Abstract
Objectives
To identify patient-reported paediatric advance care planning (pACP) needs of adolescents living with HIV and to examine the congruence with their family’s perception of their needs.
Methods
A cross-sectional survey among six paediatric hospital-based outpatient HIV specialty clinics. Participants included 48 adolescent/family dyads (n=96 participants) within a larger study facilitating pACP. The main outcome measure was the Lyon Advance Care Planning Survey – Adolescent and Surrogate Versions-Revised.
Results
Adolescents’ mean age was 18 years (range ≥14–<21); 54% male; 92% African-American; 27% with prior AIDS diagnosis. If dying, 92% believed in completing an advance directive; 85% preferred to die at home;88% knowing how to say good bye; 71% being off machines that extend life and 77% dying a natural death. Best timing for end-of-life (EOL) decisions was while healthy (38%), when first diagnosed (17%), when first sick from a life-threatening illness (4%), when first hospitalised (8%), if dying (4%) and all of the above (19%). Prevalence-adjusted bias-adjusted Kappa (PABAK) measured congruence in pACP needs within adolescent/family dyads. There was substantial congruence in that being free from pain (PABAK=0.83), and understanding your treatment choices (PABAK=0.92) were very important or important. There was discordance about being off machines that extend life (PABAK=0.08) and when is the best time to bring up EOL decisions (PABAK=0.32).
Conclusions
Areas of discordance were associated with life-sustaining choices and when to have the EOL conversation. Targeted, adolescent/family-centred, evidence-based pACP interventions are needed to improve family understanding of youth’s EOL wishes.
Trial registration number
NCT01289444; Results.
INTRODUCTION
Medical advances have transformed HIV into a chronic condition,1 yet much of the treatment success has not translated to the adolescent and young adult population with HIV,2 particularly for African-American and Latino/Hispanic adolescents and young adults in the USA.3–5 HIV requires intensive life-long treatment aimed at maintaining quality of life and is therefore appropriate for advance care planning6 as part of the standard of care for paediatric/adolescent patients.7
Thus paediatric advance care planning (pACP) is appropriate for this group to ensure the adolescent’s goals of care are honoured, if the adolescent becomes unable to communicate. The value of pACP for children is increasingly recognised as contributing to quality of life,8,9 yet a knowledge gap remains about how well family members are able to accurately represent adolescents. This paper reports on the results of a pACP survey given to participants in the intervention arm of the FAmily CEntered (FACE) ACP randomised clinical trial (RCT).10 Study aims were (1) to identify patient-reported pACP needs of adolescents living with HIV/AIDS and (2) to examine the congruence of adolescent self-reported needs with their family’s perception of their end-of-life (EOL) needs.
METHOD
Design
The FACE ACP study was a multisite, two-arm RCT designed to assess the feasibility, acceptability and effectiveness of an adequately powered pACP intervention (figure 1). The FACE protocol is a standardised model of communication and decision making to prepare adolescents and their families for EOL decision making. For this study, ‘family’ refers to the surrogate decision maker or chosen person who will make decisions for the adolescent if he or she becomes unable to speak for himself/herself. The design and methods for this study have been published in detail elsewhere.10 The research reporting herein follows Strengthening the Reporting of Observational Studies in Epidemiology statement. See Strobe Checklist.
Figure 1.
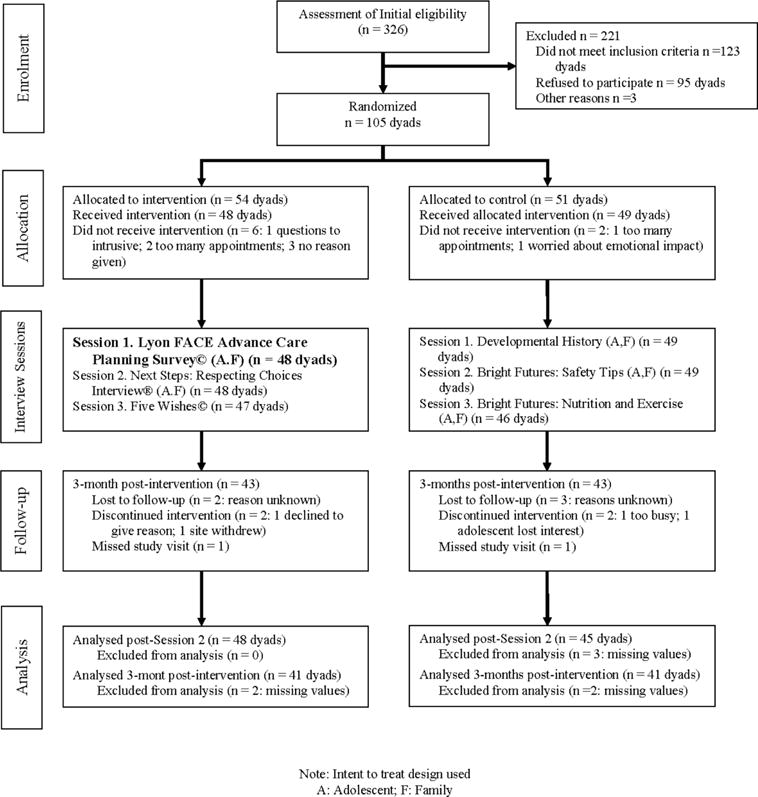
Consort diagram describing the whole trial from which these data arise.
