Abstract
Fear of falling presents a significant problem for many older adults by reducing physical function and increasing the risk of future falls. Several different types of interventions have improved fear of falling and a summary of efficacious interventions will help clinicians recommend treatment options. Using the Arksey and O’Malley Framework for scoping reviews, the purpose of this review was to identify efficacious interventions for treating fear of falling among community-dwelling older adults in order to provide a list of potential treatment options for care providers. A total of 45 publications were identified for inclusion in this review.
Keywords: fear of falling, falls, scoping review, older adults
Introduction
Fear of falling, defined as a “persistent feeling related to the risk of falling during one or more activities of daily living”,1 is a significant problem among older adults. The prevalence of fear of falling is between 20–39% among community-dwelling older adults.2–5 Although approximately one half of individuals who fall develop a fear of falling,6 research suggests that fear of falling is also present in people who have not fallen and is an independent risk factor for disability.7 Fear of falling has been associated with reductions in physical and social activity as well as reduced quality of life.6 Additionally, high levels of fear of falling have been shown to increase an individual’s risk of future falls, although low levels of fear of falling have been shown to have a protective effect against falls, regardless of the presence of balance impairments.8 Given the prevalence of fear of falling among community-dwelling older adults and significant impact that fear of falling can have on physical function and risk of future falls it is important for healthcare providers to assess fear of falling and consider implementing strategies to reduce fear of falling as part of a comprehensive care plan.
In the past two decades, a significant number of studies have examined the effectiveness of interventions to improve fear of falling. In 2007, Zijlstra and colleagues9 published a systematic review of interventions to reduce fear of falling in which 19 articles were eligible for inclusion. Of the effective trials included in that review, fall-related multifactorial programs were most common, followed by tai chi and exercise interventions. Since 2007, numerous studies have examined the effectiveness of fear of falling interventions and an overview of the interventions is needed to provide clinicians with options for addressing fear of falling with their patients.
Purpose
Therefore, given the significant impact that fear of falling can have on mobility, independence, and quality of life and the lack of guidelines for management of fear of falling among older adults, we sought to conduct a scoping review to answer the following question: “What interventions investigated with randomized controlled trials improve fear of falling among community-dwelling older adults?” Following the principles of the Arksey and O’Malley Framework for scoping reviews,10 we summarize the existing evidence related to interventions for the management of fear of falling and provide recommendations for interventions clinicians could consider for their patients who experience fear of falling.
Method
Eligibility and Search Strategy
A librarian with systematic review expertise helped the investigators create a search strategy to find eligible articles. Four databases, Ovid MEDLINE, CINHAL, EMBASE, and PsychINFO were searched on May 3, 2017 using a complex combination of search terms (i.e., fear*, concern*, worry*, afraid, fall, balance confidence*). The search was limited to articles published in English between 2007 and the search date, as a rigorous systematic review on fear of falling interventions for community dwelling older adults was published that year.9 To be included in the review publications had to focus on community-dwelling adults age 65 years and older, be a randomized controlled trial with a sample size of at least 60 participants, investigate an intervention lasting 6 weeks or longer, and include fear of falling as either a primary or secondary outcome. As the focus of this review is to provide evidence-based recommendations for the management of fear of falling among independently living older adults in the community, studies meeting any of the following criteria were excluded from this review: nursing home or assisted living population, mean age less than 65 years, disease specific population (e.g., Parkinson’s disease, multiple sclerosis, acute stroke, osteoporosis) and focus on rehabilitation following acute health events (e.g., stroke, paraplegia).
Abstract and Full Text Screening
All three investigators screened abstracts and full text documents for eligibility. Only one investigator reviewed each citation. When questions about eligibility arose, all three investigators reviewed the full text document and came to a consensus about eligibility. Excel spreadsheets were used to track decisions made during abstract and full text screening and the results were summarized in a flow diagram as recommended by PRISMA guidelines.11
Data Collection from Eligible Articles
All three investigators collected data from the eligible articles, but data from each publication was only abstracted by one investigator. Data was abstracted into a standardized Excel spreadsheet that elicited information on sample size and characteristics; the intervention components, setting, interventionist, and duration; follow-up period; and fear of falling measures and outcomes. It was noted whether or not the study found a statistically significant improvement in fear of falling.
Data Synthesis
As the heterogeneity between publications precluded meta-analysis and the review was designed to be scoping in nature, the tables of abstracted data were used to conduct a qualitative synthesis of findings.12 Articles were described by population, intervention type, length of follow-up period, outcomes measured, and overall findings.
Quality Assessment
The Cochrane Collaboration’s tool for assessing risk of bias was used to appraise the quality of eligible publications.13 Using this assessment tool, the reviewer rated the risk of bias in six domains (sequence generation, allocation concealment, blinding of participants, personnel, and outcome assessors, incomplete outcome data, selective outcome reporting, and other) as low, unclear, or high. Each publication was assessed by one investigator, when questions arose, all three investigators reviewed the full text document and came to a consensus on its status.
