Abstract
Context
Little is known about the health of transgender adults in the United States, a growing population. There have been no large reports examining differences in health status and cardiometabolic disease in subgroups of transgender adults [female-to-male (FTM), male-to-female (MTF), and gender nonconforming (GNC)] in the United States.
Objective
Compare the health status and prevalence of cardiometabolic disease among specific subgroups of transgender adults (FTM, MTF, GNC) with those of cisgender adults in the United States.
Design
Secondary data analysis based on the 2015 Behavioral Risk Factor Surveillance System survey.
Setting
The 22 states in the United States that asked about transgender identity.
Participants
Noninstitutionalized adults age ≥18 years who reside in the United States, identified through telephone-based methods.
Main Outcome Measures
Data were extracted for respondents who answered the transgender identity question. Weighted percentages are given for all measures. Adjusted odds ratios (ORs) are reported for health status and cardiometabolic disease measures.
Results
FTM adults have a higher odds of being uninsured than both cisgender women [OR 3.8; 95% confidence interval (CI), 2.1 to 7.1] and cisgender men (OR 2.5; 95% CI, 1.4 to 4.7). MTF adults have a higher odds of reporting myocardial infarction than cisgender women (OR 2.9; 95% CI, 1.6 to 5.3) but not cisgender men.
Conclusions
There are significant differences in health status measures and cardiometabolic health between subgroups of transgender adults and cisgender adults. There is a need for additional research to understand the societal and medical (e.g., hormone therapy) effects on these outcomes.
Keywords: gender nonconforming, health insurance, myocardial infarction, transgender
There are differences in health status and cardiometabolic health among subgroups of transgender adults compared with cisgender adults on the 2015 Behavioral Risk Factor Surveillance System survey.
Recent reports show that 0.5% of adults and 3% of youth in the United States identify as transgender, meaning that their gender identity differs from birth sex [1–3]. Some data suggest that an increasing percentage of young people identify as somewhere in the middle of the gender spectrum, with identities that include gender fluid, gender nonconforming (GNC), agender, and others [3]. Despite increased recognition of transgender people in the United States, many still experience harassment or discrimination in medical settings [4], medical providers are inadequately trained [5], and guidelines for care of this population are based largely on expert opinion and small, retrospective studies, primarily from Europe [6, 7]. Understanding transgender-specific health needs is a research priority of the Institute of Medicine [8]; however, the health disparities of specific transgender subgroups are likely to be distinct. Furthermore, the majority of transgender adults receive gender-affirming hormone therapy [4], yet the long-term effects of these therapies on cardiometabolic health are not well understood.
The Behavioral Risk Factor Surveillance System (BRFSS), a large national survey in the United States, began including questions about transgender identity in select states in 2014 [1, 2], providing, for the first time, an opportunity to better understand the specific health needs of transgender adults nationally. Initial reports of the 2014 BRFSS survey showed that compared with cisgender adults (those whose gender identity aligns with birth sex), transgender adults were more likely to report fair or poor health, lack access to a personal health care provider, and lack health insurance [1]. However, these analyses did not analyze results by important subgroups, including male-to-female (MTF), female-to-male (FTM), and GNC adults, populations for whom health status measures are likely to be distinct because of the potentially different societal stressors experienced or medical therapies sought. A recent review [9] and meta-analysis [10] found that hormone therapy, including testosterone and estradiol, may be associated with worsening cardiometabolic risk factors, although there are several limitations to the available data.
In this study, we used the 2015 BRFSS database to compare the health status and prevalence of self-reported cardiometabolic disease among specific subgroups of transgender adults (FTM, MTF, and GNC) compared with cisgender adults, adjusting for important covariates. We hypothesized that all subgroups of transgender adults (MTF, FTM, and GNC) would have a higher odds of being uninsured compared with cisgender adults. Additionally, we hypothesized that MTF adults would have a higher odds of myocardial infarction (MI) compared with both cisgender men and women.
1. Subjects and Methods
The Colorado Multiple Institutional Review Board reviewed the protocol, and because this report includes only a review of deidentified, previously collected data and there was no interaction, no intervention, and no privately identifiable data collected from living human beings by our team, the Institutional Review Board determined that this research did not meet the definition of research involving human subjects.
A. BRFSS Survey
The yearly BRFSS survey started in 1984. All 50 states, the District of Columbia, Puerto Rico, Guam, and the US Virgin Islands now participate. It is administered by the Centers for Disease Control. The objective of the BRFSS is “to collect uniform, state-specific data on preventive health practices and risk behaviors that are linked to chronic diseases, injuries, and preventable infectious diseases that affect the adult population” [11]. Each year there are “core sections,” which every state includes, and several “optional modules” states can choose to include. In 2014, the BRFSS offered an optional “sexual orientation and gender identity” module, which 19 states and Guam included in their survey. In 2015, 22 states (Colorado, Connecticut, Delaware, Georgia, Hawaii, Idaho, Illinois, Indiana, Iowa, Kansas, Maryland, Massachusetts, Minnesota, Missouri, Nevada, New York, Ohio, Pennsylvania, Texas, Virginia, West Virginia, and Wisconsin) included this module (module 21) [12].
B. Study Subjects
Participants in the BRFSS include noninstitutionalized adults age ≥18 years who reside in the United States, identified through telephone-based methods (cellular and landlines). Question #2 of the “sexual orientation and gender identity module” asked, “Do you consider yourself to be transgender?” Of the 199,113 respondents in the 22 states that included the “sexual orientation and gender identity” module in the 2015 BRFSS survey, 169,559 respondents answered this question. Of those, 2500 (1.5%) refused or did not know, leaving 167,059 (98.5%) respondents for the analysis.
For the cardiometabolic analyses, respondents with chronic obstructive pulmonary disease or cancer were also excluded (n = 27,870, 16.7%) because these conditions could bias the results. These conditions were excluded because chronic obstructive pulmonary disease is known to increase the risk of cardiovascular disease by twofold to threefold [13]. Cancer was excluded because the type of cancer was not specified, and certain past or present treatments for cancer may increase the risk of cardiometabolic disease.
