Abstract
Background
Super-responders (SRs) are defined as patients who show crucial cardiac function improvement after cardiac resynchronization therapy (CRT). The purpose of this study is to identify and validate predictors of SRs after CRT.
Methods
This study enrolled 201 patients who underwent CRT during the period from 2010 to 2014. Clinical and echocardiographic evaluations were conducted before CRT and 6 months after. Patients with a decrease in New York Heart Association (NYHA) functional class ≥ 1, a decrease in left ventricular end-systolic volume (LVESV) ≥ 15%, and a final left ventricular ejection fraction (LVEF) ≥ 45% were classified as SRs.
Results
29% of the 201 patients who underwent CRT were identified as SRs. At baseline, SRs had significantly smaller left atrial diameter (LAD), LVESV, left ventricular end-diastolic volume (LVEDV) and higher LVEF than the non-super-responders (non-SRs). The percentage of patients using angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (ACEI/ARB) was higher in SRs than non-SRs. Most SRs had Biventricular (BiV) pacing percentage greater than 98% six months after CRT. In the multivariate logistic regression analysis, the independent predictors of SRs were lower LVEDV [odd ratios (OR): 0.93; confidence intervals (CI): 0.90–0.97], use of ACEI/ARB (OR: 0.33; CI: 0.13–0.82) and BiV pacing percentage greater than 98% (OR: 0.29; CI: 0.16–0.87).
Conclusion
Patients with a better compliance of ACEI/ARB and a less ectatic ventricular geometry before CRT tends to have a greater probability of becoming SRs. Higher percentage of BiV pacing is essential for becoming SRs.
Keywords: Biventricular pacing, Cardiac resynchronization therapy, Heart failure, Super-responders
1. Introduction
Cardiac resynchronization therapy (CRT) has been widely used as a regular treatment for heart failure (HF) patients with ventricular desynchrony. However, patients' reaction to CRT vary greatly. About 1/3 of the patients showed disappointing results, even though they fulfilled inclusion criteria according to the guidelines.[1],[2] About 20%–30% of the patients' cardiac anatomy and function could reach normal conditions after CRT, those patients are identified as super-responders(SRs) to CRT implantation.
Although several studies have presented various factors predicting super-response to CRT, there still exist unknown factors that could contribute to greater recovery of cardiac function. Therefore, we conducted the following study to search for potential predictors of super-response to CRT.
2. Methods
2.1. Patients
The study population consists of 201 patients who successfully received CRT from November 2010 to November 2014 in Fuwai hospital. Before receiving CRT implantation, they were all treated with optimal guideline-based medical therapy for at least three months and the effect were found to be limited. They all met the criteria for CRT: HF graded as New York Heart Association (NYHA) class II, III or IV despite optimal pharmacological therapy, left ventricular ejection fraction (LVEF) ≤ 0.35, and QRS duration ≥ 120 ms with left bundle branch block (LBBB) configuration or QRS duration ≥ 150 ms with non-LBBB configuration. The baseline data, preoperative and postoperative indicators, and follow-up data were collected from the enrolled patients. The authors had access to information that could identify individual participants during and after data collection. This study complied with the Declaration of Helsinki.
2.2. Device implantation
Technical aspects of device implantation were described in detail previously.[3] Briefly, the coronary sinus (CS) was cannulated from left subclavian and/or cephalic entry site using a commercially available long peelable guiding sheath. Left ventricular (LV) pacing lead was positioned in the venous system, preferably in the lateral or posterolateral vein. The right atrial (RA) and right ventricular (RV) leads were placed regularly at the RA appendage and the RV apex. Fluoroscopy was used to assess the final position of the LV pacing lead. A routine optimization of device parameters was performed before discharge.
2.3. Echocardiographic assessment
In echocardiography evaluation, parameters were measured according to the recommendations of the American Society of Echocardiography.[4] Left ventricular end-diastolic volume (LVEDV) and left ventricular end-systolic volume (LVESV) were acquired from apical two- and four-chamber views. LVEF was calculated by using the Simpson's methods. Left atrial diameters (LAD) were assessed mainly by using M mode methods. The degree of mitral regurgitation was categorized into five grades (grade 0–4); grades 3 and 4 were considered to be significant functional mitral regurgitation (FMR).
