Abstract
IMPORTANCE
Studies suggest that a postnatal parental intervention may reduce the incidence of abusive head trauma (AHT) of infants and young children.
OBJECTIVE
To assess the effect of statewide universal AHT education for parents on AHT hospitalization rates in Pennsylvania and on parents’ self-reported knowledge gains and parenting behaviors.
DESIGN, SETTING, AND PARTICIPANTS
Changes in AHT hospitalization rates in Pennsylvania before and during the intervention were compared with those in 5 other states lacking universal parental AHT education during the same period. Data were collected from maternity units and birthing centers throughout Pennsylvania from the parents of 1 593 834 infants born on these units from January 1, 2003, to December 31, 2013. Parental behavior and knowledge were assessed through immediate (n = 16 111) and 7-month postintervention (n = 146) parent surveys in a per protocol analysis of evaluable parents.
INTERVENTIONS
Parents read a brochure, viewed an 8-minute video about infant crying and AHT, asked questions of the nurse, and signed a commitment statement affirming their participation. Educational posters were displayed on each unit.
MAIN OUTCOMES AND MEASURES
Changes in AHT hospitalization rates before and during the intervention in Pennsylvania and 5 other states. Secondary outcomes included self-reported knowledge gains and changes in parenting practices.
RESULTS
A total of 1 180 291 parents (74.1%) of children ranging in age from 0 to 23 months signed a commitment statement. Incidence rate ratios for hospitalization for AHT increased in Pennsylvania from 24.1 (95% CI, 22.1-26.3) to 26.6 (95% CI, 24.9-28.4) per 100 000 children aged 0 to 23 months during the intervention period; changes in Pennsylvania were not significantly different from aggregate changes in the 5 other states, from 22.4 (95% CI, 21.2-23.6) to 22.0 (95% CI, 21.2-22.8) per 100 000 children aged 0 to 23 months. A total of 16 111 parents (21.5% men, 78.5% women) completed the postnatal survey. Despite an overall 74.1% adherence with the intervention, only 20.6% of parents saw the brochure and video and only 5.7% were exposed to the entire intervention. Among the respondents answering individual questions on the postnatal surveys, 10 958 mothers (91.0%) and 2950 fathers (88.6%) reported learning a lot about understanding infant crying as normal; 11 023 mothers (92.2%) and 2923 fathers (88.9%), calming their infant, 11 396 mothers (94.6%) and 3035 fathers (91.9%), calming themselves; 10 060 mothers (85.1%) and 2688 fathers (83.4%), selecting other infant caregivers; and 11 435 mothers (94.8%) and 3201 fathers (95.8%), that the information would decrease the likelihood of shaking an infant. Among the 143 respondents completing the 7-month survey, 109 (76.2%) reported remembering the information while their child was crying.
CONCLUSIONS AND RELEVANCE
This intervention was not associated with a reduction in pediatric AHT hospitalization rates but was associated with self-reported gains in parental knowledge that were retained for 7 months.
Abusive head trauma (AHT) accounts for most deaths due to physical abuse and most serious head injuries in infants.1 Several prevention efforts have been undertaken and resulted in improved parent knowledge,2–4 but few have examined the effect of such interventions on AHT incidence.5,6 In 1998, Dias and colleagues5 implemented a universal, postnatal parent education program in Upstate New York (Safe Babies New York [SBNY])7 to teach parents about normal infant crying, calming a crying infant, reducing caregiver frustration, and the dangers of violent infant shaking. The program was associated with a 47% reduction in AHT incidence during 6 years.5 An independent study of the program in another region of New York6 observed a 75% reduction. Likely because of these published results, at least 18 states, including Pennsylvania, have passed legislation mandating postnatal education about AHT for all parents. Based on the success of these pilot programs, we enacted a similar statewide intervention in Pennsylvania with the hypothesis that this program would significantly reduce AHT hospitalization rates.
Methods
Intervention
Following a state legislative mandate enacted in 2002, the Pennsylvania Shaken Baby Syndrome Prevention Program8 began in 2003 in 31 central Pennsylvania counties and expanded in 2004 to include the remaining 22 western and 14 eastern counties. To the 4 objectives of the SBNY program, we added a fifth (wisely selecting caregivers). The study was approved by Penn State College of Medicine’s institutional review board, which provided a waiver of consent.
Our program included the following key principles: (1) educate parents of all infants; (2) educate especially fathers and father figures; (3) provide information at a consistent time; (4) have nurses deliver the intervention; (5) incorporate multimedia and native languages; (6) administer before infants leave the hospital; (7) have parents sign a commitment statement affirming participation; and (8) require little time from nurses or parents.