Results
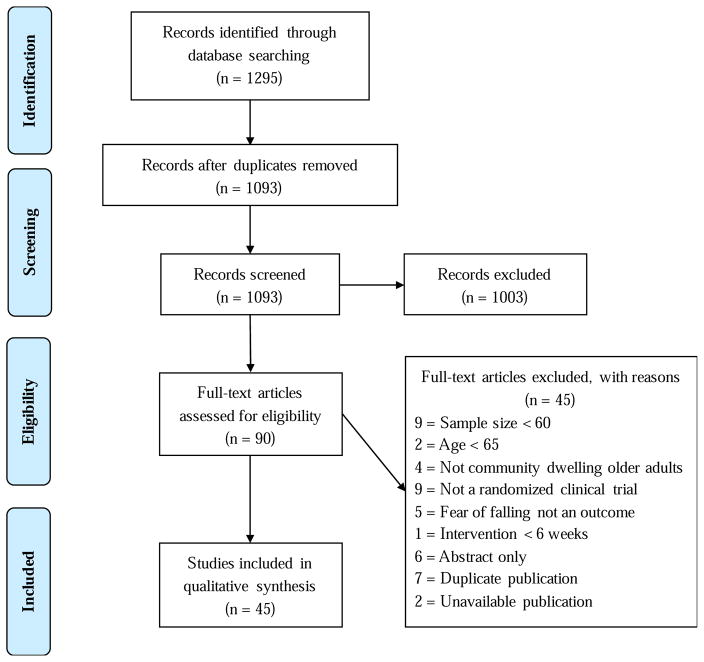
The database searches identified 1,295 citations. The reviewers screened 1,093 non-duplicative abstracts and 90 full text documents for eligibility. Figure 1 presents the number of documents identified at each stage of screening and reasons for ineligibility.
Figure 1.
Flow of records during literature search and document reviewing process.
Forty-five publications, representing 44 unique studies, were identified for inclusion in the review.14–58 Two manuscripts reported data from the same study, though reporting data from differing follow-up times.23,24 The publications included in this review summarize a variety of interventions that were designed specifically to reduce fear of falling, or report the results of studies that have included fear of falling as a secondary outcome of interest (see Table 1). Fear of falling was the primary target of the chosen intervention for nine of the studies,14–22 all of which were effective at reducing fear of falling. Twenty-three studies were designed to primarily target fall prevention,23–45 ten of these interventions were effective in reducing fear of falling.23–32 Fear of falling was the secondary outcome for 13 studies,46–58 seven of which demonstrated efficacy.46–52
Table 1.
Number of Eligible Articles (N = 45, 44 unique studies) by Intervention Target & Efficaciousness
| Intervention Target | Number of Articles | Citations |
|---|---|---|
| Fear of falling was primary target | ||
| All studies were efficacious | 9 | 14–22 |
| Fall prevention was primary target | ||
| Efficacious studies | 10 | 23–32 |
| Non-efficacious studies | 13 | 33–45 |
| Fear of falling was secondary outcome of non-fall prevention trial | ||
| Efficacious | 7 | 46–52 |
| Non-efficacious | 6 | 53–58 |
Overall, 26 of the forty-five articles included in this review (58%) reported the results of effective fear of falling interventions.14–32,46–52 Of these studies, a total of 8314 older adults were enrolled with sample sizes ranging from 60 to 1256.23,24,28 Intervention periods of the effective studies ranged from 6 weeks to 2 years, with follow-up periods over six weeks to two years.22,46 Fear of Falling was measured most frequently (n=16) using the Falls Efficacy Scale or a modified FES. Other fear of falling measures utilized included the Geriatric Fear of Falling Measure,14 Activities-specific Balance Scale,18,21 and Survey of Activities and Fear of Falling in the Elderly (SAFFE).28 A number of studies utilized the approach of asking one to two questions to evaluate fear of falling, with yes no response50 or with options designed to evaluate level of fear of falling.9,18,19,25,29,46
Efficacious Interventions
Interventions were considered effective if they reported a statistically significant fear of falling outcome improvement at any point during their follow-up period; results did not have to be sustained to be considered efficacious. The efficacious studies included interventions that were single and multi-component.
Single-component studies most often tested a form of exercise, compared exercise modalities, or exercise delivery mechanisms. The types of exercise that proved effective in reducing fear of falling were those aimed at improving strength, balance, agility, and flexibility, either specifically or in combination. Studies that used specific types of exercise included tai chi,14,26 walking,21,50 and water-based training.47 Non-exercise single component interventions included guided relaxation,22 a virtual reality trainer,28 and cognitive behavior therapy.17 Training delivery methods that were effective included Wii,15 in-home training,21,31 and group training.48
An intervention was considered multi-component when two or more differing methods of intervention were applied within one treatment arm. Defined this way, eleven studies utilized a multi-component intervention.14,16,19,20,27,29,30,46,50–52 Cognitive behavioral therapy was one of the most common components included in multi-component interventions; five studies evaluating multi-component interventions included CBT.14,16,19,20,27 CBT was coupled with tai chi,14 or included activity training as a component in their CBT protocol.16,19,20,27 Other than CBT, effective multi-component interventions included fall prevention education,29,30 vitamin D supplementation,46 whole-body vibration therapy,51 and motor training.52
Quality Assessment
Each efficacious (Table 3) and non-efficacious study (Table 4) was appraised for risk of bias.13 As expected for the type of interventions reported here, few studies reported participant blinding.22,42,43,52 Likewise, none of the interventionists were blinded, though many of the researchers took steps to keep the outcome assessors blinded (n=25). Attrition rates among the studies ranged from 0.03–0.49.
Table 3.