2.4. Follow-up and definition of super-response
After the implantation, atrioventricular (AV) and interventricular (VV) intervals received optimization under the guidance of echocardiography. Before CRT and 6 months after, clinical, demographic and echocardiographic parameters were systematically assessed. During the 6 months follow-up, patients were classified as SRs to CRT with a reduction of one or more NYHA functional classes, a decrease in the LVESV ≥ 15% and a LVEF absolute value ≥ 45%. Non-responders were defined with a decrease in the LVESV ≤ 15% or who had been re-hospitalized for the reason of heart failure or died during follow-up.
2.5. Statistical analysis
Continuous variables were reported as mean ± standard deviation and were compared using Student's t test. Categorical variables were reported as number and percentage of the total and were compared using the Fisher exact test or Chi-square test. Logistic regression analysis was employed to determine the potential predictors of super-response. The factors with P values < 0.1 in the univariate analysis were entered into a multivariate logistic regression model using a forward stepwise method to identify the independent predictors. A receiver operating characteristic (ROC) curve was used to assess the ability to predict CRT super-response. A P value < 0.05 was considered statistically significant. All statistical analyses were conducted with SPSS 20.0 (SPSS, Chicago, IL, USA).
3. Results
3.1. Study population
In the study population, 129 patients were male (64.2%) and 72 were female (35.8%). The mean age was 57.7 ± 11.2 years. thirty patients were in NYHA class IV (14.9%), 121 in class III (60.2%), and 50 in class II (24.9%). The cause of heart failure was ischemic in 22 (10.9%) patients and non-ischemic in 179 (89.1%) patients. The mean ECG QRS duration was 162.4 ± 18.4 ms, with 183 patients (91%) presenting LBBB morphology, 28 patients (13.9%) presenting chronic atrial fibrillation (AF). Most patients presented dilation of the LV (mean LVEDV of 263.7 ± 81.4 mL, and mean LVESV of 190.6 ± 71.6 Ml), associated with a mean LVEF of 28.8 ± 8.3%. (Table 1)
Table 1. Demographics, baseline clinical parameters and pharmacological treatment of the two groups of patients.
| SRs (59) | Non-SRs (142) | Total (201) | P value | |
| Demographic | ||||
| Male gender | 34 (57.6%) | 95 (66.9%) | 129 (64.2%) | 0.212 |
| Age, yrs | 58.8 ± 10.6 | 57.3 ± 11.4 | 57.7 ± 11.2 | 0.390 |
| Etiology | ||||
| NICM | 53 (89.8%) | 126 (88.7%) | 179 (89.1%) | 0.820 |
| ICM | 6 (10.2%) | 16 (11.3%) | 22 (10.9%) | |
| NYHA Class | ||||
| II | 17 (28.8%) | 33 (23.2%) | 50 (24.9%) | 0.206 |
| III | 38 (64.4%) | 83 (58.5%) | 121 (60.2%) | 0.170 |
| IV | 4 (6.8%) | 26 (18.3%) | 30 (14.9%) | 0.037 |
| UCG and ECG variables | ||||
| LVEF, % | 32.2 ± 8.5 | 27.4 ± 7.3 | 28.8 ± 8.3 | < 0.001 |
| LVESV, mL | 156.5 ± 49.7 | 205.0 ± 74.5 | 190.6 ± 71.6 | < 0.001 |
| LVEDV, mL | 228.4 ± 58.9 | 278.3 ± 85.1 | 263.7 ± 81.4 | < 0.001 |
| LAD, mm | 41.3 ± 7.1 | 44.8 ± 7.0 | 43.7 ± 7.2 | 0.002 |
| FMR | 1.3 ± 0.8 | 1.6 ± 0.8 | 1.5 ± 0.8 | 0.046 |
| QRS duration, ms | 164.5 ± 16.0 | 161.5 ± 19.3 | 162.4 ± 18.4 | 0.289 |