C. Data Elements and Definitions
If respondents identified as transgender, they were then asked, “Do you consider yourself to be (1) male-to-female, (2) female-to-male, or (3) gender nonconforming?” If the participant asked about the definition of transgender, the interviewer replied, “Some people describe themselves as transgender when they experience a different gender identity from their sex at birth. For example, a person born into a male body but who feels female or lives as a woman would be transgender. Some transgender people change their physical appearance so that it matches their internal gender identity. Some transgender people take hormones, and some have surgery. A transgender person may be of any sexual orientation: straight, gay, lesbian, or bisexual.” If the participant asked about the definition of gender nonconforming, the interviewer note stated, “Some people think of themselves as gender nonconforming when they do not identify only as a man or only as a woman” [12].
C-1. Demographic characteristics
For demographics (section 7), we extracted age, sex, race, ethnicity, marital status, completed level of education, employment status, income, and sexual orientation. The response categories for all variables are shown in Table 1. For the sex variable, the following instructions to the interviewer were included: “Indicate sex of respondent. Ask only if necessary” (male or female). The sex of the respondent may have been asked in the screening process if the call was made to a landline and there were several adults in a household (e.g., the interviewer would ask to speak with the “oldest male”), and then the sex would not be asked again. It is not known what percentage of the time the sex was inferred.
Table 1.
Comparisons of Demographic Characteristics Between Transgender and Cisgender Overall and Between Transgender Subgroups
| All Transgender, n = 764 |
All Cisgender, n = 166,295 |
χ
2 Transgender vs Cisgender |
Transgender FTM, n = 239 |
Transgender MTF, n = 369 |
Transgender GNC, n = 156 |
χ
2 FTM vs MTF vs GNC |
|
|---|---|---|---|---|---|---|---|
| Variable | % (95% CI) | % (95% CI) | P | % (95% CI) | % (95% CI) | % (95% CI) | P |
| Age, y | 0.014 | 0.002 | |||||
| 18–24 | 18.8 (13.2–24.4) | 11.9 (11.5–12.3) | 14.4 (4.8–23.9) | 17.1 (9.8–24.4) | 28.2 (14.2–42.2) | ||
| 25–34 | 14.6 (10.0–19.1) | 15.3 (14.9–15.7) | 13.6 (5.8–21.5) | 14.7 (7.7–21.6) | 15.6 (6.4–24.8) | ||
| 35–44 | 19.3 (12.7–26.0) | 16.1 (15.8–16.5) | 37.2 (21.8–52.6) | 13.0 (5.6–20.4) | 11.1 (3.1–19.1) | ||
| 45–54 | 14.4 (10.5–18.2) | 18.2 (17.8–18.5) | 9.3 (4.1–14.5) | 18.9 (12.5–25.4) | 10.4 (4.2–16.7) | ||
| 55–64 | 15.7 (11.7–19.8) | 17.8 (17.5–18.1) | 10.7 (5.4–16.1) | 18.8 (12.4–25.2) | 15.2 (7.0–23.3) | ||
| ≥65 | 17.2 (13.2–21.3) | 20.7 (20.5–21.0) | 14.8 (8.8–20.8) | 17.5 (12.3–22.8) | 19.5 (8.1–31.0) | ||
| Sex | <0.001 | <0.001 | |||||
| Male | 65.0 (59.0–71.1) | 47.7 (47.3–48.2) | 41.1 (26.8–55.5) | 80.7 (74.5–86.9) | 59.7 (46.5–73.0) | ||
| Female | 35.0 (28.9–41.0) | 52.3 (51.8–52.7) | 58.9 (44.5–73.2) | 19.3 (13.1–25.5) | 40.3 (27.0–53.5) | ||
| Race or ethnicity | <0.001 | 0.28 | |||||
| White, non-Hispanic | 56.4 (49.5–63.2) | 69.9 (69.4–70.4) | 50.1 (36.1–64.0) | 61.3 (52.0–70.7) | 53.1 (39.1–67.1) | ||
| Black, non-Hispanic | 10.9 (6.8–15.0) | 11.9 (11.5–12.2) | 8.1 (2.1–14.1) | 12.9 (6.4–19.4) | 10.0 (1.7–18.4) | ||
| Hispanic | 20.4 (14.3–26.6) | 12.9 (12.5–13.2) | 31.5 (17.7–45.2) | 12.7 (5.7–19.7) | 24.0 (10.6–37.4) | ||
| Other race, non-Hispanic | 12.3 (6.9–17.6) | 5.4 (5.1–5.6) | 10.3 (0.0–22.4) | 13.1 (5.8–20.4) | 12.9 (3.9–21.9) | ||
| Sexual orientation | <0.001 | 0.24 | |||||
| Straight | 74.6 (68.4–80.9) | 96.3 (96.1–96.4) | 79.9 (68.7–91.1) | 77.4 (68.8–86.1) | 62.2 (48.2–76.3) | ||
| Lesbian or gay | 4.5 (1.8–7.3) | 1.5 (1.3–1.6) | 5.7 (0.0–12.6) | 2.6 (0.4–4.8) | 7.5 (0.0–15.1) | ||
| Bisexual | 15.9 (10.6–21.1) | 1.9 (1.7–2.0) | 11.2 (2.4–20.0) | 13.7 (6.8–20.6) | 26.2 (13.1–39.3) | ||
| Other | 5.0 (1.3–8.7) | 0.4 (0.3–0.5) | 3.2 (0.0–7.8) | 6.3 (0.0–12.6) | 4.1 (0.0–9.6) | ||
| Marital status | 0.013 | 0.71 | |||||
| Married | 45.3 (38.6–52.0) | 52.3 (51.9–52.8) | 51.9 (37.9–65.8) | 44.3 (35.4–53.2) | 39.6 (26.2–53.0) | ||
| Formerly married (divorced, widowed, separated) | 18.9 (14.5–23.3) | 20.3 (20.0–20.7) | 17.8 (9.3–26.3) | 19.4 (13.2–25.7) | 19.1 (10.1–28.0) | ||
| Never married (never married or unmarried couple) | 35.8 (29.3–42.3) | 27.3 (26.9–27.8) | 30.3 (17.5–43.1) | 36.3 (27.5–45.0) | 41.3 (27.3–55.3) | ||
| Employment status | 0.001 | 0.087 | |||||
| Employed (for wages or self-employed) | 49.7 (43.1–56.3) | 57.5 (57.1–58.0) | 53.5 (40.2–66.8) | 48.6 (39.7–57.6) | 47.7 (33.9–61.4) | ||
| Unemployed (out of work) | 8.5 (4.2–12.8) | 5.4 (5.2–5.7) | 6.2 (1.0–11.4) | 10.5 (3.1–18.0) | 6.6 (0.9–12.3) | ||
| Homemaker | 5.5 (2.3–8.6) | 6.6 (6.3–6.8) | 12.1 (2.7–21.6) | 2.6 (0.4–4.7) | 4.2 (0.0–10.2) | ||
| Student | 10.1 (5.7–14.5) | 5.3 (5.1–5.6) | 6.4 (0.9–11.8) | 9.0 (3.5–14.5) | 16.9 (4.1–29.7) | ||