Study participants
Between July 2010 and June 2014, adolescents aged 14–<21 years with HIV/AIDS and their healthcare surrogates were recruited from six urban paediatric hospital-based HIV specialty clinics in the geographical south of the USA: Maryland, District of Columbia, Tennessee and Florida. This region of the USA has the highest morbidity and mortality from HIV/AIDS.4 Adolescents >18 years were asked to choose a healthcare surrogate decision maker to participate in the study with them, while adolescent minors’ legal guardians participated as their surrogate. To ensure no conflict of interest or impaired decision making, potential participants were excluded if they were a ward of the state and developmentally delayed, or if on secondary screening (including surrogates) were assessed to be significantly depressed, suicidal,11 homicidal, psychotic12 or evidenced to have HIV-related dementia.13 Both adolescents and surrogate decision-makers needed to know the youth’s HIV status.
Procedure
Adolescent/family dyads were randomised to either the FACE-HIV intervention or an active control condition using a computerised 1:1 randomly permuted block design. The FACE-HIV intervention involved three sessions conducted by a certified facilitator with participants individually and included: Session 1: Lyon Advance Care Planning Survey-Adolescent and Surrogate Versions-Revised14; Session 2: Respecting Choices Interview15; and Session 3: Completion of Five Wishes, a legal advance directive document.16 The three-session active control was facilitated by a research assistant as follows: Session 1: developmental history17; Session 2: safety tips18; and Session 3: nutrition and exercise counselling.18 Each session was approximately 60 min, scheduled approximately 1 week apart. Participants were interviewed individually for session 1 and seen as a dyad for sessions 2 and 3. The results reported herein are from the Lyon Survey14 conducted in session 1.
Measures
Demographic Data Form
Demographic Data Form was administered by a trained research assistant (RA) assessor, not the survey facilitator, to obtain patient-reported sociodemographic information. Medical data were obtained by the RA assessor through chart review and abstraction.
Lyon Advance Care Planning Survey – Adolescent and Surrogate Versions-Revised
Lyon Advance Care Planning Survey – Adolescent and Surrogate Versions-Revised11,19 assessed the adolescents’ values, beliefs and life experiences with illness and EOL care, and the surrogate version assessed the legal guardian’s or family member’s perception of their adolescent’s needs using parallel items for each question. The questionnaire comprised 31 items across four domains: (1) advance care planning and preparation; (2) thoughts about death and dying; (3) dealing with dying; and (4) spiritual well-being. In this study, the original Likert scale was modified slightly to improve psychometric properties, adding a neutral item and removing ‘no response,’ yielding a 6-point Likert scale as follows: 1=very important, 2=somewhat important, 3=neither important nor unimportant, 4=not very important, 5=not at all important to 8=don’t know.
The Advance Care Planning (ACP) Survey was adapted with permission from the American Association of Retired Persons (AARP)20 and Edinger and Smucker,21 who surveyed adult patients. The adapted survey was further revised, validated and piloted with adolescents living with HIV and bereaved families of children who had died of AIDS.11,19,22 Questions were clarified, reading difficulty was lowered to sixth grade level and the number of items was reduced through meetings with community advisory boards. Although the survey can be self-administered, trained facilitators administered the surveys to all participants as an interview. This enabled the facilitator to monitor emotional reactions, ensure understanding of the questions and assure data completeness. Dyad pairs completed the survey individually in a private room. The issues raised in the survey were intended to prepare the dyad for the topics to be discussed together during the two sessions that followed. Responses were recorded by the facilitator onto a form that was later scanned into the database and verified.
Analysis
Data were entered into a REDCap Database and analysed using Base SASV.9.3. Descriptive statistics were calculated. Responses were collapsed and recoded as dichotomous variables (eg, very important or important vs otherwise) and to adjust for bias in Kappa statistics caused by imbalanced responses (eg, high prevalence of ‘very important’ responses). The prevalence-adjusted bias-adjusted Kappa (PABAK) was used for assessment of agreement.23 Interpretation of PABAK is similar to Kappa24: 1.0–0.8 almost perfect agreement; 0.79–0.6 substantial agreement; 0.59–0.4 moderate agreement; 0.39–0.2 fair agreement; 0.19–>0 slight agreement; and 0 or <0 no agreement. Fisher’s exact test was used to test significance of adolescent responses by demographic characteristics.
Ethics
The study protocol was approved by the institutional review boards of the six participating sites. All surrogates and youth participants provided written informed consent or, if under the age of 18, assent before participation, per local institutional requirements. Written consent was obtained from legal guardians for all minor participants.
RESULTS
Participant characteristics
Three hundred and twenty-six adolescent/family dyads met initial study eligibility criteria (figure 1). The data presented here report on the 48 adolescent/family dyads (n=96 total participants) in the intervention arm of the study who attended session 1 of the three-session intervention, bolded in figure 1. All completed the survey. Mean age of adolescents was 18 years (range 14–21), 54% were male, 92% were African-American and 75% were perinatally infected with HIV. Nearly one-third (27%) had an AIDS diagnosis, and all resided in states with high rates of AIDS cases for African-Americans.25 Half of adolescents (46%) had an undetectable viral load at study entry. Table 1 provides further sociodemographic characteristics of the adolescent participants. Half, 50%, of all participants lived in households with incomes below the federal poverty level.
Table 1.
