is Not Indicated (NI).
Mixed methods studies. Because Cochrane tool only applies to assessing risk of bias in quantitative studies, only quantitative aspects of study evaluated in this table.
Outcome Evaluation: Confidence and Self-Esteem
Two research studies reported changes in confidence and/or self-esteem as a result of participation in structured cooking interventions. In semistructured qualitative interviews with 12 mental health inpatients who had participated in unit-based baking classes, Haley and McKay (2004) reported that participation in baking sessions led to improved self-esteem, primarily as a result of increased concentration, coordination, and confidence. Participants reported that producing a product they could keep or give away to others as being beneficial and rewarding.
In a nonrandomized intervention study, Herbert et al. (2014) examined the influence of 10 weeks of a weekly 90-minute cooking program (Jaime Oliver’s Ministry of Food) on cooking skills and nutritional outcomes in Australian adults from communities experiencing lower socioeconomic status and high rates of obesity (Herbert et al., 2014). While the primary outcomes were skill and nutrition related, Herbert et al. (2014) found a statistically significant difference from baseline to completion in self-esteem scores (Rosenberg Global Self Esteem Scale) in members in the intervention group compared with those in the waitlist control group (p < .001). In qualitative interviews 6 months postintervention, participants who completed the intervention reported that the cooking program contributed to feelings of accomplishment and confidence, similar to themes found in Haley and McKay (2004). While self-esteem rose in the intervention group from baseline to program completion (p < .001), no changes in self-esteem were found from completion of the program to 6 months postintervention. This suggests that any influence of the cooking intervention on self-esteem occurred during the intervention and may plateau postintervention.
Outcome Evaluation: Socialization
All the studies reviewed involved repeated participation in a cooking group, and all had other group activities including either a group meal, group clean up, or group discussion, thus allowing socialization to occur. The community kitchen studies had many such group activities, and all showed a positive influence on socialization (Crawford & Kalina, 1997; Engler-Stringer & Berenbaum, 2007; Lee, McCartan, Palermo, & Bryce, 2010; Marquis, Thomson, & Murray, 2001; Tarasuk & Reynolds, 1999). Three of the other reviewed studies made reference to socialization improvements (Haley & McKay, 2004; Herbert et al., 2014; Hill, O’Brien, & Yurt, 2007). In the qualitative study involving inpatient mental health patients (Haley & McKay, 2004), participants reported that the group led to a sense of belonging, a sharing of common interests, and an opportunity to enjoy the company of others. In Hill et al.’s (2007) study involving patients hospitalized on a burn unit, all participants reported a general lack of socialization prior to the start of cooking groups, and 78% (p < .05) reported that participation in the cooking group helped them to meet people with whom they could talk about their burns. There was some evidence that socialization benefits might extend beyond the cooking interventions, as some participants continued to report improved social interactions at home and with family, and they continued to prepare meals as household teams even 6 months later (Herbert et al., 2014).
Outcome Evaluation: Mood and Affect
Hill et al. (2007) directly evaluated the impact of the cooking intervention on anxiety. In this study, 38% (n = 10) of 27 burn unit patients “strongly agreed or agreed” that they were less anxious in the kitchen after participating in cooking groups (p < .05), including all seven patients who suffered burns in kitchens at home. Seventy-eight percent “strongly agreed or agreed” that the group activity distracted them from thinking about their burns, providing one possible explanation for the reduced anxiety.
Fitzsimmons and Buettner (2003) evaluated behavioral changes in affect following participation in their clinical trial involving a cooking intervention for elderly females with dementia. Using the Cochrane-Mansfield Agitation Inventory and Passivity in Dementia Scale, they found that dementia patients randomized into the cooking intervention had improved pretest to posttest scores for agitation (p < .001) and passivity (p <.001). No changes in either agitation (p = 2.18) or passivity (p = .586) occurred in the control group.