| Retired | 16.4 (12.2–20.7) | 18.7 (18.4–19.0) | 10.8 (6.0–15.6) | 18.2 (12.0–24.4) | 19.1 (8.3–30.0) | ||
| Unable to work | 9.8 (6.6–13.0) | 6.4 (6.2–6.6) | 11.0 (4.5–17.6) | 11.1 (6.4–15.8) | 5.5 (0.5–10.5) | ||
| Completed level of education | <0.001 | 0.009 | |||||
| Did not graduate high school | 25.3 (18.7–32.0) | 13.0 (12.6–13.4) | 40.8 (26.4–55.3) | 21.0 (12.6–29.4) | 15.6 (3.9–27.2) | ||
| Graduated high school | 35.4 (29.3–41.5) | 29.1 (28.6–29.5) | 33.9 (20.8–47.0) | 38.5 (30.2–46.9) | 30.2 (18.7–41.6) | ||
| Attended college or technical school | 23.9 (18.3–29.4) | 30.9 (30.4–31.3) | 13.6 (6.6–20.6) | 24.7 (17.0–32.4) | 34.8 (20.8–48.7) | ||
| Graduated from college or technical school | 15.5 (11.5–19.4) | 27.1 (26.8–27.5) | 11.7 (6.2–17.3) | 15.7 (9.9–21.5) | 19.5 (10.2–28.8) | ||
| Income | <0.001 | 0.24 | |||||
| <$15,000 | 16.1 (10.9–21.2) | 9.6 (9.3–9.9) | 12.8 (4.5–21.1) | 19.0 (11.3–26.8) | 13.3 (2.8–23.9) | ||
| $15,000 to <$25,000 | 24.0 (17.6–30.5) | 16.2 (15.8–16.6) | 23.7 (9.7–37.6) | 24.6 (15.7–33.4) | 23.2 (10.6–35.8) | ||
| $25,000 to <$35,000 | 14.4 (8.6–20.3) | 10.3 (10.0–10.6) | 23.5 (8.7–38.4) | 14.0 (6.1–21.9) | 5.2 (1.0–9.4) | ||
| $35,000 to <$50,000 | 11.5 (8.1–14.9) | 14.1 (13.8–14.5) | 12.5 (5.9–19.2) | 10.9 (6.2–15.7) | 11.6 (4.4–18.7) | ||
| ≥$50,000 | 34.0 (27.3–40.7) | 49.8 (49.3–50.3) | 27.4 (12.7–42.2) | 31.4 (23.4–39.5) | 46.7 (32.0–61.4) |
All percentages and CIs were design adjusted, whereas sample size was not.
C-2. Health status
For health status, we report on health status (BRFSS section 1), number of healthy days (section 2), health care access (section 3), tobacco use (section 8), alcohol consumption (section 9), and exercise (section 11). Specific measures included general health rating (excellent, very good, good, fair, or poor, which we categorized into a binary variable: excellent/very good/good vs fair, poor); activity limitation due to physical, mental, or emotional problems; number of days their physical health was not good; number of days their mental health was not good; number of days their physical or mental health was not good out of the last 30 days (we categorized the number of days into 0 to 13 days or ≥14 days); for those <65 years old, whether they have health care coverage (because Medicare eligibility begins at age 65); whether they have one or more primary doctors; length of time since their last routine checkup; current smoker; binge drinking (defined as drinking ≥5 drinks on an occasion for men or ≥4 drinks on an occasion for women); and whether they are meeting aerobic exercise recommendations (calculated as 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous activity per week).
C-3. Cardiometabolic disease
For cardiometabolic disease we reported on overweight or obesity, history of hypertension (BRFSS section 4.1), MI (section 6.1), angina or coronary heart disease (CHD; section 6.2), stroke (section 6.2), or diabetes (section 6.12). Body mass index was calculated from reported weight and height (weight in kilograms divided by height in meters squared); overweight was defined as a body mass index of 25 to 29.9 kg/m2 and obesity as ≥30 kg/m2.
D. Data Analysis
The primary outcome for health status was no health care coverage, and the primary outcome for cardiometabolic disease was MI. Weighted percentages and 95% confidence intervals (CIs) were calculated for the demographic categories for transgender vs cisgender adults and for the subgroups of transgender adults (FTM, MTF, GNC). Design-adjusting Rao-Scott χ2 tests were used to compare differences between groups. All health status and cardiometabolic outcomes were binary; logistic regression was performed to estimate unadjusted and adjusted odds ratios (ORs), 95% CIs, and P values. Adjusting variables included categorical age (18 to 24, 25 to 34, 35 to 44, 45 to 54, 55 to 64, or ≥65 years), race or ethnicity, and income. Only adjusted results are presented here because there were differences in health status measures and cardiometabolic health measures between the unadjusted results and the adjusted results. To preserve the sample size in the subgroups of interest, a missing category was added to income (data missing for 15% of respondents). Those missing race or ethnicity (missing for 1%) were categorized as “Non-Hispanic white.” No respondent was missing age. Custom hypothesis tests in proc surveylogistic were constructed to test differences in the six-category transgender variable via an F test, specifically FTM vs cisgender women, FTM vs cisgender men, MTF vs cisgender women, MTF vs cisgender men, gender nonconforming adults with a recorded male sex (GNC-M) vs cisgender men, and gender nonconforming adults with a recorded female sex (GNC-F) vs cisgender women for all health status and cardiometabolic health measures. A dichotomous variable replaced the six-category variable to test transgender vs all cisgender.