Parents of infants born at all maternity units and birthing centers, but not born at home, from January 1, 2003, to December 31, 2013, were asked to read a brochure,9 view an 8-minute video Portrait of Promise (Midwest Children’s Resource Center), ask questions of the nurse, and sign the commitment statement. Posters (“Never, Never, Never, Never Shake a Baby”; SBS Prevention Plus) were also displayed on the unit. Mothers and, whenever present, fathers and father figures were asked to participate. English- and Spanish-language brochures and videos were provided; other brochure languages were available from the Pennsylvania Department of Health (http://www.doh.pa.gov/shakenbaby). Nurses were asked to provide AHT information separately from other safety information. Both parents individually signed the commitment statement; parents’ signature lines were obscured to preserve anonymity. Hospital adherence was measured by the percentage of signed commitment statement forms.
From January 1, 2008, to December 31, 2011, we introduced an additional intervention for parents, delivered through pediatric primary care professionals’ offices in 16 randomly selected central Pennsylvania counties. This intervention, to be provided at the 2-, 4-, and 6-month office visits, was intended as a supplement to the postnatal information. Parents were asked to read a “crying card” focused on how to respond to infant crying and the dangers of violent infant shaking and sign a response card, similar to the commitment statement, confirming their participation. Only 30% of pediatric care professionals’ offices in the selected counties participated, and we received signed response forms from parents of only 20.5% of infants born in these counties. Moreover, no significant changes in state registry reports of AHT were found among these counties during the intervention compared with counties that lacked this booster program. We therefore combined the hospitalization rates for all counties in our analyses.
Nurse Training
Hospital nurses were trained by 3 research nurse coordinators (C.M.R., K.M.C., and M.E.R.) who provided multiple 1-hour in-service programs (approved for continuing education credit) for each unit to review the purpose of the intervention, the legislative mandate, the consequences of AHT, the importance of consistently delivering the intervention and collecting the signed commitment statement, and confronting barriers to implementation. Nurses reviewed the brochure and video that parents would see. The nurse coordinators maintained frequent contact with nurse managers, with a mean of 26 telephone, email, and face-to-face communications with each manager per year, and disseminated quarterly newsletters.
Tracking AHT Hospitalization Rates
A statewide discharge data set from the Pennsylvania Healthcare Cost Containment Council (PHC4)10 was queried to identify nonfatal probable AHT cases using Center for Disease Control and Prevention–defined combinations of diagnosis and cause-of-injury codes from the International Classification of Diseases, Ninth Revision.11 Hospitalization rates per 100 000 same-aged population were calculated using probable case definitions and broad hospitalization rates previously published by the Centers for Disease Control and Prevention.11 This method has been used to calculate a range of AHT hospitalization rates12–14; probable case definitions and broad rates are best suited to assess the effect of prevention efforts.11 Case ascertainment based on these definitions may have a sensitivity and specificity as high as 92% and 96%, respectively.15 For comparison purposes, AHT hospitalization rates were similarly calculated from Healthcare Cost and Utilization Project (HCUP) state inpatient data sets for 5 states (Arizona, Colorado, Florida, Oregon, and South Carolina) that had complete data for the period of interest and lacked universal AHT prevention efforts; we compared PHC4 hospitalization rates with the mean hospitalization rates from the other 5 states.
Hospitalization rates from Pennsylvania and the 5 other states were compared during 1996 to 2002 (period 1), immediately preceding the intervention16; 2003 to 2006 (period 2), when statewide compliance with the intervention rose steadily toward 90%; and 2007 to 2013 (period 3), when statewide compliance rates were consistently 90% or greater. For each data set, preintervention rates (period 1) were compared with rates during the entire intervention period (periods 2 + 3) and during the period after full implementation (period 3) using Poisson regression models with incidence rate ratios (IRRs) and 95% CIs. Changes in the Pennsylvania hospitalization rates during the intervention were then compared with the changes in the other 5 states during these same periods using a ratio of the 2 IRRs. Because no individual-level descriptors were available in either of these data sets, no analysis of covariates was possible. All statistical analyses were performed using SAS software (version 9.4; SAS Institute Inc) with a significance level of P < .05.