Quality Appraisal of Efficacious Studies
| Author, year | Intervention Target |
Sequence Generation |
Allocation Concealment |
Blinding of Participants |
Blinding of Interventionists |
Blinding of outcome assessors |
Incomplete outcome data |
Selective outcome reporting |
Other source of bias |
Attrition Rate |
|---|---|---|---|---|---|---|---|---|---|---|
| Huang, 201114 | FOF | + | + | − | ? | + | + | − | − | 0.05 |
| Kwok, 201615 | FOF | + | ? | − | − | ? | − | − | − | 0.2 |
| Zijlstra, 200916 | FOF | + | − | − | − | + | − | − | − | 0.25 |
| Dorresteijn, 201617 | FOF | + | + | − | − | + | ? | + | + | 0.2 |
| Oh, 201218 | FOF | + | ? | − | − | ? | + | + | + | 0.15 |
| van Haastregt, 201319 | FOF | + | + | − | − | − | + | + | + | 0.25 |
| Parry, 201620 | FOF | + | + | − | − | − | + | − | + | 0.25 |
| Cyarto, 200821 | FOF | + | + | − | − | + | + | + | + | 0.11 |
| Kim, 201222 | FOF | + | + | + | − | − | ? | + | + | 0.16 |
| Iliffe, 201423 | Falls | + | + | − | − | − | + | + | + | 0.34 |
| Iliffe, 201524 | Falls | ? | − | − | − | − | − | − | − | 0.44 |
| Lin, 200725 | Falls | + | − | − | − | + | − | − | − | 0.17 |
| Hwang, 201626 | Falls | + | + | − | − | + | + | + | + | 0.27 |
| Barban, 201727 | Falls | + | − | − | ? | + | + | + | + | 0.03 |
| Duque, 201328 | Falls | ? | ? | − | − | ? | + | + | + | 0.07 |
| Jeon, 201429 | Falls | + | ? | − | − | ? | + | + | + | 0.11 |
| Siegrist, 201630 | Falls | + | + | − | − | ? | − | − | − | 0.21 |
| Gallo, 201631 | Falls | ? | + | ? | − | − | − | − | − | 0.49 |
| Boongird, 201732 | Falls | + | + | − | − | + | + | + | + | 0.02 |
| Patil, 201546 | Other | − | − | − | − | ? | − | − | − | 0.1 |
| Oh, 201547 | Other | + | + | − | − | − | ? | + | + | 0.16 |
| Sheffield, 201348 | Other | ? | ? | − | − | − | − | + | + | 0.33 |
| Freiberger, 201349 | Other | + | − | − | − | − | + | + | + | 0.14 |
| Yamada, 201250 | Other | + | + | − | − | + | + | + | − | 0.08 |
| Pollock, 201251 | Other | + | + | − | − | + | + | + | + | 0.27 |
| Schoene, 201552 | Other | + | + | + | − | + | + | + | + | 0.1 |
Note: (−) indicates “high risk of bias”, (+) indicates “low risk of bias”, and (?) indicates “unclear risk of bias”.
Table 4.
Quality Appraisal of Non-Efficacious Studies
| Record Number | Intervention Target |
Sequence Generation |
Allocation Concealment |
Blinding of Participants |
Blinding of Interventionists |
Blinding of Outcome Assessors |
Incomplete Outcome Data |
Selective Outcome Reporting |
Other Source of Bias |
Attrition Rate |
|---|---|---|---|---|---|---|---|---|---|---|
| Frieberger, 201233 | Falls | + | + | − | − | ? | − | − | − | 0.26 |
| Pighills, 201134 | Falls | − | − | − | − | + | − | − | − | 0.24 |
| Karinkanta, 201235 | Falls | + | − | − | ? | ? | − | − | + | 0.2 |
| Zhao, 201636 | Falls | + | − | − | − | ? | − | − | − | 0.08 |
| El-Khoury, 201537 | Falls | + | + | − | − | + | + | + | + | 0.19 |
| Gawler, 201638 | Falls | + | + | − | ? | ? | − | + | + | 0.52 |
| Cockayne, 201739 | Falls | + | + | ? | − | − | + | + | + | 0.12 |
| Vind, 201040 | Falls | + | ? | − | − | + | + | + | + | 0.07 |
| Markle-Reid, 201041 | Falls | + | + | − | − | + | + | + | + | 0.16 |
| Corrie, 201542 | Falls | + | ? | + | − | + | + | + | + | 0.1 |
| Gschwind, 201543 | Falls | + | + | + | − | + | − | + | + | 0.18 |
| Logghe, 200944 | Falls | + | + | − | − | + | + | + | + | 0.07 |
| Talley, 201445 | Falls | + | + | − | − | + | + | + | + | 0.07 |
| Gitlin, 200853 | Other | ? | − | − | − | + | + | − | − | 0.11 |
| Scheffer, 201254 | Other | − | − | − | − | − | − | − | − | 0.33 |
| Beyer, 200755 | Other | + | ? | − | − | − | ? | + | + | 0.22 |
| Wu, 201056 | Other | + | ? | − | − | ? | ? | + | + | 0.2 |
| Metzelthin, 201357 | Other | + | − | − | − | + | + | + | + | 0.22 |
| Kim, 201158 | Other | + | ? | ? | ? | ? | − | + | − | 0.03 |
Note: (−) indicates “high risk of bias”, (+) indicates “low risk of bias”, and (?) indicates “unclear risk of bias”.
Discussion
Numerous studies have examined interventions to reduce fear of falling in the past 10 years. The interventions found to be effective in this review are similar to those summarized by Zijlstra and colleagues.9 This scoping review also extends the results of the systematic review conducted by Zijlstra and colleagues9 by including 44 additional studies examining fear of falling interventions. In both reviews, the effective interventions typically were multi-component programs that included exercise (primarily balance and strength training or tai chi) and cognitive behavioral therapy.
Characteristics that were common among effective interventions included ongoing support such as weekly sessions, extended treatment periods and booster sessions.16,19,20 Studies showing statistically significant improvement also included those based on previously established effective fear of falling interventions such as A Matter of Balance17,19 or protocols based on prior work.14,16,24 In contrast, fear of falling was not the primary aim of any of the non- effective interventions. In addition, non-effective studies included un-supervised interventions and interventions that did not include ongoing supportive contact.34,54 Non-effective treatments also included one-time assessments without resources for participants to carry out the recommended improvements,34 though a similar study where resources were provided was also ineffective.53 However, 84% of the non-effective studies had intervention dosing and follow-up durations similar to the effective interventions.