In the sole study examining affect in a community setting, Barak-Nahum, Haim, and Ginzburg (2016) evaluated the effect of 10 weeks of a group cooking intervention on patient-reported affect in 190 cancer patients. Compared with the control group, individuals in the intervention group exhibited significant increases over time in positive affect and decreases in negative affect (p < .001, both). The researchers also examined whether intuitive eating habits and healthy food choices, both of which changed positively in the intervention group compared with controls (p < .001, both), might mediate the relationship between the intervention with positive and negative affect. The effect of the intervention on both positive (p < .05) and negative (p < .01) affect was mediated by the presence of the specific intuitive eating habit of “permission to eat” as well as by healthy food choices (p < .001, both). Regardless of group, higher scores for both healthy eating and unconditional permission to allow oneself to eat were associated with higher positive affect and lower negative affect scores.
Outcome Evaluation: Factors Affecting Well-Being and Health-Related Quality of Life
Two studies examined outcomes related to well-being or quality of life. Barak-Nahum et al. (2016) used the SF-12 Health-Related Quality of Life (HRQOL) questionnaire, a 12-item self-rated health measure of an individual’s physical and mental function, at baseline and 10 weeks after their cooking intervention for cancer patients. The researchers found a significant effect of the study group on HRQOL (p = .005), and this effect was mediated by an increase in healthy food choices (p < .05). Jyväkorpi et al. (2014) used questions that were previously validated in research to assess if a nutrition education and cooking class intervention led to changes in self-reported well-being in 59 healthy, home-dwelling individuals. The results of the intervention showed a statistically significant improvement in psychological well-being from baseline to 4 months postintervention (p = .02).
Strengths, Weaknesses, Limitations, and Bias
Overall, the reviewed studies contained significant weaknesses and limitations (Table 2); however, a few strengths are worth noting. Three studies used high-quality survey instruments that had been validated in previous research (Barak-Nahum et al., 2016; Fitzsimmons & Buettner, 2003; Herbert et al., 2014). One study, Fitzsimmons and Buettner (2003), used a pretest/posttest experimental design, whereas Herbert et al. (2014) used a large sample size and a strong repeated-measures design. Barak-Nahum et al. (2016) conducted a large community culinary intervention study with multiple mediation analyses. All the community kitchen studies used independent interviewers and triangulation of data to strengthen study findings (Crawford & Kalina, 1997; Engler-Stringer & Berenbaum, 2007; Lee et al., 2010; Marquis et al., 2001; Tarasuk & Reynolds, 1999). Unfortunately, only one of the large-scale community cooking programs used randomization (Barak-Nahum et al., 2016).
Provision for the collection of qualitative data within food and nutrition studies provides a richness and depth of understanding regarding the experience of participating in cooking interventions, potentially providing information that might be missed in quantitative questionnaires. For example, the inclusion of qualitative interviews by Herbert et al. (2014) provided valuable information about long-term influences of cooking interventions, such as reports that participants continued working as a “household team” to prepare meals 6 months postintervention. While Haley and McKay (2004) also provided an important participant-driven point of view about baking, the use of the same staff for both the intervention and the qualitative interviews may have introduced bias and calls for careful interpretation of the results.
Two studies used small sample sizes of 12 participants (Fitzsimmons & Buettner, 2003; Haley & McKay, 2004), and almost none used group randomization. Other key factors limiting the strength of the findings include the use of unvalidated, investigator-designed questions or instruments and a lack of clear descriptions of time intervals between the conclusion of the intervention and the collection of postintervention data (Crawford & Kalina, 1997; Haley & McKay, 2004; Hill et al., 2007; Marquis et al., 2001). Unfortunately, no studies used the same psychosocial outcome measurements, making it impossible to make direct cross-study comparisons. Confounding factors may have influenced the findings in the reviewed studies. For example, some interventions allowed participants to engage in outside activities or to communicate and socialize with individuals not participating in the intervention (Barak-Nahum et al., 2016), including past cooking program participants (Fitzsimmons & Buettner, 2003).
Discussion
Overall, the evidence supporting a beneficial effect of cooking interventions on psychosocial outcomes is minimal at present. While the evidence base was small, there were novel findings and similar themes among studies warranting further consideration. Despite varying types of measurement tools and different patient populations, these studies reported a positive influence associated with participation in cooking interventions on psychosocial outcomes, including self-esteem (Haley & McKay, 2004; Herbert et al., 2014), social interaction (Crawford & Kalina, 1997; Engler-Stringer & Berenbaum, 2007; Fitzsimmons & Buettner, 2003; Herbert et al., 2014; Lee et al., 2010; Marquis et al., 2001; Tarasuk & Reynolds, 1999), as well as decreased anxiety (Hill et al., 2007), psychological well-being (Jyväkorpi et al., 2014), and quality of life (Barak-Nahum et al., 2016).