Parent Surveys
Two sets of surveys were distributed to parents from 2008 to 2011. During 1 month of every year, each hospital distributed a written postnatal survey to all parents immediately after the intervention asking what program elements they received and which element was most effective. Using a 4-point Likert scale (3, strongly agree; 2, agree; 1, disagree; and 0, strongly disagree), parents were asked whether they learned “a lot” about understanding infant crying as normal, calming a crying infant, calming themselves, and selecting other caregivers and whether the intervention would reduce the likelihood that a parent would shake an infant. Respondents provided 5 demographic characteristics—parents’ sex, age, highest educational attainment, marital status, and race/ethnicity—statistically associated with AHT in Pennsylvania16 and contact information for a follow-up survey. Three hundred families randomly selected from among postnatal survey respondents were mailed follow-up surveys at 7 postnatal months. The follow-up survey tested parents’ memory of the program and how it had influenced their decision making. The results of these surveys are presented descriptively.
Results
From January 1, 2003, to December 31, 2013, 1 180 291 signed commitment statements were returned, representing 74.1% of 1 593 834 births during this period; 98.6% of commitment statements were signed by mothers and 69.8% by fathers. After December 31, 2006, signed commitment statements were consistently returned, representing 90% or more of live births in Pennsylvania.
AHT Hospitalization Rates
Calculated AHT hospitalization rates for the PHC4 and HCUP data sets (Figure) remained static or rose during the intervention (periods 2 + 3 and period 3 alone) for all age ranges compared with the preintervention period (period 1) in Pennsylvania (Table 1). We found no significant differences in the preintervention vs postintervention changes in Pennsylvania compared with the 5 other states for infants and children aged 0 to 11 or 0 to 23 months, although a significant increase in AHT hospitalization rates in Pennsylvania among children aged 12 to 23 months favored the comparison states (ratio of IRRs for periods 1 vs 3, 0.6; 95% CI, 0.4–0.9; ratio of IRRs for periods 1 vs 2 + 3, 0.7; 95% CI, 0.5–1.0) (Table 1).
Figure. Annual Rates of Hospitalization for Abusive Head Trauma.
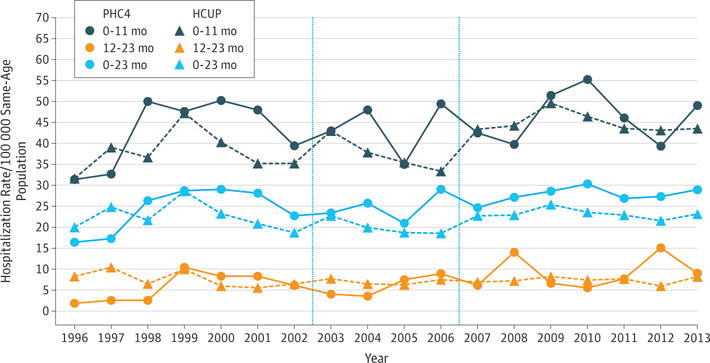
Rates are calculated among infants and children aged 0 to 11, 12 to 23, and 0 to 23 months in the Pennsylvania Healthcare Cost Containment Council (PHC4) data set and 5 other states (Healthcare Cost and Utilization Project [HCUP] data set) before (1996–2002), during (2003–2006), and after (2007–2013) fully implementing the educational intervention. Vertical lines separate the 3 periods.
Table 1.
Hospitalization Rates for AHT per 100 000 Same-Aged Population
| Data Set by Age Range | IRR (95% CI) | |||||
|---|---|---|---|---|---|---|
| PHC4 Data Set | PHC4 vs HCUP Data Setsa | |||||
| Period 1 (1996–2002) | Period 2 (2003–2006) | Period 3 (2007–2013) | Period 2 + 3 (2003–2013) | Period 1 vs 3 | Period 1 vs (2 + 3) | |
| 0–11 mo | ||||||
| PHC4 | 42.7 (38.9–46.9) | 43.7 (38.6–49.4) | 46.1 (42.1–50.4) | 45.2 (42.0–48.6) | 1.1 (0.9–1.3) | 1.0 (0.9–1.2) |
| HCUP | 37.9 (35.7–40.1) | 37.2 (34.6–40.0) | 44.8 (42.6–47.1) | 42.0 (40.4–43.8) | ||
| 12–23 mo | ||||||
| PHC4 | 5.7 (4.4–7.4) | 6.0 (4.3–8.3) | 9.2 (7.5–11.3) | 8.0 (6.8–9.6) | 0.6 (0.4–0.9) | 0.7 (0.5–1.0) |
| HCUP | 7.4 (6.5–8.4) | 7.0 (6.1–8.1) | 7.4 (6.7–8.2) | 7.3 (6.7–7.9) | ||
| 0–23 mo | ||||||
| PHC4 | 24.1 (22.1–26.3) | 24.7 (22.1–27.8) | 27.7 (25.5–30.0) | 26.6 (24.9–28.4) | 0.9 (0.8–1.0) | 0.9 (0.8–1.0) |
| HCUP | 22.4 (21.2–23.6) | 19.9 (18.7–21.3) | 23.1 (22.1–24.2) | 22.0 (21.2–22.8) | ||
Abbreviations: AHT, abusive head trauma; HCUP, Healthcare Cost and Utilization Project; IRR, incidence rate ratio; PHC4, Pennsylvania Healthcare Cost Containment Council.