There were some conflicting findings. For example, tai chi was included as the exercise coupled with CBT in an intervention that demonstrated improvement in fear of falling, but did not result in improvement in fear of falling when used independently in three trials.36,44,56 This was also true of the varying types of single-component exercise training interventions. Among the effective interventions, eight of the included studies15,18,23–26,28,32 demonstrated improvement in fear of falling, when using exercise to improve functionality, while nine trials that also utilized exercise were non-effective.33,35–39,44,55,56
Implications for Clinical Practice
Although the importance of fear of falling intervention is clearly established in our review, this review did not reveal clear recommendations regarding clinical intervention and screening. However, the high prevalence and impact of fear of falling on function indicate a need to proactively identify patients experiencing fear of falling and to provide an intervention plan and resources. We recommend clinicians begin by identify patients for whom intervention is most effective and are most at risk for fear of falling. Fear of falling could be assessed using a validated tool, such as the FES, SAFFE, etc. as well using a single item similar to those used by many of the articles included in this review. Finally, the clinician should assess the patient’s interest in participating in fear of falling interventions. Interventions have been trialed in home and community group settings, with varying degrees of success in terms of fear of falling and intervention adherence.59 Similarly, no form of exercise has shown better efficacy than any other, although many studies have included strength and balance training in some format.14,17,60,61 Evidence does suggest that combining psychotherapy and exercise is most effective,9,14,59 and we recommend patients receive the referrals and resources necessary to initiate both simultaneously.
It is important to note that the majority of the included studies examined an intervention (often multi-component) when compared to usual care. Given the lack of head-to-head comparisons of different types of interventions or intervention components, there is no clear consensus as to which type of intervention is best. Rather, the most appropriate evidence-based recommendation given the current state of the literature is to determine which intervention is the best fit for a patient and his or her circumstances. Engaging in an intervention (such as multi-component programs, exercise, CBT) has consistently been shown to be superior to standard care and thus some type of action is recommended. Further research should examine the effectiveness of different types of interventions in comparison to one another, as well as examine the intervention components that are most efficacious, to provide clinicians with guidance as to which interventions should be preferentially selected.
Limitations and Strengths
There are several limitations to the present review. Most studies available have targeted falls and examined fear of falling among older adults as a secondary outcome. Additionally, most of these studies have been done with individuals who have experienced a previous fall, thus little is known about the effects of these programs in the prevention of fear of falling with or without a history of falls. Future research is needed to examine the efficacy of such programs in individuals who have not fallen, as fear of falling is present in older adults who have not fallen and is an independent risk factor for disability.7 Additionally, there are little data available reporting long-term outcomes of interventions to reduce fear of falling (longest duration study was 2 years46), so we are unable to comment on the potential long-term effects of the proposed interventions. Similarly, there have not been any studies that have conducted direct comparisons of different modes of exercise training (e.g., aerobic, resistance, balance), and so we are unable to make specific recommendations on the type of exercise. Future studies should consider the implications of reducing fear of falling on long-term outcomes such as disability and quality of life and evaluate the comparative effectiveness of different types of exercise programs.
Despite these limitations, there are a number of key strengths to the present scoping review. This scoping review includes a wide variety of interventions that provide the clinician with the opportunity to tailor the intervention to a specific individual. For example, a patient with significant fear of falling and visual impairment due to cataracts may experience reduced fear of falling following surgical cataract repair, but may benefit from both CBT and environmental hazard modification. Alternatively, an older adult with fear of falling without visual impairment would not benefit from this strategy. Thus, this review provides a menu of evidence-based strategies that may be helpful for and appealing to specific patients.
Conclusion
In this scoping review, we summarized efficacious evidence-based interventions that care providers should consider for patients with fear of falling. Fear of falling can have a substantial impact on physical function of older adults and increase their risk of future falls. Thus, it is important for healthcare providers to assess fear of falling and consider implementing strategies to reduce fear of falling as part of a comprehensive care plan.
Table 2.
