Abstract
Objective
This study was designed to compare the effects of catheter drainage alone and combined with ozone in the management of multiloculated pyogenic liver abscess (PLA).
Methods
The prospective study included 60 patients diagnosed with multiloculated PLA. All patients were randomly divided into two groups: catheter drainage alone (group I) and catheter drainage combined with ozone (group II). Drainage was considered successful when (1) the abscess cavity was drained and (2) clinical symptoms were resolved. Kruskal-Wallis nonparametric test was used to compare the success rates, length of stay (LOS), and need for further surgery of the two groups. P < 0.05 indicates significant difference.
Results
All patients' catheters were successfully placed under CT guidance. Group I was treated with catheters alone and group II was treated with catheters and ozone. The success rates of groups I and II were 86% and 96%, respectively (P < 0.05). And compared with group II, the duration of fever in group I was longer (P < 0.05), and the LOS was also longer (P < 0.05).
Conclusion
Catheter drainage combined with ozone is an effective and safe treatment in multiloculated PLA. The Clinical Registration Number is ChiCTR1800014865.
1. Introduction
Therapy of pyogenic liver abscess (PLA) includes antibiotics alone or in combination with percutaneous or surgical drainage [1, 2]. A number of studies have shown that percutaneous abscess drainage is effective and safe, and it is minimally invasive and does not require general anesthesia [3]. However, the optimal treatment of multiloculated abscesses is still a subject of debate, as the multiloculated PLA often contain viscid pus, or small locules of the abscesses cannot communicate with each other, which may make percutaneous drainage difficult [3–6].
Multiloculated liver abscess was defined as an abscess with enhancing internal septations [7]. Studies have been showed that the presence of multiloculated abscess lesions has been considered as one of the factors that increase the risk of percutaneous catheter drainage failure [7, 8]. And these literatures showed that the mortality rates for multiloculated pyogenic liver abscesses range from 44% to 22.1%, which was higher than single PLA [8, 9]. In addition, multiloculated PLA may need multiple percutaneous drains or surgical intervention in an attempt to achieve source control and hence some authors advocate surgical intervention [10]. Moreover, some patients with multiloculated PLA have various infections, where using antibiotics alone often has a poor effect [11]. Long-term use of antibiotics, in addition, can cause bacteria resistance [6].
Ozone can inactivate bacteria, viruses, yeasts, protozoa, and fungi and stimulate the immune system and oxygen metabolism, so ozone has been widely considered to be one of the best sterilization, antifungal, and antiviral agents [12]. For some chronic wounds, such as nutrition ulcers, ischemic ulcers, and diabetic wounds, ozone has also been empirically used as clinical therapeutic agent [13–15].
In order to improve the therapeutic effect of multiloculated PLA, this study intends to compare catheter drainage alone and its combination with ozone therapy in the treatment of multiloculated PLA.
2. Materials and Methods
This prospective study was approved by our Hospital Institutional Review Board (HIRB), which included 60 patients who were diagnosed with multiloculated PLA (32 males and 28 females, aged 37–71 years; median age of 47.4 years) between January 2014 and October 2017. All patients had given written consent for this study. Diagnosis of the pyogenic abscess was proved by aspiration or microbiologic findings in all patients. Patients with cancer or diabetes were excluded from this study.
Inclusion criteria were as follows:
(1) Multiloculated PLA more than 5 cm in size
(2) Multiloculated PLA in mature stage (a capsule was formed around the necrotic cavity)
Exclusion criteria were as follows:
(1) Multiple abscesses
(2) Abscess ruptured into thoracic and peritoneal cavity
All patients have been uniformly managed with antibiotics throughout the study period, usually a combination of a third-generation cephalosporin along with metronidazole. Subsequently antibiotic therapy is tailored according to culture and sensitivity results of blood or pus.
Patients were randomly allocated into two groups with the help of a computer-generated table of random numbers: catheter drainage alone (group I) and catheter drainage combined with ozone (group II). Contrast-enhanced CT scans were performed in all patients to determine the size, location, and extent of the lesion and choose transhepatic route to avoid injuring other organs, blood vessel, and biliary systems. All catheters were placed by CT guidance, performed under local anesthesia. 10F pigtail catheters were placed into the patients by using the Seldinger technique. Attention should be taken to ensuring the side holes of catheter were placed within the abscess cavity. In this way, we avoid secondary liver infection. Abdominal CT images were obtained immediately after abscess drainage to assess the catheter location, abscess cavity, and complications such as bleeding. Then the valve of catheter was unclamped for open drainage.