Represented as a ratio of both IRRs.
Postnatal Survey Results
A total of 16 111 postnatal surveys were returned. Although fathers signed 69.8% of the commitment statements, they represented only 3467 (21.5%) survey respondents. Respondents were exposed most frequently to only 1 or 2 program elements; only 584 mothers (4.6%) and 232 fathers (6.7%) had been exposed to all 5 elements (Table 2). Although 11 457 mothers (90.6%) and 3160 fathers (91.1%) had read the brochure or watched the video, only 2605 mothers (20.6%) and 708 fathers (20.4%) had done both. Respondents exposed to all program elements cited the video as most important. Respondents ranging from 74.7% to 94.6% reported learning a lot about the educational domains, although the normalcy of infant crying and how to calm themselves and their infant were more frequently cited than wisely choosing other caregivers (eTable 1 in the Supplement). Eighty-seven percent of respondents thought the information would decrease the likelihood that parents would shake an infant.
Table 2.
Exposure to Program Elements Among Postnatal Parent Survey Respondents
| Parts of Program Received | Respondents, No. (%) | |
|---|---|---|
| Mothers (n = 12 644) |
Fathers (n = 3467) |
|
| Read a pamphlet or brochure | 7525 (59.5) | 2011 (58.0) |
| Watched a video | 6537 (51.7) | 1857 (53.6) |
| Talked with a nurse | 4487 (35.5) | 1299 (37.5) |
| Saw posters on the maternity unit | 1694 (13.4) | 666 (19.2) |
| Signed a paper or form | 5593 (44.2) | 1490 (43.0) |
| Read brochure or watched video | 11457 (90.6) | 3160 (91.1) |
| Read brochure and watched video | 2605 (20.6) | 708 (20.4) |
| Read brochure, watched video, and signed paper or form | 1838 (14.5) | 534 (15.4) |
| No. of program elements received | ||
| 0 | 202 (1.6) | 33 (1.0) |
| 1 | 5343 (42.3) | 1522 (43.9) |
| 2 | 3164 (25.0) | 757 (21.8) |
| 3 | 2159 (17.1) | 565 (16.3) |
| 4 | 1192 (9.4) | 358 (10.3) |
| 5 | 584 (4.6) | 232 (6.7) |
7-Month Survey Results
The 7-month surveys were returned by 146 of 300 parents (48.7% response rate); 3 surveys were excluded because the respondent did not indicate parent type. Among surveys having complete demographic information, 7-month survey respondents were demographically similar to the postnatal survey respondents for age, educational attainment, and marital status but were more frequently white (125 of 137 [91.2%] vs 11 774 of 14 793 [79.6%]; P = .001). All 93 mothers and 43 of 44 fathers (97.7%) who responded to the question recalled the postnatal intervention. Among those answering each individual survey question, respondents most frequently remembered signing the commitment statement (94 of 96 mothers [97.9%] and 41 of 42 fathers [97.6%]) and reading the brochure (91 of 97 mothers [93.8%] and 41 of 42 fathers [97.6%]); they least frequently remembered the video (71 of 96 mothers [74.0%] and 26 of 42 fathers [61.9%]) (eTable 2 in the Supplement). Most 7-month respondents reported learning a lot about the educational domains as noted in eTable 2 in the Supplement. Most (90 of 98 mothers [91.8%] and 40 of 42 fathers [92.2%]) thought the information would decrease the likelihood that parents would shake an infant. Seventy-four of 99 mothers (74.7%) and 35 of 44 fathers (79.5%) reported recalling the information while their infant was crying. The information was shared with others by 46 of 98 mothers (46.9%) and 15 of 43 fathers (34.9%), including parents’ relatives (26 of 99 mothers [26.3%] and 11 of 44 fathers [25.0%]), friends (16 of 99 mothers [16.2%] and 2 of 44 fathers [4.5%]), and the infants’ babysitters (5 of 98 mothers [5.1%] and 4 of 44 fathers [9.1%]). One hundred nine of 143 respondents (76.2%) thought the information helped them to select other caregivers, and 38 of 143 (26.6%) changed their selection of caregivers based on this information.