| LBBB | 56 (94.9%) | 127 (89.4%) | 183 (91.0%) | 0.215 |
| De novo | 55 (93.2%) | 138 (97.2%) | 193 (96.1%) | 0.191 |
| CRT-D | 32 (54.2%) | 80 (56.3%) | 112 (55.7%) | 0.636 |
| Co-morbidity | ||||
| Chronic AF | 9 (15.3%) | 19 (13.4%) | 28 (13.9%) | 0.727 |
| Hypertension | 19 (32.2%) | 35 (24.6%) | 54 (26.9%) | 0.456 |
| Diabetes mellitus | 9 (15.3%) | 31 (21.8%) | 40 (19.9%) | 0.285 |
| Medication | ||||
| Diuretics | 56 (94.9%) | 141 (99.3%) | 197 (98.0%) | 0.077 |
| ACEI/ARB | 52 (88.1%) | 98 (69.0%) | 150 (74.6%) | 0.005 |
| β-Blockers | 55 (93.2%) | 139 (97.9%) | 194 (96.5%) | 0.100 |
| Nitrates | 20 (33.9%) | 44 (31.0%) | 64 (31.8%) | 0.686 |
| Class III | 11 (18.6%) | 29 (20.4%) | 40 (19.9%) | 0.774 |
| Antiarrhythmics | ||||
| Spironolactone | 56 (94.9%) | 130 (91.5%) | 186 (92.5%) | 0.408 |
| Digoxin | 9 (15.9%) | 30 (21.2%) | 39 (19.4%) | 0.511 |
| Anticoagulants | 7 (11.9%) | 12 (8.5%) | 39 (9.5%) | 0.221 |
Data given as n (%) or mean ± SD. AF: atrial fibrillation; ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; CRT-D: cardiac resynchronization therapy-defibrillator; ECG: electrocardiographic; FMR: functional mitral regurgitation; ICM: ischemic cardiomyopathy; LAD: left atrial diameter; LBBB: left bundle branch block; LVEDV: left ventricular end-diastolic volume; LVEF: left ventricular ejection fraction; LVESV: left ventricular end-systolic volume; NICM: non-ischemic cardiomyopathy; NYHA class: New York Heart Association functional class; Non-SRs: non-super responders; SRs: super-responders; UCG: ultrasonic cardiogram.
3.2. Incidence of SRs
Among the 201 patients with HF, 59 (29%) patients were considered as SRs to CRT. A re-admission rate of zero was found in the SRs 6 months after CRT, and a re-admission rate of 9.9% was found in non-SRs. All patients were alive during the 6-month follow-up with the pharmacotherapy adjusted, basically the increase or decrease of the doses.
3.3. Differences of baseline characteristics between SRs and non-SRs
In terms of baseline characteristics, SRs had significantly smaller LAD, LVESV, LVDSV, FMR, and higher LVEF. The percentage of patients using angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (ACEI/ ARB) is higher in SRs than non-SRs. SRs also had less frequently NYHA class IV than non-SRs. There were no significant differences regarding other parameters between SRs and non-SRs. (Table 1)
3.4. Effects of cardiac resynchronization therapy: follow-up 6 month after CRT
After CRT, we observed a significant improvement of NYHA functional class, LVEF, and FMR in both groups. LVESV and LVEDV showed a significant decrease in both groups. Regarding the magnitude of response, LVEDV, LVESV and LVEF showed a significantly greater improvement in SRs than in non-SRs. The variation of NYHA functional class and FMR was not significantly different between the two groups. Moreover, most SRs had Biventricular (BiV) pacing percentage greater than 98% while the percentage is generally lower in non-SRs (98.3% vs. 84.5%, P = 0.005 ). (Table 2)
Table 2. Changes of clinical and echocardiographic parameters from baseline to six months follow-up.