There are a few overlapping explanations for the influence of cooking interventions on positive psychosocial outcomes. First, cooking is an activity that involves a mixed use of skills including parallel multitasking that relates to executive function (Cook, 2008; Provencher et al., 2013). Cognitive remediation therapy, which is designed to improve executive functioning, has been successfully used to improve anxiety and depression in psychologically and socially disadvantaged populations (Tchanturia, Lounes, & Holttum, 2014), much like the populations in some of our reviewed studies (Haley & McKay, 2004; Herbert et al., 2014; Hill et al., 2007). Another explanation is that cooking interventions might provide a “reminiscence therapy experience,” a type of group therapy that entails recalling pleasurable memories (J. J. Wang, 2007). Indeed, all the participants in the dementia study had a positive history with cooking (Fitzsimmons & Buettner, 2003).
Second, because cooking is an activity in which individuals participate daily and may be linked to acquisition of specific skills, it provides an opportunity for repeated “mastery.” This may explain why both cooking self-efficacy and self-esteem increased and plateaued at similar time intervals in Herbert et al. (2014). Whether linked to cooking self-efficacy or because of its value as an important life task, identifying cooking as a way to improve self-esteem could have public health value by affecting intrapersonal barriers to healthy living (Robinson, 2008).
Third, it may be argued that, as a result of engaging in cooking, improvements in one’s nutritional status alone may positively influence psychosocial factors, such as mood and affect. Good evidence supports the relationship between diet and mood disorders such as depression (Lopresti, Hood, & Drummond, 2013). Barak-Nahum et al.’s (2016) finding that improvements in health-related quality of life are associated with healthy food choices provides some evidence that this connection may extend beyond mood. While improvements in psychosocial outcomes may be related to improved nutritional status, the three reviewed studies conducted in inpatient settings (Fitzsimmons & Buettner, 2003; Haley & McKay, 2004; Hill et al., 2007) occurred in settings where, presumably, no changes in nutritional intake took place. This suggests that there may be other pathways whereby cooking interventions lead to improved psychosocial outcomes.
Fourth, socialization during group sessions may explain some of the positive psychosocial outcomes in the reviewed studies. Since all the reviewed studies used group-based cooking interventions, it is unclear from the studies whether the benefits found were related to the act of learning to cook or to the act of learning to cook with others. Group interaction has been used as a therapeutic modality in psychotherapy for more than 100 years (Barlow, Burlingame, & Fuhriman, 2000), and other experience-based group activities in therapeutic settings have been shown to have similar psychosocial effects (Catlin, Milliorn, & Milliorn, 1992). While two studies incorporated waitlist control groups, none added an interactive control group participating in another type of group activity. In the absence of a control group participating in another activity, one cannot determine whether the effectiveness of the intervention may be attributed to the key element of cooking or to the benefit of group interventions. The ability of these cooking group participants to experience psychosocial benefits is impressive, and these benefits were not limited exclusively to at-risk populations, as evidenced by reports of increased confidence and family socialization in both of the inpatient studies and in one community study (Fitzsimmons & Buettner, 2003; Haley & McKay, 2004; Herbert et al., 2014; Hill et al., 2007). Because of the inherent cooperative nature of community kitchens, it is not surprising that multiple community kitchens showed positive benefits in socialization (Crawford & Kalina, 1997; Engler-Stringer & Berenbaum, 2007; Lee et al., 2010; Marquis et al., 2001; Tarasuk & Reynolds, 1999). Because socialization in and of itself is a health benefit (Umberson & Montez, 2010), it may be valuable for cooking interventions in general to follow the model found in community kitchen settings by being more process rather than task oriented.
