Abstract
Objective
To document variability among caregivers’ priorities when considering medication to treat their child’s attention-deficit/hyperactivity disorder (ADHD) and explore associations between these priorities and medication-related improvements.
Methods
Caregivers of children, ages four to 14-years, diagnosed with ADHD were recruited from outpatient clinics and support groups across Maryland. A survey gathered data on caregiver-reported concerns when considering ADHD medication, demographic characteristics, and observed and desired improvements in their child’s ADHD. A validated best-worst scaling instrument assessed priorities among 16 concerns when considering ADHD medication. Latent class analysis identified subgroups with similar ADHD medication concerns. Differences in self-reported medication-related improvements were examined across subgroups.
Results
The 184 participants (mean=42 years) were primarily the biological mother, 68% white and 25% black. Their children were mostly male (73%) and using medication (81%). Overall, the most important ADHD medication concerns were the child becoming a successful adult (p<.0001), school behavior improvements (p<.0001), and better grades (p<.0001). Others thinking badly of the child was a significantly less important concern (p<.0001). Three subgroups were identified: short-term outcomes-oriented (39%), long-term outcomes-oriented (37%), and side-effects/safety-oriented (27%). Relative to the other two groups, a smaller proportion of the side-effects/safety-oriented group desired these improvements (p<0.2618).
Conclusions
Most caregivers prioritize short- and long-term outcomes when considering ADHD medication. However, those most concerned with long- or short-term outcomes tended to desire additional improvements in their child’s ADHD.
Keywords: Attention-deficit/hyperactivity disorder (ADHD), Children and adolescents, Family-centered care, Best-worst scaling, Stated preferences
The American Academy of Pediatrics (AAP) clinical guidelines for attention-deficit/hyperactivity disorder (ADHD) diagnosis and management emphasize the consideration of family preferences when developing a treatment plan.1 Pediatric providers can face several challenges when attempting to implement these guidelines because the decision to use medication is a difficult process for many families. Most parents of a child diagnosed with ADHD often are hesitant to initiate medication, may consider medication unacceptable,2,3 and often face strong social influences impeding engagement in care.4–9 The perception that individuals in their community do not understand ADHD leads to mixed attitudes among families considering medication as part of an ADHD treatment plan.10–12,13 Those who feel supported by friends, family, and providers more willingly initiate medication.14 These attitudes stem from family influence and social beliefs that stimulants are not safe,6,7 that children will be labeled and stigmatized, and that use will lead to future drug abuse.6,7,15
Pediatric providers serve an important role in guiding parents through the informed consent process when deciding to use ADHD medication for their child. Parents differ considerably in terms of their preferences and concerns with ADHD medication, and they must integrate competing priorities (e.g., “I want to limit any medication exposure to avoid side effects” versus “I want to seek optimal treatment that will help my child do well in school”) to make a final decision about what is best for their child. When considering ADHD medication for their child, parents are weighing social influences to avoid ADHD medication, the likelihood of complete symptom resolution, the unknown long-term effects,16,17 and the potential for serious side effects.18,19 Despite several decades of research on ADHD treatment, the research literature is quite limited in guiding the practicing clinician on how to best identify these competing parental concerns in treatment decision-making for their child. Not all parents weigh the benefits and risks of ADHD treatment similarly,20 and so identifying sub-groups with differing concerns could inform more patient-centered engagement in ADHD treatment.21
The present study aims to document variation in caregivers’ most important concerns when considering medication to treat their child’s ADHD and to explore associations between these priorities and medication-related improvements. The specific focus was on four domains known to influence preferences: 1) short-term medication effects, 2) long-term medication effects, 3) social network support, and 4) stigma/isolation associated with having a child with ADHD. Here the term caregiver is used to represent the parent or other legal guardian.
METHODS
Study Design and Procedures
A cross-sectional computer-facilitated survey elicited the relative importance of concerns that caregivers have when considering ADHD medication for their child. Primary caregivers of children aged four to 14 years old who had received an ADHD diagnosis were recruited between January 2013 and March 2015 from primary care and mental health pediatric outpatient clinics, parent support groups in public schools, and caregiver support organizations throughout [state blinded for review]. Participants provided written consent. Exclusions were made for those with cognitive impairments that would prevent them from completing the survey or if they did not speak English. A brief telephone screen was conducted to determine eligibility and to confirm willingness to participate.
A research assistant scheduled a date and time to meet in person with eligible caregivers in order to review the consent form. To determine comprehension of what they would be asked to do if they joined the study, caregivers were asked to explain the study’s purpose, what was expected of them, and what they could do if they no longer wished to participate in the study. Written consent was obtained only if individuals could answer the aforementioned questions.
The survey was completed in a private location either at the recruiting clinic or a public library. Before starting, the research staff went over the survey instructions. Caregivers completed the survey independently, but the research staff clarified any questions participants might have had. The survey took approximately 45 minutes to complete and caregivers received a $25 gift card as compensation for their time. The [blinded for review] Institutional Review Board (IRB) approved the study protocol.
