Abstract
Objective
To report a rare uterine anomaly of a septate uterus, double cervix and double vagina in patient who conceived spontaneously and delivered vaginaly.
Design
Case report.
Setting
Department of Obstetrics and Gynecology, Zagreb University School of Medicine, Clinical Hospital “Sveti Duh”, Zagreb, Croatia.
Patient(s)
A 34-year-old nulligravida who underwent clinical, radiological, surgical and intrapartal workup.
Intervention(s)
Clinical examination and intrapartal surgical resection of vaginal septum followed by vaginal delivery.
Main Outcome Measure(s)
Description and treatment for a rare Müllerian anomaly and a subsequent literature search.
Result(s)
Successful intrapartal resection of longitudinal vaginal septum and double cervix followed by vaginal delivery without complication.
Conclusion(s)
Reconstructive surgical procedures may be considered for providing spontaneous pregnancies and intrapartal surgical technique could be taken into consideration in order to prevent unnecessary cesarean sections, upon strict estimation of the obstetrician.
Keywords: Müllerian anomalies, Complete septate uterus, Double cervix, Longitudinal vaginal septum, Intrapartal surgical treatment, Vaginal delivery
Highlights
-
•
We present a rare anomaly of a septate uterus, double cervix and double vagina.
-
•
Reconstructive procedures may be considered for providing spontaneous pregnancies.
-
•
Intrapartal resection of longitudinal vaginal septum and double cervix was done.
-
•
Intrapartal procedures could prevent unnecessary cesarean sections.
-
•
If vaginal delivery is indicated experienced obstetrical team should supervise it.
1. Introduction
The incidence of congenital uterine anomalies is estimated to be 0.001–10% in general population [1], however the true incidence is not know because only those anomalies that result in pregnancy loss or cause symptoms are usually described and reported [2].
Septate uterus with double cervix and longitudinal vaginal septum represents one of the Müllerian anomalies “without a classification” [3]. Surgical treatment in patients with this rare malformation includes resection of the vaginal septum with or without hysteroscopic resection of the uterine septum. If these women reach term pregnancy, elective cesarean section is a usual delivery option [3], [4], [5].
We discuss a rare case of Müllerian anomaly “without a classification”: modality of treatment, pregnancy outcome and final intrapartal surgical intervention that resulted in a successful vaginal delivery.
2. Case Report
A 34-year-old nulligravida presented to our clinic at 6th week of gestation and with history of laparoscopic-assisted hysteroscopic resection of uterine septum. She was diagnosed with septate uterus with cervical duplication and longitudinal vaginal septum, and was without any symptoms. Vaginal examination revealed longitudinal vaginal septum 2 cm long in the upper third of the vagina with two normal-appearing cervices. Transvaginal sonography has shown septate uterus. During endoscopic procedure uterus and both adnexa appeared normal. Uterine septum was resected, but vaginal not, for unknown reasons.
5 years after the procedure patient spontaneously conceived for the first time. Pregnancy was uneventful. She was admitted in the delivery room with 385/7 weeks due to contractions. At admission vaginal septum was about 1 cm thick and both cervices dilated 2 cm by bimanual palpation and documented by transvaginal sonography (Fig. 1). Epidural analgesia was indicated.
Fig. 1.
Status at admission: vaginal septum about 1 cm thick and both cervices dilated 2 cm, documented by transvaginal ultrasound.
3. Procedure
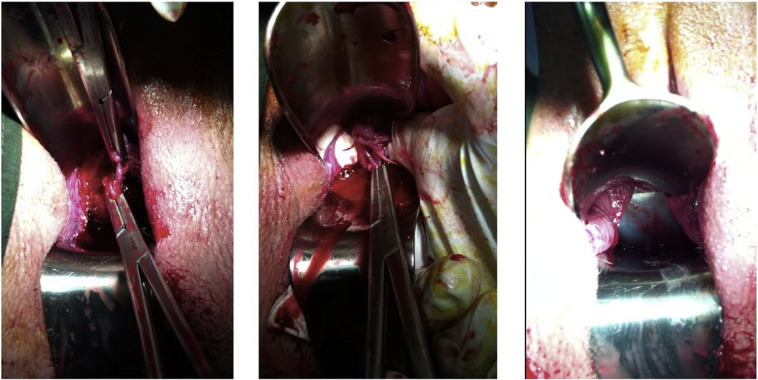
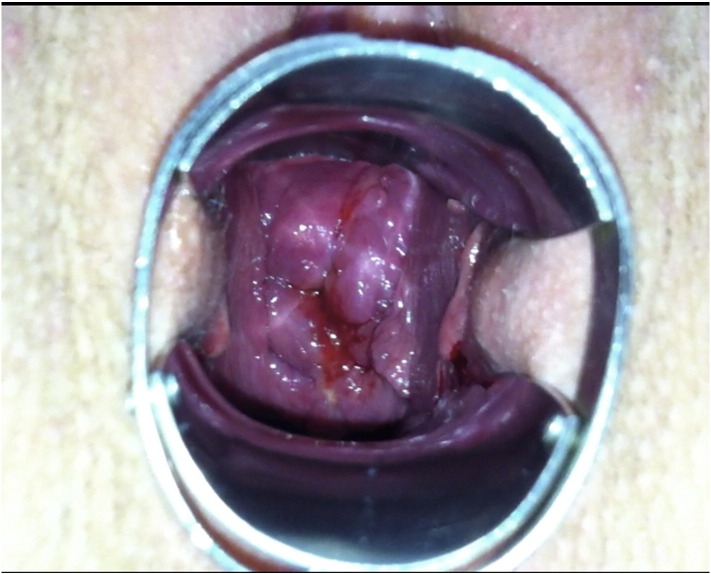
When both cervices were dilated 3–4 cm, we proceeded with resection of vaginal septum (Fig. 2) and double cervix (Fig. 2b). Septum was clamped, sutured with vicryl 1–0 and resected; resection of double cervix was preceded in a similar manner. Bleeding was within normal range. Intrapartal condition after described procedures and before subsequent amniotomy is shown in Fig. 2c. She gave birth to health male 3450/51, Apgar score 10/10, and was delivered without episiotomy, with perineal rupture grade 1. Due to uterus atony, compressive sutures (sec. Habitch) were placed. Transabdominal sonography was performed after delivery, revealed normal continuity of the uterus and absence of free fluid. Postpartal laboratory findings were within normal range. Routine gynecological examination 6 weeks after the delivery revealed single normal-appearing cervix (Fig. 3).
Fig. 2.
a: Image shows both cervices dilated 3–4 cm and resection of vaginal septum.
b: Resection of double cervix.