Discussion
This study is, to our knowledge, the largest study of universal hospital-based parent education about AHT to date. Despite widespread dissemination of the intervention as a whole and the admission by most parents that the intervention provided significant educational value, this statewide AHT prevention program failed to reduce rates of hospitalization for AHT in Pennsylvania. Another study of hospital-based parental education in North Carolina that used different materials (Period of PURPLE Crying program; National Center on Shaken Baby Syndrome)17 also failed to significantly reduce AHT rates.
The combined results of these 2 large studies contradict the conclusions of earlier, smaller studies in Upstate5 and Downstate New York6 that had suggested a positive effect of postnatal parental education on AHT rates. A case-control study of a similar intervention in Utah by Keenan and Leventhal18 had warned that the effect might not be intervention specific because reductions of AHT incidence also correlated with exposure to alternative parenting messages such as car seat use, sleep positioning, and bathwater temperature. Nonetheless, the results of preliminary studies sparked widespread local and statewide efforts to reduce AHT through universal parent education. Several programs, such as the “Don’t Shake the Baby,”19 “Love Me…Never Shake Me,”20 the Period of PURPLE Crying,2–4 and the SBNY model,5,6 were shown to increase parents’ knowledge of and attitudes toward infant crying and infant soothing, reduce their frustration and anger, and improve their understanding about the consequences of violent infant shaking. Most participants recommended such interventions to all parents of newborn infants.5,6,20 The present study confirms and extends these observations that the information is valuable for parents, over three-quarters of whom thought about it while their infant was crying during the ensuing months and many of whom used it to select other caregivers. Although a sizeable minority of parents shared the information with others, reaching caregivers (particularly new father figures) that enter later into the infant’s life remains a challenge.
The reductions in AHT incidence in prior studies may be a statistical aberration, although the duration (6 years) during which the effect in the SBNY program was demonstrated and its stability over this time, the replication of the results in another region at a different time, and the low incidence rates during the intervention in these regions compared with other published incidence rates12–14,21–23 makes these findings more compelling. One must therefore carefully examine the reason(s) we were unable to demonstrate a similar effect of this intervention in Pennsylvania. We considered 6 potential explanations for this discrepancy. The most obvious explanation is that the intervention, however well intentioned, is simply not effective, and the conclusions drawn from smaller initial studies were premature. The results of this and the North Carolina study17 suggest that, although providing parents with a single educational experience may improve their knowledge, it unfortunately does not change their behavior. However, we considered 5 other potential explanations for our negative results. First, greater recognition of AHT may have occurred during the Pennsylvania intervention, although no evidence supports this hypothesis. In fact, the PHC4 hospitalization rate was higher than the HCUP rate, particularly among the group aged 0 to 11 months, and, for the groups aged 0 to 11 and 0 to 23 months, did not rise to a significantly greater degree than the HCUP rates during the intervention period (Table 2).
Second is the difficulty of maintaining program fidelity on a much larger scale. The postnatal survey results suggest a significant problem delivering the entire program. Nearly half of the parents had not seen the video that they consider the most important element of the intervention in this and other studies,5,24 and only 20.5% had seen the brochure and video. This finding is striking in that the maternity units knew they were being evaluated during survey months, and the surveys were completed immediately after the intervention (reducing recall bias). Anecdotally, several parents who knew about the program told us they had not received it; one parent who asked was told “we no longer offer that here.” Hospital adherence often declined in association with changes in nursing leadership or staffing. Some lost, and temporarily stopped showing, their video. Finally, 1 hospital had parents sign the commitment statement on admission before the program was delivered. In sum, the full extent of implementation challenges and how they affected the outcomes are unclear.
Third, the intervention may not have adequately reached families at higher risk for AHT based on demographics.16 However, we found no clinically significant differences in program delivery based on parent demographics. Perhaps combining postnatal education with additional interventions, such as home visitation,25,26 might be more effective for high-risk families.
Fourth, several studies27–30 have documented a substantial rise in AHT rates (≤65%) during the US great recession from December 2007 through June 2009 and from which the country has subsequently struggled to emerge. These rates have not dropped substantially in subsequent years.30 Rates of hospitalization for AHT in the PHC4 and HCUP data sets rose significantly across all 3 age ranges after 2006. Such a rise may have masked reductions brought about by the intervention, although the rise in Pennsylvania was similar to that in the 5 other states for infants and children aged 0 to 11 and 0 to 23 months (it is unlikely that the rise in the group aged 12-23 months would be due to the intervention, absent similar differences in the other age groups).