Characteristics of Efficacious Studies
| Author, Year | Primary Target | Design/Intervention | Duration | Follow-up period | N | Sample Description | FOF Measure(s) |
|---|---|---|---|---|---|---|---|
| Huang, 201114 | FOF | 3 arms: CBT; CBT + tai chi; control | 2 months | 5 months | 186 | 60+ yrs, community dwelling | Geriatric Fear of Falling Measure FES |
| Kwok, 201615 | FOF | 2 arms: Wii exercise; gym exercise | 3 months | 6 months, 12 months | 80 | community dwelling 60+ yrs; not routine exercisers | Modified FES |
| Zijlstra, 200916 | FOF | 2 arms: multi- component with CBT; control | 2 months + 1 session at 6 months | 12 months | 540 | 70+ yrs, community dwelling with FOF or activity avoidance | Single item: Are you concerned about falling? (1–5) Single item: Do you avoid certain activities due to concerns about falling? (1–5) Frenchay Activities Index |
| Dorresteijn, 201617 | FOF | 2 arms: home- based CBT program; usual care | 5 months | 5 months, 12 months | 389 | 70+ yrs, fair or poor perceived health, concern about falling and activity avoidance | FES-I FES-IAB (activity avoidance) GARS |
| Oh, 201218 | FOF | 2 arms: education + exercise; education only | 3 months | 3 months | 65 | 65+ yrs, community dwelling, fallen in previous year | Single item: How afraid are you of falling down? (0–4) ABC Scale – Korean version |
| van Haastregt, 201319 | FOF | 2 arms: multi- component (CBT, environmental modification, exercise); control | 14 months | 2 months, 8 months, 14 months | 540 | 70+ yrs, report some fear of falling and activity avoidance | Single item: Are you afraid of falling? (0–4) Single item: Do you avoid certain activities due to fear of falling? (0–4) |
| Parry, 201620 | FOF | 2 arms: STRIDE – CBT-based intervention; control | 2 months | 12 months | 415 | 60+ yrs, community dwelling, express fear of falling | FES-I Single item: Fear of falling (0– 10) |
| Cyarto, 200821 | FOF | 3 arms: home- based resistance and balance training; group- based resistance and balance training; group based walking | 5 months | 5 months | 9 clusters, 167 participants | 65–96 yrs, independently living retirement village residents | ABC Scale |
| Kim, 201222 | FOF | 2 arms: guided relaxation with imagery; guided relaxation | 6 weeks | 6 weeks | 91 | 60+ yrs, report a fear of falling | 7-item FES-I |
| Iliffe, 201423 and Iliffe, 201524 | Falls | 3 arms: group- based exercise (FaME); home based exercise (Otago); usual care | 6 months | 18 months | 1256 | 65+ yrs, able to take part in exercise class | Confidence in Balance scale FES-I |
| Lin, 200725 | Falls | 3 arms: education, home safety and modification; exercise training | 4 months | 8 months | 150 | 65+ years, recent fall | VAS (0–10) |
| Hwang, 201626 | Falls | 2 arms: tai chi; lower extremity training | 6 months | 6 months, 18 months | 456 | 60+ yrs, had a fall- related emergency department visit at least 6 months ago, ambulate independently | FES-I |
| Barban, 201727 | Falls | 4 arms: motor training only (stretching, balance, gait); motor + cognitive exercises delivered via i-walker; cognitive training only; control | 3 months | 6 months | 496 | 65+ yrs, at risk of falling | FES-I |
| Duque, 201328 | Falls | 2 arms: balance training; usual care | 6 weeks | 6 weeks, 9 months | 60 | 65+ yrs, at least 1 fall in the previous 6 months, poor balance (posturography) | SAFFE |
| Jeon, 201429 | Falls | 2 arms: multi- component (strength, balance, education); control | 3 months | 3 months | 70 | 65+ yrs, female, residing in rural area, at least 3 falls in previous year | Single item: Do you fear falling? (0–3) FES |
| Siegrist, 201630 | Falls | 2 arms: muscle strengthening and balance training; usual care | 4 months | 12 months | 378 | older adults, independently living, at high risk for falling | FES-I |
| Gallo, 201631 | Falls | 2 arms: individualized home-based exercise program; usual care | 6 months | 6 months | 69 | 65+ yrs, living independently, at risk of falling | ABC Scale |
| Boongird, 201732 | Falls | 2 arms: home- based exercise program (modified Otago); control | 12 months | 6 months | 439 | older adults, balance impairment unrelated to neurological condition | FES – Thai version |
| Patil, 201646 | Other | 4 arms: vitamin D + exercise; vitamin D only; placebo + exercise; placebo only | 24 months | 24 months | 409 | home-dwelling women with fall in previous year | FES-I VAS (0–100) |
| Oh, 201547 | Other | 2 arms: water- based exercise; land based exercise | 10 weeks | 10 weeks | 80 | 65+ yrs, more than 1 fall in previous 3 months, not regular exercisers | Modified FES |
| Sheffield, 201348 | Other | 2 arms: individualized assessment with adaptive equipment and home modifications; control | 3 months | 3 months | 90 | 65+ yrs, currently receiving some sort of agency service (significant impairments in ADLs) | FES-I |
| Freiberger, 201349 | Other | 2 arms: complex exercise (balance, gait, muscle strength, body awareness, motor coordination, self- efficacy); usual care | 4 months | 4 months | 33 clusters, 378 participants | 65+ yrs, one or more fall in past 12 months or fear of falling or physical fall risk | FES-I – German version |
| Yamada, 201250 | Other | 2 arms: pedometer based walking; control | 6 months | 6 months | 87 | older adults, community dwelling, sedentary | Single item: Are you afraid of falling? (yes/no) |
| Pollock, 201251 | Other | 2 arms: whole body vibration; exercise | 2 months | 6 months | 77 | frail older fallers | FES-I |
| Schoene, 201552 | Other | 2 arms: interactive videogame for cognitive-motor step training; control | 3 months | 4 months | 90 | 70+ yrs, independent living | Icon-FES |