Demographics of the adolescent participants (n=48)
| Demographic | N (%) |
|---|---|
| Sex | |
| Male | 26 (54.2) |
| Female | 22 (45.8) |
| Ethnicity | |
| American Indian or Alaska Native | 1 (2.1) |
| African American | 44 (91.7) |
| White | 2 (4.2) |
| Declined | 1 (2.1) |
| Sexual orientation | |
| Heterosexual | 31 (64.6) |
| Homosexual | 8 (16.7) |
| Bisexual | 7 (14.6) |
| Unknown/unreported | 2 (4.2) |
| Source of transmission | |
| Behaviourally infected | 11 (22.9) |
| Perinatally infected | 36 (75.0) |
| Other infected | 1 (2.1) |
| Known diagnosis | |
| 2 years or less | 12 (25.0) |
| More than 2 years | 36 (75.0) |
| Hospitalisation history | |
| Hospitalised in past 4 weeks (M (SD)) | 3 (6.2) |
| Hospitalised in last year (M (SD)) | 2.4 (5.8) |
| Hospitalised psychiatrically (M (SD)) | 0.6 (3.3) |
| Ever hospitalised in life (M (SD)) | 6.6 (13.7) |
| # of ER visits in your life (M (SD)) | 16.3 (35.0) |
| Age of surrogate years (M (SD)) | 46 (15.2) |
| Age of adolescent years (M (SD)) | 18 (1.9) |
ER, emergency room.
Family participants randomised to the intervention (n=48) were 83% female, 92% African-American, 29% full-time employed and 23% on disability. One-fourth, 23%, had no high school diploma and 38% had a high school diploma or General Equivalency Degree. The remainder had at least some college education. Nineteen family participants, 40%, self-reported they were HIV positive.
Adolescent preferences
Figure 2 illustrates that 78% of adolescents believed it was appropriate to initiate EOL decision making early in the course of their disease (38% before becoming ill; 17% at time of diagnosis; 4% when first ill; or 19% at each stage of illness), 13% preferred to wait until later (when first hospitalised (8%), or if dying (4%)), while 10% said they did not know (see online supplementary material). The person whom adolescents most preferred to bring up EOL decisions was their physician (56%).
Figure 2.
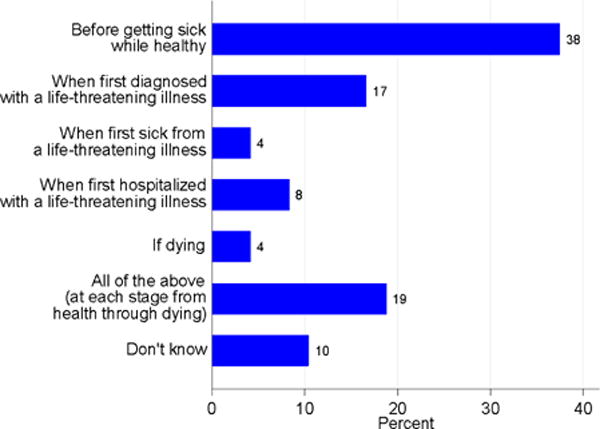
Adolescents’ self-report on best timing for end-of-life conversations
As shown in table 2, more than 90% of adolescents rated the following as very important in dealing with ‘your own dying’: H\having family and friends visit; honest answers from the doctor; being able to complete an advance directive to let loved ones know my wishes; fulfilling personal goals; and understanding my treatment choices. Although adolescents considered it important to receive honest answers from their doctor (96%), only 46% endorsed, ‘If someone could tell me when I could die, I would want to know’. Most adolescents (94%) thought it was important to say everything they wanted to say to their family if they were dying and 88% thought it was important to know how to say good bye.
Table 2.
Patient-reported end of life needs for adolescents living with HIV/AIDS
| Question | Important N (%) | Not important/or don’t know N (%) |
|---|---|---|
| How important would each of the following be to you if you were dealing with your own dying? | ||
| Family/friends visiting me | 44 (92) | 4 (8) |
| Staying in my own home | 41 (85) | 7 (15) |
| Honest answers from your doctor | 46 (96) | 2 (4) |
| Comfort from church services or persons such as a minister, priest, imam or rabbi | 31 (65) | 17 (35) |
| Planning my own funeral | 32 (68) | 15 (32) |
| Being able to complete an advance directive that would let loved ones know my wishes | 44 (92) | 4 (8) |
| Fulfilling personal goals/pleasure | 46 (96) | 2 (4) |
| Reviewing your life history with my family | 39 (81) | 9 (19) |
| Having healthcare professionals visit you at your home | 41 (85) | 7 (15) |
| Understanding your treatment choices | 46 (96) | 2 (4) |
| How important are each of the following to you when you think about dying? | ||
| Being physically comfortable | 43 (90) | 5 (10) |
| Being free from pain | 46 (96) | 2 (4) |
| Saying everything I want to say to people in my family | 45 (94) | 3 (6) |
| Being at peace spiritually | 45 (4) | 3 (6) |
| Not being a burden to loved ones | 42 (88) | 6 (12) |
| Knowing how to say good bye | 42 (88) | 6 (12) |
| Having a sense of my own worth or value | 42 (88) | 6 (12) |
| Being off machines that extend life, such as life support | 34 (71) | 14 (29) |
| Dying a natural death | 37 (77) | 11 (23) |
| Agree | Disagree/don’t know | |
| How strongly do you agree or disagree that if someone could tell me when I would die, I would want to know? | 22 (46) | 26 (54) |
| I would only take pain medicines when the pain is severe. | 31 (65) | 17 (35) |
| I would take the lowest amount of medicine possible to save larger doses for later when the pain is worse | 26 (54) | 22 (46) |
| I am afraid I will become addicted to the pain medicines over time. | 4 (8) | 42 (92) |
| When you think about death and dying, how concerned are you that you will be a burden to, or overload, my family or friends? | Concerned 22 (46) |
Not Concerned/don’t know 26 (54) |
Responses on Likert scale ranged from 1=very important, 2=somewhat important, 3=neither important nor unimportant, 4=not very important, 5=not at all important, 8=don’t know. Then regrouping as dichotomous response in the table as important=1 and 2, not important or don’t know=3, 4 and 5.