c: Image shows intrapartal condition after described procedures and before subsequent amniotomy.
Fig. 3.
6 weeks after the delivery examination revealed single normal-appearing cervix.
4. Discussion
This unusual Müllerian anomaly of complete uterine septum, double cervix and longitudinal vaginal septum does not fit in the commonly used classification system of anomalies suggested by Buttram and Gibbons [6], Acién and coworkers classified it as anomalies “without a classification” [3] and finally ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies properly classified this type of anomaly according to anatomical variations [7]. This rare type of anomaly is reported in several publications [8], [9], [10], the largest case series of 16 patients from Patton et al. [11]. For diagnostic purposes some authors have emphasized the utility of laparoscopic-assisted hysteroscopy, whereas others used MRI for definitive and noninvasive diagnosis. Transvaginal sonography is used as an initial diagnostic tool. Transvaginal 3D- sonography appears to be extremely accurate for the diagnosis and classification of congenital uterine anomalies, even more than MRI and office hysteroscopy [12]. With improvement of the technique it is becoming mandatory step in the assessment in the of the uterine anomalies especially septate or bicornuate uterus.
Cervical duplication is usually associated with few others Müllerian anomalies from which uterus didelphys is the most common, but other rare anomalies include a communicating septate uterus with a double cervix and a duplicated cervix and a longitudinal vaginal septum. When double cervices are visualized the majority of clinicians do not perform further diagnostic work-up because they correlate it with uterus didelphys. For this reason, the incidence of this specific anomaly could be even greater than previously anticipated.
Although the cause of most uterine anomalies remains unclear, they could potentially be due to a failure of fusion of the Müllerian ducts and/or the resorption of the septum. It is believed that this type of anomaly is “transitional”, providing evidence for the bidirectional theory of the septum resorption from the isthmus, a discrepancy that seems frequent in the processes of fusion and resorption between the convergent and divergent portions of the Müllerian ducts. Acién [6] states that fusion and resorption defects frequently affect just the superior uterine segment or both segments, within the transversal limit of junction between both of them at an isthmic level.
Due to a small number of cases; data about long-term outcomes are failing, and clinicians are still uncertain what type of treatment is necessary to maintain the best reproductive capacity. It is believed that treatment is necessary when patients are symptomatic with hematometra, dysmenorrhea, amenorrhea, infertility or recurrent pregnancy loss [1]. Reconstructive surgery is recommended when a complete uterine septum is diagnosed. Both transabdominal and hysteroscopic metroplasty are successful in improving reproductive performance in this group of patients, but hysteroscopy is considered to be a superior technique. According to Patton and coworkers [11], significant pregnancy loss, obstetric complications, and dyspareunia are common in women with this rare reproductive malformation. In 2004 he reported about 16 symptomatic patients with this particular anomaly who underwent reconstructive surgery: 11 hysteroscopic incisions of the uterine septum and 5 modified Tompkins metroplasty were performed. Of the 16 pregnancies that were conceived prior to surgical reconstruction, none resulted in term deliveries of live infants. 12 women conceived postoperatively for a total of 17 pregnancies, there were 14 term live births (their number and mode of delivery is not stated in the article) or ongoing pregnancies in the third trimester. Although most reproductive specialists agree that hysteroscopic treatment is indicated in patients with a uterine septum and a recurrent pregnancy loss, it is considered to be controversial for fertile asymptomatic and nulligravid women. Reconstructive surgery results in overall benefit in terms of first and second trimester losses, prematurity and neonatal complications. Therefore, Patton [11] recommends corrective surgery whenever a complete uterine septum is diagnosed. According to the literature, mode of the delivery was not discussed and elective cesarean section was performed in all reported cases. In this particular case, patient entered the delivery room with regular contractions and engaged fetal head. Obstetrical team estimated that there are good odds for vaginal delivery. After signing informed consent, we proceeded with described interventions that resulted in vaginaly delivery without complications.