Survey Instrument
The survey instrument comprised three sections: 1) sociodemographic characteristics of the caregiver and the child as well as the child’s ADHD management; 2) Best-Worst Scaling (BWS) to elicit preferences for ADHD medication; 3) caregiver-reported improvement in their child’s ADHD.
Sociodemographic Information
Caregivers self-reported demographic characteristics of themselves and their child, the child’s ADHD treatment. Caregiver demographic information included their relation to the child, age, gender, race, education, annual household income, insurance type, number of individuals living in the same household, marital status, and occupation. Child demographic and ADHD care management information included the child’s age, gender, years since diagnosed with ADHD, use of stimulant and other psychotropic medications, and receipt of therapy.
Best-Worst Scaling (BWS)
BWS is a stated preference method with origins in marketing research but increasingly used in healthcare research.22,23 We designed a BWS to elicit priorities when considering jointly competing concerns associated with an ADHD medication treatment decision for their child. The merits of BWS have been well documented,22,23 and offer many advantages over traditional Likert type response surveys. For one, Likert scales elicit preferences for one attribute at a time. However, BWS presents the attributes simultaneously, forcing a choice (i.e., trade-offs) among potentially competing concerns. Also, since a choice is made in relation to other attributes, the item scores can be ranked in order of priority. Finally, BWS is more representative of real-life decision-making where individuals often consider many factors when making a decision.
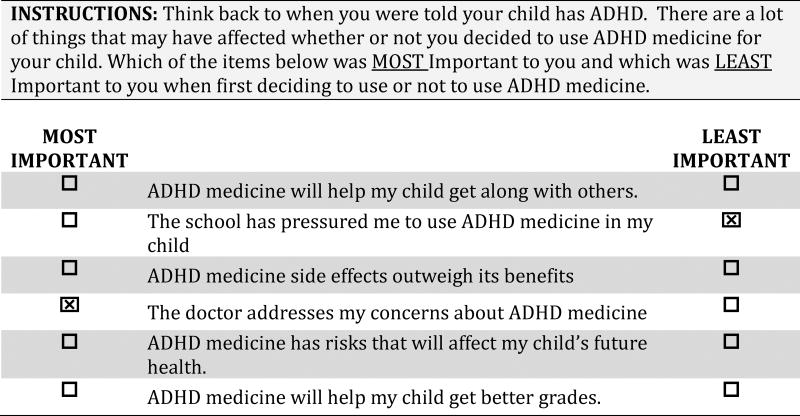
Using a previously validated instrument,24,25 we evaluated preferences for 16 attributes related to the short-term and long-term impact of ADHD medication on their child’s well-being, societal views of using ADHD medication, and the influence of a social network. To reduce cognitive burden, we used a block design where each question (i.e., referred to as a choice task profile) displayed six of the 16 attributes (Figure 1). To ensure a balanced opportunity to select any one attribute, each of the 16 attributes appeared an equal number of times across all 16 choice task profiles. For each choice task profile, respondents selected one attribute that was most important and the one attribute that was least important when considering ADHD medication.
Figure 1.
Example of a Best-Worst Choice-Task
ADHD Improvement
Several questions gathered self-reported observed and desired improvements in the child’s ADHD in an open-ended free text format. Caregivers indicated whether their child’s ADHD improved, was unchanged, or worsened as a result of treatment. Using free-text format, caregivers noted any observed improvements or worsening of symptoms as well as additional changes they desired, if any.
Data Analysis
Caregiver and child demographics and self-reported observed and additional desired improvements in the child’s ADHD were summarized using descriptive statistics. The research team coded free-text descriptions of observed and additional desired improvements into three categories: behavior (e.g., “better control of behavior, better attention, less distracted”), executive functioning (e.g., “better focused, more organized, completes tasks”), and school (e.g., “better grades at school, fewer problems at school”). The categories were not mutually exclusive since a caregiver could have observed or desired improvements in more than one domain.
Data were analyzed using Latent Gold Choice® 5.1 Software to estimate attribute scores. The software uses a hybrid of Expectancy Maximization and Newton-Raphson algorithms.26 Larger estimated scores reflected stronger preference for the attribute. A positive value indicated the attribute was an important influence on decision-making whereas a negative value indicated the attribute was a less important influence on decision-making. The scores can be ranked in order of importance (i.e., priority) to determine which is most important relative to all other attributes.
To assess subgroups differences in preferences, we conducted a latent class analysis. Models were tested with one and up to five classes to identify the model that best fit the data. All models were scale-adjusted for intra-subject variability in responses. Bayesian Information Criterion (BIC) and Akaike Information Criterion (AIC) fit statistics were used to select the best fitting model that generated theoretically interpretable classes. The Z-scores and associated p-values were used to assess the significance of subgroup-specific importance scores (p<0.05).
Bivariate chi-square statistics were used to compare differences in observed and desired outcomes as well as the ADHD treatment the child was currently receiving across latent groups. Analyses were conducted at the 5% significance level.