In group II, in addition to drainage, according to the size of the abscess cavity, 10.0–20.0 mL oxygen-ozone gas mixture (ozone concentration 25 μg/ml, based on our previous experiments [12]) was given through catheter, until the amount of drainage was less than 20 mL per day. We used an ozone generator (Herrmann, Kleinwallstadt, Germany) to produce oxygen-ozone gas mixtures prior to injection. After oxygen-ozone gas mixture injection, the catheter was clamped for one hour and then left unclamped for 23 hours to allow for open drainage.
The drainage was considered successful when clinical symptoms of patients were resolved and the abscess cavities were drained. And the patients were referred for further surgical treatment when (1) the abscess failed to resolve, (2) the follow-up imaging (ultrasound or CT) showed that the abscess wall becomes thicker and cannot be aspirated, or (3) the patients have ongoing sepsis after drainage.
We evaluated the patient characteristics differences between the two groups and the technical success of catheter placement, as well as the length of hospital stay (LOS). Clinical details such as patients with ongoing sepsis, duration of fever (morning oral temperature of >37.5°C), and patients who converted into further surgery treatment were also written down.
We used SPSS software (version 20.0; SPSS Corporation, New York, USA) for statistical analyses of the two groups. The mean and standard deviation (SD) of each variable from two groups were calculated. Kruskal-Wallis nonparametric test was used to calculate statistical differences between two groups, with a P value of less than 0.05 considered significant. And the descriptive statistical analysis was calculated too.
3. Results
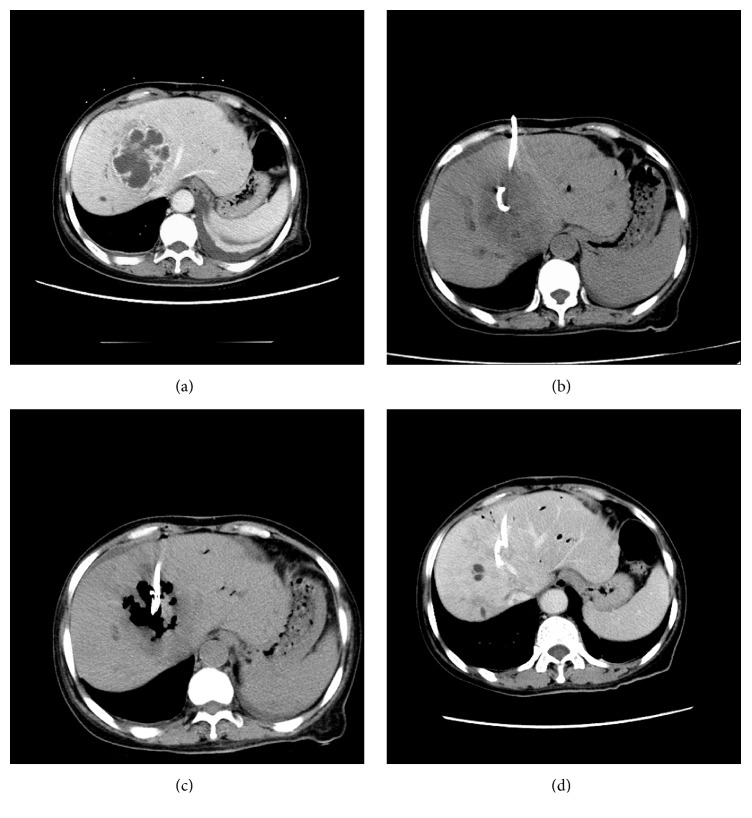
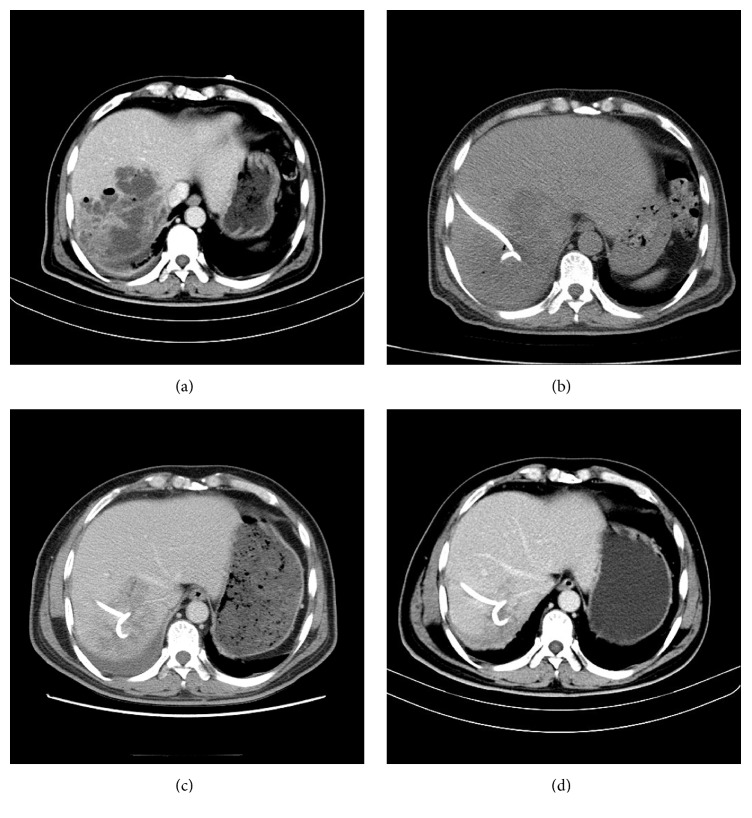
All of the 60 patients' catheters were successfully placed under CT guidance. Group I was treated with catheters alone (Figure 1) and group II was treated with catheters and ozone (Figure 2). Different variables of the two groups are all shown in Table 1. Mean age, abscess sizes, and number of two groups were not significantly different (P = 0.437; P = 0.471; Table 1). Among the 60 patients, bacteriologic study of cultures had positive findings in 100% of patients; some patients have mixed infection (Table 2). The remaining abscesses were diagnosed based on increased white blood cell count in the aspirated fluid but had negative findings on culture. Streptococcus species were the main bacteria isolated, followed by Enterococcus species, Escherichia coli, and Klebsiella species.