According to current literature, this is the first patient who possesses this rare Müllerian anomaly and delivered vaginally a term infant, as a result of described hysteroscopic and intrapartal surgical interventions.
Note: This case report was presented in abstract form on the 18th World Congress on Controversies in Obstetrics, Gynecology & Infertility (COGI), Vienna, Austria, October 24–27, 2013.
Conflict of Interest
None to declare.
Acknowledgements
None.
References
- 1.Lin P.C., Kunwar P.B., Nettleton G.S., Nakajima S.T. Female genital anomalies affecting reproduction. Fertil Steril. 2002;78:899–915. doi: 10.1016/s0015-0282(02)03368-x. [DOI] [PubMed] [Google Scholar]
- 2.Ganesh A., Gupta N.J., Chakravarty B. Surgical correction of rare Müllerian anomalies and spontaneous pregnanicies: a case report. Fertil Steril. 2008;89(3):723. doi: 10.1016/j.fertnstert.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Acién P., Acién M., Sánchez-Ferrer M.L. Müllerian anomalies “without a classification”: from the didelphys-unicollis uterus to the bicervical uterus with or without septate vagina. Fertil Steril. Jun 2009;91(6):2369–2375. doi: 10.1016/j.fertnstert.2008.01.079. [DOI] [PubMed] [Google Scholar]
- 4.Duffy D.A., Nulsen J., Maier D., Schmidt D., Benadiva C. Septate uterus with cervical duplication: a full-term delivery after resection of a vaginal septum. Fertil Steril. 2004 Apr;81(4):1125–1126. doi: 10.1016/j.fertnstert.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 5.Pavone M.E., King J.A., Vlahos N. Septate uterus with cervical duplication and a longitudinal vaginal septum: a müllerian anomaly without a classification. Fertil Steril. Feb 2006;85(2):494. doi: 10.1016/j.fertnstert.2005.07.1324. e9-10. [DOI] [PubMed] [Google Scholar]
- 6.Buttram V.C., Jr., Gibbons W.E. Müllerian anomalies: a purposed classification (an analysis of 144 cases) Fertil Steril. 1979;32:40–46. doi: 10.1016/s0015-0282(16)44114-2. [DOI] [PubMed] [Google Scholar]
- 7.Grimbizis G.F., Gordts S., Di Spiezio S.A., Brucker S., De Angelis C., Gergolet M. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod. 2013;28(8):2032–2044. doi: 10.1093/humrep/det098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Balasch J., Moreno E., Martinez-Román S., Moliní J.L., Torné A., Sánchez-Martín F. Septate uterus with cervical duplication and longitudinal vaginal septum: a report of three new cases. EJOG. 1996;65:241–243. doi: 10.1016/0301-2115(95)02333-x. [DOI] [PubMed] [Google Scholar]
- 9.Hundley A.F., Fielding J.R., Hoyte L. Double cervix and vagina with septate uterus: an uncommon Müllerian malformation. Obstet Gynecol. 2001;98(5):982–985. doi: 10.1016/s0029-7844(01)01559-9. [DOI] [PubMed] [Google Scholar]
- 10.Chang A.S., Siegel C.L., Moley K.H., Ratts V.S., Odem R.R. Septate uterus with cervical duplication and longitudinal vaginal septum: a report of five new cases. Fertil Steril. 2004;81(4):1133–1136. doi: 10.1016/j.fertnstert.2003.08.051. [DOI] [PubMed] [Google Scholar]
- 11.Patton P.E., Novy M.J., Lee D.M., Hickok L.R. The diagnosis and reproductive outcome after surgical treatment of the complete septate uterus, duplicated cervix and vaginal septum. Am J Obstet Gynecol. 2004;190(6):1669–1678. doi: 10.1016/j.ajog.2004.02.046. [DOI] [PubMed] [Google Scholar]
- 12.Faivre E., Fernandez H., Deffieux X., Gervaise A., Frydman R., Levaillant J.M. Accuracy of three-dimensional ultrasonography in differential diagnosis of septate and bicornuate uterus compared with office hysteroscopy and pelvic magnetic resonance imaging. J Minim Invasive Gyenecol. 2012;19(1):101–106. doi: 10.1016/j.jmig.2011.08.724. [DOI] [PubMed] [Google Scholar]