RESULTS
Demographic Characteristics
A total of 184 caregivers of children aged four to 14 years and in care for ADHD completed the survey, for a 61% response rate. Caregivers were mainly white (68%), black (25%), or Hispanic (6.5%), 40 years old or younger (48%), the child’s biological mother (84%), married (64%), and completed at least some college education (74%). Most children were male (71%), had been diagnosed within the past four years (56%), and were taking at least one ADHD medication (81%) at the time of the survey. Children were, on average, 9.5 (± 2.5) years old.
Attribute Importance
Table 1 presents the rank order attribute scores for the aggregate sample. Most important concerns when deciding to use ADHD medication for their child was the child becoming a successful adult (m=1.83, SE=0.09), the medication helping the child’s behavior in school (m=1.57, SE=0.08), and the medication helping the child’s grades (m=1.48, SE=0.08). The influence of societal views and of their supportive network had large negative mean scores, suggesting that were less important concerns in ADHD medication treatment decisions.
Table 1.
Caregiver and Child Characteristics, Overall and Stratified by Preference Group
| Overall Sample (N=184) N(%) |
Short-Term Outcomes- Oriented (n=72) N(%) |
Long-Term Outcomes- Oriented (n=68) N(%) |
Side Effects/ Safety-Oriented (n=44) N(%) |
p | ||
|---|---|---|---|---|---|---|
| Race | White | 125 (67.9) | 50 (69.4) | 43 (63.2) | 32 (72.7) | 0.6287 |
| Black | 46 (25.0) | 17 (23.6) | 21 (30.9) | 8 (17.4) | ||
| Hispanic | 12 (6.5) | 4 (5.6) | 4 (5.9) | 4 (9.1) | ||
| Other | 1 (0.5) | 1 (1.4) | 0 (0.0) | 0 (0.0) | ||
| Age | 27–40 | 88 (47.8) | 35 (48.6) | 35 (51.5) | 18 (40.9) | 0.1443 |
| 41–50 | 73 (39.7) | 26 (31.1) | 23 (33.8) | 24 (54.6) | ||
| 51–70 | 23 (12.5) | 11 (15.3) | 10 (14.7) | 2 (5.6) | ||
| Relationship to Child | Mother | 155 (84.2) | 62 (86.1) | 54 (79.4) | 39 (88.6) | 0.6135 |
| Father | 8 (4.4) | 3 (4.2) | 3 (4.4) | 2 (4.6) | ||
| Other | 21 (11.4) | 7 (9.7) | 11 (16.2) | 3 (6.8) | ||
| Marital Status | Married | 119 (64.7) | 46 (63.9) | 44 (64.7) | 29 (65.9) | 0.4029 |
| Divorced/Widowed | 37 (20.1) | 18 (25.0) | 10 (14.7) | 9 (20.5) | ||
| Never Married | 23 (15.2) | 8 (11.1) | 14 (20.6) | 6 (13.6) | ||
| Education | ≤High School | 44 (23.9) | 14 (19.4) | 20 (29.4) | 10 (22.7) | 0.5651 |
| College | 80 (43.5) | 35 (48.6) | 28 (41.2) | 17 (38.6) | ||
| Postgraduate | 60 (32.6) | 23 (31.9) | 20 (29.4) | 17 (38.6) | ||
| Annual Household | ≤$25,000 | 32 (17.4) | 12 (16.7) | 13 (19.1) | 7 (15.9) | 0.8622 |
| Income | $26,000–$50,000 | 36 (19.6) | 13 (18.1) | 15 (22.1) | 8 (18.2) | |
| $51,000–$75,000 | 32 (17.4) | 15 (20.8) | 8 (11.8) | 9 (20.5) | ||
| ≥$75,000 | 84 (45.7) | 32 (44.4) | 32 (47.1) | 20 (45.5) | ||
| Type of Insurance | Private | 101 (54.9) | 42 (58.3) | 29 (42.7) | 30 (68.2) | 0.0224* |
| Public | 83 (45.1) | 30 (41.7) | 39 (57.4) | 14 (31.8) | ||
| Child’s Age | <10 | 92 (50.5) | 27 (37.5) | 39 (58.2) | 26 (60.5) | 0.0168* |
| 10+ | 90 (49.5) | 45 (62.5) | 28 (41.8) | 17 (39.5) | ||