Figure 1.
A 49-year-old male presented with fever and right back pain for one week. (a) A lager multiloculated liver abscess in the right hepatic lobes was shown by enhanced CT, and small amount of fluid can be seen in the left chest. (b) Catheter was placed under CT guidance, without injection of oxygen-ozone gas. (c) Three-week follow-up showing that abscess was not fully absorbed. (d) Abscess was fully absorbed after eight weeks.
Figure 2.
A 43-year-old male presented with fever and right abdominal pain for five days. (a) Enhanced CT shows a lager multiloculated liver abscess in the right hepatic lobe. The abscess cavity has gas formation, which is associated with mortality. (b) Catheter was placed under CT guidance. (c) After the pus was pulled out, oxygen-ozone gas mixture was given through catheter and filled the small locules of the abscesses; some separation was broken. (d) Abscess was absorbed after three weeks.
Table 1.
Comparison of preadmission variables among treatment groups.
| Variable, mean (SD) | Group I | Group II |
|---|---|---|
| Number of patients | 30 | 30 |
| Average age (yr) | 41.4 (10.4) | 38.2 (13.6) |
| Duration of symptoms (d) | 14.5 (8.9) | 14.3 (7.9) |
| Initial WBC (×103) | 14.9 (9.4) | 15.4 (9.2) |
| Total lymphocytes (×103) | 11.4 (6.7) | 10.9 (6.9) |
| Abscess size (cm) | 6.8 (2.6) | 6.7 (2.5) |
| Catheter size (Fr) | 10 | 10 |
Table 2.
Positive results of bacterial culture among treatment groups.
| Variable, mean | Group I | Group II |
|---|---|---|
| Bacterial culture | 17 | 16 |
| Streptococcus species | 7 | 6 |
| Enterococcus species | 5 | 6 |
| Escherichia coli | 4 | 4 |
| Klebsiella species | 3 | 2 |
Initial white blood cell count (WBC), lymphocytes, and duration of symptoms were different in two groups but were not significant (P > 0.05). Success rates of groups I and II were 86% and 96%, respectively. And compared with group II, the duration of fever in group I was longer (P < 0.05), and the LOS was also longer (P < 0.05). Furthermore, there were significant differences when comparing patients who converted into further surgery between the two groups (14% versus 4%; P < 0.05) (Table 3). Complications included three patients with minimal perihepatic bleeding. No other complications were founded.
Table 3.