Fifth, the intervention may work better for parents in Upstate New York than those in Pennsylvania. To investigate this possibility, we compared the demographics in both regions from the 2010 US Census and found no important differences in median household income, employment rates, and the proportions of high school graduates, population living below the poverty line, and population moving out of state. Other demographic differences may not have been identified.
Limitations
The study would have been strengthened by comparing 2 contemporaneous groups (with and without the intervention) in Pennsylvania. However, the state mandate requiring AHT education for parents of all newborn infants made this attempt impossible. Second, unrecognized confounders in Pennsylvania or the other states might have affected the results. Third, the study excluded fatal cases of AHT that never made it to a hospital and therefore underestimates the true incidence. However, assuming this number is small and similar between Pennsylvania and the other states, this exclusion does not affect the analyses. Fourth, a potential selection bias existed among the postnatal and 7-month survey respondents. Finally, 7-month survey respondents are subject to recall bias.
Conclusions
Our results demonstrate that a postnatal, hospital-based parent intervention is well received by parents of newborn infants and provides information that enhances their understanding of infant crying and violent infant shaking. Unfortunately, neither our intervention nor a similar postnatal intervention in North Carolina17 reduced rates of hospitalizations for AHT. Although these results are certainly disappointing, they should not dissuade us from continuing our efforts to reduce AHT. Perhaps supplementing this information repeatedly to parents over time (eg, with serial text messages); combining such information with family and community supports, such as home visitation for high-risk families25,26,31; and/or providing policies, such as paid family leave,32 that better support families during this critical period would reduce AHT.
Supplementary Material
Key Points.
Question
Does universal parental education about infant crying and the dangers of violent infant shaking during the immediate postnatal period reduce hospitalization rates for abusive head trauma?
Findings
In this prospective comparative study, a statewide abusive head trauma intervention was not associated with a significant reduction in the overall hospitalization rates for abusive head trauma among infants aged 0 to 23 months compared with 5 other states lacking such a statewide intervention, although parents did report significant knowledge gains from the intervention.
Meaning
Other or additional types of interventions may be needed to reduce hospitalization rates for abusive head trauma of infants and young children.
Acknowledgments
Funding/Support: This study was supported by grant 5U49CE001274-04 from the CDC.
Role of the Funder/Sponsor: The CDC had a specific role in the design of the study; interpretation of the data; preparation, review, and approval of the final manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Dias had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Dias, Rottmund, Cappos, Reed, Shaffer, Hollenbeak, Paul, Klevens.
Acquisition, analysis, or interpretation of data: Dias, Rottmund, Cappos, Reed, Wang, Stetter, Shaffer, Hollenbeak, Paul, Christian, Berger.
Drafting of the manuscript: Dias.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Wang, Stetter, Shaffer, Hollenbeak.
Obtained funding: Dias, Paul, Berger, Klevens.
Administrative, technical, or material support: Dias, Rottmund, Cappos, Reed, Paul, Christian, Berger.
Study supervision: Dias, Rottmund, Cappos, Reed.
Conflict of Interest Disclosures: Dr Dias and Mss Rottmund, Cappos, and Reed report receiving salary support from grants from the CDC and the Pennsylvania Department of Health. Drs Dias and Christian report receiving compensation for expert witness testimony in cases of abusive head trauma. No other disclosures were reported.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Additional Contributions: Adam Zolotor, MD, and Meghan Shanahan, PhD, University of North Carolina Injury Prevention Center, assisted in obtaining other state data sets. Likang Xu, PhD, and Sharyn Parks, PhD, CDC, provided the Healthcare Cost and Utilization Project data and the CDC-derived search strategy for identifying cases from the data sets. None of these individuals received compensation specific to these tasks.
Contributor Information
Mark S. Dias, Department of Neurosurgery, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania; Department of Pediatrics, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania.
Carroll M. Rottmund, Department of Neurosurgery, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania.
Kelly M. Cappos, Department of Neurosurgery, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania.
Marie E. Reed, Department of Neurosurgery, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania.
Ming Wang, Department of Public Health Sciences, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania.
Christina Stetter, Department of Public Health Sciences, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania.
Michele L. Shaffer, Department of Public Health Sciences, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania; Department of Pediatrics, University of Washington, Seattle; Children’s Core for Biomedical Statistics, Seattle Children’s Research Institute, Seattle, Washington.
Christopher S. Hollenbeak, Department of Pediatrics, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania; Department of Public Health Sciences, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania.