| Child’s | Male | 130 (70.7) | 51 (70.8) | 47 (69.1) | 32 (72.7) | 0.5534 |
| Female | 48 (26.0) | 19 (26.4) | 17 (25.0) | 12 (27.3) | ||
| Missing | 6 (3.3) | 2 (2.8) | 4 (5.9) | 0 (0.0) | ||
| Current Use of ADHD | Yes | 149 (81.0) | 64 (88.9) | 60 (88.2) | 25 (56.8) | <0.0001* |
| Medication | No | 35 (19.0) | 8 (11.1) | 8 (11.8) | 19 (43.2) | |
| Stimulant Medication | Yes | 133 (75.0) | 58 (80.6) | 56 (82.3) | 24 (55.6) | 0.0015* |
| No | 46 (25.0) | 14 (19.4) | 12 (17.7) | 20 (45.4) | ||
| Years Since ADHD Diagnosis | Mean (SE) | 3.7 (0.19) | 4.1 (0.35) | 3.6 (0.30) | 3.2 (0.31) | 0.2096 |
Statistically significant (p<0.05)
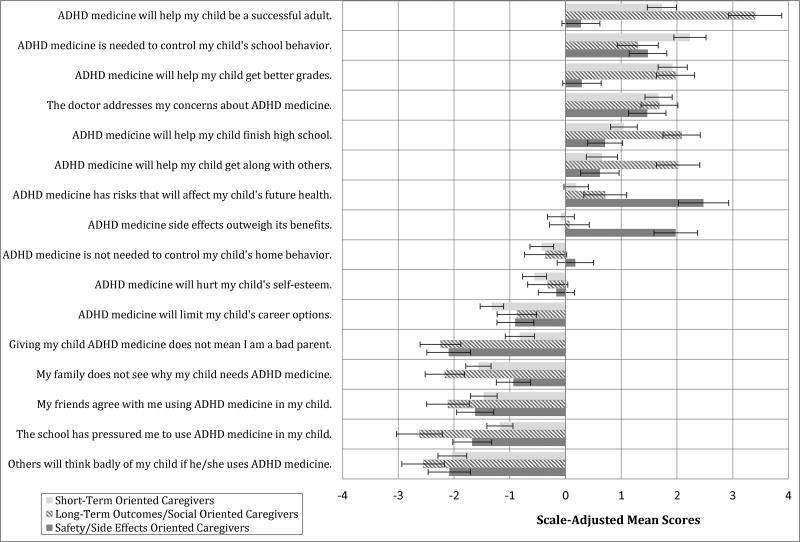
Preference Subgroups
A scale-adjusted three-class solution was the best fitting model. The latent classes were: short-term outcomes-oriented (n= 72; 39%), long-term outcomes-oriented (n=68; 37%), and side-effects/safety-oriented (n=44; 24%). Subgroup-specific attribute scores and 95% confidence intervals are displayed in Figure 2. The short-term outcomes-oriented group prioritized medicine improving the child’s school behavior (m=2.23, SE=0.17) and getting better grades (m=1.92, SE=0.11; Table 1). The long-term outcomes-oriented group prioritized ADHD medicine helping the child to become a successful adult (m=3.4, SE=0.24) and finishing high school (m=2.08, SE=0.17). The side effects/safety-oriented group prioritized the effect of ADHD medicine on the child's future health (m=2.47, SE=0.23) and the medication side effects outweighing its benefits (m=1.98, SE=0.20).
Figure 2.
Caregivers’ Scale-Adjusted Mean Scores by each Preference Subgroup
 Short-term Oriented Caregivers
Short-term Oriented Caregivers
 Long-term Outcome Caregivers
Long-term Outcome Caregivers
 Safety/Side Effects Oriented Caregivers
Safety/Side Effects Oriented Caregivers
Factors that were least important also differed across the groups. Concerns about others thinking badly of the child using ADHD medication (m=−2.03, SE=0.13) were least important to the short-term outcome-oriented group when deciding to use ADHD medication. Concerns about school pressure to medicate their child, (m=−2.62, SE=0.21) were least concerning for the long-term outcomes-oriented group. Concerns about being viewed by others as a bad parent (m=−2.10, SE=0.20) or others thinking badly of their child (m=−2.09, SE=0.19) were least influential to the side-effects/safety-oriented group.
Many of the demographic characteristics were not statistically significantly different across preference subgroups (Table 2). Caregivers in the long-term outcomes-oriented group were more likely to have public insurance compared to the other two groups (χ2=7.6, p=0.0224). Children of caregivers in the short-term outcomes-oriented group were more likely to be aged 10 or older whereas children of caregivers in the other two subgroups were more likely to be younger than 10 years old (χ2=8.17, p=0.0168). A smaller proportion of side-effects/safety-oriented caregivers (58%) reported using ADHD medication for their child compared with the short- (89%) or long-term (88%) outcomes-oriented caregivers (χ2=19.9, p<0.0001).
Table 2.