Comparison of hospitalization and outcome variables among treatment groups.
| Variable, mean (SD) | Group I | Group II |
|---|---|---|
| Technical success of catheter placement | 100% | 100% |
| Success rate of management | 86% | 96% |
| LOS (d) | 26.1 (10.3) | 21.4 (8.2) |
| Duration of fever (d) | 5.5 (3.0) | 3.5 (2.1) |
| Converted into further surgery | 4 (14%) | 1 (4%) |
| With ongoing sepsis | 6 (20%) | 1 (4%) |
4. Discussion
Despite advances in diagnostic technology and new strategies for treatment, PLA remains a big therapeutic challenge. Conventional treatment of PLA is antibiotic therapy and image-guided percutaneous drainage or aspiration [16]. However, the study reported that percutaneous catheter drainage still has high failure rates, especially in patients with multiloculated PLA [8, 17]. The possible reason behind such high failure rate is either the presence of viscid pus within the abscesses or the inability of multiple small locals of the abscesses to fuse together and communicate with each other [2]. And no matter any intervention type for an abscess was used, the bacteria may release into the bloodstream [18]. Some studies have showed the chance of postprocedure sepsis after liver abscess drainage [7, 16, 19].
Our study used catheter drainage combined with ozone to improve the effects of treatment for multiloculated PLA and achieved relatively higher success rates (96%) than when using catheter drainage only [16, 20]. And the rates of ongoing sepsis and LOS were decreased significantly.
The operation of this study was carried out under CT guidance. CT imaging can more accurately display the lesion and the septae of the abscess, which is critical to the success rate of treatment. And we used a Seldinger technique which a guide wire was placed through abscess cavities; in this way, the septae of abscess may disrupt, and then the abscess can be drained more effectively. Through this method, compared with the standard catheter drainage treatment, we can get a better therapeutic effect. Abscesses with small collections and with presence of air as well as those closely abutting the diaphragm are poorly defined on US. CT imaging was found to be superior in depicting such abscesses [21].
Clinical application has proven that ozone is a powerful and reliable antimicrobial agent and can inactivate bacteria, fungi, protozoa, and viruses [12, 22, 23]. From a century ago, ozone therapy has been widely used and studied. Its mechanism action is through stimulating the oxygen metabolism and the immune system of bacteria, viruses, fungi, yeast, and protozoa, to achieve inactivation [12, 22, 23].
Using antibiotics only sometimes cannot achieve satisfactory results as most multiloculated PLA patients have mixed infections. In addition, long-term use of antibiotics can lead to bacterial resistance [2, 6, 24]. And the excess and indiscriminate use of antimicrobial drugs appears to be the most significant factor in the emergence of resistant microorganisms in recent years. In 2016, a global alliance consists of a multidisciplinary task force from 79 different countries developing a consensus on the rational use of antimicrobials for patients with intra-abdominal infections (IAIs). The consensus demonstrates the necessity of a multidisciplinary and collaborative approach in the battle against antimicrobial resistance in surgical infections. The use of ozone as a secondary antibacterial agent to treat multiloculated PLA has achieved a better effect.
Identifying pathogenic organisms has a great clinical importance. Experiences, however, have shown that this was not always possible because many patients were treated before fluid was obtained for culture [2]. Therefore, the blood culture of some patients in two groups of our study was negative. We observe that commonest organism in our study is neither Klebsiella nor E. coli and this is contradictory to global reports [25]. Prophylactic antibiotics for E. coli are usually used in clinical practice in our institution. This may result in negative bacteria culture in some patients who were originally infected with E. coli. There was a decreased mortality in culture negative PLA patients who receive percutaneous drainage. And there was no difference in outcomes of percutaneous drainage between E. coli PLA and Klebsiella PLA.
The study found that the beneficial effects of ozone on the wound healing might be assumed due to increased oxygen tension by ozone exposure in the wound area and then ameliorated impaired wounds healing [23]. Another study reported that ozone exposure could activate transcription factors. And this is important to adjust inflammatory reactions and eventually the whole process of wounds healing [22]. Therefore, ozone has also been used empirically as a clinical therapeutic agent for chronic wounds, such as ischemic ulcers, trophic ulcers, and diabetic wounds [26]. Furthermore, ozone can be dispersed into the cavity of the abscess, causing abscess wall dehydration [15]. Moreover, injection of ozone can break the septae of abscess and separate the adhesion in abscess cavity to make the drainage more effective (Figure 2) [12]. So the use of drainage combined with ozone has a synergistic effect on the management of liver abscess.