Ian M. Paul, Department of Pediatrics, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania; Department of Public Health Sciences, Penn State University College of Medicine, Penn State Children’s Hospital, Hershey, Pennsylvania.
Cindy W. Christian, Department of Pediatrics, University of Pennsylvania School of Medicine, Children’s Hospital of Philadelphia, Philadelphia.
Rachel P. Berger, Department of Pediatrics, University of Pittsburgh School of Medicine, Children’s Hospital of Pittsburgh of the University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania.
Joanne Klevens, Division of Violence Prevention, Centers for Disease Control and Prevention (CDC), Atlanta, Georgia.
References
- 1.Billmire ME, Myers PA. Serious head injury in infants: accident or abuse? Pediatrics. 1985;75(2):340–342. [PubMed] [Google Scholar]
- 2.Barr RG, Barr M, Fujiwara T, Conway J, Catherine N, Brant R. Do educational materials change knowledge and behaviour about crying and shaken baby syndrome? a randomized controlled trial. CMAJ. 2009;180(7):727–733. doi: 10.1503/cmaj.081419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barr RG, Rivara FP, Barr M, et al. Effectiveness of educational materials designed to change knowledge and behaviors regarding crying and shaken-baby syndrome in mothers of newborns: a randomized, controlled trial. Pediatrics. 2009;123(3):972–980. doi: 10.1542/peds.2008-0908. [DOI] [PubMed] [Google Scholar]
- 4.Fujiwara T, Yamada F, Okuyama M, Kamimaki I, Shikoro N, Barr RG. Effectiveness of educational materials designed to change knowledge and behavior about crying and shaken baby syndrome: a replication of a randomized controlled trial in Japan. Child Abuse Negl. 2012;36(9):613–620. doi: 10.1016/j.chiabu.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Dias MS, Smith K, DeGuehery K, Mazur P, Li V, Shaffer ML. Preventing abusive head trauma among infants and young children: a hospital-based, parent education program. Pediatrics. 2005;115(4):e470–e477. doi: 10.1542/peds.2004-1896. [DOI] [PubMed] [Google Scholar]
- 6.Altman RL, Canter J, Patrick PA, Daley N, Butt NK, Brand DA. Parent education by maternity nurses and prevention of abusive head trauma. Pediatrics. 2011;128(5):e1164–e1172. doi: 10.1542/peds.2010-3260. [DOI] [PubMed] [Google Scholar]
- 7.Safe Babies New York. Kaleida Health, Women & Children’s Hospital of Buffalo website. http://www.kaleidahealth.org/Childrens/services/display.asp?s=694. Accessed January 4, 2017.
- 8.Shaken baby: Pennsylvania Shaken Baby Syndrome Prevention Program. PennState Health, Children’s Hospital website. http://www.pennstatehershey.org/web/shakenbaby. Accessed January 4, 2017.
- 9.My Baby Keeps on Crying…I Just Want the Crying to Stop. Pennsylvania Dept of Health; http://www.health.pa.gov/My%20Health/Infant%20and%20Childrens%20Health/Newborns%20and%20Infants/Documents/ShakenBabyBrochure%20Eng-Spa.pdf. Revised November 2012. Accessed January 4, 2017. [Google Scholar]
- 10.Pennsylvania Health Care Cost Containment Council. http://www.phc4.org. Accessed January 4, 2017.