Scale-Adjusted Mean Scores (SE) Overall and Stratified by Preference Subgroup
| Latent Class Preference Groups | ||||
|---|---|---|---|---|
|
|
||||
| Attribute Statement (ranked by aggregate mean score) | Overall Sample of Caregivers (N=184) |
Short-Term Outcomes- Oriented (n=72) |
Long-Term Outcomes- Oriented (n=68) |
Side-Effects/ Safety- Oriented (n=44) |
| ADHD medicine will help my child be a successful adult. | 1.83 (0.09) | 1.73 (0.13) | 3.40 (0.24) | 0.28 (0.17) * |
| ADHD medicine is needed to control my child's school behavior. | 1.57 (0.08) | 2.23 (0.15) | 1.30 (0.19) | 1.48 (0.17) |
| ADHD medicine will help my child get better grades. | 1.48 (0.08) | 1.92 (0.13) | 1.97 (0.17) | 0.29 (0.18) * |
| The doctor addresses my concerns about ADHD medicine. | 1.41 (0.08) | 1.67 (0.12) | 1.69 (0.17) | 1.47 (0.17) |
| ADHD medicine will help my child finish high school. | 1.26 (0.07) | 1.05 (0.12) | 2.08 (0.17) | 0.71 (0.16) |
| ADHD medicine will help my child get along with others. | 1.02 (0.08) | 0.65 (0.14) | 2.02 (0.20) | 0.62 (0.18) |
| ADHD medicine has risks that will affect my child's future health. | 0.84 (0.07) | 0.19 (0.11) * | 0.71 (0.20) | 2.47 (0.23) |
| ADHD medicine side effects outweigh its benefits. | 0.48 (0.08) | −0.08 (0.12) * | 0.07 (0.18) * | 1.98 (0.20) |
| ADHD medicine is not needed to control my child's home behavior. | −0.28 (0.07) | −0.43 (0.11) | −0.36 (0.19) * | 0.18 (0.17) * |
| ADHD medicine will hurt my child's self-esteem. | −0.42 (0.07) | −0.56 (0.11) | −0.32 (0.18) * | −0.16 (0.17) * |
| ADHD medicine will limit my child's career options. | −1.05 (0.07) | −1.32 (0.11) | −0.87 (0.18) | −0.90 (0.17) |
| Giving my child ADHD medicine does not mean I am a bad parent. | −1.46 (0.08) | −0.82 (0.13) | −2.24 (0.19) | −2.10 (0.20) |
| My family does not see why my child needs ADHD medicine. | −1.51 (0.08) | −1.56 (0.12) | −2.17 (0.18) | −0.93 (0.16) |
| My friends agree with me using ADHD medicine in my child. | −1.56 (0.08) | −1.47 (0.12) | −2.11 (0.20) | −1.62 (0.17) |
| The school has pressured me to use ADHD medicine in my child. | −1.63 (0.08) | −1.18 (0.12) | −2.62 (0.21) | −1.67 (0.18) |
| Others will think badly of my child if he/she uses ADHD medicine. | −1.98 (0.09) | −2.03 (0.13) | −2.55 (0.19) | −2.09 (0.19) |
Not statistically significant (p>0.05)
Bolded mean scores indicate the three most strongly important considerations to caregivers in each latent group.
Underlined mean scores indicate the three most strongly least important considerations to caregivers in each latent group.
Observed Improvements and Additional Desired Improvements in ADHD
Among the caregivers who used ADHD medication in their child, 134 (89%) noticed an improvement in their child’s ADHD, 13 (8%) felt as though their child’s ADHD had remained the same, and 4 (3%) reported a worsening of their child’s ADHD symptoms. Based on the free-text responses of observed improvements in the child’s ADHD, 36% noted behavioral improvements (e.g., “a noticeable decrease in impulsivity and aggression”), 44% noted executive functioning improvements (e.g., “a distinct difference in her ability to concentrate”), and 13% noted school improvements (e.g., “better school grades and focus”).
When asked whether they desired additional improvements in their child’s ADHD, nearly one-third of the caregivers who had noted improvements, still reported seeking additional improvements. In particular, a large proportion of those who had seen either behavioral or executive functioning improvements, desired further improvements in these areas. Thirty-four percent of 68 caregivers who observed a behavioral improvement in their child desired additional behavioral improvements. Among 81 caregivers who observed executive functioning improvements, 28% desired additional improvement in their child’s executive functioning. Only 8% of 24 caregivers who observed improvement in school were still seeking additional improvement in school performance.
Caregiver report of additional desired changes in their child’s ADHD differed significantly between those who used and those who did not use ADHD medication for their child. More than half (59%) of caregivers who had a child using ADHD medication desired additional improvements in their child’s ADHD, compared to 18% of caregivers whose child did not use ADHD medication (χ2=19.4, p<0.0001). Further, a smaller proportion of the side-effects/safety-oriented group (41%) reported that they would like to see additional improvements in their child’s ADHD when compared with the long-term outcomes-oriented group (54%) and short-term outcomes-oriented group (56%), however this did not reach statistical significance (χ2=2.7, p<0.2618).
DISCUSSION
Although a number of studies have examined caregivers’ concerns with ADHD medication, this study elicited trade-offs among different social and contextual issues influencing concerns with ADHD medication. The issues examined in this study are not necessarily specific to ADHD as caregivers of children with other developmental and behavioral pediatric conditions are often faced with decisions related to the safety of medications, stigma, and social support.25 Stigma and social network support can be barriers to engagement in pediatric ADHD treatment.10–12 The present study found that when assessing these factors in relation to other concerns, caregivers prioritized short- and long-term medication effects over stigma and social network influences. It also was notable that despite known sociodemographic differences in willingness to engage in ADHD treatment,27 these characteristics were not significantly different across preference subgroups in the present study. This suggests that sociodemographic characteristics may not adequately distinguish the relative importance of contextual factors underlying treatment decisions. The findings offer recommendations for the management of ADHD.