Adolescents with HIV were consistent in rating the importance to them of dying a natural death (77%) and being off machines that extend life, such as life support (71%). Most adolescents (85%) responded it would be important to stay in their own home if dying; 73% responded they had heard of hospice services. Of those who had heard of hospice, 38% knew of someone who had used hospice, while four had volunteered at a hospice service and one had used hospice services in the past. Among those who knew about hospice, half (54%) indicated they would want hospice support if they were dying.
Adolescents rarely reported having completed an advance directive (8%) despite 63% having talked to someone about their EOL wishes. Of these, 27% of the conversations were with a parent. Most adolescents (83%) thought their parent/guardian understood their wishes. The majority (88%) thought the doctor or hospital would respect their wishes about medical care and 71% believed they would be able to change their mind after making an important medical decision.
Adolescents rated their current overall health as excellent (31%), very good (40%), good (17%) and fair (13%). No association was observed between self-reported health (fair vs otherwise) and the timing preference of EOL conversations (Fisher’s exact test, Degrees of Freedom=6, value=6.4762, p=0.5144).
Adolescents feared dying painfully (71%). Nonetheless, many indicated that they might restrict administration of pain medications. Specifically, 65% reported they would only take pain medication when the pain is severe, with 54% stating they would take the least amount of pain medicine possible saving larger doses for when pain worsens. Only 8% of adolescents feared becoming addicted to pain medications and few feared their doctor might not believe they were in pain (6%).
Adolescents identified the following as worse than death: not being able to communicate their wishes for care to family and friends (54%); living with great pain (54%); and total physical dependency on others (27%). When thinking about dying, being at peace spiritually was important (94%).
Congruence
As shown in table 3, family perception of the importance of understanding treatment choices to their adolescent was almost perfect (PABAK=0.92). Nearly all dyads (94%) concurred that understanding treatment choices was important, 2% (1 dyad) agreed this was not important and 4% were not congruent about whether understanding treatment choices was important. Family accurately perceived the importance to their child of being spiritually at peace with substantial congruence (PABAK=0.75). Dyads concurred that being spiritually at peace is important (85%), while 2% were in congruence that it was not important or did not know and 13% had no congruence. Family understood that their child thought it important to be at home, if dying, with moderate congruence (PABAK=0.42). Nearly three-fourths of dyads concurred that the adolescent staying in their own home was important if dying (71%), while 29% had no congruence. No one reported it was not important or did not know.
Table 3.
The congruence on end of life needs for adolescents living with HIV/AIDS between adolescent and surrogate (n=48 dyads)
| Question | Important N (%) |
Not important/or don’t know N (%) |
PABAK |
|---|---|---|---|
| How important would each of the following be to you if you were dealing with your own dying? | |||
| Family/friends visiting me | 43 (89.6) | 0 (0) | 0.79 |
| Staying in my own home | 34 (70.8) | 0 (0) | 0.42 |
| Honest answers from my doctor | 46 (95.8) | 0 (0) | 0.92 |
| Comfort from church services or persons such as a minister, priest, imam or rabbi | 26 (54.2) | 6 (12.5) | 0.33 |
| Planning my own funeral | 19 (40.4) | 10 (21.3) | 0.23 |
| Being able to complete an advance directive that would let loved ones know my wishes | 37 (77.1) | 0 (0) | 0.54 |
| Fulfilling personal goals/pleasure | 40 (83.3) | 1 (2.1) | 0.71 |
| Reviewing my life history with my family | 29 (60.4) | 3 (6.3) | 0.33 |
| Having healthcare professionals visit you at your home | 28 (58.3) | 2 (4.2) | 0.25 |
| Understanding your treatment choices | 45 (93.8) | 1 (2.1) | 0.92 |
| How important are each of the following to you when you think about dying? | |||
| Being physically comfortable | 40 (83.3) | 1 (2.1) | 0.71 |
| Being free from pain | 44 (91.7) | 0 (0) | 0.83 |
| Saying everything I want to say to people in my family | 39 (83.0) | 1 (2.1) | 0.70 |
| Being at peace spiritually | 41 (85.4) | 1 (2.1) | 0.75 |
| Not being a burden to loved ones | 33 (68.8) | 1 (2.1) | 0.42 |
| Knowing how to say good bye | 34 (70.8) | 1 (2.1) | 0.46 |
| Having a sense of my own worth or value | 36 (75.0) | 0 (0) | 0.50 |
| Being off machines that extend life, such as life support | 23 (47.9) | 3 (6.3) | 0.08 |
| Dying a natural death | 29 (60.4) | 3 (6.3) | 0.33 |
| How comfortable are you talking about death? | Comfortable 10 (20.8) |
Not comfortable or don’t know 14 (29.2) |
0.00 |
| When you think about death and dying, | Concerned | Not concerned/don’t know | |
| how concerned are you that you will be a burden to, or overload, my family or friends? | 9 (18.8) | 14 (29.2) | −0.04 |
| I am afraid the doctor may not believe I am in pain and treat my pain | Agree 3 (6.3) |
Don’t agree/don’t know 22 (45.8) |
0.04 |
Responses on Likert scale ranged from 1=very important, 2=somewhat important, 3=neither important nor unimportant, 4=not very important, 5=not at all important, 8=don’t know. Then regrouping as dichotomous response in the table as important=1 and 2, not important or don’t know=3, 4 and 5.