To account for noncoverage and nonresponse bias, the data are weighted with an iterative proportional fitting technique called raking. Raking accounts for both the sampling design and nonresponse to the survey. The Centers for Disease Control provides these weights along with details of the weighting technique on their Web site [11]. Incorporating weights is important in analysis of survey data because it adjusts results so that they are more representative of the true population (e.g., if a particular stratum is oversampled this would be corrected through weights) and adjusts for nonresponse bias. All analyses were conducted with SAS version 9.4 (SAS Institute, Inc., Cary, NC). Given the number of comparisons, a more conservative alpha of 0.01 (two-sided) was considered significant.
2. Results
A. Demographics
Of the 167,059 (98.5%) respondents in the analysis, 764 answered “yes,” they identified as transgender (0.57%; 95% CI, 0.50% to 0.65%). Of those who answered “yes,” 369 identified as MTF (0.29%; 95% CI, 0.24% to 0.34%), 239 as FTM (0.16%; 95% CI, 0.12% to 0.21%), and 156 as GNC (0.13%; 95% CI, 0.09% to 0.16%). A total of 166,295 respondents answered “no,” they did not identify as transgender (reported here as cisgender, 99.42%; 95% CI, 99.35% to 99.50%). The results provided represent unweighted frequencies and weighted percentages.
The demographic characteristics of all transgender, all cisgender, FTM, MTF, and GNC adults are shown in Table 1. There were significant differences in demographics between transgender and cisgender adults for sex (P < 0.001), race or ethnicity (P < 0.001), sexual orientation (P < 0.001), employment status (P = 0.001), completed level of education (P < 0.001), and income (P < 0.001).
There were significant differences between transgender groups (FTM vs MTF vs GNC) for age (P = 0.002), sex (P < 0.001), and completed level of education (P = 0.009). It appears that there is a trend toward a younger age group for those who identified as GNC. The sex variable is different between groups, and the results show that some transgender adults answered this question based on their natal sex and others based on their gender identity.
B. All Transgender Compared With All Cisgender Adults
Weighted percentages and 95% CIs for all measures of health status and cardiometabolic health for all transgender compared with all cisgender adults are listed in Table 2. Transgender adults had a higher odds of lacking health care coverage (OR 1.7; 95% CI, 1.2 to 2.5; P = 0.006). Transgender adults did not have a higher odds of reporting overweight or obesity, hypertension, MI, angina or CHD, stroke, or diabetes.
Table 2.
Health Status and Cardiometabolic Health of All Transgender vs All Cisgender Adults
| All Transgender, n = 764 |
All Cisgender, n = 166,295 |
|
|---|---|---|
| Variable | % (95% CI) | % (95% CI) |
| General health fair or poor | 20.9 (16.0–25.8) | 16.8 (16.4–17.1) |
| Activity limitation due to physical, mental, or emotional problems | 24.4 (19.2–29.6) | 20.1 (19.7–20.4) |
| ≥14 d in the last 30 d physical health not good | 12.6 (8.9–16.2) | 11.7 (11.4–12.0) |
| ≥14 d in the last 30 d mental health not good | 17.0 (11.8–22.2) | 10.9 (10.6–11.2) |
| ≥14 d in the last 30 d poor physical or mental health prevented usual activities | 13.0 (8.5–17.5) | 7.5 (7.3–7.8) |
| No health care coverage | 25.4 (17.7–33.1)a | 13.6 (13.1–14.0) |
| No personal doctor | 24.3 (17.9–30.8) | 19.1 (18.7–19.6) |
| >1 y since last routine checkup | 32.1 (25.8–38.4) | 28.9 (28.5–29.4) |
| Current smoker | 19.7 (14.4–24.9) | 16.8 (16.5–17.2) |
| Binge drinking | 17.6 (12.2–23.0) | 16.4 (16.1–16.8) |
| Does not meet physical activity aerobic recommendations | 57.6 (50.9–64.2) | 50.4 (50.0–50.9) |
| n = 632 | n = 138,557 | |
| Overweight or obese | 71.3 (64.3–78.2) | 65.2 (64.7–65.7) |
| Hypertension | 27.9 (22.0–33.8) | 29.4 (29.0–29.9) |
| MI | 4.4 (2.3–6.4) | 3.3 (3.1–3.4) |
| Angina or CHD | 3.2 (1.6–4.9) | 3.0 (2.8–3.1) |
| Stroke | 2.3 (1.0–3.5) | 2.4 (2.3–2.6) |
| Diabetes | 9.5 (5.7–13.2) | 9.3 (9.0–9.5) |
Design-adjusted percentage and 95% CIs for self-reported health status measures of disease among transgender and cisgender adults.
Significant results for adjusted ORs: Statistically significant difference between all transgender and all cisgender adults, P < 0.01.
C. FTM Compared With Cisgender Adults
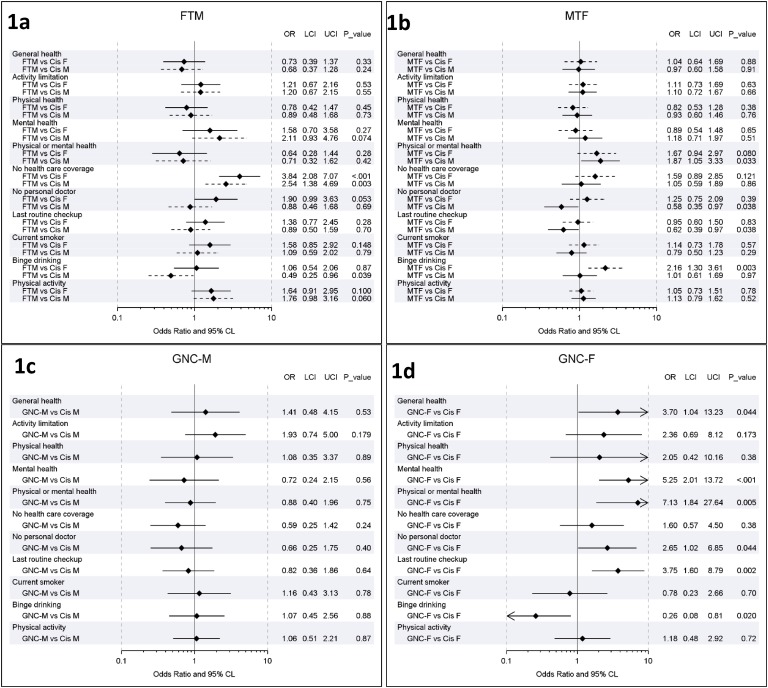
Comparisons of health status measures between FTM adults and cisgender men and women are listed in Table 3 (weighted percentages and 95% CIs) and Fig. 1a (adjusted ORs and 95% CI). FTM adults were significantly more likely to lack health care coverage than both cisgender women (OR 3.8; 95% CI, 2.1 to 7.1; P < 0.001) and cisgender men (OR 2.5; 95% CI, 1.4 to 4.7; P = 0.003).