Abbreviations: ABC = Activity-specific Balance Confidence; FES = Falls Efficacy Scale; FOF = Fear of Falling; GARS = Groningen Activity Restriction Scale; SAFFE = Survey of Activities and Fear of Falling in the Elderly; VAS = Visual Analogue Scale;
Acknowledgments
The authors would like to thank Liz Weinfurter, MLIS for her valuable assistance in conducting the database search. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Abbreviations
- ABC
Abilities-Specific Balance Confidence Scale
- FES
Falls Efficacy Scale
- FES-I
Falls Efficacy Scale – International
- FOF
Fear of Falling
- GARS
Groningen Activity Restriction Scale
- RCT
randomized controlled trial
- SAFFE
Survey of Activities and Fear of Falling in the Elderly
- VAS
Visual Analogue Scale
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Kumar A, Delbaere K, Zijlstra GAR, et al. Exercise for reducing fear of falling in older people living in the community: Cochrane systematic review and Meta-Analysis. Age Ageing. 2016;45(3):345–352. doi: 10.1093/ageing/afw036. [DOI] [PubMed] [Google Scholar]
- 2.Arfken CL, Lach HW, Birge SJ, Miller JP. The prevalence and correlates of fear of falling in elderly persons living in the community. Am J Public Health. 1994;84(4):565–570. doi: 10.2105/AJPH.84.4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Friedman SM, Munoz B, West SK, Ruben GS, Fried LP. Falls and fear of falling: Which comes first? A longitudinal secondary prevention study. J Am Geriatr Soc. 2002;50(8):1329–1335. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 4.Lach HW. Incidence and risk factors for developing fear of falling in older adults. Public Health Nurs. 2003;22(1):45–52. doi: 10.1111/j.0737-1209.2005.22107.x. [DOI] [PubMed] [Google Scholar]
- 5.Bertera EM, Bertera RL. Fear of falling and activity avoidance in a national sample of older adults in the United States. Health Soc Work. 2008;33(1):54–62. doi: 10.1093/hsw/33.1.54. [DOI] [PubMed] [Google Scholar]
- 6.Legters K. Fear of falling. Phys Ther. 2002;82(3):264–272. [PubMed] [Google Scholar]
- 7.Scheffer AC, Schuurmans MJ, Van dijk N, Van der hooft T, De rooij SE. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37(1):19–24. doi: 10.1093/ageing/afm169. [DOI] [PubMed] [Google Scholar]
- 8.Delbaere K, Close JCT, Brodaty H, Sachdev P, Lord SR. Physiological risk of falling among elderly people: Cohort Study. BMJ. 2010;341:c4165. doi: 10.1136/bmj.ABSTRACT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zijlstra GAR, Van Haastregt JCM, Van Rossum E, Van Eijk JTM, Yardley L, Kempen GIJM. Interventions to reduce fear of falling in community-living older people: A systematic review. J Am Geriatr Soc. 2007;55(4):603–615. doi: 10.1111/j.1532-5415.2007.01148.x. [DOI] [PubMed] [Google Scholar]
- 10.Arksey H, Malley LO. Scoping studies: Towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2010;8(2010):b2535. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levac D, Colquhoun H, Brien KKO. Scoping studies: Advancing the methodology. Implement Sci. 2010;5(69) doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration; 2011. [updated March 2011] Available from http://handbook.cochrane.org. [Google Scholar]
- 14.Huang TT, Yang LH, Liu CY. Reducing the fear of falling among community-dwelling elderly adults through cognitive-behavioural strategies and intense Tai Chi exercise: A randomized controlled trial. J Adv Nurs. 2011;67(5):961–971. doi: 10.1111/j.1365-2648.2010.05553.x. [DOI] [PubMed] [Google Scholar]
- 15.Kwok BC, Pua YH. Effects of WiiActive exercises on fear of falling and functional outcomes in community-dwelling older adults: A randomised control trial. Age Ageing. 2016;45(5):621–628. doi: 10.1093/ageing/afw108. [DOI] [PubMed] [Google Scholar]
- 16.Zijlstra GAR, Van Haastregt JCM, Ambergen T, et al. Effects of a multicomponent cognitive behavioral group intervention on fear of falling and activity avoidance in community-dwelling older adults: Results of a randomized controlled trial. J Am Geriatr Soc. 2009;57(11):2020–2028. doi: 10.1111/j.1532-5415.2009.02489.x. [DOI] [PubMed] [Google Scholar]
- 17.Dorresteijn TA, Zijlstra GA, Ambergen AW, Delbaere K, Vlaeyen JW, Kempen GI. Effectiveness of a home-based cognitive behavioral program to manage concerns about falls in community-dwelling, frail older people: results of a randomized controlled trial. BMC Geriatr. 2016;16(1):2. doi: 10.1186/s12877-015-0177-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oh DH, Park JE, Lee ES, et al. Intensive exercise reduces the fear of additional falls in elderly people: Findings from the Korea falls prevention study. Korean J Intern Med. 2012;27(4):417–425. doi: 10.3904/kjim.2012.27.4.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Haastregt JCM, Zijlstra GAR, Hendriks MRC, Goossens MEJB, van Eijk JTM, Kempen GIJM. Cost-Effectiveness of an intervention to reduce fear of falling. Int J Technol Assess Health Care. 2013;29(3):219–226. doi: 10.1017/S0266462313000275. [DOI] [PubMed] [Google Scholar]
- 20.Parry SW, Bamford C, Deary V, et al. Cognitive–behavioural therapy-based intervention to reduce fear of falling in older people: Therapy development and randomised controlled trial – the strategies for increasing independence, confidence and energy (STRIDE) study. Health Technol Assess (Rockv) 2016;20(56):1–206. doi: 10.3310/hta20560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cyarto EV, Brown WJ, Marshall AL, Trost SG. Comparative effects of home- and group-based exercise on balance confidence and balance ability in older adults: Cluster randomized trial. Gerontology. 2008;54(5):272–280. doi: 10.1159/000155653. [DOI] [PubMed] [Google Scholar]
- 22.Kim BH, Newton RA, Sachs ML, Glutting JJ, Glanz K. Effect of guided relaxation and imagery on falls self-efficacy: A randomized controlled trial. J Am Geriatr Soc. 2012;60(6):1109–1114. doi: 10.1111/j.1532-5415.2012.03959.x. [DOI] [PubMed] [Google Scholar]