Recommendations for Future Research and Practice
There has been recent interest in developing and validating assessment measures in community-based cooking classes (Pinard, Uvena, Quam, Smith, & Yaroch, 2015), and the development of such tools is important to expanding the science in this area. Studies using adequate sample sizes and sound methodologies are needed to clarify which psychosocial patient-reported outcomes improve or are affected by engagement in cooking interventions including self-esteem, social isolation, subjective well-being, as well as symptoms such as anxiety and depression. The addition of brief psychosocial measures to cooking interventions designed to change nutritional outcomes could be a simple first step in developing a better evidence base.
As more detailed frameworks are developed examining the benefits of cooking interventions, it will be possible to explore the interconnectedness of psychosocial factors such as socialization, self-efficacy and/or mood, as well how those concepts interact with nutritional changes to lead to improved mental and physical health outcomes. For example, cooking interventions have been found to increase cooking self-efficacy (Reicks et al., 2014), and it may be valuable to evaluate the influence of gaining cooking self-efficacy on an individual’s self-esteem. Future studies using complex statistical modeling could help further explain these relationships. Such studies require large sample sizes, underscoring the importance of studies that recruit adequate numbers of participants.
An important area for further consideration involves whether psychosocial outcomes might improve in home-cooking environments. Cooking has been identified as a context-specific activity, and there are differences between an individual’s home environment and the clinical environment in which the skill of cooking is taught (Niestadt, 1994). For example, some commonly reported barriers to home cooking such as having the proper ingredients, tools, and cooking knowledge (Rees et al., 2012; Wolfson et al., 2016), might not be problematic in a planned cooking intervention. Despite these differences there may be readily transferable skills from interventions that influence psychosocial outcomes that warrant further investigation.
In conclusion, few published studies have evaluated cooking interventions in general (Rees et al., 2012; Reicks et al., 2014), and according to our review, even fewer studies have used validated assessment tools to evaluate psychosocial outcomes in cooking interventions. Our review was limited in that it focused only on published articles and therefore was not representative of the many cooking programs that occur daily in rehabilitation or occupational therapy settings and are unreported. While we made every effort to use careful database searches and strong methodology, as with any review of the literature, our findings may have had been limited by the choice and strength of our search terms and/or methods. Despite these limitations, these early findings of psychosocial benefits warrant future exploration. Findings of psychosocial outcome improvement associated with cooking interventions may encourage an increase in frequency and utilization of cooking in a variety of populations. Because sustained healthier food options may be challenging for at-risk populations with food-access difficulty, finding the pathways whereby cooking can influence psychosocial outcomes is important. Furthermore, according to social cognitive behavioral theory (Bandura, 2004), if positive influences on psychosocial factors are truly present, then there may be broader public health benefits of cooking, such as the ability of cooking to influence other positive health behavior changes.
Acknowledgments
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Adams J, Goffe L, Adamson AJ, Halligan J, O’Brien N, Purves R, … White M. Prevalence and socio-demographic correlates of cooking skills in UK adults: Cross-sectional analysis of data from the UK National Diet and Nutrition Survey. International Journal of Behavioral Nutrition and Physical Activity. 2015;12:99. doi: 10.1186/s12966-015-0261-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiello LC, Wheeler P. The expensive-tissue hypothesis—The brain and the digestive system in human and primate evolution. Current Anthropology. 1995;36:199–221. doi: 10.1086/204350. [DOI] [Google Scholar]