Table 3.
Health Status of Transgender Subgroups and Cisgender Adults
| FTM, n = 239 |
MTF, n = 369 |
GNC-M, n = 79 |
GNC-F, n = 77 |
Cis M, n = 70,123 |
Cis F, n = 96,172 |
|
|---|---|---|---|---|---|---|
| Variable | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) |
| General health fair or poor | 14.7 (7.3–22.1) | 20.4 (13.7–27.1) | 22.1 (9.3–34.9) | 41.8 (20.8–62.8) | 16.1 (15.6–16.6) | 17.4 (17.0–17.9) |
| Activity limitation due to physical, mental, or emotional problems | 21.2 (11.8–30.7) | 23.5 (16.7–30.4) | 27.2 (11.9–42.5) | 34.9 (14.7–55.0) | 19.2 (18.7–19.7) | 20.9 (20.4–21.4) |
| ≥14 d in the last 30 d physical health not good | 10.7 (4.9–16.4) | 12.2 (7.6–16.8) | 10.8 (1.0–20.6) | 22.6 (2.8–42.4) | 10.3 (9.9–10.7) | 12.9 (12.5–13.3) |
| ≥14 d in the last 30 d mental health not good | 19.8 (7.7–31.9) | 13.6 (7.7–19.6) | 7.0 (0.3–13.8) | 42.1 (20.7–63.6)a | 9.3 (8.8–9.7) | 12.5 (12.0–12.9) |
| ≥14 d in the last 30 d poor physical or mental health prevented usual activities | 5.6 (1.5–9.8) | 15.0 (8.0–21.9) | 5.7 (1.6–9.8) | 35.9 (14.3–57.5)b | 6.7 (6.4–7.0) | 8.3 (8.0–8.7) |
| No health care coverage | 42.8 (26.3–59.3)a,c | 20.1 (10.1–30.2) | 10.3 (2.2–18.4) | 17.9 (1.8–33.9) | 15.0 (14.3–15.7) | 12.2 (11.6–12.8) |
| No personal doctor | 31.5 (17.3–45.6) | 19.9 (11.4–28.4) | 21.6 (5.7–37.4) | 31.2 (11.7–50.8) | 24.5 (23.8–25.2) | 14.3 (13.7–14.8) |
| >1 y since last routine checkup | 34.9 (22.2–47.6) | 26.3 (17.9–34.8) | 30.4 (13.3–47.5) | 59.3 (40.5–78.1)b | 33.8 (33.1–34.5) | 24.4 (23.9–25.0) |
| Current smoker | 22.7 (10.6–34.7) | 19.4 (12.5–26.3) | 19.5 (5.7–33.3) | 11.9 (0.0–23.7) | 19.1 (18.5–19.7) | 14.8 (14.3–15.2) |
| Binge drinking | 12.2 (5.2–19.3) | 21.0 (12.5–29.5)b | 26.1 (8.6–43.5) | 3.5 (0.0–7.1) | 22.2 (21.5–22.8) | 11.2 (10.8–11.6) |
| Does not meet physical activity aerobic recommendations | 66.6 (52.7–80.4) | 54.7 (45.8–63.7) | 50.7 (32.2–69.2) | 56.8 (36.8–76.9) | 49.1 (48.4–49.8) | 51.7 (51.1–52.3) |
Design-adjusted percentage and 95% CIs for self-reported health status measures of disease among transgender individuals (including FTM, MTF, GNC-M, GNC-F) and cisgender adults (including Cis M and Cis F).
Significant results for adjusted ORs (see Fig. 1): Statistically significant difference between either FTM, MTF, or GNC-F and cisgender women (aP < 0.001, bP < 0.01); statistically significant difference between either FTM, MTF, or GNC-M and cisgender men (cP < 0.01, dP < 0.001).
Figure 1.
Odds of self-reported health status measures among transgender subgroups vs cisgender men and women. Forest plots depicting adjusted ORs and lower 95% confidence intervals (LCIs) and upper 95% confidence intervals (UCIs) for health status measures among (a) FTM vs cisgender men and women, (b) MTF vs cisgender men and women, (c) GNC-M vs cisgender men, and (d) GNC-F vs cisgender women. Comparisons on the basis of natal sex are depicted with a solid line (FTM vs Cis F, MTF vs Cis M, GNC-M vs Cis M, GNC-F vs Cis F), and comparisons on the basis of gender identity are depicted with a dashed line (FTM vs Cis M, MTF vs Cis F). Cis F, cisgender female, female sex and female gender identity; Cis M, cisgender male, male sex and male gender identity.
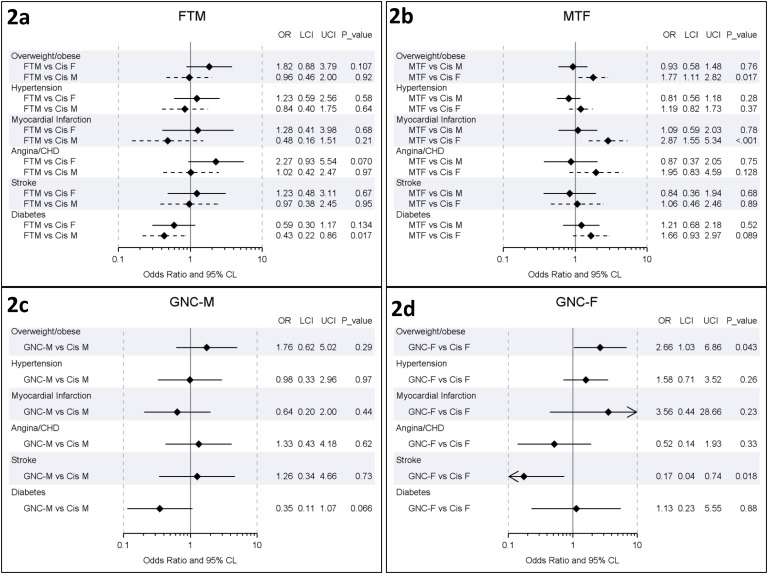
Comparisons of self-reported cardiometabolic disease between FTM adults and cisgender men and women are listed in Table 4 and Fig. 2a. There were no differences in self-reported cardiometabolic factors between FTM adults and cisgender men or women.