PABAK, prevalence-adjusted bias-adjusted Kappa.
Family perceptions of their adolescent’s comfort with talking about death was poor (PABAK=0); 50% of dyads were discordant and only 21% of adolescent/family dyads agreed that the adolescent was comfortable talking about death. Almost half of adolescents (46%) were concerned they would be a burden to family or friends. Congruence with their families’ perception of their fears of being a burden was poor (PABAK=−0.04), with only 19% of dyads concurring that the adolescent was concerned about being a burden; 29% concurred they were not concerned about being a burden or agreed they did not know. Half (52%) of dyads did not concur about whether being a burden was a concern.
Congruence with families’ perceptions of their adolescents’ preferences for life support was slight (PABAK=0.08). Almost half of dyads (48%) concurred that ‘being off machines that extend life, such as life support’ is important; 6% thought it was not important or did not know. Discordance existed for 46% of dyads. Families reported a fair understanding of the value to their child of dying a natural death (PABAK=0.33). Dyadic congruence that dying a natural death was important to the adolescent was 60%. One-third (34%) had no congruence and 6% were in congruence that dying a natural death was not important or did not know.
Families’ perceptions of their adolescents’ fear that the doctor might not believe they were in pain was slight (PABAK=0.04). There was congruence for 6% of dyads that the doctor might not believe the adolescent is in pain and treat the pain, while for 46% of dyads there was congruence that this was not true, or they did not know. Forty-eight per cent had discordance. Although 73% of families in this study thought EOL decision-making conversations should happen early in the course of the disease, congruence between the adolescent/family dyad was slight (PABAK=0.32).
Demographic influences
Adolescent survey responses differed by mode of HIV transmission (perinatal vs non-perinatal) and income. The answer to the question ‘where to die?’ significantly differed by mode of transmission (p=0.0355). Non-perinatally infected adolescents were more likely than perinatally infected youth to choose to ‘Die in a hospital’ (33% vs 6%), less likely to choose ‘Don’t know’ (17% vs 42%), while equally likely to choose ‘At home’ (n=48, 50% vs 53%). The best timing for bringing up EOL decision making significantly differed by income (p=0.0377). Adolescents whose family income was equal or below the poverty level, compared with those with higher income, or unknown income, respectively, preferred to talk to their families about EOL treatment choices earlier in the course of their illness, when first diagnosed or ill (67% vs 58% vs 20%), rather than later, when first hospitalised or if dying (13% vs 0% vs. 60%). Poor adolescents also were less likely to prefer to talk about advance care planning at each stage of their illness (13% vs 26% vs 20%) and ‘Don’t know’ (8% vs 16% vs 0%). The importance of ‘reviewing my life with family’ also significantly differed by income (p=0.0310) with poorer adolescents preferring to review their life with their family than those with higher or unknown income, respectively (92% vs 79% vs 40%). Adolescent survey responses did not significantly differ by age, gender, race or ethnicity.
DISCUSSION
Among a cohort of adolescent patients with HIV/AIDS, survey results identified areas of congruence and discordance in families’ perceptions of their adolescents’ values and goals for pACP. Strengths and competencies of families are suggested by those results with the highest congruence: they agreed on importance of understanding treatment choices and the desire to be spiritually at peace, if dying. Nevertheless, a high prevalence of adolescent/family discordance about the timing of EOL decision making was observed whereby adolescents preferred to talk about EOL goals and values early in the course of their illness. Additionally, adolescents were also willing to consider being off life support and to die a natural death. Their families did not know this. These findings suggest priority areas for early pACP interventions. Perhaps in the same way that parents of children with incurable cancer who had accurate expectations about their child’s survivability were willing to focus treatment on integrating palliative care,26 parents of adolescents who know their youth may want early pACP would learn about and consider supporting their adolescent’s choices. Findings also capture the spirit of adolescents who may not want to know if they are dying, but who otherwise want to be involved in EOL decision making, have the opportunity to say good bye to their families and receive honest answers from their doctors, which is in keeping with the ethical principles of autonomy and justice.