The categories of PLA often included biliary infection, portal vein seeding, direct extension, hepatic arterial seeding, penetrating trauma, and cryptogenic cause [25]. In our study, the biliary obstruction with cholangitis is the most common cause of PLA. Some complications from catheter drainage, such as hemorrhage owing to intercostal vessel and liver parenchyma injury, catheter-related pain, and subcutaneous emphysema, have been reported [11]. In this study, we did not encounter any serious complications. And there was no significant clinical bleeding noted in any patient in groups I and II.
5. Conclusions
In short, combined treatment of catheter drainage and ozone is a safe and valid therapeutic procedure in multiloculated PLA. This technology can decrease the ratio of surgical interventions and the LOS and should be confirmed with a larger patient series in other medical institutions.
Abbreviations
- PLA:
Pyogenic liver abscess
- LOS:
Length of stay
- PCD:
Percutaneous drainage catheter
- WBC:
White blood cell count.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Authors' Contributions
Han Feng Yang and Bing Li designed the study. Bing Li performed percutaneous drainage. Bing Li, Yang Li, Chuan Zhang, Lang Wang, and Chuan Liu performed examinations and collected the date. Han Feng Yang, Yong Du, and Xiao-xue Xu contributed to the analysis and supervised the report. Bing Li and Han Feng Yang wrote this paper together. Bing Li, Xiao-xue Xu, and Chuan Liu revised the paper.
References
- 1.Dulku G., Mohan G., Samuelson S., Ferguson J., Tibballs J. Percutaneous aspiration versus catheter drainage of liver abscess: A retrospective review. Australasian Medical Journal. 2015;8(1):7–18. doi: 10.4066/AMJ.2015.2240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jun C. H., Yoon J. H., Wi J. W., et al. Risk factors and clinical outcomes for spontaneous rupture of pyogenic liver abscess. Journal of Digestive Diseases. 2015;16(1):31–36. doi: 10.1111/1751-2980.12209. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed S., Chia C. L. K., Junnarkar S. P., Woon W., Shelat V. G. Percutaneous drainage for giant pyogenic liver abscess - Is it safe and sufficient? The American Journal of Surgery. 2016;211(1):95–101. doi: 10.1016/j.amjsurg.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Lai K.-C., Cheng K.-S., Jeng L.-B., et al. Factors associated with treatment failure of percutaneous catheter drainage for pyogenic liver abscess in patients with hepatobiliary-pancreatic cancer. The American Journal of Surgery. 2013;205(1):52–57. doi: 10.1016/j.amjsurg.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 5.Liao W.-I., Tsai S.-H., Yu C.-Y., et al. Pyogenic liver abscess treated by percutaneous catheter drainage: MDCT measurement for treatment outcome. European Journal of Radiology. 2012;81(4):609–615. doi: 10.1016/j.ejrad.2011.01.036. [DOI] [PubMed] [Google Scholar]
- 6.Srivastava A., Yachha S. K., Arora V., Poddar U., Lal R., Baijal S. S. Identification of high-risk group and therapeutic options in children with liver abscess. European Journal of Pediatrics. 2012;171(1):33–41. doi: 10.1007/s00431-011-1481-y. [DOI] [PubMed] [Google Scholar]
- 7.Liu C.-H., Gervais D. A., Hahn P. F., Arellano R. S., Uppot R. N., Mueller P. R. Percutaneous Hepatic Abscess Drainage: Do Multiple Abscesses or Multiloculated Abscesses Preclude Drainage or Affect Outcome? Journal of Vascular and Interventional Radiology. 2009;20(8):1059–1065. doi: 10.1016/j.jvir.2009.04.062. [DOI] [PubMed] [Google Scholar]
- 8.Chou F.-F., Sheen-Chen S.-M., Chen Y.-S., Chen M.-C. Single and multiple pyogenic liver abscesses: Clinical course, etiology, and results of treatment. World Journal of Surgery. 1997;21(4):384–389. doi: 10.1007/PL00012258. [DOI] [PubMed] [Google Scholar]
- 9.Giorgio A., De Stefano G., Di Sarno A., Liorre G., Ferraioli G. Percutaneous needle aspiration of multiple pyogenic abscesses of the liver: 13-Year single-center experience. American Journal of Roentgenology. 2006;187(6):1585–1590. doi: 10.2214/AJR.05.1104. [DOI] [PubMed] [Google Scholar]