| SRs (59) | Non-SRs (142) | Total (201) | P value | |
| NYHA Class | ||||
| Baseline | 2.8 ± 0.6 | 2.9 ± 0.7 | 2.9 ± 0.6 | |
| Follow-up | 2.2 ± 0.7 | 2.5 ± 0.7 | 2.4 ± 0.7 | |
| Change | 0.6 ± 0.8 | 0.4 ± 0.7 | 0.5 ± 0.7 | 0.095 |
| P Value | < 0.001 | < 0.001 | < 0.001 | |
| LVEF, % | ||||
| Baseline | 32.2 ± 8.5 | 27.4 ± 7.8 | 28.8 ± 8.3 | |
| Follow-up | 53.2 ± 5.4 | 32.4 ± 8.1 | 38.5 ± 12.1 | |
| Change | −21.0 ± 8.4 | −4.9 ± 7.3 | −9.7 ± 0.7 | < 0.001 |
| P Value | < 0.001 | < 0.001 | < 0.001 | |
| LVEDV, mL | ||||
| Baseline | 228.3 ± 58.9 | 278.3 ± 85.1 | 263.7 ± 81.4 | |
| Follow-up | 145.2 ± 46.7 | 250.5 ± 77.0 | 219.6 ± 84.4 | |
| Change | 83.2 ± 56.7 | 27.8 ± 59.5 | 44.0 ± 63.7 | < 0.001 |
| P Value | < 0.001 | < 0.001 | < 0.001 | |
| LVESV, mL | ||||
| Baseline | 156.5 ± 49.7 | 205.0 ± 74.5 | 190.8 ± 71.5 | |
| Follow-up | 68.7 ± 25.9 | 173.2 ± 68.3 | 142.5 ± 75.9 | |
| Change | 87.9 ± 46.5 | 31.8 ± 4.3 | 48.2 ± 56.3 | < 0.001 |
| P Value | < 0.001 | < 0.001 | < 0.001 | |
| FMR | ||||
| Baseline | 1.3 ± 0.9 | 1.6 ± 0.8 | 1.5 ± 0.8 | |
| Follow-up | 0.7 ± 0.7 | 1.1 ± 0.8 | 1.0 ± 0.8 | |
| Change | 0.6 ± 0.8 | 0.4 ± 0.7 | 0.5 ± 0.7 | 0.101 |
| P Value |
< 0.001 |
< 0.001 |
< 0.001 |
|
| Biv Pacing > 98% | 58 (98.3%) | 120 (84.5%) | 178 (88.6%) | 0.005 |
Data given as mean ± SD. Biv: Biventricular; FMR: functional mitral regurgitation; LVEDV: left ventricular end-diastolic volume; LVEF: left ventricular ejection fraction; LVESV: left ventricular end-systolic volume; NYHA class: New York Heart Association functional class; Non-SRs: non-super responders; SRs: super responders.
3.5. Predictors of super-response to cardiac resynchronization therapy
In the univariate analysis, variables correlated with super-response to CRT were smaller FMR, smaller LAD, smaller LVEDV, smaller LVESV, higher LVEF, less NYHA IV, use of ACEI/ARB and BiV pacing > 98%. In the multivariate logistic regression analysis, the independent predictor of SRs were lower LVEDV [odds ratios (OR): 0.93; confidence intervals (CI): 0.90–0.97], use of ACEI/ ARB (OR: 0.33; CI: 0.13–0.82) and BiV pacing > 98% (OR: 0.29; CI: 0.16–0.87). (Table 3)
Table 3. Univariate and multivariate logistic regression analysis of predictors for SRs.
| Parameters | Univariable |
Multivariable |
|||
| HR (95% CI)* | P-value | HR (95% CI)* | P-value | ||
| Male gender | 1.49 (0.80–2.77) | 0.213 | – | – | |
| Age | 0.99 (0.96–1.02) | 0.388 | – | – | |
| LVEF | 0.93 (0.90–0.97) | < 0.001 | 0.96 (0.93–1.22) | 0.397 | |
| LVEDV | 1.01 (1.00–1.01) | < 0.001 | 0.93 (0.90–0.97) | < 0.001 | |
| LVESV | 1.01 (1.01–1.02) | < 0.001 | 1.08 (0.94–1.09) | 0.243 | |
| LAD | 1.08 (1.03–1.13) | 0.002 | 0.93 (0.90–1.11) | 0.132 | |
| ACEI/ARB | 0.30 (0.13–0.71) | 0.006 | 0.33 (0.13–0.82) | 0.017 | |
| Digoxin | 2.16 (0.94–4.06) | 0.058 | 1.87 (0.93–3.75) | 0.079 | |
| Diuretics | 7.55 (0.77–74.16) | 0.083 | 1.88 (0.91–3.88) | 0.087 | |
| β-Blockers | 3.37 (1.18–3.27) | 0.119 | |||
| NYHA IV# | 3.08 (1.03–9.26)# | 0.045# | 0.95 (0.50–1.81)# | 0.867# | |
| Baseline FMR# | 1.46 (1.00–2.13)# | 0.048# | 1.30 (0.57–1.43)# | 0.661# | |
| BiV Pacing > 98% | 0.27 (0.16–0.82) | 0.004 | 0.29 (0.16–0.87) | 0.010 | |
*Hazard ratio (HR) and 95% CI. Only variables with P < 0.10 on univariable analyses were included in multivariable models. ACEI: angiotensin-converting enzyme inhibitor; ARB: angiotensin receptor blocker; Biv: Biventricular; CI: confidence intervals; FMR: functional mitral regurgitation; HR: hazard ratio; LAD: left atrial diameter; LVEDV: left ventricular end-diastolic volume; LVEF: left ventricular ejection fraction; LVESV: left ventricular end-systolic volume; NYHA class: New York Heart Association functional class; SRs: super responders.