A doctor addressing the caregivers’ concerns was highly valued by this caregiver sample when considering ADHD medication for their child. A family-centered approach that considers caregivers’ goals and priorities when developing care plans is vital11,28 and the importance of the provider-patient relationship and shared decision-making is documented in the literature.28–30 Understanding caregivers’ priorities for short- and long-term outcomes, stigma concerns, and ADHD medication side effects could guide initial ADHD treatment planning, ongoing monitoring, and managing social influences that can impede the delivery of evidence-based care.
Involving families in their child’s care is among the AAP clinical recommendations,1 and the present study suggests that managing expectations for treatment outcomes over the course of care may be important for engagement in care. Among those who observed improvements in their child’s ADHD, a large portion was still hoping for additional improvements. Compared with caregivers that prioritized the long and short-term treatment outcomes, fewer of those concerned primarily with the safety and side effects of ADHD medication reported seeking additional improvements in their child’s ADHD. Understanding caregiver priorities for treatment outcomes may help clinicians to gauge perceptions of their child’s ADHD improvement and caregiver engagement in treatment. Further research is warranted to determine whether caregivers who are seeking additional improvements over what already has been observed and those who are most concerned with the risks of ADHD medication are more likely to disengage from treatment, which is a commonly reported issue in pediatric mental health.31,32 Managing these expectations with caregivers may facilitate continued engagement in ADHD treatment.
The study is limited in several ways. One potential limitation is that all participants were recruited from one geographical area and the results may not be generalizable to all caregivers of children with ADHD. Additionally, despite efforts to recruit a diverse sample of participants by partnering with family support groups for low-income families, and pediatric clinics that serve underserved families, the majority of the sample had more than a high school diploma and a high income, which may limit the generalizability of the results. Furthermore, all participants had a child with a clinician-assigned diagnosis of ADHD. It is possible that the sample of caregivers of a child already in care for ADHD had overcome some of the contextual and stigma-related barriers to engaging in care. This would explain the lower emphasis on these attributes relative to the outcome-oriented attributes. Caregivers’ positive and negative experiences with medications the child or the caregivers’ other children have taken previously could impact their views on and preferences ADHD treatments and their propensity to start or continue medications. It is also possible that the child’s comorbid conditions and past academic history, including past grade retention, suspensions, and expulsions could influence ADHD treatment preferences, particularly school-related factors. Similarly, it is possible that caregivers’ experiences with managing ADHD and with interactions with the child’s school influenced their responses. Although the scale-adjusted analysis accounted for potential response bias, it was not possible to control for severity of the child’s ADHD, which also may have affected caregivers’ priorities for treatment. Future studies should examine the contextual issues, such as past experience with ADHD medications, past school suspensions, and impending school expulsions influence caregivers’ preferences compared to those who are not facing such contextual issues.
Despite the aforementioned limitations, there are several strengths worthy of mention. This study fills a gap in the existing literature on preference elicitation for ADHD treatment by simultaneously accounting for the social context influencing care management decisions. The priority ranking of preferences obtained from the BWS also is an important and novel contribution. Using a discrete choice experiment design, which like the BWS forces a choice among competing alternatives, Cunningham and colleagues identified three subgroups with different information needs for the management of child mental health problems.33 By comparison, a recently published study using a Likert response survey to assess the information preferences of caregivers in deciding upon treatment for their child’s anxiety reported little variability in attribute importance that could guide clinical practice, i.e., nearly every attribute was rated important.34 In this case, attributes considered independently cannot be priority ranked because respondents were not asked to consider the importance of one attribute over the other when answering the question. Additionally, the findings from the present study offer some preliminary evidence for the correlation between stated preferences and actual behaviors regarding treatment engagement. Ideally this would have clinical practice relevance by guiding treatment plans towards the outcomes most important to caregivers. Finally, the preference elicitation methods used in the present study provide a unique opportunity to investigate the medical and social issues that often are competing alternatives in real-world healthcare decision-making.
Conclusion
This study is important as the field is increasingly examining multi-attribute facets of health and healthcare decision-making.35–37 These methods highlight the relative importance of competing alternatives in healthcare decision-making, and thus are of value to a range of stakeholders, including policymakers, insurers, physicians, and patients, who must prioritize healthcare resources in an environment of limited funding. Furthermore, acknowledging early in the encounter the heterogeneity of preferences and how these may be correlated with treatment expectations could assist clinicians in developing family-centered treatment plans. The field of stated preference research in health-related areas has expanded tremendously in the past 10 years. The potential to link preferences for health care decisions with clinical data on impairment and severity is on the horizon as data linkages with electronic health records increases.
Acknowledgments
Funding: This work was supported by a grant from the National Institute of Mental Health [R34 MH093502; PI: dosReis].