- 10.Luo M., Yang X.-X., Tan B., et al. Distribution of common pathogens in patients with pyogenic liver abscess in China: a meta-analysis. European Journal of Clinical Microbiology & Infectious Diseases. 2016;35(10):1557–1565. doi: 10.1007/s10096-016-2712-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cioffi L., Belli A., Limongelli P., et al. Laparoscopic Drainage as First Line Treatment for Complex Pyogenic Liver Abscesses. Hepato-Gastroenterology. 2014;61(131):771–775. [PubMed] [Google Scholar]
- 12.Li B., Liu C., Li Y., et al. Computed tomography-guided catheter drainage with urokinase and ozone in management of empyema. World Journal of Radiology. 2017;9(4):212–216. doi: 10.4329/wjr.v9.i4.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andreula C. Ozone therapy. Neuroradiology. 2011;53(Supplement 1):S207–S209. doi: 10.1007/s00234-011-0930-7. [DOI] [PubMed] [Google Scholar]
- 14.Li B., Xu X. X., Du Y., et al. CT-guided chemonucleolysis combined with psoas compartment block in lumbar disc herniation: A randomized controlled study. Pain Medicine. 2014;15(9):1470–1476. doi: 10.1111/pme.12491. [DOI] [PubMed] [Google Scholar]
- 15.Re L., Rowen R., Travagli V. Ozone Therapy and Its Use in Medicine: Further Comments. Cardiology (Switzerland) 2017;136(4):p. 269. doi: 10.1159/000452618. [DOI] [PubMed] [Google Scholar]
- 16.Thomas J., Turner S. R., Nelson R. C., Paulson E. K. Postprocedure sepsis in imaging-guided percutaneous hepatic abscess drainage: How often does it occur? American Journal of Roentgenology. 2006;186(5):1419–1422. doi: 10.2214/AJR.04.1914. [DOI] [PubMed] [Google Scholar]
- 17.Chen S.-C., Lee Y.-T., Tsai S.-J., et al. Clinical Outcomes and Prognostic Factors of Cancer Patients with Pyogenic Liver Abscess. Journal of Gastrointestinal Surgery. 2011;15(11):2036–2043. doi: 10.1007/s11605-011-1650-3. [DOI] [PubMed] [Google Scholar]
- 18.Sharma N., Kaur H., Kalra N., Bhalla A., Kumar S., Singh V. Complications of Catheter Drainage for Amoebic Liver Abscess. Journal of Clinical and Experimental Hepatology. 2015;5(3):256–258. doi: 10.1016/j.jceh.2015.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kusumoto K., Hamada A., Kusaka T., et al. A patient with sepsis and a gas-forming liver abscess caused by Clostridium perfringens treated with continuous perfusion drainage. Nihon Shokakibyo Gakkai Zasshi. 2014;111(7):1416–1423. [PubMed] [Google Scholar]
- 20.Bari S., Sheikh K. A., Malik A. A., Wani R. A., Naqash S. H. Percutaneous aspiration versus open drainage of liver abscess in children. Pediatric Surgery International. 2007;23(1):69–74. doi: 10.1007/s00383-006-1812-7. [DOI] [PubMed] [Google Scholar]
- 21.Takeuchi Y., Okabe H., Myojo S., Fujimoto S. CT-guided drainage of a mediastinal pancreatic pseudocyst with a transhepatic transdiaphragmatic approach. Hepato-Gastroenterology. 2002;49(43):271–272. [PubMed] [Google Scholar]
- 22.Elvis A. M., Ekta J. S. Ozone therapy: a clinical review. Journal of Natural Science, Biology and Medicine. 2011;2(1):66–70. doi: 10.4103/0976-9668.82319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta G., Mansi B. Ozone therapy in periodontics. Journal of Medicine and Life. 2012;5(1):59–67. [PMC free article] [PubMed] [Google Scholar]
- 24.Lo J. Z. W., Leow J. J. J., Ng P. L. F., et al. Predictors of therapy failure in a series of 741 adult pyogenic liver abscesses. Journal of Hepato-Biliary-Pancreatic Sciences. 2015;22(2):156–165. doi: 10.1002/jhbp.174. [DOI] [PubMed] [Google Scholar]
- 25.Webb G. J., Chapman T. P., Cadman P. J., Gorard D. A. Pyogenic liver abscess. Frontline Gastroenterology. 2013;5(1):60–67. doi: 10.1136/flgastro-2013-100371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yu G., Liu X., Chen Z. Ozone therapy could attenuate tubulointerstitial injury in adenine-induced CKD rats by mediating Nrf2 and NF-kappaB. Iranian Journal of Basic Medical Sciences. 2016;19(10):1136–1143. [PMC free article] [PubMed] [Google Scholar]