We drew an ROC curve for pre-implant LVEDV to predict the CRT super-response [Area under curve (AUC) = 0.848; P < 0.0001]. A pre-implant LVEDV of 184 ml is the cut-off value to identify SRs, with 79.7% sensitivity and 59.9% specificity. (Figure 1)
Figure 1. ROC to show pre-implant LVEDV for predicting the CRT super-response (AUC = 0.848; P < 0.0001).
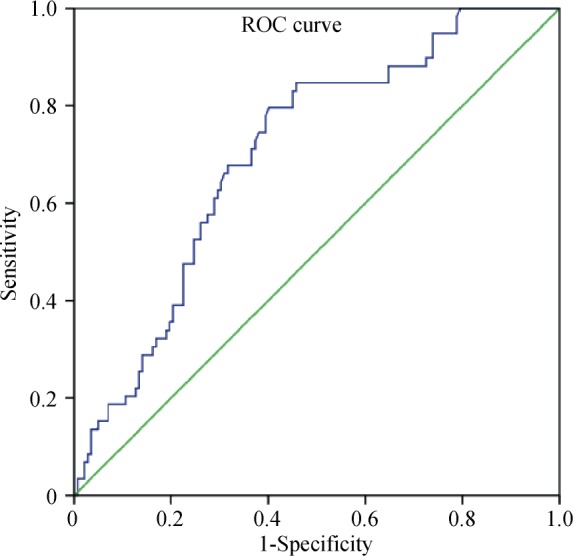
AUC: area under curve; CRT: cardiac resynchronization therapy; LVEDV: left ventricular end-diastolic volume; ROC: receiver operating characteristic.
4. Discussion
Despite the encouraging results from CRT in recent trials, HF patients response significantly different to CRT. Some patients did not improve at all or even did worse after CRT, while others had a super-response to CRT. In our population, 29% of the patients treated with CRT for HF were identified as SRs. This percentage was similar to previously reported results.[5],[6]
4.1. Definition of SRs
Previous studies have demonstrated that the long-term outcomes of SRs to CRT is significantly better than non-SRs.[6]–[9] However, the definitions of SRs vary in different studies. Castellant, et al.[5] proposed to consider patients as SRs if they fulfilled two criteria: functional recovery and LVEF ≥ 50%. Claudia, et al.[7] classified patients with a decrease in LVESV ≥ 30% at 6 months as SRs. In our study, we concurrently considered both of the NYHA class and echocardiographic parameters, similar to the standard proposed by Natalia, et al.[10] who described SRs as patients with a decrease in NYHA class ≥ 1, a two-fold or more increase of LVEF or a final LVEF ≥ 45%, and a decrease in LVESV ≥ 15%. We found the SRs in our cohort showed better reversed cardiac remodeling than non-SRs.
4.2. Predictors of SRs
Previous studies have reported several predictors of super-response to CRT, such as gender, non-ischemic etiology, duration of HF symptom, LBBB, smaller LAD with milder FMR, and upgrading from consistent RV pacing.[10]–[17]
In our study, patients with a lower LVEDV have a higher possibility of becoming SRs with a complete reverse remodeling than those with irreversible altered ventricular geometry. LVEDV ≤ 184 mL was an independent predictor of super-response to CRT. Despite the SRs have a significantly higher LVEF, a lower LAD, LVESV and FMR at baseline; these parameters were not independent predictors of super-response to CRT. According to the study of António, et al.[10] SRs had significantly smaller LVEDD before CRT. In addition, clinical studies concluded that patients with a smaller LV volume had a higher probability to benefit from CRT.[14],[18] Our previous study has also demonstrated that patients with smaller LVEDD would have a better chance to become SRs to CRT,[19] and that the size of LV is related to the extent of structural remodeling in HF patients. Gürtl, et al.[20] demonstrated that degeneration and loss of viable cardiocytes are related to the pathogenesis of HF. Therefore, for HF patients with dilated LV size, the loss of cardiocytes and myocardial fibrosis were thought to be more severe and extensive, which is an important contributing factor to a lower percentage of SRs in this group.