- 23.Iliffe S, Kendrick D, Morris R, et al. Multicentre cluster randomised trial comparing a community group exercise programme and home-based exercise with usual care for people aged 65 years and over in primary care. Health Technol Assess (Rockv) 2014;18(49):1–105. doi: 10.3310/hta18490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iliffe S, Griffin M, Haworth D, et al. Promoting physical activity in older people in general practice: ProAct65+ cluster randomised controlled trial. Br J Gen Pract. 2015;65(640):e731–e738. doi: 10.3399/bjgp15X687361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin M-RR, Wolf SL, Hwang H-FF, Gong S-YY, Chen C-YY. A randomized, controlled trial of fall prevention programs and quality of life in older fallers. J Am Geriatr Soc. 2007;55(4):499–506. doi: 10.1111/j.1532-5415.2007.01146.x. [DOI] [PubMed] [Google Scholar]
- 26.Hwang HF, Chen SJ, Lee-Hsieh J, Chien DK, Chen CY, Lin MR. Effects of home-based tai chi and lower extremity training and self-practice on falls and functional outcomes in older fallers from the emergency department: A randomized controlled trial. J Am Geriatr Soc. 2016;64(3):518–525. doi: 10.1111/jgs.13952. [DOI] [PubMed] [Google Scholar]
- 27.Barban F, Annicchiarico R, Melideo M, et al. Reducing fall risk with combined motor and cognitive training in elderly fallers. Brain Sci. 2017;7(2) doi: 10.3390/brainsci7020019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duque G, Boersma D, Loza-Diaz G, et al. Effects of balance training using a virtual-reality system in older fallers. Clin Interv Aging. 2013;8:257–263. doi: 10.2147/CIA.S41453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jeon MY, Jeong H, Petrofsky J, Lee H, Yim J. Effects of a randomized controlled recurrent fall prevention program on risk factors for falls in frail elderly living at home in rural communities. Med Sci Monit. 2014;20:2283–2291. doi: 10.12659/MSM.890611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Siegrist M, Freiberger E, Geilhof B, et al. Fall prevention in a primary care setting. Dtsch Ärzteblatt Int. 2016;113(21):365–372. doi: 10.3238/arztebl.2016.0365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gallo E, Stelmach M, Frigeri F, Ahn D-H. Determining whether a dosage-specific and individualized home exercise program with consults reduces fall risk and falls in community-dwelling older adults with difficulty walking. J Geriatr Phys Ther. 2016:1. doi: 10.1519/JPT.0000000000000114. [DOI] [PubMed] [Google Scholar]
- 32.Boongird C, Keesukphan P, Phiphadthakusolkul S, Rattanasiri S, Thakkinstian A. Effects of a simple home-based exercise program on fall prevention in older adults: A 12-month primary care setting, randomized controlled trial. Geriatr Gerontol Int. 2017:1–7. doi: 10.1111/ggi.13052. [DOI] [PubMed] [Google Scholar]
- 33.Freiberger E, Häberle L, Spirduso WW, Rixt Zijlstra GA. Long-term effects of three multicomponent exercise interventions on physical performance and fall-related psychological outcomes in community-dwelling older adults: A randomized controlled trial. J Am Geriatr Soc. 2012;60(3):437–446. doi: 10.1111/j.1532-5415.2011.03859.x. [DOI] [PubMed] [Google Scholar]
- 34.Pighills AC, Torgerson DJ, Sheldon TA, Drummond AE, Bland JM. Environmental assessment and modification to prevent falls in older people. J Am Geriatr Soc. 2011;59(1):26–33. doi: 10.1111/j.1532-5415.2010.03221.x. [DOI] [PubMed] [Google Scholar]
- 35.Karinkanta S, Nupponen R, Heinonen A, et al. Effects of exercise on health-related quality of life and fear of falling in home-dwelling older women. J Aging Phys Act. 2012;20(2):198–21417p. doi: 10.1123/japa.20.2.198. [DOI] [PubMed] [Google Scholar]
- 36.Zhao Y, Chung PK, Tong TK. Effectiveness of a community-based exercise program on balance performance and fear of falling in older nonfallers at risk for falling: A randomized, controlled study. J Aging Phys Act. 2016;24(4):516–524. doi: 10.1123/japa.2015-0224. [DOI] [PubMed] [Google Scholar]
- 37.El-Khoury F, Cassou B, Latouche A, Aegerter P, Charles M-A, Dargent-Molina P. Effectiveness of two year balance training programme on prevention of fall induced injuries in at risk women aged 75–85 living in community: Ossébo randomised controlled trial. BMJ. 2015;351:h3830. doi: 10.1136/bmj.h3830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gawler S, Skelton DA, Dinan-Young S, et al. Reducing falls among older people in general practice: The ProAct65+ exercise intervention trial. Arch Gerontol Geriatr. 2016;67:46–54. doi: 10.1016/j.archger.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 39.Cockayne S, Adamson J, Clarke A, et al. Cohort randomised controlled trial of a multifaceted podiatry intervention for the prevention of falls in older people (The REFORM Trial) PLoS One. 2017;12(1):1–15. doi: 10.1371/journal.pone.0168712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vind AB, Andersen HE, Pedersen KD, Joergensen T, Schwarz P. Effect of a program of multifactorial fall prevention on health-related quality of life, functional ability, fear of falling and psychological well-being. A randomized controlled trial. Aging Clin Exp Res. 2010;22(3):249–2546p. doi: 10.3275/6628. [DOI] [PubMed] [Google Scholar]
- 41.Markle-Reid M, Browne G, Gafni A, et al. The effects and costs of a multifactorial and interdisciplinary team approach to falls prevention for older home care clients “at risk” for falling: A randomized controlled trial. Can J Aging. 2010;29(1):139–161. doi: 10.1017/S0714980809990377. [DOI] [PubMed] [Google Scholar]
- 42.Corrie H, Brooke-Wavell K, Mansfield NJ, Cowley A, Morris R, Masud T. Effects of vertical and side-alternating vibration training on fall risk factors and bone turnover in older people at risk of falls. Age Ageing. 2015;44(1):115–122. doi: 10.1093/ageing/afu136. [DOI] [PubMed] [Google Scholar]