Table 4.
Frequency of Cardiometabolic Disease in Transgender Subgroups and Cisgender Adults
| FTM, n = 197 |
MTF, n = 307 |
GNC-M, n = 68 |
GNC-F, n = 61 |
Cis M, n = 60,009 |
Cis F, n = 78,548 |
|
|---|---|---|---|---|---|---|
| Variable | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) |
| Overweight or obese | 72.3 (56.6–88.0) | 68.7 (59.2–78.2) | 75.9 (59.6–92.2) | 76.6 (59.0–94.3) | 71.6 (70.9–72.3) | 58.6 (57.9–59.3) |
| Hypertension | 25.2 (12.7–37.8) | 29.2 (21.5–36.8) | 23.0 (7.9–38.1) | 37.0 (15.9–58.2) | 31.7 (31.0–32.3) | 27.3 (26.8–27.9) |
| MI | 2.0 (0.0–4.3) | 5.5 (2.5–8.6)a | 2.1 (0.0–4.3) | 8.7 (0.0–22.0) | 4.4 (4.2–4.7) | 2.2 (2.0–2.3) |
| Angina or CHD | 3.1 (0.4–5.8) | 3.5 (0.8–6.3) | 3.4 (0.0–6.7) | 1.3 (0.0–2.8) | 3.9 (3.6–4.1) | 2.1 (2.0–2.3) |
| Stroke | 2.3 (0.2–4.3) | 2.6 (0.5–4.7) | 2.3 (0.0–5.1) | 0.6 (0.0–1.3) | 2.5 (2.3–2.7) | 2.4 (2.2–2.6) |
| Diabetes | 4.4 (1.5–7.4) | 13.4 (6.8–19.9) | 3.2 (0.0–6.6) | 12.7 (0.0–26.9) | 10.0 (9.6–10.4) | 8.6 (8.2–8.9) |
Design-adjusted percentage and 95% CIs for self-reported health status measures of disease among transgender adults (including FTM, MTF, GNC-M, and GNC-F) and cisgender adults (including Cis M and Cis F).
Significant results for adjusted ORs (see Fig. 2): Statistically significant difference between either FTM, MTF, or GNC-F and cisgender women, P < 0.01.
Figure 2.
Odds of self-reported cardiometabolic disease among transgender subgroups vs cisgender adults. Forest plots depicting adjusted ORs and lower 95% confidence intervals (LCIs) and upper 95% confidence intervals (UCIs) 95% CIs for cardiometabolic disease measures among (a) FTM vs cisgender men and women, (b) MTF vs cisgender men and women, (c) GNC-M vs cisgender men, and (d) GNC-F vs cisgender women. Comparisons on the basis of natal sex are depicted with a solid line (FTM vs Cis F, MTF vs Cis M, GNC-M vs Cis M, GNC-F vs Cis F), and comparisons on the basis of gender identity are depicted with a dashed line (FTM vs Cis M, MTF vs Cis F). Cis F, cisgender female, female sex and female gender identity; Cis M, cisgender male, male sex and male gender identity.
D. MTF Compared With Cisgender Adults
Comparisons of health status measures between MTF adults and cisgender men and women are listed in Table 3 and Fig. 1b. There was no significant difference in health insurance coverage for MTF compared with either cisgender men or cisgender women. MTF adults were more likely to report binge drinking than cisgender women (OR 2.2; 95% CI, 1.3 to 3.6; P = 0.003), but there were no significant differences compared with cisgender men.
Comparisons of self-reported cardiometabolic disease between MTF adults and cisgender men and women are listed in Table 4 and Fig. 2b. MTF adults had higher odds of reporting an MI than cisgender women (OR 2.9; 95% CI, 1.6 to 5.3; P < 0.001) but not cisgender men.
E. GNC Compared With Cisgender Adults
Comparisons of health status measures between GNC adults and cisgender men and women are listed in Table 3 and Fig. 1c and 1d. There were no significant differences in health status measures between GNC-M adults and cisgender men (Fig. 1c). GNC-F adults had several significant differences in health status measures compared with cisgender women (Fig. 1d). They had a higher odds of reporting that their mental health was not good ≥14 days out of the last 30 days (OR 5.3; 95% CI, 2.03 to 13.7; P < 0.001), that poor physical or mental health prevented usual activities for ≥14 days out of the last 30 days (OR 7.1; 95% CI, 1.8 to 27.6; P = 0.005), and that it had been more than a year since their last routine checkup (OR 3.8; 95% CI, 1.6 to 8.9; P = 0.002).
Comparisons of self-reported cardiometabolic disease between GNC adults and cisgender men and women are listed in Table 4 and Fig. 2c and 2d. There were no significant differences in self-reported cardiometabolic measures between GNC-M and cisgender men or GNC-F and cisgender women.
3. Discussion
This report on the health status and cardiometabolic health of specific subgroups of transgender adults in the United States is based on national survey data. We show that although transgender adults are more likely to lack health care coverage than cisgender adults, this difference appears to be specific to FTM adults. MTF and GNC adults in this sample do not have any differences in health care coverage compared with cisgender adults. MTF adults had higher odds of reporting MI compared with cisgender women but not men.