Previous studies showed that evidence-based HF medications, including ACEI or ARBs, were underused or underdosed in patients receiving CRT.[21],[22] Moreover, these studies also pointed out that patients who received no or low doses of ACEI/ARB have more comorbidity compared with patients treated with high doses.[22],[23] Likewise, we found that only 74.6% of the HF patients in our cohort used ACEI or ARB at baseline. The percentage of patients using ACEI/ARB was significantly higher in SRs than their counterparts. Our study emphasized the great significance of HF medications on the base of CRT implantation.
After studying our database of the 201 cases, we found that the use of ACEI/ARB is the strongest predictor, and this predictor has never been reported before. This conclusion has important implications for clinical strategies after CRT implantation. Treatment with CRT improves hemodynamics and clinical symptoms, and prevents bradycardia[24] which might allow further optimization of HF medication treatment. Thus, after CRT implantation, re-evaluation of HF medication is crucial. The increased blood pressure and the improved renal function might facilitate initiation or further optimize medical therapy in patients who previously could not tolerate this treatment.
The use of other HF medications, including beta blockers (BB), did not show predictive value for SRs, probably because our patients received higher mean percentages of BB at baseline.
4.3. Biventricular pacing percentage
The importance to maximize BiV pacing percentage has been emphasized since 2006, when Gasparini, et al.[25] used an arbitrary cut off rate of BiV pacing of 85% of the pacing time need to define CRT as effective in AF patients. After that, several consistent data has raised this standard to 90%,[26] 92%[27] and eventually 98%[28]. Our work assessed the probability of obtaining high BiV pacing and its link to changes in echo-cardiographic parameters, since the definition of SRs focused on the reduction of LVEF and LVEDV. Indeed, CRT requires BiV pacing percentage to be as close to 100% as possible to gain the maximal benefits.
There are a lot of barriers that inhibit gaining higher BiV pacing percentage: presence of atrial and ventricular ectopic beats; long atrioventricular delay programming; atrial tachycardia or AF; loss of LV pacing due to dislodgment or lack of capture of the LV lead. In our population, 23 patients were found with BiV pacing percentage < 98%. Among them, 13 (56.5%) had 10% or more ectopic beats including premature ventricular complexes (PVCs) or atrial premature complexes (APCs), which have been ensured by the 24 hours Holter at the follow up. Eight (34.8%) patients with persistent atrial fibrillation and refused to do atrioventricular junction (AVJ) ablation. One patient was determined loss of LV capture intermittently during the programming procedure.
BiV pacing > 98% as an independent predictor for SRs have never been reported before as we know. The maximum BiV pacing percentage should always be pursued and achieved for CRT patients. For this purpose, atrioventricular nodal-blocking therapy, AVJ ablation or atrioventricular delay reprogramming in sinus rhythm patients should be evaluated. In addition, the BiV percentage should be recalculated at every follow-up and, if possible, monitored with a home system.
4.4. Study limitations
Our study has some limitations. This is a single-centre, observational cohort study with limited sample size. Further studies with larger number of patients are suggested to verify the relevance of the discussed parameters. Furthermore, we conducted multivariate analysis incorporating possible predictors to reduce the influence of confounding factors; however, unknown confounding factors we didn't cover in this study should not be excluded.
5. Conclusions
Our work demonstrated that there is a considerable percentage of SRs after CRT in real practice. Additionally, these results suggest that patients with a less ectatic ventricular geometry, a better compliance to ACEI/ARB and a high percentage of BiV pacing have a greater probability of becoming SRs. This may have important therapeutic implications. If confirmed by large, long-term, multi-centre studies, these results may lead to CRT applied to these selected HF patients and higher probability of complete reverse remodeling.