- 43.Gschwind YJ, Eichberg S, Ejupi A, et al. ICT-based system to predict and prevent falls (iStoppFalls): results from an international multicenter randomized controlled trial. Eur Rev Aging Phys Act. 2015;12:10. doi: 10.1186/s11556-015-0155-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Logghe IHJ, Zeeuwe PEM, Verhagen AP, et al. Lack of effect of tai chi chuan in preventing falls in elderly people living at home: A randomized clinical trial. J Am Geriatr Soc. 2009;57(1):70–75. doi: 10.1111/j.1532-5415.2008.02064.x. [DOI] [PubMed] [Google Scholar]
- 45.Talley KMC, Wyman JF, Gross CR, Lindquist Ra, Gaugler JE. Change in balance confidence and its associations with increasing disability in older community-dwelling women at risk for falling. J Aging Health. 2014;26(4):616–636. doi: 10.1177/0898264314526619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patil R, Karinkanta S, Tokola K, Kannus P, Sievänen H, Uusi-Rasi K. Effects of vitamin D and exercise on the wellbeing of older community-dwelling women: A randomized controlled trial. Gerontology. 2016;62(4):401–408. doi: 10.1159/000442441. [DOI] [PubMed] [Google Scholar]
- 47.Oh S, Lim J-M, Kim Y, Kim M, Song W, Yoon B. Comparison of the effects of water- and land-based exercises on the physical function and quality of life in community-dwelling elderly people with history of falling: a single-blind, randomized controlled trial. Arch Gerontol Geriatr. 2015;60(2):288–293. doi: 10.1016/j.archger.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 48.Sheffield C, Smith CA, Becker M. Evaluation of an agency-based occupational therapy intervention to facilitate aging in place. Gerontologist. 2013;53(6):907–918. doi: 10.1093/geront/gns145. [DOI] [PubMed] [Google Scholar]
- 49.Freiberger E, Blank WA, Salb J, et al. Effects of a complex intervention on fall risk in the general practitioner setting: A cluster randomized controlled trial. Clin Interv Aging. 2013;8:1079–1088. doi: 10.2147/CIA.S46218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yamada M, Mori S, Nishiguchi S, et al. Pedometer-based behavioral change program can improve dependency in sedentary older adults: A randomized controlled trial. J Frailty Aging. 2012;1(1):39–44. doi: 10.14283/jfa.2012.7. [DOI] [PubMed] [Google Scholar]
- 51.Pollock RD, Martin FC, Newham DJ. Whole-body vibration in addition to strength and balance exercise for falls-related functional mobility of frail older adults: a single-blind randomized controlled trial. Clin Rehabil. 2012;26(10):915–923. doi: 10.1177/0269215511435688. [DOI] [PubMed] [Google Scholar]
- 52.Schoene D, Valenzuela T, Toson B, et al. Interactive cognitive-motor step training improves cognitive risk factors of falling in older adults - A randomized controlled trial. PLoS One. 2015;10(12):1–18. doi: 10.1371/journal.pone.0145161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gitlin LN, Winter L, Dennis MP, Hauck WW. Variation in response to a home intervention to support daily function by age, race, sex, and education. Journals Gerontol Ser A Biol Sci Med Sci. 2008;63A(7):745–7506p. doi: 10.1093/gerona/63.7.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Scheffer AC, Scholte Op Reimer WJ, Van Dijk N, et al. Effect of a mobile safety alarm on going outside, feeling safe, fear of falling, and quality of life in community-living older persons: A randomized controlled trial. J Am Geriatr Soc. 2012;60(5):987–989. doi: 10.1111/j.1532-5415.2012.03932.x. [DOI] [PubMed] [Google Scholar]
- 55.Beyer N, Simonsen L, Bulow J, et al. Old women with a recent fall history show improved muscle strength and function sustained for six months after finishing training. Aging Clin Exp Res. 2007;19(4):300–309. doi: 10.1007/BF03324706. [DOI] [PubMed] [Google Scholar]
- 56.Wu G, Keyes L, Callas P, Ren X, Bookchin B. Comparison of telecommunication, community, and home-based tai chi exercise programs on compliance and effectiveness in elders at risk for falls. Arch Phys Med Rehabil. 2010;91(6):849–856. doi: 10.1016/j.apmr.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 57.Metzelthin SF, van Rossum E, de Witte LP, et al. Effectiveness of interdisciplinary primary care approach to reduce disability in community dwelling frail older people: cluster randomised controlled trial. BMJ. 2013;347(September):f5264. doi: 10.1136/bmj.f5264. doi: http://dx.doi.org/10.1136/bmj.f5264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kim H, Yoshida H, Suzuki T. The effects of multidimensional exercise on functional decline, urinary incontinence, and fear of falling in community-dwelling elderly women with multiple symptoms of geriatric syndrome: A randomized controlled and 6-month follow-up trial. Arch Gerontol Geriatr. 2011;52(1):99–105. doi: 10.1016/j.archger.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 59.Jung D, Lee J, Lee S. A meta-analysis of fear of falling treatment programs for the elderly. West J Nurs Res. 2009;31(1):6–16. doi: 10.1177/0193945908320466. [DOI] [PubMed] [Google Scholar]
- 60.Liu YWJ, Tsui CM. A randomized trial comparing Tai Chi with and without cognitive-behavioral intervention (CBI) to reduce fear of falling in community-dwelling elderly people. Arch Gerontol Geriatr. 2014;59(2):317–325. doi: 10.1016/j.archger.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 61.Tennstedt S, Howland J, Lachman M, Peterson E, Kasten L, Jette A. A randomized , controlled trial of a group intervention to reduce fear of falling and associated activity restriction in older adults. J Gerontol Psychol Sci. 1998;53(6):384–392. doi: 10.1093/geronb/53b.6.p384. [DOI] [PubMed] [Google Scholar]