Footnotes
Conflicts of Interest: The authors have no conflict of interest to declare.
References
- 1.Wolraich M, Brown L, Brown RT, et al. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011 Nov;128(5):1007–1022. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.dosReis S, Mychailyszyn MP, Evans-Lacko SE, et al. The meaning of ADHD medication and parents’ initiation and continuity of treatment for their child. Journal of Child and Adolescent Psychopharmacology. 2009;19(4):377–383. doi: 10.1089/cap.2008.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leslie LK, Aarons GA, Haine RA, et al. Caregiver depression and medication use by youths with ADHD who receive services in the public sector. Psychiatric Services. 2007 Jan;58(1):131–134. doi: 10.1176/ps.2007.58.1.131. [DOI] [PubMed] [Google Scholar]
- 4.Charach A, Ickowicz A, Schachar R. Stimulant treatment over five years: adherence, effectiveness, and adverse effects. Journal of the American Academy of Child Adolescent Psychiatry. 2004;43(5):559–567. doi: 10.1097/00004583-200405000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Marcus SC, Wan GJ, Kemner JE, et al. Continuity of methylphenidate treatment for attention-deficit/hyperactivity disorder. Archives of Pediatrics and Adolescent Medicine. 2005;159:572–578. doi: 10.1001/archpedi.159.6.572. [DOI] [PubMed] [Google Scholar]
- 6.dosReis S, Butz A, Lipkin P, et al. Attitudes About Stimulant Medication for Attention-Deficit/Hyperactivity Disorder Among African-American Families in an Inner City Community. Journal of Behavioral Health Services & Research. 2006;33(4):423–430. doi: 10.1007/s11414-006-9038-y. [DOI] [PubMed] [Google Scholar]
- 7.dosReis S, Zito JM, Safer DJ, et al. Parental perceptions and satisfaction with stimulant medication for attention-deficit/hyperactivity disorder. Journal of Developmental and Behavioral Pediatrics. 2003;24(3):155–162. doi: 10.1097/00004703-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Schnittker J, Freese J, Powell B. Nature, nurture, neither, nor: Black-white differences in beliefs about the causes and appropriate treatment of mental illness. Social Forces. 2000;78(3):1101–1132. [Google Scholar]
- 9.Croghan TW, Tomlin M, Pescosolido BA, et al. American attitudes toward and willingness to use psychiatric medications. Journal of Nervous and Mental Disease. 2003;191(4):166–174. doi: 10.1097/01.NMD.0000054933.52571.CA. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed R, McCaffery KJ, Aslani P. Factors influencing parental decision making about stimulant treatment for attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2013 Apr;23(3):163–178. doi: 10.1089/cap.2012.0087. [DOI] [PubMed] [Google Scholar]
- 11.Coletti DJ, Pappadopulos E, Katsiotas NJ, et al. Parent perspectives on the decision to initiate medication treatment of attention-deficit/hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology. 2012 Jun;22(3):226–237. doi: 10.1089/cap.2011.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.dosReis S, Barksdale CL, Sherman A, et al. Stigmatizing Experiences of Parents of Children Newly Diagnosed with ADHD. Psychiatric Services. 2010;61(8):811–816. doi: 10.1176/ps.2010.61.8.811. [DOI] [PubMed] [Google Scholar]
- 13.Charach A, Skyba A, Cook L, et al. Using stimulant medication for children with ADHD: what do parents say? A brief report. J Can Acad Child Adolesc Psychiatry. 2006;15:75–83. [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmed R, Borst J, Wei YC, et al. Parents' Perspectives About Factors Influencing Adherence to Pharmacotherapy for ADHD. Journal Attention Disorders. 2013 Aug 30; doi: 10.1177/1087054713499231. [DOI] [PubMed] [Google Scholar]
- 15.Pescosolido BA, Perry BL, Martin JK, et al. Stigmatizing attitudes and beliefs about treatment and psychiatric medications for children with mental illness. Psychiatric Services. 2007 May;58(5):613–618. doi: 10.1176/ps.2007.58.5.613. [DOI] [PubMed] [Google Scholar]
- 16.The MTA Cooperative Group. National Institute of Mental Health multimodal treatment study of ADHD follow-up: 24-Month outcomes of treatment strategies for attention-deficit/hyperactivity disorder. Pediatrics. 2004;113(4):754–761. doi: 10.1542/peds.113.4.754. [DOI] [PubMed] [Google Scholar]
- 17.The MTA Cooperative Group. National Institute of Mental Health multimodal treatment study of ADHD follow-up: Changes in effectiveness and growth after the end of treatment. Pediatrics. 2004;113(4):762–769. doi: 10.1542/peds.113.4.762. [DOI] [PubMed] [Google Scholar]
- 18.Zito JM, Burcu M. Stimulants and Pediatric Cardiovascular Risk: A Review. J Child Adolesc Psychopharmacol. 2016 Jun 3; doi: 10.1089/cap.2015.0239. [DOI] [PubMed] [Google Scholar]