In conclusion, patients with a better compliance of ACEI/ARB, a less ectatic ventricular geometry before CRT implantation and high percentage of biventricular pacing have a greater probability of becoming SRs.
References
- 1.Cleland JG, Daubert JC, Erdmann E, et al. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med. 2005;352:1539–1549. doi: 10.1056/NEJMoa050496. [DOI] [PubMed] [Google Scholar]
- 2.Abraham WT, Fisher WG, Smith AL, et al. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002;346:1845–1853. doi: 10.1056/NEJMoa013168. [DOI] [PubMed] [Google Scholar]
- 3.Cai C, Hua W, Ding LG, et al. Association of body mass index with cardiac reverse remodeling and long-term outcome in advanced heart failure patients with cardiac resynchronization therapy. Circ J. 2014;78:2899–2907. doi: 10.1253/circj.cj-14-0812. [DOI] [PubMed] [Google Scholar]
- 4.Schiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989;2:358–367. doi: 10.1016/s0894-7317(89)80014-8. [DOI] [PubMed] [Google Scholar]
- 5.Castellant P, Fatemi M, Bertault-Valls V, et al. Cardiac resynchronization therapy: "nonresponders" and "hyperresponders". Heart Rhythm. 2008;5:193–197. doi: 10.1016/j.hrthm.2007.09.023. [DOI] [PubMed] [Google Scholar]
- 6.Franke J, Keppler J, Abadei AK, et al. Long-term outcome of patients with and without super-response to CRT-D. Clin Rese Cardiol. 2016;105:341–348. doi: 10.1007/s00392-015-0926-0. [DOI] [PubMed] [Google Scholar]
- 7.Ypenburg C, van Bommel RJ, Borleffs CJ, et al. Long-term prognosis after cardiac resynchronization therapy is related to the extent of left ventricular reverse remodeling at midterm follow-up. J Am Coll Cardiol. 2009;53:483–490. doi: 10.1016/j.jacc.2008.10.032. [DOI] [PubMed] [Google Scholar]
- 8.Zecchin M, Proclemer A, Magnani S, et al. Long-term outcome of 'super-responder' patients to cardiac resynchronization therapy. Europace. 2014;16:363–371. doi: 10.1093/europace/eut339. [DOI] [PubMed] [Google Scholar]
- 9.Hurlimann D, Schmidt S, Seifert B, et al. Outcome of super-responders to cardiac resynchronization therapy defined by endpoint-derived parameters of left ventricular remodeling: a two-center retrospective study. Clin Res Cardiol. 2015;104:136–144. doi: 10.1007/s00392-014-0763-6. [DOI] [PubMed] [Google Scholar]
- 10.Antonio N, Teixeira R, Coelho L, et al. Identification of 'super-responders' to cardiac resynchronization therapy: the importance of symptom duration and left ventricular geometry. Europace. 2009;11:343–349. doi: 10.1093/europace/eup038. [DOI] [PubMed] [Google Scholar]
- 11.Hsu JC, Solomon SD, Bourgoun M, et al. Predictors of super-response to cardiac resynchronization therapy and associated improvement in clinical outcome: the MADIT-CRT (multicenter automatic defibrillator implantation trial with cardiac resynchronization therapy) study. J Am Coll Cardiol. 2012;59:2366–2373. doi: 10.1016/j.jacc.2012.01.065. [DOI] [PubMed] [Google Scholar]
- 12.Ellenbogen KA, Huizar JF. Foreseeing super-response to cardiac resynchronization therapy: a perspective for clinicians. J Am Coll Cardiol. 2012;59:2374–2377. doi: 10.1016/j.jacc.2011.11.074. [DOI] [PubMed] [Google Scholar]
- 13.van Bommel RJ, Bax JJ, Abraham WT, et al. Characteristics of heart failure patients associated with good and poor response to cardiac resynchronization therapy: a PROSPECT (Predictors of Response to CRT) sub-analysis. Eur Heart J. 2009;30:2470–2477. doi: 10.1093/eurheartj/ehp368. [DOI] [PubMed] [Google Scholar]
- 14.Rickard J, Kumbhani DJ, Popovic Z, et al. Characterization of super-response to cardiac resynchronization therapy. Heart Rhythm. 2010;7:885–889. doi: 10.1016/j.hrthm.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 15.Stefan L, Sedlacek K, Cerna D, et al. Small left atrium and mild mitral regurgitation predict super-response to cardiac resynchronization therapy. Europace. 2012;14:1608–1614. doi: 10.1093/europace/eus075. [DOI] [PubMed] [Google Scholar]