Study findings are consistent with earlier preliminary studies of adolescents with chronic illnesses,19 HIV11 and cancer27 indicating that adolescents preferred to talk about their goals of care before dying, 84%, 92% and 75%, respectively. This preference not being known to their families is also consistent, further validating the current findings, and supports other research indicating that communication about goals of care is a key factor affecting chronically ill adolescents and their families.28 Ideally, these adolescent patient-informed data will improve the quality of pACP practice, especially as pACP becomes standard of care in paediatric hospitals.7 Study findings also confirm that adolescents want to have a voice in their own EOL care.28–32
Adolescents with family incomes below the poverty level were more likely to want to have the opportunity to review their life with their family and to have a discussion about EOL treatment choices earlier in the course of their illness than others. Poor children and adults are more likely to die younger33 and therefore more likely to have experienced death and dying among family and friends, making this a more salient topic for them. Perhaps those with higher incomes are more future oriented and therefore more willing to defer the conversation. Perinatally infected adolescents have more experience with hospitalisations that might account for their certainty about not wanting to die in a hospital compared with non-perinatally infected adolescents. This finding merits further research, as does the influence of the family participant’s HIV status on the adolescent.
Interestingly, in stark contrast to the pilot survey in 2011,14 in the present study, three-fourths of the adolescents had heard of hospice, more than one-third knew someone who had used hospice, four adolescents volunteered at a hospice, one adolescent had used hospice and slightly more than half would want to use a hospice, if dying. In 2011, 72% of adolescents reported they had never heard of hospice, and of those who had, only one-fourth knew someone who had used hospice. Of those who knew about hospice, only 7% would want to use hospice services, if dying.14 These findings suggest an increase in level of awareness and acceptance of hospice use among HIV-positive adolescents. The reasons for this are unclear as they do not reflect nationwide trends among adults. The National Hospice and Palliative Care Organization report on Hospice in America shows minimal increase (8.4% to 8.6%)%) of hospice use nationwide by African-Americans from 2012 to 2013 and rare use of hospice services by patients with AIDS (0.2%).34 It is comforting to know that today’s youth are better informed and more likely to access available hospice services when needed.
In contrast to adult studies,35,36 stage of illness did not influence adolescents’ attitudes about the timing of EOL conversations. One-third of adolescents had an AIDS diagnosis, almost half had a detectable viral load, and they averaged seven hospitalisations, yet at the same time no one perceived their health as poor, even the participant who had been in hospice. This finding may reflect the ‘disability paradox’ whereby patients who clearly have significant health and functional problems or intrusive symptoms do not rate their quality of life commensurate with their health.37 Discrepancies also might arise as patients adapt to illness. Because of contrast effects, negative life events may be perceived as less severe by comparison. Patients may view their illness in terms of the benefits of being alive, rather than the costs38 associated with having HIV/AIDS.
Strengths and limitations of the study
Strengths of this study include the multisite design and completion of surveys in real-world hospital-based HIV specialty clinics, which increases the generalisability of findings to clinical practice. Adolescents’ and families’ participation demonstrate a willingness to be invited early into pACP conversations. Although the sample size is relatively small, this is the largest adolescent/family dyadic sample for a pACP study in youth with HIV to date. Results may not generalise beyond the geographic south of the USA; however, the sample did capture those living in US cities with the highest HIV/AIDS mortality rates4 and AIDS cases among African-Americans.25 Validity is enhanced by replication of earlier pilot studies. With respect to the timing of pACP conversations, first hospitalisation and time of diagnosis may not be mutually exclusive. Social desirability bias may have influenced responding, if adolescents said what they thought the facilitator wanted to hear, rather than how they truly felt. To proactively prevent against such bias, facilitators were trained to be neutral during survey administration. An inherent limitation is that surveys only allow for identification of beliefs for which individuals have conscious awareness and are willing to express. As this was a cross-sectional survey, it is not possible to make any conclusions about cause and effect. Selection bias likely existed with those adolescents and families most comfortable with discussing death and dying choosing to participate, and youth who have not disclosed their diagnosis likely declining participation, potentially limiting the generalisability of the study, although half of those approached agreed to participate.
CONCLUSIONS
The focus of pACP needs to be on improving communication between competent adolescent patients and their families, as an initial step towards improving communication with treating physicians to support the youth’s engagement in health-related decisions, especially with regard to the timing of EOL decision making and treatment preferences, the area of greatest discordance.39 Next, pACP needs to become integrated into standard care and mechanisms need to be in place to ensure all interested adolescent patients and their families have access to and provision of pACP prior to a medical crisis.40 Finally, allied health professionals should be trained to provide pACP in settings where physicians do not have the time, training or willingness to do so in order to put into practice the consensus of policy makers supporting adolescent engagement in health-related decisions about their own goals for care and EOL care.
Supplementary Material
Acknowledgments
We would like to thank our adolescents and families for their participation. We would also like to thank our coinvestigators Pamela Hinds, PhD, Lawrence J. D’Angelo, MD, Natella Rakhmanina, MD and Tomas Silber, MD, Children’s National; Nancy Hutton, MD, John’s Hopkins; Ronald Dallas, PhD, Patricia Flynn, MD and Megan Wilkins, PhD, St. Jude Children’s Research Hospital; Larry Friedman, MD and Ana Garcia, PhD, University of Miami; Sohail Rana, MD and Patti Houston, Howard University Medical Center; and Ana Puga, MD and Patricia A. Garvie, PhD, Children’s Diagnostic & Treatment Center. We would like to thank our consultants Drs Beatrice Krauss and Bruce Rapkin for their participation in the Safety Monitoring Committee. We would also like to thank our research assistants, clinical coordinators as well as our healthcare providers and case managers who referred families to our study.