- 19.Riddle MA, Geller B, Ryan N. Another sudden death in a child treated with desipramine. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(4):792–797. doi: 10.1097/00004583-199307000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Ross CK, Steward CA, Sinacore JM. The importance of patient preferences in the measurement of health care satisfaction. Medical Care. 1993 Dec;31(12):1138–1149. doi: 10.1097/00005650-199312000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Miller CL, Druss BG, Rohrbaugh RM. Using qualitative methods to distill the active ingredients of a multifaceted intervention. Psychiatric Services. 2003 Apr;54(4):568–571. doi: 10.1176/appi.ps.54.4.568. [DOI] [PubMed] [Google Scholar]
- 22.Flynn T, Marley AAJ. Best-worst scaling: Theory and methods. In: Hess S, Daly A, editors. Handbook of Choice Modelling. Northhampton, MA: Edward Elgar Publishing, Inc.; 2014. [Google Scholar]
- 23.Louviere JJ, Flynn TN. Using best-worst scaling choice experiments to measure public perceptions and preferences for healthcare reform in australia. Patient. 2010 Dec 1;3(4):275–283. doi: 10.2165/11539660-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 24.Ross M, Bridges JF, Ng X, et al. A best-worst scaling experiment to prioritize caregiver concerns about ADHD medication for children. Psychiatric Services. 2015 Feb 1;66(2):208–211. doi: 10.1176/appi.ps.201300525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.dosReis S, Castillo WC, Ross M, et al. Attribute Development Using Continuous Stakeholder Engagement to Prioritize Treatment Decisions: A Framework for Patient-Centered Research. Value in Health. 2016 Sep-Oct;19(6):758–766. doi: 10.1016/j.jval.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 26.Vermunt JK, Magidson J. Technical Guide for Latent GOLD 4.0: Basic and advanced. Belmont, MA: 2005. [Google Scholar]
- 27.Waschbusch DA, Cunningham CE, Pelham WE, et al. A discrete choice conjoint experiment to evaluate parent preferences for treatment of young, medication naive children with ADHD. Journal of Clinical Child & Adolescent Psychology. 2011;40(4):546–561. doi: 10.1080/15374416.2011.581617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Davis CC, Claudius M, Palinkas LA, et al. Putting families in the center: family perspectives on decision making and ADHD and implications for ADHD care. J Atten Disord. 2012 Nov;16(8):675–684. doi: 10.1177/1087054711413077. [DOI] [PubMed] [Google Scholar]
- 29.Brinkman WB, Hartl Majcher J, Poling LM, et al. Shared decision-making to improve attention-deficit hyperactivity disorder care. Patient Educ Couns. 2013 Oct;93(1):95–101. doi: 10.1016/j.pec.2013.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fiks AG, Hughes CC, Gafen A, et al. Contrasting parents' and pediatricians' perspectives on shared decision-making in ADHD. Pediatrics. 2011 Jan;127(1):e188–196. doi: 10.1542/peds.2010-1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Horwitz S, Demeter C, Hayden M, et al. Parents' perceptions of benefit of children's mental health treatment and continued use of services. Psychiatric Services. 2012 Aug;63(8):793–801. doi: 10.1176/appi.ps.201100460a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kazdin AE, Holland L, Crowley M. Family experience of barriers to treatment and premature termination from child therapy. J Consult Clin Psychol. 1997 Jun;65(3):453–463. doi: 10.1037//0022-006x.65.3.453. [DOI] [PubMed] [Google Scholar]
- 33.Cunningham C, Deal K, Rimas H, et al. Modeling the Information Preferences of Parents and Children with Mental Health Problems: A Discrete Choice Conjoint Experiment. Journal of Abnormal Child Psychology. 2008;36:1123–1138. doi: 10.1007/s10802-008-9238-4. [DOI] [PubMed] [Google Scholar]
- 34.Mak L, Walker JR, Hiebert-Murphy D, et al. Information Needs and Preferences of Parents Considering Treatment of Child Anxiety. Journal of Developmental and Behavioral Pediatrics. 2017 Apr;38(3):173–180. doi: 10.1097/DBP.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 35.Muhlbacher AC, Kaczynski A, Zweifel P, et al. Experimental measurement of preferences in health and healthcare using best-worst scaling: an overview. Health Economics Review. 2016 Dec;6(1):14. doi: 10.1186/s13561-015-0079-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schatz NK, Fabiano GA, Cunningham CE, et al. Systematic Review of Patients' and Parents' Preferences for ADHD Treatment Options and Processes of Care. Patient. 2015;8:483–497. doi: 10.1007/s40271-015-0112-5. [DOI] [PubMed] [Google Scholar]
- 37.Cheung KL, Wijnen BF, Hollin IL, et al. Using Best-Worst Scaling to Investigate Preferences in Health Care. PharmacoEconomics. 2016 Jul 11; doi: 10.1007/s40273-016-0429-5. Online Access:15. [DOI] [PMC free article] [PubMed] [Google Scholar]