- 11.Parks SE, Annest JL, Hill HA, Karch DL. Pediatric Abusive Head Trauma: Recommended Definitions for Public Health Surveillance and Research. Atlanta, GA: Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 12.Parks SE, Kegler SR, Annest JL, Mercy JA. Characteristics of fatal abusive head trauma among children in the USA: 2003–2007: an application of the CDC operational case definition to national vital statistics data. Inj Prev. 2012;18(3):193–199. doi: 10.1136/injuryprev-2011-040128. [DOI] [PubMed] [Google Scholar]
- 13.Parks S, Sugerman D, Xu L, Coronado V. Characteristics of non-fatal abusive head trauma among children in the USA, 2003–2008: application of the CDC operational case definition to national hospital inpatient data. Inj Prev. 2012;18(6):392–398. doi: 10.1136/injuryprev-2011-040234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ellingson KD, Leventhal JM, Weiss HB. Using hospital discharge data to track inflicted traumatic brain injury. Am J Prev Med. 2008;34((4)(suppl)):S157–S162. doi: 10.1016/j.amepre.2007.12.021. [DOI] [PubMed] [Google Scholar]
- 15.Berger RP, Parks S, Fromkin J, Rubin P, Pecora PJ. Assessing the accuracy of the International Classification of Diseases codes to identify abusive head trauma: a feasibility study. Inj Prev. 2015;21(e1):e133–e137. doi: 10.1136/injuryprev-2013-040924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kesler H, Dias MS, Shaffer M, Rottmund C, Cappos K, Thomas NJ. Demographics of abusive head trauma in the Commonwealth of Pennsylvania. J Neurosurg Pediatr. 2008;1(5):351–356. doi: 10.3171/PED/2008/1/5/351. [DOI] [PubMed] [Google Scholar]
- 17.Zolotor AJ, Runyan DK, Shanahan M, et al. Effectiveness of a statewide abusive head trauma prevention program in North Carolina. JAMA Pediatr. 2015;169(12):1126–1131. doi: 10.1001/jamapediatrics.2015.2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keenan HT, Leventhal JM. A case-control study to evaluate Utah’s shaken baby prevention program. Acad Pediatr. 2010;10(6):389–394. doi: 10.1016/j.acap.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Showers J. “Don’t Shake the Baby”: the effectiveness of a prevention program. Child Abuse Negl. 1992;16(1):11–18. doi: 10.1016/0145-2134(92)90004-b. [DOI] [PubMed] [Google Scholar]
- 20.Deyo G, Skybo T, Carroll A. Secondary analysis of the “Love Me…Never Shake Me” SBS education program. Child Abuse Negl. 2008;32(11):1017–1025. doi: 10.1016/j.chiabu.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 21.Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH. A population-based study of inflicted traumatic brain injury in young children. JAMA. 2003;290(5):621–626. doi: 10.1001/jama.290.5.621. [DOI] [PubMed] [Google Scholar]
- 22.Barlow KM, Minns RA. Annual incidence of shaken impact syndrome in young children. Lancet. 2000;356(9241):1571–1572. doi: 10.1016/S0140-6736(00)03130-5. [DOI] [PubMed] [Google Scholar]
- 23.Fujiwara T, Barr RG, Brant RF, Rajabali F. Using International Classification of Diseases, 10th Edition, codes to estimate abusive head trauma in children. Am J Prev Med. 2012;43(2):215–220. doi: 10.1016/j.amepre.2012.04.028. [DOI] [PubMed] [Google Scholar]
- 24.Russell BS, Trudeau J, Britner PA. Intervention type matters in primary prevention of abusive head injury: event history analysis results. Child Abuse Negl. 2008;32(10):949–957. doi: 10.1016/j.chiabu.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Olds DL, Henderson CR, Jr, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics. 1986;78(1):65–78. [PubMed] [Google Scholar]
- 26.Olds DL, Eckenrode J, Henderson CR, Jr, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect: fifteen-year follow-up of a randomized trial. JAMA. 1997;278(8):637–643. [PubMed] [Google Scholar]
- 27.Xiang J, Shi J, Wheeler KK, Yeates KO, Taylor HG, Smith GA. Paediatric patients with abusive head trauma treated in US emergency departments, 2006–2009. Brain Inj. 2013;27(13–14):1555–1561. doi: 10.3109/02699052.2013.831126. [DOI] [PubMed] [Google Scholar]
- 28.Huang MI, O’Riordan MA, Fitzenrider E, McDavid L, Cohen AR, Robinson S. Increased incidence of nonaccidental head trauma in infants associated with the economic recession. J Neurosurg Pediatr. 2011;8(2):171–176. doi: 10.3171/2011.5.PEDS1139. [DOI] [PubMed] [Google Scholar]
- 29.Berger RP, Fromkin JB, Stutz H, et al. Abusive head trauma during a time of increased unemployment: a multicenter analysis. Pediatrics. 2011;128(4):637–643. doi: 10.1542/peds.2010-2185. [DOI] [PubMed] [Google Scholar]
- 30.Wood JN, French B, Fromkin J, et al. Association of pediatric abusive head trauma rates with macroeconomic indicators. Acad Pediatr. 2016;16(3):224–232. doi: 10.1016/j.acap.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 31.Mikton C, Butchart A. Child maltreatment prevention: a systematic review of reviews. Bull World Health Organ. 2009;87(5):353–361. doi: 10.2471/BLT.08.057075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klevens J, Luo F, Xu L, Peterson C, Latzman NE. Paid family leave’s effect on hospital admissions for pediatric abusive head trauma. Inj Prev. 2016;22(6):442–445. doi: 10.1136/injuryprev-2015-041702. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