In this analysis, 0.57% of the adult respondents in the 2015 BRFSS survey identified as transgender. There appear to be differences in the age distributions of FTM, MTF, and GNC adults, with the GNC group having the highest percentage of participants between ages 18 and 24 years. In a report on 417 transgender adults in Colorado, 24% of respondents identified as gender queer or gender fluid, agender (or no gender), or other [14]. In the Human Rights Campaign’s 2012 Youth Survey, 9% of youth (925/10,000) identified as gender expansive, with one-third identifying as transgender and two-thirds as other [3]. The US transgender population is increasingly younger, and a greater proportion of young people fall somewhere in the middle of the gender spectrum, reporting GNC, gender fluid, or agender identities. The characteristics of this population are distinct from those who identify as MTF or FTM.
In this report, we show that there were no significant differences between GNC-M adults and cisgender men. However, there were several significant differences between GNC-F adults and cisgender women. GNC-F adults reported higher odds of poor mental and physical health than cisgender women. They were also more likely to report it had been more than a year since their last routine checkup. These differences in the health status of GNC adults deserve additional study, especially because this is a rapidly growing segment of the US population. Furthermore, unlike MTF and FTM adults, who often seek medical advice for medical or surgical therapies as a part of their transition (gender-affirming hormones such as testosterone or estradiol and gender-affirming surgeries), it is unclear what, if any, medical or surgical therapies are desired by GNC youth and adults. Lastly, the higher rate of poor physical and mental health, particularly in a segment of the GNC population, warrants additional investigation to determine how best to support this group.
Contrary to our initial hypothesis, our analysis suggests that the lack of health care coverage in the transgender population is specific to the FTM population and probably accounts for the overall difference in health care coverage previously reported between transgender and cisgender adults [1]. The BRFSS survey did not specifically ask respondents whether they were prescribed gender-affirming hormones, a part of physical transition for many transgender people [6]. It is unclear why there would be a difference in health care coverage for FTM adults because previous surveys have shown that most transgender adults are on hormone therapy [4], which would generally require frequent doctor visits.
MTF adults had higher adjusted odds of reporting MI than cisgender women but not men. We hypothesized that MTF adults would have a higher odds of MI compared with both cisgender men and cisgender women, based on the available literature. There are limited data on the long-term cardiometabolic health of transgender people, especially in the United States, with which to compare our data. Previous reports using BRFSS data have shown that transgender adults have a higher odds of reporting MI when adjusted for age, but this difference was not broken down by transgender subgroup [1]. Studies in the Netherlands have shown that MTF adults have higher mortality rates from ischemic heart disease compared with the general population (standardized mortality ratio 1.64; 95% CI, 1.43 to 1.87), and the use of ethinylestradiol is significantly associated with cardiovascular mortality (hazard ratio adjusted for age and smoking of 3.64; 95% CI, 1.52 to 8.73) [15]. A recent review showed that estradiol therapy in MTF adults may be associated with an increase in cardiovascular mortality [9]. We do not know what proportion of MTF adults in the 2015 BRFSS survey were on estradiol but in 2010 a national survey found that 71% of MTF adults were on hormone therapy [4]. However, use of ethinylestradiol has fallen out of favor [16, 17], and long-term studies on the effects of oral 17 beta-estradiol or transdermal estradiol, the preparations primarily used in the United States, are lacking. This is an important area of study because there are known sex differences for heart disease risk, with higher rates in cisgender men compared with women [18]. The sex hormones estradiol and testosterone can both be a risk factor and a protective factor for heart disease and diabetes in cisgender adults [19–24]. In cisgender women, estrogen/progestin combination therapy has been associated with increased risk of MI and stroke [25, 26]. The effects of hormone therapy on heart health are of critical importance for transgender adults, and additional studies are needed to delineate the genetic and hormonal effects on MI. If most of the MTF adults in this study were on estradiol (which we do not know), these data may suggest that estradiol therapy in this population does not markedly increase MI or stroke risk above that associated with their biologic sex because there were no differences in odds of self-reported MI or strokes in MTF adults compared with cisgender men. Furthermore, if most of the FTM adults in this study were on testosterone, these data may also suggest that testosterone does not increase cardiometabolic disease because there were no differences between FTM adults and cisgender men and women.
Strengths of this study include the highlighting of important health status differences in subgroups of transgender adults in a large group of MTF, FTM, and GNC adults in the United States. There are several limitations, including the fact that this is a secondary data analysis using self-report data from 22 states. Because the data are weighted, they are probably more representative of the US population as a whole. It is unclear what percentage of the time the respondent’s sex (male vs female) was given by the respondents or was not asked and inferred, based on the screening process. This limitation may have introduced significant bias in the results, particularly for the GNC adults (e.g., if a higher proportion of one of the GNC groups had the sex inferred from the screening questions rather than directly asked). This limitation is less likely to affect the results for FTM or MTF adults because the comparisons were based on their transgender identity, not sex. This limitation is unlikely to significantly affect the results for cisgender respondents. We do not know how long respondents have identified as transgender or GNC. We do not know what proportion of these respondents were on hormone therapy or for how long because this question was not included, although hormone therapy probably affects overall health status, including cardiometabolic health. Given the multiple tests conducted, some potential findings might be spurious. We used a more conservative P value of 0.01, given the number of comparisons. These results should be confirmed with additional studies and in future BRFSS surveys.
4. Conclusions
There are significant differences in health status measures and cardiometabolic health between subgroups of transgender adults and cisgender adults. There is a need for additional research to elucidate the societal and medical (e.g., hormone therapy) effects on these outcomes. Additionally, a growing proportion of young people identify as GNC, and their health status and mental and physical health needs are distinct from those who identify as FTM or MTF, and they warrant additional study.
Acknowledgments
Disclosure: The authors report no conflicts of interest in this work.
Glossary
Abbreviations:
- BRFSS
Behavioral Risk Factor Surveillance System
- CHD
coronary heart disease
- CI
confidence interval
- Cis F
cisgender female
- Cis M
cisgender male
- FTM
female-to-male
- GNC
gender nonconforming
- GNC-F
gender nonconforming adults with a recorded female sex
- GNC-M
gender nonconforming adults with a recorded male sex
- MI
myocardial infarction
- MTF
male-to-female
- OR
odds ratio.