- Aycinena A, Jennings K, Gaffney A, Koch P, Contento I, Gonzalez M, … Greenlee H. Development of a culturally-based nutrition education curriculum for Hispanic breast cancer survivors using a theory-driven procedural model. Health Education & Behavior. 2017;44:13–22. doi: 10.1177/1090198116642236. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion by social cognitive means. Health Education & Behavior. 2004;31:143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Barak-Nahum A, Haim L, Ginzburg K. When life gives you lemons: The effectiveness of culinary group intervention among cancer patients. Social Science & Medicine. 2016;166:1–8. doi: 10.1016/j.socscimed.2016.07.046. [DOI] [PubMed] [Google Scholar]
- Barlow SH, Burlingame GM, Fuhriman A. Therapeutic applications of groups: From Pratt’s “thought control classes” to modern group psychotherapy. Group Dynamics: Theory, Research, and Practice. 2000;4:115–134. doi: 10.1037/1089-2699.4.1.115. [DOI] [Google Scholar]
- Baum CM, Connor LT, Morrison T, Hahn M, Dromerick AW, Edwards DF. Reliability, validity, and clinical utility of the Executive Function Performance Test: A measure of executive function in a sample of people with stroke. American Journal of Occupational Therapy. 2008;62:446–455. doi: 10.5014/ajot.62.4.446. [DOI] [PubMed] [Google Scholar]
- Bendixen HJ, Waehrens EE, Wilcke JT, Sorensen LV. Self-reported quality of ADL task performance among patients with COPD exacerbations. Scandinavian Journal of Occupational Therapy. 2014;21:313–320. doi: 10.3109/11038128.2014.899621. [DOI] [PubMed] [Google Scholar]
- Bogin B. From caveman cuisine to fast food: The evolution of human nutrition. Growth Hormone & IGF Research. 1998;8:79–86. doi: 10.1016/s1096-6374(98)80027-0. [DOI] [PubMed] [Google Scholar]
- Carmody RN, Wrangham RW. The energetic significance of cooking. Journal of Human Evolution. 2009;57:379–391. doi: 10.1016/j.jhevol.2009.02.011. [DOI] [PubMed] [Google Scholar]
- Catlin PA, Milliorn AB, Milliorn MR. Horticulture therapy promotes “wellness,” autonomy in residents. Provider. 1992;18(7):40. [PubMed] [Google Scholar]
- Chen RCY, Lee MS, Chang YH, Wahlqvist ML. Cooking frequency may enhance survival in Taiwanese elderly. Public Health Nutrition. 2012;15:1142–1149. doi: 10.1017/S136898001200136X. [DOI] [PubMed] [Google Scholar]
- Clark A, Bezyak J, Testerman N. Individuals with severe mental illnesses have improved eating behaviors and cooking skills after attending a 6-week nutrition cooking class. Psychiatric Rehabilitation Journal. 2015;38:276–278. doi: 10.1037/prj0000112. [DOI] [PubMed] [Google Scholar]
- Cohen DJ, Crabtree BF. Evaluative criteria for qualitative research in health care: Controversies and recommendations. Annals of Family Medicine. 2008;6:331–339. doi: 10.1370/afm.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook C. An exploration of the neural control of multitasking and the implications for practice. British Journal of Occupational Therapy. 2008;71:241–247. [Google Scholar]
- Crawford S, Kalina L. Building food security through health promotion: community kitchens. Journal of the Canadian Dietetic Association. 1997;58:197–201. [Google Scholar]
- Crookes D, Shelton R, Tehranifar P, Aycinena C, Gaffney A, Koch P, … Greenlee H. Social networks and social support for healthy eating among Latina breast cancer survivors: Implications for social and behavioral interventions. Journal of Cancer Survivorship. 2016;10:291–301. doi: 10.1007/s11764-015-0475-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A, Rehm CD. Energy intakes of US children and adults by food purchase location and by specific food source. Nutrition Journal. 2013;12:59. doi: 10.1186/1475-2891-12-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engler-Stringer R, Berenbaum S. Exploring social support through collective kitchen participation in three Canadian cities. Canadian Journal of Community. 2007;26:91–105. [Google Scholar]
- Fitzsimmons S, Buettner L. Therapeutic cooking for older adults with dementia: Effects on agitation and apathy. American Journal of Recreational Therapy, Fall. 2003:23–33. [Google Scholar]