Funding Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number R01NR012711-06 from the National Institute of Nursing Research (NINR) at the National Institutes of Health (NIH). Space was provided through the NIH National Center for Advancing Translational Sciences Clinical Training Science Institute at Children’s National UL1TR0000075. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINR or NIH.
Footnotes
Contributors MEL is the principal investigator and together with JW conceived and designed the study, analysed and interpreted the data and drafted the article. RHD contributed to the concept, design, analyses, collection of the data, verification of the data and interpretation of the data for this manuscript and approved the final manuscript as submitted. PAG, MLW and AG contributed to the collection of the data, interpretation of the data, reviewed and revised the final manuscript and approved the final manuscript as submitted. JW and YIC analysed and verified all of data. YIC prepared all tables and figures and contributed to the interpretation of results, verification of all data and revising the manuscript. All authors have read and gave final approval of the version to be published.
Competing interests None declared.
Patient consent Obtained.
Ethics approval This study was approved by the Children’s National Institutional Review Board, IRBear no 1345, originally IRB no 4972. Children’s National was the coordinating centre. The respective institutional review board of each of the other five participating hospitals also approved the study: St Jude Children’s Research Hospital, Children’s Diagnostic & Treatment Center, Howard University Hospital, Johns Hopkins University and the University of Miami Miller School of Medicine.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement Original survey data (frequency distributions) for the adolescent and family surveys are available upon request from Dr MEL at mlyon@childrensnational.org.
References
- 1.Patel K, Wang J, Jacobson DL, et al. Aggregate risk of cardiovascular disease among adolescents perinatally infected with the human immunodeficiency virus. Circulation. 2014;129:1204–12. doi: 10.1161/CIRCULATIONAHA.113.001978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heron M. Leading causes for 2011. Nat Vital Stat Reports. 2015;64:27–59. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Fast facts: HIV among youth. http://www.cdc.gov/hiv/group/age/youth/ (accessed 1 Jul 2016).
- 4.Centers for Disease Control and Prevention (CDC) Issue Brief. HIV in the Southern United States. 2016 www.cdc.gov/hiv/pdf/policies/cdc-hiv-in-the-south-issue-brief.Pdf.
- 5.Castel AD, Kalmin MM, Hart RL, et al. Disparities in achieving and sustaining viral suppression among a large cohort of HIV-infected persons in care - Washington, DC. AIDS Care. 2016;28:1355–64. doi: 10.1080/09540121.2016.1189496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Himelstein BP, Hilden JM, Boldt AM, et al. Pediatric palliative care. N Engl J Med Overseas Ed. 2004;350:1752–62. doi: 10.1056/NEJMra030334. [DOI] [PubMed] [Google Scholar]
- 7.Weaver MS, Heinze KE, Kelly KP, et al. Palliative care as a standard of care in pediatric oncology. Pediatr Blood Cancer. 2015;62(Suppl 5):S829–S833. doi: 10.1002/pbc.25695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heckford E, Beringer AJ. Advance care planning: challenges and approaches for pediatricians. J Palliat Med. 2014;17:1049–53. doi: 10.1089/jpm.2013.0374. [DOI] [PubMed] [Google Scholar]
- 9.Liberman DB, Pham PK, Nager AL. Pediatric advance directives: parents’ knowledge, experience, and preferences. Pediatrics. 2014;134:e436–e443. doi: 10.1542/peds.2013-3124. [DOI] [PubMed] [Google Scholar]
- 10.Dallas RH, Wilkins ML, Wang J, et al. Longitudinal Pediatric Palliative Care: Quality of Life & Spiritual Struggle (FACE): design and methods. Contemp Clin Trials. 2012;33:1033–43. doi: 10.1016/j.cct.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Beck AT, Steer RA, Brown GK. Beck Depression Inventory Manual. 2nd. San Antonio, TX: The Psychological Corporation, Harvourt Brace and Co; 1996. [Google Scholar]
- 12.Shaffer D, Schwab-Stone M, Fisher P, et al. The Diagnostic Interview Schedule for Children-Revised Version (DISC-R): I. Preparation, field testing, interrater reliability, and acceptability. J Am Acad Child Adolesc Psychiatry. 1993;32:643–50. doi: 10.1097/00004583-199305000-00023. [DOI] [PubMed] [Google Scholar]
- 13.Power C, Selnes OA, Grim JA, et al. HIV Dementia Scale: a rapid screening test. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;8:273–8. doi: 10.1097/00042560-199503010-00008. [DOI] [PubMed] [Google Scholar]
- 14.Garvie PA, He J, Wang J, et al. An exploratory survey of end-of-life attitudes, beliefs, and experiences of adolescents with HIV/AIDS and their families. J Pain Symptom Manage. 2012;44:373–85. doi: 10.1016/j.jpainsymman.2011.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammes BJ, Briggs L. Respecting choices®: advance care planning facilitator manual-Revised. La Crosse, WI: Gundersen Lutheran Medical Foundation; 2007. [Google Scholar]
- 16.Towey J. The Five Wishes: Aging with dignity a service program developed through a grant from The Robert Wood Johnson Foundation. 1990 www.agingwithdignity.org/.