- 16.Manne M, Rickard J, Varma N, et al. Normalization of left ventricular ejection fraction after cardiac resynchronization therapy also normalizes survival. Pacing ClinElectrophysiol. 2013;36:970–977. doi: 10.1111/pace.12174. [DOI] [PubMed] [Google Scholar]
- 17.Yanagisawa S, Inden Y, Shimano M, et al. Clinical characteristics and predictors of super-response to cardiac resynchronization therapy: a combination of predictive factors. Pacing ClinElectrophysiol. 2014;37:1553–1564. doi: 10.1111/pace.12506. [DOI] [PubMed] [Google Scholar]
- 18.Vidal B, Delgado V, Mont L, et al. Decreased likelihood of response to cardiac resynchronization in patients with severe heart failure. Eur J Heart Fail. 2010;12:283–287. doi: 10.1093/eurjhf/hfq003. [DOI] [PubMed] [Google Scholar]
- 19.Qiao Q, Ding LG, Hua W, et al. Potential predictors of non-response and super-response to cardiac resynchronization therapy. Chin Med J. 2011;124:1338–1441. [PubMed] [Google Scholar]
- 20.Gurtl B, Kratky D, Guelly C, et al. Apoptosis and fibrosis are early features of heart failure in an animal model of metabolic cardiomyopathy. Int J Exp Pathol. 2009;90:338–346. doi: 10.1111/j.1365-2613.2009.00647.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heywood JT, Fonarow GC, Yancy CW, et al. Comparison of medical therapy dosing in outpatients cared for in cardiology practices with heart failure and reduced ejection fraction with and without device therapy: report from IMPROVE HF. Circ Heart Fail. 2010;3:596–605. doi: 10.1161/CIRCHEARTFAILURE.109.912683. [DOI] [PubMed] [Google Scholar]
- 22.Schmidt S, Hurlimann D, Starck CT, et al. Treatment with higher dosages of heart failure medication is associated with improved outcome following cardiac resynchronization therapy. Eur Heart J. 2014;35:1051–1060. doi: 10.1093/eurheartj/eht514. [DOI] [PubMed] [Google Scholar]
- 23.Mantziari L, Guha K, Khalique Z, et al. Relation of dosing of the renin-angiotensin system inhibitors after cardiac resynchronization therapy to long-term prognosis. Am J Cardiol. 2012;109:1619–1625. doi: 10.1016/j.amjcard.2012.01.387. [DOI] [PubMed] [Google Scholar]
- 24.Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. New Engl J Med. 2004;350:2140–2150. doi: 10.1056/NEJMoa032423. [DOI] [PubMed] [Google Scholar]
- 25.Gasparini M, Auricchio A, Metra M, et al. Long-term survival in patients undergoing cardiac resynchronization therapy: the importance of performing atrio-ventricular junction ablation in patients with permanent atrial fibrillation. Eur Heart J. 2008;29:1644–1652. doi: 10.1093/eurheartj/ehn133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koplan BA, Kaplan AJ, Weiner S, et al. Heart failure decompensation and all-cause mortality in relation to percent biventricular pacing in patients with heart failure: is a goal of 100% biventricular pacing necessary? J Am Coll Cardiol. 2009;53:355–360. doi: 10.1016/j.jacc.2008.09.043. [DOI] [PubMed] [Google Scholar]
- 27.Delnoy PP, Ottervanger JP, Luttikhuis HO, et al. Comparison of usefulness of cardiac resynchronization therapy in patients with atrial fibrillation and heart failure versus patients with sinus rhythm and heart failure. Am J Cardiol. 2007;99:1252–1257. doi: 10.1016/j.amjcard.2006.12.040. [DOI] [PubMed] [Google Scholar]
- 28.Hayes DL, Boehmer JP, Day JD, et al. Cardiac resynchronization therapy and the relationship of percent biventricular pacing to symptoms and survival. Heart Rhythm. 2011;8:1469–1475. doi: 10.1016/j.hrthm.2011.04.015. [DOI] [PubMed] [Google Scholar]