- Flego A, Herbert J, Gibbs L, Swinburn B, Keating C, Waters E, Moodie M. Methods for the evaluation of the Jamie Oliver Ministry of Food program, Australia. BMC Public Health. 2013;13:411. doi: 10.1186/1471-2458-13-411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flego A, Herbert J, Waters E, Gibbs L, Swinburn B, Reynolds J, Moodie M. Jamie’s Ministry of Food: Quasi-experimental evaluation of immediate and sustained impacts of a cooking skills program in Australia. Plos One. 2014;9(12) doi: 10.1371/journal.pone.0114673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia A, Reardon R, McDonald M, Vargas-Garcia EJ. Community interventions to improve cooking skills and their effects on confidence and eating behavior. Current Nutrition Reports. 2016;5:315–322. doi: 10.1007/s13668-016-0185-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godbout L, Grenier MC, Braun CM, Gagnon S. Cognitive structure of executive deficits in patients with frontal lesions performing activities of daily living. Brain Injury. 2005;19:337–348. doi: 10.1080/02699050400005093. [DOI] [PubMed] [Google Scholar]
- Haley L, McKay EA. “Baking Gives You Confidence”: Users’ views of engaging in the occupation of baking. British Journal of Occupational Therapy. 2004;67:125–128. doi: 10.1177/030802260406700305. [DOI] [Google Scholar]
- Herbert J, Flego A, Gibbs L, Waters E, Swinburn B, Reynolds J, Moodie M. Wider impacts of a 10-week community cooking skills program—Jamie’s Ministry of Food, Australia. BMC Public Health. 2014:14. doi: 10.1186/1471-2458-14-1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, … Sterne JA. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill KH, O’Brien KA, Yurt RW. Therapeutic efficacy of a therapeutic cooking group from the patients’ perspective. Journal of Burn Care and Research. 2007;28:324–327. doi: 10.1097/BCR.0B013E318031A24C. [DOI] [PubMed] [Google Scholar]
- Iacovou M, Pattieson D, Truby H, Palermo C. Social health and nutrition impacts of community kitchens: A systematic review. Public Health Nutrition. 2012;16:535–543. doi: 10.1017/S1368980012002753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jyväkorpi S, Pitkälä K, Kautiainen H, Puranen T, Laakkonen M, Suominen M. Nutrition education and cooking classes improve diet quality, nutrient intake, and psychological well-being of home-dwelling older people—A pilot study. Morbidity and Mortality. 2014;1(2):4–8. [Google Scholar]
- Lee JH, McCartan J, Palermo C, Bryce A. Process evaluation of community kitchens: Results from two Victorian local government areas. Health Promotion Journal of Australia. 2010;21:183–188. doi: 10.1071/he10183. [DOI] [PubMed] [Google Scholar]
- Lock L, Williams H, Bamford B, Lacey JH. The St George’s eating disorders service meal preparation group for inpatients and day patients pursuing full recovery: A pilot study. European Eating Disorders Review. 2012;20:218–224. doi: 10.1002/erv.1134. [DOI] [PubMed] [Google Scholar]
- Lopresti AL, Hood SD, Drummond PD. A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep and exercise. Journal of Affective Disorders. 2013;148:12–27. doi: 10.1016/j.jad.2013.01.014. [DOI] [PubMed] [Google Scholar]
- Marquis S, Thomson C, Murray A. Assisting people with low income to start and maintain their own community kitchens. Canadian Journal of Dietetic Practice and Research. 2001;62:130–132. [PubMed] [Google Scholar]
- Mills S, White M, Brown H, Wrieden W, Kwasnicka D, Halligan J, … Adams J. Health and social determinants and outcomes of home cooking: A systematic review of observational studies. Appetite. 2017;111:116–134. doi: 10.1016/j.appet.2016.12.022. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- Niestadt M. Perceptual retraining for adults with diffuse brain injury. American Journal Occupational Therapy. 1994;48:225–233. doi: 10.5014/ajot.48.3.225. [DOI] [PubMed] [Google Scholar]
- Pinard C, Uvena L, Quam J, Smith T, Yaroch A. Development and Testing of a Revised Cooking Matters for Adults Survey. American Journal of Health Behavior. 2015;39:866–873. doi: 10.5993/AJHB.39.6.14. [DOI] [PubMed] [Google Scholar]
- Poncet F, Swaine B, Taillefer C, Lamoureux J, Pradat-Diehl P, Chevignard M. Reliability of the cooking task in adults with acquired brain injury. Neuropsychological Rehabilitation. 2015;25:298–317. doi: 10.1080/09602011.2014.971819. [DOI] [PubMed] [Google Scholar]