References and Notes
- 1. Meyer IH, Brown TNT, Herman JL, Reisner SL, Bockting WO. Demographic characteristics and health status of transgender adults in select US regions: Behavioral Risk Factor Surveillance System, 2014. Am J Public Health. 2017;107(4):582–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Crissman HP, Berger MB, Graham LF, Dalton VK. Transgender demographics: a household probability sample of US adults, 2014. Am J Public Health. 2017; 107(2):213–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Baum J, Brill S, Brown J, Delpercio A, Kahn E, Kenney L, Nicoll A. Supporting and Caring for Our Gender Expansive Youth: Lessons From the Human Rights Campaign’s Youth Survey. Washington, DC: Human Rights Campaign Foundation and Gender Spectrum; 2012. Accessed 28 November 2017. www.hrc.org/youth-gender. [Google Scholar]
- 4. Grant JM, Mottet LA, Tanis J, Herman JL, Harrison J, Keisling M. National Transgender Discrimination Survey Report on Health and Health Care. Washington,DC: National Center for Transgender Equality and National Gay and Lesbian Task Force Washington; 2010:1–23. [Google Scholar]
- 5. Grant JM, Mottet L, Tanis JE, Harrison J, Herman J, Keisling M. Injustice at Every Turn: A Report of the National Transgender Discrimination Survey. Washington,DC: National Center for Transgender Equality; 2011. [Google Scholar]
- 6. Hembree WC, Cohen-Kettenis P, Delemarre-van de Waal HA, Gooren LJ, Meyer WJ III, Spack NP, Tangpricha V, Montori VM; Endocrine Society . Endocrine treatment of transsexual persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2009;94(9):3132–3154. [DOI] [PubMed] [Google Scholar]
- 7. Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, Rosenthal SM, Safer JD, Tangpricha V, T’Sjoen GG. Endocrine treatment of gender-dysphoric/gender-incongruent persons: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2017;102(11):3869–3903. [DOI] [PubMed] [Google Scholar]
- 8. Institute of Medicine The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 9. Streed CG Jr, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: a narrative review. Ann Intern Med. 2017;167(4):256–267. [DOI] [PubMed] [Google Scholar]
- 10. Maraka S, Singh Ospina N, Rodriguez-Gutierrez R, Davidge-Pitts CJ, Nippoldt TB, Prokop LJ, Murad MH. Sex steroids and cardiovascular outcomes in transgender individuals: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2017;102(11):3914–3923. [DOI] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System [Internet] Available at: https://www.cdc.gov/brfss/about/index.htm. Accessed 28 November 2017.
- 12. Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System Questionnaire 2015 [Internet] Available at: https://www.cdc.gov/brfss/questionnaires/pdf-ques/2015-brfss-questionnaire-12-29-14.pdf. Accessed 28 November 2017.
- 13. Sin DD, Man SFP. Why are patients with chronic obstructive pulmonary disease at increased risk of cardiovascular diseases? The potential role of systemic inflammation in chronic obstructive pulmonary disease. Circulation. 2003;107:1514–1519. [DOI] [PubMed] [Google Scholar]
- 14. One Colorado Education Fund Transparent: The State of Transgender Health in Colorado. Denver, CO: One Colorado Education Fund; 2014. [Google Scholar]
- 15. Asscheman H, Giltay EJ, Megens JAJ, de Ronde WP, van Trotsenburg MAA, Gooren LJG. A long-term follow-up study of mortality in transsexuals receiving treatment with cross-sex hormones. Eur J Endocrinol. 2011;164(4):635–642. [DOI] [PubMed] [Google Scholar]
- 16. Asscheman H, Gooren LJ, Eklund PL. Mortality and morbidity in transsexual patients with cross-gender hormone treatment. Metabolism. 1989;38(9):869–873. [DOI] [PubMed] [Google Scholar]
- 17. Gooren LJ, Wierckx K, Giltay EJ. Cardiovascular disease in transsexual persons treated with cross-sex hormones: reversal of the traditional sex difference in cardiovascular disease pattern. Eur J Endocrinol. 2014;170(6):809–819. [DOI] [PubMed] [Google Scholar]
- 18. Lerner DJ, Kannel WB. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am Heart J. 1986;111(2):383–390. [DOI] [PubMed] [Google Scholar]
- 19. Elting MW, Korsen TJ, Bezemer PD, Schoemaker J. Prevalence of diabetes mellitus, hypertension and cardiac complaints in a follow-up study of a Dutch PCOS population. Hum Reprod. 2001;16(3):556–560. [DOI] [PubMed] [Google Scholar]
- 20. Lewy VD, Danadian K, Witchel SF, Arslanian S. Early metabolic abnormalities in adolescent girls with polycystic ovarian syndrome. J Pediatr. 2001;138(1):38–44. [DOI] [PubMed] [Google Scholar]
- 21. Patel SS, Truong U, King M, Ferland A, Moreau KL, Dorosz J, Hokanson JE, Wang H, Kinney GL, Maahs DM, Eckel RH, Nadeau KJ, Cree-Green M. Obese adolescents with polycystic ovarian syndrome have elevated cardiovascular disease risk markers. Vasc Med. 2017;22(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wild S, Pierpoint T, McKeigue P, Jacobs H. Cardiovascular disease in women with polycystic ovary syndrome at long-term follow-up: a retrospective cohort study. Clin Endocrinol (Oxf). 2000;52(5):595–600. [DOI] [PubMed] [Google Scholar]
- 23. Maggio M, Basaria S. Welcoming low testosterone as a cardiovascular risk factor. Int J Impot Res. 2009;21:261–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Laughlin GA, Barrett-Connor E, Bergstrom J. Low serum testosterone and mortality in older men. J Clin Endocrinol Metab. 2008;93(1):68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Manson JE, Hsia J, Johnson KC, Rossouw JE, Assaf AR, Lasser NL, Trevisan M, Black HR, Heckbert SR, Detrano R, Strickland OL, Wong ND, Crouse JR, Stein E, Cushman M; Women’s Health Initiative Investigators . Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med. 2003;349(6):523–534. [DOI] [PubMed] [Google Scholar]
- 26. Wassertheil-Smoller S, Hendrix SL, Limacher M, Heiss G, Kooperberg C, Baird A, Kotchen T, Curb JD, Black H, Rossouw JE, Aragaki A, Safford M, Stein E, Laowattana S, Mysiw WJ; WHI Investigators . Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative: a randomized trial. JAMA. 2003;289(20):2673–2684. [DOI] [PubMed] [Google Scholar]