- 17.Barkley RA. Attention-deficit hyperactivity disorder: a clinical workbook. New York, NY: The Guilford Press; 1993. [Google Scholar]
- 18.Patrick K, Spear B, Holt K, et al. Bright Futures in Practice: National Center for Education in Maternal and Child Health. 2001 [Google Scholar]
- 19.Lyon ME, McCabe MA, Patel KM, et al. What do adolescents want? An exploratory study regarding end-of-life decision-making. Journal of Adolescent Health. 2004;35:529.e1–529.e6. doi: 10.1016/j.jadohealth.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 20.AARP. North Carolina End of Life Care Survey African American Members. AARP Report prepared by Rachelle Cummins. 2003 http://assets.aarp.org/rgcenter/health/nc_eol.Pdf.
- 21.Edinger W, Smucker DR. Advance directives survey of adult outpatients. J of Fam Prac. 1992;35:650–3. [PubMed] [Google Scholar]
- 22.Lyon ME, Garvie PA, Briggs L, et al. Development, feasibility, and acceptability of the Family/Adolescent-Centered (FACE) Advance Care Planning intervention for adolescents with HIV. J Palliat Med. 2009;12:363–72. doi: 10.1089/jpm.2008.0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Byrt T, Bishop J, Carlin JB. Bias, prevalence and kappa. J Clin Epidemiol. 1993;46:423–9. doi: 10.1016/0895-4356(93)90018-v. [DOI] [PubMed] [Google Scholar]
- 24.McGinn T, Wyer PC, Newman TB, Keitz S, Leipzig R, Guyatt G. Tips for learners of evidence-based medicine: 3. Measures of observer variability (kappa statistic) Can Med Assoc J. 2004;171:1369–73. doi: 10.1503/cmaj.1031981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention & Kaiser Family Foundation. Top 15 States by Number of Share of New AIDS Cases among Blacks, 2005. statehealthfacts.org. Data Source CDC, Special Data Request, 2007. An Overview of HIV/AIDS in Black America (July 2007), Figure 23 & 24. 2006 www.kff.org/hivaids/7660.Cfm.
- 26.Wolfe J, Klar N, Grier HE, et al. Understanding of prognosis among parents of children who died of cancer: impact on treatment goals and integration of palliative care. JAMA. 2000;284:2469–75. doi: 10.1001/jama.284.19.2469. [DOI] [PubMed] [Google Scholar]
- 27.Jacobs S, Perez J, Cheng YI, et al. Adolescent end of life preferences and congruence with their parents’ preferences: results of a survey of adolescents with cancer. Pediatr Blood Cancer. 2015;62:710–4. doi: 10.1002/pbc.25358. [DOI] [PubMed] [Google Scholar]
- 28.Hinds PS, Schum L, Baker JN, et al. Key factors affecting dying children and their families. J Palliat Med. 2005;8:s-70–s-78. doi: 10.1089/jpm.2005.8.s-70. [DOI] [PubMed] [Google Scholar]
- 29.Lyon ME, Garvie PA, McCarter R, et al. Who will speak for me? Improving end-of-life decision-making for adolescents with HIV and their families. Pediatrics. 2009;123:e199–e206. doi: 10.1542/peds.2008-2379. [DOI] [PubMed] [Google Scholar]
- 30.Hinds PS, Drew D, Oakes LL, et al. End-of-life care preferences of pediatric patients with cancer. J Clin Oncol. 2005;23:9146–54. doi: 10.1200/JCO.2005.10.538. [DOI] [PubMed] [Google Scholar]
- 31.Wiener L, Ballard E, Brennan T, et al. How I wish to be remembered: the use of an advance care planning document in adolescent and young adult populations. J Palliat Med. 2008;11:1309–13. doi: 10.1089/jpm.2008.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wiener L, Zadeh S, Battles H, et al. Allowing adolescents and young adults to plan their end-of-life care. Pediatrics. 2012;130:897–905. doi: 10.1542/peds.2012-0663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Galea S, Tracy M, Hoggatt KJ, et al. Estimated deaths attributable to social factors in the United States. Am J Public Health. 2011;101:1456–65. doi: 10.2105/AJPH.2010.300086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.National Hospice and Palliative Care Organization (NHPCO) Facts and figures: hospice care in America. 2014:1–18. http://www.nhpco.org/sites/default/files/public/Statistics_Research/2014_Facts_Figures.Pdf.
- 35.Johnston SC, Pfeifer MP, McNutt R. The discussion bout advance directives. Patient and physician opinions regarding when and how it should be conducted. Arch of Intern med. 1995;155:1025–30. doi: 10.1001/archinte.155.10.1025. [DOI] [PubMed] [Google Scholar]
- 36.Tierney WM, Dexter PR, Gramelspacher GP, et al. The effect of discussions about advance directives on patients’ satisfaction with primary care. J Gen Intern Med. 2001;16:32–40. doi: 10.1111/j.1525-1497.2001.00215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Carr AJ. Are quality of life measures patient centred? BMJ. 2001;322:1357–60. doi: 10.1136/bmj.322.7298.1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ubel PA, Loewenstein G, Jepson C. Whose quality of life? A commentary exploring discrepancies between health state evaluations of patients and the general public. Qual Life Res. 2003;12:599–607. doi: 10.1023/a:1025119931010. [DOI] [PubMed] [Google Scholar]
- 39.Feenstra B, Boland L, Lawson ML, et al. Interventions to support children’s engagement in health-related decisions: a systematic review. BMC Pediatr. 2014;14:1–11. doi: 10.1186/1471-2431-14-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. 2010;153:256–61. doi: 10.1059/0003-4819-153-4-201008170-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