- Poole JL, Sadek J, Haaland KY. Meal preparation abilities after left or right hemisphere stroke. Archives of Physical Medicine and Rehabilitation. 2011;92:590–596. doi: 10.1016/j.apmr.2010.11.021. [DOI] [PubMed] [Google Scholar]
- Provencher V, Demers L, Gelinas I, Giroux F. Cooking task assessment in frail older adults: Who performed better at home and in the clinic? Scandinavian Journal of Occupational Therapy. 2013;20:374–383. doi: 10.3109/11038128.2012.743586. [DOI] [PubMed] [Google Scholar]
- Putzke JD, Williams MA, Daniel FJ, Bourge RC, Boll TJ. Activities of daily living among heart transplant candidates: Neuropsychological and cardiac function predictors. Journal of Heart and Lung Transplantation. 2000;19:995–1006. doi: 10.1016/s1053-2498(00)00183-2. [DOI] [PubMed] [Google Scholar]
- Raphael-Greenfield E. Assessing executive and community functioning among homeless persons with substance use disorders using the executive function performance test. Occupational Therapy International. 2012;19:135–143. doi: 10.1002/oti.1328. [DOI] [PubMed] [Google Scholar]
- Rees R, Hinds K, O’Mara-Eves A, Thomas J. Communities that cook: A systematic review of the effectiveness and appropriateness of interventions to introduce adults to home cooking. London, England: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London; 2012. [Google Scholar]
- Reicks M, Trofholz AC, Stang JS, Laska MN. Impact of cooking and home food preparation interventions among adults: Outcomes and implications for future programs. Journal of Nutrition Education and Behavior. 2014;46:259–276. doi: 10.1016/j.jneb.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson T. Applying the socio-ecological model to improving fruit and vegetable intake among low-income African Americans. Journal of Community Health. 2008;33:395–406. doi: 10.1007/s10900-008-9109-5. [DOI] [PubMed] [Google Scholar]
- Smith LP, Ng SW, Popkin BM. Trends in US home food preparation and consumption: Analysis of national nutrition surveys and time use studies from 1965–1966 to 2007–2008. Nutrition Journal. 2013;12:45. doi: 10.1186/1475-2891-12-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterne JA, Hernán MA, Reeves BC, Savovi3 J, Berkman ND, Viswanathan M, … Boutron I. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarasuk V, Reynolds R. A qualitative study of community kitchens as a response to income-related food insecurity. Canadian Journal of Dietetic Practice and Research. 1999;60:11–16. [PubMed] [Google Scholar]
- Tchanturia K, Lounes N, Holttum S. Cognitive remediation in anorexia nervosa and related conditions: A systematic review. European Eating Disorder Review. 2014;22:454–462. doi: 10.1002/erv.2326. [DOI] [PubMed] [Google Scholar]
- Umberson D, Montez J. Social relationships and health: A flashpoint for health policy. Journal of Health and Social Behavior. 2010;51(1 Suppl):S54–S66. doi: 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Utter J, Denny S, Lucassen M, Dyson B. Adolescent cooking abilities and behaviors: Associations with nutrition and emotional well-being. Journal of Nutrition Education and Behavior. 2016;48:35–41e1. doi: 10.1016/j.jneb.2015.08.016. [DOI] [PubMed] [Google Scholar]
- Wang JJ. Group reminiscence therapy for cognitive and affective function of demented elderly in Taiwan. International Journal of Geriatric Psychiatry. 2007;22:1235–1240. doi: 10.1002/gps.1821. [DOI] [PubMed] [Google Scholar]
- Wang MY, Chang CY, Su SY. What’s cooking? Cognitive training of executive function in the elderly. Frontiers in Psychology. 2011;2:228. doi: 10.3389/fpsyg.2011.00228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson JA, Bliech SN, Clegg Smith K, Frattaroli S. What does cooking mean to you? Perceptions of cooking and factors related to cooking behavior. Appetite. 2016;97:146–154. doi: 10.1016/j.appet.2015.11.030. [DOI] [PubMed] [Google Scholar]
- Worsley A, Wang W, Ismail S, Ridley S. Consumers’ interest in learning about cooking: The influence of age, gender and education. International Journal of Consumer Studies. 2014;38:258–264. doi: 10.1111/ijcs.12089. [DOI] [Google Scholar]
- Wrangham RW, Jones JH, Laden G, Pilbeam D, Conklin-Brittain N. The raw and the stolen—Cooking and the ecology of human origins. Current Anthropology. 1999;40:567–594. doi: 10.1086/300083. [DOI] [PubMed] [Google Scholar]